Abstract
Office-based procedures in laryngology are emerging in the last years and keep on increasing not only due to better imaging and instrumentation. Besides the basic interventions like injections and biopsies, laser procedures are getting more and more practicable and precise and sometimes even may be first-line indications for non-sedated patients for an in-office procedure. Transnasal flexible surgery is taking over transoral approaches, although transoral interventions still play an important role in office-based interventions. Still, there are obstacles in establishing a state-of-the-art office surgery unit with the latest high-resolution endoscopes, videostroboscopy, and lasers, where high initial setup costs are significant to purchase instruments, solving associated problems of cleaning, decontamination, disinfection, and reprocessing of endoscopes and instruments. Finally, dealing with appropriate handling of corona pandemic-related issues of personal protective equipment, aerosol-generating procedures, and the like is of utmost importance. However, this all did not stop the advancement of office-based procedures. More and more diagnostic examinations and therapeutic treatments are done in the office, since they are lowering risks for the patients, decrease costs, and improve comfort and convenience in manifold cases where highest precision like in microlaryngoscopy is not mandatory. A well-defined, certified future training for ENT colleagues is highly desirable and would help further use of office-based procedures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Office-based interventions
- In-office procedures
- Corona pandemic
- Personal protective equipment
- Powered air purifying respirator
- Vocal fold injection
- Vocal fold biopsy
- Blue laser
- KTP laser
- Dysphonia
- Dysphagia
- Transnasal esophagoscopy
- Transnasal tracheoscopy
-
Office-based diagnostic examinations and interventions lower risks for patients, decrease costs, and improve comfort and convenience in manifold cases where highest precision like in microlaryngoscopy is not mandatory.
-
Injections, biopsies, and laser procedures become more frequent as the latest endoscopes provide high-resolution imaging and further information from spectral imaging features.
-
Transnasal flexible surgery is taking over transoral approaches, although transoral interventions still play an important role in office-based interventions.
-
Unsedated transnasal esophagoscopy (TNE) and transnasal tracheoscopy (TNT) extend the endoscopic spectrum for diagnosis and treatment.
12.1 Introduction
Indirect laryngeal interventions are known since far more than 130 years. However, there is a renaissance of indirect, office-based interventions noticeable in the last time [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Within the last 10 years, office-based procedures have boomed worldwide. There are many reasons for this development. Imaging has improved with new camera systems like chip-on-tip technology, and refined image resolution with high-definition (HD) cameras is available. Flexible endoscopes are nowadays thinner, enabling easy nasal passage without too much of a limitation in image quality.
Many patients appreciate rapid interventions using topical anesthesia, which also is encouraging for laryngologists when surgery can be performed in shorter time, including faster patient-to-patient turnover time. For voice surgery, it cannot be stressed enough how advantageous the immediate testing of voice outcome in the awake patient is. Furthermore, it should not be forgotten that general anesthesia-related safety concerns can be bypassed with topical anesthesia. Health insurance companies indirectly encourage laryngologists by monetary incentives to avoid general anesthesia surgery and to use more office-based interventions within ambulatory settings.
The aim of this chapter is to briefly sketch the spectrum of office-based procedures, keeping in mind that only a few procedures can be covered in more detail. It should be mentioned at this point that all statements made in this chapter represent the authors’ opinion and are based on 25 years’ experience in performing indirect surgery at various clinics.
12.2 Possible Interventions in Office-Based Phonosurgery
Laryngeal procedures through suspension microlaryngoscopic techniques are referred to as “direct” techniques. “Direct” indicates that the optical axis of the microscope is in a direct line when visualizing the larynx. Thus, the term “indirect” refers to all other ways of imaging of the larynx (mirrors, angled rigid endoscopes, flexible endoscopes with glass fibers, or chip-on-tip cameras). In a generalized sense, “indirect” is also taken as a synonym for office-based or in-office procedures.
12.2.1 Biopsy/Excision
The classic indirect intervention in laryngology is taking a biopsy from an endolaryngeal site via transoral access. The “workhorse” instrument for this is the cupped forceps, which is turned to one side (left/right or rotatable). When more than a biopsy is taken and a lesion is removed completely, the surgery is called excision. With good surgical skills, excisions, for instance, of nodules and polyps are doable in indirect transoral techniques. The abovementioned procedures can also be performed with instruments passed through the channel of a flexible, transnasally routed endoscope, although this approach is different in using smaller instruments (a disadvantage), but accessibility might be easier (an advantage).
Dissections are not a domain of indirect phonosurgery, since most indirect office-based interventions are one-handed instrument procedures, making dissections almost impossible within this setting.
12.2.2 Injection
Injections are mostly used for intramuscular application of botulinum toxin, subepithelial steroid injection, hydrodissection of Reinke’s space, intralesional infiltration of cidofovir or bevacizumab in papilloma, etc. Injections can be performed through transoral, transnasal, and percutaneous approaches.
12.2.3 Augmentation
A rapidly emerging field is the injection augmentation with fillers for vocal fold medialization (syn. “injection laryngoplasty”). Different ways to insert the cannula can be chosen: (a) transorally, (b) transnasally, or (c) percutaneously via a transcartilaginous, cricothyroid, or thyrohyoid approach. No matter which approach is chosen for positioning the cannula tip into the vocal fold, it is a straightforward procedure making augmentation an immediately rewarding intervention. Explanation of injection laryngoplasty and associated issues cannot be presented comprehensively in this chapter.
12.2.4 Laser
Laser treatment within office-based surgery requires a set of prerequisites and additionally specific safety conditions. Nowadays, we essentially have two different laser techniques which take advantage of different tissue energy absorption properties.
