Abstract
Social circumstances, behavioral patterns, environmental exposures, and genetic predispositions generate significant impacts on health. The substantive nature of these impacts is garnering increasing attention from health policy analysts, health insurance plan administrators, Medicare and Medicaid program administrators, and clinicians. This chapter focuses on the two factors that are particularly relevant for psychologists working in integrated care: social circumstances and behavioral patterns. The social circumstances evaluated are related to socioeconomic status, such as housing quality, food security, education, and income. These factors influence health at various stages in the life cycle (adulthood, childhood, infancy) via indirect mechanisms. The behavioral patterns investigated in this chapter include obtaining vaccinations, utilizing contraceptives, practicing good nutrition, and avoiding smoking and heavy drinking. Social circumstances interact with behavioral patterns to influence health. For example, we find that education affects cognitive ability and health behaviors. This has a consequential effect on overall health. Healthcare providers are faced with these consequences in delivering care to patients of various socioeconomic backgrounds. We provide solutions involving integrated care settings to mitigate the impacts of social circumstances and behavioral patterns on health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Healthcare
- Health
- Social determinants of health
- Healthcare policy
- Healthcare providers
- Healthcare administrators
- Integrated care
1 Introduction
Social circumstances, behavioral patterns, environmental exposures, and genetic predispositions generate significant impacts on health. The substantive nature of these impacts is garnering increasing attention from health policy analysts, health insurance plan administrators, Medicare and Medicaid program administrators, and clinicians. This chapter focuses on the two factors that are particularly relevant for psychologists working in integrated care: social circumstances and behavioral patterns. Statistical analyses indicate that these two factors account for at least half of all preventable deaths (McGinnis et al., 2002). We provide an overview of statistical work indicating both causal and associative relationshipsFootnote 1 of these factors on health, and we discuss implications for clinicians.
While healthcare is an important tool for strengthening health and preventing adverse health outcomes, other factors may generate larger impacts on health. McGinnis et al. (2002) concluded that gaps in healthcare account for only 10–15% of preventable deaths, while social circumstances and behavioral patterns account for more than half of all preventable deaths (McGinnis et al., 2002). Advances in pharmaceutical and surgical treatments for cardiac diseases, cancers, and conditions responsible for infant mortality have generated improved outcomes for patients; however, social circumstances and behavioral patterns continue to affect health in significant ways.
Social circumstances and behavioral patterns can also have significant implications for healthcare providers. Medical professionals are held accountable for health outcomes, yet these factors exert larger influences on health than medical care. Providers working under value-based payment (VBP) models face incentives to generate good health outcomes. While clinicians face incentives to develop strategies to mitigate these impacts, they cite numerous barriers that hinder these efforts, including lack of control over relevant decisions and processes in healthcare organizations and in social service agencies (Winfield et al., 2018). Finally, the complexity of the web of factors affecting health makes it difficult to identify and implement effective programs.
Several terms are used to describe the set of factors encompassing social circumstances and behavioral patterns, including “social determinants of health” and “health-related social needs.” In this chapter we focus on four components of these constructs: income, education, housing security, and food security.
This chapter has four sections. The section following this introduction summarizes evidence describing the relationship between social circumstances, behavioral patterns, and health. We discuss this relationship that occurs at three stages in the life cycle: adulthood, childhood, and infancy. The third section of the chapter explores intervention strategies and discusses strategic issues facing clinicians as they work to mitigate the health impacts of social circumstances and behavioral patterns.
2 Factors That Affect Health
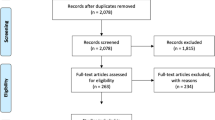
This section summarizes the results of statistical analyses designed to yield evidence about impacts of social circumstances and behavioral patterns on health. We focus on studies that examine relationships between social circumstances and health or between behavioral patterns and health. The body of evidence is substantial. Many studies document associations between social circumstances, behavioral patterns, and health, while others used experimental design strategies to generate evidence of causal links between social circumstances, behavioral patterns, and health.
Evidence indicates intergenerational relationships of income, education, and health. Adult health is affected by the adult’s own social circumstances and behavioral patterns and by her health as an infant and then as a child. When this adult becomes a parent, her health behaviors and social circumstances can affect the health of her children – who will be part of the next generation of adults. The relationship between social circumstances and health may also reflect two-way causality between income and health: income can affect one’s health, and one’s health can affect income if poor health limits one’s work hours.
Because studies typically focus on impacts that occur at a specific life stage, this section includes three subsections that summarize evidence about impacts on adults, children, and infants. We include overviews of studies that address four components of the social circumstances construct: housing security, food security, education, and income. We also include overviews of studies that address socioeconomic components of health behavior patterns. There are strong interactions between social circumstances and behavioral patterns. For example, education is typically categorized as a social circumstance. However, it is associated with behavioral patterns. Similarly, income is associated with the availability of safe outdoor recreation spaces, which could be a factor shaping propensity to exercise.
2.1 Health as an Adult
Adult health can be affected by the individual’s health as an infant and child and by the adult’s social circumstances and behavioral patterns. This subsection begins by summarizing evidence about the impacts of adult social circumstances and behavioral patterns on health.
Social circumstances and health behaviors are intertwined. Exercise can reduce the effect of age-related losses in muscle mass and strength (Distefano & Goodpaster, 2018). However, access to exercise resources such as equipment and safe outdoor spaces can be a product of socioeconomic factors. High-quality diets that entail good nutrition are associated with better physical functioning in older ages (Artaud et al., 2017; Hagan et al., 2016; Robinson, 2018). However, good nutrition requires convenient and affordable access to nutritious food and basic knowledge of nutrition and cooking strategies.
In this subsection, we examine the impacts of social circumstances on adult health. The first subsection reviews evidence on the impacts of housing security and housing quality on health outcomes. The second focuses on the associations of food insecurity with health concerns and higher medical expenditures. The third section reports evidence on the impact of education on health behaviors, cognitive ability, and the management of chronic illnesses. The last section explores impacts of income on health, through pathways shaped by access to transportation, ability to fund copayments, financial access to good nutrition, and financial access to long-term services and supports (LTSS).
2.1.1 Housing Security and Quality
Housing security and housing quality affect health. Homelessness is associated with infectious diseases, mental illness, mortality, a higher need for medical services, and longer hospital stays (McCormick & White, 2016; Morrison, 2009; Williams & Bryant, 2018). Low-quality housing is linked to poor health and higher mortality rates. This section will explore associations between housing and health.
The incidence of tuberculosis, hepatitis C virus (HCV), and human immunodeficiency virus (HIV) is higher among homeless individuals than among those with secure housing. In population-dense homeless groups, such as those living in downtown Los Angeles, 26.7% of sampled adults tested positive for HCV, and almost half of them were unaware of the infection (Beijer et al., 2012; Gelberg et al., 2012).
In addition to infectious diseases, homeless groups also suffer from mental illnesses. About 26% of all sheltered persons who are homeless have a severe mental illness, and almost 35% of all sheltered, homeless adults have a chronic substance abuse issue (Substance Abuse and Mental Health Services Administration, 2011).
The high prevalence of disease and mental illness contributes to the high mortality rates for homeless individuals. Homelessness carries an all-cause mortality hazard ratio of 1.6 compared to non-homeless cohorts, after controlling for age, sex, prior hospital admissions, and contributing socioeconomic conditions. Hospital admissions for drug-related causes raise the hazard ratio of death by 3.9 for the general population, but for homeless individuals, this statistic is 7.2 (Morrison, 2009).
Homeless individuals require more medical services. This can be a costly burden. Housing insecurity is associated with longer hospital stays, more emergency department visits, and higher in-hospital mortality rates (Hunter et al., 2017; McCormick & White, 2016). Homeless individuals who did not achieve residential stability, had higher rates of unmet physical care needs compared to those who did not achieve residential stability (Jaworsky et al., 2016). Individuals with insecure housing also report delaying physician visits due to financial issues (Stahre et al., 2015). These patterns are also observed among veterans (Kushel et al., 2002). Veterans in the United States without a home are four times more likely to visit the emergency room within 1 year than non-homeless veterans (Tsai et al., 2013).
There are federal resources available to secure housing for homeless veterans. The Veterans Affairs (VA) implements evidence-based programs such as the Housing and Urban Development-Veterans Affairs Supportive Housing vouchers (HUD-VASH). The HUD-VASH program utilizes the “housing first” model in which veterans are given a housing choice voucher. The individual is then paired with a VA case manager and supportive services to assist in sustaining the housing agreement and recovering from physical or mental health problems. Another program similar to this is the Grant and Per Diem (GPD) Program which are VA grants awarded to community-based agencies to create transitional housing programs (National Conference of State Legislatures, 2020).
