Abstract
Diabetic retinopathy (DR) is a microvascular complication that afflicts virtually all patients who have had diabetes mellitus for more than a decade (Klein R, Klein BE, Diabetes in America 1:293-<last-page>, 1995). Despite many years of research, DR remains the leading cause of new-onset blindness in working-aged Americans (<Spi_Author>, Atlanta, GA: Centers for Disease Control and Prevention. U.S, Dept of Health and Human Services, 2020). However, older and newer therapies exist which can be remarkably effective if DR is identified in a timely manner, graded appropriately, and correct intervention is initiated when indicated. This chapter reviews the pathophysiology of DR, the clinical manifestations of the disease, and current guidelines for appropriate disease management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Retinopathy
- Retinal microcirculation
- Vasoproliferative factor
- Glycated proteins
- Isoform
- Vascular endothelial growth factor
Introduction
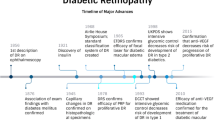
Diabetic retinopathy (DR) is a microvascular complication that afflicts virtually all patients who have had diabetes mellitus for more than a decade [1]. Despite many years of research, there is presently no known cure or means of preventing DR, and DR remains the leading cause of new-onset blindness in working-aged Americans [2]. Nationwide clinical trials in the 1980s and 1990s demonstrated that scatter (panretinal) laser photocoagulation reduces the 5-year risk of severe vision loss (i.e., best corrected visual acuity of 5/200 or worse) from proliferative DR (PDR) from as high as 60% to less than 4%. In addition, these trials demonstrated the efficacy of focal/grid macular laser for treatment of patients with diabetic macular edema (DME). Beginning in the early 2000s, availability of intravitreally delivered vascular endothelial growth factor (VEGF) inhibitors (anti-VEGF) and steroid therapies further improved visual acuity outcomes in patients with DME. Anti-VEGF injections have become the primary therapy for center involving DME with vision loss and also provided an alternative for patients with PDR, as well as vitreous hemorrhages secondary to neovascularization from PDR. Vitrectomy surgery, with endolaser photocoagulation as indicated, can frequently prevent further vision loss or restore useful vision in eyes that have non-resolving vitreous hemorrhage or traction retinal detachment threatening central vision. Although numerous new therapies are currently in development, until a prevention or cure for diabetes and diabetic retinopathy is discovered, the keys to preventing vision loss from DR are regular eye examinations to determine the need for timely laser photocoagulation or anti-VEGF intervention, and rigorous control of blood glucose and any accompanying systemic medical conditions, such as hypertension, renal disease, and dyslipidemias (Fig. 15.1).
Different diabetic retinopathy (DR) severity levels. (Panel a) An eye with no DR and no macular edema on OCT. (Panel b) Moderate–severe NPDR. The eye has extensive cotton wool spots, hemorrhages/microaneurysms, and intraretinal microvascular abnormalities (IRMA). (Panel c) An eye with high-risk proliferative diabetic retinopathy (PDR). Large areas of neovascularization on the disc (NVD) and elsewhere (NVE) along the superotemporal and inferotemporal arcades are seen. (Panel d) An eye with mild NPDR and diabetic macular edema. The macular area has areas of retinal swelling and extensive hard exudate (yellow spots) deposition. An OCT B-scan of the foveal area shows fluid cysts and loss of normal foveal contour
This chapter reviews the current understanding of the etiology and pathophysiology of DR, the clinical manifestations of the disease, and current guidelines for appropriate disease management and future treatment strategies.
Pathophysiology of Diabetic Retinopathy
Early Studies
Diabetic retinopathy is a highly specific retinal vascular complication of both type 1 and type 2 diabetes. Initial studies [3,4,5] of DR concentrated on retinal microaneurysms, an early clinical sign of retinal disease. Cogan, Toussaint, and Kuwabara pioneered many of these early investigations to elucidate the pathophysiology of DR. [3] Microaneurysms were shown to develop bordering areas of occluded capillaries with either normal or hyperplastic endothelial linings [5]. Additionally, a loss of mural cells in the diabetic vessels resulted in outpouchings of the capillary walls. The retinal microaneurysms appeared to develop from these areas that were deficient in mural cells.
The relative retinal ischemia common to DR and numerous other retinal vascular disorders is thought to underlie the development of retinal neovascularization and edema [6, 7]. In 1948, Michaelson postulated that retinal ischemia initiated the release of a vasoproliferative factor [6]. This putative vasoproliferative factor resulted in new vessel growth at the optic disc and other areas of the retina and iris, and might account for the increased vascular permeability associated with these disorders. As discussed below, recent studies have greatly increased our understanding of several now-identified vasoproliferative factors.
Studies using experimentally induced diabetes in dogs demonstrated that hyperglycemia, characterized by deficient insulin activity, is capable of eliciting DR, even in animals that do not have hereditary forms of diabetes [8,9,10,11,12]. Engerman’s studies of alloxan-induced diabetic dogs showed that progression of DR is related to the level of glycemic control, further underscoring the role of hyperglycemia as the underlying etiology of DR.
Present Understanding
Multiple investigations of DR have focused on the biochemical basis of the disease. Studies of numerous biochemical pathways, including the sorbitol pathway, advanced glycation end products (AGEs), and the protein kinase C (PKC) pathway, demonstrate that biochemical changes occur in the retina long before clinically evident abnormalities are observed. These studies suggest that if appropriate novel therapeutic interventions can be identified, early intervention might prevent or reverse the microvascular abnormalities associated with diabetic retinopathy.
Numerous studies have focused on the polyol pathway due to the increased flux through this pathway in the diabetic condition. Aldose reductase is present in the pericytes of the retinal capillaries and since damage to the pericytes occurs early in the evolution of DR, the role of aldose reductase in the pathogenesis of DR has been extensively evaluated. Furthermore, aldose reductase is present in nerve tissue and induces depletion of myoinositol, leading to a decrease in nerve conduction velocity in diabetic neuropathy. Inhibitors of aldose reductase have been effective in preventing damage to the lens, in preventing thickening of retinal capillary basement membranes in diabetic animals, and in improving nerve conduction velocity in patients with diabetic neuropathy. Thus, it has been postulated that aldose reductase inhibitors may also be able to prevent, delay, or halt the development or progression of DR. Unfortunately, clinical trials of the aldose reductase inhibitor sorbinil have not proved clinically effective in preventing the progression of DR. [13, 14]
Additional studies have evaluated advanced glycation end products (AGEs). The presence of high concentrations of glucose can result in the glycation of numerous proteins, especially albumin [15]. These glycated proteins adversely affect cellular and capillary function, structure, and metabolism. Exposure to glycated proteins induces changes in the glomerulus similar to those observed in diabetes, as well as changes in the nerves resembling diabetic neuropathy. The effect of AGE in the eye is being actively studied. AGE can affect both the neuronal and vascular components of the eye, as well as induce numerous growth factors. As such, it may play a role in the progression of diabetic retinopathy.
Other studies have concentrated on the hyperglycemia-induced activation of protein kinase C (PKC), which can affect a wide range of vascular functions, including vascular permeability, contractility, retinal blood flow, and growth factor expression and signal transduction [16, 17]. Hyperglycemia is known to increase the level of diacylglycerol (DAG), which is the physiologic activator of PKC. Much of the vascular dysfunction associated with diabetes is thought to be mediated through this increased action of PKC. There are numerous isoforms of PKC; however, in the retina, PKC α, β, and δ are primarily expressed. Investigations have suggested that the β isoform of PKC is principally associated with the pathology associated with the diabetic state [18]. In laboratory animals, PKC β selective inhibitors have been shown to ameliorate renal dysfunction, retinal blood flow abnormalities, vascular permeability [19], and neovascularization associated with diabetes and diabetes-like models [20]. In addition, activation of PKC is partially involved in the expression of critical growth factors, such as vascular endothelial growth factor (VEGF) [14], which mediates much of the neovascularization and vascular permeability in the eye. Thus, inhibition of the β isoform PKC may possibly block numerous pathological processes in the diabetic condition that result in the vascular dysfunction and ocular complications associated with DR. Since a PKC β selective inhibitor has been shown to be well tolerated in animals and ameliorates many of the abnormalities associated with diabetes, these molecules have also been evaluated in clinical trials. These studies have demonstrated that although PKC beta inhibition using ruboxistaurin does not prevent the progression of diabetic retinopathy, it may have a beneficial effect on macular edema and on reducing vision loss and need for laser therapy for diabetic macular edema [21, 22]. The magnitude of the effect however, did not support further use in the clinic.
The 50-Year Medalist study at the Joslin Diabetes Center has evaluated over 1000 patients who have survived 50 or more years of insulin-dependent diabetes [23, 24]. The study has identified a potential factor associated with protection from advanced DR in this cohort. Retinol binding protein 3 (RBP3) was found at higher concentrations in retina and vitreous samples from Medalist patients with no to mild NPDR versus PDR [25]. Data from preclinical studies have since suggested that this photoreceptor-secreted protein may have effects on the vascular and neural retina mediated by its binding to GLUT1 receptors and secondary decreased expression of vascular endothelial growth factor (VEGF).