First, tissue coagulation, carbonization, vaporization, and ablation, i.e., many kinds of tissue destruction, are possible with all fiber-guided lasers (e.g., CO2-, diode-, thulium-, and neodym-YAG lasers). With the introduction of hollow fibers as beam delivery system, the use of CO2 lasers may make this kind of office-based intervention even more feasible, since CO2 lasers are available at almost all ENT clinics worldwide.
Second, photoangiolytic lasers like pulse dye laser (PDL) and kalium-titanyl-phosphate (KTP) laser as well as the newer-generation blue laser (BL) are more and more popular for local therapy of selected laryngeal lesions. Papilloma, Reinke’s edema, polyps, contact granuloma, ectatic vessels, leukoplakia, dysplasia, and other lesions with a red or brown chromophore are a domain of these selective “photoangiolytic” lasers. In some cases, these photoangiolytic lasers are the first choice of treatment. Laser surgery can be performed through transoral, transnasal, and percutaneous approaches.
12.2.5 Arytenoid Mobility Test
Office-based assessment of arytenoid mobility is a very helpful diagnostic transoral procedure to exclude arytenoid dislocation, (sub)luxation, or fixation. With topical anesthesia and use of a transorally routed blunt cotton-coated probe, arytenoid mobility testing is a rapid, safe, and easy method for the differential diagnosis of arytenoid immobility. From our experience, passive mobility could be proven in almost all cases of endoscopically visualized arytenoid immobility—showing us that arytenoid (sub)luxation and joint fixation could be ruled out in the vast majority of cases and suggesting that recurrent nerve paresis and paralysis were most likely.
12.2.6 EMG
Laryngeal electromyography (LEMG) is a classic office-based procedure. However, LEMG is still an underestimated diagnostic method for laryngeal examination. Electrophysiologic examination of selected laryngeal muscles with precise needle positioning in awake patients is an indispensable diagnostic tool to assess neuromuscular laryngeal function. Trained skills for the exact placement of EMG needles and routine analysis of biosignals are mandatory for meaningful neuromuscular function testing. We recommend that it should become a routine method in all professional voice centers. LEMG needle positioning, for example, for botulinum toxin injections, may be combined with other endoscopic procedures such as transnasal percutaneous injections. LEMG can be performed through transoral and percutaneous approaches.
12.2.7 Varia
Within this chapter, we can only mention other surgery-related fields of laryngology like stroboscopy, videokymography, high-speed imaging, narrow-band imaging (NBI) illumination, transnasal tracheoscopy (TNT), transnasal esophagoscopy (TNE), etc. These techniques and procedures are of great importance and certainly play an important role in a laryngology department, where outpatient comprehensive assessment and office-based therapy are offered. The reader is kindly referred to the great body of literature for more information on these topics.
12.3 Setting
In awake patient surgery, the appropriate setting is of crucial importance. Since the patient knows that “an operation” is performed, anxiety, discomfort, and nervousness are quite frequent. Confidence and trust are essential, and reassurance must be mediated by all staff members, resulting in a high level of patient compliance and finally making the operation successful. The patient should feel well cared for at all steps of the operation (Fig. 12.1).
(a) Sketch of examination room. (b) Examination room with enough space for the patient, examiner, assistant, and nurse. Endoscope equipment and ENT instruments within reach of the surgeon and assistant. Light is dimmable. Monitor position permits the surgeon to observe the patient and view the screen. Assistant supports with anesthesia, instruments, and suctioning
12.3.1 Corona Virus and Protective Measures
The 2020 corona virus pandemic has changed a lot in terms of protective measures and equipment. Aerosol-generating procedures (AGPs), which include rigid laryngoscopies, but much more transnasal flexible endoscopies, are highly likely aerosol generating and increase the risks of infection for surgical staff. Furthermore, laser surgery of the larynx is definitely producing more aerosols when tissues are evaporated. Vegetative reactions such as coughing, throat clearing, as well as sneezing are accompanied with in-office procedures producing droplets and aerosols. Thus, they can jeopardize the surgeon when standing directly in front of the patient. Powered air purifying respirator (PAPR) usage or at least FFP2/3 (or N95) masks, gowns, and gloves are mandatory in potentially infectious patients. Adequate room ventilation is key to avoid infections due to increased room air aerosol concentration. In sum, surgeons and medical staff need to protect themselves with adequate personal protective equipment (PPE) according to regulations (Figs. 12.2 and 12.3).
12.3.2 Patient Position
For transoral operations, the patient is sitting in front of the surgeon. Patients are asked to hold their tongue with a gauze square. In transnasal and percutaneous operations, patients can sit, lean back in an angled position, or lie supine on the back.
12.3.3 One Surgeon or Two Surgeons?
Transoral surgery mostly means that there is one surgeon holding the endoscope with one hand and keeping the other hand for interventions. Transoral surgery is prototypical for one surgeon using one instrument. Transnasal and percutaneous operations mostly need two persons (surgeon and assistant). In these cases, the patient may be sitting or lying in an angled position or on a plinth in supine position, with one person on each side. Typically, the surgeon should focus on the surgical intervention itself. The assistant focuses on laryngeal imaging via flexible endoscopy. When transnasal laser operations are performed, the surgeon almost always needs an assistant.
12.3.4 Instrumentation
Special instruments are mandatory for each kind of approach, whether it is performed transorally or transnasally.
Transoral surgery requires curved instruments following the curvature of the upper airways. Preferably, instruments should be long enough for tall male patients with low larynx position, and rigidity of the intracorporal part of the instrument should be high enough to resist counterpressure from the tongue. In the authors’ opinion, angled, cupped forceps are the most useful instruments. Palpation, pinching-like and pointed tissue pull, gripping of larger tissue areas, and biopsing are possible with this one instrument. A curved, large-bore, hollow cannula for delivery of flexible needles (for injection) and routing of glass fibers (for laser operations) is also very valuable. A small number of customized instruments are available on the market nowadays.
