Summary
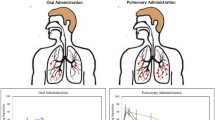
Tuberculosis (TB) is a historical disease that can trace its impact on humanity back in time thousands of years. A bacterial infection by Mycobacterium tuberculosis (M. tb) that primarily strikes the pulmonary system appears in patients as latent, active, drug-resistant, and multidrug-resistant forms. While regiments recommended by medical institutions focus primarily on tablets, inhalation offers an approach that should deliver lower doses resulting in lower side effects. This chapter will review different approaches to inhalation therapy over the past one hundred years and their impact on the different forms of M. tb infection. It will conclude by suggesting a method to apply specific dosages of a front-line anti-TB drug to treat latent, active, and resistant forms of M. tb using an electronic vaporization technique.
Graphical Abstract

Fatty acid (stearic acid) nanoparticles encasing isoniazid are pictured being inhaled by a patient (Made by Jenu Thomas Richardson)
In the mortality bills, pneumonia is an easy second, to tuberculosis; indeed, in many cities the death-rate is now higher and it has become, to use the phrase of Bunyan, ‘the Captain of the men of death.
William Osier
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mycobacterium tuberculosis
- Bacterial infection
- Delivery
- Inhalation therapy
- Inhalers
- Pulmonary tuberculosis
- Resistance
- Treatment
- Vaporization
1 Introduction
The inhalation of medicinal compounds has been tested and documented in the peer-reviewed scientific literature as a delivery method to rid a patient of Mycobacterium tuberculosis (M. tb) infection for over a century [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77]. M. tb infections have ravaged humanity for at least ten thousand years [76]. TB is spread through the air by someone expelling water droplets infected with M. tb through a cough or sneeze. Water droplets containing M. tb can float in the air for several hours, making it possible for someone else nearby to inhale the bacteria. The most common form of TB, pulmonary TB (PTB), occurs when the bacteria attack the lungs. Extrapulmonary TB (EPTB) occurs when the bacteria infect other parts of the body, including the brain [11]. Contradictory to PTB, EPTB is rarely transmitted to others. The combination of isoniazid (INH), rifampin (RIF), and other first- and second-line anti-TB medications, are widely used to treat M. tb infections and can take six to nine months to complete the regimen. Combination therapy reduces the risk of the bacteria becoming drug-resistant (DR) [4]. DR-TB is a type of infection in which the bacteria become resistant to the primary drugs used to treat TB. This condition can arise from improper use of medications and regimens and not completing the full course of treatment. Totally DR-TB and extensively drug-resistant (XDR) TB are the most severe forms of M. tb infections. Bacille Calmette-Guérin (BCG) is a vaccine used for TB but has limited efficacy. BCG is recommended for children and adults at an increased risk of infection or exposure to TB disease.
Infection by M. tb does not necessarily result in immediate disease expression. When a subject is infected, granulomas are formed around the bacterium [84] to isolate and prevent its growth. The human body is efficient in containing outbreaks of TB after infection by sealing the disease in lesions. Although the TB is contained, the body cannot eradicate it, so latent TB infection (LTBI), or inactive TB, is expressed once the immune system is compromised. This can be observed in the syndemic relationship between TB and HIV; HIV drastically weakens the immune system, causing a TB outbreak to proliferate. Tuberculin-based skin tests are used to test for TB in travelers. There are two types of TB tests that are economical and routinely utilized by medical professionals: the skin test and the blood test. A positive test indicates that the patient has been infected with the M. tb but does not determine whether or not it is latent or active TB. Further diagnostic tests are needed to determine whether TB is latent or active in the patient [10]. Lifestyle, as well as environmental factors, play a significant role in TB recovery. People with active TB self-quarantine to avoid infecting others. Patients may be recommended directly observed therapy (DOT), which requires you to take your medicine in front of your doctor several times a week. DOT helps prevent DR; however, it tends to add staggering costs to the patient.
2 History
Before the first mass production of penicillin in the 1940s and the introduction of antibiotics used to treat M. tb infections in the 1950s through the 1970s, there was no established treatment for the disease. The following three papers give an insight into some of the inhalation treatments tested. In a paper published in 1898, a medical professional had up to 2000 TB patients under his care. The infectious disease caused by M. tb was typically advanced in the patients [1]. The inhalation treatment was focused on the application of a vapor composed of:
-
eucalyptol (C10H18O), which is a cyclic ether and a monoterpenoid, also called 1,8-cineol;
-
oil of cloves (oil extracted from the clove plant, Syzygium aromaticum found in Southeast Asia, and is composed of β-caryophyllene, α-humulene, eugenyl acetate, and eugenol; and other ingredients
A quote from the author summarizes the results:
“symptoms have improved in all cases, though some have improved significantly more than others”.
