Abstract
The longevity of conventional particulate filler resin composite (PFC) is uncertain in large restorations with high occlusal stresses. From a biomimetic point of view, the use of short fiber-reinforced resin composite (SFRC) as bulk dentin-replacing material appears a promising treatment strategy and may solve some potential problems associated with conventional PFC restoration in high stress-bearing areas. This chapter briefly presents the theoretical background, benefits, and clinical applications of SFRC in dentistry. Using clinical cases, with packable and flowable versions of SFRC (everX Posterior and everX Flow, GC Corporation, Tokyo, Japan) as bulk fill dentine-replacing material or thick core under surface layer of enamel-replacing PFC, i.e., biomimetic or bilayered composite restorations, to improve the load-bearing capacity and clinical longevity of resin-based composite restorations.
Within the limitations of this case series of clinical indications, the presented restorative approach is a promising and cost-efficient way to extend the indication range of direct resin composite restorations and gives the clinician alternative treatment options.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Large restoration
- Biomimetic approach
- Short fiber-reinforced composite
- Dentine-replacing material
- Restorative dentistry
7.1 Introduction
Direct conventional resin composite restorations, i.e., particulate filler resin composite (PFC) restorations are a routine approach of treating lost tooth structure conservatively. Beside the ability to bond to hard tooth tissues, mediated by adhesive systems, they feature the advantage of natural shade and are less expensive compared with cast gold and ceramic indirect restorations [1]. The use of resin composites has increased tremendously during the last two decades. Today, resin composites are selected on a regular basis for direct (bulk fill or layered) and laboratory made posterior restorations, as an extension to their original indication, which was limited to direct restorations in anterior teeth. Their use has been widened not only to the posterior intra-coronal area, but also to extra-coronal restorations [2]. In addition, resin composites are used for the fabrication of resin-bonded fixed dental prostheses (RBFDP) following the introduction of fiber-reinforced composites (FRC). However, inadequate material properties limited the success of resin composite restorations in high stress-bearing areas [3, 4]. Resin composites were introduced to the dental community in the 1960s [5]. Since then, significant material improvements have been introduced. However, resin composite still suffers from a lack of mechanical properties and polymerization shrinkage. Resin composite restorations have shown good overall clinical performance in small and medium sized posterior restorations with annual failure rates between 1% and 3% [3, 6]. Secondary caries and fracture are among the most important reasons for clinical failure [6, 7]. Survival of posterior restorations strongly correlates with the size of the restorations. Bernardo et al. reported an increase in annual failure rate from 0.95% for single-surface restorations to 9.43% for four or more surface restorations [8]. Large restorations were more prone to fracture-related failures resulting in decreased longevity [9, 10]. The higher susceptibility of large resin composite restorations to fracture may be related to the use of glass-ionomer lining material, strength-related properties of the resin composite material itself and patient factors such as bruxism [6, 11]. Besides restoration size the endodontic status of a tooth strongly affects the longevity of resin composite restorations. Clinical studies revealed a decreased longevity for resin composite restorations in endodontically treated teeth, with an increased annual failure rate of 2–12.4% when compared to vital teeth [6, 12]. Furthermore, non-vital teeth are susceptible to unfavorable subgingival cusp fractures [13]. The above-mentioned reasons make the restoration of endodontically treated teeth a true challenge.
It is clear from the literature that contemporary resin composites still demonstrate limitations due to their insufficient mechanical properties when used in large restorations. Due to failures of this kind, it is still controversial, whether restorative resin composites should be used in large high stress-bearing applications such as in direct posterior restorations or core build-ups [3, 14]. The relatively high brittleness and low fracture toughness of current PFCs still hinder their use in these large stress-bearing restorations [15, 16]. Appropriate physical and mechanical properties and satisfactory esthetic are all characteristics that restorative resin composite should achieve.
7.2 Biomimetic Dentistry
Contemporary restorative dentistry uses direct, semi-direct as well as indirect restorations to restore lost tooth tissue with biomimetics as the new driving force. Biomimetic dentistry tries to mimic nature by studying the structure, function and biology of the tooth organ as a model for the design and engineering of new or improved materials and techniques to restore or replace teeth in biomechanically optimal way [17]. From a biomimetic point of view, we strive to replace lost tooth tissue by biomaterials with similar physical properties, especially with reference to fracture toughness, elastic modulus, strength, and thermal expansion coefficient [18, 19]. A well accepted biomimetic restorative approach advocates replacing enamel with feldspathic porcelain or glass ceramic and dentine by conventional PFCs [19, 20]. Although such approach seems effective, there are still relevant mechanical properties, such as fracture toughness, not considered. Fracture toughness of PFC is still lower than that of dentine [1]. Furthermore, the microstructure of PFC does not resemble that of dentine. PFC consists of filler particles embedded in a resin matrix while dentine consists of collagen fibers embedded in a hydroxyapatite matrix. Therefore, dentine should be rather seen as a fiber-reinforced composite. Collagen fibers act as crack stopper and gives dentine unique properties by making it resilient, flexible and tough at the same time. For that reason, improvement might be found when taking advantage of a more dentine-like and high toughness resin composite as dentine replacement.
