Abstract
As the pressing need to expand the delivery of healthcare has surpassed the traditional limits of implementation, the substantial burden of the COVID-19 pandemic has placed the provision of healthcare services under duress. We explore the outcomes associated with the implementation of telehealth technology in healthcare ecosystems, we are mindful of the challenge in bridging the gap between the potential for extending healthcare technology to overcome the disruption in the provision of health services and the possible effect on the quality of healthcare services. This paper aims to learn from the literature on the impact of Telehealth diffusion on the delivery of quality care. We develop a scoping review and evaluate the outcome through the lens of the six aims of improvement of healthcare quality. We synthesize the literature around managing the disruption, identifying the risks of unintended consequences and factors affecting adoption. We also offer learnings and call to action.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
After decades of measured implementation of telemedicine and telehealth [1], the COVID-19 pandemic has dramatically changed not only the frequency of patient-clinician visits conducted via technology across a distance, but also the urgency to practice at a distance, in order to prevent the spread of the pandemic [2]. Telehealth became a component of the personal protective equipment gear, designated as Electronic PPE (ePPE), in the medical practice [3], giving this new interaction experience a mainstream [4, 5]. Thus, bridging the digital divide for a tranche of the population and creating new challenges for others vulnerable sectors of society [6]. Hence, telehealth is a technology that built a new bridge between the patient and the service enabling a level of sustainability of the medical practice and the continuum of care. Now, clinicians could practice from the hospital and from home. While practitioners used teleconferencing equipment and connected remote devices to collect their patient’s vitals and provide a remote assessment [7], patients were able to access their information through their mobile app, interfaced with the health record [8]. Technology implementers have joined the front line of the medical provider workforce to deploy and maintain the platforms that make these “at a distance” services possible.
The aims for healthcare quality imply that a Telehealth provisioned service shall be the equivalent to a traditional in person service in a healthcare setting when delivered virtually. It shall be safe, effective, patient-centered, timely, efficient, and responsive, offering an equitable and standardized service to all patient categories [9]. As we introduce technology to a new level of interaction between the care team and the care seekers, a new set of complexity arises. A tradeoff must be managed between the potential value added and the benefits in care quality as opposed to risks incurred through unintended consequences of the benefits. Therefore, we propose to answer the following questions: How could we use telehealth to improve Care Quality? What does the literature inform on managing the potential disruption caused by the diffusion of telehealth? What learning can we conclude from the existing research?
This paper summarizes the evidence from very recent and not-so-recent studies on telehealth quality and presents a wide literature review on works dealing with the adoption of telehealth, which in a nutshell, can be described as all the solutions built around digitals tools for providing healthcare services remotely. In our study, we identify some quality-of-care benefits and improvements of care outcome through telehealth using the lens of dimensions of quality of care. We also build the argument around the tradeoff that unintended consequences pose to this technological diffusion phenomenon. The underlying theory, building on sociotechnical systems theory [10], is that the implementation and use of the technological systems for a specific task will influence the device operators performing the tasks and their organizational setting.
2 Approach
We start this scoping review to explore the state of the literature in the context of telehealth deployment and consequential impact on quality of care. We follow the recommendations of [11] and similar studies in telehealth [12] to explore the potential of telehealth diffusion in addressing Care Quality. We also focus on understanding the disruption from telehealth diffusion while we aim at learning from the literature on how to address such challenges.
2.1 Scoping Review Criteria
As we prepare for our review, we identify relevant studies and develop a decision plan for where to search, which terms and what sources to use. The search encompasses online databases including but not limited to PubMed, Journal of Telemedicine and Telecare, Journal of American College of Surgeons, International Journal of Medical Informatics, New England Journal of Medicine, JAMA Dermatology, NEJM Catalyst Innovations in Care Delivery, JMIR Public Health Surveillance, International Journal of Environmental Research and Public Health, and JAMA Intern Med.
We base our inclusion criteria on the specifics of the research question and on new familiarity with the subject matter through reading the studies. In scanning the literature, we found that the terms telehealth and telemedicine are often used interchangeably. We then perform the searches twice, once using the filter of “Telehealth” AND “Impact on Quality of Care” in which 221 articles are retrieved and the second time using the filter of “Telemedicine” and “Impact on Quality of Care” in which 313 papers are returned. We then isolate and remove the duplicate papers and narrow down the search to 209 distinct articles. We screen the papers and identify relevant articles written in the English language. We read the articles in full and exclude duplicate findings in publications, citations, and student dissertations, then narrow our listing to 57 uniquely relevant articles. After independent review by each author individually, we document the body of literature on this topic. As a final step of this data collection effort, we catalog the findings based on outcome, context and findings related to impact on quality of care. We pay attention to the clarity and the nuances in the consulted studies then classify them based on a coding technique [11]. For better sense making and to effectively answer the research question we follow a coding technique that uses the framework of the six aims of improvement of healthcare quality that was introduced by Institute of Medicine (2001), in their seminal work, “Crossing the Quality Chasm” [9]. These aims stipulate that health care should be safe, effective, patient-centered, timely, efficient, and equitable, in order to be of quality (Table 1).