Genetic Risk Factors
From early concordant twin studies it has been postulated that genetic risk factors exist between onset, severity, and progression of DR. [26] There has been recent focus on possibly elucidating these genetic risk factors which may delay or hasten the progression to severe PDR. There are published reports on two unique cohorts of patients with type 1 DM of more than 50 years. A possible genetically determined protective effect against the development of diabetic nephropathy and large vessel disease was seen in the Golden Years cohort in the UK [24]. The Joslin Diabetes Center’s 50-year Medalist cohort has observed that only approximately 50% of type 1 diabetic patients with extreme duration diabetes have developed PDR despite decades of hyperglycemia [27]. These two cohorts point to a possible genetic susceptibility or resistance to the development of PDR in these unique cohorts with extreme durations of diabetes. In addition, common genetic factors may be involved in the development of PDR and end-stage renal disease among diabetic patients due to the high degree of concordance of these two complications [28].
Candidate gene approaches look at specific allele or gene variants associated with disease mechanism. These studies have evaluated a large number of potential genetic associations with diabetic eye disease but have not yielded consistent of reproducible results. The best known and most studied is the VEGF gene [29,30,31]. The most common polymorphism, rs2010963, has yielded inconsistent results with only one out of four large meta-analyses confirming its relationship with advanced diabetic retinopathy [32,33,34,35]. Studies have identified a specific SNP at the promoter of the erythropoietin gene, located at 7q21, that is associated with higher rates of development of severe diabetic eye and kidney complications [36]. Erythropoietin has previously been shown to be angiogenic in the eye [37]. The promoter polymorphism identified [36] results in the formation of an AP1 transcription binding site with 25-fold increase in promoter activity. Indeed, patients with this polymorphism have 7.5-fold increased erythropoietin concentration in the vitreous of the eye. One of the largest studies to look at candidate genes in DR was the Candidate gene Association Resource (CARe) [38]. Upon evaluating 2691 participants with type 2 DM, the study did not find an association between the commonly studied candidate genes and DR.
In contrast to the candidate gene approach, genome-wide association studies (GWAS) explore the entire genome, offering an unbiased approach to all potential genetic associations [39, 40]. The GWAS approach has been used in many populations, but results have been variable and most identified variants have not been reproduced in other populations or independent cohorts [41,42,43,44]. Possible reasons could include relatively small sample sizes in these studies, failure to account for potential confounders, such as diabetes duration, and a frequent lack of clear definitions for cases and controls [45].
Whole exome sequencing (WES) attempts to overcome some of the limitations in GWAS by sequencing only the protein coding regions (exons), thereby not including non-coding regions [46]. There have only been a few studies that have implemented this technique and future studies with larger cohorts will demonstrate if an association between specific gene variants and DR can be found using this approach [47, 48].
Natural History and Clinical Features of Diabetic Retinopathy
Epidemiology
In 2019, it was estimated that 463 million people worldwide have diabetes [49, 50]. This number is projected to increase to 700 million by 2045. A recent meta-analysis that included data from 22,896 patients with diabetes found that the overall prevalence was 34.6% for any DR, 6.81% for DME, and 10.2% for vision threatening diabetic retinopathy (combination of moderate NPDR or worse and DME) [51].
Early data from the 1980s suggested that 25% of patients with type 1 and 15.5% with type 2 DM developed advanced proliferative diabetic retinopathy (PDR) after 15 years of diabetes [52, 53]. Of note, these numbers were reported prior to landmark clinical trials establishing the importance of intensive glycemic control on limiting DM complications both systemically and within the eye. The change in trend was reflected in a large meta-analysis looking at 27,120 diabetic patients with 10 years or more of follow-up and determined that the 4 and 10 year risk of progression to PDR was substantially lower in the 1986–2008 cohort compared to the 1975–1985 one [54].
DR is the most frequent cause of new-onset blindness among American adults aged 20–74 years. In the Wisconsin Epidemiologic Study of Diabetic Retinopathy, approximately 4% of younger-onset patients (aged <30 years at diabetes diagnosis) and nearly 2% of older-onset patients (aged ≥30 years at diabetes diagnosis) were legally blind. In the younger-onset group, 86% of blindness was attributable to DR. In the older-onset group, where other eye diseases were also common, 33% of the cases of legal blindness were due to DR. [55, 56] Rates of blindness and visual impairment from DR have decreased in some developed countries in the modern era due to improvements in DR screening programs, patient education, systemic control, and advances in treatment. However, diabetes-related blindness is still a common cause of vision loss globally and results in health care costs in the United States in excess of $500 million annually [57].
Duration of diabetes is closely associated with the onset and severity of DR. Clinical signs of DR are rare in prepubescent patients with type 1 diabetes, but nearly all patients with type 1 diabetes and more than 60 percent of patients with type 2 diabetes will develop some degree of DR after 20 years [55, 56]. In patients with type 2 diabetes, approximately 20% will have DR at the time of diabetes diagnosis, and most will develop some degree of DR over subsequent decades.
Level of glycemic control is another significant risk factor for the onset and progression of DR. [58,59,60,61,62,63,64,65] Both the Diabetes Control and Complications Trial (DCCT) and the Epidemiology of Diabetes Interventions and Complications (EDIC) Study demonstrated a clear and sustained relationship between hyperglycemia and diabetic microvascular complications, including retinopathy, nephropathy, and neuropathy, among type 1 diabetic patients [58,59,60,61,62,63,64,65] In the DCCT, 1441 patients with type 1 diabetes who had either no retinopathy at baseline (primary prevention cohort) or minimal-to-moderate nonproliferative diabetic retinopathy (NPDR) (secondary progression cohort) were treated by either conventional diabetes therapy (i.e., one or two injections of insulin daily) or intensive diabetes management (i.e., three or more daily insulin injections or a continuous subcutaneous insulin infusion.) The patients were followed for 4–9 years. The DCCT showed that intensive insulin therapy reduced or prevented the development of DR by 27% as compared with conventional therapy. Additionally, intensive therapy reduced the progression of DR by 34–76% and had a substantial beneficial effect over the entire range of DR. This improvement was achieved with an average 10% reduction in HbA1c from 8 to 7.2%. The EDIC study has followed patients enrolled in the DCCT study for nearly three decades after their original DCCT participation. Participants who had been assigned to intensive treatment were encouraged to continue, and participants originally assigned to conventional treatment were advised to change to intensive treatment. The risk reductions observed in the DCCT between the rates of microvascular complications in the intensive compared to conventional treatment were sustained throughout 18 years of follow-up [60, 66]. These beneficial effects were achieved despite a continuously narrowing difference in HbA1c between groups which was not statistically significant by 5 years of follow-up [60]. Furthermore, over a median follow-up of 23 years, intensive glycemic control was associated with a 48% risk reduction in diabetes-related ocular surgeries and a 37% risk reduction in all ocular procedures [67]. This finding underscores the need for intensive diabetes management as soon as it is safely possible which should be sustained with a target HbA1c level of 7.0% or less. Although intensive therapy does not prevent DR completely, when begun early before microvascular complications are present; it is effective in significantly reducing the risk of development and progression of DR.
The United Kingdom Prospective Diabetes Study (UKPDS) found similar results for patients with type 2 diabetes. In the UKPDS, 4209 patients with newly diagnosed type 2 diabetes who had either no DR at baseline (primary prevention cohort) or minimal-to-moderate NPDR (secondary progression cohort) were randomly assigned to conventional or intensive blood glucose control, using sulfonylureas and/or insulin. The UKPDS showed that intensive therapy reduced the risk of all microvascular endpoints, including vitreous hemorrhage, retinopathy requiring laser photocoagulation, and renal failure by 25%. Overall, intensive control resulted in a 29% reduction in need for laser photocoagulation, a 17% reduction in a two-step progression of DR, a 24% reduction in the need for cataract extraction, a 23% reduction in vitreous hemorrhage, and a 16% reduction in legal blindness. This improvement was achieved with an average 10% reduction in HbA1c from 7.9% to 7.0% [68, 69].
Renal disease, as manifested by microalbuminuria and proteinuria, is yet another significant risk factor for onset and progression of DR. [70, 71] Similarly, hypertension has been associated with PDR in some studies and may be a risk factor for the development of macular edema [72, 73]. Both renal retinopathy and hypertensive retinopathy can be superimposed on DR. Additionally, elevated serum lipid levels are associated with lipid deposits in the retina (hard exudates) and visual loss [37, 74, 75]. Thus, systemic control of blood pressure, renal disease, and serum lipids are critically important components in the management of DR. [76] In addition, several studies suggest that pregnancy in patients with type 1 diabetes patients may aggravate DR. [77,78,79]
Clinical Findings in Diabetic Retinopathy
Clinical findings associated with early and progressing DR include hemorrhages and/or microaneurysms (H/Ma), cotton wool spots (CWS), hard exudates (HE), intraretinal microvascular abnormalities (IRMA), and venous caliber abnormalities (VCAB), including venous loops, venous tortuosity, and venous beading. Microaneurysms are saccular outpouchings of the capillary walls. These microaneurysms can leak fluid, causing areas of hyperfluorescence on a fluorescein angiogram. Ruptured microaneurysms, as well as leaking capillaries and intraretinal microvascular abnormalities, result in intraretinal hemorrhages. These intraretinal hemorrhages can be “flame shaped” or spot-like in appearance, reflecting the architecture of the layer of the retina in which they occur. Flame-shaped hemorrhages are generally in the nerve fiber layer of the retina, which runs parallel to the retinal surface. Dot or pinpoint hemorrhages are deeper in the retina, reflecting cells that are arranged perpendicular to the retinal surface.