Extensive research has been conducted to improve the reinforcing phase of restorative PFC in order to increase their suitability for use in high stress-bearing areas. Attempts have been made to change the type of filler or the filler size and their silanization [21,22,23,24,25,26]. Reinforcing the resin composite with short glass fibers has been one of the most effective approaches among the methods that have been studied [23, 27, 28]. Short fibers enhanced the ability of the material to resist the crack propagation, as well as to reduce the stress intensity at the crack tip from which a crack propagates in an unstable manner. As a consequence, an increased resin composite toughness should be expected. A number of manufacturers have developed short fiber-reinforced composites (SFRCs) which claimed to overcome the weakness of conventional PFC (Table 7.1). However, comparative studies from the literature showed that commercial SFRCs have different properties, structures, and reinforcing capacities [29, 30]. Recent studies showed that millimeter and micrometer scales SFRCs (everX Posterior and everX Flow; GC Corporation) had a significant superior fracture toughness and reinforcing capability when compared to other commercial SFRCs (Alert, NovaPro-Flow, NovaPro-Fill, EasyCore, Build-It and TI-Core) [29, 30]. Based on this, everX Posterior and everX Flow are the most interesting dentine-replacing materials because of their close resemblance to dentine at the level of microstructure and mechanical properties [18, 31, 32].
7.3 Structure and Properties
Many of the properties of SFRCs are strongly dependent on microstructural parameters such as fiber diameter, fiber length, fiber orientation, fiber loading, and adhesion of fibers to the polymer matrix [33]. For a fiber to act as an effective reinforcement for polymers, stress transfer from the polymer matrix to the fibers is essential [33]. This is achieved by having a fiber length equal to or greater than the critical fiber length and the given fiber aspect ratio in the range of 30–94 [33,34,35]. Aspect ratio, critical fiber length, and fiber loading are the main factors that could improve or impair the mechanical properties of SFRCs. Aspect ratio is the fiber length to fiber diameter ratio (l/d). It affects the tensile strength and the reinforcing efficiency of the fiber-reinforced material [33]. It should be noted that adhesion of the fibers to the polymer matrix also influences to the critical fiber length. Sufficient adhesion between fiber and matrix provides good load transfer between the two components, which ensures that the load is transferred to the stronger fiber, and this is how the fiber actually works as reinforcement. However, if the adhesion is not strong and if any voids appear between the fiber and the polymer matrix, these voids may act as initial fracture sites in the matrix and facilitate the breakdown of the material [36].
For instance, Alert has fiber length in micrometer scale (20–60 μm) and diameter of 7 μm (Fig. 7.1), while NovaPro composites have fiber diameter in nanometer scale (50–200 nm) and length in range between 100 and 150 μm, which is well below the critical fiber length and desired aspect ratio [30]. This explained the difference in fracture toughness values between the commercial SFRCs. These differences were seen by SEM analysis (Figs. 7.1 and 7.3), which prove that materials with different microstructure characteristic and fiber aspect ratio (length and diameter) could differ with regards to physical properties and toughness.
Earlier formulations of SFRC showed a high failure rate due to secondary caries and bulk fracture [37, 38]. Bulk fracture of earlier SFRC formulations was related to sub-optimal reinforcement of the polymer matrix by short fibers. These SFRCs did not fulfill the reinforcing requirements. Aspect ratio and critical fiber length have implications towards fracture toughness (KIc), a property of major influence on the clinical performance of a material [39]. Fracture toughness of earlier SFRC formulations is much lower than that of dentine [1].
Following this knowledge, a millimeter scales packable SFRC (everX Posterior) was launched in 2013. It consists of a combination of a resin matrix (24 wt%), randomly orientated E-glass fiber (9 wt%) and inorganic particulate fillers (67 wt%) [27, 34]. The resin matrix comprises cross-linked monomers bis-GMA and TEGDMA accompanied with linear PMMA. This combination of resins enables the formation of the semi interpenetrating polymer network (semi-IPN) during the polymerization of the material, which provides good bonding properties and improved toughness of the resin composite [36]. The short, randomly oriented fiber on the other hand, provide an isotropic reinforcing effect when placed in bulk, which means that the strength of the material is independent of the fracture load direction, i.e., it is the same in all directions. Nevertheless, in the origin isotropic SFRC material (3D fiber orientation and fiber reinforcing factor of 0.2) becomes anisotropic and subsequently more biomimetic when applied in incremental layers up to 2 mm thick, due to alignment of fibers in the plane of application (2D fiber orientation and fiber reinforcement factor of 0.38) [33].
In 2019, the flowable version of SFRC (everX Flow) was introduced with the promise of easy handling and better adaptability in limited spaces. It consists of a combination of a resin matrix (30 wt%), randomly orientated glass microfibers (25 wt%) and inorganic silanated particulate fillers (45 wt%) (Fig. 7.2) [40, 41].