Transnasal interventions need instruments that can be passed through an instrument channel of a flexible endoscope, limiting the maximum instrument diameter to the diameter of the instrument channel (mostly 2 mm). Alternatively, with two flexible endoscopes, subsequently two instruments can be utilized—enhancing the interventional options.
12.3.5 Combined Methods
Of course, theoretically any combination of transoral/transnasal visualization and instrument routing can be used. When combined techniques are used and transnasal and transoral passages are chosen, predominantly transnasal fibroscopic visualization is selected for monitoring the endolarynx, while the surgical instrument is routed transorally or percutaneously, providing more degrees of freedom for lateral instrument movements and furthermore allowing to pass thicker instruments into the larynx.
12.4 Medication and Anesthesia
12.4.1 Medication
Sedation is needed only very rarely. Sedation can be achieved by 3.5–7 mg midazolam per oral 2 h before operation. Anti-cough medication (e.g., 30 drops of codeine) has proven advisable for some patients. Antibiotics are not administered in most cases; steroids are given for patients with augmentation or major manipulation within the larynx (e.g., 100 mg prednisolone per oral after surgery and same dosage the day after surgery). For food and beverage intake prior to surgery, we consider 2 h fasting (nil per os - nothing by mouth) as sufficient. Some patients who were fasting for more than 2 h seemed to have a nervousness level that was disadvantageous for indirect surgery. Besides pharmacological anesthetization, sufficient “verbal anesthesia” with reassuring the patient during the entire procedure is of utmost importance for successful office-based larynx surgery (Fig. 12.4).
12.4.2 Monitoring
Vital signs are checked pre- and postoperatively in most cases: blood pressure, heart beat rate, and pulse oximetry. Throughout the entire surgery, a pulse oximeter monitors heart beat rate and oxygen saturation. Normally, up to 2 h of postoperative monitoring of vital signs is sufficient. According to the type of intervention, a postoperative laryngoscopic check is advisable to rule out complications. In cases of patient sedation (definitively when midazolam was administered), the monitoring may have to be extended from 1 up to 8 h (especially in elderly patients). National medical and legal aspects apply and may differ widely from country to country.
12.4.3 “Verbal” Anesthesia
Patients appointed to office-based surgery have a strong sensibility is better for all circumstances related to “their” surgery. It was already pointed out that confidence, trust, and reassurance must be accomplished. “Verbal anesthesia” in a trustworthy environment significantly comforts patients, reduces gag response, and helps to calm the patients down—making interventions of all kinds easier for the surgeon.
12.4.4 Intranasal Anesthesia
Lidocaine 4% topically instilled onto lower and/or middle turbinates is very effective (1–2 cc). In rare cases, nasal decongestants and packages with topical anesthesia are used (Fig. 12.5).
12.4.5 Intraoral Anesthesia
For transoral (and in parts also for transnasal) approaches, topical anesthesia is usually administered: under the tongue, bilaterally at faucial arches, base of tongue, posterior wall of mesopharynx, and lateral side of epiglottis. Lidocaine (2%, 4%, or even 10%) can be applied with spray, by dripping the anesthetic, or topically with a blunt, soaked cotton swab. The swab has the advantage of testing “touch sensitivity,” training the patient in getting acquainted to the new touch sensations during transoral operation and also predicting tolerance of further instrumental intervention. Tetracaine is also a very useful anesthetic. Some authors use cocaine, which is one of the most potent substances, for topical anesthesia. However, such drugs have drawbacks and can be avoided (Fig. 12.6).
12.4.6 Anesthesia of the Pharynx and Larynx
As soon as topical anesthesia is applied onto the surfaces of the oral cavity and mesopharynx, the surgeon should—without losing time—move on with the procedure and administer lidocaine into the pharynx and larynx. Spraying should be avoided because of (corona) protection purposes as it is an AGP. The supralarynx, false vocal folds, and vocal folds can be anesthetized transorally with a lidocaine-soaked cotton swab. Touching of surfaces with the swab is helpful in checking the effect of sufficient numbing. The easier a reflex is elicited, the more numbing is needed. As a rule of thumb, the more posterior the endolaryngeal regions (toward the arytenoids), the more likely a gag response is elicited. Caveat: Fixation of the cotton wadding covering the tip of the curved cotton holder instrument (the “swab”) must be checked by all means before intracorporal use, since slipping off of the cotton due to inappropriate fixation of the cotton would risk its aspiration.
For transnasally applied anesthesia, we prefer dripping lidocaine 4% directly into the endolarynx through the instrument channel or a small catheter while observing proper placement of the anesthetic. The patient is asked to produce a long gargle or to phonate so as to increase the contact time of the anesthetic in the endolarynx. Using this technique, we almost never need to apply topical anesthesia percutaneously.
Some colleagues prefer inhaled topical anesthesia, and some have the patients mouthwash with lidocaine for additional numbing. Subglottic and tracheal interventions require adequate numbing that can be achieved by flexible endoscopy (see above) or with percutaneous intraluminal injection of the anesthetic through the cricothyroid or thyrohyoid membrane.
12.5 Complications and Failures
In the past 30 years of performing office-based procedures, we have not encountered any serious complication. In the very rare cases of laryngospasm, which may occur, e.g., when too much lidocaine is suddenly applied in large amounts into the larynx, we interrupt the procedure and ask to cough effortfully, to swallow all secretions, and to breathe through the nose while closing the mouth. Although this last maneuver sounds paradox, it is clinical experience that transnasal breathing is a very good trigger for vocal fold abduction and results in widening the glottis. Of course, there are other causes for gag response or laryngospasm, e.g., when the mucosa wasn’t anesthetized sufficiently or an instrument touches the mucosa too forcefully. This can easily happen in the posterior part of the larynx and anywhere at the arytenoid hump—a typical gag-triggering response area with high touch sensitivity.
