Abstract
Transoral laser microsurgery (TOLMS) is a widely used surgical approach for treating early glottic and supraglottic carcinomas. It is generally accepted that, in selected patients, it leads to oncological results comparable to other treatment modalities, while treatment-related morbidity is significantly reduced and functional outcomes are equal, if not better, in the long run. A thorough preoperative workup is mandatory before TOLMS and should involve transnasal videolaryngoscopy with the adjunction of bioendoscopic techniques like narrowband imaging, videolaryngostroboscopy, intraoperative rigid telescope evaluation, and, in selected cases, radiologic imaging. TOLMS usually involves the use of a carbon dioxide laser coupled to a surgical microscope through a suspended laryngoscope under general anesthesia. Tumor removal can be carried out en bloc or by serial and oriented piecemeal resections in case of bulkier tumors. A close follow-up is mandatory after this kind of narrow-margin conservative surgery. TOLMS procedures have been categorized by the European Laryngological Society classifications and, consequently, transoral approaches for laryngeal carcinoma are now standardized and lead to reproducible results in the hands of trained surgeons. However, tumors with an anterior transcommissural extension and/or impaired vocal fold mobility should be managed carefully by TOLMS and referred only to highly experienced centers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Early laryngeal cancer
- Transoral laser microsurgery
- Optical biopsy
- Anterior commissure
- Vocal cord mobility impairment
- Laryngeal exposure
- Excisional biopsy
- Surgical margins
- Cordectomy
- Endoscopic supraglottic laryngectomy
-
Transoral laser microsurgery (TOLMS) is suited for the curative treatment of most T1–T2 carcinomas of the glottic and supraglottic larynx.
-
The main advantage of this mini-invasive surgical approach is the minimization of perioperative morbidity and hospital stay. Tracheotomy is rarely required.
-
TOLMS of laryngeal tumors requires a meticulous preoperative evaluation in order to precisely define their superficial and deep extension. The diagnostic workup encompasses in-office transnasal videolaryngoscopy with the implementation of bioendoscopic techniques like narrowband imaging to obtain an “optical biopsy” of the lesion’s nature, videolaryngostroboscopy, computed tomography and/or magnetic resonance in selected cases, preoperative assessment of laryngeal exposure, and rigid angled telescope evaluation under general anesthesia to define the precise superficial extension of the lesion.
-
Classification systems for glottic and supraglottic TOLMS procedures have helped to standardize interventions, improve outcomes research, and ensure reproducible results.
-
Dental injuries, mucosal tears, minor bleeding, postoperative aspiration following wider resections for supraglottic tumors, and glottic synechiae for major transcommissural resections are the most common complications and sequelae.
-
Comprehensive technical equipment, including high-performance optical and carbon dioxide laser systems, focusing devices, operating laryngoscopes, multiple suction devices, and specifically designed instruments are required for successful TOLMS.
-
TOLMS is not suited for tumors with arytenoid fixation. Anterior transcommissural tumors with vertical extension can be managed by TOLMS but are associated with worse oncological and vocal outcomes.
-
With very rare exemptions, subglottic carcinomas are not suited for TOLMS.
24.1 Introduction
The higher frequency of laryngeal cancers is observed at the glottic level (approximately two-thirds), followed by the supraglottic area, while purely subglottic tumors are extremely rare. Among all laryngeal cancers, 53% are diagnosed when still limited to their local extension, when 5-year relative survival is estimated to be 78% (SEER data 2010–2016). Thus, these malignances can be potentially treated at an early stage when treatments can offer sound oncological and good functional outcomes.
Particularly for glottic cancer, hoarseness is often present from the very beginning of the neoplastic process, when the delicate multilayered structure of the vocal folds can be easily altered even by the presence of quite small lesions. Moreover, the predilection site for tumor origin at the level of the vocal cord is represented by its free margin, where the impact of tumor growth on mucosal vibration and its undulatory pattern may be even greater, causing a quite evident dysphonia. This peculiarity of glottic cancers, together with their low propensity to nodal spreading, means that nearly 75% of them are usually diagnosed at an early stage, in contrast with patients affected by supraglottic carcinomas who have, in the majority of cases, intermediate to advanced diseases at their first medical consultation. The distribution of laryngeal cancer burden varies consistently among different countries: the highest incidence is observed in Europe (5.45 new cases per 100,000), especially in the Southern and Mediterranean areas where, by far, the highest incidence of laryngeal cancer in men is reported [1]. Also for this reason, in European countries, surgery for laryngeal cancer has a long and well-established history, with a ratio between death and incidence of this type of cancer reported to be one of the lowest in the world (0.47) [2] (Fig. 24.1).
In contrast to the multimodal approaches usually needed for the management of more advanced stages, for early laryngeal carcinomas (Tis–T2), unimodal treatment (surgery or radiation) is strongly recommended. In the past, to preserve speech and swallowing while avoiding tracheostomy, early-staged cancers were treated by external radiation therapy (RT), keeping surgery (mainly total laryngectomy and open partial laryngectomies) in reserve for salvage. However, over the course of the past 30 years, advances in technology and instrumentation have offered transoral laser microsurgery (TOLMS) as an alternative for the upfront treatment of early laryngeal tumors. With technical advances in transoral surgery achieved during the 1960s by Kleinsasser [3] and his microlaryngoscopic technique of endolaryngeal surgery and the implementation of medical laser systems by Strong and Jako in the 1970s [4], things gradually changed beginning from the early 1980s. Clinical pioneers such as Grossenbacher, Motta, Rudert, and Steiner in Europe and Vaughn, Davis, and Shapshay in North America were able to demonstrate that highly selected malignant lesions of the upper aerodigestive tract could now be treated transorally within narrow margin to preserve the maximal amount of surrounding healthy tissues thus achieving the best possible functional outcomes. The data presented in their studies demonstrated that carbon dioxide (CO2) laser surgery causes minimal morbidity, offers good functional results, and provides an oncologically sound and cost-effective alternative to open surgical procedures and RT. Therefore, CO2 TOLMS (as defined by Remacle and colleagues [5]) is now a widely accepted surgical approach to glottic and supraglottic T1–T2 carcinomas [6, 7]. Nevertheless, CO2 TOLMS for laryngeal cancer is far from being worldwide established, as it encompasses the integration of specific individual clinical expertise and the availability of cutting-edge surgical devices. Notwithstanding, with the advent of new technological devices, CO2 TOLMS is evolving and taking advantage of modern 3D exoscopes, capable to provide a widescreen 3D-magnified vision of the surgical field, that may one day substitute the more traditional operating microscopes [8].
24.2 Preoperative Diagnostic Procedures
A meticulous patient selection is an essential prerequisite in order to successfully treat early laryngeal cancers by CO2 TOLMS. A rigorous preoperative diagnostic workup allows to correctly select cases and minimize intraoperative unexpected findings. This protocol aims not only to define the nature of the lesion but to provide a solid preoperative surgical plan by precisely delineating its superficial and deep extension. In this light, the possibility of intraoperatively tailoring the resection based on the endoscopic evaluation of the tumor provides the surgeon with an additional degree of freedom not conceivable with the traditional open-neck approaches.
The first step of preoperative evaluation starts in the office by a flexible transnasal videolaryngoscopy. The white light endoscopic appearance of laryngeal epithelial abnormalities is highly nonspecific, and preoperative clinical assessment is not reliable in regard to their true final pathology. The same macroscopic appearance can in fact correspond to a large spectrum of possible lesions, ranging from keratosis with or without atypia to invasive carcinoma. Therefore, this initial examination should also encompass a videostroboscopy and bioendoscopy by advanced light filters to enhance the vascular patterns of the lesion. Among the latter, narrowband imaging (NBI) is an established optical technique that enhances the diagnostic capability of endoscopes in characterizing tissues by using narrow bandwidth filters. These filters cut all wavelengths of white light except two narrow wavelengths corresponding to the peak of absorption of hemoglobin and therefore emphasize the darker framework of the capillary vessels on a blue-green mucosal background. Malignant lesions are identified by neoangiogenetic changes in their vascularity, shifting from a parallel course to a perpendicular one, enriched by the presence of intrapapillary capillary loops, designing dark spots that can be spotted within the lesion (Fig. 24.2). On the other hand, the loss of the vocal fold’s mucosal wave at videolaryngostroboscopy (VLS) in a nonpreviously operated/radiated larynx is particularly suspicious for an invasive carcinoma that has transgressed the basal membrane and invaded the underlying vocal ligament, thus impairing the vocal fold vibratory properties [9]. Modern high-definition television devices may deliver clear, magnified images providing a superbly defined delineation of the superficial extent of the lesion. Moreover, this examination, conducted in the awake patient, exploits the precious opportunity to assess laryngeal mobility and sensibility. To date, there is no standard objective measurement of vocal fold/arytenoid range of motion; thus, it can only be subjectively expressed by generic terms ranging from impaired vocal cord mobility (due to tumor mass or vocal muscle invasion) to arytenoid fixation (for posterior paraglottic space invasion, cricoarytenoid joint infiltration, or recurrent nerve involvement). Last but not least, in this clinical setting, a comprehensive examination of the upper aerodigestive tract through oral examination and with the aid of a transnasal flexible videoendoscopy should be always undertaken in order to rule out any synchronous primary tumor.