The micrometer scale SFRC (everX Flow) had an aspect ratio of more than 30 because the diameter of microglass fibers used was 6 μm and the length in the range of 200–300 μm. everX Posterior had fiber (Ø17 μm) length distribution between 0.3 and 1.5 mm, which is in the range of the reported critical fiber length and desired aspect ratio (Fig. 7.3). It is therefore not surprising that everX Posterior and everX Flow have superior fracture toughness in comparison to all other commercial fiber filled resin composite.
These SFRCs were reported to exhibit improved mechanical properties regarding strength, fracture toughness, fatigue resistance, and polymerization shrinkage and to show a more favorable (repairable) type of failure behavior in comparison to PFCs [27, 28, 35, 40, 42,43,44,45]. The use of fiber fillers with a length in the range of the reported critical fiber length and desired aspect ratio, increased KIc of SFRCs up to 2.6–3.1 MPa m0.5 [35, 40, 46, 47] in comparison to 1.2–1.8 MPa m0.5 of conventional PFC [48]. Therefore, it can be hypothesized that the replacement of dentine by a high toughness SFRCs can reduce bulk fractures and therefore increase longevity of large resin composite restorations.
There is little evidence comparing bond durability of SFRC to dentine with that of other conventional PFCs [49, 50]. A study by Tsujimoto et al. determined that the relationship between mechanical properties and dentine bond durability of SFRC using universal adhesives showed improvements compared to conventional PFCs [49]. Regardless of adhesive type and etching modes, the ratios of shear fatigue strength and shear bond strength of SFRC were higher than those of conventional PFCs. The authors clarified that superior mechanical properties of SFRC, especially fracture toughness, could improve its bond durability with universal adhesives [49, 50]. Studies have debated if short fibers might have a reinforcing effect on the oxygen-inhibited layer of the adhesive and they emphasized that, with enhanced mechanical properties and bond durability, SFRC might perform better in high stress-bearing situations.
Curiously, SFRCs have the ability to conduct and scatter the curing light better than conventional PFCs and thus it is suitable for use in bulk of 4–5 mm layer thickness [40, 51, 52]. Surface roughness, wear and esthetic related limitations of SFRCs can be overcome by adopting a biomimetic restorative approach, in which dentine is replaced by SFRC and covered by a more wear-resistant PFC [1, 18]. Such approach not only has the benefits of better wear resistance but also increased strength and fatigue resistance. SFRCs are suitable as a bulk base or core foundation and should not be used as final restoration. Although, microfibers filler loading was not seen to be worsening the wear or the gloss of the flowable SFRC (everX Flow) [40, 53]. Clinically, it is widely recommended nowadays to use a layer of composite bulk base (dentine replacing) material in order to improve the esthetic, to reduce the polymerization stress and to develop better mechanical properties [54]. The latter is accomplished by decreasing the tensile stress concentrations at the restoration interface and reducing the cuspal strain [54]. Published clinical results of bilayered restorations (Fig. 7.4) containing SFRC as bulk composite base in high stress-bearing areas have shown good clinical performance. However, the time frame and case numbers for these clinical trials were not of such duration and number as to indicate the long-term suitability of the tested restorations [55,56,57].
7.4 Benefits of Using SFRCs as Bulk
Bilayered composite structure of SFRC as substructure and PFC as top surface layer (Fig. 7.4) has been evaluated in several in vitro investigations and with different applications [58,59,60,61,62,63]. SFRC base has already been used to reinforce large direct composites restorations in vital teeth [64,65,66,67,68] as well as in endodontically treated teeth [69,70,71,72,73], as prosthesis infrastructure [74,75,76,77,78], onlay restorations [59, 79], and endodontic post/core foundations [70,71,72,73].
The effect of the thickness of the SFRC substructure versus the thickness of the overlaying PFC, static and fatigue load-bearing capacity of materials combination and the interface between SFRC and PFC are among the issues that have been studied [21, 22, 80, 81].
These studies demonstrate that SFRC substructure supports the PFC layer and serve as a crack preventative layer. SFRC substructure’s thickness is important, as it influences the failure mode and the crack arresting mechanism. The mechanism of arresting the crack propagation is greatly influenced by the distance between the SFRC substructure and the surface where the stress initiates. The applied SFRC and PFC layers thickness is extremely important. The ratio between the SFRC base and surface PFC should be an analogue to the dentine and enamel structure. In vitro it was observed that optimal thickness of the veneering PFC composite over the SFRC substructure is around 1 mm [21, 22, 80]. It is important to point out that less benefit is achieved if the layer of SFRC is not sufficiently thick [77, 81]. Other advantages of SFRC-based biomimetic restorations can be seen at the level of the interface between SFRC and PFC [82, 83]. After application of the SFRC layer some fibers are protruding from the surface which can be embedded in the veneering PFC layer and form an interface similar to that found at the dentine-enamel junction (DEJ). At the DEJ, collagen fiber originating from dentine extends into enamel creating a fiber-reinforced connection between enamel and dentine. It is known that the microscopic architecture and the unique mechanical properties of the DEJ acts as a natural crack arrest barrier [84].
Theoretically, the significant advantage of this bilayered or biomimetic restoration is their ability to mimic the natural behavior of enamel and dentine. To the author’s knowledge, these SFRCs are the only available resin composites that mimics structurally the dentine at this time.
