Abstract
In this study, a novel polycaprolactone/gelatin/polydimethylsiloxane (PCL/G/PDMS) scaffold with improved mechanical properties and controllable porous structure was prepared through electrospinning method. In this research, the biocompatibility was evaluated, using mouse uterine cells. MTT, Hematoxylin-Eosin (H&E) staining results indicated that the growth of endometrial cells developed in the PCL/G/PDMS scaffold. The results also showed that the mouse embryo good adaptation with the scaffold and the scaffold transplantation to the mouse uterus showed that the uterine tissue was completely perfused after one month. Our data suggests that the PCL/G/PDMS scaffold is a new suitable scaffold material for tissue engineering. The purpose of this project is to eliminate of problems similar to damaged uterus, Rennet uterus (surrogacy), Lack of womb for women's using a scaffold like uterine tissue.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Scientists in regenerative medicine and tissue engineering are currently applying the principles of cell transplantation, materials science, and bioengineering to build biological alternatives that restore and maintain normal function in diseased and damaged tissues. Some of the therapeutic approaches stemming from tissue engineering efforts have now successfully entered the clinical setting, indicating the promise of a regenerative medicine for the future (Atala 2009). Uterine infertility is a factor of approximately 1:500 women of childbearing age (Bandstein and Hellström 2016). A study aimed at reconstructing engineered uterine tissues (EUTs) containing a smooth muscle layer resembles a normal uterine wall (Lü et al. 2009). Also, endometrial cell sheets help as a new treatment to restore functional endometrium (Takagi et al. 2014). Thus, tissue engineering programs using biomass and stem cells may replace the need for a living donor and may prevent the suppressive treatment of the required immune system (Hellström et al. 2014).
2 Materials and Methods
2.1 Animal
For uterine cell isolation, syrian mices (25 weeks) (Yazd Reproductive Sciences Institute) were used. All mouses were kept under specific conditions at the Animal Center of Yazd Reproductive Sciences Institute in accordance with facility guidelines. These maintained under controlled temperature (25 ± 38 C), proper humidity (50 ± 5%) and a 12 h light/dark cycle. The Ethical Review Committee of the Institute approved the experimental protocol.
2.2 Donor Uterus Harvest of Mice
Mices were unconscious with isoflurane. The mice were placed on its back and the abdomen was cleaned with 70% ethanol. A celiotomy was performed via cut the middle line from the symphysis pubis to the xiphoid process (Miyazaki and Maruyama 2014). Then both uterine horns were separated and placed in the DMEM.
2.3 Fabrication of Scaffolds
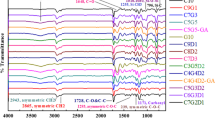
The scaffolds were produced by electrospinning method (Dehghan et al. 2020). To design and fabrication a three-dimensional scaffold of mice uterine tissue, a trilayer scaffold was produced. The inner layer consists of C3G5D2 nanofibers, the middle layer is PNIPAM nanofibers and the outer layer is C3G5D2 nanofibers The PNIPAM in water solution at 37 ℃ shranks significantly (Apsite et al. 2017) and bends to toward thin C3G5D2 scaffold and a trilayer tubular structure forms spontaneously. The C3G5D2 nanofibers are random and the PNIPAM nanofibers are aligned.
2.4 Isolation of Mouse Uterine Tissue Cells
At first, the uterine horn was separated from the immature syrian mice, and then it was washed with PBS and were minced. Minced uterine horn was treated with DMEM containing 0.1% collagenase type I at 37 ℃ for 1 h with shaking every 10 min. After an hour, the minced uterine horn was washed with PBS. The minced tissues were explanted inside the dish and the DMEM containing 10% FBS, 1% penstrep and 0.5% fungizon used as culture medium. Initially, 1000 µL of DMEM was added to the dish to attach the tissues to the dish and were incubated in a humidified incubator at 37 ºC with 5% CO2 concentration. After 24 h, 1000 µL of DMEM was added to the dish. The non-adherent tissues were removed after 48 h of culture and DMEM was added and the non-adhere cells were removed every 72 h. After 7 days, the cells were gradually extracted from the tissue and attached to the surface of the dish. On the 15 days, the cells were washed with PBS, incubated with 0.05%/0.02% (v/v) trypsin/EDTA solution and pelleted by centrifugation at 200 g for 5min. The cells were cultured in flasks and were incubated in a humidified incubator at 37ºC with 5% CO2 concentration. Cell culture was continued until the third passage. Cells were harvested at days 3, 7, and 10 for growth and evaluated using H&E staining and MTT test. By triplicate assay the activity and survival of the cells on nanofibers were calculated as a percentage of samples to controls.