These were a most unfavorable class of patients to treat, being in the advanced stage of the tubercular process with hemorrhages, emaciation, night sweats, anemia, and, in fact, scarcely able to breathe at all. In the absence of a specific symptom for TB, we believe that with proper apparatus and skillful and continued administration, much is to be hoped for in this class of patients by inhaling the antiseptic vapor. The historical literature does not explain why this promising approach was abandoned.
Benzol was the name for benzene and could be inhaled as a vapor. To put the study in perspective, penicillin was the first mass-produced antibiotic, which happened in the 1940s. The concept of an atom was not fully understood, emphasizing the Nobel prize in physics awarded to James Chadwick to discover the neutron in 1935. Benzene is now recognized by IARC as a human carcinogen that causes leukemia and non-Hodgkin lymphoma. The study did report changes in changes in the function of kidneys, liver, and hearts muscles in the mice, and the paper concluded [2]:
that with further study of this rather specific poison, we may get a little nearer the solution of some of the unsolved problems of infection and immunity.
Studies of this nature, before the modern era of antibiotics, emphasize the desperation in seeking treatments using toxic compounds that were very poorly understood.
In a 1935 paperback entitled “Inhalation Therapy Technique” by W. Collison [3], there is a chapter dedicated to inhalation therapy in PTB. First, the author outlined some oils and liquids cannot be used for inhalation therapy because the large particle sizes generated allow minimal penetration of the substance deep into the lungs. Likewise, there are medical sprayers used in that time period for treating the nasal cavity or throat maladies that do not provide the parameters needed for the mist to penetrate deep into the lungs. An Apneu Inhaling Apparatus was used to deliver the vapor to a mask that covers the patients’ faces and mouths. There is a discussion on the parameters that impact the size of the particles, as small as “1/5000th of an inch.” The apparatus is used to deliver compounds such as adrenalin, camphor, menthol, and creosote. The substances are delivered with a purpose; adrenalin is used to reduce congestion by dilating the bronchial tubes; camphor is stated to stimulate blood circulation and breathing; thymol and menthol are antiseptic; creosote is a disinfectant; pine and cypress soothed the inflamed mucous membrane, etc. A typical prescription is described as three minutes of adrenalin therapy, a three-minute rest, a three-minute camphor therapy, a three-minute rest, followed by a three-minute adrenalin dosage. While not described as a cure, it did help patients feel better or “obtain relief.”
3 Modern Work
Currently, there are three types of inhalers used for lung infection treatments:
-
i.
Small-volume nebulizer (SVN), it generates a liquid into an aerosol, and the droplets are propelled by a compressed gas, typically air or pure oxygen;
-
ii.
Dry powder nebulizer delivers the medication as a powder or small solid particles; and
-
iii.
The pressurized metered-dose inhaler (MDI), it is the most common type.
Although not placed in the same category of inhalers, anesthetics are gases that can be inhaled but are not used directly to treat a medical condition. There are some unsuccessful ventures mentioned in the literature in which gases such as carbon dioxide were used unsuccessfully.
For a medication to function properly, it should have the ability to reduce or eliminate the bacterial load contained within a macrophage without eliminating a large percentage of the macrophages residing within the lungs. Often heavy doses of antibiotics have to be given to patients to overwhelm physiological barriers such as macrophages and granuloma to eliminate the M. tb. This results in significant side effects for the patient.
We have identified the following pharmacokinetic and pharmacodynamics aspects related to the administration of inhaled agents with medicinal activity for a viral infection that need to be considered if a large fraction of the droplets will reach the desired region of the lungs and be effective in reducing the bacterial load in the lungs and entering the bloodstream to eliminate its presence throughout the body (Box 1).
Box 1
A sequential outline of the biological and chemical processes that could impact the drug delivery efficiency when inhalation is utilized
Some electronic vaporization processes can potentially cause a fraction of the medication or molecule to react or degrade; |
The medication is absorbed in the mouth or throat; |
The medication enters the digestive tract; |
The medication is absorbed in the trachea; |
The medication is absorbed in the upper lungs; |
The medication is exhaled; |
If a solid, the medication does not completely dissolve; |
The medication penetrates the granuloma model (Sarcoidosis) intact; |
If a prodrug, it has to encounter a reactive site (i.e., enzyme); |
The medication enters the macrophage; |
Depending on the MOA, the medication has to penetrate or disrupt the mycolic acid membrane; |
The medication can undergo unwanted protein binding; |
The medication enters the bloodstream and is distributed, metabolized, and excreted without interacting with any M. tb; |
The medicine is evenly distributed through the alveolus; |
The medication undergoes hydrogen bonding to an unwanted species as an H donor or acceptor; |
The water solubility of the medication limits its mobility; |
The size (high molar mass) of the medication limits its mobility; and |
The composition of the inhaled medicinal particle is such that the dissolution and delivery process of the medication falls within acceptable parameters needed to effectively treat the patient. |
For inhalation to meet each of these processes efficiently, arguably the most important parameter is the size of the particle. It should be small, with a diameter less than 200 nm, with values in the 50–70 nm range considered optimal to fully penetrate the alveoli in the lower lung. Capreomycin is a second-line antibiotic used to treat DR strains of M. tb. There are two drawbacks to its current administration, as a tablet or an injection:
-
i.
it involves an injection which can be problematic for several reasons, especially for children and emaciated adults with low muscle content; and
-
ii.
it necessitates regular visits to a health care facility.