7.5 Clinical Use of SFRCs
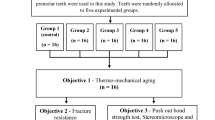
In this series of clinical cases an attempt was made by using SFRCs as bulk base or core material under surface layer of conventional PFC, i.e., direct biomimetic or bilayered composite restorations, in order to improve the load-bearing capacity and clinical longevity of resin-based composite restorations.
7.5.1 Clinical Case: everX Posterior
A 49-year-old male presented with a defective Class II amalgam restoration and a primary carious lesion on a lower second premolar (FDI #45) (Fig. 7.5a). The old restoration was removed using a pear-shaped diamond bur (830 L; Komet) in a high-speed air turbine. Dental dam was placed after opening the cavity, in order to obtain a dry working field. The minimal invasive cavity was cleaned by sandblasting with 50 μm alumina particles. A three-step etch-and-rinse adhesive (Optibond FL, Kerr) was applied according to manufacturer’s instructions. The resin composite was placed following an incremental filling technique and interproximal contacts were restored by use of metal sectional matrices in combination with separation rings (V3 matrix and ring, Triodent) (Fig. 7.5b). The centripetal filling technique was adopted to transform the three-surface cavity into a single-surface cavity (Fig. 7.5c): a first 1 mm thick layer of hybrid composite (Filtek Supreme XTE; 3 M ESPE) was placed towards the matrix and the subsequent layers (2 mm thick) of SFRC (everX Posterior; GC) were placed oblique (Fig. 7.5d). The biomimetic restoration was finalized by placing a final 1.5 mm thick increment of hybrid composite at the occlusal surface. Each increment of resin composite was light-cured with an LED-curing unit (The cure; Spring Health Products) for 40 s. Additional post-curing from the buccal and lingual aspect was performed after matrix removal. Occlusion and articulation were checked and adjusted after removal of the dental dam. The restoration was finished with fine-grit diamond burs (8862 and 862EF; Komet), abrasive discs (OptiDisc; KerrHawe) and strips (Sof-Lex strips; 3 M ESPE) and polished with rubbers (HiLuster; KerrHawe) and brushes (OccluBrush; KerrHawe) (Fig. 7.5e).
(a) Pre-operative view: Clinical view of a defective amalgam restoration in combination with a primary carious lesion at the mesial wall. (b) After removal of the old restoration and the carious lesion a dental dam is placed and countered sectional metal matrices in combination with a separation ring. (c) Interproximal walls were build-up by PFC according to a centripetal filling technique. (d) Missing dentine replaced by a semi-IPN-based bulk short fiber composite base (notice protruding fibers from the SFRC surface). (e) Post-operative view: The occlusal part is build-up with hybrid composite and the restoration is finished and adjusted in occlusion
7.5.2 Clinical Case: everX Flow
A female patient presented with secondary caries due to a defective Class II amalgam restoration on a lower first molar (FDI #36). This case was treated according to the same principles and protocol as the previous case. The main difference between this and the previous case was the SFRC used, a flowable SFRC (everX Flow) instead of packable SFRC (everX Posterior) for replacing the lost dentine tissue (Fig. 7.6a–f).
(a) Pre-operative view: Clinical view of a defective amalgam restoration and secondary caries on the lower first molar (FDI #36). (b) Countered sectional metal matrices in combination with a separation ring is placed in order to rebuild the distal wall, a part of the buccal cusp and the lingual cusp. (c) Centripetal filling technique is used to rebuild the missing distal wall and lingual cusp with several portions of enamel-replacing PFC. (d) A flowable SFRC (everX Flow) is applied in several increments to replace the missing dentine. (e, f) post-operative view: A nanohybrid composite is selected to restore the occlusal part of the tooth
7.6 Conclusion and Future Trends
Many clinical studies for direct and indirect large posterior composite restorations have identified that fracture of the restoration was the most common reason for failure with no significant differences between the two techniques. It is hypothesized that using SFRC substructure could reinforce the composite restoration for use in high stress-bearing areas of the dental arch. The function of the bulk SFRC base is assumed to be based on supporting the superficial conventional PFC and behaving as a crack arrest barrier. In other words, it mimics the natural behavior of enamel and dentine. The present chapter briefly described the structure, properties and benefits of using SFRC in many clinical situations. Within the limitations of this case series of clinical indications, SFRCs are a promising material that give the clinician the opportunity to replace missing tooth tissue in a more biomimetic way. Therefore, SFRCs can be beneficial in large stress-bearing restorations as a dentine-replacing materials, resulting into less fracture-related failures and improving overall longevity of direct and indirect resin composite restorations. Long-term clinical studies are currently in progress to determine the value and usefulness of using bilayered or biomimetic composite restorations made of a high toughness dentine-replacing SFRC and a wear-resistant and highly esthetic PFC as enamel-replacement in high stress-bearing areas.
Future developments in short fiber reinforcement technology are focused now on the optimization of the SFRC CAD/CAM blocks [85,86,87] and SFRC as 3D printing material, in order to have bilayered composite restorations. Efforts to get even closer in producing a material suitable to replace lost dentine include the investigation of using nanofibers and a compositions and structure closer to an apatite minerals in order to enhance the performance resin composite.