(a) Longitudinal vascular changes parallel to the surface of the mucosa, (b) longitudinal vascular changes at the margins of a leukoplakia in white light, (c) longitudinal vascular changes at the margins of a leukoplakia in NBI, (d) development of perpendicular vascular changes in neoplasms, (e) glottic erythroplakia in white light, (f) intrapapillary capillary loops in the context on the glottic erythroplakia. (Reproduced from Arens et al. 2016)
The next step of the clinical examination of a laryngeal tumor includes rigid endoscopy under general anesthesia during microlaryngoscopy. With this method, a more detailed multiperspective endoscopic view of the larynx can be obtained by 0° and angled (30°, 45°, 70°, and 120°) rigid telescopes (Fig. 24.3). In this way, particular zones of the larynx and hypopharynx (anterior and posterior commissures, bottom and roof of the ventricle, subglottis, apex of the piriform sinus, and postcricoid area) that are difficult to explore during awake transnasal fiber-optic laryngoscopy can be adequately visualized. At this step, with rigid telescopes, the highest definition in the visualization of the larynx can be now achieved and, with the help of angulated optics and NBI evaluation, the superficial margins of the lesions can be thoroughly assessed. Adjunctive information can be obtained by combining the use of angled telescopes with special probes and microinstrumentation to evert and palpate the free edge of the true vocal cords, lift the false vocal folds to inspect the ventricle, and divaricate the arytenoids.
In this setting, another useful maneuver is represented by saline infusion (SI). In case of glottic cancer limited to the true vocal cord, SI using an appropriately angled needle allows further confirmation of preoperative stroboscopic findings (such as impairment of mucosal wave) regarding involvement of the lamina propria by the neoplastic growth (Fig. 24.4). Complete SI hydrodissection of the mucoligamentous plane, with consequent ballooning and lifting of the lesion from the underlying intermediate layer of the lamina propria, suggests purely intraepithelial confinement of the neoplastic nests. Moreover, the mechanical expansion of Reinke’s space after SI facilitates subsequent removal of the lesion itself, serving as a plane for laser dissection and protecting the vocal ligament by excessive thermal damage when performing a subepithelial dissection. On the other hand, an incomplete or absent SI mucoligamentous hydrodissection has the same implications of a reduced or absent mucosal wave at VLS, and it is associated with the transgression of the basal membrane by neoplastic cells fixing it to the underlying vocal ligament. The results of intraoperative SI should always be integrated with those of preoperative VLS. If these two tests deliver conflicting results, especially in case of NBI-positive vascular pattern, the ensuing cordectomy should be tailored according to the more pessimistic scenario (i.e., as if they were both positive for vocal ligament involvement). Applying such a simple diagnostic algorithm, adequacy of surgical treatment can be obtained in 89% of cases [10].
Applying such a comprehensive pre- and intraoperative diagnostic workup makes, in most cases, incisional biopsy superfluous in the preoperative setting. As a matter of fact, even multiple biopsies (with or without frozen section analysis) can be frequently inadequate in obtaining a precise diagnosis. Furthermore, multiple sampling may cause undue damage and fibrosis to the multilayered and delicate microanatomy of the vocal cord, forcing the surgeon to subsequently perform a wider and deeper resection to excise the tumor and surrounding cicatricial tissues. Several studies [11] showed not only that an accurate pre- and intraoperative diagnostic workup allows to avoid any preemptive biopsy, directly treating a given glottic lesion by a single-stage CO2 TOLMS session, but that it is possible to minimize the rates of over- and undertreatments in terms of cordectomy extension, adequately treating 90% of patients in a single-stage operation [12]. In summary, if an accurate preoperative workup is conducted, the most adequate extension of surgery is selected so that the tumor can be completely excised within ultranarrow, free surgical margins in a single-step operation. This “en bloc” tailored removal of the tumor provides a reliable histopathologic diagnosis and a high local control rate with minimal morbidity and without the sacrifice of an undue amount of surrounding healthy tissue. This phonomicrosurgical approach to early laryngeal cancer has demonstrated its efficacy in several case series [9, 10, 12, 13]. However, some exceptions may require a preoperative histologic evaluation, like in the presence of submucosal lesions, doubt of persistence/recurrence in the irradiated larynx, or unconventional histotypes. Squamous cell carcinoma (SCC) is in fact reported to represent around 98% of laryngeal malignances [2]: it arises from the laryngeal mucosa and is characterized by the presence of altered superficial intrapapillary capillary loops, usually well detectable at NBI. Conversely, other histologies, especially those arising from submucosal structures such as adenocarcinomas and sarcomas, or hematologic neoplasm such as lymphomas, can turn out negative at NBI evaluation and may require different, nonsurgical treatments. In case of suspicious non-mucosal lesions, tomographic imaging should be always required as, in many cases, it can orientate towards the correct diagnosis or confirm the need for an incisional biopsy.
Integration of endoscopic findings with those from radiological imaging is mandatory in some cases even for early laryngeal cancer. Magnetic resonance (MR) has gradually emerged as the preferred method of investigation in such a field due to its superior capability of space and tissue density resolution. Dedicated laryngeal radiofrequency coils may be unavailable in the majority of centers; however, standard MR may provide additional information to conventional computed tomography (CT), especially when cartilage invasion is suspected. However, CT presents some unique advantages: its reduced examination time, especially valuable in the presence of claustrophobic patients with minimal compliance, and its wide availability make it a sound diagnostic tool. When CT findings are unclear, such as in the presence of minimal thyroid cartilage erosion and/or paraglottic space involvement, further insight by MR can increase diagnostic accuracy. The European Laryngological Society (ELS) has recently published an imaging checklist for the preoperative evaluation of laryngeal tumors to be treated by CO2 TOLMS [14] (Table 24.1). The evaluation of the majority of small-volume early laryngeal cancers can rely on the endoscopic preoperative workup described above and will not need a radiological assessment in the first place. However, some locations are more subtle due to a higher risk of deeper infiltration that cannot be uncovered otherwise. Glottic tumors that infiltrate the anterior commissure (AC), particularly those with vertical transglottic extension, should always be evaluated with tomographic imaging as the preepiglottic and paraglottic spaces are almost virtual here and the thyroid cartilage may be infiltrated, therefore excluding the possibility of an adequate CO2 TOLMS treatment. For the same reasons, a tumor that infiltrates the bottom of the laryngeal ventricle may preclude the estimation of its real deep extension at fiber-optic transnasal laryngeal endoscopy and should therefore undergo proper radiological evaluation. Supraglottic cancers, except for limited superficial tumors (such as those of the free edge of the epiglottis), should always be evaluated radiologically as the risk of arytenoid or thyroid cartilage erosion or preepiglottic space invasion is concrete. Moreover, CT and MR also allow evaluation of the regional lymph node status. This should be assessed before planning the most appropriate treatment by simultaneous or delayed neck dissection. The N category plays a definitive role in terms of prognosis of these tumors, particularly when dealing with supraglottic lesions. Combining clinically evident and occult lymph node metastases from intermediate T2 supraglottic tumors, around 20% of them can be expected to present regional disease at the time of diagnosis [15]. Therefore, if tomographic imaging is not planned, neck lymph node ultrasound is strongly recommended in these patients: if suspicious lymph nodes are detected, fine-needle aspiration cytology should be complemented. Systematic and thorough research of distant metastasis is not indicated for early laryngeal cancers. However, taking into consideration patient’s history and smoking habit, chest CT in these patients may rule out the presence of a pulmonary synchronous primary tumor.
Difficult laryngeal exposure represents the main limiting factor for CO2 TOLMS, affecting the chance to obtain free resection margins and consequently adequate tumor control. For this reason, when considering CO2 TOLMS, it is essential to preliminarily assess appropriate visualization of the surgical field through the available operating laryngoscopes. The AC is the most difficult area to properly visualize through the laryngoscope. In 2014, Piazza et al. developed the Laryngoscore, a preoperative predictive score, aimed at anticipating the degree of glottic visualization for each individual patient [16]. The Laryngoscore took into account 11 parameters: the sum of the preoperative score (range, 0–17) was found to be correlated with different ways of AC visualization. In particular, when the Laryngoscore was <6, good laryngeal exposure was obtained in 94% of patients. When the Laryngoscore was ≥6, the exposure was satisfying only in 60% of cases. When the total score was ≥9, a difficult exposure was found in 67% of patients. As stated above, complete tumor visualization is essential in obtaining an adequate CO2 TOLMS resection, and the correlation between laryngeal exposure, assessed using the Laryngoscore, and the postoperative surgical margin status demonstrated that patients with difficult laryngeal exposure based on the Laryngoscore had a higher rate of positive surgical margins [17]. In 2019, the same group published a mini-version of the Laryngoscore, a simplified, less subjective, three-item evaluation score taking into consideration just the interincisor gap, thyro-mental distance, and upper jaw dental status and demonstrating a similar efficacy in predicting adequate laryngeal exposure [18] (Table 24.2).
24.3 Surgical Technique
Under general anesthesia, a laser-safe endotracheal tube is inserted in the trachea. Shielding the endotracheal tube and cuff by cottonoids imbued with saline solution is essential to avoid serious airway complications (ignition of oxygen, perforation of the cuff with possible intraoperative blood inhalation) and a small-caliber tube is usually preferred especially for the management of glottic lesions. For posterior commissure and bulky tumors, jet ventilation might represent an adequate complementary approach [19]. Laryngeal structures are exposed by the largest operating laryngoscope available, with a built-in smoke evacuator channel. Another suction device is handled by the surgeon throughout the intervention and is used to evacuate mucus, saliva, blood, and plume and manipulate endolaryngeal tissues. The appropriate choice of laryngoscopes should meet the demands of different configurations of larynges and tumor locations. For easy exposures, large-bore laryngoscope (i.e., Dedo) allows a comfortable view and use of instruments. Narrow-caliber laryngoscopes (i.e., Ossoff-Karlan-Dedo) serve the purpose for difficult exposures, at the expense of instrument maneuverability and binocular vision. Finally, bivalved devices (i.e., Hinni or Steiner) offer a comprehensive view of the supraglottic region. Moreover, the assistant’s external manipulation of the larynx, by mobilizing it using a hand on the neck, may be necessary to reach an appropriate exposure in anteriorly located lesions.