Homeless patients also have more lengthy and more frequent hospital stays and higher in-hospital mortality rates. The average length of stay per hospital admission is longer for individuals with no fixed abode compared to those with stable housing, even after controlling for the severity of diagnosis (McCormick & White, 2016). The overall in-hospital mortality rate for homeless groups is 10% higher compared to those with housing. This higher mortality rate is mostly due to more severe diagnoses for homeless individuals.
While attention tends to focus on the housed vs. homeless dichotomy, it is also useful to consider housing as a continuous variable. Inadequate housing is associated with chronic illness, higher mortality rates, and infectious diseases (Butler et al., 2017; Desmond & Bell, 2015; Hood, 2005; Johnson, 2012; Martinez et al., 2018). Neighborhood plumbing and insulation problems are each associated with a 3.9 point lower index of General Health Status (Johnson, 2012). (See Box 4.1 for a definition of General Health Status.)
Box 4.1:Definition: General Health Status
General Health Status (GHS) is based on one question asked of household heads: “Would you say your health in general is excellent, very good, good, fair, or poor?” This question was asked at each wave of data collection between 1984 and 2005. It is highly predictive of morbidity measured in clinical surveys. A decrease in the GHS Index signifies a decrease in overall health. For more information, see Johnson, (2012).
Areas with a higher prevalence of poor housing conditions also have higher mortality rates. Rural low-income populations are susceptible to poor living conditions. Poor housing conditions are a health concern because they are associated with asthma, lead poisoning, heart disease, and developmental delays. From 2005 to 2009, rural households had a 13% higher mortality rate compared to that of metropolitan households (Martinez et al., 2018).
2.1.2 Food Security
Food insecurity is a barrier to attaining optimum physical health. This concern is most prevalent among low-income households. This subsection will explore how food insecurity is associated with health concerns and higher healthcare expenditures.
Individuals facing food insecurity have higher rates of chronic disease, disability, and health concerns. In 2019, 10.5% of US households faced food insecurity (Coleman-Jensen et al., 2020). Food-insecure households include those facing low and very low food security (see Box 4.2 for a definition of food insecurity). These households have higher rates of illnesses such as hypertension, coronary heart disease, asthma, diabetes, and other illnesses. Adults in households reporting very low food security are 15.3% more likely to have a chronic illness compared to adults reporting very high food security (Gregory & Coleman-Jensen, 2017).
Box 4.2:Definition: Food Insecurity
Households are defined to have food insecurity if they have difficulty providing food for themselves at some time during the year due to a lack of resources (Coleman-Jensen et al., 2014). Households facing low food security report reduced quality, variety, or desirability of diet. There is little to no indication of reduced food intake. Households facing very low food security report multiple indications of disrupted eating patterns and reduced food intake (Coleman-Jensen et al., 2021).
Food-insecure households incur higher healthcare expenditures (by $1863 per year) than households with food security. The extra spending stems from more ED visits, longer and more frequent hospital stays, and higher expenditures for prescriptions among food-insecure individuals than among food-secure households. This association is robust after controlling for potential confounders like age, race, education, income, and health insurance (Berkowitz et al., 2017; Nord, 2008). Food-insecure individuals are 1.47 times more likely to visit an ED than food-secure individuals (Berkowitz et al., 2017). The greatest divide was found among those enrolled in public health insurance. Among Medicare and Medicaid enrollees, food-insecure individuals are likely to have more emergency visits and hospital stays than food-secure enrollees.
2.1.3 Education
Education affects health through several pathways. It influences health behaviors, alters cognitive ability, and improves the health management of chronic illness. One additional year of schooling reduces rates of self-reported poor health by 4–6.4% points for women and 4.5–5.4% points for men (Brunello et al., 2016).
More years of schooling are linked to healthier lifestyles. Health behaviors encompass obtaining vaccinations, utilizing contraceptives, practicing good nutrition, and avoiding smoking and heavy drinking. Educated populations are associated with higher vaccination rates and contraceptive use (Brunello et al., 2016; Cutler & Lleras-Muney, 2010; Nagata et al., 2013; Rosenzweig & Schultz, 1989). This could be due to the fact that groups with more schooling also have better access to preventive healthcare. This positive association with education also occurs in couples with regard to contraceptive use. Couples with more schooling are more likely to know how to use various forms of contraception compared to couples with less education (Rosenzweig & Schultz, 1989). Cohorts with more years of schooling are less likely to smoke, practice heavy drinking, or be obese (Cutler & Lleras-Muney, 2010). An estimated 50% of all deaths in the United States are attributable to behaviors like smoking, exercise, diet, and heavy drinking (Mokdad et al., 2005). These behaviors are affected by numerous factors including individual choices and behavior patterns (Centers for Disease Control and Prevention [CDC], 1999; McGinnis & Foege, 1999). These behaviors also affect health. Diet choices, for example, are associated with coronary heart disease, stroke, diabetes, and various cancers (Walker & Walker, 1989). Similarly, a lack of exercise is associated with an increased risk for heart disease, dementia, osteoporosis, and diabetes (Manley, 1996). Smoking, another modifiable behavior, also contributes to a large portion of preventable premature deaths.
Another mechanism by which education influences health is that it alters cognitive ability (Cutler & Lleras-Muney, 2010). For example, educated individuals are more likely to implement medical recommendations for managing diabetes and the human immunodeficiency virus (HIV) (Goldman & Smith, 2002).
Educational attainment improves the management of chronic illnesses. There is a positive relationship between years of schooling and quality of at-home management of chronic conditions. Educated individuals are more likely to be aware of a diabetic condition, monitor key health metrics related to diabetes, and adhere to clinician guidelines (Goldman & Smith, 2002; Smith, 2007). In a sample of adult men with diabetes, 38% of those with a high school diploma were unaware of their diabetic condition compared to only 21% of those with more than a high school diploma (Smith, 2007). This study defined diabetes as having an HbA1c value of 6.5% or greater (see Box 4.3 for more detail). Self-management activities follow a similar gradient. More schooling is associated with higher rates of monitoring blood glucose levels and exercise and lower rates of missed insulin injections and smoking (Smith, 2007).
Box 4.3:Definition of Diabetes Used in Smith, 2007
The lab exam for diabetes in this study measures the glycosylated hemoglobin A1c (HbA1c) test. This is a measure of the percent of hemoglobin molecules bound to glucose. HbA1c is highly correlated with fasting plasma glucose levels. Smith (2007) uses the standard convention of values greater than or equal to 6.5% to indicate clinical diabetes for the purpose of this study. The results of the study are not sensitive to the specific threshold chosen.
2.1.4 Income
An individual’s income can affect health through several pathways including access to reliable transportation, ability to fund copayments, financial access to nutritious foods, and financial access to long-term services and supports (LTSS).
Unreliable transportation weakens a patient’s ability to show up for appointments and implement clinician instructions and advice (Baren et al., 2001; Heiman & Artiga, 2015; Syed et al., 2013; Virapongse & Misky, 2018). In a study of 189 Hispanic and Latino women who were recommended to receive a follow-up mammogram, over a third did not pursue follow-up care within 3 months of the recommended time frame (Parra, 2016). Breast cancer is the leading cause of cancer mortality among Hispanic and Latino women (American Cancer Society, 2018). Unreliable transportation was frequently cited as an inhibiting factor for women who were dependent on public transportation. This issue can be important for low-income, uninsured, or underinsured women. Low-income individuals are far more likely to utilize “active transportation” such as biking, walking, or public transportation, which can pose a barrier to attendance at scheduled medical appointments (McKenzie, 2014). Transportation vouchers are successful in reducing readmissions when included in hospital discharge programs (Coleman et al., 2006). Fewer providers located near a patient result in longer travel distances and consequently higher transportation costs. This is linked to significantly fewer visits (Sloan et al., 2004).
Copayments and the cost of medications can also deter proper medical follow-up. Men facing copayments over $10 or with deductibles over $250 are significantly less likely to receive a prostate cancer screening compared to men facing lower copayments (Liang et al., 2004). The cost of medication is commonly cited as a factor affecting care transitions after a hospital visit (Virapongse & Misky, 2018).
Financial access to long-term services and supports (LTSS) can be an impediment to good health for patients struggling with activities of daily living. LTSS caregivers assist with medication management, prescription adherence, and care management. They can also help monitor vital health metrics and support care logistics for older adults (Fineberg, 2008; Gitlin & Wolff, 2011; Williams et al., 2012; Wolff et al., 2016). LTSS services can be provided in an institutional or residential facility, such as a skilled nursing facility or assisted living facility, or in the home. Caregivers are essential for older adults with chronic illnesses that require self-management, such as diabetes or coronary heart disease. A lack of LTSS can pose a barrier to implementing healthcare recommendations, with adverse health consequences for the patient.