We make use of the six aims framework to help focus the study on the quality-of-care information as seen in practice and as a useful framework to advance quality of care [13]. We then follow up with discussion points that support our findings state of the literature. We enrich our findings through an investigation to identify means for potential managing the disruption, a review of factors affecting adoption, organizational considerations and close with learnings and recommendations from our review.
3 Findings
To note, upon review of the papers, we find a rush in publications during the COVID-19 pandemic—slightly more than half of the works identified (112) published after 2020. Further, while most published literature discuss quality of life [14] in connection to telehealth; our study deepens the investigation into exploring the impact of Telehealth on Quality of Care, which is a concept that is larger in scope.
We find that most telehealth literature refer to telehealth as the broader practice of delivering healthcare services at a distance and to telemedicine as the term that describes the actual practice of medicine at a distance. For our purposes, Telehealth is the delivery of healthcare services by healthcare professionals using information and communication technologies, for the exchange of valid information for diagnosis, treatment, and injuries and prevention of disease, evaluation and research, and the healthcare providers’ continuing education [15]. The modes of delivery of telehealth incorporates several means of delivery such as videoconferencing, mobile applications, and secure messaging. Telehealth services include provider-to-provider services with patient presence, provider to provider without patient presence, tele monitoring, and health education etc. [16].
3.1 Telehealth Use for Improvement of Care Quality—State of the Literature
The literature is scarce but vocal about how Telehealth improves the provisioning of quality care (Table 2).
Telehealth has made care safer, as evidenced by the reduction in mortality related to severe sepsis [17], and increase in prescription accuracy [18, 19]. Telehealth use helped prevent the potential of spread of disease [20], especially relevant in the era of the present-day COVID pandemic, and the need for the continuum of care [21, 22]. Telehealth was touted to improve compliance with clinical practice guidelines [23] care outcome [19, 24]; and quality of life in patients chronic conditions [25]. Thus, contributing to an effective means of providing quality care. Our review has also identified uses that help improve care service quality through patient engagement [17]. This patient centered approach increases ease and comfort for patients [26] and their satisfaction [28] while providing better access to personalized care [27]. Some authors recognized the benefits of timeliness, reducing wait time for care [29] and efficiency, reducing waste and costs [18, 31] and decreasing resource utilization [3, 30]. Finally, we have found mixed reports on the equity of care delivery. Some reports showed diverse outcomes of improving access to care for rural areas and underserved population [32], while bearing challenges through the need for education [33], availability of supporting technology and socio-economic status [34]. We also note studies that identified risks of inconsistent dependency on parents for children care and inequality of access [30], and accessibility for use in people with disabilities and the elderly [34, 35].
4 Discussion
4.1 Quality of Care Improvement Thru Telehealth
Providing Safe Care—Care is safe when the “priority of care is for avoiding injuries to patients from the care they receive” [9]. In the area of safety, the literature provides evidence of minimizing exposure of clinical staff to infected patients [20] and the reduction in mortality related to severe sepsis that otherwise would be a heightened risk in an in-person care setting [17]. However, the relevance of mortality rates in ICU telemedicine programs compared to the traditional onsite ICUs, have not been conclusive [19, 36]. On prescription accuracy, research reports an increase in appropriate antibiotic prescribing from 69 to 97% within six months with the use of telehealth services [19], sometimes due to a conservative approach of ordering antibiotics [18]. The use of tools such as reminders have improved prescription adherence, yet, studies have not found significant statistical relevance of guideline adherence by mode of communication, e.g. videoconference versus. telephone versus. webchat, etc. [17].
Quality through Effective Care—The aim of effectiveness points to “providing evidence-based care for all who could benefit and refraining from providing services to those not likely to benefit” [9]. Here also, the literature has connected telemedicine tools and automated reminder systems to the improvement of compliance with clinical practice guidelines and a betterment of the patient health outcome. Whilst clinical management was adherent to guidelines in 54.3% of the visits [23], prescription adherence through telemedicine visits was improved over urgent care visits [24] with an improved quality of life in patients with diabetes, blood pressure and high cholesterol levels [25]. Computer-assisted diagnosis and management in telemedicine was found to improve care service quality as it engages patients in their own health, where 92.9% of patients, during the telehealth consultation contributed to betterment of clinical management [17].