References
Manhart J, Kunzelmann KH, Chen HY, Hickel R. Mechanical properties and wear behavior of light-cured packable composite resins. Dent Mater. 2000;16:33–40.
Fennis WM, Kuijs RH, Roeters FJ, Creugers NH, Kreulen CM. Randomized control trial of composite cuspal restorations: five-year results. J Dent Res. 2014;93:36–41. https://doi.org/10.1177/0022034513510946.
Manhart J, Chen H, Hamm G, Hickel R. Buonocore memorial lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004;29:481–508.
Wilder AD, May KN, Bayne SC, Taylor DF, Leinfelder KF. Seventeen-year clinical study of ultraviolet-cured posterior composite class I and II restorations. J Esthet Dent. 1999;11:135–42.
Bowen RL. Properties of a silica-reinforced polymer for dental restorations. J Am Dent Assoc. 1963;66:57–64.
Demarco FF, Corrêa MB, Cenci MS, Moraes RR, Opdam NJM. Longevity of posterior composite restorations: not only a matter of materials. Dent Mater. 2012;28:87–101. https://doi.org/10.1016/j.dental.2011.09.003.
Brunthaler A, Konig F, Lucas T, Sperr W, Schedle A. Longevity of direct resin composite restorations in posterior teeth. Clin Oral Investig. 2003;7:63–70. https://doi.org/10.1007/s00784-003-0206-7.
Bernardo M, Luis H, Martin MD, Leroux BG, Rue T, Leitao J, DeRouen TA. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138:775–83. https://doi.org/10.14219/jada.archive.2007.0265.
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. A retrospective clinical study on longevity of posterior composite and amalgam restorations. Dent Mater. 2007;23:2–8. https://doi.org/10.1016/j.dental.2005.11.036.
Van Nieuwenhuysen JP, D’Hoore W, Carvalho J, Qvist V. Long-term evaluation of extensive restorations in permanent teeth. J Dent. 2003;31:395–405.
Opdam NJ, Bronkhorst EM, Roeters JM, Loomans BA. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent. 2007;9:469–75.
Lempel E, Lovász BV, Bihari E, Krajczar K, Jeges S, Toth A, Szalma J. Long-term clinical evaluation of direct resin composite restorations in vital vs. endodontically treated posterior teeth-retrospective study up to 13 years. Dent Mater. 2019;35(9):1308–18. https://doi.org/10.1016/j.dental.2019.06.002.
Fennis WM, Kuijs RH, Kreulen C, Roeters FJ, Creugers NH, Burgersdijk RC. A survey of cusp fractures in a population of general dental practices. Int J Prosthodont. 2002;15:559–63.
Roulet J-F. Benefits and disadvantages of tooth-coloured alternatives to amalgam. J Dent. 1997;25:459–73. https://doi.org/10.1016/S0300-5712(96)00066-8.
Wilder AJ, Bayne S, Ho H. Long-term clinical oerformance of direct posterior composites. Trans Acad Dent Mater. 1996;9:151–69.
Xu HH. Dental composite resins containing silica-fused ceramic single-crystalline whiskers with various filler levels. J Dent Res. 1999;78:1304–11.
Magne P. Pascal Magne: “it should not be about aesthetics but tooth-conserving dentistry”. Interview by Ruth Doherty. Br Dent J. 2012;213:189–91. https://doi.org/10.1038/sj.bdj.2012.769.
Keulemans F, Garoushi S, Lassila L. Fillings and core-built ups. In: Vallittu, Özcan, editors. A clinical guide to principles of fiber reinforced composites (FRCs) in dentistry. Cambridge: Woodhead Publishing; 2017.
Magne P, Belser U. Understanding the intact tooth and the biomimetic principle. In: Magne P, Belser U, editors. Bonded porcelain restorations in the anterior dentition: a biomimetic approach. Chicago: Quintessence Publishing Co; 2002. p. 23–55.
Magne P. Composite resins and bonded porcelain: the postamalgam era? J Calif Dent Assoc. 2006;34:135–47.
Garoushi S, Lassila LV, Tezvergil A, Vallittu PK. Load bearing capacity of fiber-reinforced and particulate filler composite resin combination. J Dent. 2006;34:179–84.
Garoushi S, Lassila LVJ, Tezvergil A, Vallittu PK. Static and fatigue compression test for particulate filler composite resin with fiber-reinforced composite substructure. Dent Mater. 2007;23:17–23. https://doi.org/10.1016/j.dental.2005.11.041.
Garoushi S, Vallittu PK, Lassila LV. Short glass fiber reinforced restorative composite resin with semi-inter penetrating polymer network matrix. Dent Mater. 2007;23:1356–62.
Xu HH, Quinn JB, Smith DT, Giuseppetti AA, Eichmiller FC. Effects of different whiskers on the reinforcement of dental resin composites. Dent Mater. 2003;19:359–67. https://doi.org/10.1016/S0109-5641(02)00078-7.
Zandinejad AA, Atai M, Pahlevan A. The effect of ceramic and porous fillers on the mechanical properties of experimental dental composites. Dent Mater. 2006;22:382–7. https://doi.org/10.1016/j.dental.2005.04.027.