2.2 Childhood Health
The income and food security of a child’s household can affect that child’s health. This subsection will report evidence of associations of income and food security with childhood health.
Childhood health is an important factor in contributing to long-term health status in adulthood. Case et al. (2005) found that children who report poor health have significantly lower educational status, lower health status, and lower income in adulthood, even after controlling for parental income and education. Chronic conditions developed before age 7 that persist to age 16 have a significant association with health status at age 42 (Case et al., 2005). A child’s height at age 16 is significantly associated with better health at ages 23, 33, and 42. However, a child’s height is also correlated with her father’s education and income.
Childhood health is influenced by numerous factors, including family income and food security. The following sections will discuss evidence of the impacts of these two factors on childhood health.
2.2.1 Family Income
Children from low-income households report poorer health than those in high-income households (Curtis et al., 2001). For families in the $15,000–50,000 income bracket, a $10,000 increase in annual income is associated with a 0.53% point increase in the average General Health Status of the children living in these families (Johnson & Schoeni, 2011). Doubling family income generates a four percentage point increase in the probability that a young child (ages 0–3) will have excellent or very good health (Case et al., 2002). The strength of this effect increases as the child ages: doubling family income generates a 6.4 percentage point increase in the probability that a teenager (ages 13–15) will have excellent or very good health (Currie & Stabile, 2003). One possible explanation for this result stems from the higher incidence of health shocks among children living in low-income versus higher-income families (Currie, 2009). For example, only 11% of high-income children (ages 0–3) have chronic conditions (asthma and mental health problems) compared to 23% of low-income children (Currie et al., 2007). Children from low-income households also have a higher probability of being limited by these chronic conditions during adolescence compared to others with the same chronic conditions from high-income households (Currie, 2009). One of the reasons for this is that children living in low-income families are less likely to efficiently manage their asthma than children living in high-income families, resulting in consequences lasting through their teenage years (Currie, 2009). These longer-term consequences affect the subsequent health of that individual when he becomes an adult.
2.2.2 Food Security
Household food security is associated with childhood health. Adolescents raised in food-unstable households have lower health status and higher rates of chronic illness. Children from food-insecure homes are twice as likely to report being in fair or poor health and 1.4 times more likely to have asthma compared to children raised in food-secure homes (Gundersen & Ziliak, 2015). Compared to children in food-secure homes, children enduring food insecurity are more likely to have anemia (Eicher-Miller et al., 2009; Skalicky et al., 2006). They also more likely to have depression or anxiety between the ages of 4 and 8 years old (Melchior et al., 2012). Food insecurity in childhood is also associated with a higher risk of hospitalization over the course of the child’s lifetime (Cook et al., 2006). Hunger experienced in childhood is also a strong predictor of depression, anxiety, and suicide ideation in later teenage and early adult years (McIntyre et al., 2013; Melchior et al., 2012).
2.3 Health at Birth
A child can be affected by his or her preceding health status at birth. Infant health has implications for health conditions later in adolescence and even adulthood. The following sections will discuss evidence documenting relationships between family income, mother’s education, and infant health.
Many studies demonstrate that health at birth has long-term implications for health in adulthood. For example, low birthweight is associated with developing coronary heart disease and hypertension as an adult, and it is also associated with insulin resistance syndrome in adulthood (Barker et al., 1989, 1993; Law & Shiell, 1996).
The following sections will discuss two factors that influence infant health: family income and mother’s education.
2.3.1 Family Income
Infants born into higher-income families have more favorable birth outcomes (Conley & Bennett, 2000; Currie & Lin, 2007). Data from 1985 British birth records indicate a higher prevalence of low birthweight infants whose fathers were in low-prestige occupations compared to those of high-prestige occupations (6.4% vs. 5%) (Currie & Hyson, 1999). California birth records from the 1970s found the same association when comparing birth outcomes in high-income and low-income zip codes (6% vs. 7%) (Currie, 2009). Even in countries with universal health insurance (Canada and the United Kingdom), the income gap in childhood health is present.
2.3.2 Mother’s Education
The mother’s education can influence the health of her infants by influencing her health behaviors. Maternal education is associated with lower smoking rates and higher rates of prenatal care utilization (Currie & Moretti, 2003). These health behaviors affect gestational age and the infant’s birthweight (Evans & Ringel, 1999). College-educated mothers have lower rates of smoking and higher rates of participating in prenatal care compared to mothers with less than a high school diploma (Currie & Moretti, 2003). This pattern was identified during the expansion of colleges in the United States in the early 1940s that provided educational opportunities for women. From the sample of college-educated mothers, only 2% smoked during pregnancy compared to 34% from the sample of mothers with less than a high school education. Even after the 1964 Surgeon General’s Report on Smoking and Health established that smoking is detrimental to the mother’s health while pregnant, there was an educational divide in the reaction to this new information. The smoking habits of educated pregnant women immediately dropped following the report compared to those of less educated pregnant women (Aizer & Stroud, 2010). Smoking during pregnancy is concerning because it increases the risk that an infant will have a low birthweight by a factor of two. Infant birthweight and gestational age increase with higher rates of college attendance among women. An extra year of college education reduces the likelihood of the mother having a low birthweight child by 20% and a preterm birth by 15% (Currie & Moretti, 2003). Maternal education is a key indicator of infant health because of its effects on health behaviors. An excise tax on cigarettes can increase average birthweight. A one-cent increase in the state tax rate of cigarettes leads to an increase in average birthweight by 0.21 g (Evans & Ringel, 1999).
2.3.3 Maternal Health During Pregnancy
Statistical evidence indicating impacts of parental health, income, and behavioral patterns on infant health is important because it clarifies pathways by which parental health and income can be transmitted to the next generation via two pathways: gestational health and the health behaviors of parents.
Gestational health can influence the development of the embryo in utero. Exposure to adverse health events in utero can indirectly affect the weight and overall health of the infant (Roseboom et al., 2000). The embryo relies on a stream of oxygen and nutrients. Anything that tampers with this mechanism (e.g., smoking while pregnant or poor nutrition) can have a significant effect on the infant’s health. Amsterdam records show that infants exposed to the Dutch famine while in utero from 1944 to 1945 exhibited lower glucose tolerance as adults and higher rates of coronary heart disease (Ravelli et al., 1998; Roseboom et al., 2000). The risk of lower respiratory illness before the age of 2 is greatest among children whose parents had childhood lower respiratory illness and smoked (Mann et al., 1992). Smoking while pregnant poses a moderate risk factor for preterm delivery and is a major risk factor for intrauterine growth retardation (Case & Paxson, 2002).
3 Initiatives to Mitigate the Impacts of Social Circumstances and Behavioral Patterns
Social circumstances and individual behaviors can generate adverse impacts on individual health, and these factors can weaken the impacts of clinician efforts to strengthen individual health (McGinnis et al., 2002). Healthcare organizations have two strategic options to mitigate the adverse impacts of inadequate education, insecure food and housing, and unhealthy behaviors: (i) healthcare organizations can assume primary responsibility for implementing programs within healthcare settings to offset potential adverse impacts of these factors on patient health outcomes, or (ii) these organizations can play a supporting role by strengthening coordination between healthcare entities and social service agencies and between healthcare organizations and education agencies and by advocating for increased funding to support the work of these entities. This section of the chapter describes three types of efforts currently undertaken by healthcare organizations and agencies, and it poses strategic questions raised by these efforts. Clinicians can enrich the analysis and discussion of these questions by engaging with health policy analysts and health policy makers.
3.1 Initiatives in Health Services
Some healthcare organizations are offering programs designed to offset potential adverse health impacts of low education and insecure food and housing and to help individuals adopt more healthy behavior patterns. This subsection discusses three examples of programs aiming to achieve these goals: pharmacist-led interventions, hospital discharge coordination programs, and integrated care.
First, pharmacist-led interventions provide individualized care such as medication management, programs to resolve drug therapy issues, and patient education. These programs were implemented following passage of the Affordable Care Act of 2010, which led to expansions in pharmacist scope of practice in some states (Smock, 2013; Wachino, 2017). Targeted education, pharmacotherapeutic monitoring, and health screenings led by pharmacists have been shown to cut medical costs while improving health. These programs generated an increase in medication costs that were offset by reductions in medical costs from reduced hospitalization and emergency department (ED) visits (Wang et al., 2016). Medication adherence programs successfully helped patients adhere to recommended medication regimes (Smith, 2009); achieve reductions in average lipid levels, HbA1c values, and systolic blood pressure readings (Cranor et al., 2003); prevent diabetes-related cerebrovascular or cardiovascular events (Wang et al., 2016); and reduce the number of days absent from work (Cranor et al., 2003; Fera et al., 2009). Evidence also indicates that the strategy used to provide pharmacist counseling may be important: one study concluded that counseling provided in retail settings is more effective than counseling provided during telephone calls (Brennan et al., 2012).