Intraretinal microvascular abnormalities are abnormal vessels located within the retina itself. They may represent either localized intraretinal new vessel growth or shunting vessels through areas of poor vascular perfusion. It is common for IRMA to be found adjacent to cotton wool spots, which are feathery lesions in the nerve fiber layer of the retina resembling the fluffy appearance of cotton. Cotton wool spots are caused by microinfarcts in the nerve fiber layer. Cotton wool spots in a ring or partial ring surrounding the optic nerve head are frequently signs of severe renal disease or hypertension.
Venous caliber abnormalities are a sign of severe retinal hypoxia. Venous caliber abnormalities can be associated with any of the lesions of NPDR; however, in many cases of severe retinal hypoxia, distal retinal areas may be free of nonproliferative lesions due to the extensive vascular loss present. Such “lesion free” areas are termed “featureless retina.”
Vision loss from DR can result from persistent, non-clearing vitreous hemorrhage, traction retinal detachment, retina ischemia, and/or diabetic macular edema. Neovascularization and contraction of the accompanying fibrous tissues can distort the retina and lead to traction retinal detachment. If a traction retinal detachment involves or threatens the macula, irreversible severe vision loss may result. Also, the new vessels may bleed, causing preretinal or vitreous hemorrhage. Pars plana vitrectomy can relieve the traction in cases where vision is threatened and can remove persistent vitreous hemorrhage, often restoring useful vision. The most common cause of vision loss from diabetes, however, is macular disease and macular edema. Macular edema is more likely to occur in patients with type 2 diabetes, which represents 90% or more of the diabetic population. In diabetic macular disease, macular edema or non-perfusion of the capillaries in the macular area results in the loss of central vision.
Classification of Diabetic Retinopathy
DR is broadly classified as nonproliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR). The lesions of NPDR include dot and blot hemorrhages and/or microaneurysms, cotton wool spots, hard exudates, venous caliber abnormalities, and intraretinal microvascular abnormalities. Based on the presence and extent of these retinal lesions, NPDR is further classified as mild, moderate, severe, or very severe NPDR. (Table 15.1) PDR is characterized by new vessels on the optic disc (NVD), new vessels elsewhere on the retina (NVE), preretinal hemorrhage (PRH), vitreous hemorrhage (VH), and/or fibrous tissue proliferation (FP). Based on the presence or absence of proliferative lesions, their severity, and their location, PDR is classified as early PDR or high-risk PDR. (Table 15.1) Diabetic macular edema (DME) can be present with any level of diabetic retinopathy and needs to be evaluated in addition to the level of DR. DME that involves or threatens the center of the macula is termed clinically significant macular edema (CSME). (Table 15.1) The level of NPDR establishes the risk of progression to sight-threatening retinopathy and appropriate clinical management as specifically detailed in Table 15.2.
In elucidating the natural history of DR, the Early Treatment Diabetic Retinopathy Study (ETDRS) evaluated the risks of progression from no or minimal DR to sight-threatening PDR. Importantly, the ETDRS showed that certain nonproliferative lesions, particularly venous beading, intraretinal microvascular abnormalities, and hemorrhages and/or microaneurysms are significant prognosticators for the development of proliferative disease within a 12-month period. Pregnancy, puberty, and cataract surgery can accelerate these changes.
In an effort to standardized classification of DR across international borders and among different health care providers, leaders from various groups and nations (the Global Diabetic Retinopathy Project Group) established and promulgated the Proposed International Classification of Diabetic Retinopathy [80]. (Table 15.3) This classification identifies three levels of NPDR and one level of PDR. With regard to macular edema, two major categories—macular edema present and macular edema absent—are identified. If macular edema is present, three categories are defined: macular edema not threatening the center of the macula, macula edema threatening the center of the macula, and macula edema involving the center of the macula.
Recently, optical coherence tomography (OCT) has become the benchmark to diagnose and monitor diabetic macular edema. OCT has also been accompanied by widespread use of intravitreal anti-VEGF and steroid medications to treat DME. OCT has been used to monitor patient response to injections and drive therapy. Clinical trials exploring the effects of anti-VEGF as well as novel therapeutics routinely use OCT. As such, current diabetic macular edema classification is based on central subfield thickness (CST), which is the average thickness of a circular area 1 mm in diameter centered around the center point [81]. A large multicenter study looking at CST OCT measurements in patients with mild or no DR proposed values of ≥320 μm for males and 305 μm for females (approximately 2 SDs above the average of the normative cohort) to be used to determine the presence or absence of DME [82]. Of note, these measurements are for the Heidelberg OCT machine and values are different on other devices [83]. These cut-off values are routinely used in clinical trials to enroll, treat, and monitor patients. If a patient has CST values greater than the cut-off they are deemed to have center involved macular edema (ciDME), while if edema is present but CST values are below threshold they are graded as having non-ciDME.
While CST values are diagnostic for ciDME, they are not the only determinant for treatment. Post hoc analysis by the DRCR Retina Network has found only a moderate correlation between CST thickness and visual acuity [84]. As such, there are patients with extensive thickening and excellent VA, while others have mild thickening and poor VA. Therefore, in current treatment algorithms, both VA and CST are used to determine initiation, continuance, and deferral of therapy.
Treatment of Diabetic Retinopathy
Overview
Appropriate clinical management of DR was initially defined by five major, randomized, multicentered clinical trials: the Diabetic Retinopathy Study (DRS) [85,86,87,88,89,90,91,92,93,94,95], the Early Treatment Diabetic Retinopathy Study (ETDRS) [73, 74, 96,97,98,99,100,101,102,103], the Diabetic Retinopathy Vitrectomy Study (DRVS) [104,105,106,107,108], the Diabetes Control and Complications Trial (DCCT) [58, 61,62,63,64,65], and the United Kingdom Prospective Diabetes Study (UKPDS) [68, 109]. These studies elucidated delivery and proper timing for laser photocoagulation surgery for the treatment of both DR and DME [110,111,112,113,114,115]. They also established guidelines for vitrectomy surgery. The DRS demonstrated that scatter (panretinal) laser photocoagulation was effective in reducing the risk of severe vision loss from PDR by 50% or more.
The ETDRS was a multicenter, randomized clinical study designed to test [1] whether 650 mg of aspirin per day had any effect on the progression of diabetic retinopathy, [2] whether focal laser photocoagulation for macular edema reduced the risk of moderate vision loss (i.e., a doubling of the visual angle, e.g., 20/20 reduced to 20/40), and [3] whether scatter laser photocoagulation was more beneficial in reducing the risk of severe vision loss (i.e., best corrected visual acuity of 5/200 or worse) when applied prior to the development of high-risk PDR, as defined below. The ETDRS enrolled 1377 patients at 22 centers nationwide. Major conclusions of the ETDRS were as follows: [1] a daily dose of 650 mg of aspirin does not prevent the development of high-risk proliferative retinopathy and does not reduce the risk of visual loss, nor does it increase the risk of vitreous hemorrhage; [2] focal laser photocoagulation for diabetic macular edema reduces the risk of moderate visual loss by at least 50%, from nearly 30% to less than 15%; and [3] both early scatter laser photocoagulation and photocoagulation at the time of reaching high-risk PDR result in significant reduction in the risk of severe visual loss to less than 4%, although some groups, including those with type 2 diabetes or type 1 diabetes of long duration, have a greater benefit from early treatment [116]. As mentioned above, the ETDRS also clarified the natural history of DR and the risk of progression of DR based on the baseline level of retinopathy [110,111,112,113].(Table 15.1) Finally, the ETDRS identified specific lesions that placed an eye at high risk for visual loss [111]. These lesions include H/Ma, VCAB, and IRMA as detailed in Table 15.1. Based on ETDRS findings, proper diagnosis of the level of DR (Table 15.2) determines appropriate timing of follow-up evaluation and when to initiate laser photocoagulation.
The DRVS demonstrated that early vitrectomy was useful in restoring vision for some persons who have severe vision loss due to vitreous hemorrhage. In addition, the DRVS demonstrated that persons with severe fibrovascular proliferation were more likely to obtain better vision, and less likely to have poor vision, when PPV as performed early. The DRVS demonstrated the value of vitrectomy in restoring useful vision, particularly in patients with type 1 diabetes. The treatment benefits demonstrated in the DRVS, which was completed in 1989, are not totally applicable today due to dramatic advances in surgical techniques, the advent of endolaser photocoagulation, and the use of anti-VEGF therapy.