Studies by Garcia-Contreras et al. [21, 24] developed a low-density particle that was produced by a sprayed dry technique that contained capreomycin. The study produced pharmacokinetics data when the particles were inhaled by guinea pigs with an optimum dose of 14.5 mg/kg, which for a 70 kg adult would translate to a dose of 1.015 g. It was argued that if the approach was applied to humans, it would eliminate injections and lower side effects. A scanning electron micrograph supplied an image that indicated the particles are in the range of approximately two to four micrometers in diameter. Alveolar and interstitial macrophages, which can be M. tb reservoirs in the lung, have 17.1 and 13.2 µm diameters for nonsmokers, 23.7 and 11.3 µm for smokers, and 23.7 and 11.8 µm for chronic obstructive pulmonary disease patients. The medicine has to penetrate the macrophage before acting on the bacterium. Significantly reducing the size of the capreomycin particles, coupled with a coating that might make the particle appear as cellular debris and/or a nutrient to the macrophage, might increase the uptake rate.
Antibiotics used to treat DR strains of M. tb can result in significant side effects, including ototoxicity and nephrotoxicity. Barberis et al. [76] compared capreomycin to amikacin for up to 192 days for patients with MDR-TB and up to 735 days with XDR-TB. Their study revealed that amikacin was up to five times more likely than capreomycin to result in severe ototoxicity. Amikacin had less hypokalemia (low potassium levels in serum) than capreomycin. Both sets of patients, those given amikacin or capreomycin, experienced a similar increase in the creatinine levels.
In a follow-up publication [24], the same group measured pharmacokinetic (PK) parameters related to the same capreomycin particles being inhaled by guinea pigs. This study focused on doses of 20 mg/kg. The capreomycin concentration in bronchoalveolar fluid and lung tissue of the animal was up to one-hundred times greater than in the plasma when compared to guinea pigs that received the medication via injection.
DR strains of M. tb have become more problematic worldwide. The treatments for MDR, XDR, and TDR have more severe side effects when compared to latent or active TB. Attempts to develop a method that could deliver the antibiotics more efficiently seem to be a natural progression in order to penetrate the lungs. Capreomycin is a second-line TB drug that belongs to a group of medications called glycosides and has been on the market since 1979. It is administered by injection daily for two to four months and then reduced to two or three times per week but varies with the patient’s condition. Patients who suffer from trypanophobia or fear of injections and those with very low muscle mass, such as a child or an adult with a chronic condition, often will quickly stop taking the medication. Administering capreomycin via an inhalation route not only removes the use of injections but should also lower the dose and, subsequently, the side effects.
In a rare study involving human patients [44], capreomycin was formulated as micrometer-sized particles, which was produced by a dry spray technique. An aerosol approach was used to deliver the micron-sized particles to the lungs. This was a phase 1 trial using 20 healthy adults with the goal of measuring several pharmacokinetic parameters. This study incorporated a relatively simple but efficient method for the patients to self-medicate, a tremendous improvement over visiting a medical office on a daily basis for injection or an IV. The single daily doses administrated were 25, 75, 150, or 300 mg doses of capreomycin, with five patients in each dosage group. The doses were 25 mg of capreomycin with 5 mg lysine serving as an excipient. The 300 mg administration required the patient to sequentially self-administer twelve doses of the medication.
The patients had their blood sampled for capreomycin four times before the antibiotic was delivered and at eight points (1, 2, 4, 6, 8, 12, and 24 h) after delivery. A sample of the mean area under the curve (AUC) values over a finite time interval for each of five patients was measured; 969 (h ng/ml) for the 25 mg dose group; 3555 (h ng/ml) for the 75 mg group; 7019 (h·ng/ml) for the 150 mg dose group; and 19,959 (h ng/ml) for the 300 mg dose group. The Cmax values measured were 169, 569, 972, and 2315 ng/mL, correspondingly. The published in vitro MIC value for capreomycin treating M. tb was 2 μg/ml (or 2000 ng/ml). The Cmax for the 300 mg dose group was the only value that was above the MIC value.
