Abstract
Systemically administered targeted gene therapy can benefit many diseases. This chapter focuses on mRNA-mediated gene delivery. We discuss why mRNA is superior to DNA for this purpose, especially for treating diseases like cancer, where it is necessary to kill also quiescent cells; and measures to increase mRNA stability. As vectors for directed mRNA delivery, lipid nanoparticles (LNPs) have many advantages, such as the ease of large-scale production and delivery of large molecules. Approaches to make them targeted include manipulating their chemical composition and charge. An example of the latter is successful CRISPR/Cas-mediated PTEN editing in targeted organs. LNP lipids can be immunogenic and toxic, but measures are being pursued to counter this. More recently, the extracellular vesicles (EVs, also called exosomes), “nature’s antigen delivery system,” have attracted much attention for being biocompatible and likely to be non-antigenic. While many small RNAs have been targeted using EVs, their loading with mRNA has only recently been accomplished; this has necessitated the use of special plasmids, although it has also now been done more directly. mRNA-loaded EVs displaying targeting peptides have, in preclinical studies, successfully treated implanted tumors in mice without side effects. The attachment of targeting peptides to EVs has been accomplished using, for example, the C1C2 domain of lactadherin, which not only binds tightly to EV lipid membranes but also, by masking their surface phosphatidylserine, increases their circulation time. Advantages of LNPs as vectors include the ease of their large-scale production and capacity to deliver large molecules; those of EVs are their biocompatibility, and relative non-toxicity and immunogenicity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- LNPs
- Extracellular vesicles
- Exosomes
- Systemic administration
- Targeted gene delivery
- mRNA
- Cancer
- Gene replacement
- Gene repair
- Gene silencing
1 Introduction
It is widely recognized that the treatment of many diseases can greatly benefit by targeted delivery of a gene(s) specifically to the intended site. Examples include diseases resulting from inherited defective genes or those altered by unfavorable mutations after birth. Treatment of diseases, including cancer, can be made more effective by this approach. One example is treatment involving prodrugs. Prodrugs are innocuous in their native state but can be converted to highly toxic drugs by a bacterial or viral enzyme. If the delivery of the gene encoding the converting enzyme is confined to the cancer, the drug toxicity would be restricted to the tumor, rendering the drug effective at low doses and obviating the severe side effects that accompany conventional non-directed chemotherapy (Rautio et al. 2008; Thorne et al. 2009).
Gene delivery has generally focused on DNA, but its delivery via mRNA has many advantages and marked progress in mRNA-based gene delivery has recently been made. Examples are the mRNA vaccines for immunization against cancer and—currently of great relevance—against the SARS Cov2 virus.
This chapter will focus on disease treatment by mRNA-based directed gene delivery following systemic injection of the gene-carrying vehicle. Although lipid nanoparticles (LNPs) have been discussed in other chapters of this book, we will mention some examples of such directed therapy also with LNPs.
Recently, much interest has focused on the use of extracellular membrane vesicles (EVs; also called exosomes) for directed mRNA-based gene delivery (Jayasinghe et al. 2021; Forterre et al. 2020; Wang et al., 2018); this will be discussed in greater detail.
2 Gene Delivery with mRNA Versus DNA
2.1 The Comparison
But first, let us address the question of why use mRNA for gene delivery? As opposed to DNA, mRNA does not pose the danger of insertion into the host genome, which can result in harmful outcomes. Further, to be effective in generating the desired protein, DNA needs to be transported into the nucleus for transcription, while the mRNA can be translated right upon entry into the cytosol. DNA transport from the cytosol to the nucleus mainly occurs during mitosis and is inefficient, particularly in non-growing cells. Also, mRNA can be produced at a large scale by in vitro transcription (IVT) in a cell-free environment that dispenses microbes and cultured cells—it requires, besides RNA polymerase, only the template DNA and the trinucleotides (TNPs); DNase treatment following manufacture eliminates the DNA template providing the mRNA in a pristine state.
But the DNA upon nuclear entry can generate several copies of mRNA. How do then the two nucleic acids compare in gene delivery? We focus here on non-growing cells—they are important, for instance, in cancer. Cancer cells grow rapidly, many becoming distant from the tumor blood vessels, and the resulting nutrient deprivation ushers them into the G0, non-growing, quiescent phase (Shibamoto and Streffer 1991). This phase is reversible and leads to cancer resurgence, which can be metastatic (Dudjak 1992): effective cancer treatment clearly must kill also non-growing cells.