The understanding of the role of growth factors in DR and DME has grown significantly over the past decade [29, 117]. Multiple growth factors mediate both the neovascularization of PDR and the increased permeability associated with DME. VEGF is believed to be one of the fundamental growth factors involved in these processes in the eye. This central role of VEGF in the pathogenesis of retinal neovascularization and vascular leakage has triggered a new paradigm in the management of retinal disease with pharmacologic agents. Intravitreal injections of anti-VEGF agents have been shown to inhibit the development of choroidal and retinal neovascularization and decrease the amount of vascular leakage. These compounds are injected into the vitreous cavity of the eye on a repetitive basis and have robust and consistent clinical data to demonstrate beneficial activity. The marked beneficial effect induced by anti-VEGF agents in eyes with severe neovascularization of the retina and anterior segment has dramatically improved the treatment of those cases where the severity of the condition precluded laser treatment [118, 119]. Ranibizumab and aflibercept have been FDA approved for the treatment indications of DR and DME.
Many of the clinical studies and trials that have shaped clinical care for DR and DME in the modern era have been performed by the DRCR Retina Network. The DRCR Retina Network is a National Institutes of Health-sponsored collaborative network dedicated to multicenter clinical trial research of retinal diseases, including DR, DME, and associated disorders. Results of phase 3 clinical trials initiated and completed by the Network have established anti-VEGF therapy as the standard of care in the management of DME. They have also established its safety and efficacy in the management of eyes with PDR. These studies have also defined treatment algorithms for the administration of intravitreal medications in both DME and PDR as well as how to incorporate retinal imaging in the management and care of patients.
Proliferative Diabetic Retinopathy
Panretinal Photocoagulation
Both the DRS and the ETDRS demonstrated the value of scatter (panretinal) laser photocoagulation for treating PDR. In scatter laser photocoagulation, 1200 to 1800 laser burns are applied to the peripheral retinal tissue, focused at the level of the retinal pigment epithelium. Large vessels are avoided, as are areas of preretinal hemorrhage. It has been previously thought that treatment should be divided into two or more sessions, spaced one to two weeks apart with follow-up after 3 months from completion of the treatment. Evidence from a multicenter prospective, non-randomized trial has shown that single session PRP may not be as detrimental as previously thought, and may be the same or even better long term than divided treatment [120].
The response to scatter laser photocoagulation varies. The most desirable effect is to see a regression of the new vessels. In some cases, there may be a stabilization of the neovascularization, with no further growth. This response may be acceptable, with careful clinical monitoring. In some cases, new vessels continue to proliferate, requiring additional scatter laser photocoagulation. In cases where neovascularization continues and does not respond to further laser photocoagulation, vitreous hemorrhage and/or traction retinal detachment may occur, possibly requiring surgical intervention with pars plana vitrectomy if vision is threatened. Eyes with high-risk PDR should receive prompt scatter laser photocoagulation. Eyes approaching high-risk characteristics (i.e., eyes with PDR less than high risk, and eyes with severe or very severe NPDR) may also be candidates for scatter laser photocoagulation. Recent progression of the eye disease, status of the fellow eye, compliance with follow-up, concurrent health concerns, such as hypertension or kidney disease, and other factors must be considered in determining if laser surgery should be performed in these patients. In particular, patients with type 2 diabetes should be considered for panretinal photocoagulation prior to the development of high-risk PDR since the risk of severe visual loss and the need for PPV can be reduced by 50% in these patients by early scatter treatment, especially when macular edema is present [116].
Anti-VEGF Therapy
The DRCR Retina Network Protocol S compared the use of intravitreal anti-VEGF (ranibizumab) to PRP in the management of PDR. The study demonstrated that ranibizumab therapy was non-inferior to PRP with regard to visual acuity (VA) outcomes at 2 and 5 years [121]. Moreover, this trial found that eyes treated with anti-VEGF had less visual field loss, less need for vitrectomy, and less frequent development of DME than eyes that received PRP. The effectiveness of intravitreal anti-VEGF therapy for PDR was further confirmed by the CLARITY study, which compared the safety and efficacy of intravitreal aflibercept versus PRP in patients with active PDR [122]. This trial found that aflibercept treatment resulted in superior VA outcomes at 1 year compared to PRP.
Patients in DRCR Protocol S were followed for a total of 5 years. Although, average VA at year 5 was excellent (mean 20/25 in both the ranibizumab and PRP groups), most patients still required at least 1 injection during year 5 [123]. On average, patients received 2.9 injections in both years 4 and 5, with a mean total of 19.2 injections over the 5 years [123]. Therefore, the large number of visits and increased cost associated with anti-VEGF therapy as well as the need for close continued monitoring to manage recurrences are important factors to consider prior to initiating therapy [124].
Diabetic Macular Edema
Focal Laser Photocoagulation
Focal laser for CSME has been shown to be effective in reducing the risk of moderate visual loss [125]. In focal laser photocoagulation, lesions from 300 microns to 3000 microns from the center of the macula that are contributing to thickening of the macula area are directly photocoagulated. These lesions are generally identified by fluorescein angiography and consist primarily of leaking microaneurysms. Although fluorescein angiography is generally used to identify treatable lesions for focal laser photocoagulation, fluorescein angiography is not necessary for the diagnosis of CSME.
Follow-up evaluation following focal laser surgery generally occurs after 3 or 4 months. In the cases where macular edema persists, further treatment may be necessary. Macular laser has a diminished role for treatment of DME in the era of anti-VEGF therapy, but is still of use in eyes that are not candidates for anti-VEGF or as adjunctive therapy when edema persists despite intravitreal anti-VEGF treatment.
Steroid Therapy
Both periocular and intravitreal steroids have been used for the treatment of DME. To validate the initial findings from small case series and uncontrolled clinical trials, two multicenter randomized prospective clinical trials were undertaken to address both the effectiveness and safety of both routes of steroid administration. Peribulbar steroid injections were found to have no significant benefit for the treatment of DME and further study of the approach has been currently abandoned [126]. The results of a 2-year trial comparing intravitreal steroids to focal laser have shown that despite an initial rapid reduction in retinal thickness and improvement in vision with the intravitreal steroid injection, by 1 year the results were no better than laser photocoagulation, and after 2 years, the steroid was inferior to the laser treatment in both visual outcome and retinal thickness. In addition, there was an approximately fourfold increase in the rate of intraocular pressure complications and a fourfold increase in need for cataract surgery in the steroid-treated group [125].
Another large multicenter study compared intravitreal anti-VEGF to macular laser and intravitreal steroid therapy (Triamcinolone) and demonstrated that although intravitreal steroids were associated with initial VA gains, this was followed by a decrease in mean VA after week 24 [127, 128]. At years 1 and 2, VA gains were not significantly different between the steroid group and the laser group (+1.1 letters and −1.5 letters mean difference at 1 and 2 years, respectively) [127, 128]. These findings may have been due in part to the development of cataracts or the negative impact of cataract surgery on macular edema in triamcinolone group eyes. A subgroup analysis in triamcinolone-treated eyes that were pseudophakic at baseline demonstrated that the visual acuity results were substantially better than for phakic eyes. Approximately 50% of eyes in the triamcinolone group had an intraocular pressure (IOP) elevation >10 mmHg from baseline, IOP >30, or initiation of IOP lowering medications at 1 or more visits during 2 years of follow-up. In addition, 59% required cataract surgery during the 2 years of follow-up. Given these results, intravitreal steroid therapy is generally regarded as second-line treatment for most eyes with DME unless they are not candidates for anti-VEGF injections.
Anti-VEGF Therapy
The DRCR Retina Network Protocol I was one the first phase 3 study to compare the following treatments for ci-DME: intravitreal ranibizumab, intravitreal triamcinolone (TA), and macular laser. The study helped establish anti-VEGF as the current standard of care in the management of patients with ci-DME. This trial showed that ranibizumab therapy was highly effective in the treatment of ci-DME, with patients gaining on average 8 or 9 letters compared to only 3 letters in the laser group at 1 year [127, 128]. Furthermore, the visual acuity (VA) gains achieved in the first year with ranibizumab were maintained all through the 5-year follow-up with a decreasing frequency of injections reaching a median of 0–1 injections in the fourth and fifth year [129].
The DRCR Retina Network also sought to compare available anti-VEGF medications and in a large multicenter study (Protocol T) compared the three available treatments; bevacizumab, ranibizumab, and aflibercept [130]. The study demonstrated that in patients with a baseline VA of 20/32–20/40, visual outcomes with all three anti-VEGF medications were similar [130]. In contrast, in patients with a VA of 20/50 or worse at baseline, aflibercept was associated with significantly more VA gains and DME resolution compared to both ranibizumab and bevacizumab at 1 year. By the second year, although the differences between aflibercept and ranibizumab decreased and were no longer significant, aflibercept was still superior to bevacizumab [131].
Because the inclusion criteria for most initial studies of anti-VEGF for DME required a baseline VA of 20/32 or worse, there were no clear guidelines for patients with a VA of 20/25 or better and ci-DME [132]. The DRCR Retina Network Protocol V explored a strategy of initial observation with anti-VEGF if needed for visual worsening during follow-up, macular laser with anti-VEGF treatment if needed for vision loss or initial intravitreal aflibercept (anti-VEGF) at baseline in patients with a VA of 20/25 or better and ci-DME on OCT. The study concluded that the rates of visual loss were similar in all three groups and at 2 years the mean visual acuity was 20/20 in each group. These findings suggest that for most eyes with good baseline vision despite ciDME, a strategy of initial observation with subsequent initiation of anti-VEGF if VA were to decrease is a viable strategy. The subsequent Protocol AC study demonstrated that a specific form of step therapy using bevacizumab first, followed by aflibercept when outcomes were suboptimal, resulted in similar visual acuity outcomes to aflibercept monotherapy in eyes with moderate visual impairment from CI-DME.