4 The Future
The following is a proposed structure and administration route that could be applied for latent, active, and resistant M. tb strains. It utilizes electronic vaporization as a method to form an aerosol and deliver the medication. Our group has incorporated copper in selected cancer drugs and antibiotics for several reasons [78,79,80,81,82,83,84]. Metal–ligand complexes composed of Cu(II)-sucrose and Cu(II)-DALB (denatured albumin) were built to minimize unwanted interactions such as protein binding or the Cu(II) cation generating reactive oxidation species prematurely. Mostly, M. tb is impacted by the toxicity of copper metal or the copper ion (Cu(II), Cu(I), Cu(0)). We demonstrated that a copper-capreomycin complex has a higher efficacy against active and resistant strains of M. tb [84]. The MIC values were up to 200 times lower for the copper-capreomycin complex than for pure capreomycin. The complex was synthesized and characterized in our lab and tested at the National Institutes of Health (Bethesda, MD, USA) against active INH-R (isoniazid-resistant), RMP-R (rifampin-resistant), and OFX-R (Ofloxacin resistant) strains of M. tb. While adding the Cu(II) cation to the capreomycin molecule improves parameters related to Lipinski’s Rules, such as water solubility and the number of hydrogen bonds possible, it also lowered the MIC value significantly [83]. The presence of copper might raise toxicity concerns when administrated orally due to higher doses. Applying the complex directly to the lungs decreases the dose, lowers side effects associated with higher doses given by tablet, and can increase the effectiveness of the treatment.
The results of a time-of-flight mass spectrometry analysis (Fig. 1) illustrate that denatured human serum albumin (DALB), used as a drug delivery platform, can be electronically vaporized using a Propylene Glycol-Glycerol-Ethanol solvent and transported as a vapor through two feet of 0.3 cm inside diameter tubing [75]. Figure 2 provides a novel complex to deliver the copper-capreomycin molecule. The DALB structure is denatured using ethanol, allowing the glucose molecules and the copper (II)-capreomycin complex to attach (bond) to it. Glucose is added via a glycation reaction and included so that macrophages and M. tb recognize it as an energy source and increase the medication uptake rate. DALB may also be consumed by the macrophage because it is recognized as cellular debris, providing an easy entry to the location of the M. tb reservoir. Also, both the macrophage and M. tb, sensing amino acids, would consume the complex to fulfill its nutrient and energy needs. Copper strongly binds the amines on capreomycin (CAP) molecules and to the amines on the protein structure, serving as an atomic level connection. The copper (II) cation is highly toxic to M. tb and, because of its high metal-ligand stability constant, is somewhat protected by the protein from dissociating from the complex. The protein-glucose-copper-capreomycin complex (PGCC) is small enough to be engulfed/phagocytosed by local cells or to leave the lungs and be transported through the circulatory system. In pulmonary tuberculosis (PTB), a common form of the disease, M. tb enters the lungs and is consumed by a macrophage as a single complex would be the desired route.
There are review papers that take the reader back hundreds and even thousands of years and outline the impact that M. tb infections had on various cultures and time periods [76]. With modern chemical separation, synthesis, and analysis techniques providing a more detailed look at the compositions of medical treatments, this review focused on modern developments. There are two key messages taken away from this review:
-
i.
inhalation therapy should be examined in closer detail as a method of treatment for the different forms of TB; and
-
ii.
because of some unique features of M. tb, such as its waxy (mycolic acid) outer membrane and its ability to reside within a macrophage for long periods, treatments should be devised at a molecular level with these considerations in mind, rather than borrowing techniques and technologies from disorders that have a different set of biological and chemical conditions.
There is a significant crossover and adaption of inhalation technologies from other conditions such as cystic fibrosis and viral infections.
5 Conclusion
With a rise in antibiotic resistance, new techniques are needed to treat patients. This paper reviewed inhalation therapy first from a historical basis. Despite the fact that PTB is very common, there has been very little work using inhalation therapy that has been brought to clinical trials. For the future, with the right delivery mechanism, capable of making the small droplets needed to penetrate into the lower lungs, coupled with using a solvent mixture and a formulation that can attack the M. tb with several mechanisms of action, inhalation therapy may prove to be part of the solution.
Core Messages
-
Inhalation therapy offers the potential to transform the treatment of all levels of TB therapies.
-
Existing vaporization and inhalation technology can be adapted to drug delivery.
-
Millions of users have tested the units, and delivery parameters are well understood.
-
Ethanol and glycerol can be used for inhalation and delivery, having minimal impact on the patient.
-
We welcome collaboration with any group interested in delivering CuINH or CuCAP for pulmonary TB.