Patient-Centered Care—Patient-centered care is about “providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions” [9]. Technology platforms will soon become permanent gears within the patient homes. This facility will reduce costs associated with hospital stays, increased ease, and comfort for patients. On the other hand, by placing the technologies directly in patients’ homes or at local clinics, care becomes more available [27] and personalized; in fact, 66% of consumers are willing to use telehealth for everything from prescription renewals to chronic disease management and behavioral health [28].
Timely Care—By reducing waits and sometimes-harmful delays for both those, who receive and those who give care, this aim for improvement of care is met [9]. Both patients and clinicians can benefit from improvements in timeliness with e-visit and telemedicine. They receive timely and immediate access to automated clinical information, diagnostic tests, and treatment results [9]. Patients have received useful immediate advice in 86% of cases [29]. Timely diagnosis of minor illnesses in children and adolescents, improved school attendance, and decreased emergency department utilization by 22% [30]. In Florida (Pediatric Associates in Florida), one research has found 75% reduction in patient wait times for urgent care conditions through its telehealth triage program, using virtual visits for low-acuity patients, the emergency departments wait times reduced from 2.5 h to 40 min [28].
Efficient Care—Efficient care is about avoiding waste, in particular waste of equipment, supplies, ideas, and energy, as by reducing redundant laboratory tests, for instance [9]. The use of telemedicine has caused visits of emergency department to decrease from 40 to 70% [3], almost eliminating inappropriate pediatric consultations in the first 14 months and increasing completeness of medical documentation from 45 to 85% within six months of use [19]. Studies reveal the good story about reduced hospital admissions by 35% among its home telehealth patient population [28]. As a direct improvement in care outcome, other studies report that the use of telemedicine has reduced hospitalizations by 50%, length of stay by 50%, and 30-day readmission rate by 75% [19]. Video visits combined with remote patient monitoring will enable healthcare organizations to better monitor patients. Additionally, telehealth programs can be cost saving for intermediate and high-risk patients over a 1- to 5-year window [31]. Costs are lower for e-visits [18], bringing the efficiency back into the health plan covering the patient [28] and then the patient’s insurance rates [29].
Equitable Care (Equal Access)—Equitable care is about providing care with equal access. “Care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status”. Telemedicine has taken care into hard to reach rural areas and underserved population [32]. Both the high-speed internet and mass spread of smartphones combined shall make it possible to implement telehealth consultations and quickly deploy video teleconsultations from a patient’s home [37, 38]. Tele-audiology [39] and tele-dermatology [12] have reduced the number of patients required to attend face-to-face consultations. The adoption of telehealth as a recourse for some contagious conditions enhance the continuum of care, while preventing direct contact, promoting inclusion of all types of illnesses and improve patient outcome [21, 32]. Unfortunately, nearly half of the world population remains offline. Older adults with low socioeconomic status have limited access to internet-based services, a study found, especially in households of regions in Africa (71.8%), and Asia Pacific (51.6%) [34]. Poverty and the lack of education are the biggest barrier to the adoption of telemedicine in the developing world [33]. Equitable access also must address different age groups. Children pose different challenges during examination in relation to the degree of cooperation from a child during the video conferencing and the need to rely on another person to elicit the physical signs to be able to make the proper diagnoses [30]. It is also essential to fund telemedicine infrastructure and ensure telemedicine technologies are compatible and easy to use for individuals with disabilities and older adults [34]. Older population experience barriers to telemedicine, namely, trust of technology, design, cognitive impairment, and physical limitations such as poor vision, hearing, or sensory impairment [35].
4.2 Managing Disruption
On the question of disruption, the second research objective, the scarce literature is vocal about the fact that telehealth utilization requires many adjustments. We have found works reviewing elements that may promote or impede adoption, depending on how they were addressed in the early stages of telehealth implementation. These factors are related to technology diffusion, lack of regulatory framework, relating adoption to type of practice, supply chain disruption and other organizational considerations. This section summarizes these factors with references from the literature findings (Table 3).
Elements of Technology Adoption—In the past, even prior to the pandemic, studies have attributed the slow adoption of telemedicine to technically challenged staff, resistance to change, patient demography and literacy [40, 41], high cost and reimbursement [42]. These are among the classical barriers to telehealth adoption, however, closer to the communities of practice, the slow uptake in Telehealth has been connected at the level of policy, reimbursement, organizational readiness, clinical are of focus, etc. [43]. Hence, practitioners and academia are collaborating to understand the essential components to successful implementation of a telehealth platform. Provider and staff training [34], patient education, an existing electronic medical record system, patient and provider investment in hardware, billing and coding integration, information technology support, audiovisual platforms, and patient and caregiver participation, etc. are some [21]. Others connect device interoperability [42], data integration, privacy, security of data handling to telehealth success [44] while enumerating clinical, administrative concerns [45], in addition to the socio-technical aspects of patient engagement and the patient-provider relationship [16].