Ferracane JL, Berge HX, Condon JR. In vitro aging of dental composites in water—effect of degree of conversion, filler volume, and filler/matrix coupling. J Biomed Mater Res. 1998;42:465–72.
Garoushi S, Sailynoja E, Vallittu PK, Lassila L. Physical properties and depth of cure of a new short fiber reinforced composite. Dent Mater. 2013;29:835–41. https://doi.org/10.1016/j.dental.2013.04.016.
Garoushi S, Vallittu PK, Watts DC, Lassila LV. Polymerization shrinkage of experimental short glass fiber-reinforced composite with semi-inter penetrating polymer network matrix. Dent Mater. 2008;24(2):211–5.
Garoushi S, Vallittu PK, Lassila L. Mechanical properties and wear of five commercial fiber-reinforced filling materials. Chin J Dent Res. 2017;20(3):137–43.
Lassila L, Keulemans F, Vallittu PK, Garoushi S. Characterization of restorative short-fiber reinforced dental composites. Dent Mater J. 2020;39(6):992–9.
Garoushi S, Gargoum A, Vallittu PK, Lassila L. Short fiber-reinforced composite restorations: a review of the current literature. J Investig Clin Dent. 2018;9(3):e12330. https://doi.org/10.1111/jicd.12330.
Garoushi S, Tanner J, Keulemans F, Le Bell-Rönnlöf AM, Lassila L, Vallittu PK. Fiber reinforcement of endodontically treated teeth: what options do we have? Literature review. Eur J Prosthodont Restor Dent. 2020;28(2):54–63.
Vallittu PK. High-aspect ratio fillers: fiber-reinforced composites and their anisotropic properties. Dent Mater. 2014;31:1–7. https://doi.org/10.1016/j.dental.2014.07.009.
Lassila L, Garoushi S, Vallittu PK, Säilynoja E. Mechanical properties of fiber reinforced restorative composite with two distinguished fiber length distribution. J Mech Behav Biomed Mater. 2016;60:331–8. https://doi.org/10.1016/j.jmbbm.2016.01.036.
Bijelic-Donova J, Garoushi S, Lassila LV, Keulemans F, Vallittu PK. Mechanical and structural characterization of discontinuous fiber-reinforced dental resin composite. J Dent. 2016;52:70–8.
Lastumäki TM, Lassila LV, Vallittu PK. The semi-interpenetrating polymer network matrix of fiber-reinforced composite and its effect on the surface adhesive properties. J Mater Sci Mater Med. 2003;14:803–9.
Fagundes TC, Barata TJ, Carvalho CA, Franco EB, van Dijken JW, Navarro MF. Clinical evaluation of two packable posterior composites: a five-year follow-up. J Am Dent Assoc. 2009;140:447–54. https://doi.org/10.14219/jada.archive.2009.0194. 140/4/447[pii]
van Dijken JW, Sunnegardh-Gronberg K. Fiber-reinforced packable resin composites in class II cavities. J Dent. 2006;34:763–9.
Heintze SD, Ilie N, Hickel R, Reis A, Loguercio A, Rousson V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-a systematic review. Dent Mater. 2017;33:101–14.
Lassila L, Säilynoja E, Prinssi R, Vallittu P, Garoushi S. Characterization of a new fiber-reinforced flowable composite. Odontology. 2019;107(3):342–52.
Garoushi S, Vallittu P, Lassila L. Mechanical properties and radiopacity of flowable fiber-reinforced composite. Dent Mater J. 2019;38(2):196–202.
Garoushi S, Vallittu PK, Lassila LV. Fracture toughness, compressive strength and load-bearing capacity of short glass fiber-reinforced composite resin. Chin J Dent Res. 2011;14:15–9.
Petersen RC. Discontinuous fiber-reinforced composites above critical length. J Dent Res. 2005;84:365–70.
Tiu J, Belli R, Lohbauer U. R-curve behavior of a short-fiber reinforced resin composite after water storage. J Mech Behav Biomed Mater. 2020;104:103674.
Tiu J, Belli R, Lohbauer U. Rising R-curves in particulate/fiber-reinforced resin composite layered systems. J Mech Behav Biomed Mater. 2020;103:103537.
Abouelleil H, Pradelle N, Villat C, Colon P, Grosgogeat B. Comparison of mechanical properties of a new fiber reinforced composite and bulk filling composites. Restor Dent Endod. 2015;7658:1–8.
Lassila L, Keulemans F, Säilynoja E, Vallittu PK, Garoushi S. Mechanical properties and fracture behavior of flowable fiber reinforced composite restorations. Dent Mater. 2018;34(4):598–606.
Ilie N, Hickel R, Valceanu AS, Huth KC. Fracture toughness of dental restorative materials. Clin Oral Investig. 2012;16:489–98. https://doi.org/10.1007/s00784-011-0525-z.
Tsujimoto A, Barkmeier WW, Takamizawa T, Watanabe H, Johnson WW, Latta MA, Miyazaki M. Relationship between mechanical properties and bond durability of short fiber-reinforced resin composite with universal adhesive. Eur J Oral Sci. 2016;124:480–9.