Second, healthcare organizations are developing and implementing comprehensive hospital discharge programs (also known as transitional care interventions) to improve health outcomes. These programs may include monitoring patient status following hospital discharge, or they may utilize nurse advocates who arrange follow-up patient appointments, confirm medication reconciliation, and conduct patient education. These strategies can effectively reduce hospitalization following the initial hospital discharge (Jack, 2009).
Some programs focus on specific populations, such as high-risk patients, elderly patients, or adults with chronic homelessness. Transitional care interventions focused on high-risk patients have reported reductions in readmissions, hospital days, and medical costs. A 2008 North Carolina transitional care program for Medicaid recipients with chronic conditions was successful in reducing readmissions with care that involved comprehensive medication management, face-to-face medication education, and outpatient follow-up (Jackson et al., 2013).
For elderly patients with chronic conditions, comprehensive discharge programs demonstrate a reduction in short-term readmission rates, medical expenditures, and number of rehospitalizations (Naylor et al., 1999).
Chronically homeless adults also benefit from transitional care including transition coaches and emphasizing patient-centered communication (Buchanan et al., 2006). Programs that provide housing and case management are linked to reduced inpatient hospitalizations and ED visits for these populations (Sadowski et al., 2009).
Third, integrated care can be a cost-effective strategy for improving quality of care. Compared with patients who received care in traditional settings, integrated care patients enjoyed better adherence to treatment recommendations and fewer symptoms. Insurers benefited from lower total medical care expenditures, and clinicians reported increased satisfaction (Blount, 2003; Katon, 1995; Lenz et al., 2018).
Integrated care programs can deliver medical and behavioral care via coordinated, co-located, or integrated strategies (Blount, 2003; Coleman et al., 1979; Cummings et al., 2009). All methods require communication between primary and behavioral healthcare providers. Coordination requires significant time and effort from both medical and behavioral health providers. Nonetheless, the Hawaii Project I, led by Nicholas A. Cummings and Herbert Dorken implemented widespread coordinated care for Hawaii Medicaid beneficiaries in the 1980s (Cummings, 1990). The program improved patient adherence to recommended medical regimens and prompted significant patient lifestyle changes.
In the co-located model, behavioral and primary care providers are physically located in the same suite of offices to facilitate collaboration. The first widespread HMO implementation of this strategy demonstrated a rich exchange of information between providers. Patients were more likely to keep their behavioral health appointments if they were introduced to the behavioral health provider during the primary care visit (Blount, 2003). Co-located settings can also mitigate barriers of access to care for patients who lack reliable transportation to visit providers. Primary care providers in co-located settings reported feeling more comfortable to ask about psychosocial issues knowing that they could readily refer the patient to an expert (Blount, 2003).
The integrated care model offers an additional advantage: the patient receives a unified treatment plan that includes both behavioral and medical elements. This integration can be useful for patients with both chronic illness and depression (Blount, 2003).
Implementation of these programs highlights the importance of determining whether each program is cost-effective in each specific setting. Useful programs that are not cost-effective use organization resources that could have been deployed to fund alternate programs. This situation requires careful analyses to assess whether each program generates sufficient benefits to justify allocating resources away from other programs. The question of whether a program is cost-effective in a specific setting requires site-specific analysis. Program costs and benefits can vary across settings due to differences in the characteristics of patient populations, differences in professional compensation and facility costs, and differences in the local availability of complementary or substitute resources and programs.
In addition to these efforts, some states are exploring strategies to incentivize nonprofit hospitals to design and implement “community benefit” programs that address key health equity issues (NASHP, 2021). Federal Internal Revenue Service regulations mandate that these hospitals must engage in community benefit activities as a prerequisite for maintaining tax-exempt status. Some states are considering strategies to require hospitals to focus these activities on social determinants of health and to audit the impacts of these activities on health and health disparities.
3.2 Initiatives to Address Gaps in Education, Food Security, and Housing Security
Instead of focusing on implementing programs to offset the health effects of income, healthcare organizations could focus on addressing gaps in education, food security, and housing security directly. Healthcare organizations could consider two strategies for undertaking this work: (i) provide food and housing to high-risk individuals or (ii) partner with community organizations that focus on education, food security, and housing security. Some healthcare organizations are implementing the first strategy. For example, some managed care companies provide housing for individuals with chronic conditions who also experience chronic homelessness. Some nonprofit hospitals invest in affordable housing to meet federal requirements, stating that tax-exempt hospitals must generate community benefits (Tanumihardjo et al., 2021). These programs typically target individuals with high healthcare expenditures and frequent visits to hospital emergency departments. While these programs can demonstrate good results, the magnitudes of these programs tend to be small relative to the magnitude of the population of homeless individuals.
In contrast, the federal Department of Housing and Urban Development provides subsidized housing on a larger scale. Even this is not sufficient: only 25% of individuals eligible for this assistance actually receive it due to funding limitations (Katch & Bailey, 2020). Nonetheless, some Medicaid programs partner with state housing authorities to develop systems for housing individuals with complex health conditions or individuals who need help with activities of daily living.
This raises the question: How should healthcare organizations direct their efforts and resources? Should they continue to develop targeted small-scale programs or should they invest resources to build partnerships with social service and education agencies and advocate for increased funding for these agencies?
Healthcare organizations considering these options will note that the strategy of providing housing for limited numbers of individuals faces several challenges. First, Medicaid programs cannot reimburse organizations for providing housing due to constraints imposed by federal law. Second, adult membership in a specific health plan, or a Medicaid managed care plan, can be short term if the adult gains or loses Medicaid eligibility or if the adult chooses a new health plan at the end of a plan year. It is not clear how housing provided by a healthcare organization would be affected by changes in health plan coverage. Finally, healthcare organizations may not have experience and expertise in managing housing programs (Katch & Bailey, 2020).
Preschool programs for disadvantaged children illustrate two additional dilemmas facing healthcare providers. Programs such as the Perry Preschool and Head Start yield positive effects on adult outcomes (Deming, 2009; Heckman et al., 2010). For example, evaluation of the Perry Preschool Program indicates that participants enjoyed higher education and earnings and increased participation in healthy behaviors at age 40 compared to children who were not enrolled in the program (Heckman et al., 2010). Despite the positive impact on adult health, however, these programs are not likely to be cost-effective for healthcare organizations due to the long lag between the educational investment and the subsequent improvement in adult health. In addition, evidence indicating that health is affected by an array of factors suggests that it may not be realistic to expect the healthcare system to assume a primary role in addressing each of the factors (McGinnis et al., 2002). Instead, it might be more useful for healthcare organizations to assume supporting roles in addressing these issues.
The Centers for Medicare & Medicaid Services (CMS) is testing one strategy to help healthcare organizations assume an effective supporting role. CMS funded a set of Accountable Health Communities (AHCs) beginning in 2017 as pilot programs.Footnote 2 AHCs build information technology infrastructure to facilitate partnerships between healthcare and community organizations (Alley et al., 2016; Brown et al., 2020). The partnerships develop and implement systematic processes to link Medicare and Medicaid beneficiaries with community resources offering services designed to address health-related social needs including housing and food security, reliable transportation, and paying for home utility bills. The partnerships are designed to solve a two-part problem: First, some individuals who are eligible for assistance do not apply for it. Second, some healthcare organizations employ social workers to help individuals identify likely sources of assistance and complete applications, but these efforts are not typically supported by an efficient referral and communication system. For example, a social worker might refer a patient to a specific social service agency. In many communities, that social worker will not receive feedback about this referral to indicate whether the patient applied for assistance, whether the patient was deemed to be eligible, and whether the patient renewed the application in a timely manner. Without this information, the social worker is not equipped to organize an efficient referral system.
The AHC model links traditional healthcare systems with a “bridge organization” that provides referrals to community services. Bridge organizations serve as system hubs that implement a three-step process: awareness, assistance, and alignment. The first step screens beneficiaries for unmet health-related social needs, the second provides community service referrals, and the last aligns community service partners with healthcare providers.
Bridge organizations can include health networks, hospitals, healthcare payers, or academic institutions. For example, St. Joseph’s, a nonprofit healthcare system in Syracuse, New York, implemented the AHC model in 2018. It serves as the hub or bridge organization. St. Joseph’s screens eligible beneficiaries for unmet social needs and refers these individuals to appropriate community services. Preliminary results show a 9% reduction in ED visits in the first year after screening. Program evaluation, to be conducted at the end of the 5-year period in 2022, will provide insights about (i) the relationship between unmet social needs and health and (ii) and the usefulness of this strategy for meeting those needs.