2.5 In Vitro Fertilization and Embryo Assessment
The sperm was collected from mices 8–12 weeks for in vitro fertilization (IVF). The sperms were released into the medium and dispersed for 15 min at 37 C. After dispersal, the sperm concentration was determined to achieve the final concentration of 1 * 106 sperm/ml. Then, the insemination dishes were incubated for 1–2 h before addition of oocytes. The melted eggs were transferred from each group separately to 100 µl drops of G-IVF medium. After 5 h of incubation with spermatozoa, the oocytes were washed and cultured in G1 medium. The embryonic development progression was monitored every 24 h for 3 days until blastocyst stage (Mohammadzadeh et al. 2018). Then blastocyst was placed on the C3G5D2 scaffold.
3 Results and Discussions
The uterine tissue culture of the mouse and its cell extraction in the DMEM medium to the third passage are shown in Fig. 1. Attachment, proliferation and morphology of cells on scaffolds with H&E staining on 1, 3 and 7 days were shown in Fig. 2. After 7 days, a pervasive network of cells on the scaffolds proliferated and attached.
Figure 3 shown mouse embryos which were attached on scaffold and good compatibility with PCL/G/PDMS scaffold. 3D tubular scaffold for mouse uterine tissue produced and transplanted to mouse. After one month, the transplanted uterine tissue is stained by H&E and progesterone receptor (PRs) and is shown that the mouse uterine tissue is formed (Fig. 4).
4 Conclusion
The self-assembly of endometrial cells and stromal cells could make the reconstructed tissues closer to natural tissues in structure. Transplantation of engineered tissue in vivo and birth of offspring could be the next confirmatory step. These findings could be the first phase for the uterine tissue engineering, ready for animal study and then a clinical trial.
References
Atala, A.: Engineering organs. Curr. Opin. Biotechnol. 20(5), 575–592 (2009). ISSN: 0958-1669
Bandstein, S., Hellström M.: Tissue engineered uterine tissue supports pregnancy in a rat model. In: Programme in Medicine, Gothenburg, Sweden (2016)
Lü, S.-H., et al.: Reconstruction of engineered uterine tissues containing smooth muscle layer in collagen/matrigel scaffold in vitro. Tissue Eng. Part A 15(7), 1611–1618 (2009). ISSN: 1937-3341
Hellström, M. et al.: Towards the development of a bioengineered uterus: comparison of different protocols for rat uterus decellularization. Acta Biomater. 10(12), 5034–5042 (2014), ISSN: 1742-7061
Miyazaki, K., Maruyama, T.: Partial regeneration and reconstruction of the rat uterus through recellularization of a decellularized uterine matrix. Biomaterials 35(31), 8791–8800 (2014), ISSN: 0142-9612
Dehghan, M. et al.: Modeling and optimizing a polycaprolactone/gelatin/polydimethylsiloxane nanofiber scaffold for tissue engineering: using response surface methodology, J. Text. Inst. 112(3), 482–493 (2021). ISSN: 0040–5000
Psite, I., et al.: Porous stimuli-responsive self-folding electrospun mats for 4D biofabrication. Biomacromolecules 18(10), 3178–3184 (2017). ISSN: 1525-7797
Mohammadzadeh, M. et al.: Influential effect of age on oocyte morphometry, fertilization rate and embryo development following IVF in mice. Middle East Fertil. Soc. J. 23(2), 117–120 (2018). ISSN: 1110-5690
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Dehghan, M., Mehrizi, M.K., Nikukar, H. (2022). The Production of Hybrid Nano-fiber Scaffolds for Tissue Engineering of the Mouse Uterus. In: Msahli, S., Debbabi, F. (eds) Advances in Applied Research on Textile and Materials - IX. CIRATM 2020. Springer Proceedings in Materials, vol 17. Springer, Cham. https://doi.org/10.1007/978-3-031-08842-1_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-08842-1_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08841-4
Online ISBN: 978-3-031-08842-1
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)