Estimates of the proportion of quiescent cells in several cancers have been made; this includes the very serious ones, like melanoma and O771 adenocarcinoma. In one study, cytochalasin B was employed, which blocks cytoplasmic but not nuclear division. Scoring of multinucleated cells and the total number of nuclei and cells permitted estimation of non-growing cells: It showed that up to 67% of tumor cells can be quiescent (Shibamoto and Streffer 1991). So, how effective is mRNA versus DNA-based gene delivery in non-growing cells?
In primary neuronal cortical cells, which do not grow, luciferase reporter gene transfection was examined. mRNA-mediated transfection resulted in luciferase expression within 1 h, peaking at 5–7, and ending at 12 h. With DNA, no expression was seen until 7 h, but peak expression, which occurred at 36–48 h, was an order of magnitude greater (Zou et al. 2010). But if gene delivery is intended to kill the recipient cells, the delayed higher expression with DNA is irrelevant, as dead cells would have no expression. The results imply that mRNA would be better for killing non-growing cells by gene delivery.
Subsequent findings validate this. Bax gene delivery in malignant melanoma cells was examined (Okumura et al. 2008). Bax protein promotes apoptosis and cell killing. When liposome-Bax mRNA formulations were used for gene delivery to mice with this implanted cancer, Bax production occurred at 12 h; in contrast, with liposome Bax-DNA delivery, there was only a minor increase in Bax protein even after 24 h. Greater TUNEL-positive cells resulted with mRNA-compared to DNA-NLPs, and the apoptotic index (indicating the proportion of apoptotic cells) was 4.6-fold higher with mRNA. The tumor growth slowed significantly between 20 and 30 days with mRNA; with DNA-NLPs, only minor growth inhibition occurred at day 20 with no further mitigation. A similar finding has been made in prodrug cancer therapy, as is discussed below. Thus, mRNA is superior, especially when treatment requires killing also of non-growing cells.
2.2 Improving IVT mRNA for Clinical Use
This involves increasing mRNA stability and minimizing its antigenicity and toxicity.
2.2.1 Stability
mRNA can be highly unstable. Approaches to increase stability and expression include manipulation of mRNA five-prime cap (5′ Cap), its nucleotides, and its Poly(A) tail. The 5′ cap in eukaryotic RNAs is an altered nucleotide [7-methylguanosine (m7G)] at the 5′ end. It protects against mRNA degradation, promotes its translation, and mitigates its immunogenicity. Thus, for IVT mRNA synthesis, the DNA templates used incorporate anti-reverse cap analogs (ARCAs) along with NTPs and RNA polymerase. Examples of the ARCAs are 3′-O-Me-m7GpppG (Sahin et al. 2014) and the modified cap analogues, phosphorothiolate and imidodiphosphate; the latter two also render mRNA resistant to decapping enzymes, enhancing its stability (Wojtczak et al. 2018).
As regards the mRNA 5′- and 3′-untranslated regions (UTRs) and nucleotides, incorporation of β-globin and/or the TEV start site in the UTRs (Russell and Liebhaber 1996; Adibzadeh et al. 2019), and substituting uridine by pseudouridine and/or cytidine by 5-methylcytidine promote stabilization and enhance translation (Khan et al. 2009; Gallie 2001; Steinle et al. 2017). Reversible addition–fragmentation chain transfer (RAFT) polymerization is another promising approach: triblock copolymers are used to mediate mRNA condensation enhancing stability, biocompatibility, and cytosolic entry (Cheng et al. 2012).
Increasing the IVT mRNA in the producer cells by enhancing its entry in them can boost mRNA content in the EVs generated by the cells. Complexing the mRNA with lipofectin and using a nonlipid cationic reagent such as TransMessenger can accomplish this (Weissman et al. 2000).
It is thought that increased length of the polyA tail of mRNA enhances translation. However, many mRNAs that are efficiently translated have short tails, indicating that the optimal length may be transcript specific. This may thus need to be determined for a given mRNA and the required tail length incorporated in the DNA template (Holtkamp et al. 2006).