In general, good topical anesthesia of the endolarynx should lead to sufficient numbing in more than 80% of cases. This anesthesia condition can be achieved in some patients in 2–3 min; in others, it takes 10 or more minutes. Approximately 5–10% of patients will not “allow” sufficient time or access for a complete surgery due to early onset of gagging, repetitive swallowing, and coughing. However, there are a habituation effect and a “learning curve” for most patients. Therefore, if a procedure doesn’t work because of early onset of gagging, the same procedure might work at a second trial. Only about 5% of patients are by no means laryngeally accessible for indirect surgery. A last chance to get access into the larynx in cases with continuing gag response is to additionally infiltrate an anesthetic next to the interior branch of the superior laryngeal nerve (iSLN) via transcutaneous infiltration nerve block (e.g., lidocaine with epinephrine 1%) in the region of the inferior part of the thyrohyoid membrane. This injection is not as easily performed as it sounds, because precise positioning of injection in the desired region may be quite difficult in patients with thicker necks.
12.6 Transoral Surgery
The transoral technique is the oldest approach to the larynx and was used since more than 140 years. Before performing the intervention, one should always touch the larynx with a lidocaine-soaked cotton swab during anesthesia and carefully “map” the individual gag trigger zones for response levels. The lateral laryngeal approach, i.e., passing the instrument over the aryepiglottic fold and avoiding touching of the tip of the epiglottis as well as the arytenoid hump, makes this pathway most favorable. In some cases, midline passage over the median part of the tongue base and sliding over the tip of the epiglottis is easier than the lateral laryngeal approach. However, in the authors’ opinion, the lateral pathway is the first choice (Fig. 12.7).
Whatever is planned for surgery, it should be performed in a speedy, but not rushed, manner. Fortunately, in many patients, pathologic lesions are located at the midmembranous part of the vocal folds, which is—luckily!—not very sensitive to manipulation, making interventions easy when the most sensitive gag response-triggering zones of the supralarynx are passed by the instrument.
12.6.1 Palpation-Biopsy-Excision
Many interventions can be performed with an angled cupped forceps. The operation is started with the cotton swab, which anticipates all movements that will follow during intervention. This imitation of the movements gives a good feedback to the patient (immediate tolerance learning curve!) and also to the surgeon on how the procedure might be tolerated. Once the basic movements are tolerated, the cotton swab is laid aside, and the instrument is introduced in the same manner and position as the swab. When using cupped forceps, they should be introduced in closed position, avoiding scratching of mucosa in cases of sudden, unexpected movements. Again, brief palpation of the vocal folds, the lesion, and adjacent tissue immediately before grasping gives an impression of how much the following movements will be tolerated.
Superficial lesions of the vocal folds are checked for pliability in an inferior-superior (up and down) and posterior-anterior (back and forth) palpation movement.
In patients with a soft vocal fold polyp, we suggest to proceed as follows: First, take a gentle grasp of the lesion by not closing the forceps completely. Then make two predetermined epithelial notches at the anterior and posterior margins of the lesion by pinching and tearing the marginal epithelium carefully. These two epithelial discontinuities (notches) will help to avoid inadvertent de-epithelialization of adjacent and healthy mucosa by undesired stripping during instrumental pull on the body of the lesion. Second, grasp the polyp with a delicate squeeze, let loose, and check the new tissue indentation marks for how much tissue you would have excised if you would have punched it out. If your grasp was placed correctly, continue with the third step, i.e., grasp the entire polyp and remove it with the identical tissue grip. The pulling direction of the instrument is preferably from anterior to posterior, and the vector is almost in parallel with the longitudinal axis of the vocal fold. Every medial pull is unfavorable, because with medial pull unpredictable tear and stripping of adjacent, normal epithelium would be very likely. The anterior-to-posterior pull will tear the epithelium at the anterior notch and will stop at the posterior notch. Finally, straighten edge for epithelial “corners” at the notches, the so-called dog’s ears, by grasping with the tip of the cupped forceps (Figs. 12.8 and 12.9).
Hemorrhage by capillary bleeding can follow—and it shouldn’t frighten the surgeon when some drops of blood spread intralaryngeally. The surgeon shouldn’t worry about the red-colored endolarynx when a few blood drops are spread by swallowing or throat clear, since blood is very effective in coloring saliva. The authors have never experienced a severe bleeding after many hundreds of interventions. After a short soft (!) throat clear or wiping of the vocal fold with the closed forceps (still containing the tissue specimen) directly after the excision while the instrument is in the larynx, the surgeon will get an occasion to visualize the vocal fold and decide whether it is straight or if additional trimming is needed. For the assessment of voice function, it would be most favorable to immediately switch over and use videolaryngostroboscopy to assess vibratory behavior and phonation, with the endoscope and instrument still in place, before lamina propria swelling begins.
12.6.2 Injection and Augmentation
Again, as with indirect transoral excisions, the patient is transorally anesthetized with a cotton swab soaked with local anesthetic (see above). Wherever the injection is planned to be placed, it may be advisable to perform several pushing maneuvers onto the tissue with the blunt swab and inform the patient that this is what it feels like when the cannula is going to be inserted in a couple of seconds. Once the movements are tolerated, the cotton swab is laid aside, and the instrument with the curved cannula is taken. Make sure that, before you inject, the injectable is already advanced through the cannula lumen (so-called priming)—cannulas occasionally can have a lumen up to almost 0.5 cc, which means that before priming there is air instead of medication or implant inside the lumen. Also, a big lumen is a significant source of expensive implant loss. The curved cannula follows the same pathway as the swab. Advancement of the cannula requires visual control, avoiding pricking of the uvula, tonsils, tongue, epiglottis, and posterior oropharyngeal mucosa. In the beginning of insertion, the cannula is seen directly. As soon as the cannula passes the isthmus faucium, the cannula tip position may be visually controlled indirectly by rigid endoscopy. The injection itself can last up to 1 min, giving time for intracordal spread of the injectable. After withdrawal of the cannula, watch the injection site and check for bleeding or swelling.