Effectiveness of Telehealth Use and Adoption Seems to Vary by Practice—When compared with in-person sessions, for instance, attendance to group therapy sessions virtually was significantly lower by more than threefold. Common reasons cited for not attending virtual sessions were unavailability of technology, technological malfunction or poor digital literacy and the issues of maintaining conditions of privacy [46]. Whereas, chronic care patients have enjoyed convenience and cost savings from the comforts of their own home compared with an in-person visit [21].
Lack of Regulatory Framework—It is evident that the lack a regulatory framework to authorize, integrate, and reimburse telemedicine services, including in emergency and outbreak situations has held back the implementation of Telehealth services, in some cases, notably France and Italy [37].
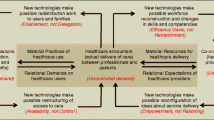
Disruption in the Supply Chain—Broader telehealth use and adoption may result in the emergence of new services corridors that disturb existing ones, introduce the risk of fragmentation of current services, which may lead to significant changes in the responsibilities of each actor in the supply chain of services [49].
Organizational Considerations—Integrating innovative technology into a business not only necessitates a large financial investment, but people partnership, policies, and technological aspects. The literature identifies key aspects of telehealth service delivery. Among these, physician leadership traits, reimbursement and licensure rules, liability and the human factor relate to organizational characteristics [50]. The disruption introduced by Telehealth could spawn several adjustments for organizations, such as additional investments and resources [49], authors reflect on factors of leadership, perceived value of telemedicine, and the organizational characteristics as key for the effectiveness of telehealth [51]. Pollard et al. [47] believed that the use of the telehealth model could enhance an organization’s ability to evaluate adherence to protocols, standards, and professional behavior. They recommended establishing policies to safeguard both at the individual and organization level. These policies include informed consent, care coordination, privacy, and confidentiality, resources needed at home to optimize the treatment environment and troubleshooting technology, and direct-provider communication with the patient [48].
4.3 The Risk of Unintended Consequences and Gaps in the Literature
Telehealth technologies augment the efficiency and effectiveness of care by predominantly extending the boundary of competences of organization and the people to perform the tasks [52]. This phenomenon is supported by the socio-technical perspective [10], postulating that the technological aspects in the use of the technology place demands on the operators’ perceptual, cognitive, or motor capabilities, and consequently, negative outcomes can be expected [53], sometimes beyond human factors and ergonomics [54].
Our search has identified valuable input for academia and practice, related to potential unintended consequences that must be considered, when implementing Telehealth. Such consequences can be factors that affect quality of care, improve or impede adoption, and therefore, need to be carefully assessed to enhance the governance of telehealth diffusion and reduce the risks. For illustration, we outline some unintended consequences found in the literature reviewed, serving to shape come best practice recommendations.
Risks of Unintended Consequences:
-
Impact of technology interruption on the care provided.
-
Risks from data collection and manipulation practice.
-
Ethical risks in practice including concerns of legal, privacy and confidentiality.
-
Practitioner’s frustration with technology and virtual care (risk of misdiagnosis).
-
Information technology infrastructure and social challenges.
-
Fit for use and usability during normal condition and crisis.
The COVID-19 pandemic coupled with the rapid diffusion of telehealth services grant an unparalleled opportunity to examine related ethical, legal, privacy and confidentiality, information technology infrastructure and social challenges during a time of crisis in healthcare. Practitioners must address ethical concerns for collected health data such as traceability data, during and post pandemic [55]. Further, the diffusion of Telehealth warrants a focus on data collection and manipulation practices. Missing, incorrect, imprecise, and irrelevant data will affect the clinical decisions and in turn jeopardize the quality of care [56]. A quality improvement system shall be established to ensure that services are being provided within best practice guidelines. Guidelines may target education and training, review of clinical records and the ability to intervene in real time with all stakeholders in the system and monitor the quality of the services in telehealth [44, 47, 57, 58].
The literature stipulates that, the rapid diffusion of telehealth services grant an unparalleled opportunity to examine related ethical, legal, privacy and confidentiality, information technology infrastructure and social challenges in healthcare during a time of crisis. Maeder et al. [45] outlined that broadly clinical, administrative concerns, technical issues, legal/ethical concerns, and several other unintended consequences in the delivery of telehealth exist along with challenges affecting its adoption. Nevertheless, the governance of quality of the care provided virtually shall be ensured by monitoring compliance to standardized treatment protocols, data collection procedures, and professional behavior. DeJong et al. [59] elaborated that uniform transparency about care and referral protocols would be helpful. Creating a consumer-dominated regulator, which could compile information on e-visit websites’ performance, may improve outcomes [59]. Future literature should focus on guidance for best practice on ethical data manipulation that may involve user engagement, full disclosure and feedback on justifiable use of information in order to maintain quality care in the ever-extending digital health ecosystem [55].