Self-amplifying circular RNA (circRNA) holds great promise. It lacks the free ends that the nucleases for mRNA degradation utilize and therefore has a longer half-life than its linear counterpart (Wesselhoeft et al. 2019). Linear mRNA encodes only the therapeutic protein but circRNA encodes also proteins which enable mRNA replication (Vogel et al. 2018). An internal ribosome entry site (IRES) allows translation, so high levels and prolonged protein synthesis can result (Daijogo and Semle 2011).
2.2.2 Immunogenicity
Although, as mentioned above, the 5′cap m7G minimizes mRNA immunogenicity, it does not eliminate it. RNAs can interact with RNA sensors in humans such as the toll-like receptors, RIG-I, and PKR (Yu and Levine 2011). Danger signals are activated by this, which interfere with mRNA translation. mRNA can also activate type I interferons and proinflammatory cytokine production (Freund et al. 2019; Dammes and Peer 2020). Some of the measures mentioned above for increasing mRNA stability can also minimize this propensity. In addition, the use of pseudouridine and methylpseudouridine, and chemical modification of the phosphate backbone and mRNA termini also minimize immunogenicity.
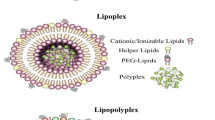
3 Targeted LNPs
As is noted in other chapters of this book, lipid nanoparticles (LNPs) are widely used in mRNA delivery. They are easy to make –mixing a lipid solution in ethanol with mRNA in water and using microfluidic devices. Further, LNPs have the capacity to deliver large molecules (Hou et al. 2021). Given the theme of our chapter, we mention salient examples of targeted mRNA-based gene delivery by systemically administered LNPs to therapeutic effect.
Measures to target LNPs include manipulating their chemical composition. For example, cholesteryl oleate incorporation confers selectivity on LNPs for liver endothelial cells as opposed to hepatocytes and this specificity is enhanced by oxidative changes in the cholesterol tail. And manipulation of alkyl length of a lipid can direct the LNPs to liver or spleen (Hou et al. 2021). A library of ionizable amino-polyesters (APEs) was synthesized by ring-opening polymerization (ROP) of lactones using tertiary amino-alcohols; the number of repeating monomer units was controlled to generate degradable polymers (Kowalski et al. 2018). Mixing APEs with the appropriate lipids and mRNA generated mRNA-APE-LNPs. The APE-LNP library was tested for uptake capacity in HeLa cells; top-performing APEs contained four and two amines (A-TD3, B-DD3 and I-DD3). LNPs containing this had organ selectivity: ATD3 for spleen, B-DD3 for lungs.
A notable accomplishment is the targeted NLP-mediated delivery of clustered regularly interspersed palindromic repeats enzyme system (CRISPR/Cas) for gene manipulation. Cas is an endonuclease which, when directed by a guide RNA (sgRNA), can introduce a DNA double-stranded break (DSB) at essentially any site in the genome; this gap can be replaced with a desired DNA fragment by flanking it with sequences homologous to the DSB region. The technology can precisely edit genes, correct disease-causing mutations, and eliminate aberrant protein expression. mRNA-instead of DNA-based delivery of Cas is preferable, as the former is easy to produce, results in rapid expression whose transience minimizes off-target cleavage.
Selective organ targeting (SORT) approach was used for targeted delivery of mRNA-LNPs to deliver the CRISPR/Cas system. As LNP charge can affect their organ tropism, SORT molecules were added to traditional LNPs (‘mDLNPs’) to make them organ-specific (Cheng et al. 2020). Increasing molar percentage of the SORT molecule, 1,2-dioleoyl-3-trimethylammonium-propane (DOTAP, a cationic lipid), altered organ tropism of the NPs. While the base mDLNPs without DOTAP targeted liver, the SORT-LNPs containing 10–15% DOTAP targeted spleen, and those containing 50% of this lipid targeted the lungs. Incorporation of 10–40% of the negatively charged 1,2-dioleoyl-sn-glycero-3-phosphate (18PA), resulted in highly selective targeting of the spleen. SORT-LNPs successfully edited phosphatase and tensin homolog (PTEN), a tumor suppressor expressed in most cells. Cas9 mRNA and sgPTEN co-loaded in SORT-LNPs were i.v. injected in mice, and PTEN deletion was quantified. Both base mDLNPs and 20% DOTAP SORT-LNPs caused PTEN editing in liver, but not in spleen or lung, while 50% DOTAP SORT-LNPs-mediated PTEN editing only in the lungs. No off-target editing was seen (Cheng et al. 2020; Rosenblum et al. 2020). Mechanical properties of the liposome core can affect LNP stiffness; layer-by-layer (LbL) NPs with controlled stiffness can have enhanced circulation, tumor penetration, and accumulation (Kong et al. 2021).