The most common laser used is the CO2 laser beam, in the infrared region of the light spectrum, with a wavelength of 10.6 μm. This straight laser beam is directed in the surgical field by pairing the micromanipulator with the microscope in a coaxial way and offers several advantages, such as minimal scatter, minimal reflection, and strong absorption by water. The area of surrounding necrosis is less than 0.5 μm with an absorption depth of 0.2 mm. For these reasons, so far, the CO2 surgical laser clearly represents the gold standard tool for the oncological surgery of the larynx. For this purpose, it is generally set at an output power of 2–6 watts in a superpulse, ultrapulse, or continuous mode, at a spot size of approximately 0.8 mm2.
The principle of laser surgery is complete tumor removal, but, unlike open surgery, access to the lesion does not require opening of the laryngeal framework box with the ensuing risk of sacrificing normal tissues such as prelaryngeal muscles, neurovascular bundles, and unaffected laryngeal or pharyngeal mucosa. Therefore, tumor resection is precisely customized and tailored to each individual patient following the specific size and pathways of diffusion of the lesion to be treated. However, in every case, tumors must be resected with sufficiently safe surgical margins (at least 1 mm in width at definitive histopathology is the generally accepted rule for confirmation of an R0 resection). Specimens are excised in one piece whenever possible: while the “en bloc” technique is ideal for limited superficial lesions, on the other hand, due to the small operative field, it is often required to transect larger tumors to assess their depth of invasion and create the necessary visualization and space for piecemeal (or multi-bloc) tumor disassembling and composite resection. Removal of a tumor in two or more portions (a concept first introduced by Wolfgang Steiner, Göttingen, Germany) apparently does not comply with the generally accepted basics of oncologic surgery but is usually reserved for more advanced tumors and has been largely legitimized in other endoscopic surgical procedures like transnasal skull base tumor resections. After removal, however, specimens should be carefully oriented and marked with ink, to facilitate histopathological examination of the most meaningful margins (Fig. 24.5). The value of frozen sections in such a context remains unclear to date, and not all experienced laser surgeons use them routinely.
Scheme of a multiblock excision: (a) trans-tumoral incisions are made in order to assess the depth of infiltration, (b) the first piece is removed, (c) the deep margins of the residual tumor can be assessed, (d) the step is repeated with the adjacent blocks, (e) the final result after the tumor has been excised completely, (f) the blocks are carefully oriented for the pathological evaluation
In early-stage glottic cancer, elective treatment of the neck lymph nodes is not justified as the rate of occult metastases usually does not exceed 8%: this makes these lesions particularly suitable for one-step CO2 TOLMS. By contrast, in supraglottic cancers, treatment of both sides of the neck by selective neck dissection or with RT is strongly warranted, at least for T2 lesions, due to the higher incidence (around 20% of cases) of occult metastases detected [15]. However, the need for an elective neck treatment does not preclude the chance to manage the primary tumor by a transoral approach, possibly associating concomitant or 15-day delayed uni- or bilateral neck dissection according to the relationship of the lesion with the midline.
For what concerns subglottic carcinomas, apart from being very rare, they are generally not suitable for CO2 TOLMS due to exposure issues, being RT or open-neck surgery the preferred treatment options.
24.3.1 Classification of Procedures for Glottic Carcinoma
In 2000, the ELS Working Committee on Nomenclature proposed a classification of endoscopic procedures for the treatment of glottic dysplasia and carcinoma. They did so intending to reach better agreement and uniformity concerning the extent and depth of resection among different cordectomies by offering reproducibility to laryngologists and allow relevant comparisons with the literature when presenting/publishing their oncological and functional outcomes [20]. The classification described eight types of cordectomy: subepithelial (type I), subligamental (type II), transmuscular (type III), total (type IV), and extended cordectomies including the extension to the contralateral vocal fold and the AC (type Va), one arytenoid cartilage (type Vb), subglottic structures (type Vc), or the ventricle and paraglottic space (type Vd). This classification was subsequently widely used internationally by many surgeons to describe their endoscopic procedures. A new cordectomy, encompassing the AC, the anterior part of both true and false vocal folds, and the petiole of the epiglottis (type VI), was later introduced by the ELS Working Committee on Nomenclature in 2007 [21]. A synthesis of the 2000 classification and its 2007 modification is given here (Fig. 24.6).
24.3.1.1 Subepithelial Cordectomy (Type I)
It involves the resection of the vocal fold epithelium, passing through the superficial layer of the lamina propria. This surgical procedure spares the deeper layers of the lamina propria and thus the vocal ligament. Subepithelial cordectomy is performed for cases of vocal fold lesions suspected of premalignant transformation. Ideally, the lesion intended to be treated by type I cordectomy should not be suspicious for malignancy at NBI and should present an intact mucosal wave at VLS. In this circumstance, SI finds its role as it ensures that no infiltration of the vocal ligament is present while facilitating the individuation of the most adequate resection plane. The amount of tissue resected with this procedure makes it inadequate for oncologic purposes: therefore, the main role of type I cordectomy is diagnostic. It can also play a therapeutic role whenever histological results confirm hyperplasia, dysplasia, or, at most, carcinoma in situ without signs of microinvasion. Indeed, by definition, these lesions are in fact limited to the epithelium. On the other hand, if microinvasive carcinoma is identified, subepithelial resection may not achieve safe deep resection margins, and thus, a further procedure (e.g., type II cordectomy) is required.
24.3.1.2 Subligamental Cordectomy (Type II)
It involves the resection of the epithelium, Reinke’s space, and underlying vocal ligament up to the very superficial fibers of the vocal muscle. It is performed by cutting along the interface between the vocal ligament and muscle. The latter is however preserved as much as possible. The resection may extend from the vocal process to the anterior macula flava and may be performed bilaterally if needed. This procedure is indicated whenever a lesion shows clinical signs of neoplastic transformation, especially at NBI, and VLS examination indicates deep infiltration, or impairment/absence of mucosal wave (“vibratory silence”). SI displays no mucoligamentous hydrodissection (absent or incomplete ballooning). When palpated, the vocal cord feels thickened and the mucosa cannot be freely moved over the underlying structures. At a therapeutic level, subligamental cordectomy is indicated for microinvasive or invasive glottic carcinoma (cT1), the latter being limited to the vocal ligament in 95% of cases [11, 13].
24.3.1.3 Transmuscular Cordectomy (Type III)
It is performed by cutting through the vocalis muscle. The resection encompasses the epithelium, lamina propria, and medial portion of the vocalis muscle. The resection may extend from the vocal process to the AC. Partial resection of the ventricular fold may be necessary to expose the lateral extent of the entire vocal fold at the level of the floor of the ventricle, up to the point of its reflection into the bottom and roof of the ventricular cavity. Transmuscular cordectomy is indicated for bulky T1 of the vocal fold causing reduced mobility for a mass effect (without the possibility to precisely evaluate a limited vocal muscle infiltration) or in true T2 lesions infiltrating the vocal muscle itself. In the authors’ hands, however, type III cordectomy is the ideal tool to manage previously biopsied lesions whenever the dissection planes and neoplasm margins are difficult to be ascertained due to the presence of scar tissue. In this scenario, the sacrifice of part of the vocal muscle, at the expense of the vocal outcome, will result in safer resection margins without the need for further reinterventions, which would have a higher cost in terms of vocal muscle volume loss and oncologic outcomes.
24.3.1.4 Total or Complete Cordectomy (Type IV)
It longitudinally extends from the arytenoid to the AC. The depth of the surgical margins reaches the internal perichondrium of the thyroid cartilage ala. Sometimes the perichondrium is included within the resection. Anteriorly, the incision is made in the midline of the AC detaching the macula flava and the Broyle’s ligament from the inner surface of the thyroid cartilage. Total cordectomy is reserved for glottic cancer infiltrating the vocal muscle with impairment of vocal fold mobility (T2) or with limited involvement of the anterior paraglottic space at the glottic level (T3). This condition should be however clearly differentiated from arytenoid hypomobility/fixation due to massive posterior paraglottic space encroachment which, instead, is considered an absolute contraindication to CO2 TOLMS.
24.3.1.5 Extended Cordectomy Encompassing the Contralateral Vocal Fold (Type Va)
Extended cordectomies were meant to describe a heterogeneous array of possible procedures extending beyond the confines of one vocal fold. In particular, type Va is a complete cordectomy extended to the AC and, according to the extent of the tumor, possibly to a segment or the entire length of the contralateral vocal fold. This procedure is somewhat controversial because resection around the AC may be technically demanding, especially in patients with suboptimal laryngeal exposure, and usually leads to poor phonatory results. In case of intraoperative detection of minor thyroid cartilage erosion, CO2 TOLMS should be abandoned in favor of an open-neck procedure (open partial laryngectomies or total laryngectomy according to the different clinical scenarios) or nonsurgical organ preservation attempts.