Some analysts argue that healthcare organizations should also provide vigorous support for increased government funding for social service agencies, for education, and for other government-provided services that boost health. Unless these organizations also support tax increases, this strategy requires careful consideration of the trade-offs facing federal and state lawmakers. While this issue is important at both the federal and state levels, it is most clear at the state level. In fiscal year 2019, before states were affected by the economic effects of COVID-19, states spent 38% of state general revenue on education and 16% on Medicaid (Kaiser Family Foundation, 2019). With these two expenditure categories accounting for more than half of state expenditures, substantial increases in expenditures for social services would pose difficult trade-offs for state lawmakers.
3.3 Initiatives to Adjust Provider Quality Metrics
Because social circumstances and behavioral patterns can impact patient health, they can also affect provider performance on quality metrics. Performance on these metrics can affect provider revenue when payment systems include a quality-based incentive. They can also affect the provider’s reputation when the quality scores are publicly available. To the extent that low education and insecure food and housing exert adverse impacts on patient implementation of medical recommendations and patient health outcomes, providers treating disproportionate numbers of patients with low income (SES) are likely to have lower quality scores than comparable providers treating more affluent patients (Kassel, 2014). In this situation, providers treating disproportionate numbers of patients with low SES will receive lower payments than clinicians providing comparable services to more affluent patients. This scenario has generated concern that quality-based incentive payment systems could generate the unintended consequence of reducing resources available to practices focusing on patients with low SES.
In this subsection, we will describe (i) the value-based payment system currently used to adjust Medicare payments, (ii) potential reputation impacts of publicly available quality scores, and (iii) the current policy discussion about differential impacts of value-based payment systems on providers treating more (versus fewer) patients with low SES.
Payments to clinicians for providing care to patients covered by Medicare are adjusted to reflect performance on four types of quality metrics. The system was mandated by Congress in the 2015 Medicare Access and CHIP Reauthorization Act (MACRA). Under the most widely used MACRA track, four types of quality metrics are used to assess clinician or practice performance: traditional quality metrics, total healthcare expenditures for patients attributed to the clinician (or the practice), engagement in quality improvement activities, and the use of interoperable electronic systems to record, store, and exchange health information. Under MACRA, payments to clinicians with low-quality scores are reduced by as much as 9%, while payments to clinicians with high scores are increased by as much as 9% (Centers for Medicare & Medicaid Services, 2020). Top-performing clinicians can receive additional bonus payments (The National Council, 2017).
In addition to this monetary incentive system, Medicare posts clinician-level and practice-level scores online. This creates an additional reputation incentive to earn high scores in the four areas. In addition, many states are creating all-payer claims databases (APCD) which are large state-run databases that include information on the treatments and procedures that generated all healthcare claims submitted to public and private insurers in the state. In many situations, the information will be made available to insurers and researchers to conduct analyses to support efforts to improve healthcare affordability, efficiency, and cost transparency. These databases will contain sufficient data to support analyses of efficiency and quality at the practice level. Currently, more than 30 states maintain an APCD or are developing one (Agency for Healthcare Research and Quality, 2017).
Publicly available performance data are not new. CMS has been posting organization-level data on managed care organization performance on quality measures specified in the Healthcare Effectiveness Data and Information Set (HEDIS) system. These measures provide a broad set of standardized performance measures, to support consumer efforts to select high-quality managed care plans.
These efforts to incentivize healthcare organizations to deliver high-quality healthcare are designed to pursue an important goal. However, the potential adverse – and unintended – consequences for providers treating high numbers of patients with low SES are concerning. Providers affected by value-based payment incentives, such as MACRA, may avoid serving disadvantaged populations and shift to serving more affluent populations. Incentivizing providers to implement strategies to boost patient compliance has also led to discussions of whether providers should be able to “fire” noncompliant patients.
In 2014, the National Quality Forum convened a panel of 26 national experts to consider whether CMS should set a lower performance threshold for providers treating a disproportionate number of patients with low SES, to avoid this unintended consequence (Kassel, 2014). This policy option offers both benefits and costs. The proposal’s key benefit is that it would reduce or eliminate the expected adverse impact of the MACRA system on providers treating disproportionate numbers of patients with low SES. On the other hand, however, the proposal would create a two-tiered definition of quality in which providers can earn comparable rewards by providing lower-quality care to patients with low SES or higher-quality care to patients with patients with higher SES.
Sheingold et al. (2021) suggest that it will be useful to frame the discussion as consideration of two competing viewpoints:
-
(i)
Payment incentives are designed to incentivize providers to deliver high-quality care that is evidence-based and consistent with medical guidelines. Statistical evidence indicates, however, that patients with moderate or high SES receiving this care are likely to experience better health outcomes than patients with low SES who receive the same care. The incentive system should be adjusted to avoid penalizing providers who treat disproportionate numbers of individuals with low SES.
-
(ii)
The payment incentive system should be designed to incentivize providers to generate good health outcomes for all patients. While all patients should receive high-quality care, individuals with low SES may require additional services, including social services, to achieve good health outcomes. Physicians treating disproportionate numbers of these individuals should receive the additional resources needed to achieve these results.
The difference between these two viewpoints highlights the importance of the question of whether those additional services should be funded by healthcare payers and delivered by healthcare provider organizations, or whether it would be more effective to channel those resources directly to agencies responsible for providing social services. It also highlights the limited scope of using payment incentive risk adjustment, as a key strategy for addressing the role of SES in generating health disparities.
4 Conclusion
Evidence indicates that social circumstances and individual health behaviors affect health directly, and they mediate the impact of clinician efforts on patient health. Healthcare organizations face two types of strategic choices. Healthcare organizations could implement programs to mitigate the effects of social circumstances on health, or they could work to address the underlying gaps in social services. If they opt to address gaps in social services, they can either implement programs to address the gaps themselves or they can assume a supportive role by partnering with social service agencies.
Each strategy presents a dilemma that requires careful consideration. If healthcare organizations opt to implement programs designed to mitigate the effects of social circumstances on health, it is important to determine whether these programs are cost effective. If they do not generate sufficient financial benefits to offset the costs, these programs use organizational resources that could be allocated to other programs or services. Organization administrators and clinicians must weigh the trade-offs between programs designed to mitigate the effects of social circumstances on health and competing programs that may serve the same set of patients or different sets of patients.
Second, if the organization opts to focus on the underlying gaps in social services, they face two strategic questions. Can they utilize their resources more effectively by providing services such as housing directly, or should they use these resources to build partnerships with existing social service agencies? In addition, they face an associated question. Should they advocate for increased funding for social service agencies, even if that might encourage lawmakers to reduce funding for healthcare expenditures? Given the interactions among healthcare and other factors that affect health, it is possible that transferring funds from healthcare to social services might strengthen population health. Essentially, healthcare organizations face the question of whether the social service agencies can administer assistance programs more effectively than healthcare organizations.
Finally, current emphasis on value-based payment initiatives poses a difficult question: Should these systems include a more lenient performance standard for providers who treat disproportionate numbers of patients with low income (SES)? This is a thorny question, with logical arguments supporting both sides of the issue. To the extent that social circumstances affect patient health and mediate the health impacts of clinician efforts, applying the same performance standards to practices that do (and do not) treat disproportionate numbers of patients with low SES will shift resources from practices treating disproportionate numbers of low-income patients to practices treating more affluent patients. On the other hand, reducing the performance standard for providers who treat disproportionate numbers of patients with low incomes raises concerns about the implications of a two-tiered quality standard. Recognizing that both of these options pose substantive issues, some analysts argue that it would be useful to enlarge the discussion to consider alternate payment structures.
Notes
- 1.
Causal relationships are identified via experimental design methods. Associative relationships are established via basic regression analysis.
- 2.
See Sheingold et al. (2021) for a discussion of additional steps CMS could take to support efforts to strengthen health equity.