References
Johnson GW (1898) A report of the treatment of pulmonary tuberculosis by the inhalation of antiseptic vapors. JAMA 6:315–317
White W, Gammon A (1914) The influence of benzol inhalation on experimental pulmonary tuberculosis in rabbits. Trans Assoc Amer Phys 29:332–337
Charnock B (1933) Inhalation therapy in pulmonary tuberculosis by the Apneu Collison inhaler. Report of the Central Tuberculosis Officer, Lancashire, i933
Banyai A (1934) Carbon dioxide inhalation in pulmonary tuberculosis. Am Rev Tuberc 30(6):642–652
Charnock G (1935) Inhalation therapy in pulmonary tuberculosis. Br J Tuberc 29(4):227–232
Hewer C, Hadfield C (1941) Trichlorethylene as an inhalation anaesthetic. BMJ 1(4198):924
Barach A, Molomut N, Soroka M (1942) Inhalation of nebulized promin in experimental tuberculosis: sodium P,P’-diaminodiphenylsulfone-N,N’-didextrose sulfonate. Am Rev Tuberc 46(3):268–276
Lurie M, Abramson S, Heppleston A (1952) On the response of genetically resistant and susceptible rabbits to the quantitative inhalation of human type tubercle bacilli and the nature of resistance to tuberculosis. J Exp Med 95(2):119–134
Kim A, Krasnova T, Romanova V (1987) Use of inhalation of ultrasonic aerosols and galvanic current in the treatment of patients with pulmonary tuberculosis. Ter Arkh 59(11):96–98
Hungund B, Goldstein D, Villegas F, Cooper T (1988) Formation of fatty acid ethyl esters during chronic ethanol treatment in mice. Biochem Pharmacol 37(15):3001–3004
Shaikh W (1992) Pulmonary tuberculosis in patients treated with inhaled beclomethasone. Allergy 47(4):327–330
Wards D, Hanes J, Caponetti G, Hrkach J, Ben-Jebria A, Eskew M, Mintzes J, Deaver D, Lotan N, Langer R (1997) Large porous particles for pulmonary drug delivery. Science 276:1868–1872
Converse P, Dannenberg A, Shigenaga T, McMurray D, Phalen S, Stanford J, Rook G, Koru-Sengul T, Abbey H, Estep J, Pitt M (1998) Pulmonary bovine-type tuberculosis in rabbits: bacillary virulence, inhaled dose effects, tuberculin sensitivity, and Mycobacterium vaccae immunotherapy. Clin Diagn Lab Immunol 5(6):871–881
Yokota S, Miki K (1999) Effects of INH (Isoniazid) inhalation in patients with endobronchial tuberculosis (EBTB). Kekkaku: [Tuberculosis] 74(12):873–877
Iseman M (2001) Some healthy skepticism about inhaled therapy for tuberculosis. Clin Infect Dis 33(2):266–266
Sharma R, Saxena D, Dwivedi A, Misra A (2001) Inhalable microparticles containing drug combinations to target alveolar macrophages for treatment of pulmonary tuberculosis. Pharm Res 18(10):1405–1410
Schwebach J, Chen B, Glatman-Freedman A, Casadevall A, McKinney J, Harb J, McGuire P, Barkley W, Bloom B, Jacobs W (2002) Infection of mice with aerosolized Mycobacterium tuberculosis: use of a nose-only apparatus for delivery of low doses of inocula and design of an ultrasafe facility. Applied and Environmental Microbiology 68(9):4646–4649
Sherry E, Warnke P (2004) Successful use of an inhalational phytochemical to treat pulmonary tuberculosis: a case report. Phytomedicine: Int J Phytother Phytopharmacol 11(2–3):95–98
Pandey R, Khuller G (2005) Antitubercular inhaled therapy: opportunities, progress and challenges. J Antimicrob Chemother 55(4):430–435
Vail W, Vai M (2006) Methods and apparatus to prevent treat and cure infections of the human respiratory system by pathogens causing severe acute respiratory syndrome (SARS), U.S. Patent 7,048,953 B2
Garcia-Contreras L, Fiegel J, Telko M, Elbert K, Hawi A, Thomas M, VerBerkmoes J, Germishuizen W, Fourie P, Hickey A, Edwards D (2007) Inhaled large porous particles of capreomycin for treatment of tuberculosis in a guinea pig model. Antimicrob Agents Chemother 51(8):2830–2836
Sanders M (2007) Inhalation therapy: an historical review. Primary Care Respir J: J Gen Pract Airways Group 16(2):71–81
Coowanitwong I, Arya V, Kulvanich P, Hochhaus G (2008) Slow release formulations of inhaled rifampin. AAPS J 10(2):342–348
Fiegel J, Garcia-Contreras L, Thomas M, VerBerkmoes J, Elbert K, Hickey A, Edwards D (2008) Preparation and in vivo evaluation of a dry powder for inhalation of capreomycin. Pharm Res 25(4):805–811
Mitnick C, McGee B, Peloquin C (2009) Tuberculosis pharmacotherapy: strategies to optimize patient care. Expert Opin Pharmacother 10(3):381–401