An mRNA-based LNP drug, NTLA-2001, which utilizes the CRISPR-CAS system is currently in clinical trial to treat transthyretin amyloidosis, a life-threatening disease caused by the accumulation of misfolded protein transthyretin (TTR) in nerves and cardiomyocytes. Apolipoprotein E (ApoE)-targeted LNPs can transduce liver hepatocytes by binding to low-density lipoprotein (LDL) receptors. These were loaded with Cas-encoding mRNA and the corresponding guide RNA. Their intravenous injection resulted in CRISPR/Cas-mediated inactivation of TTR followed by DNA repair by non-homologous end-joining. Serum TTR in patients was reduced by ca. 96%, which may potentially lead to disease amelioration (Gillmore et al. 2021). In this relatively short-term 28-day study, no adverse effects were seen but as the LDL receptor is present also on other cells, possible off-target effects require careful monitoring.
Incorporation of polyethylene glycol (PEG; ‘pegylation’) in LNPs is another means of making directed LNPs by linking specific antibodies to PEG; pegylation also promotes avoidance by LNP of mononuclear phagocytes and renal filtration, thus increasing circulation residence time. This approach enabled targeted mRNA-LNPs to treat inflammatory bowel disease as well as cancer (Rosenblum et al. 2020). Neoantigens, which are usually specific to cancers, can thus also be used for targeted delivery (Kowalski et al. 2019).
There are, however, safety and other issues with LNPs. PEG-lipids stimulate the complement system inducing hypersensitivity, and the antigenic response can also result in shortened circulation time with accelerated blood clearance, mitigating therapeutic efficacy. Attaching PEG molecules on LNP surface through labile bonds sensitive to, e.g., serum albumin, to promote slow de-pegylation, and manipulation of PEG surface density/chain length are possible countermeasures (Abu Lila et al. 2013a, b). Lipid components can cause lung and liver injuries in mice; the solution may be to improve LNP biocompatibility by using biodegradable lipids (Sedic et al. 2018).
4 Extracellular Vesicles (EVs, Aka Exosomes)
The use of extracellular vesicles (EVs, also called exosomes; Fig. 1) for nucleic acids and drug delivery has engendered considerable excitement. EVs are constitutively generated by body cells.

Source (Wang et al., 2018). Reproduced by permission of the corresponding author and the Journal
Left: TEM of EVs; center: their NanoSight sizing; right: presence in them of proteins, which conform to standards of EV definition. The EVs were made by differential centrifugation: [600 xg (to remove cells); 2,000 xg (to remove apoptotic bodies); 100,000 xg (to pellet EVs).
They are lipid bilayers and contain nucleic acids, proteins, and other biomolecules whose identity depends on their cellular origin. This ‘native’ content has been shown to be transferred to the cytoplasm of the neighboring or distant recipient cells. Thus, EVs serve as natural antigen delivery systems and are therefore likely to be biocompatible and minimally immunogenic/toxic: indeed, exosomes of human kidney embryo 293 (HEK293) cells (the ‘work horse’ of EV research) are harmless in mice (Wang et al. 2018; Zhu et al. 2017; Forterre et al. 2020). EVs derived from mesenchymal stem cells (Lee et al. 2021) or from patient's own, e.g., dendritic cells (DC), may be completely safe for gene/drug delivery; indeed, DC-derived EVs have been found to be safe in human clinical trials (Pitt et al. 2016).
As regards targeting, EVs have the advantage of intrinsic tissue tropism due to their membrane proteins. For example, integrin (ITG) αVβ5 possessing EVs bind specifically to liver Kupffer cells and EVS with ITGα6β4 and ITGα6β1expression have affinity for fibroblasts and epithelial cells in the lung, respectively (Capasso et al. 2020). Their natural ability to extravasate through fenestrations in tumor blood vessels makes them suitable vectors also in treating cancers in general. However, these inherent advantages are by themselves not sufficient for effective targeted therapy; this requires display on the EV surface of specific directing moieties. Examples of directing molecules resulting in successful treatment by EVs are as follows. Av-integrins [doxorubicin delivery to tumors (Tian et al. 2014)]. Epidermal growth factor receptor-targeting moiety [let-7ainordertodeliverlet-7a (let7a) delivery to breast cancer in mice (Kooijmans et al. 2016; Ohno et al. 2013)]. And asialoglycoprotein hepatocyte receptor-targeting ligand [delivery of siRNAs to blood cells for selective silencing of genes responsible for disease causation (Wahlgren et al. 2012)]. These examples also underscore the fact that EVs can evade the lysosomal–endosomal pathway well enough to deliver the required therapeutic agent to the targeted cells in sufficient strength to treat diseases.