Special points: Occasionally, the exact cannula tip position can only be found out during injection augmentation when watching the ballooning of the vocal fold. As a rule of thumb, the injection for augmentation should be interrupted when 0.2 cc do not show any effect of tissue augmentation (no matter which injection technique was chosen). Videostroboscopy with the optics in place can help in making decisions if additional augmentation is needed. In vocal fold augmentation, slight overcorrection is almost always advisable because of later filler distribution within the vocal fold. Depending on the implant material and technique used, overcorrection goes up to 50% (e.g., for some hyaluronic acid augmentations). In selected cases, molding of the vocal fold with a blunt instrument or with a cotton swab can help to mold the vocal fold in a favorable manner, mostly by straightening out a rounded, convex fold surface by soft massaging. Because vocal fold augmentation encompasses many special aspects, this topic actually needs to be covered in a separate chapter.
Botulinum toxin injections for the treatment of spasmodic dysphonia of adductor type (ADSD) are placed into the thyroarytenoid muscle or lateral cricoarytenoid muscle, i.e., always lateral to Reinke’s space, or into the posterior cricoarytenoid muscle. Injections may also be advisable into the ventricular folds. Botulinum toxin injections can also alleviate vocal tremor; therefore, several intra- and extralaryngeal muscles may be targeted.
Steroids may be injected in patients with vocal fold scars, Reinke’s edema, nodules, chronic cough, or granuloma. Intralesional steroid injections (ISI) may also help when endolaryngeal scars at any region are present. Choice of pharmacological formulation of the steroid depends on surgeon’s choice, for instance, if long-lasting drugs are desired (crystalline suspension—triamcinolone) or short-term (water-based—dexamethasone) solutions. We very often use triamcinolone 10%, sometimes triamcinolone 40%.
Hematoma and bleeding may follow injections, but need not. Even in patients under anticoagulation therapy, bleeding after lateral paraglottic injection of augmentation material (hyaluronic acid, calcium hydroxylapatite) is mostly limited to some drops of blood.
12.6.3 Laser Surgery
Transoral glass fiber-guided laser application is a very favorable procedure when combined with rigid transoral or transnasal laryngoscopy. The transoral rigid laryngoscopy with a 70° video endoscope allows to take advantage of separation of optical axis and instrument positioning. It is one more—and significantly advantageous—degree of freedom when compared with the transnasal technique.
Nowadays, papilloma, edema, polyps, and many more lesions can be treated with photoangiolytic laser surgery (blue laser, KTP laser, PDL).
12.7 Transnasal Surgery
Almost all abovementioned transoral techniques can also be performed through a transnasal approach. However, while transoral techniques separate visualization and surgical instrument handling, this is not the case in transnasal (single) endoscope techniques. When a flexible endoscope with instrument channel is used, it must be kept in mind that endoscope movements (for better visualization of the endolarynx) inevitably result in movements of the instrument that is routed through the instrument channel. If a flexible endoscope with instrument channel is not available, a channeled single-use sheath can be used to cover the endoscope and deliver an instrument through the paralleled channel adjacent to the endoscope. Although it sounds that transnasal approaches are more disadvantageous, the advantages outweigh. Transnasal flexible procedures are far more tolerable to most patients. Some surgeon colleagues prefer that imaging and instrument movement is actually coupled in channeled fibroscopic approaches. Furthermore, the possibility of getting very close to target by dipping and rotating the flexible endoscope gives easier access to the inferior aspect of the vocal folds and also for Morgagni’s ventricle.
Most transnasal procedures need an assistant. As soon as two persons work together, coordinated and concerted actions have to be trained before a harmonized intervention can be performed.
An exemplary team approach was realized by Ricci-Maccharini, de Rossi, and Borragan. These colleagues pushed their office-based, transnasal intervention techniques to a very high level of expertise (even when not all interventions are true in-office procedures because some of them require analgo-sedation, which is provided by an anesthesiologist in the operating room).
12.7.1 Palpation-Biopsy-Excision
Before surgery, the surgeon might want to palpate the targeted tissues. One can touch the surface with an instrument for assessing the pliability and softness (or rigidity) of the tissue. We mostly use the catheter of the (still shielded) injection cannula routed through the working channel, or we palpate with the closed biopsy forceps. When patients tolerate endolaryngeal interventions, one can also use the stiffness of a 400 μm laser glass fiber for superficial palpation. These palpatory procedures are also recommended before surgery to check whether the patient tolerates an intervention. Indentation and shearing gives a lot of information of the covering tissues, definitely useful on the surfaces of the vocal folds. Sometimes we also use this technique to search for a sulcus vocalis, to move pediculated mass lesions, and to scratch off coagulated tissues during laser procedures (Figs. 12.10 and 12.11).
For a biopsy or excision, it is important to be able to rotate the forceps within the working channel until you have the two cups in an advantageous angle for the tissue to be grasped. Palpation in between with closed forceps is also possible. As the next step, one can hold the tissue with very little closing pressure and move it to get more information, e.g., pedunculated polyp or not (communicate this with the assistant). After excision, some bleeding may follow. Sometimes, the tearing of the tissue is easier when one combines pulling and endoscope rotation. The bleeding will of course usually stop by itself, but it disturbs the visibility of the surfaces. Depending on how big the specimen is after excision, one can remove only the forceps through the channel or, in most cases better, the endoscope with the specimen within the forceps’ cups but still outside of the working channel so to not shear off parts of the specimen.