Omran TA, Garoushi S, Abdulmajeed AA, Lassila LV, Vallittu PK. Influence of increment thickness on dentin bond strength and light transmission of composite base materials. Clin Oral Investig. 2017;21(5):1717–24.
Garoushi S, Vallittu P, Shinya A, Lassila L. Influence of increment thickness on light transmission, degree of conversion and micro hardness of bulk fill composites. Odontology. 2015;104(3):291–7. https://doi.org/10.1007/s10266-015-0227-0.
Miletic V, Pongprueksa P, De., Munck, J., Brooks, N.R., Van., Meerbeek, B. Curing characteristics of flowable and sculptable bulk-fill composites. Clin Oral Investig. 2017;21(4):1201–12.
Lassila L, Säilynoja E, Prinssi R, Vallittu PK, Garoushi S. The effect of polishing protocol on surface gloss of different restorative resin composites. Biomater Investig Dent. 2020;7:1–8.
Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJP. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012;40:500–5. https://doi.org/10.1016/j.jdent.2012.02.015.
Garoushi S, Tanner J, Vallittu P, Lassila L. Preliminary clinical evaluation of short fiber-reinforced composite resin in posterior teeth: 12-months report. Open Dent J. 2012;6:41–5. https://doi.org/10.2174/1874210601206010041TODENTJ-6-41.
Tanner J, Tolvanen M, Garoushi S, Säilynoja E. Clinical evaluation of fiber-reinforced composite restorations in posterior teeth-results of 2.5 year follow-up. Open Dent J. 2018;12:476–85.
ElAziz RH, Mohammed MM, Gomaa HAF. Clinical performance of short-fiber-reinforced resin composite restorations vs resin composite onlay restorations in complex cavities of molars (randomized clinical trial). J Contemp Dent Pract. 2020;21(3):296–303.
Garoushi S, Vallittu PK, Lassila LV. Use of short fiber-reinforced composite with semi-interpenetrating polymer network matrix in fixed partial dentures. J Dent. 2007;35:403–8.
Garoushi SK, Lassila LV, Vallittu PK. Fiber-reinforced composite substructure: load-bearing capacity of an onlay restoration. Acta Odontol Scand. 2006;64:281–5.
Garoushi S, Vallittu PK, Lassila LV. Fracture resistance of short, randomly oriented, glass fiber-reinforced composite premolar crowns. Acta Biomater. 2007;3:779–84.
Garoushi S, Vallittu PK, Lassila LV. Direct restoration of severely damaged incisors using short fiber-reinforced composite resin. J Dent. 2007;35:731–6.
Garoushi SK, Hatem M, Lassila LVJ, Vallittu PK. The effect of short fiber composite base on microleakage and load-bearing capacity of posterior restorations. Acta Biomater Odontol Scand. 2015;1:6–12. https://doi.org/10.3109/23337931.2015.1017576.
Keulemans F, Palav P, Aboushelib MMN, van Dalen A, Kleverlaan CJ, Feilzer AJ. Fracture strength and fatigue resistance of dental resin-based composites. Dent Mater. 2009;25:1433–41. https://doi.org/10.1016/j.dental.2009.06.013.
Fráter M, Forster A, Keresztúri M, Braunitzer G, Nagy K. In vitro fracture resistance of molar teeth restored with a short fiber-reinforced composite material. J Dent. 2014;42:1143–50. https://doi.org/10.1016/j.jdent.2014.05.004.
Bijelic J, Garoushi S, Vallittu PK, Lassila LV. Short fiber reinforced composite in restoring severely damaged incisors. Acta Odontol Scand. 2013;71:1221–31. https://doi.org/10.3109/00016357.2012.757640.
Sáry T, Garoushi S, Braunitzer G, Alleman D, Volom A, Fráter M. Fracture behaviour of MOD restorations reinforced by various fiber-reinforced techniques—an in vitro study. J Mech Behav Biomed Mater. 2019;98:348–56. [published correction appears in J Mech Behav Biomed Mater. 2020 Feb;102:103505]. https://doi.org/10.1016/j.jmbbm.2019.07.006.
Szabó B, Garoushi S, Braunitzer G, Szabó PB, Baráth Z, Fráter M. Fracture behavior of root-amputated teeth at different amount of periodontal support—a preliminary in vitro study. BMC Oral Health. 2019;19(1):261. Published 2019 Nov 27. https://doi.org/10.1186/s12903-019-0958-3.
Garoushi S, Mangoush E, Vallittu PK, Lassila L. Short fiber reinforced composite: a new alternative for direct onlay restorations. Open Dent J. 2013;7:181–5. Published 2013 Dec 30. https://doi.org/10.2174/1874210601307010181.
Ozsevik AS, Yildirim C, Aydin U, Culha E, Surmelioglu D. Effect of fiber-reinforced composite on the fracture resistance of endodontically treated teeth. Aust Endod J. 2015;42(2):82–7. http://www.ncbi.nlm.nih.gov/pubmed/26611674. Accessed 5 Nov 16.