The native EV content as well as non-EV biomolecules that may co-isolate with them can be affected by their method of preparation (Veerman et al. 2021). These might be co-delivered along with the intended therapeutic agent to the recipient cells. No harmful effects have so far been reported resulting from such unintended co-delivery, but future studies may point to the need for specific EV preparation methods for particular therapeutic ends.
4.1 mRNA Loading of EVs
As stated, EVs have been successfully used for targeted delivery of si- and miRNAs. But loading them with foreign larger molecules, such as mRNA, proved challenging. Electroporation did not work. EVs generated by HEK293 producer cells transiently expressing Luc–RFP contained the mRNA of this reporter, but the mRNA was degraded in the recipient cells (Kanada et al. 2015). A bacteriophage protein bridge between the EVs and mRNA also succeeded in loading EVs with mRNA, but again it was nonfunctional in the recipient cells (Hung and Leonard 2016).
The first successful EV-mediated delivery of functional mRNA to treat cancer was accomplished with HchrR6 mRNA, which encodes an improved and humanized version of Escherichia coli nitroreductase (HchrR6) (Barak et al. 2006, 2008). This enzyme is therapeutically important, as it reductively activates several prodrugs used to treat cancer, such as CNOB which is converted to the drug 9-amino-6-chloro-5H-benzo[a]phenoxazine-5-one (MCHB) (Fig. 2); and CB1954 (tretazicar), which is transformed to the drug 5-(aziridine-1-yl)–2,4-N-acetoxy-2-nitrobenzamide (MPNQ) (Patel et al. 2009). [Activation of a harmless prodrug to a toxic drug by a bacterial or viral enzyme for treatment is termed gene-directed prodrug therapy (GDEPT)].

Source (Thorne et al., 2009). Reproduced by permission of the corresponding author and the Journal
a Prodrug 6-chloro-9-nitro-5-oxo-5H-benzo[a]phenoxazine (CNOB), and b its reduced product, the drug 9-amino-6-chloro-5H-benzo[a]phenoxazine-5-one (MCHB).
Both MCHB and MPNQ cause DNA intercalation and kill both growing and non-growing tumor cells, which is advantageous, as discussed above, for cancer treatment. Both also have an excellent bystander effect (BE), meaning that the cytotoxic drug can readily leak out from the cells and thus also kills the neighboring cells not expressing the required enzyme-encoding gene. As no method of gene delivery is effective enough to transfect all cells in a tumor and given that the targeted receptor/ligand is often not expressed by all cancer cells (Filho et al. 2021). BE is important for GDEPT success.
CNOB is a new prodrug (Thorne et al. 2009), not yet clinically tested. But it has the useful feature that the drug it generates, MCHB, (Fig. 2B) by the activity of HchrR6 enzyme is highly fluorescent, and is easily visualizable in vitro and in living mice; this is shown for the latter in Fig. 3 (Thorne et al. 2009; Wang et al. 2016). This facilitated the development of GDEPT approaches discussed below in ensuring that the targeted EVs activated the prodrug in the tumor. Tretazicar’s activated drug, MPNQ, requires involved methods for detection, but it has been clinically tested with its safe dose established (Patel et al. 2009); it is thus a prime candidate for GDEPT transfer to the clinic; the MCHB fluorescence has paved the way for this transfer as is discussed below. It should be noted that no reductive prodrug has as yet been approved by the FDA for cancer treatment.