References
Agency for Healthcare Research and Quality. (2017, March). All-payer claims databases. https://www.ahrq.gov/data/apcd/index.html
Aizer, A., & Stroud, L. (2010). Education, knowledge and the evolution of disparities in health. National Bureau of Economic Research. https://doi.org/10.3386/w15840
Alley, D. E., Asomugha, C. N., Conway, P. H., & Sanghavi, D. M. (2016). Accountable health communities-Addressing social needs through Medicare and Medicaid. New England Journal of Medicine, 374(1), 8–11. https://doi.org/10.1056/nejmp1512532
American Cancer Society. (2018). Cancer facts & figures for Hispanics/Latinos 2018–2020. American Cancer Society, Inc. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf
Artaud, F., Sabia, S., Dugravot, A., Kivimaki, M., Singh-Manoux, A., & Elbaz, A. (2017). Trajectories of unhealthy behaviors in midlife and risk of disability at older ages. Innovation in Aging, 1(Suppl_1), 75–75. https://doi.org/10.1093/geroni/igx004.311
Baren, J. M., Shofer, F. S., Ivey, B., Reinhard, S., DeGeus, J., Stahmer, S. A., Panettieri, R., & Hollander, J. E. (2001). A randomized, controlled trial of a simple emergency department intervention to improve the rate of primary care follow-up for patients with acute asthma exacerbations. Annals of Emergency Medicine, 38(2), 115–122. https://doi.org/10.1067/mem.2001.116593
Barker, D. J., Osmond, C., Golding, J., Kuh, D., & Wadsworth, M. E. (1989). Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ, 298(6673), 564–567. https://doi.org/10.1136/bmj.298.6673.564
Barker, D. J., Hales, C. N., Fall, C. H., Osmond, C., Phipps, K., & Clark, P. M. (1993). Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): Relation to reduced fetal growth. Diabetologia, 36(1), 62–67. https://doi.org/10.1007/bf00399095
Beijer, U., Wolf, A., & Fazel, S. (2012). Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: A systematic review and meta-analysis. The Lancet Infectious Diseases, 12(11), 859–870. https://doi.org/10.1016/s1473-3099(12)70177-9
Berkowitz, S. A., Seligman, H. K., & Basu, S. (2017). Impact of food insecurity and SNAP participation on healthcare utilization and expenditures. University of Kentucky Center for Poverty Research Discussion Paper Series. https://uknowledge.uky.edu/ukcpr_papers/103/
Blount, A. (2003). Integrated primary care: Organizing the evidence. Families, Systems & Health: The Journal of Collaborative Family Healthcare, 21(2), 121–133. https://doi.org/10.1037/1091-7527.21.2.121
Brennan, T. A., Dollear, T. J., Hu, M., Matlin, O. S., Shrank, W. H., Choudhry, N. K., & Grambley, W. (2012). An integrated pharmacy-based program improved medication prescription and adherence rates in diabetes patients. Health Affairs, 31(1), 120–129. https://doi.org/10.1377/hlthaff.2011.0931
Brown, J. A., Berzin, O., Clayton, M., Cluff, L., Derzon, J., Evans, L., Farrel, K., Fraze, T., Haber, S., Hessler, D., Husick, C., Liu, E., Parish, W., Payne, J., Renaud, J., Smith, L., Stockdaye, H., & Vincent, A. (2020). Accountable health communities (ahc) model evaluation first evaluation report. RTI International. https://innovation.cms.gov/data-and-reports/2020/ahc-first-eval-rpt
Brunello, G., Fort, M., Schneeweis, N., & Winter-Ebmer, R. (2016). The causal effect of education on health: What is the role of health behaviors? Health Economics, 25(3), 314–336. https://doi.org/10.1002/hec.3141
Buchanan, D., Doblin, B., Sai, T., & Garcia, P. (2006). The effects of respite care for homeless patients: A cohort study. American Journal of Public Health, 96(7), 1278–1281. https://doi.org/10.2105/ajph.2005.067850
Butler, S. M., Matthew, D. B., & Cabello, M. (2017, February 15). Re-balancing medical and social spending to promote health: Increasing state flexibility to improve health through housing. Brookings Institution. https://www.brookings.edu/blog/usc-brookings-schaeffer-on-health-policy/2017/02/15/re-balancing-medical-and-social-spending-to-promote-health-increasing-state-flexibility-to-improve-health-through-housing
Case, A., & Paxson, C. (2002). Parental behavior and child health. Health Affairs, 21(2), 164–178. https://doi.org/10.1377/hlthaff.21.2.164
Case, A., Lubotsky, D., & Paxson, C. (2002). Economic status and health in childhood: The origins of the gradient. The American Economic Review, 92(5), 1308–1334. https://doi.org/10.1257/000282802762024520
Case, A., Fertig, A., & Paxson, C. (2005). The lasting impact of childhood health and circumstance. Journal of Health Economics, 24(2), 365–389. https://doi.org/10.1016/j.jhealeco.2004.09.008
Centers for Disease Control and Prevention (CDC). (1999). Cigarette smoking among adults–United States, 1997. MMWR. Morbidity and Mortality Weekly Report, 48(43), 993–996.
Centers for Medicare and Medicaid Services. (2020, March 23). Quality payment program. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs
Coleman, J. V., Patrick, D. L., Eagle, J., & Hermalin, J. A. (1979). Collaboration, consultation and referral in an integrated health-mental health program at an HMO. Social Work in Health Care, 5(1), 83–96. https://doi.org/10.1300/j010v05n01
Coleman, E. A., Parry, C., Chalmers, S., & Min, S.-J. (2006). The care transitions intervention: Results of a randomized controlled trial. Archives of Internal Medicine, 166(17), 1822–1828. https://doi.org/10.1001/archinte.166.17.1822
Coleman-Jensen, A., Gregory, C., & Singh, A. (2014). Household food security in the United States in 2013. U.S. Department of Agriculture, Economic Research Service. www.ers.usda.gov/publications/err-economic-research-report/err173.aspx
Coleman-Jensen, A., Rabbitt, M., Gregory, C. A., & Singh, A. (2020). Household food security in the United States in 2019. U.S. Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/publications/pub-details/?pubid=99281
Coleman-Jensen, A., Rabbitt, M. P., & Gregory, C. A. (2021, March 21). Food Security in the U.S. US Department of Agriculture, Economic Research Service. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/.
Conley, D., & Bennett, N. G. (2000). Is biology destiny? Birth weight and life chances. American Sociological Review, 65(3), 458–467. https://doi.org/10.2307/2657467
Cook, J. T., Frank, D. A., Levenson, S. M., Neault, N. B., Heeren, T. C., Black, M. M., Berkowitz, C., Casey, P. H., Meyers, A. F., Cutts, D. B., & Chilton, M. (2006). Child food insecurity increases risks posed by household food insecurity to young children’s health. The Journal of Nutrition, 136(4), 1073–1076. https://doi.org/10.1093/jn/136.4.1073
Cranor, C. W., Bunting, B. A., & Christensen, D. B. (2003). The Asheville project: Long-term clinical and economic outcomes of a community pharmacy diabetes care program. Journal of the American Pharmaceutical Association, 43(2), 173–184. https://doi.org/10.1331/108658003321480713
Cummings, N. A. (1990). The impact of psychological intervention on healthcare utilization and costs: The Hawaii Medicaid project. Biodyne Institute.
Cummings, N. A., O’Donohue, W. T., & Cummings, J. L. (2009). The financial dimension of integrated behavioral/primary care. Journal of Clinical Psychology in Medical Settings, 16(1), 31–39. https://doi.org/10.1007/s10880-008-9139-2
Currie, J. (2009). Healthy, wealthy, and wise: Socioeconomic status, poor health in childhood, and human capital development. Journal of Economic Literature, 47(1), 87–122. https://doi.org/10.1257/jel.47.1.87
Currie, J., & Hyson, R. (1999). Is the impact of health shocks cushioned by socioeconomic status? The case of low birthweight. The American Economic Review, 89(2), 245–250. https://doi.org/10.1257/aer.89.2.245
Currie, J., & Lin, W. (2007). Chipping away at health: More on the relationship between income and child health. Health Affairs, 26(2), 331–344. https://doi.org/10.1377/hlthaff.26.2.331
Currie, J., & Moretti, E. (2003). Mother’s education and the intergenerational transmission of human capital: Evidence from college openings. The Quarterly Journal of Economics, 118(4), 1495–1532. https://doi.org/10.1162/003355303322552856
Currie, J., & Stabile, M. (2003). Socioeconomic status and child health: Why is the relationship stronger for older children? The American Economic Review, 93(5), 1813–1823. https://doi.org/10.1257/000282803322655563
Currie, A., Shields, M. A., & Price, S. W. (2007). The child health/family income gradient: Evidence from England. Journal of Health Economics, 26(2), 213–232. https://doi.org/10.1016/j.jhealeco.2006.08.003
Curtis, L. J., Dooley, M. D., Lipman, E. L., & Feeny, D. H. (2001). The role of permanent income and family structure in the determination of child health in Canada. Health Economics, 10(4), 287–302. https://doi.org/10.1002/hec.591
Cutler, D. M., & Lleras-Muney, A. (2010). Understanding differences in health behaviors by education. Journal of Health Economics, 29(1), 1–28. https://doi.org/10.1016/j.jhealeco.2009.10.003
Deming, D. (2009). Early childhood intervention and life-cycle skill development: Evidence from Head Start. American Economic Journal: Applied Economics, 1(3), 111–134. https://doi.org/10.1257/app.1.3.111
Desmond, M., & Bell, M. (2015). Housing, poverty, and the law. Annual Review of Law and Social Science, 11(1), 15–35. https://doi.org/10.1146/annurev-lawsocsci-120814-121623
Distefano, G., & Goodpaster, B. H. (2018). Effects of exercise and aging on skeletal muscle. Cold Spring Harbor Perspectives in Medicine, 8(3). https://doi.org/10.1101/cshperspect.a029785
Eicher-Miller, H. A., Mason, A. C., Weaver, C. M., McCabe, G. P., & Boushey, C. J. (2009). Food insecurity is associated with iron deficiency anemia in US adolescents. The American Journal of Clinical Nutrition, 90(5), 1358–1371. https://doi.org/10.3945/ajcn.2009.27886
Evans, W. N., & Ringel, J. S. (1999). Can higher cigarette taxes improve birth outcomes? Journal of Public Economics, 72(1), 135–154. https://doi.org/10.1016/s0047-2727(98)00090-5
Fera, T., Bluml, B. M., & Ellis, W. M. (2009). Diabetes ten city challenge: Final economic and clinical results. Journal of the American Pharmacists Association, 49(3), 383–391. https://doi.org/10.1331/japha.2009.09015
Fineberg, H. V. (2008). Retooling for an aging America. Medscape Journal of Medicine, 10(8), 188.