24.3.1.6 Extended Cordectomy Encompassing the Arytenoid (Type Vb)
It is a complete cordectomy encompassing the arytenoid and is indicated for vocal fold carcinoma involving the vocal process or superficially extending to the arytenoid cartilage posteriorly. The cartilage is thus partially or totally resected. The posterior arytenoid mucosa may be preserved if this decision is oncologically sound. The arytenoid should be mobile and posterior paraglottic space not infiltrated. Otherwise, CO2 TOLMS is usually contraindicated for the high risk of positive surgical margins. The necessary full exposure of the posterior commissure and arytenoid may be reached by either dislodging the orotracheal tube anteriorly and intercalating the operating laryngoscope in between the tube and the posterior commissure or using jet ventilation through a small transglottic catheter [17, 19].
24.3.1.7 Extended Cordectomy Encompassing the Ventricular Fold (Type Vc)
Total cordectomy can be also extended to the mucosa of the laryngeal ventricle, ventricular fold, and paraglottic fat pad. This procedure is indicated for ventricular or transglottic cancers spreading to the bottom and roof of the ventricle (cT2–cT3).
24.3.1.8 Extended Cordectomy Encompassing the Subglottis (Type Vd)
If necessary, an extended cordectomy can be enlarged to include the structures below the glottic plane to expose the cricothyroid membrane and cricoid cartilage. In selected cases, this procedure may be indicated for the removal of cT2 carcinoma with limited subglottic extension without cartilage invasion and/or extension through the cricothyroid and crico-tracheal membranes.
24.3.1.9 Extended Cordectomy for Cancers Arising from the Anterior Commissure (Type VI)
Type VI cordectomy is indicated for tumors originating from the AC, extended (or not) to one or both true and false vocal folds, to the petiole of the epiglottis and/or anterior subglottis, without infiltration of the thyroid cartilage. This procedure includes resection of the AC with the anterior thirds of the true and false vocal cords, Broyle’s tendon, and conoid ligament. To remove the entire AC area within safe margins, the incision should be started above the plane of the false vocal folds, at the level of the epiglottic insertion on the thyroid notch, and then extended downwards through the Broyle’s ligament, at least until the inferior margin of the thyroid cartilage. Inclusion of the subglottic mucosa and cricothyroid membrane into the surgical specimen is justified since AC cancers tend to spread towards the anterior subglottic lymphatic vessels. This technique is the ideal tool for treating AC cancers with vertical extension (anterior transcommissural tumors) and properly clear the inside aspect of the anterior laryngeal box.
24.3.2 Classification of Procedures for Supraglottic Carcinoma
Among the indications of CO2 TOLMS for laryngeal cancer, supraglottic laryngectomies for early-stage supraglottic lesions definitively play a prominent role. This is mainly due to the oncological outcomes described, comparable to those obtained by other therapeutic options, and to the better functional results (especially when compared to those achieved by OPHL) [22]. Of course, there remain various indications for conservative open neck approaches like, for example, OPHL type I which is, again, a good reason why head and neck surgeons should be trained in the wide field of transoral and open laryngeal surgery, not focusing uniquely on one treatment method, especially when dealing with oncologic issues. The main advantage of CO2 TOLMS for supraglottic tumors is that the resection can be personalized and tailored to the precise extent of a given tumor. Moreover, hospitalization times are shorter, and morbidity is lower, as it avoids tracheostomy in the vast majority of cases [23]. “En bloc” resection is mainly possible for small (cT1 to small-volume cT2), circumscribed carcinomas of the supraglottis. Surgical technique is comparable to resection of early glottic cancer even though tumors in this area should be resected with wider margins since they are well known to have a more aggressive biologic behavior than glottic tumors, a higher tendency of lymphatic spread, and such increased surgical aggressiveness usually do not compromise vocal outcomes and swallowing. If multi-bloc (or piecemeal) resection is needed (especially in large-volume cT2–cT3 lesions), it mandates a high accuracy in the precise orientation of the specimen, close cooperation with the pathologist to accurately assess the adequacy of the resection margins, and true multidisciplinary teamwork in understanding the three-dimensional tumor volume and nature of surgical margins in order to appropriately select those patients needing adjuvant treatments.
Tumor extension of infrahyoid epiglottic carcinomas is rather difficult to determine preoperatively, particularly in the petiolar area. Thus, it is often difficult to differentiate between superficial T1 and deeper T3 carcinomas before surgery, even in the presence of a state-of-the-art imaging. However, clinical experience shows that preepiglottic space infiltration should be anticipated for all tumors of the infrahyoid region. However, in the case of the demonstrated deep involvement of such a visceral space, CO2 TOLMS is not contraindicated, but the treating surgeon should be prepared to comprehensively manage a cT3 lesion. Bleeding of vessels in this area is usually well controlled by conventional electrocautery and titanium clips, which have proved to be appropriate especially when the superior laryngeal pedicle is encountered at the level of the lateral portion of the pharyngoepiglottic fold. Depending on the extent of planned resection, unilateral arytenoid sacrifice can be considered, knowing that it will cause the highest degree of postoperative swallowing difficulties encountered after CO2 TOLMS [24]. However, resection of both arytenoids must be avoided to prevent persistent severe postoperative dysphagia with massive aspiration.
In contrast to open neck surgery, nasogastric feeding tube, when needed, can be maintained for a few days only, and temporary tracheostomy can be generally avoided. In the authors’ experience, nasogastric feeding tube is mainly indicated for those procedures involving wider supraglottic resections, especially when one arytenoid has been (sub)totally resected. Of course, this does not mean that supraglottic partial laryngectomy by CO2 TOLMS is a risk-free method: there are cases with significant postoperative bleeding or persistent functional deficits such as swallowing difficulties with aspiration. Therefore, as for every other therapeutic approach, proper patient selection with respect to age, functional status, and extent of surgical resection should be always taken into account, as postoperative rehabilitation may be demanding. Regarding the risk of postoperative bleeding, it should be ensured that patients remain under continuous supervision, with daily fiber-optic transnasal endoscopies, at least during the first 5–6 postoperative days, so they can be adequately treated in case of an emergency, including rapid intubation if required.
Several complications, regarding around 30% of the overall procedures, have been reported for CO2 TOLMS of supraglottic carcinomas: local infection, chondronecrosis, subcutaneous emphysema, salivary fistula, bleeding, respiratory distress due to stenosis or edema, swallowing difficulties, and aspiration pneumonia [25]. The complication rate is determined mainly by the surgeon’s experience and extent of resection. This is the reason why clinical training should start with procedures for circumscribed supraglottic lesions and, later, after gaining adequate experience, the treatment spectrum can be enlarged to more extended supraglottic carcinomas.
In 2009, the ELS Working Committee on Nomenclature proposed a classification for endoscopic supraglottic partial laryngectomies [26]. A synthesis of this classification is herein discussed (Fig. 24.7).
24.3.2.1 Limited Excision (Type I)
This type of supraglottic resection entails the excision of small superficial tumors on the free border of the epiglottis, aryepiglottic fold, arytenoid or ventricular fold, or any other part of the supraglottis.
24.3.2.2 Medial Supraglottic Laryngectomy with Partial Resection of the Preepiglottic Space (Type II)
In the case of small and superficial T1 tumors of the laryngeal surface of the epiglottis, located above the hyoid bone, the resection may include half of the suprahyoid epiglottis (type IIa). For tumors extending below the hyoid bone, a total epiglottectomy may be needed (type IIb). The section line goes through the preepiglottic space without its complete excision. The pharyngoepiglottic, aryepiglottic, and ventricular folds are preserved.
24.3.2.3 Medial Supraglottic Laryngectomy with Resection of the Preepiglottic Space (Type III)
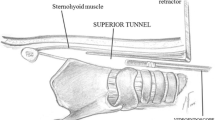
Resection of T2 tumors extending to the petiole of the epiglottis must include the preepiglottic space (type IIIa). The surgical incision is carried along the valleculae until the hyoid bone is reached. The dissection then moves caudally from the hyoid bone towards the thyrohyoid membrane until the upper border of the thyroid cartilage is exposed. From this point, the whole entity of the preepiglottic space is removed along the inner surface of the thyroid laminae together with the epiglottis towards the anterior commissure of the vocal folds. T2 tumors of the infrahyoid epiglottis extending to the ventricular fold can be resected with the same technique (type IIIb). The ventricular folds can be completely dissected from the thyroid cartilage along the inner surface towards the laryngeal ventricle.
24.3.2.4 Lateral Supraglottic Laryngectomy (Type IV)
In case of tumors of the three-folds’ region, which includes the lateral free edge of the epiglottis, the aryepiglottic, and the pharyngoepiglottic folds with possible extension to the ventricular bands, the resection includes the free edge of the epiglottis, the medial wall of the piriform sinus, and the ventricular fold (type IVa). In case of extension to the arytenoid, the resection will encompass the most advanced and aggressive form of supraglottic resection, potentially including a significant portion of the adjacent piriform sinus (type IVb).
Since its publication, the ELS classification system has been cited hundreds of times in the literature [27]. Numerous centers in various countries have adopted this system to describe the type of resection made. This classification allows reproducibility of the technique and serves to improve the teaching and training of inexperienced surgeons in endoscopic cordectomy and supraglottic partial resections.
24.4 Recurrence: Follow-Up, Diagnosis, and Management
One essential prerequisite for the transoral management of laryngeal tumors is ensuring adequate patient compliance to a compulsive postoperative follow-up. Tailored endoscopic resections are often performed within millimetric safe margins and such an ultraconservative approach is potentially dangerous if patients escape regular controls. Detection of early recurrence is, in fact, important since transoral procedures can still be an option for managing recurrences in these patients. Therefore, the rationale behind the need for a postoperative follow-up includes evaluation of treatment response, early identification of recurrence, possible detection of further metachronous tumors, management of complications, and optimization of voice/swallowing rehabilitation.