Fráter M, Sáry T, Néma V, Braunitzer G, Vallittu PK, Lassila L, Garoushi S. Fatigue failure load of immature anterior teeth: influence of different fiber post-core systems. Odontology. 2020;10:222–30. https://doi.org/10.1007/s10266-020-00522-y.
Lassila L, Oksanen V, Fráter M, Vallittu PK, Garoushi S. The influence of resin composite with high fiber aspect ratio on fracture resistance of severely damaged bovine incisors. Dent Mater J. 2020;39(3):381–8. https://doi.org/10.4012/dmj.2019-051.
Fráter M, Lassila L, Braunitzer G, Vallittu PK, Garoushi S. Fracture resistance and marginal gap formation of post-core restorations: influence of different fiber-reinforced composites. Clin Oral Investig. 2020;24(1):265–76.
Fráter M, Sáry T, Jókai B, Braunitzer G, Säilynoja E, Vallittu PK, Lassila L, Garoushi S. Fatigue behavior of endodontically treated premolars restored with different fiber-reinforced designs. Dent Mater. 2021;37(3):391–402.
Keulemans F, Van Dalen A, Kleverlaan CJ, Feilzer AJ. Static and dynamic failure load of fiber-reinforced composite and particulate filler composite cantilever resin-bonded fixed dental prostheses. J Adhes Dent. 2010;12:207–14. https://doi.org/10.3290/j.jad.a17653.
Keulemans F, De Jager N, Kleverlaan CJ, Feilzer AJ. Influence of retainer design on two-unit cantilever resin-bonded glass fiber reinforced composite fixed dental prostheses: an in vitro and finite element analysis study. J Adhes Dent. 2008;10:355–64.
Bijelic-Donova J, Garoushi S, Vallittu PK, Lassila LVJ. Mechanical properties, fracture resistance, and fatigue limits of short fiber reinforced dental composite resin. J Prosthet Dent. 2016;115:95–102. https://doi.org/10.1016/j.prosdent.2015.07.012.
Lassila L, Säilynoja E, Prinssi R, Vallittu PK, Garoushi S. Fracture behavior of bi-structure fiber-reinforced composite restorations. J Mech Behav Biomed Mater. 2020;101:103444. https://doi.org/10.1016/j.jmbbm.2019.103444.
Nagata K, Garoushi SK, Vallittu PK, Wakabayashi N, Takahashi H, Lassila LVJ. Fracture behavior of single-structure fiber-reinforced composite restorations. Acta Biomater Odontol Scand. 2016;2(1):118–24. Published 2016 Sep 5. https://doi.org/10.1080/23337931.2016.1224670.
Bijelic-Donova J, Keulemans F, Vallittu PK, Lassila LVJ. Direct bilayered biomimetic composite restoration: the effect of a cusp-supporting short fiber-reinforced base design on the chewing fracture resistance and failure mode of molars with or without endodontic treatment. J Mech Behav Biomed Mater. 2020;103:103554.
Lassila L, Säilynoja E, Prinssi R, Vallittu P, Garoushi S. Bilayered composite restoration: the effect of layer thickness on fracture behavior. Biomater Investig Dent. 2020;7(1):80–5.
Garoushi S, Sungur S, Boz Y, Ozkan P, Vallittu PK, Uctasli S, Lassila L. Influence of short-fiber composite base on fracture behavior of direct and indirect restorations. Clin Oral Investig. 2021;25(7):4543–52.
Omran TA, Garoushi S, Lassila L, Shinya A, Vallittu PK. Bonding interface affects the load-bearing capacity of bilayered composites. Dent Mater J. 2019;38(6):1002–11. https://doi.org/10.4012/dmj.2018-304.
Omran TA, Garoushi S, Lassila LV, Vallittu PK. Effect of interface surface design on the fracture behavior of bilayered composites. Eur J Oral Sci. 2019;127(3):276–84. https://doi.org/10.1111/eos.12617.
Imbeni V, Kruzic JJ, Marshall GW, Marshall SJ, Ritchie RO. The dentin-enamel junction and the fracture of human teeth. Nat Mater. 2005;4:229–32.
Mangoush E, Garoushi S, Vallittu PK, Lassila L. Influence of short fiber- reinforced composites on fracture resistance of single-structure restorations. Eur J Prosthodont Restor Dent. 2020;28(4):189–98.
Mangoush E, Lassila L, Vallittu PK, Garoushi S. Microstructure and surface characteristics of short-FIBER reinforced CAD/CAM composite blocks. Eur J Prosthodont Restor Dent. 2021;29(3).
Mangoush E, Lassila L, Vallittu PK, Garoushi S. Shear-bond strength and optical properties of short fiber-reinforced CAD/CAM composite blocks. Eur J Oral Sci. 2021;129(5):e12815.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Garoushi, S., Keulemans, F., Lassila, L., Vallittu, P.K. (2023). Short Fiber Based Filling Composites. In: Sabbagh, J., McConnell, R. (eds) Bulk Fill Resin Composites in Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-031-16388-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-031-16388-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-16387-6
Online ISBN: 978-3-031-16388-3
eBook Packages: MedicineMedicine (R0)