Muttil P, Wang C, Hickey A (2009) Inhaled drug delivery for tuberculosis therapy. Pharm Res 26(11):2401–2416
Sung J, Garcia-Contreras L, VerBerkmoes J, Peloquin C, Elbert K, Hickey A, Edwards D (2009) Dry powder nitroimidazopyran antibiotic PA-824 aerosol for inhalation. Antimicrob Agents Chemother 53(4):1338–1343
Garcia-Contreras L, Sung J, Muttil P, Padilla D, Telko M, VerBerkmoes J, Elbert K, Hickey A, Edwards D (2010) Dry powder PA-824 aerosols for treatment of tuberculosis in guinea pigs. Antimicrob Agents Chemother 54(4):1436–1442
Nikander K, Sanders M (2010) The early evolution of nebulizers. Medicamundi 54:47–53
Wang C, Hickey AJ (2010) Isoxyl aerosols for tuberculosis treatment: preparation and characterization of particles. Aaps Pharmscitech 11(2):538–549
Brassard P, Suissa S, Kezouh A, Ernst P (2011) Inhaled corticosteroids and risk of tuberculosis in patients with respiratory diseases. Am J Respir Crit Care Med 183(5):675–678
Geller DE, Jeffry W, Silvia H (2011) Development of an inhaled drypowder formulation of tobramycin using PulmoSphere™ technology. J Aerosol Med Pulm Drug Deliv 24(4):175–182
Mercedes G-J, O’Sullivan Mary P (2011) Optimization of inhaled therapies for tuberculosis: the role of macrophages and dendritic cells. Tuberculosis 91(1):86–92
Amit M, Hickey AJ, Carlo R, Gerrit B, Hiroshi T, Kimiko M, Bernard FP, Paolo C (2011) Inhaled drug therapy for treatment of tuberculosis. Tuberculosis 91(1):71–81
Pinheiro M, Lucio M, Lima JL, Reis S (2011) Liposomes as drug delivery systems for the treatment of TB. Nanomedicine 6(8):1413–1428
Kumar VR, Kumar SA, Mradul M, Kumar AA, Amit M (2011) Inhaled therapies for tuberculosis and the relevance of activation of lung macrophages by particulate drug-delivery systems. Ther Deliv 2(6):753–768
Garcia-Contreras L, Pavan M, Fallon JK, Mohan K, Robert G, Hickey AJ (2012) Pharmacokinetics of sequential doses of capreomycin powder for inhalation in guinea pigs. Antimicrob Agents Chemother 56(5):2612–2618
Garcia-Contreras L, Awashthi S, Hanif SNM, Hickey AJ (2012) Inhaled vaccines for the prevention of tuberculosis. J Mycobac Dis S 1:002
Masayuki H, Motoyasu I, Satoshi H, Haruhito S, Nobuyuki K, Koichiro K (2012) Increased risk of nontuberculous mycobacterial infection in asthmatic patients using long-term inhaled corticosteroid therapy. Respirology 17(1):185–190
Rojanarat W, Nakpheng T, Thawithong E, Yanyium N, Srichana T (2012) Inhaled pyrazinamide proliposome for targeting alveolar macrophages. Drug Delivery 19(7):334–345
Son YJ, McConville JT (2012) Preparation of sustained release rifampicin microparticles for inhalation. J Pharm Pharmacol 64(9):1291–1302
Willis L, Hayes D, Mansour HM (2012) Therapeutic liposomal dry powder inhalation aerosols for targeted lung delivery. Lung 190(3):251–262
Claire A, Rikke N, Thomsen VØ, Pierre D, Toft SH, Wernich TR (2013) Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax 68(3):256–262
Dharmadhikari AS, Mohan K, Bob G, Hickey AJ, Bernard FP, Edward N (2013) Phase I, single-dose, dose-escalating study of inhaled dry powder capreomycin: a new approach to therapy of drug-resistant tuberculosis. Antimicrob Agents Chemother 57(6):2613–2619
Lee C-H, Kim K, Hyun MK, Jang EJ, Lee NR, Yim J-J (2013) Use of inhaled corticosteroids and the risk of tuberculosis. Thorax 68(12):1105–1113
Ober CA, Lonji K, Hulda S, Gupta RB (2013) Preparation of rifampicin/lactose microparticle composites by a supercritical antisolvent-drug excipient mixing technique for inhalation delivery. Powder Technol 236:132–138
Park J-H, Jin H-E, Kim D-D, Chung S-J, Shim W-S, Shim CK (2013) Chitosan microspheres as an alveolar macrophage delivery system of ofloxacin via pulmonary inhalation. Int J Pharm 441(1–2):562–569
Salomon JJ, Pauline G, Nanette S, Morow PR, Diana SeverynseStevens, Hanno H, Nicole D, Lehr Claus-Michael J, Anthony H, Carsten E (2013) Biopharmaceutical in vitro characterization of CPZEN-45, a drug candidate for inhalation therapy of tuberculosis. Ther Deliv 4(8):915–923
Sven S, Kopp S, Borchard G, Shah VP, Senel S, Dubey R, Urbanetz N et al (2013) Developing and advancing dry powder inhalation towards enhanced therapeutics. Eur J Pharm Sci 48(1–2):181–194