Vitrectomy for Advanced PDR
In cases with vitreous hemorrhage secondary to PDR, a recent randomized controlled trial compared a strategy of intravitreal aflibercept versus immediate vitrectomy with PRP [133]. The study reported there were no significant differences in mean VA score between both groups at 24 weeks. Eyes assigned to vitrectomy had faster visual recovery and greater clearance of vitreous hemorrhage over the first 4 weeks of the study. The study thus suggests that both treatment strategies are reasonable approaches to cases of vitreous hemorrhage from PDR that are uncomplicated by macula-threatening vitreoretinal traction. However, vitrectomy still remains the only treatment available to relieve traction that involves or threatens the center of the macula.
Novel Treatments
Numerous recent advances in our understanding of the basic mechanisms underlying the progression of DR have raised the possibility of novel therapies against the progression of NPDR, PDR, and DME.
Fenofibrate
Two phase 3 studies of the peroxisome proliferator-activated receptor α medication, fenofibrate, have suggested that this oral agent may prevent worsening of early stage DR. The Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study randomized 9795 study participants with type 2 diabetes to fenofibrate versus placebo [134]. The need for laser treatment for DR or DME was significantly lower in the fenofibrate group (HR 0.69, 95% CI 0.56–0.84, P = 0.0002) [135]. In addition, eyes with existing DR at baseline demonstrated a significant reduction in DR worsening with fenofibrate treatment (3.1% versus 14.6%, P = 0.004). The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial subsequently evaluated ocular-specific outcomes in participants randomized within a 2x2 factorial design to simvastatin in combination with either fenofibrate or placebo [136]. At 4 years, DR worsening was significantly less frequent in the fenofibrate group (6.5% versus 10.2%, adjusted OR, 0.60, 95% CI, 0.42–0.86, P = 0.0056). The DRCR Retina Network is currently conducting a phase 3 trial of fenofibrate versus placebo for prevention of DR worsening in eyes with mild to moderately severe NPDR.
Plasma Kallikrein Inhibitors (PKI)
Preclinical data has demonstrated that plasma kallikrein contributes to DME development through both VEGF-dependent and -independent mechanisms [137, 138]. Although there are several PKI in development, KVD001 is the furthest one along. A phase 2 clinical trial compared two doses of intravitreal KVD001 (6 μg and 3 μg) with sham injections in patients with ci-DME [139]. There were no significant differences between VA gains in the treatment groups vs sham. However, the group treated with KVD001 6 μg had less vision loss than that given sham injections (32.5% vs. 54.5%, p = 0.042) at 16 weeks. Larger clinical trials are needed to definitively establish efficacy or lack thereof for the indication of DME.
Ang-Tie2 Targeting Drugs
The Tie2 signaling pathway is specific to vascular endothelial cells. Tie2 signaling is responsible for the maintenance of vascular health, promoting endothelial cell survival and stability. Angiopoietin 1 (Ang1) is a Tie2 agonist, while Ang2 is predominantly a Tie2 inhibitor. Under conditions of hypoxia and hyperglycemia, Ang2 is upregulated and in turn potentiates the action of VEGF [140,141,142]. The inhibition of Tie2 receptors by Ang2 disrupts its pro-vascular stabilizing effects, in turn resulting in increased vascular permeability and disruption of vascular structure [143, 144].
There have been many drugs targeting this signaling pathway but the only one currently in phase 3 clinical trials for DME is faricimab. Faricimab is a bispecific antibody that binds to both VEGF and Ang2. Recent results from the phase 2 BOULEVARD trial demonstrated that the 6.0 mg faricimab dose demonstrated a statistically significant gain of vision compared to ranibizumab 0.3 mg (+3.6 letters, p = 0.03) at 24 weeks [145]. In addition, an observation period from week 24 to week 36 showed that eyes treated with faricimab had a longer time to re-treatment compared to ranibizumab. Phase 3 results from the YOSEMITE and RHINE studies were recently reported as showing non-inferior visual outcomes of intravitreal faricimab to aflibercept treatment after 1 year of treatment. Extended dosing with treatment intervals of 16 weeks were achieved by over 50% of study participants treated with Faricimab [146].
Photobiomodulation
Photobiomodulation (PBM), or irradiation by light in the far-red (FR) to near-infrared (NIR) light spectrum (630–900 nm), has recently been explored for the treatment of DME. In the retina of diabetic mice PBM inhibited the generation of superoxide and decreased the expression of iNOS and MnSOD [147, 148]. In addition, PBM decreased vascular leakage and capillary degeneration [149]. Preliminary human studies enrolling 4 to 10 patients with DME were consistent with a favorable anatomic response with improvement in edema in PBM-treated eyes and an acceptable safety profile [150, 151]. However, the DRCR Retina Network Protocol AE, a phase 2 randomized trial did not find any clinical benefit from PBM versus placebo in the eyes of patients with ciDME and vision of 20/25 or better.
Conclusions/Summary
Appropriate management of DR and diabetic eye disease requires a thorough knowledge of both diabetes mellitus and the findings from key multicentered, randomized clinical trials, such as the DRS, ETDRS, DRVS, DCCT, UKPDS, and the recent trials by the DRCR Retina Network. Accurate diagnosis of DR severity level is essential to determine appropriate care and follow-up schedules and to assess the need for timely laser photocoagulation for PDR and DME. Since DR usually causes no symptoms when it is most amenable to treatment, strategies to reduce the risk of vision loss must stress the need for regular eye examination, even in patients with no ocular complaints [152]. (Table 15.4) Currently, patients with type 1 diabetes ten years of age and older are encouraged to have a comprehensive, dilated retinal eye examination within three to five years of diagnosis, and at least annually thereafter. Patients with type 2 diabetes are encouraged to have a comprehensive, dilated eye examination at the time of diagnosis, and at least annually thereafter. Patients contemplating pregnancy should have their eyes examined prior to conception whenever possible and pregnant women should have their eyes examined early in the first trimester and each trimester thereafter. In all cases, abnormal findings may require accelerated examination schedules, and the presence of concurrent medical conditions, such as hypertension and renal disease, may also require more frequent ocular examination and should be aggressively controlled in conjunction with the patient’s internist or diabetologist.
Our understanding of DR has expanded dramatically in the past 30 years. Treatment modalities that can substantially reduce visual loss have been developed and extensively validated; however, these therapies are not yet ideal and active research is continuing into methods of curing or preventing DR. Until these milestones are reached, current strategies must continue to address the critical need for regular eye examination, optimal systemic control and prompt, appropriate laser photocoagulation, intravitreal anti-VEGF therapy, and/or vitrectomy when indicated.
ADA Guidelines [116, 152]
-
1.
Patients >10 years of age with type 1diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 3–5 years after the onset of diabetes. In general, screening for diabetic eye disease is not necessary before 10 years of age. Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist shortly after the diagnosis of diabetes is made.
-
2.
Subsequent examinations for both type 1 and type 2 diabetic patients should be repeated annually by an ophthalmologist or optometrist who is knowledgeable and experienced in diagnosing the presence of diabetic retinopathy and is aware of its management. Examinations will be required more frequently if retinopathy is progressing.
-
3.
When planning pregnancy, women with preexisting diabetes should have a comprehensive eye examination and should be counseled on the risk of development and/or progression of diabetic retinopathy. Women with diabetes who become pregnant should have a comprehensive eye examination in the first trimester and close follow-up throughout pregnancy. This guideline does not apply to women who develop gestational diabetes because such individuals are not at increased risk for diabetic retinopathy.
-
4.
Patients with any level of macular edema, severe NPDR, or any PDR require the prompt care of an ophthalmologist who is knowledgeable and experienced in the management and treatment of diabetic retinopathy. Referral to an ophthalmologist should not be delayed until PDR has developed in patients who are known to have severe non-proliferative or more advanced retinopathy. Early referral to an ophthalmologist is particularly important for patients with type 2 diabetes and severe NPDR, since laser treatment at this stage is associated with a 50% reduction in the risk of severe visual loss and vitrectomy.
-
5.
Patients who experience vision loss from diabetes should be encouraged to pursue visual rehabilitation with an ophthalmologist or optometrist who is trained or experienced in low-vision care.
Abbreviations
- CSME:
-
Clinically significant diabetic macular edema
- DCCT:
-
Diabetes Control and Complications Trial
- DME:
-
Diabetic macular edema
- DR:
-
Diabetic retinopathy
- EDIC:
-
Epidemiology of Diabetes Interventions and Complications study
- H/Ma:
-
Hemorrhages and microaneurysms
- IRMA:
-
Intraretinal microvascular abnormalities
- NPDR:
-
Nonproliferative diabetic retinopathy
- NVD:
-
New vessels on the disc
- NVE:
-
New vessels elsewhere
- PDR:
-
Proliferative diabetic retinopathy
- PKC:
-
Protein kinase C
- PPV:
-
Pars plana vitrectomy
- PRP:
-
Panretinal photocoagulation (scatter laser treatment)
- UKPDS:
-
United Kingdom Prospective Diabetes Study
- VCAB:
-
Venous caliber abnormalities
- VEGF:
-
Vascular endothelial growth factor
- WESDR:
-
Wisconsin Epidemiologic Study of Diabetic Retinopathy
References
Klein R, Klein BE. Vision disorders in diabetes. Diabetes in America. 1995;1:293.