Gelberg, L., Robertson, M. J., Arangua, L., Leake, B. D., Sumner, G., Moe, A., Andersen, R. M., Morgenstern, H., & Nyamathi, A. (2012). Prevalence, distribution, and correlates of hepatitis C virus infection among homeless adults in Los Angeles. Public Health Reports, 127(4), 407–421. https://doi.org/10.1177/003335491212700409
Gitlin, L. N., & Wolff, J. (2011). Family involvement in care transitions of older adults: What do we know and where do we go from here? Annual Review of Gerontology & Geriatrics, 31(1), 31–64. https://doi.org/10.1891/0198-8794.31.31
Goldman, D. P., & Smith, J. P. (2002). Can patient self-management help explain the SES health gradient? Proceedings of the National Academy of Sciences of the United States of America, 99(16), 10929–10934. https://doi.org/10.1073/pnas.162086599
Gregory, C. A., & Coleman-Jensen, A. (2017, July 31). Food insecurity, chronic disease, and health among working-age adults. Economic Research Service U.S. Department of Agriculture. https://ageconsearch.umn.edu/record/261813/
Gundersen, C., & Ziliak, J. P. (2015). Food insecurity and health outcomes. Health Affairs, 34(11), 1830–1839.
Hagan, K. A., Chiuve, S. E., Stampfer, M. J., Katz, J. N., & Grodstein, F. (2016). Greater adherence to the alternative healthy eating index is associated with lower incidence of physical function impairment in the nurses’ health study. The Journal of Nutrition, 146(7), 1341–1347. https://doi.org/10.3945/jn.115.227900
Heckman, J. J., Moon, S. H., Pinto, R., Savelyev, P. A., & Yavitz, A. (2010). The rate of return to the HighScope Perry Preschool Program. Journal of Public Economics, 94(1), 114–128.
Heiman, H. J., & Artiga, S. (2015). Beyond health care: The role of social determinants in promoting health and health equity (Issue brief Vol. 4). The Kaiser Commission on Medicaid and the Uninsured. https://www.issuelab.org/resources/22899.pdf
Hood, E. (2005). Dwelling disparities: How poor housing leads to poor health. Environmental Health Perspectives, 113(5). https://doi.org/10.1289/ehp.113-a310
Hunter, S., Harvey, M., Briscombe, B., & Cefalu, M. (2017). Housing for health: A state-of-the-art program for reducing homelessness in Los Angeles County. RAND Corporation. https://www.rand.org/pubs/research_briefs/RB10000.html
Jack, B. W. (2009). A reengineered hospital discharge program to decrease rehospitalization. Annals of Internal Medicine, 150(3), 178. https://doi.org/10.7326/0003-4819-150-3-200902030-00007
Jackson, C. T., Trygstad, T. K., DeWalt, D. A., & DuBard, C. A. (2013). Transitional care cut hospital readmissions for North Carolina Medicaid patients with complex chronic conditions. Health Affairs, 32(8), 1407–1415. https://doi.org/10.1377/hlthaff.2013.0047
Jaworsky, D., Gadermann, A., Duhoux, A., Naismith, T. E., Norena, M., To, M. J., Hwang, S. W., & Palepu, A. (2016). Residential stability reduces unmet health care needs and emergency department utilization among a cohort of homeless and vulnerably housed persons in Canada. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(4), 666–681. https://doi.org/10.1007/s11524-016-0065-6
Johnson, R. C. (2012). Health dynamics and the evolution of health inequality over the life course: The importance of neighborhood and family background. The B.E. Journal of Economic Analysis & Policy, 11(3). https://doi.org/10.1515/1935-1682.2823
Johnson, R. C., & Schoeni, R. F. (2011). The influence of early-life events on human capital, health status, and labor market outcomes over the life course. The B.E. Journal of Economic Analysis & Policy, 11(3). https://doi.org/10.2202/1935-1682.2521
Kaiser Family Foundation. (2019). Distribution of state expenditures (in millions). https://www.kff.org/other/state-indicator/distribution-of-state-spending/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
Kassel, C. (2014, March 27). Should provider performance measures be risk-adjusted for sociodemographic factors? Health Affaris Blog. https://www.healthaffairs.org/do/10.1377/hblog20140327.038175/full/
Katch, H., & Bailey, P. (2020, January 17). Medicaid doesn’t pay for housing. Here’s what it can do to help meet enrollees’ social needs. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20200110.134351/full/
Katon, W. (1995). Collaborative care: Patient satisfaction, outcomes, and medical cost-offset. Family Systems Medicine, 13(3–4), 351–365. https://doi.org/10.1037/h0089387
Kushel, M. B., Perry, S., Bangsberg, D., Clark, R., & Moss, A. R. (2002). Emergency department use among the homeless and marginally housed: Results from a community-based study. American Journal of Public Health, 92(5), 778–784. https://doi.org/10.2105/ajph.92.5.778
Law, C. M., & Shiell, A. W. (1996). Is blood pressure inversely related to birth weight? The strength of evidence from a systematic review of the literature. Journal of Hypertension, 14(8), 935–941. https://doi.org/10.1097/00004872-199608000-00002
Lenz, A. S., Dell’Aquila, J., & Balkin, R. S. (2018). Effectiveness of integrated primary and behavioral healthcare. Journal of Mental Health Counseling, 40(3), 249–265. https://doi.org/10.17744/mehc.40.3.06
Liang, S.-Y., Phillips, K. A., Tye, S., Haas, J. S., & Sakowski, J. (2004). Does patient cost sharing matter? Its impact on recommended versus controversial cancer screening services. The American Journal of Managed Care, 10(2 Pt 1), 99–107.
Manley, A. F. (1996). Physical activity and health: A report of the surgeon general. DIANE Publishing.