Moreover, physicians might perceive the absence of the physical contact with the patient leads to inadequate evaluation, missing a diagnosis, inappropriate treatment due to the lack of the tactile examination component, which may delay effective treatment [46, 49]. The delay in patient treatment may lead to higher care expenditures due to potentially preventable conditions. Further, the practice of virtual administration of care may expose health care professionals to “zoom fatigue” which reflects the tiredness and burnout with over utilizing of virtual platforms of communication [60].
Other examples of unintended consequences can range from ethical risks in practice to concerns of misdiagnosis and practitioner’s frustration. The literature reviewed does not provide specific guidance for the safeguards needed in telehealth technologies to reduce such risks. To some degree, cases of abuse and maltreatment are detected when receiving care in person at healthcare organizations. When implementing telemedicine, organizations shall be aware of how to detect such cases (child abuse and other types of abuse) and enforce all the applicable reporting laws [47].
5 Contribution and Further Research Prospects
Telehealth can encourage personalized encounters and assist healthcare providers by increasing their ability to develop improved relationships with patients, which may lead to better patient compliance and thus enhance patient outcomes. Leveraging telehealth may produce a higher level of access and new ways for patients and providers to participate in the care system resulting in increased satisfaction for both patients and providers. Telemedicine while evolving and changing the current landscape of healthcare, it can in a way take us back to a time when home visits were a part of normal practice; however, it is now conducted virtually [58].
We recommend that future research and evaluation studies consider how risks and factors of potential unintended consequences inform telehealth projects, from their planning until their scaling-up [49]. For example, when evaluating the literature, there was lack of evidence in the context of the potential impact of technology interruption on the care provided. The literature did not completely address whether any adverse events took place while providing care virtually and more importantly, how an interruption in the virtual service affected the outcome. Poor connectivity issues, frequent interruptions in the telemedicine calls, login issues, and inadequate quality of image are some of the major technology related drawbacks to easing adoption, with an eminent risk of missed diagnosis [30], hampering the delivery of quality care. Therefore, access to telemedicine software shall be escorted with simple guidelines on its proper use and what to do in case an interruption happens.
Telehealth technologies contribute to equitable and patient centered by paving the way to address other pivotal challenges such as access to rural and underserved areas, availability of technological infrastructure, different people needs, data security, and regulatory framework in order to better help in the deployment of the global telehealth. The implementation of telehealth will help deliver the services and this is measured through the six aims of quality where it shall be as safe, effective, timely and effective, patient centered and responsive to a regular visit. This will help in bridging the gap between the provider and the patient, shorten the distances and expedite care.
Bridging the gap through care at a distance must account for the tradeoff of unintended consequences. Socio-technical theory depicts the harmonic synchronization between the technological aspects and social aspects to gain a successful implementation of a telehealth system [61]. When telehealth technologies are used, decision-making shall incorporate what services to retain or expand and how to measure success, ensure financing, and engage patients and staff [62]. Some noteworthy inquiries about the implementation of telehealth are value, effectiveness, privacy, security, connectivity, reimbursement, and availability issues that may arise from the adoption of telehealth [62]. When scoping to the future, healthcare organizations shall assess the organizational readiness, put the policies in places, and provide education and continuous support, check financial reimbursements, consider technology breakdowns, elaborate laws of physician provisioned services within these new boundaries, and most importantly, consider privacy and confidentiality.
6 Conclusion
From our review, we can infer that, telehealth is proclaimed to improve accessibility, especially in underserved areas, to meet patient needs [34]. Hence, telehealth may ameliorate the convenience for patients whilst lessening the health services cost and expanding opportunities for clinicians. As we look forward, virtual care will persist to build the needed foundation to provide safe and effective care with the right clinician, at the right time, and at the convenience of the patient.
Our scoping study was quite informative and good guidance for research and for practice in telehealth diffusion. Our work underscores the need for attention to how such technology diffusion impacts quality measures in care delivery and outcome. The provision of health care services through telehealth technologies has revealed a reassuring effect in the lives of patients. It has the potential to offer safe, timely and effective interaction with the healthcare provider at the convenience of the patient (according to his or her time schedule, saving travel time for those in rural areas). Hence, the delivery of quality care is possible through innovation in telehealth.
In conclusion, our investigation has provided adequate evidence to support the research objective. Yet, we beg to ask the following question: will telehealth remain a support system for well-defined needs or will it expand from specific applications to the mainstream of care delivery? How will the implementation of telehealth with the constantly evolving supportive technology empower healthcare system resilience? We are positive that these questions will prove as good contexts for further research and discovery.