National Diabetes Statistics Report, 2020. Atlanta, GA: centers for disease control and prevention, U.S. Dept of Health and Human Services, 2020.
Cogan DG, Toussaint D, Kuwabara T. Retinal vascular patterns. IV. Diabetic retinopathy. Arch Ophthalmol. 1961;66:366–78.
Cogan DG, Kuwabara T. Capillary shunts in the pathogenesis of diabetic retinopathy. Diabetes. 1963;12:293–300.
Cogan DG, Kuwabara T. The mural cell in perspective. Arch Ophthalmol. 1967;78:133–9.
Michaelson IC. The mode of development of the vascular system in the retina: with some observations on its significance for certain retinal diseases. Trans Ophthalmol Soc. 1948;68:137–80.
Ashton N, Ward B, Serpell G. Effect of oxygen on developing retinal vessels with particular reference to the problem of retrolental fibroplasia. Br J Ophthalmol. 1954;38:397–432.
Engerman RL, Kern TS. Experimental galactosemia produces diabetic-like retinopathy. Diabetes. 1984;33:97–100.
Engerman RL, Kern TS. Progression of incipient diabetic retinopathy during good glycemic control. Diabetes. 1987;36:808–12.
Engerman RL, Kern TS. Is diabetic retinopathy preventable? Int Ophthalmol Clin. 1987;27:225–9.
Engerman RL. Pathogenesis of diabetic retinopathy. Diabetes. 1989;38:1203–6.
Engerman RL, Kern TS. Aldose reductase inhibition fails to prevent retinopathy in diabetic and galactosemic dogs. Diabetes. 1993;42:820–5.
Kikkawa U, Nishizuka Y. The role of protein kinase C in transmembrane signalling. Annu Rev Cell Biol. 1986;2:149–78.
Xia P, Aiello LP, Ishii H, et al. Characterization of vascular endothelial growth factor's effect on the activation of protein kinase C, its isoforms, and endothelial cell growth. J Clin Invest. 1996;98:2018–26.
Monnier VM, Kohn RR, Cerami A. Accelerated age-related browning of human collagen in diabetes mellitus. Proc Natl Acad Sci U S A. 1984;81:583–7.
A randomized trial of sorbinil, an aldose reductase inhibitor, in diabetic retinopathy. Sorbinil retinopathy trial research group. Arch Ophthalmol. 1990;108:1234–44.
The sorbinil retinopathy trial: Neuropathy results. Sorbinil Retinopathy Trial Research Group. Neurology. 1993;43:1141–9.
Ishii H, Jirousek MR, Koya D, et al. Amelioration of vascular dysfunctions in diabetic rats by an oral PKC beta inhibitor. Science. 1996;272:728–31.
Aiello LP, Bursell SE, Clermont A, et al. Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective beta-isoform-selective inhibitor. Diabetes. 1997;46:1473–80.
Danis RP, Bingaman DP, Jirousek M, Yang Y. Inhibition of intraocular neovascularization caused by retinal ischemia in pigs by PKCbeta inhibition with LY333531. Invest Ophthalmol Vis Sci. 1998;39:171–9.
Aiello LP, Davis MD, Girach A, et al. Effect of ruboxistaurin on visual loss in patients with diabetic retinopathy. Ophthalmology. 2006;113:2221–30.
Davis MD, Sheetz MJ, Aiello LP, et al. Effect of ruboxistaurin on the visual acuity decline associated with long-standing diabetic macular edema. Invest Ophthalmol Vis Sci. 2009;50:1–4.
Grunwald JE, Brucker AJ, Schwartz SS, et al. Diabetic glycemic control and retinal blood flow. Diabetes. 1990;39:602–7.
Bain SC, Gill GV, Dyer PH, et al. Characteristics of type 1 diabetes of over 50 years duration (the Golden years cohort). Diabet Med. 2003;20:808–11.
Yokomizo H, Maeda Y, et al. Retinol binding protein 3 is increased in the retina of patients with diabetes resistant to diabetic retinopathy. Sci Transl Med. 2019;11:eaau6627.
Leslie RD, Pyke DA. Diabetic retinopathy in identical twins. Diabetes. 1982;31:19–21.
Keenan HA, Costacou T, Sun JK, et al. Clinical factors associated with resistance to microvascular complications in diabetic patients of extreme disease duration: the 50-year medalist study. Diabetes Care. 2007;30:1995–7.
Clustering of long-term complications in families with diabetes in the diabetes control and complications trial. The diabetes control and complications trial research group. Diabetes. 1997;46:1829–39.
Aiello LP, Avery RL, Arrigg PG, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331:1480–7.
Aiello LP. Angiogenic pathways in diabetic retinopathy. N Engl J Med. 2005;353:839–41.
Miller JW, Adamis AP, Aiello LP. Vascular endothelial growth factor in ocular neovascularization and proliferative diabetic retinopathy. Diabetes Metab Rev. 1997;13:37–50.
Han L, Zhang L, Xing W, et al. The associations between VEGF gene polymorphisms and diabetic retinopathy susceptibility: a meta-analysis of 11 case-control studies. J Diabetes Res. 2014;2014:805801.
Qiu M, Xiong W, Liao H, Li F. VEGF -634G>C polymorphism and diabetic retinopathy risk: a meta-analysis. Gene. 2013;518:310–5.
Lu Y, Ge Y, Shi Y, Yin J, Huang Z. Two polymorphisms (rs699947, rs2010963) in the VEGFA gene and diabetic retinopathy: an updated meta-analysis. BMC Ophthalmol. 2013;13:56.
Xie XJ, Yang YM, Jiang JK, Lu YQ. Association between the vascular endothelial growth factor single nucleotide polymorphisms and diabetic retinopathy risk: a meta-analysis. J Diabetes. 2017;9:738–53.
Tong Z, Yang Z, Patel S, et al. Promoter polymorphism of the erythropoietin gene in severe diabetic eye and kidney complications. Proc Natl Acad Sci U S A. 2008;105:6998–7003.
Watanabe D, Suzuma K, Matsui S, et al. Erythropoietin as a retinal angiogenic factor in proliferative diabetic retinopathy. N Engl J Med. 2005;353:782–92.
Sobrin L, Green T, Sim X, et al. Candidate gene association study for diabetic retinopathy in persons with type 2 diabetes: the candidate gene association resource (CARe). Invest Ophthalmol Vis Sci. 2011;52:7593–602.
Chang M, He L, Cai L. An overview of Genome-Wide association Studies. Methods Mol Biol. 2018;1754:97–108.
Dehghan A. Genome-Wide Association Studies. Methods Mol Biol. 2018;1793:37–49.
Fu YP, Hallman DM, Gonzalez VH, et al. Identification of diabetic retinopathy genes through a Genome-Wide association study among Mexican-Americans from Starr County, Texas. J Ophthalmol. 2010;2010:861291.
Grassi MA, Tikhomirov A, Ramalingam S, Below JE, Cox NJ, Nicolae DL. Genome-wide meta-analysis for severe diabetic retinopathy. Hum Mol Genet. 2011;20:2472–81.
Meng W, Shah KP, Pollack S, et al. A genome-wide association study suggests new evidence for an association of the NADPH oxidase 4 (NOX4) gene with severe diabetic retinopathy in type 2 diabetes. Acta Ophthalmol. 2018;96:e811–9.
Awata T, Yamashita H, Kurihara S, et al. A genome-wide association study for diabetic retinopathy in a Japanese population: potential association with a long intergenic non-coding RNA. PLoS One. 2014;9:e111715.
Cho H, Sobrin L. Genetics of diabetic retinopathy. Curr Diab Rep. 2014;14:515.
Lalonde E, Albrecht S, Ha KC, et al. Unexpected allelic heterogeneity and spectrum of mutations in fowler syndrome revealed by next-generation exome sequencing. Hum Mutat. 2010;31:918–23.
Shtir C, Aldahmesh MA, Al-Dahmash S, et al. Exome-based case-control association study using extreme phenotype design reveals novel candidates with protective effect in diabetic retinopathy. Hum Genet. 2016;135:193–200.
Ung C, Sanchez AV, Shen L, et al. Whole exome sequencing identification of novel candidate genes in patients with proliferative diabetic retinopathy. Vis Res. 2017;139:168–76.
https://idf.org/aboutdiabetes/what-is-diabetes/facts-figures.html.
Cho NH, Shaw JE, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. IX. Four-year incidence and progression of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1989;107:237–43.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. X. Four-year incidence and progression of diabetic retinopathy when age at diagnosis is 30 years or more. Arch Ophthalmol. 1989;107:244–9.
Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16–64 years), 1999–2000 with 2009–2010. BMJ Open. 2014;4:e004015.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. II. Prevalence and risk of diabetic retinopathy when age at diagnosis is less than 30 years. Arch Ophthalmol. 1984;102:520–6.
Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin epidemiologic study of diabetic retinopathy. III. Prevalence and risk of diabetic retinopathy when age at diagnosis is 30 or more years. Arch Ophthalmol. 1984;102:527–32.
Diabetic Retinopathy. https://www.cdc.gov/visionhealth/pdf/factsheet.pdf.
DCCT Research Group. Are continuing studies of metabolic control and microvascular complications in insulin-dependent diabetes mellitus justified? The diabetes control and complications trial. N Engl J Med. 1988;318:246–50.
Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the epidemiology of diabetes interventions and complications (EDIC) study. JAMA. 2003;290:2159–67.
Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Effect of intensive therapy on the microvascular complications of type 1 diabetes mellitus. JAMA. 2002;287:2563–9.
Hypoglycemia in the Diabetes Control and Complications Trial. The diabetes control and complications trial research group. Diabetes. 1997;46:271–86.
Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group. JAMA. 1996;276:1409–15.
Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the diabetes control and complications trial. Diabetes. 1995;44:968–83.
Progression of retinopathy with intensive versus conventional treatment in the diabetes control and complications trial. Diabetes control and complications trial research group. Ophthalmology. 1995;102:647–61.
Moriarty AP, Spalton DJ, Shilling JS, Ffytche TJ, Bulsara M. Breakdown of the blood-aqueous barrier after argon laser panretinal photocoagulation for proliferative diabetic retinopathy. Ophthalmology. 1996;103:833–8.
Aiello LP, Sun W, Das A, et al. Intensive diabetes therapy and ocular surgery in type 1 diabetes. N Engl J Med. 2015;372:1722–33.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK prospective diabetes study (UKPDS) group. Lancet. 1998;352:837–53.
Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008;359:1565–76.
Chase HP, Jackson WE, Hoops SL, Cockerham RS, Archer PG, O'Brien D. Glucose control and the renal and retinal complications of insulin-dependent diabetes. JAMA. 1989;261:1155–60.
Blood glucose control and the evolution of diabetic retinopathy and albuminuria. A preliminary multicenter trial. N Engl J Med. 1984;311:365–72.
Krolewski AS, Canessa M, Warram JH, et al. Predisposition to hypertension and susceptibility to renal disease in insulin-dependent diabetes mellitus. N Engl J Med. 1988;318:140–5.
Chew EY, Klein ML, Ferris FL 3rd, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early treatment diabetic retinopathy study (ETDRS) report 22. Arch Ophthalmol. 1996;114:1079–84.
Chew EY, Klein ML, Murphy RP, Remaley NA, Ferris FL 3rd. Effects of aspirin on vitreous/preretinal hemorrhage in patients with diabetes mellitus. Early treatment diabetic retinopathy study report no. 20. Arch Ophthalmol. 1995;113:52–5.
Chew EY, Williams GA, Burton TC, Barton FB, Remaley NA, Ferris FL 3rd. Aspirin effects on the development of cataracts in patients with diabetes mellitus. Early treatment diabetic retinopathy study report 16. Arch Ophthalmol. 1992;110:339–42.
Aiello LP, Cahill MT, Wong JS. Systemic considerations in the management of diabetic retinopathy. Am J Ophthalmol. 2001;132:760–76.
Moloney JB, Drury MI. The effect of pregnancy on the natural course of diabetic retinopathy. Am J Ophthalmol. 1982;93:745–56.
Serup L. Influence of pregnancy on diabetic retinopathy. Acta Endocrinol Suppl (Copenh). 1986;277:122–4.
Phelps RL, Sakol P, Metzger BE, Jampol LM, Freinkel N. Changes in diabetic retinopathy during pregnancy. Correlations with regulation of hyperglycemia. Arch Ophthalmol. 1986;104:1806–10.
Wilkinson CP, Ferris FL 3rd, Klein RE, et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110:1677–82.
Browning DJ, Glassman AR, Aiello LP, et al. Optical coherence tomography measurements and analysis methods in optical coherence tomography studies of diabetic macular edema. Ophthalmology. 2008;115(1366–71):1371.e1.
Chalam KV, Bressler SB, Edwards AR, et al. Retinal thickness in people with diabetes and minimal or no diabetic retinopathy: Heidelberg Spectralis optical coherence tomography. Invest Ophthalmol Vis Sci. 2012;53:8154–61.
Bressler SB, Edwards AR, Andreoli CM, et al. Reproducibility of Optovue RTVue optical coherence tomography retinal thickness measurements and conversion to equivalent Zeiss stratus metrics in diabetic macular edema. Transl Vis Sci Technol. 2015;4:5.
Browning DJ, Glassman AR, Aiello LP, et al. Relationship between optical coherence tomography-measured central retinal thickness and visual acuity in diabetic macular edema. Ophthalmology. 2007;114:525–36.
Diabetic Retinopathy Study Research Group. Preliminary report on effects of photocoagulation therapy. Am J Ophthalmol. 1976;81:383–96.
Photocoagulation treatment of proliferative diabetic retinopathy: The second report of diabetic retinopathy study findings. Ophthalmology. 1978;85:82–106.
Four risk factors for severe visual loss in diabetic retinopathy. The third report from the diabetic retinopathy study. The diabetic retinopathy study research group. Arch Ophthalmol. 1979;97:654–5.
Photocoagulation treatment of proliferative diabetic retinopathy: relationship of adverse treatment effects to retinopathy severity. Diabetic retinopathy study report no. 5. Dev Ophthalmol 1981;2:248–261.
Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of diabetic retinopathy study (DRS) findings, DRS report number 8. The diabetic retinopathy study research group. Ophthalmology. 1981;88:583–600.
Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy. Invest Ophthalmol Vis Sci 1981;21:1–226.
Ederer F, Podgor MJ. Assessing possible late treatment effects in stopping a clinical trial early: a case study. Diabetic Retinopathy Study report No. 9. Control Clin Trials. 1984;5:373–81.
Rand LI, Prud'homme GJ, Ederer F, Canner PL. Factors influencing the development of visual loss in advanced diabetic retinopathy. Diabetic Retinopathy Study (DRS) Report No. 10. Invest Ophthalmol Vis Sci. 1985;26:983–91.
Ferris FL 3rd, Podgor MJ, Davis MD. Macular edema in diabetic retinopathy study patients. Diabetic retinopathy study report number 12. Ophthalmology. 1987;94:754–60.
Kaufman SC, Ferris FL 3rd, Swartz M. Intraocular pressure following panretinal photocoagulation for diabetic retinopathy. Diabetic retinopathy report no. 11. Arch Ophthalmol. 1987;105:807–9.
Kaufman SC, Ferris FL 3rd, Seigel DG, Davis MD, DeMets DL. Factors associated with visual outcome after photocoagulation for diabetic retinopathy. Diabetic retinopathy study report #13. Invest Ophthalmol Vis Sci. 1989;30:23–8.
Photocoagulation for diabetic macular edema. Early treatment diabetic retinopathy study report number 1. Early treatment diabetic retinopathy study research group. Arch Ophthalmol. 1985;103:1796–806.
Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early treatment diabetic retinopathy study report number 2. Early treatment diabetic retinopathy study research group. Ophthalmology. 1987;94:761–74.
Kinyoun J, Barton F, Fisher M, Hubbard L, Aiello L, Ferris F 3rd. Detection of diabetic macular edema. Ophthalmoscopy versus photography--Early Treatment Diabetic Retinopathy Study Report Number 5. The ETDRS Research Group. Ophthalmology. 1989;96:746–50; discussion 750-1
Prior MJ, Prout T, Miller D, Ewart R, Kumar D. C-peptide and the classification of diabetes mellitus patients in the early treatment diabetic retinopathy study. Report number 6. The ETDRS research group. Ann Epidemiol. 1993;3:9–17.
Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. The Early Treatment Diabetic Retinopathy Study Research Group. Int Ophthalmol Clin. 1987;27:254–64.
Case reports to accompany early treatment diabetic retinopathy study reports 3 and 4. The early treatment diabetic retinopathy study research group. Int Ophthalmol Clin. 1987;27:273–333.
Flynn HW Jr, Chew EY, Simons BD, Barton FB, Remaley NA, Ferris FL 3rd. Pars plana vitrectomy in the early treatment diabetic retinopathy study. ETDRS report number 17. The early treatment diabetic retinopathy study research group. Ophthalmology. 1992;99:1351–7.
Focal photocoagulation treatment of diabetic macular edema. Relationship of treatment effect to fluorescein angiographic and other retinal characteristics at baseline: ETDRS report no. 19. Early Treatment Diabetic Retinopathy Study Research Group. Arch Ophthalmol. 1995;113:1144–55.
Two-year course of visual acuity in severe proliferative diabetic retinopathy with conventional management. Diabetic retinopathy vitrectomy study (DRVS) report #1. Ophthalmology. 1985;92:492–502.
Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Two-year results of a randomized trial. Diabetic retinopathy vitrectomy study report 2. The diabetic retinopathy vitrectomy study research group. Arch Ophthalmol. 1985;103:1644–52.
Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision. Results of a randomized trial--Diabetic Retinopathy Vitrectomy Study Report 3. The Diabetic Retinopathy Vitrectomy Study Research Group. Ophthalmology. 1988;95:1307–20.
Early vitrectomy for severe proliferative diabetic retinopathy in eyes with useful vision. Clinical application of results of a randomized trial--Diabetic Retinopathy Vitrectomy Study Report 4. The Diabetic Retinopathy Vitrectomy Study Research Group. Ophthalmology. 1988;95:1321–34.
Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Four-year results of a randomized trial: diabetic retinopathy vitrectomy study report 5. Arch Ophthalmol. 1990;108:958–64.
UK Prospective Diabetes Study Group. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK prospective diabetes study group. BMJ. 1998;317:713–20.
Grading diabetic retinopathy from stereoscopic color fundus photographs--an extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology. 1991;98:786–806.
Fundus photographic risk factors for progression of diabetic retinopathy. ETDRS report number 12. Early treatment diabetic retinopathy study research group. Ophthalmology. 1991;98:823–33.
Classification of diabetic retinopathy from fluorescein angiograms. ETDRS report number 11. Early treatment diabetic retinopathy study research group. Ophthalmology. 1991;98:807–22.
Fluorescein angiographic risk factors for progression of diabetic retinopathy: ETDRS report number 13. Ophthalmology. 1991;98:834–40.
Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early treatment diabetic retinopathy study research group. Ophthalmology. 1991;98:766–85.
Effects of aspirin treatment on diabetic retinopathy. ETDRS report number 8. Early treatment diabetic retinopathy study research group. Ophthalmology. 1991;98:757–65.
Ferris F. Early photocoagulation in patients with either type I or type II diabetes. Trans Am Ophthalmol Soc. 1996;94:505–37.
Aiello LP, Wong JS. Role of vascular endothelial growth factor in diabetic vascular complications. Kidney Int Suppl. 2000;77:S113–9.
Avery RL. Regression of retinal and iris neovascularization after intravitreal bevacizumab (Avastin) treatment. Retina. 2006;26:352–4.
Adamis AP, Shima DT, Tolentino MJ, et al. Inhibition of vascular endothelial growth factor prevents retinal ischemia-associated iris neovascularization in a nonhuman primate. Arch Ophthalmol. 1996;114:66–71.
Brucker AJ, Qin H, Antoszyk AN, et al. Observational study of the development of diabetic macular edema following panretinal (scatter) photocoagulation given in 1 or 4 sittings. Arch Ophthalmol. 2009;127:132–40.
Gross JG, Glassman AR, Jampol LM, et al. Panretinal photocoagulation vs Intravitreous Ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314:2137–46.
Sivaprasad S, Prevost AT, Vasconcelos JC, et al. Clinical efficacy of intravitreal aflibercept versus panretinal photocoagulation for best corrected visual acuity in patients with proliferative diabetic retinopathy at 52 weeks (CLARITY): a multicentre, single-blinded, randomised, controlled, phase 2b, non-inferiority trial. Lancet. 2017;389:2193–203.
Gross JG, Glassman AR, Liu D, et al. Five-year outcomes of Panretinal photocoagulation vs Intravitreous Ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA Ophthalmol. 2018;136:1138–48.
Obeid A, Su D, Patel SN, et al. Outcomes of eyes lost to follow-up with proliferative diabetic retinopathy that received Panretinal photocoagulation versus intravitreal anti-vascular endothelial growth factor. Ophthalmology. 2019;126:407–13.
Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115:1447–9, 1449.e1–10.
Chew E, Strauber S, Beck R, et al. Randomized trial of peribulbar triamcinolone acetonide with and without focal photocoagulation for mild diabetic macular edema: a pilot study. Ophthalmology. 2007;114:1190–6.
Elman MJ, Aiello LP, Beck RW, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064–1077.e35.
Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2011;118:609–14.
Elman MJ, Ayala A, Bressler NM, et al. Intravitreal Ranibizumab for diabetic macular edema with prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology. 2015;122:375–81.
Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372:1193–203.
Jampol LM, Glassman AR, Bressler NM, Wells JA, Ayala AR. Anti-vascular endothelial growth factor comparative effectiveness trial for diabetic macular edema: additional efficacy post hoc analyses of a randomized clinical trial. JAMA Ophthalmol. 2016;134
Baker CW, Glassman AR, Beaulieu WT, et al. Effect of initial management with Aflibercept vs laser photocoagulation vs. observation on vision loss among patients with diabetic macular edema involving the Center of the Macula and Good Visual Acuity: a randomized clinical trial. JAMA. 2019;321:1880–94.
Antoszyk AN, Glassman AR, Beaulieu WT, et al. Effect of Intravitreous Aflibercept vs vitrectomy with Panretinal photocoagulation on visual acuity in patients with vitreous hemorrhage from proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2020;324:2383–95.
Keech A, Simes RJ, Barter P, et al. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes mellitus (the FIELD study): randomised controlled trial. Lancet. 2005;366:1849–61.
Keech AC, Mitchell P, Summanen PA, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370:1687–97.
Chew EY, Ambrosius WT, Davis MD, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010;363:233–44.
Gao BB, Clermont A, Rook S, et al. Extracellular carbonic anhydrase mediates hemorrhagic retinal and cerebral vascular permeability through prekallikrein activation. Nat Med. 2007;13:181–8.
Clermont A, Murugesan N, Zhou Q, et al. Plasma Kallikrein mediates vascular endothelial growth factor-induced retinal dysfunction and thickening. Invest Ophthalmol Vis Sci. 2016;57:2390–9.
KalVista pharmaceuticals reports phase 2 clinical trial results in patients with diabetic macular edema. business wire. This is a press release: https://www.businesswire.com/news/home/20191209005372/en/KalVista-Pharmaceuticals-Reports-Phase-2-Clinical-Trial-Results-in-Patients-with-Diabetic-Macular-Edema
Ohashi H, Takagi H, Koyama S, et al. Alterations in expression of angiopoietins and the Tie-2 receptor in the retina of streptozotocin induced diabetic rats. Mol Vis. 2004;10:608–17.
Oh H, Takagi H, Suzuma K, Otani A, Matsumura M, Honda Y. Hypoxia and vascular endothelial growth factor selectively up-regulate angiopoietin-2 in bovine microvascular endothelial cells. J Biol Chem. 1999;274:15732–9.
Peters S, Cree IA, Alexander R, et al. Angiopoietin modulation of vascular endothelial growth factor: effects on retinal endothelial cell permeability. Cytokine. 2007;40:144–50.
Menden H, Welak S, Cossette S, Ramchandran R, Sampath V. Lipopolysaccharide (LPS)-mediated angiopoietin-2-dependent autocrine angiogenesis is regulated by NADPH oxidase 2 (Nox2) in human pulmonary microvascular endothelial cells. J Biol Chem. 2015;290:5449–61.
Ziegler T, Horstkotte J, Schwab C, et al. Angiopoietin 2 mediates microvascular and hemodynamic alterations in sepsis. J Clin Invest. 2013;123:3436–45.
Sahni J, Patel SS, Dugel PU, et al. Simultaneous inhibition of Angiopoietin-2 and vascular endothelial growth factor-a with Faricimab in diabetic macular edema: BOULEVARD phase 2 randomized trial. Ophthalmology. 2019;126:1155–70.
https://www.roche.com/media/releases/med-cor-2020-12-21.htm.
Tang J, Du Y, Lee CA, Talahalli R, Eells JT, Kern TS. Low-intensity far-red light inhibits early lesions that contribute to diabetic retinopathy: in vivo and in vitro. Invest Ophthalmol Vis Sci. 2013;54:3681–90.
Saliba A, Du Y, Liu H, et al. Photobiomodulation mitigates diabetes-induced retinopathy by direct and indirect mechanisms: evidence from intervention Studies in pigmented mice. PLoS One. 2015;10:e0139003.
Cheng Y, Du Y, Liu H, Tang J, Veenstra A, Kern TS. Photobiomodulation inhibits long-term structural and functional lesions of diabetic retinopathy. Diabetes. 2018;67:291–8.
Tang J, Herda AA, Kern TS. Photobiomodulation in the treatment of patients with non-center-involving diabetic macular oedema. Br J Ophthalmol. 2014;98:1013–5.
Eells JT, Gopalakrishnan S, Connor TB, et al. 670 nm Photobiomodulation as a therapy for diabetic macular edema: a pilot study. Invest Ophthalmol Vis Sci. 2017;58:932.
Fong DS, Aiello L, Gardner TW, et al. Retinopathy in diabetes. Diabetes care. 2004;27:s84–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ashraf, M., Sun, J.K., Silva, P.S., Cavallerano, J., Aiello, L.P. (2023). Diabetic Retinopathy. In: Johnstone, M., Veves, A. (eds) Diabetes and Cardiovascular Disease. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-031-13177-6_15
Download citation
DOI: https://doi.org/10.1007/978-3-031-13177-6_15
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-031-13176-9
Online ISBN: 978-3-031-13177-6
eBook Packages: MedicineMedicine (R0)