Mann, S. L., Wadsworth, M. E., & Colley, J. R. (1992). Accumulation of factors influencing respiratory illness in members of a national birth cohort and their offspring. Journal of Epidemiology and Community Health, 46(3), 286–292. https://doi.org/10.1136/jech.46.3.286
Martinez, O., Jr, Poepsel, M. S., Rolf, M. K., Taylor, B., Dfaapa, P., Wergin, R. L., & Wheeler, P. (2018). National Advisory Committee on rural health and human services. U.S. Department of Health and Human Services. https://uscopdcoalition.org/wp-content/uploads/2020/06/Rural-COPD-Report-December-2018.pdf
McCormick, B., & White, J. (2016). Hospital care and costs for homeless people. Clinical Medicine, 16(6), 506–510. https://doi.org/10.7861/clinmedicine.16-6-506
McGinnis, J. M., & Foege, W. H. (1999). Mortality and morbidity attributable to use of addictive substances in the United States. Proceedings of the Association of American Physicians, 111(2), 109–118. https://doi.org/10.1046/j.1525-1381.1999.09256.x
McGinnis, M. J., Williams-Russo, P., & Knickman, J. R. (2002). The case for more active policy attention to health promotion. Health Affairs, 21(2), 78–93. https://doi.org/10.1377/hlthaff.21.2.78
McIntyre, L., Williams, J. V. A., Lavorato, D. H., & Patten, S. (2013). Depression and suicide ideation in late adolescence and early adulthood are an outcome of child hunger. Journal of Affective Disorders, 150(1), 123–129. https://doi.org/10.1016/j.jad.2012.11.029
McKenzie, B. (2014). Modes less traveled-Bicycling and walking to work in the United States: 2008–2012. American Community Survey Reports. United States Census Bureau. https://www2.census.gov/library/publications/2014/acs/acs-25.pdf
Melchior, M., Chastang, J.-F., Falissard, B., Galéra, C., Tremblay, R. E., Côté, S. M., & Boivin, M. (2012). Food insecurity and children’s mental health: A prospective birth cohort study. PLoS One, 7(12), e52615. https://doi.org/10.1371/journal.pone.0052615
Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2005). Correction: Actual causes of death in the United States, 2000. JAMA: The Journal of the American Medical Association, 293(3), 293–294. https://doi.org/10.1001/jama.293.3.293
Morrison, D. S. (2009). Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. International Journal of Epidemiology, 38(3), 877–883. https://doi.org/10.1093/ije/dyp160
Nagata, J. M., Hernández-Ramos, I., Kurup, A. S., Albrecht, D., Vivas-Torrealba, C., & Franco-Paredes, C. (2013). Social determinants of health and seasonal influenza vaccination in adults ≥65 years: A systematic review of qualitative and quantitative data. BMC Public Health, 13(1), 388. https://doi.org/10.1186/1471-2458-13-388
National Conference of State Legislatures. (2020). Veteran homelessness: Overview of state and federal resources. https://www.ncsl.org/research/military-and-veterans-affairs/veteran-homelessness-an-overview-of-state-and-federal-resources.aspx
National Conference of State Legislatures. (2021, March 16). How states can leverage hospital community benefit policies to advance health equity. https://www.nashp.org/how-states-can-leverage-hospital-community-benefit-policy-to-advance-health-equity/
Naylor, M. D., Brooten, D., Campbell, R., Jacobsen, B. S., Mezey, M. D., Pauly, M. V., & Schwartz, J. S. (1999). Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA: The Journal of the American Medical Association, 281(7), 613–620. https://doi.org/10.1001/jama.281.7.613
Nord, M. (2008, February 1). Disability is an important risk factor for food insecurity. Economic Research Service U.S. Department of Agriculture. https://www.ers.usda.gov/amber-waves/2008/february/disability-is-an-important-risk-factor-for-food-insecurity/
Parra, S. (2016). Predictors of inadequate follow-up of screening mammograms in Hispanic/Latinas in the Northeastern United States. Public Health Theses Yale University. https://elischolar.library.yale.edu/ysphtdl/1223/
Ravelli, A. C., van der Meulen, J. H., Michels, R. P., Osmond, C., Barker, D. J., Hales, C. N., & Bleker, O. P. (1998). Glucose tolerance in adults after prenatal exposure to famine. The Lancet, 351(9097), 173–177. https://doi.org/10.1016/s0140-6736(97)07244-9
Robinson, S. M. (2018). Improving nutrition to support healthy ageing: What are the opportunities for intervention? The Proceedings of the Nutrition Society, 77(3), 257–264. https://doi.org/10.1017/s0029665117004037
Roseboom, T. J., van der Meulen, J. H. P., & Osmond, C. (2000). Coronary heart disease after prenatal exposure to the Dutch famine, 1944–45. Heart, 84(6), 595–598. https://doi.org/10.1136/heart.84.6.595
Rosenzweig, M. R., & Schultz, T. P. (1989). Schooling, information and nonmarket productivity: Contraceptive use and its effectiveness. International Economic Review, 30(2), 457–477. https://doi.org/10.2307/2526657
Sadowski, L. S., Kee, R. A., VanderWeele, T. J., & Buchanan, D. (2009). Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. JAMA: The Journal of the American Medical Association, 301(17), 1771–1778.
Sheingold, S., Zuckerman, R., DeLew, N., & Sommers, B. (2021, July 28). Health equity and value-based payment systems: Moving beyond social risk adjustment. Health Affairs Blog. https://doi.org/10.1377/hblog20210726.546911
Skalicky, A., Meyers, A. F., Adams, W. G., Yang, Z., Cook, J. T., & Frank, D. A. (2006). Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Maternal and Child Health Journal, 10(2), 177–185. https://doi.org/10.1007/s10995-005-0036-0
Sloan, F. A., Brown, D. S., Carlisle, E. S., Picone, G. A., & Lee, P. P. (2004). Monitoring visual status: Why patients do or do not comply with practice guidelines. Health Services Research, 39(5), 1429–1448. https://doi.org/10.1111/j.1475-6773.2004.00297.x
Smith, J. (2007). Diabetes and the rise of the SES health gradient. National Bureau of Economic Research. https://doi.org/10.3386/w12905
Smith, M. (2009). Pharmacists’ role in improving diabetes medication management. Journal of Diabetes Science and Technology, 3(1), 175–179. https://doi.org/10.1177/193229680900300120
Smock, N. (2013, January 14). Affordable Care Act regards pharmacists as health care providers, not just prescription dispensers. Pharmacy Times. https://www.pharmacytimes.com/view/affordable-care-act-regards-pharmacists-as-health-care-providers-not-just-prescription-dispensers
Stahre, M., VanEenwyk, J., Siegel, P., & Njai, R. (2015). Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Preventing Chronic Disease, 12, E109. https://doi.org/10.5888/ped12.140511
Substance Abuse and Mental Health Services Administration. (2011). Current statistics on the prevalence and characteristics of people experiencing homelessness in the United States (Vol. 201). Substance Abuse and Mental Health Services Administration.
Syed, S. T., Gerber, B. S., & Sharp, L. K. (2013). Traveling towards disease: Transportation barriers to health care access. Journal of Community Health, 38(5), 976–993. https://doi.org/10.1007/s10900-013-9681-1
Tanumihardjo, J. P., Gunter, K. E., & Peek, M. E. (2021, June 23). As they take on food insecurity, community-based health care organizations have found four strategies that work. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20210616.615098/abs/
The National Council. (2017). MACRA’s quality payment program: What does it mean for your agency’s Medicare reimbursement? The National Council.
Tsai, J., Doran, K. M., & Rosenheck, R. A. (2013). When health insurance is not a factor: National comparison of homeless and nonhomeless US veterans who use Veterans Affairs Emergency Departments. American Journal of Public Health, 103(S2), S225–S231. https://doi.org/10.2105/ajph.2013.301307
Virapongse, A., & Misky, G. J. (2018). Self-identified social determinants of health during transitions of care in the medically underserved: A narrative review. Journal of General Internal Medicine, 33(11), 1959–1967. https://doi.org/10.1007/s11606-018-4615-3
Wachino, V. (2017, January 17). State flexibility to facilitate timely access to drug therapy by expanding the scope of pharmacy practice using collaborative practice agreements, standing orders or other predetermined protocols. Center for Medicaid and CHIP Services. https://www.medicaid.gov/federal-policy-guidance/downloads/cib011717.pdf
Walker, A. R., & Walker, B. F. (1989). The surgeon general’s report on nutrition and health. The American Journal of Clinical Nutrition, 50(4), 884–886. https://doi.org/10.1093/ajcn/50.4.884
Wang, Y., Yeo, Q. Q., & Ko, Y. (2016). Economic evaluations of pharmacist-managed services in people with diabetes mellitus: A systematic review. Diabetic Medicine: A Journal of the British Diabetic Association, 33(4), 421–427. https://doi.org/10.1111/dme.12976
Williams, S. P., & Bryant, K. L. (2018). Sexually transmitted infection prevalence among homeless adults in the United States: A systematic literature review. Sexually Transmitted Diseases, 45(7), 494–504. https://doi.org/10.1097/olq.0000000000000780
Williams, S. W., Zimmerman, S., & Williams, C. S. (2012). Family caregiver involvement for long-term care residents at the end of life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 67(5), 595–604. https://doi.org/10.1093/geronb/gbs065
Winfield, L., DeSalvo, K., & Muhlestein, D. (2018). Social determinants matter, but who is responsible? 2017 survey of physicians on social determinants of health. 2018 Annual Research Meeting. https://academyhealth.confex.com/academyhealth/2018arm/meetingapp.cgi/Paper/24695
Wolff, J. L., Spillman, B. C., Freedman, V. A., & Kasper, J. D. (2016). A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Internal Medicine, 176(3), 372–379. https://doi.org/10.1001/jamaintermed.2015.7664
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Katsikas, A. (2022). Social Circumstances and Behavioral Patterns: Impacts on Health and Initiatives to Mitigate These Impacts. In: James, L.C., O’Donohue, W., Wendel, J. (eds) Clinical Health Psychology in Military and Veteran Settings. Springer, Cham. https://doi.org/10.1007/978-3-031-12063-3_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-12063-3_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-12062-6
Online ISBN: 978-3-031-12063-3
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)