References
Flores, A.P.D.C., Lazaro, S.A., Molina-Bastos, C.G., Guattini, V.L.D.O., Umpierre, R.N., Gonçalves, M.R., Carrard, V.C.: Teledentistry in the diagnosis of oral lesions: a systematic review of the literature. JAMIA 27(7), 1166–1172 (2020)
Turer, R.W., Jones, I., Rosenbloom, S.T., Slovis, C., Ward, M.J.: Electronic personal protective equipment: a strategy to protect emergency department providers in the age of COVID-19. JAMIA 27(6), 967–971 (2020)
Wosik, J., Fudim, M., Cameron, B., Gellad, Z.F., Cho, A., Phinney, D., Tcheng, J.: Telehealth transformation: COVID-19 and the rise of virtual care. JAMIA. 27(6), 957–962 (2020)
Vilendrer, S., Patel, B., Chadwick, W., Hwa, M., Asch, S., Pageler, N., Sharp, C.: Rapid deployment of inpatient telemedicine in response to COVID-19 across three health systems. JAMIA. 27(7), 1102–1109 (2020)
Li, G., Fan, G., Chen, Y., Deng, Z.: What patients “see” doctors in online fever clinics during COVID-19 in Wuhan? JAMIA 27(7), 1067–1071 (2020)
Ramsetty, A., Adams, C.: Impact of the digital divide in the age of COVID-19. JAMIA 27(7), 1147–1148 (2020)
Badr, N.G., Carrubbo, L., Ruberto, M.: Responding to COVID-19: potential hospital-at-home solutions to re-configure the healthcare service ecosystem (2021)
Mann, D.M., Chen, J., Chunara, R., Testa, P.A., Nov, O.: COVID-19 transforms health care through telemedicine: evidence from the field. JAMIA 27(7), 1132–1135 (2020)
Baker, A.: Book: crossing the quality chasm: a new health system for the 21st century. BMJ 323(7322), 1192 (2001)
Bostrom, R.P., Heinen, J.S.: MIS problems and failures: a socio-technical perspective. Part I: The causes. MIS Quarterly 1(3), 17 (1977)
Levac, D., Colquhoun, H., O’Brien, K.K.: Scoping studies: advancing the methodology. Implement. Sci. 5(1), 1–9 (2010)
Snoswell, C., Smith, A.C., Scuffham, P.A., Whitty, J.A.: Economic evaluation strategies in telehealth: obtaining a more holistic valuation of telehealth interventions. J. Telemed. Telecare 23(9), 792–796 (2016)
Slonim, A.D., Pollack, M.M.: Integrating the institute of medicine’s six quality aims into pediatric critical care: relevance and applications. Pediatr. Crit. Care Med. 6(3), 264–269 (2005)
Ekeland, A.G., Bowes, A., Flottorp, S.: Effectiveness of telemedicine: a systematic review of reviews. Int. J. Med. Inform. 79(11), 736–771 (2010)
Fisk, M., Livingstone, A., Pit, S.W.: Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 22(6), e19264 (2020)
Tuckson, R.V., Edmunds, M., Hodgkins, M.L.: Telehealth. N. Engl. J. Med. 377(16), 1585–1592 (2017)
Steinman, M., Morbeck, R.A., Pires, P.V., Abreu Filho, C.A.C., Andrade, A.H.V., Terra, J.C.C., Teixeira Junior, J.C., Kanamura, A.H.: Impact of telemedicine in hospital culture and its consequences on quality of care and safety. Einstein (São Paulo) 13(4), 580–586 (2015)
Mehrotra, A., Paone, S., Martich, G.D., Albert, S.M., Shevchik, G.J.: A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern. Med. 173(1), 72 (2013)
Kahn, J.M., Rak, K.J., Kuza, C.C., Ashcraft, L.E., Barnato, A.E., Fleck, J.C., Hershey, T.B., Hravnak, M., Angus, D.C.: Determinants of intensive care unit telemedicine effectiveness. An ethnographic study. Am. J. Respir. Crit.Al Care Med. 199(8), 970–979 (2019)
Bains, J., Greenwald, P.W., Mulcare, M.R., Leyden, D., Kim, J., Shemesh, A.J., Sharma, R.: Utilizing telemedicine in a novel approach to COVID-19 management and patient experience in the emergency department. Telemed. E-Health. 27(3), 254–260 (2021)
Smith, W.R., Atala, A.J., Terlecki, R.P., Kelly, E.E., Matthews, C.A.: Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 231(2), 216-222.e2 (2020)
Monaghesh, E., Hajizadeh, A.: The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 20(1) (2020)
Schoenfeld, A.J., Davies, J.M., Marafino, B.J., Dean, M., DeJong, C., Bardach, N.S., Kazi, D.S., Boscardin, W.J., Lin, G.A., Duseja, R., Mei, Y.J., Mehrotra, A., Dudley, R.A.: Variation in quality of urgent health care provided during commercial virtual visits. JAMA Intern. Med. 176(5), 635 (2016)