In this context, ventricular fold resection before approaching every glottic lesion gives not only the advantage to enhance the exposure during primary surgery, but it also facilitates subsequent transnasal fiber-optic laryngoscopy control during follow-up. Particularly when dealing with tumors at high risk of recurrence (e.g., T2 glottic lesions with anterior transcommissural extension, or supraglottic tumors with lateral extension to the bottom of the ventricle and paraglottic space), an even closer clinical follow-up is strongly recommended. In particular, when dealing with such intermediate to advanced tumors, a CT and/or MR follow-up should be also combined and scheduled twice a year for the first 2 years after surgery, even in case of a negative clinical evaluation [28].
In 2014, a working group of the Head and Neck Cancer Committee of the ELS published a paper containing evidence-based recommendations regarding laryngeal cancer follow-up [29]. According to their work, patients should be followed up for a minimum of 5 years with prolonged surveillance for those with a high risk of late recurrence (e.g., active smokers). When the risk of locoregional recurrence is high, patients should be followed up at least bimonthly in the first 2 years and quarterly to every 6 months in the subsequent years. However, longer intervals can be proposed for smaller lesions (i.e., glottic T1) with clear margins. Clinical assessment should be conducted by a dedicated otolaryngologist and it should include an adequate examination of the entire mucosal lining of the upper aerodigestive tract (in order to detect possible second primary tumors) and neck palpation. Seriated video-recorded examinations using high-resolution flexible endoscopes are of paramount value for sharing opinions between different examiners, storing images of individual patients, and making comparisons during the entire posttherapeutic period. NBI, possibly associated with high-definition television technology, can enhance the chance of detecting superficial persistence/recurrences or second primary tumors (Fig. 24.8). A second-look microlaryngoscopy should be reserved to selected cases, as for uncertain (close or altered for iatrogenic artifacts) surgical margins, granulomas, webs, or other post-excisional abnormal tissue growth at the level of the primary resection site, and should not be performed before 8 weeks from surgery for possible confounding factors due to the ongoing healing process.
As previously described in the preoperative setting, strict cooperation between the surgeon and an experienced radiologist is mandatory during follow-up. The authors’ policy encompasses periodic CT and/or MR (even in the absence of endoscopic abnormalities) in patients with T2 or more advanced glottic and supraglottic tumors. Any endoscopic abnormalities deemed not related to normal postoperative sequelae and hiding possible deep patterns of disease progression should be immediately evaluated by the appropriate imaging modality. Neck monitoring can be performed simply with clinical examination for early glottic tumors, especially considering their low propensity for nodal involvement. An ultrasonography every 4 months during the first 2 years, when not performing CT, is indicated in patients with T2 supraglottic tumors submitted to a “wait and see” policy of the neck, while longer intervals (i.e., once a year) can be adopted for patients treated by elective neck dissection. In case of suspicious ultrasonographic findings, fine-needle aspiration cytology is strongly recommended. For early glottic cancer, imaging for distant metastasis detection may not be required, even though monitoring of the chest in the quest of metachronous lung tumors is strongly warranted, especially in active smokers. This type of surveillance may be also indicated for T2 supraglottic cancers, especially if nodal involvement was present at the time of treatment.
Recurrences after transoral surgery can follow completely different patterns of progression. Aside from superficial persistence/recurrence of mucosal dysplasia with possible progression to invasive cancer, directly detectable by endoscopic evaluation, the main concerns of follow-up examination should always be directed to early diagnosis of deep submucosal progression to the visceral spaces, laryngeal framework, and/or soft tissues of the neck (Fig. 24.9). Symptoms such as worsening dysphonia and progressive dysphagia with associated otalgia should always be taken into account, with a prompt, careful search for submucosal laryngo-hypopharyngeal bulging, impaired vocal cord and/or arytenoid mobility, or subglottic mass. The presence of any of these clinical features should require immediate evaluation by neck CT or MR.
If local recurrence is detected, a larger number of retreatment options are still available after initial CO2 TOLMS than after initial RT or OPHL. In fact, after transoral surgery, no increased rate of wound complications was reported for redo-CO2 TOLMS, different from what was observed after previous RT. Moreover, in this case, the laryngeal framework is still intact, thus preventing early extralaryngeal spread of local failures. These characteristics make local recurrences after transoral surgery still manageable either by CO2 TOLMS again or open surgery: however, when detected early, local recurrences can be safely treated by organ preservation surgery or radiotherapy [30]. If superficial recurrence occurs, the oncological outcomes are usually not worsened in such a salvage scenario, being comparable to those observed in the primary therapeutic setting. By contrast, a submucosal progression of residual neoplastic cells towards the deep visceral spaces is certainly burdened by worse prognosis, even if still manageable by salvage treatments. In fact, previous transoral removal of some natural barriers to the tumor spread (Broyle’s ligament, conus elasticus, vocal ligament, quadrangular membrane, and epiglottis) makes the subsequent patterns of tumor diffusion somewhat unpredictable. However, preservation of the cartilaginous laryngeal framework during initial laser surgery usually prevents recurrences from spreading beyond the larynx for a long time.
24.5 Oncological Outcomes
Oncological data on CO2 TOLMS for T1–T2 carcinomas of the larynx are exclusively based on retrospective studies and meta-analyses (level III and IV evidence). Prospective randomized trials comparing oncological outcomes of different therapeutic approaches are currently not available.
24.5.1 Glottic Cancer
The existing data on T1 glottic carcinomas reveal a good 5-year local control ranging from 85% to 100% after transoral surgery, open partial laryngectomies, or RT with no significant difference between these treatment modalities. Slightly lower control rates (66%–100%) are reported after transoral surgery for T2 glottic carcinomas, with results comparable to OPHL and RT as well [31, 32]. Similarly, the meta-analyses present in the literature do not show a significant difference in terms of local control after CO2 TOLMS or RT [33, 34]: nevertheless, a trend towards better laryngectomy-free survival for transoral surgery was observed in some studies [33, 35]. This can be explained by the fact that, when RT is used as the primary treatment modality, if recurrence occurs, patients can only be further treated surgically, by total laryngectomy as the gold standard treatment for salvage. On the other hand, when CO2 TOLMS is applied as the first-line treatment, in case of recurrence, RT can still be used as salvage therapy. Moreover, one final advantage of transoral surgery is that, in contrast to OPHL, age does not represent a contraindication.
24.5.2 Supraglottic Cancer
As for glottic carcinoma, when discussing the optimal treatment option for supraglottic cancer, it must be considered that the primary tumor can be successfully treated either by CO2 TOLMS, OPHL, or RT in most cases. For what concerns transoral surgery, the reported 5-year local control rates range from 66% to 92% for T1–T2 supraglottic carcinomas, with laryngeal preservation obtainable in 85%–90% of cases [23, 36, 37]. A 2016 meta-analysis by Patel et al. suggests that patients undergoing primary organ-preservation surgery have better survival than those treated by primary RT [38]: in this review, OPHLs were also included; however, long-term oncologic outcomes comparing CO2 TOLMS and open surgery suggest that their results are similar [39]. From the oncological point of view, one of the advantages of transoral surgery combined with neck dissection compared to RT is the ability of the former approach to identify patients with occult nodal metastasis in the neck. This is an important consideration given that up to 20% of patients with early supraglottic cancer may have occult nodal metastasis [15]. Thus, although these patients are early staged at the time of recruitment, the discovery of positive nodal metastases after elective neck dissection can result in upstaging and adjuvant therapy may be recommended as needed.
24.5.3 Transoral Laser Microsurgery Excision Margins
The development of modern laser systems permits laser application with lower power settings, so that charring and artifacts at the level of the specimen margins are greatly reduced in comparison to what was observed in the past using older laser systems. Thus, it is nowadays easier for pathologists to properly evaluate the resection margins. It is widely accepted that ≥1 millimeter free resection margins, especially at the level of the glottic plane, should be considered as negative. Below this threshold, a close resection margin is usually defined [40]. As every narrow margin surgery, CO2 TOLMS may present close and positive margins in around 50% of the cases at the final histopathologic report: nevertheless, up to 80% of close and positive margins may result negative at a subsequent second-look, being indeed false positives [38,49,42]. Post-resection and postfixation shrinkage of the surgical specimen and artifacts caused by the CO2 laser thermal effect may alter the histological evaluation and are at least partially responsible for the high incidence of apparently unsafe surgical margins. Therefore, contrary to conventional open surgery, the report of a final close/positive margin after transoral laser surgery may not always require a reexcision. Indeed, the impact of margin status on survival rates remains controversial: whereas some authors found close and positive margins to be independent risk factors for recurrence and poorer survival rates, others did not find any significant variations compared with negative ones.
On a retrospective multi-institutional series of 634 patients by Fiz and coworkers, close and positive single superficial margins did not negatively affect DSS in respect to negative ones (98.7%, 100%, and 100%). However, positive multiple superficial, as well as positive deep margins, determined a slight, but significant, reduction of DSS compared with the negative ones (93.6% and 97% vs. 100%, respectively) [43]. Therefore, the authors’ policy is to perform a watchful waiting in patients with close superficial and positive single superficial margins. Instead, a second-look microlaryngoscopy seems preferable in case of deep and positive multiple superficial margins. Finally, according to some authors, intraoperative assessment of margins by means of frozen section can limit the need for second-look surgeries. Remacle and colleagues assessed the reliability of this method by comparing frozen section outcomes with the results of the final histology in 97 patients submitted to CO2 TOLMS for glottic carcinomas at different stages: 94.8% of the frozen sections were later histologically confirmed at definitive examination after formalin fixation [44]. This surgical technique may be indeed time-consuming if implemented routinely but offer a reliable aid in selected complex cases.