Verma RK, Germishuizen WA, Motheo MP, Agrawal AK, Singh AK, Mohan M, Gupta P, Gupta UD, Cholo M, Anderson R, Fourie PB, Misra A (2013) Inhaled microparticles containing clofazimine are efficacious in treatment of experimental tuberculosis in mice. Antimicrob Agents Chemother 57(2):1050–1052
Chan JG, Tyne AS, Pang A, Chan HK, Young PM, Britton WJ, Duke CC, Traini D (2014) A rifapentine-containing inhaled triple antibiotic formulation for rapid treatment of tubercular infection. Pharm Res 31(5):1239–1253
Marcel H, Paul H, Frijlink HW, de Boer HW (2014) Developments and strategies for inhaled antibiotic drugs in tuberculosis therapy: a critical evaluation. Eur J Pharm Biopharm 86(1):23–30
Eleonora M, Tiziana R, Moreno B, Maria AC, Miriam H, Eliana L, Francesca S, Valentina I (2014) Inhaled solid lipid microparticles to target alveolar macrophages for tuberculosis. Int J Pharm 462(1–2):74–82
Mortensen NP, Phillip D, Hickey AJ (2014) The role of particle physico-chemical properties in pulmonary drug delivery for tuberculosis therapy. J Microencapsul 31(8):785–795
Rajesh P, Sonali D, Pooja A, Leena P (2014) Inhaled microparticles of antitubercular antibiotic for in vitro and in vivo alveolar macrophage targeting and activation of phagocytosis. J Antibiot 67(5):387–394
Patil-Gadhe A, Kyadarkunte A, Pereira M, Jejurikar G, Patole M, Risbud A, Pokharkar V (2014) Rifapentine-proliposomes for inhalation: in vitro and in vivo toxicity. Toxicol Int 21(3):275
Cilfone N, Pienaar E, Thurber G, Kirschner D, Linderman JJ (2015) Systems pharmacology approach toward the design of inhaled formulations of rifampicin and isoniazid for treatment of tuberculosis. CPT: Pharmacometrics Syst Pharmacol 4(3):193–203
Shyamal D, Tucker I, Stewart P (2015) Inhaled dry powder formulations for treating tuberculosis. Curr Drug Deliv 12(1):26–39
Fennelly K, Jones-López E (2015) Quantity and quality of inhaled dose predicts immunopathology in tuberculosis. Front Immunol 6:313
Lee W-H, Loo C-Y, Traini D, Young P (2015) Nano-and micro-based inhaled drug delivery systems for targeting alveolar macrophages. Expert Opin Drug Delivery 12(6):1009–1026
Dinh-Duy P, Fattal E, Tsapis N (2015) Pulmonary drug delivery systems for tuberculosis treatment. Int J Pharm 478(2):517–529
Kirtimaan S, Chakraborty S, Bhattacharyya R, Banerjee D (2015) Combined inhalation and oral supplementation of Vitamin A and Vitamin D: a possible prevention and therapy for tuberculosis. Med Hypotheses 84(3):199–203
Hickey A, Durham P, Dharmadhikari A, Nardell E (2016) Inhaled drug treatment for tuberculosis: past progress and future prospects. J Control Release 240:127–134
Maretti E, Rustichelli C, Romagnoli M, Balducci A, Buttini F, Sacchetti F, Leo E, Iannuccelli V (2016) Solid Lipid Nanoparticle assemblies (SLNas) for an anti-TB inhalation treatment—a design of experiments approach to investigate the influence of pre-freezing conditions on the powder respirability. Int J Pharm 511(1):669–679
Young E, Hickey A, Braunstein M (2016) Testing inhaled drug therapies for treating tuberculosis. Delivery systems for tuberculosis prevention and treatment (advances in pharmaceutical technology). Wiley, pp 113–130
Young E, Perkowski E, Malik HJ, Durham P, Zhong L, Welch J, Braunstein M, Hickey A (2016) Inhaled pyrazinoic acid esters for the treatment of tuberculosis. Pharm Res 33(10):2495–2505
Bai X, Stitzel J, Bai A, Zambrano C, Phillips M, Marrack P, Chan E (2017) Nicotine impairs macrophage control of Mycobacterium tuberculosis. Am J Respir Cell Mol Biol 57(3):324–333
Giovagnoli S, Schoubben A, Ricci M (2017) The long and winding road to inhaled TB therapy: not only the bug’s fault. Drug Dev Ind Pharm 43(3):347–363
Maretti E, Costantino L, Rustichelli C, Leo E, Croce M, Buttini F, Truzzi E, Iannuccelli V (2017) Surface engineering of Solid Lipid Nanoparticle assemblies by methyl α-d-mannopyranoside for the active targeting to macrophages in anti-tuberculosis inhalation therapy. Int J Pharm 528(1–2):440–451
Sinnott T (2017) One woman’s journey for a tuberculosis cure. Retrieved from: https://hekint.org/2017/02/01/one-womans-journey-for-a-tuberculosis-cure/