12.7.2 Injection and Augmentation Laryngoplasty
An easy way of injecting fluids with very low viscosity (steroids, botulinum toxin, cidofovir, bevacizumab, etc.) into the vocal folds is the transnasal technique through the working channel. We prefer to use a long, flexible, single-use catheter with a 25 G cannula. The cannula is sheathed and can be advanced externally through the handpiece by the assistant. For all injections, one therefore needs an assistant.
A typical indication is the injection of botulinum toxin for treating adductor-type spasmodic dysphonia. Compared with the percutaneous approach, one has the advantage of getting access to the false vocal folds as well—which shows good results with less side effects. Another common indication is the injection of steroids for treating scars on the surface, for instance, of the vocal folds. The injection must be done with precision to administer a few drops exactly into the superficial lamina propria.
Paraglottic injection augmentation of a vocal fold is more challenging. Of course, when the patient’s preference is to receive a rapid treatment in the office once the diagnosis of, say, unilateral vocal fold paresis/paralysis is made and general anesthesia should be avoided, this is a significant advantage. Furthermore, there is a big advantage in monitoring the voice during the procedure as well as seeing how the filler medializes the vocal fold with normal muscle tone, when compared to surgery in general anesthesia. One of the drawbacks is that vocal folds cannot be easily molded once the filler is in the paraglottic space. Injecting a filler through the catheter routed through a flexible scope is probably not feasible because of the viscosity of most fillers. However, transoral or transnasal laryngoscopy combined with percutaneous augmentation is easier (Figs. 12.12, 12.13, and 12.14).
12.7.3 Laser Surgery
Glass fiber-guided laser application via a transnasal approach is an easily performed procedure. With a 400 μm glass fiber routed through the working channel, one can approach many areas within the hypopharynx and larynx. In combination with the dipping maneuver and rotation laryngoscopy, the surgeon has access also to Morgagni’s ventricle and the inferior aspect of the vocal fold. With the use of a four-way direction flexible fiberscope tip, maneuvering of the glass fiber is even more facilitated. With sufficient anesthesia, procedures can be performed up to 30 min duration. Skilled handling of the endoscope with the laser glass fiber and appropriate choice of laser settings are mandatory and should be trained in endoscopy courses. Laser safety measures are extremely important. Special attention should be addressed for the correct selection of appropriate laser light filtering eye wear. Indications for laser surgery can be manifold from debulking of masses (granuloma, cysts, polyps, papilloma, edema) down to small lesions like hemangioma and vascular ectasias. The debulking laser procedures can be done with all fiber-guided lasers. Biofilm (“photodisinfection”), leukoplakia, dysplasia, and small cancers can also be treated in the office, and preferably photoangiolytic lasers are chosen for these indications (e.g., PDL, KTP, BL).
Technically, laser in-office procedures are performed by a surgeon with an assistant. Support is needed for suctioning, changing of laser settings, and activating and deactivating the laser and since the corona pandemic changed hygiene requirements making donning and doffing more cumbersome—so any assistance is very helpful (Figs. 12.15, 12.16, 12.17, and 12.18).
12.8 Percutaneous Procedures
The percutaneous approach is defined by the route of instrument passed through the skin of the anterior neck. It is combined with laryngoscopy, e.g., in cases of augmentation, or without endolaryngeal visualization, e.g., for botulinum toxin injections. Laser procedures can also be pone via this approach, but is only performed in selected cases.
12.8.1 Injections
Mostly, injection cannulas and laryngeal EMG needles are passed percutaneously. Three main pathways can be chosen: trans-cricothyroid, trans-cartilage (thyroid ala), and trans-thyrohyoid. The most easy way is the cricothyroid technique for passing an EMG needle, e.g., a 25 G botulinum toxin cannula, or a 20–25 G and >30-mm-long cannula for vocal fold augmentation. The posterior cricoarytenoid muscle can be reached by a median trans-cricothyroid membrane and transcartilaginous (cricoid) approach or from lateral behind the larynx. All this is preferably done in combination with LEMG (Fig. 12.19).
To bypass a cough reflex, the needle/cannula may be inserted ipsilaterally and approx. 5 mm paramedian, avoiding intraluminal passage. It is the endolaryngeal epithelium that is most sensitive to all kinds of intervention by eliciting a sudden cough, swallow reflex, or gag response. It may help to apply topical anesthesia, sprayed onto the mucosa through the upper airways, or intraluminally applied onto the laryngeal mucosa through a percutaneously and medially inserted cannula.
12.8.2 Vocal Fold Medialization
The percutaneous approach for vocal fold medialization is a rewarding procedure in office-based phonosurgery. In principle, the augmentation procedure resembles the transoral technique. But in percutaneous augmentation, the visualization is provided by an assistant handling a flexible endoscope, while injections are performed by the surgeon through the abovementioned percutaneous approaches. The authors prefer having the patient supine with the head overextended, but the patient can also sit. The cricothyroid approach with a 40-mm-long cannula (20–25 G), angled up 45°, is good for (mostly higher) female larynges. Thinner needles (e.g., 25 G) may be too flexible for some male patients. However, we now favor the trans-thyrohyoid approach with a 23 G 60 mm cannula, sometimes additionally bent, to better reach the vocal folds. This works in males and females; however, in low larynx positions, it is easier (mostly males). Monitoring of correct cannula placement is ensured via transnasal endoscopy (Fig. 12.20).