Native mRNAs in EVs contain a common sequence, called the ‘zipcode’ (Bolukbasi et al. 2012), and this was utilized in loading EVs with HchrR6 mRNA. Two tandem (DNA counterparts of) zipcode sequences were inserted in the UTR of the HchrR6 DNA under a constitutive promoter, and the construct was cloned into the System Biosciences ‘XPort’ plasmid (Wang et al. 2018). The resulting plasmid (named ‘pXPort/HchrR6 mRNA’) was used to transfect the HEK293 producer cells, which generated HchrR6 mRNA containing EVs; these were made targeted to the HER2 receptor of BT474 human HER2+ cells as described below. (The mRNA-loaded, directed EVs are termed, EXODEPTs.) When the EXODEPTs were mixed with the (HER2+) BT474 cells, the latter acquired the ability to activate the prodrugs; this is shown for CNOB activation in Fig. 4: the activation could be easily ‘seen’ due to MCHB fluorescence. Acquisition of this capability was not affected by actinomycin D (‘ActD’, transcription inhibitor) but was by cycloheximide (‘CHX’, protein synthesis inhibitor; Fig. 4). Thus, it was the HchrR6 mRNA that the EVs transferred, which the recipient cells translated into the HchrR6 enzyme.

Source (Wang et al., 2018). Reproduced by permission of the corresponding author and the Journal
mRNA transferred to HER2+ BT474 cells via the EXODEPTs is functional. Upon CNOB addition, MCHB is generated, as detected by its fluorescence. This process is actinomycin D (ActD) resistant and is abolished by cycloheximide (CHX), showing that it’s the HchrR6 mRNA that was transferred to the BT474 cells, which translated it to the HchrR6 enzyme making them capable of CNOB activation.
In a related study, several plasmids were used to generate EVs capable of transferring catalase-encoding mRNA to recipient cells (Kojima et al. 2018). However, the catalase activity of the producer cells was not reported; nor whether catalase expression in the recipients was insensitive to actinomycin D. Thus, the catalase activity in the recipient cells could have resulted from the transfer of catalase-encoding plasmid and/or the catalase protein itself, rather than the catalase-encoding mRNA.
An additional method for loading EVs with mRNA relied on the application of transient electrical pulses to a small area of the recipient cell’s membrane (Yang et al. 2020, 2021). A cellular nanoporation (CNP) biochip was used to cultivate various producer cells, including embryonic fibroblasts and the DC cells. An array of nanochannels in the chips provided the electrical pulse, which shuttled PTEN plasmids from the buffer into the cell monolayers attached to the CNP surface. The authors report that the method increased mRNA loading into the EVs by 2000–10,000-fold. How the electric pulse enhanced plasmid entry into the nucleus for transcription of the mRNA that got loaded into the EVs was not clarified. The resulting EVs were made capable of targeted delivery of PTEN to a murine glioma model (see below).
The above methods relied on transfection of producer cells with plasmids, which were likely transferred to the EVs that the cells generated, and from the EVs into the recipient cells. This is potentially problematic for clinical EV use, as plasmid introduction into patients can have unpredictable effects. Moreover, the use of plasmids to generate mRNA in the producer cells for transfer to their EVs is constrained by the need of the plasmid entry into the nucleus for transcription which, as noted, is inefficient, diminishing mRNA loading of the EVs (see below). Therefore, the plasmid use was replaced by direct loading of the EVs with vitro transcribed (IVT) HchrR6 mRNA (Forterre et al. 2020). This required several steps (Fig. 5); naked mRNA being prone to instability, these workers ensured the mRNA’s functionality through these steps by a facile method described below.

Source (Forterre et al. 2020). Reproduced by permission of the corresponding author and the Journal
Steps in making and using the IVT-EXODEPTs.
4.2 Strategies to Target mRNA-Loaded EVs and Their Therapeutic Use
Making EVs effective therapeutic agents requires display on their surface of specific targeting moieties, as mentioned above. This has been accomplished by constructing fusion proteins consisting of a targeting domain and an EV anchor domain. Salient examples of the EV anchors are as follows.
4.2.1 Lamp2b
An early example of the anchoring approach is the use of Lamp2b protein, which is abundant in EVs. It was fused to the N-terminal of neuron-targeting rabies viral glycoprotein. EVs displaying this fusion delivered siRNA to the brain and caused significant knockdown in mice of BACE1, a target in Alzheimer’s disease (Alvarez-Erviti et al. 2011). Others, however, had problems with this approach, such as degradation of the peptides fused to Lamp2b upon EV-mediated transfer (Hung and Leonard 2016; Wang et al. 2018). It is now recognized that incorporation of a glycosylation motif in the Lamp2b fusions can protect the peptides (Hung and Leonard 2016). This approach can therefore be effective also in targeted mRNA delivery, although no such attempts have so far been published.