24.5.4 Anterior Commissure Involvement and Vocal Fold Mobility Impairment
Among early glottic cancers, several tumors with different locations and sizes are sometimes grouped together. Recent publications have underlined that not all sites and subsites of the larynx, when involved, share the same prognosis when treated by CO2 TOLMS. As such, we designed a 3D map of the larynx characterizing diverse zones with different oncologic outcomes [45]. According to this approach, there are two broad categories of early glottic tumors burdened by a potentially worse prognosis: tumors involving the AC with vertical extension towards the supra- and/or subglottis and tumors deeply invading the vocal muscle.
The oncological meaning of neoplastic AC invasion has been repeatedly debated throughout the literature. From the most recent systematic review on the theme by Hendriksma and Sjögren, no consistent results emerge analyzing the series present in the literature, though a trend towards poorer outcomes can be observed [46]. This might be explained by the fact that no standard definition and reporting on AC exist. In the authors’ opinion, the AC should not be considered a single spot in the glottis but, instead, a 3D space in close relation with the adjacent visceral spaces (i.e., the preepiglottic upwards and the anterosuperior paraglottic spaces laterally). Several studies have shown that AC involvement is a significant variable affecting both local control and organ preservation rate, and therefore, they all propose a more aggressive treatment for these kinds of tumor [45, 47, 48]. It is the authors’ opinion that particular attention should be paid when vertically AC-involving tumors are managed by CO2 TOLMS (Fig. 24.10): in these cases, a type VI cordectomy should be used to clear all the anterior laryngeal compartment, potentially from the mid-true and false cords to the epiglottic petiole, cricoid arch, and inner perichondrium of the thyroid laminae. To achieve safe oncological results, standard requirements should include a proper diagnostic workup with optical biopsy (to correctly assess the tumor margins) and tomographic imaging (to exclude cartilage involvement), complete tumor exposure, and adequate surgical expertise [49]. The latter has been demonstrated to significantly increase the outcomes in this kind of tumors [47, 50]. The slightly worse results offered by CO2 TOLMS for AC-infiltrating tumors in respect to OPHL may be due to the higher difficulty to completely expose the AC in many patients and the close proximity of the underlying cartilage that, if infiltrated, offers low chances to be controlled by laser alone. Therefore, in fit patients, supracricoid OPHL may be more appropriate for these lesions, as consistent data in the literature demonstrate that satisfying local control rates can be achieved with this technique [51, 52].
Vocal fold mobility impairment should be clearly distinguished from vocal fold fixation. The latter is, in fact, the result of the arytenoid fixation and therefore defines a posterior-invading T3 carcinoma not suitable for CO2 TOLMS resection. On the other hand, vocal fold hypomobility, which clinically defines a T2 tumor, arises when the vocal muscle is deeply infiltrated [53]. Nevertheless, also tumors superficially spreading to the supraglottis and subglottis are categorized as T2 (formerly T2a in older versions of the TNM as distinguished from T2b for vocal cord mobility impairment), but according to some authors, these two subsets of patients may still have different outcomes and should be distinguished along with all the statistical analysis on the subject. According to the latest review on the topic [54], the few studies reporting separately oncologic outcomes of T2a and T2b demonstrated poorer outcomes of the latter category. In this regard, T2 for impaired mobility should be treated more aggressively with at least a type IV cordectomy in order to fully resect all the vocal muscle. Moreover, considering that no clear boundaries exist between the vocal muscle and the paraglottic space as the muscle fibers gradually fade in the adipose tissue, some authors have argued that all the lateral paraglottic compartment up to the vocal process of the arytenoid should be surgically cleared for these tumors. One of the remaining problems concerning the definition of the T2 category in case of vocal cord hypomobility is the difficulty in clinically quantifying it in an objective way. During pathological evaluation, however, significant invasion of the thyroarytenoid muscle (up to its half in depth or more) might define a pT2 carcinoma [55], as it has been demonstrated that vocal muscle infiltration is almost absent in the histological evaluation of T1 lesions [13].
24.6 Functional Outcomes
Functional preservation during the treatment of early glottic cancer should aim to guarantee the best vocal and swallowing outcomes. Swallowing is usually not impaired after standard cordectomies. However, an impairment may arise when the surgeon embraces more extended (type V and VI cordectomies) procedures to treat more advanced glottic tumors or those with significant supraglottic extension. On the other hand, voice quality after CO2 TOLMS mainly depends on the grade of glottic gap resulting from the loss of vocal fold volume after the operation. However, it should be noted that also other areas of the larynx might work as a glottis substitute after surgery. Thus, voice quality may vary significantly despite similar interventions in different patients. For early glottic cancer, both CO2 TOLMS and RT are recognized as the gold standard treatment. While the oncologic outcomes of both modalities are similar, controversy exists as to which treatment leads to better functional preservation, especially in terms of voice quality. One of the historical arguments supporting RT for early glottic cancer has always been better vocal function when compared to cordectomy through thyrotomy and vertical partial laryngectomies [56]. However, different transoral procedures can vary a lot in terms of volume of vocal cord resected and thus several studies missed the chance to draw precise comparisons between CO2 TOLMS and RT regarding vocal outcomes. In this light, the ELS classification allows defining and clearly distinguishing the extent of excision, which facilitates making meaningful comparisons between vocal outcomes after different types of cordectomy [58]. Another consequence of such a classification is the possibility to compare vocal outcomes after endoscopic surgery with those achieved after RT. The University of Brescia retrospectively analyzed the functional outcomes after different types of cordectomy performed for early glottic cancer [57, 59]. In those patients, no statistically significant difference in the voice after type I and II cordectomy compared to a group of normal subjects was observed. Significant and persistent dysphonia was documented only after type III, IV, and V resections, mainly due to two key factors: anterior commissure synechiae (particularly after type Va cordectomy) and substantial glottic gap after removal of a significant amount of vocal muscle (more than one-third of its depth), necessitating further phonosurgical procedures in order to improve voice quality. For T1b tumors involving the anterior thirds of both vocal folds or the AC in a horizontal fashion, a staged surgery separately conducted on both sides may be considered for selected patients to maximize vocal outcomes reducing the risk of anterior synechiae. A silicon keel may be also positioned at the glottic level but its removal invariably requires a second surgery. Revision phonosurgery procedures can be undertaken in patients with severe dysphonia after the histological report with negative margins. Finally, when compared to OPHL, CO2 TOLMS offers the best advantages in terms of functional outcomes: tracheotomy is avoided, vocal outcome is superior, swallowing function is intact, and the patient can restart oral diet from the day after surgery [60]. Functional preservation for the supraglottic larynx aims to maintain airway patency and oral feeding. In this regard, functional results after CO2 TOLMS are highly satisfactory with very rare sequelae [61]. Moreover, especially when compared to open surgery, transoral procedures result in a reduced incidence of dysphagia, shorter hospitalization, and a low incidence of gastrostomies and tracheostomies [60]. However, to date, no head-to-head studies are available confronting CO2 TOLMS, RT, and transoral robotic surgery in terms of functional outcomes for supraglottic cancers due to the well-known difficulties in the design and performance of prospective randomized controlled surgical trials.
24.7 Conclusions
-
CO2 TOLMS is a cost-effective and time-sparing treatment providing sound oncologic results and favorable functional outcomes with low complication rates in early glottic and supraglottic carcinomas.
-
An accurate preoperative and intraoperative workup, including the use of videolaryngostroboscopy and biologic endoscopy techniques, ensure a customized, oncologically safe resection with minimal sacrifice of surrounding healthy tissue.
-
Adequate laryngeal exposure is an essential prerequisite especially for the treatment of glottic tumors, and it should be assessed during in-office evaluation whenever possible.
-
Adequate imaging of the larynx should be performed in the presence of AC-involving glottic lesions and vocal cord mobility-impairing carcinomas and most supraglottic lesions, to assess the true extent of the tumor before planning endoscopic surgery.
-
In the absence of clinically evident metastasis, elective neck dissection is not necessary for early glottic carcinoma, while bilateral neck dissection is advised for T2 supraglottic carcinoma involving the midline.
-
With rare exceptions, subglottic carcinomas are not suited for transoral surgery.
-
En bloc resection is feasible in most cases of early laryngeal cancer. For bulkier tumors, a multi-bloc or piecemeal resection with meticulous orientation for pathological assessment is recommended.
-
Patient compliance to a compulsive postoperative follow-up is mandatory as CO2 TOLMS consists of tailored transoral microsurgery often performed within millimetric safe margins.
-
The incidence of positive margins in CO2 TOLMS is high but its real impact on oncologic outcomes is debated. In this scenario, a second-look procedure is the safest option, but it may reveal no tumor left in up to 80% of cases. A watchful waiting policy can be viable for selected cases.
-
Tumors arising from the AC, especially on a vertical plane, are particularly difficult to expose and may offer poorer outcomes if treated by CO2 TOLMS especially when not properly staged and evaluated. In these cases, open partial laryngectomies may be considered as a sound surgical alternative.
Change history
10 February 2023
The last name of Pamela Dela Cruz was unfortunately published as P. D. Cruz instead of P. Dela Cruz. This error has now been corrected.