Percutaneous augmentation with calcium hydroxylapatite. Patient supine with head reclined. (a) Surgeon passes a 20 G needle through the cricothyroid membrane, controlling the effect of augmentation on monitor. Assistant provides continuous visualization of vocal fold with transnasal flexible laryngoscopy. (b) Percutaneous augmentation via thyrohyoid approach. Again, an assistant is needed for monitoring the injection (assistant not shown)
12.8.3 Percutaneous Endolaryngeal Laser Surgery
In patients with difficult-to-expose larynges in suspension microlaryngoscopy, an office laser approach with percutaneous laser technique may be another alternative to avoid open neck surgery. Endolaryngeal laser surgery (and endolaryngeal injections) can be performed through a percutaneously routed cannula. A 60-mm-long 20-G cannula can be inserted in a thyrohyoid approach as a guiding instrument for a 300 μm laser glass fiber advanced into the endolaryngeal lumen. Joystick-like movements of the outer cannula part allow for directing the glass fiber tip to all endoluminally visible surfaces. Surgery is monitored with a flexible laryngoscope. Since there are many fiber-guided lasers utilizable for endolaryngeal surgery (KTP, BL, argon, neodym-YAG, diode, etc.), this approach extends our armamentarium for laryngeal surgery.
12.8.4 Transnasal Esophagoscopy (TNE)
Transnasal esophagoscopy in the office is possible with the use of transnasal flexible endoscopes. Patients with dysphagia, reflux disease, head and neck cancer, and many other diseases and disorders related to this area can be diagnosed unsedated without being examined in general anesthesia. Therapeutically, biopsies can be taken, injections can be applied, and furthermore small laser surgery and balloon dilation of the esophagus can be performed. TNE provides various advantages over conventional endoscopy with equivalent clinical results. Some of the advantages are patient’s convenience, comfort, personal preference, and last but not least improved safety with decreased costs (Fig. 12.21).
(a) Transnasal esophagoscopy (TNE) can easily be performed when the patient swallows approx. ten sips of water without breathing, thus “swallowing the endoscope.” (b) TNE enables endoluminal visualization of the esophagus. NBI illumination for higher contrast. Lesion on the upper left side (red). Biopsy could also be taken through channeled endoscope
12.8.5 Transnasal Tracheoscopy (TNT)
Transnasal tracheoscopy in the office is one step further to “dipping” into the endolarynx. Adequate endolaryngeal and endotracheal topical anesthesia, delivered via inhalation, via dripping through the endoscope working channel, or administered via cannula percutaneously, allows for the advancement of the flexible endoscope into the trachea and performing interventions like intralesional steroid injections, biopsies, or even laser surgery. TNT as a diagnostic procedure provides various advantages over conventional endoscopy and is easy to perform—however, the techniques according to Killian and Türck (for rigid endoscope) or the “dipping maneuver” for flexible endoscopy should be followed for best imaging results (Fig. 12.22).
12.9 Possible Complications
In the authors’ view, it is felt that the likelihood for severe complications in office-based surgery may be most frequently associated with inadequate technique within injection laryngoplasty (augmentation), so that special attention is needed for these interventions. Within injection laryngoplasty, no matter which approach is chosen (transnasal, transoral, or percutaneous), the highest risk is to inject into the wrong layer, i.e., too superficially (Reinke’s space!), or to inject too much. Whatever leads to misplacement of the injectable, e.g., movement of patient, gag response, limited visualization, unexpected migration within the paraglottic space, filling of Reinke’s space, etc.—only step-by-step learning will lead to high professionality. Thus, if in doubt, injecting less material and having a wait-and-see attitude is advisable. One can start with more “forgiving” fillers such as resorbable hyaluronic acid injections.
Another extremely rare, but potentially severe, complication may be intra-fold hematoma, hemorrhage, or bleeding which might occur by rupturing superficial capillaries or a small artery in deeper vocal fold tissues followed by rapid, potentially airway occluding swelling of the vocal fold. Therefore, it is advisable to strongly reconsider the indication for in-office augmentation in patients with anticoagulation and also to take all measures to control patients intra- and postoperatively. Choosing the thinnest cannula possible to perform augmentations is always a good choice. However, after many hundreds of augmentations in the office, we did not encounter any severe complications.
In more than 30 years of performing office-based procedures, no severe cardiovascular reaction nor bradycardia has appeared. Very few cases with vasovagal reactions of lesser degree could be handled by supine positioning—legs up! Very few short-lasting laryngospasms encountered in the office were self-limiting and were treated rapidly and effectively with reassurance and breathing techniques (see above). Since many years, we do not administer atropine anymore. Finally, except in one case of a patient with panic attacks, we do not sedate patients anymore.
12.10 Disinfection and Hygiene
There is no office-based intervention without handling the instrument reprocessing with greatest care. We are aware of the fact that regulations and guidelines may differ enormously from country to country. Thus, local regulations and guidelines for the decontamination, cleaning, disinfection, and reprocessing of instruments, for rigid and for flexible endoscopes, and especially for those with a working channel apply and have to be checked. Cleaning costs could be a major problem as well as the turnover time for flexible endoscopes which can limit the number of interventions in a laryngology unit. These additional limitations may be difficult to bear, given the lack of established billing codes and the often inadequate reimbursement. Since the corona pandemic, we see a worldwide change in usage of PPE as well as room hygiene including droplet and aerosol reduction.
12.11 Outlook
Office-based procedures are now facing a new era—for many reasons. First, we have new technology which is versatile with better imaging while using instruments through a working channel. Diagnostic time pressures force us to get a rapid and reliable diagnosis, especially when malignancy might be present. With less availability of performing surgery in general anesthesia and a focus on patient centeredness in an outpatient clinical setting, we now are able to perform one-stop treatments with diagnostics and therapy in one session. Outpatient procedures can be done with topical anesthesia only, the patient sitting and communicating with the surgeon, avoiding high risks for general anesthesia, and also having shorter postoperative recovery time. This includes unsedated injections, biopsies, augmentations, and laser procedures in the pharynx, larynx, as well as transnasal esophagus. Therefore, it is not only a highly effective but also an efficient alternative. The outlook on the improvement of our healthcare services will go along with significant cost savings when in-office procedures with latest technology and competencies, surgical skills, and knowledge come together.