Halpren-Ruder, D., Chang, A.M., Hollander, J.E., Shah, A.: Quality assurance in telehealth: adherence to evidence-based indicators. Telemed. E-Health 25(7), 599–603 (2019)
Flodgren, G., Rachas, A., Farmer, A.J., Inzitari, M., Shepperd, S.: Interactive telemedicine: effects on professional practice and health care outcomes. Published, Cochrane Database of Systematic Reviews (2015)
Donelan, K., Barreto, E.A., Sossong, S., Michael, C., Estrada, J.J., Cohen, A.B., Schwamm, L.H.: Patient and clinician experiences with telehealth for patient follow-up care. Am. J. Manag. Care. 25(1), 40–44 (2019)
Lavin, B., Dormond, C., Scantlebury, M.H., Frouin, P.Y., Brodie, M.J.: Bridging the healthcare gap: building the case for epilepsy virtual clinics in the current healthcare environment. Epilepsy Behav. 111, 107262 (2020)
Wyman, O.: Digital health’s impact on the quadruple aim. Oliver Wyman. https://health.oliverwyman.com/2020/02/digital-health-and-its-impact-on-the-quadruple-aim.html (2020)
Liddy, C., Keely, E.: Using the quadruple aim framework to measure impact of heath technology implementation: a case study of eConsult. J. Am. Board Fam. Med. 31(3), 445–455 (2018)
Gattu, R., Teshome, G., Lichenstein, R.: Telemedicine applications for the pediatric emergency medicine. Pediatr. Emerg. Care 32(2), 123–130 (2016)
Liu, S.X., Xiang, R., Lagor, C., Liu, N., Sullivan, K.: Economic modeling of heart failure Telehealth programs: when do they become cost saving? Int. J. Telemed. Appl. 2016, 1–9 (2016)
Qureshi, I., Raza, H., Whitty, M., Naqvi, Z.: Telemedicine implementation and benefits for quality and patient safety in Pakistan. Knowl. Manag. & E-Learn.: Int. J., 367–377 (2015)
Ashfaq, A., Memon, S.F., Zehra, A., Barry, S., Jawed, H., Akhtar, M., Kirmani, W., Malik, F., Khawaja, A.W., Barry, H., Saiyid, H., Farooqui, N., Khalid, S., Abbasi, K., Siddiqi, R.: Knowledge and attitude regarding telemedicine among doctors in Karachi. Published, Cureus (2020)
Zhai, Y.A.: Call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother. Psychosom. 90(1), 64–66 (2020)
Tan, L.F., Ho Wen Teng, V., Seetharaman, S.K., Yip, A.W.: Facilitating telehealth for older adults during the COVID-19 pandemic and beyond: strategies from a Singapore geriatric center. Geriatr. & Gerontol. Int. 20(10), 993–995 (2020)
Barbash, I.J., Sackrowitz, R.E., Gajic, O., Dempsey, T.M., Bell, S., Millerman, K., Weir, D.C., Caples, S.M.: Rapidly deploying critical care telemedicine across states and health systems during the covid-19 pandemic. Nejm Catal. Innov. Care Deliv. (2020). https://doi.org/10.1056/CAT.20.0301
Ohannessian, R., Duong, T.A., Odone, A.: Global telemedicine implementation and integration within health systems to fight the covid-19 pandemic: a call to action. JMIR Public Health Surveill. 6(2), e18810 (2020)
Knight, P., Bonney, A., Teuss, G., Guppy, M., Lafferre, D., Mullan, J., Barnett, S.: Positive clinical outcomes are synergistic with positive educational outcomes when using telehealth consulting in general practice: a mixed-methods study. J. Med. Internet Res. 18(2), e31 (2016)
Singh, G., Pichora-Fuller, M.K., Malkowski, M., Boretzki, M., Launer, S.: A survey of the attitudes of practitioners toward teleaudiology. Int. J. Audiol. 53(12), 850–860 (2014)
Trettel, A., Eissing, L., Augustin, M.: Telemedicine in dermatology: findings and experiences worldwide—a systematic literature review. J. Eur. Acad. Derm.Logy Venereol. 32(2), 215–224 (2018)
Scott Kruse, C., Karem, P., Shifflett, K., Vegi, L., Ravi, K., Brooks, M.: Evaluating barriers to adopting telemedicine worldwide: a systematic review. J. Telemed. Telecare 24(1), 4–12 (2018)
Nittas, V., von Wyl, V.: COVID-19 and telehealth: a window of opportunity and its challenges. Published, Swiss Medical Weekly (2020)