Abbreviations
- AC:
-
Anterior commissure
- CT:
-
Computed tomography
- ELS:
-
European Laryngological Society
- MR:
-
magnetic resonance
- NBI:
-
Narrowband imaging
- OPHL:
-
Open partial horizontal laryngectomies
- RT:
-
Radiotherapy
- SCC:
-
Squamous cell carcinoma
- SI:
-
Saline infusion
- TOLMS:
-
Transoral laser microsurgery
- VLS:
-
Videolaryngostroboscopy
References
Bradley PJ, Piazza C, Paderno A. A roadmap of six different pathways to improve survival in laryngeal cancer patients. Curr Opin Otolaryngol Head Neck Surg. 2021;29(2):65–78. https://doi.org/10.1097/MOO.0000000000000684.
Nocini R, Molteni G, Mattiuzzi C, Lippi G. Updates on larynx cancer epidemiology. Chinese J Cancer Res. 2020;32(1):18–25. https://doi.org/10.21147/j.issn.1000-9604.2020.01.03.
Kleinsasser O. Laryngomicroscopy (lens laryngoscopy) and its importance in the diagnosis of premorbid diseases and early forms of carcinoma of the labium vocale. Arch fur Ohren-Nasen- und Kehlkopfheilkd. 1962;180:724–7.
Strong MS, Jako GJ. Laser surgery in the larynx. Early clinical experience with continuous CO 2 laser. Ann Otol Rhinol Laryngol. 1972;81(6):791–8. https://doi.org/10.1177/000348947208100606.
Remacle M, Arens C, Eldin MB, et al. Laser-assisted surgery of the upper aero-digestive tract: a clarification of nomenclature. A consensus statement of the European Laryngological Society. Eur Arch Oto-Rhino-Laryngol. 2017;274(10):3723–7. https://doi.org/10.1007/s00405-017-4708-3.
Ambrosch P. The role of laser microsurgery in the treatment of laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg. 2007;15(2):82–8. https://doi.org/10.1097/MOO.0b013e3280147336.
Piazza C, Peretti G, Vander PV. Editorial: Advances in transoral approaches for laryngeal cancer. Front Oncol. 2018;8(OCT):1–3. https://doi.org/10.3389/fonc.2018.00455.
Alberto, Paderno Alberto, Deganello Davide, Lancini Cesare, Piazza. Is the exoscope ready to replace the operative microscope in transoral surgery?. Curr Opin Otolaryngol Head Neck Surg. 2022;30(2):79–86. https://doi.org/10.1097/MOO.0000000000000794.
Arens C, Piazza C, Andrea M, et al. Proposal for a descriptive guideline of vascular changes in lesions of the vocal folds by the committee on endoscopic laryngeal imaging of the European laryngological society. Eur Arch Oto-Rhino-Laryngol. 2016;273(5):1207–14. https://doi.org/10.1007/s00405-015-3851-y.
Peretti G, Piazza C, Berlucchi M, Cappiello J, Giudice M, Nicolai P. Pre- and intraoperative assessment of mid-cord erythroleukoplakias: a prospective study on 52 patients. Eur Arch Oto-Rhino-Laryngol. 2003;260(10):525–8. https://doi.org/10.1007/s00405-003-0584-0.
Mora F, Carta F, Missale F, et al. Laryngeal mid-cord erythroleukoplakias: how to modulate the transoral co2 laser excisional biopsy. Cancers (Basel). 2020;12(8):1–10. https://doi.org/10.3390/cancers12082165.
Peretti G, Cappiello J, Nicolai P, Smussi C, Antonelli AR. Endoscopic laser excisional biopsy for selected glottic carcinomas. Laryngoscope. 1994;104(10):1276–9. https://doi.org/10.1288/00005537-199410000-00017.
Hamzany Y, Shoffel-Havakuk H, Devons-Sberro S, Shteinberg S, Yaniv D, Mizrachi A. Single stage transoral laser microsurgery for early glottic cancer. Front Oncol. 2018;8(AUG):1–8. https://doi.org/10.3389/fonc.2018.00298.
Pittore B, Ismail-Koch H, Davis A, et al. Thyroarytenoid muscle invasion in T1 glottic carcinoma. Eur Arch Oto-Rhino-Laryngol. 2009;266(11):1787–91. https://doi.org/10.1007/s00405-009-0929-4.
Chiesa-Estomba CM, Ravanelli M, Farina D, et al. Imaging checklist for preoperative evaluation of laryngeal tumors to be treated by transoral microsurgery: guidelines from the European laryngological society. Eur Arch Oto-Rhino-Laryngol. 2020;277(6):1707–14. https://doi.org/10.1007/s00405-020-05869-0.
Sanabria A, Shah JP, Medina JE, et al. Incidence of occult lymph node metastasis in primary larynx squamous cell carcinoma, by subsite, t classification and neck level: a systematic review. Cancers (Basel). 2020;12(4) https://doi.org/10.3390/cancers12041059.
Piazza C, Mangili S, Del Bon F, et al. Preoperative clinical predictors of difficult laryngeal exposure for microlaryngoscopy: the laryngoscore. Laryngoscope. 2014;124(11):2561–7. https://doi.org/10.1002/lary.24803.
Piazza C, Paderno A, Grazioli P, et al. Laryngeal exposure and margin status in glottic cancer treated by transoral laser microsurgery. Laryngoscope. 2018;128(5):1146–51. https://doi.org/10.1002/lary.26861.
Incandela F, Paderno A, Missale F, et al. Glottic exposure for transoral laser microsurgery: proposal of a mini-version of the laryngoscore. Laryngoscope. 2019;129(7):1617–22. https://doi.org/10.1002/lary.27525.
Mora F, Missale F, Incandela F, et al. High frequency jet ventilation during transoral laser microsurgery for Tis-T2 laryngeal cancer. Front Oncol. 2017;7(NOV):1–5. https://doi.org/10.3389/fonc.2017.00282.
Remacle M, Eckel HE, Antonelli A, et al. Endoscopic cordectomy. A proposal for a classification by the Working Committee, European Laryngological Society. Eur Arch Oto-Rhino-Laryngol. 2000;257(4):227–31. https://doi.org/10.1007/s004050050228.
Remacle M, Van Haverbeke C, Eckel H, et al. Proposal for revision of the European Laryngological Society classification of endoscopic cordectomies. Eur Arch Oto-Rhino-Laryngol. 2007;264(5):499–504. https://doi.org/10.1007/s00405-007-0279-z.
Rudert HH, Werner JA, Höft S. Transoral carbon dioxide laser resection of supraglottic carcinoma. Ann Otol Rhinol Laryngol. 1999;108(9 I):819–27. https://doi.org/10.1177/000348949910800901.
Canis M, Martin A, Ihler F, et al. Results of transoral laser microsurgery for supraglottic carcinoma in 277 patients. Eur Arch Oto-Rhino-Laryngol. 2013;270(8):2315–26. https://doi.org/10.1007/s00405-012-2327-6.
Piazza C, Barbieri D, Del Bon F, et al. Functional outcomes after different types of transoral supraglottic laryngectomy. In: Laryngoscope, vol. 126. John Wiley and Sons Inc.; 2016. p. 1131–5. https://doi.org/10.1002/lary.25562.
Vilaseca-González I, Bernal-Sprekelsen M, Blanch-Alejandro JL, Moragas-Lluis M. Complications in transoral CO2 laser surgery for carcinoma of the larynx and hypopharynx. Head Neck. 2003;25(5):382–8. https://doi.org/10.1002/hed.10207.
Remacle M, Hantzakos A, Eckel H, et al. Endoscopic supraglottic laryngectomy: a proposal for a classification by the working committee on nomenclature, Eur Laryngological Society. Eur Arch Oto-Rhino-Laryngol. 2009;266(7):993–8. https://doi.org/10.1007/s00405-008-0901-8.
Mendelsohn AH, Remacle MJ. Vocal fold cancer transoral laser microsurgery following European Laryngological Society laser cordectomy classification. Front Oncol. 2018;8(JUN):1–8. https://doi.org/10.3389/fonc.2018.00231.
Marchi F, Piazza C, Ravanelli M, et al. Role of imaging in the follow-up of T2–T3 glottic cancer treated by transoral laser microsurgery. Eur Arch Oto-Rhino-Laryngol. 2017;274(10):3679–86. https://doi.org/10.1007/s00405-017-4642-4.
Simo R, Bradley P, Chevalier D, et al. European Laryngological Society: ELS recommendations for the follow-up of patients treated for laryngeal cancer. Eur Arch Oto-Rhino-Laryngol. 2014;271(9):2469–79. https://doi.org/10.1007/s00405-014-2966-x.
Eckel HE. Local recurrences following transoral laser surgery for early glottic carcinoma: frequency, management, and outcome. Ann Otol Rhinol Laryngol. 2001;110(1):7–15. https://doi.org/10.1177/000348940111000102.
Cesare, Piazza Alberto, Paderno Francesca, Del Bon Davide, Lancini Milena, Fior Giulia, Berretti Paolo, Bosio Alberto, Deganello Giorgio, Peretti. Long-term Oncologic Outcomes of 1188 Tis-T2 Glottic Cancers Treated by Transoral Laser Microsurgery. Otolaryngology–Head and Neck Surgery. 2021;165(2):321–28. https://doi.org/10.1177/0194599820983727.
Hartl DM, Ferlito A, Brasnu DF, et al. Evidence-based review of treatment options for patients with glottic cancer. Head Neck. 2011;33(11):1638–48. https://doi.org/10.1002/hed.21528.