Stein S, Thiel C (2017) The history of therapeutic aerosols: a chronological review. J Aerosol Med Pulm Drug Deliv 30(1):20–41
Traini D, Young P (2017) Drug delivery for tuberculosis: is inhaled therapy the key to success? Ther Deliv 8(10):819–821
Khadka P, Dummer J, Hill P, Das S (2018) Considerations in preparing for clinical studies of inhaled rifampicin to enhance tuberculosis treatment. Int J Pharm 548(1):244–254
Sibum I, Hagedoorn P, Frijlink H, Grasmeijer F (2019) Characterization and formulation of isoniazid for high-dose dry powder inhalation. Pharmaceutics 11(5):233
Manning T, Richard-Thomas J, Cowan M (2020) O etanol deve ser considerado como um tratamento para o COVID-19? J Braz Med Assoc (in press)
Barberis I, Bragazzi N, Galluzzo L, Martini M (2017) The history of tuberculosis: from the first historical records to the isolation of Koch’s bacillus. J Prev Med Hyg 58(1):E9–E12
Arnold A, Cooke G, Kon O, Dedicoat M, Lipman M, Loyse A, Ster I, Harrison T (2017) Adverse effects and choice between the injectable agents amikacin and capreomycin in multidrug-resistant tuberculosis. Antimicrob Agents Chemother 61(9):e02586–e02616
Manning T, Plummer S, Baker T (2019) Tablet composition for anti-tuberculosis antibiotics. US Patent No. 10,335,374 B2
Manning T, Thomas-Richardson J, Cowan M, Beard T (2020) Vaporization, bioactive formulations and a marine natural product: different perspectives on antivirals. Drug Discovery Today 25(6):956–958
Manning T, Slaton C, Myers N, Patel P, Arrington D, Patel Z, Phillips D, Wylie G, Goddard R (2018) A Copper10-Paclitaxel crystal; a medicinally active drug delivery platform. Bioorg Med Chem Lett 28(20):3409–3417
Manning T, Wilkerson K, Holder T, Bartley A, Jackson C, Plummer S, Phillips D, Krajewski L, Wylie G (2017) Pharmacokinetic studies of a three-component complex that repurposes the front line antibiotic isoniazid against Mycobacterium tuberculosis. Tuberculosis 107:149–155
Manning T, Plummer S, Woods R, Wylie G, Phillips D, Krajewski L (2017) Cell line studies and analytical measurements of three paclitaxel complex variations. Bioorg Med Chem Lett 27(12):2793–2799
Manning T, Mikula R, Lee H, Calvin A, Darrah J, Wylie G, Phillips D, Bythell B (2014) The copper (II) ion as a carrier for the antibiotic capreomycin against Mycobacterium tuberculosis. Bioorg Med Chem Lett 24(3):976–982
Miranda M, Breiman A, Allain S, Deknuydt F, Altare F (2012) The tuberculous granuloma: an unsuccessful host defence mechanism providing a safety shelter for the bacteria? Clin Dev Immunol 1–14
Acknowledgements
We would like to thank Dr. Jim Boyce of the Infectious Disease Section of the US National Institutes of Health for sponsoring our original work in this area. Our group has worked on inhalation therapy, first with TB and, more recently, with COVID19. We thank VSU for giving us access to our facilities during the pandemic. Finally, we would like to acknowledge that the famous American gunslinger, Doc Holiday (featured in the movie Tombstone), worked as a dentist in Valdosta, died of TB, and is now buried in a family cemetery south of Atlanta. Finally, we would like to thank the National Science Foundation for sponsoring Noyce interns that spend part of their summer working on the stearic acid nanospheres for TB drug delivery (Yalanda, Thomas, Jenu, Matthew, Jordan, Courtney, Rachel, Olin, Olivia, and Marcus). They proved that this technology has the economics in synthesis and delivery can be adapted to all corners of the globe, not just to the privileged. They had the opportunity and privilege to present their work to US Congressman Buddy Carter. We will like to thank STORZ & BICKEL for the donation of their vaporizer used to advance our work (Vatra and Anna).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Manning, T. et al. (2023). Inhalation Therapy in Pulmonary Tuberculosis. In: Rezaei, N. (eds) Tuberculosis. Integrated Science, vol 11. Springer, Cham. https://doi.org/10.1007/978-3-031-15955-8_16
Download citation
DOI: https://doi.org/10.1007/978-3-031-15955-8_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-15954-1
Online ISBN: 978-3-031-15955-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)