Chowdhury, A., Hafeez-Baig, A., Gururajan, R., Chakraborty, S.: Conceptual framework for telehealth adoption in Indian healthcare. In: 24th Annual Conference of the Asia Pacific Decision Sciences Institute: Full papers. Asia-Pacific Decision Sciences Institute (APDSI) (2019)
Larburu, N., Bults, R., van Sinderen, M., Hermens, H.: Quality-of-data management for telemedicine systems. Procedia Comput. Sci. 63, 451–458 (2015)
Maeder, A., Mars, M., Hartvigsen, G., Basu, A., Abbott, P., Gogia, S.B.: Unintended consequences of tele health and their possible solutions. Yearb. Med. Inform. 25(01), 41–46 (2016)
McKiever, M.E., Cleary, E.M., Schmauder, T., Talley, A., Hinely, K.A., Costantine, M.M., Rood, K.M.: Unintended consequences of the transition to telehealth for pregnancies complicated by opioid use disorder during the coronavirus disease 2019 pandemic. Am. J. Obstet. Gynecol. (2020)
Pollard, J.S., Karimi, K.A., Ficcaglia, M.B.: Ethical considerations in the design and implementation of a telehealth service delivery model. Behav. Anal.: Res. Pract. 17(4), 298–311 (2017)
Pirtle, C.J., Payne, K.L., Drolet, B.C.: Telehealth: legal and ethical considerations for success. Telehealth Med. Today. 4(2019)
Alami, H., Gagnon, M.P., Fortin, J.P.: Some multidimensional unintended consequences of telehealth utilization: a multi-project evaluation synthesis. Int. J. Health Policy Manag. 8(6), 337 (2019)
Jimenez, G., Spinazze, P., Matchar, D., Koh Choon Huat, G., van der Kleij, R.M., Chavannes, N.H., Car, J.: Digital health competencies for primary healthcare professionals: a scoping review. Int. J. Med. Inform. 143 (2020)
Chen, J., Sun, D., Yang, W., Liu, M., Zhang, S., Peng, J., Ren, C.: Clinical and economic outcomes of telemedicine programs in the intensive care unit: a systematic review and meta-analysis. J. Intensive Care Med. 33(7), 383–393 (2017)
Krings, B.J., Weinberger, N.: Assistant without master? Some conceptual implications of assistive robotics in health care. Technologies 6(1), 13 (2018)
Read, G.J., Salmon, P.M., Lenné, M.G., Stanton, N.A.: Designing sociotechnical systems with cognitive work analysis: putting theory back into practice. Ergonomics 58(5), 822–851 (2015)
Carayon, P.: Sociotechnical systems approach to healthcare quality and patient safety. Work (Reading, Mass.) 41(0 1), 3850 (2012)
Badr, N., Drăgoicea, M., Walletzký, L., Carrubbo, L., Toli, A.M.: Modelling for ethical concerns for traceability in time of pandemic “Do no Harm” or “Better Safe than Sorry!”. In: Proceedings of the 54th Hawaii International Conference on System Sciences, p. 1779 (2021)
Badr, N.G.: Guidelines for health IT addressing the quality of data in EHR information systems. In: Healthinf, pp. 169–181 (2019)
Kaplan, B.: Revisiting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. SSRN Electron. J. Published (2020)
Chuo, J., Macy, M.L., Lorch, S.A.: Strategies for evaluating telehealth. Pediatrics 146(5), e20201781 (2020)
DeJong, C., Santa, J., Dudley, R.A.: Websites that offer care over the internet. JAMA 311(13), 1287 (2014)
Sugarman, D.E., Horvitz, L.E., Greenfield, S.F., Busch, A.B.: Clinicians’ perceptions of rapid scale-up of telehealth services in outpatient mental health treatment. Telemed. E-Health (2021)
Mosavi, N., Santos, M.: Implementation considerations for the applied business intelligence in healthcare (2021)
Haque, S.N.: Telehealth beyond COVID-19. Psychiatr. Serv. 72(1), 100–103 (2021)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Mohtar, L.N., Badr, N.G. (2023). Digital Bridge or Tradeoff: Telehealth Adoption and Healthcare Service Quality. A Scoping Review. In: Za, S., Winter, R., Lazazzara, A. (eds) Sustainable Digital Transformation. Lecture Notes in Information Systems and Organisation, vol 59. Springer, Cham. https://doi.org/10.1007/978-3-031-15770-7_16
Download citation
DOI: https://doi.org/10.1007/978-3-031-15770-7_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-15769-1
Online ISBN: 978-3-031-15770-7
eBook Packages: Business and ManagementBusiness and Management (R0)