Abdurehim Y, Hua Z, Yasin Y, Xukurhan A, Imam I, Yuqin F. Transoral laser surgery versus radiotherapy: systematic review and meta-analysis for treatment options of T1a glottic cancer. Head Neck. 2012;34(1):23–33. https://doi.org/10.1002/hed.21686.
Higgins KM, Shah MD, Ogaick MJ, Enepekides D. Treatment of early-stage glottic cancer: meta-analysis comparison of laser excision versus radiotherapy. J Otolaryngol Head Neck Surg. 2009;38(6):603–12. https://doi.org/10.2310/7070.2009.080235.
Yoo J, Lacchetti C, Hammond JA, Gilbert RW. Role of endolaryngeal surgery (with or without laser) versus radiotherapy in the management of early (T1) glottic cancer: a systematic review. Head Neck. 2014;36(12):1807–19. https://doi.org/10.1002/hed.23504.
Giorgio, Peretti Cesare, Piazza Mohssen, Ansarin Luigi, De Benedetto Daniela, Cocco Augusto, Cattaneo Piero, Nicolai Fausto, Chiesa. Transoral CO2 laser microsurgery for Tis-T3 supraglottic squamous cell carcinomas. European Archives of Oto-Rhino-Laryngology. 2010;267(11):1735–42. https://doi.org/10.1007/s00405-010-1284-1.
Motta G, Esposito E, Testa D, Iovine R, Motta S. CO2 laser treatment of supraglottic cancer. Head Neck. 2004;26(5):442–6. https://doi.org/10.1002/hed.10395.
Patel KB, Nichols AC, Fung K, Yoo J, MacNeil SD. Treatment of early stage Supraglottic squamous cell carcinoma: meta-analysis comparing primary surgery versus primary radiotherapy. J Otolaryngol Head Neck Surg. 2018;47(1):1–8. https://doi.org/10.1186/s40463-018-0262-2.
Cabanillas R, Rodrigo JP, Llorente JL, Suárez C. Oncologic outcomes of transoral laser surgery of supraglottic carcinoma compared with a transcervical approach. Head Neck. 2008;30(6):750–5. https://doi.org/10.1002/hed.20778.
Fiz I, Koelmel JC, Sittel C. Nature and role of surgical margins in transoral laser microsurgery for early and intermediate glottic cancer. Curr Opin Otolaryngol Head Neck Surg. 2018;26(2):78–83. https://doi.org/10.1097/MOO.0000000000000446.
Canis M, Ihler F, Martin A, Matthias C, Steiner W. Transoral laser microsurgery for T1a glottic cancer: review of 404 cases. Head Neck. 2015;37(6):889–95. https://doi.org/10.1002/hed.23688.
Jumaily M, Faraji F, Osazuwa-Peters N, Walker RJ, Ward GM. Prognostic significance of surgical margins after transoral laser microsurgery for early-stage glottic squamous cell carcinoma. Oral Oncol. 2019;97:105–11. https://doi.org/10.1016/j.oraloncology.2019.08.005.
Fiz I, Mazzola F, Fiz F, et al. Impact of close and positive margins in transoral laser microsurgery for TIS-T2 glottic cancer. Front Oncol. 2017;7(OCT):1–9. https://doi.org/10.3389/fonc.2017.00245.
Remacle M, Matar N, Delos M, Nollevaux MC, Jamart J, Lawson G. Is frozen section reliable in transoral CO2 laser-assisted cordectomies? Eur Arch Oto-Rhino-Laryngol. 2010;267(3):397–400. https://doi.org/10.1007/s00405-009-1101-x.
Piazza C, Filauro M, Paderno A, et al. Three-dimensional map of isoprognostic zones in glottic cancer treated by transoral laser microsurgery as a unimodal treatment strategy. Front Oncol. 2018;8(MAY):1–7. https://doi.org/10.3389/fonc.2018.00175.
Hendriksma M, Sjögren EV. Involvement of the anterior commissure in early glottic cancer (tis-T2): a review of the literature. Cancers (Basel). 2019;11(9):1–15. https://doi.org/10.3390/cancers11091234.
Vilaseca I, Nogués-Sabaté A, Avilés-Jurado FX, et al. Factors of local recurrence and organ preservation with transoral laser microsurgery in laryngeal carcinomas; CHAID decision-tree analysis. Head Neck. 2019;41(3):756–64. https://doi.org/10.1002/hed.25422.
Carta F, Bandino F, Olla AM, Chuchueva N, Gerosa C, Puxeddu R. Prognostic value of age, subglottic, and anterior commissure involvement for early glottic carcinoma treated with CO2 laser transoral microsurgery: a retrospective, single-center cohort study of 261 patients. Eur Arch Oto-Rhino-Laryngol. 2018;275(5):1199–210. https://doi.org/10.1007/s00405-018-4890-y.
Peretti G, Piazza C, Mora F, Garofolo S, Guastini L. Reasonable limits for transoral laser microsurgery in laryngeal cancer. Curr Opin Otolaryngol Head Neck Surg. 2016;24(2):135–9. https://doi.org/10.1097/MOO.0000000000000240.
Blanch JL, Vilaseca I, Caballero M, Moragas M, Berenguer J, Bernal-Sprekelsen M. Outcome of transoral laser microsurgery for T2-T3 tumors growing in the laryngeal anterior commissure. Head Neck. 2011;33(9):1252–9. https://doi.org/10.1002/hed.21605.
Allegra E, Saita V, Azzolina A, et al. Impact of the anterior commissure involvement on the survival of early glottic cancer treated with cricohyoidoepiglottopexy: a retrospective study. Cancer Manag Res. 2018;10:5553–8. https://doi.org/10.2147/CMAR.S182854.
Del Bon F, Piazza C, Lancini D, et al. Open partial horizontal laryngectomies for T3–T4 laryngeal cancer: Prognostic impact of anterior vs. posterior laryngeal compartmentalization. Cancers (Basel). 2019;11(3) https://doi.org/10.3390/cancers11030289.
Hirano M, Kurita S, Matsuoka H, Tateishi M. Vocal fold fixation in laryngeal carcinomas. Acta Otolaryngol. 1991;111(2):449–54. https://doi.org/10.3109/00016489109137418.
Hendriksma M, Heijnen BJ, Sjögren EV. Oncologic and functional outcomes of patients treated with transoral CO 2 laser microsurgery or radiotherapy for T2 glottic carcinoma: a systematic review of the literature. Curr Opin Otolaryngol Head Neck Surg. 2018;26(2):84–93. https://doi.org/10.1097/MOO.0000000000000438.
Lionello M, Bertolin A, Nardello E, et al. Could the infiltration of the thyroarytenoid muscle define the pT2 glottic carcinoma? Head Neck. 2019;41(10):3639–46. https://doi.org/10.1002/hed.25893.
Bron LP, Soldati D, Zouhair A, et al. Treatment of early stage squamous-cell carcinoma of the glottic larynx: endoscopic surgery or cricohyoidoepiglottopexy versus radiotherapy. Head Neck. 2001;23(10):823–9. https://doi.org/10.1002/hed.1120.
Elisabeth, Sjogren Martine, Hendriksma Cesare, Piazza Dana M., Hartl Carlos, Suarez Oded, Cohen Remco, de Bree Miquel, Quer Vincent Vander, Poorten Juan Pablo, Rodrigo Francisco, Civantos Eric, Genden Luiz P., Kowalski Antti, Makitie Ashok, Shaha Robert P., Takes Alvaro, Sanabria Orlando, Guntinas-Lichius Alessandra, Rinaldo Alfio, Ferlito. Voice Outcome After Carbon Dioxide Transoral Laser Microsurgery for Glottic Cancer According to the European Laryngological Society Classification of Cordectomy Types – A Systematic Review. Journal of Voice. 2022: S0892199722000698. https://doi.org/10.1016/j.jvoice.2022.03.003.
Peretti G, Mensi MC, Piazza C, Rossini M, Balzanelli C, Antonelli AR. Preoperative and postoperative voice in Tis-T1 glottic cancer treated by endoscopic cordectomy: an additional issue for patient counseling. Ann Otol Rhinol Laryngol. 2003;112(9 I):759–63. https://doi.org/10.1177/000348940311200903.
Peretti G, Piazza C, Cantarella G, Balzanelli C, Nicolai P. Vocal outcome after endoscopic cordectomies for tis and T1 glottic carcinomas. Ann Otol Rhinol Laryngol. 2003;112(2):174–9. https://doi.org/10.1177/000348940311200212.
Peretti G, Piazza C, Cattaneo A, De Benedetto L, Martin E, Nicolai P. Comparison of functional outcomes after endoscopic versus open-neck supraglottic laryngectomies. Ann Otol Rhinol Laryngol. 2006;115(11):827–32. https://doi.org/10.1177/000348940611501106.
Davis RK, Kriskovich MD, Buntin CS, Galloway EB, Jepsen MC. Endoscopic supraglottic laryngectomy with postoperative irradiation. Ann Otol Rhinol Laryngol. 2004;113(2):132–8. https://doi.org/10.1177/000348940411300210.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Piazza, C., Eckel, H.E., Remacle, M., Dela Cruz, P., Peretti, G., Sampieri, C. (2022). Transoral Approach for Early Laryngeal Cancers. In: Remacle, M., Eckel, H.E. (eds) Textbook of Surgery of Larynx and Trachea. Springer, Cham. https://doi.org/10.1007/978-3-031-09621-1_24
Download citation
DOI: https://doi.org/10.1007/978-3-031-09621-1_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-09620-4
Online ISBN: 978-3-031-09621-1
eBook Packages: MedicineMedicine (R0)