The indication for office-based surgery is always based on multiple factors and is essentially the result of the patient’s and surgeon’s decision-making process. In general, it is always beneficial having access to office-based surgery techniques to broaden one’s spectrum of surgical procedural choices. In the authors’ opinion, office-based interventions will play a significant role in the future of laryngology. They will not replace interventions in general anesthesia, but surely give more and more alternatives for diagnostics and therapeutical interventions.
References
Bastian RW, Delsupehe KG. Indirect larynx and pharynx surgery: a replacement for direct laryngoscopy. Laryngoscope. 1996;106:1280–6.
Fleischer S, Pflug C, Hess M. Dipping and rotating: two maneuvers to achieve maximum magnification during indirect transnasal laryngoscopy. Eur Arch Otorhinolaryngol. 2020;277(5):1545–9.
Friedrich G, Remacle M, Birchall M, Marie JP, Arens C. Defining phonosurgery: a proposal for classification and nomenclature by the Phonosurgery Committee of the European Laryngological Society (ELS). Eur Arch Otorhinolaryngol. 2007;264(10):1191–200.
Hess MM, Fleischer S, Ernstberger M. New 445 nm blue laser for laryngeal surgery combines photoangiolytic and cutting properties. Eur Arch Otorhinolaryngol. 2018;275(6):1557–67.
Koufman JA, Rees CJ, Frazier WD, et al. Office-based laryngeal laser surgery: a review of 443 cases using three wavelengths. Otolaryngol Head Neck Surg. 2007;137:146–51.
Mahieu HF, Dikkers FG. Indirect microlaryngostroboscopic surgery. Arch Otolaryngol Head Neck Surg. 1992;118:21–4.
Mallur PS, Johns MM III, Amin MR, Rosen CA. Proposed classification system for reporting 532-nm pulsed potassium titanyl phosphate laser treatment effects on vocal fold lesions. Laryngoscope. 2014;124(5):1170–5.
Remacle M, Ricci-Maccarini A, Matar N, Lawson G, Pieri F, Bachy V, Nollevaux MC. Reliability and efficacy of a new CO2 laser hollow fiber: a prospective study of 39 patients. Eur Arch Otorhinolaryngol. 2012;269(3):917–21.
Rosen CA, Amin MR, Sulica L, Simpson CB, Merati AL, Courey MS, Johns MM III, Postma GN. Advances in office-based diagnosis and treatment in laryngology. Laryngoscope. 2009;119(Suppl 2):S185–212.
Shoffel-Havakuk H, Sadoughi B, Sulica L, Johns MM III. In-office procedures for the treatment of benign vocal fold lesions in the awake patient: a contemporary review. Laryngoscope. 2019;129(9):2131–8.
Volk GF, Hagen R, Pototschnig C, Friedrich G, Nawka T, Arens C, Mueller A, Foerster G, Finkensieper M, Lang-Roth R, Sittel C, Storck C, Grosheva M, Kotby MN, Klingner CM, Guntinas-Lichius O. Laryngeal electromyography: a proposal for guidelines of the European Laryngological Society. Eur Arch Otorhinolaryngol. 2012;269(10):2227–45.
Von Bruns V. Die erste Ausrottung eines Polypen in der Kehlkopfshöhle durch Zerschneiden ohne blutige Eröffnung der Luftwege nebst einer kurzen Anleitung zur Laryngoskopie. Tübingen: Laupp; 1862.
Von Bruns V. Die Laryngoskopie und die laryngoskopische Chirurgie. 2. Ausgabe. Tübingen: Laupp; 1873.
Wellenstein DJ, de Witt JK, Schutte HW, et al. Safety of flexible endoscopic biopsy of the pharynx and larynx under topical anesthesia. Eur Arch Otorhinolaryngol. 2017;274(9):3471–6.
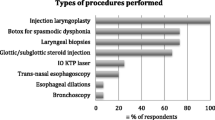
Wellenstein DJ, Schutte HW, Takes RP, Honings J, Marres HAM, Burns JA, van den Broek GB. Office-based procedures for the diagnosis and treatment of laryngeal pathology. J Voice. 2018;32(4):502–13.
Williams GT, Farquharson IM, Anthony J. Fibreoptic laryngoscopy in the assessment of laryngeal disorders. J Laryngol Otol. 1975;89:299–316.
Woo P. Office-based laryngeal procedures. Otolaryngol Clin N Am. 2006;39:111–33.
Young VN, Smith LJ, Sulica L, et al. Patient tolerance of awake, in-office laryngeal procedures: a multiinstitutional perspective. Laryngoscope. 2012;122:315–21.
Zeitels SM, Burns JA. Laser applications in laryngology: past, present, and future. Otolaryngol Clin N Am. 2006;39:159–72.
Zeitler DM, Amin MR. The thyrohyoid approach to in-office injection augmentation of the vocal fold. Curr Opin Otolaryngol Head Neck Surg. 2007;15:412–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hess, M.M., Fleischer, S. (2022). Office-Based Procedures. In: Remacle, M., Eckel, H.E. (eds) Textbook of Surgery of Larynx and Trachea. Springer, Cham. https://doi.org/10.1007/978-3-031-09621-1_12
Download citation
DOI: https://doi.org/10.1007/978-3-031-09621-1_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-09620-4
Online ISBN: 978-3-031-09621-1
eBook Packages: MedicineMedicine (R0)