4.2.2 Lactadherin C1C2 Domain
Lactadherin is a secreted protein with a C1C2 domain at the C-terminus. This domain binds to lipid membranes with high affinity, especially when phosphatidylserine (PS) is present, as is the case on the EV surface. PS is ‘eat me’ signal to eliminate apoptotic cells by phagocytosis. Use of this domain for targeting fusions in EVs thus has the advantage of masking PS, thereby mitigating EV phagocytosis, and enhancing their potential to reach the intended target (Dammes and Peer 2020; Jayasinghe et al. 2021). This approach was used by the Matin group (Wang et al. 2018; Forterre et al. 2020) to treat implanted orthotopic HER2+ breast cancer (BC) tumors in mice. The prodrugs CNOB and CB1954 were used in separate studies with the HchrR6 enzyme (that can, as mentioned, activate both). HER2+ BC has poor prognosis and results from dysregulation of tyrosine kinase signaling network due to HER2 gene amplification. Drugs like trastuzumab and lapatinib have been effective in treating it, but a 10-year follow-up study shows that ≥ 25% of early-stage patients treated with trastuzumab relapse, often with distant metastatic disease that does not respond to this drug (Cameron et al. 2017), highlighting the need for additional therapeutic approaches.
Using appropriate source plasmids, a new plasmid, pEVC1C2HER, was constructed (Wang et al. 2018). Transfection of HEK293 producer cells with this plasmid yielded EVs displaying the protein fusion termed EVHB (Fig. 6); MW, 68 kDa). It has lactadherin leader sequence (LS; to enable the protein to migrate to the EV surface), an scFv termed ML39, with high affinity to bind the HER2 receptor [K(d)109 mol/L], and a flexible linker that connects it to the C1C2 domain. Isolated and purified EVHB protein was mixed with HchrR6 mRNA-loaded EVs. In vitro, the resulting EXODEPTs displaying EVHB selectively targeted the HER2+ BT474 BC cells, but not the HER2− MCF7 cells, and converted the former to CNOB-activating agents, as measured by MCHB fluorescence. The EVs needed to be displaying EVHB—to be EXODEPTs in effect—to convert the recipient cells into CNOB activators (Fig.4). As noted above, Fig. 4 documents that the acquired CNOB-activating capability in human BT474 cells was not inhibited by actinomycin D and therefore was due to the EV-delivered mRNA to these HER2+ cells (Fig. 4).

Source (Wang et al., 2018). Reproduced by permission of the corresponding author and the Journal
Top: components of the EVHB chimeric protein; Below: its predicted structure. Colors: green, scFv antibody; red, C1C2 domain; blue, leader sequence; yellow, His tag. (Note colors in the predicted structure are different; the various components are identified within this figure).
4.2.2.1 Use of IVT mRNA and Tretazicar
As mentioned, loading EVs with the IVT mRNA required a multistep process (Fig. 5); IVT mRNA avoids the use of plasmids potentially harmful to patients and tretazicar has proven safe in humans in phases I/II clinical trials, as mentioned above. Thus, using IVT-EXODEPTs + tretazicar enhances the prospect of clinical transfer of this GDEPT. Tretazicar-activated drug, MPNQ, is difficult to detect and so a facile indirect strategy was used for ensuring that the mRNA remained competent to activate tretazicar through the multistep process of IVT loading into the EVs (Fig. 5). This relied on the fact that HchrR6 can activate both CNOB and CB1954. So, it was hypothesized that if the mRNA-translated product at various steps of IVT-EV preparation and uses (Fig. 5) generated MCHB fluorescence from CNOB, it would indicate its competence to activate tretazicar as well. At every step indicated in Fig. 5, the mRNA did indeed encode the protein that generated MCHB from CNOB; and as hypothesized, also activated tretazicar.
4.2.2.2 Systemic Administration
Until the Matin group studies (Forterre et al. 2020; Wang et al. 2018), cancer prodrug treatment pre-clinical studies had required injection of the therapy directly into the tumor. As not all cancers, especially multiple sites of metastatic cancer, are accessible to direct injection, this limited GDEPT applicability. The EXODEPT/CNOB and EXODEPT/tretazicar therapy overcame this problem, as these treatments were effective in vivo upon systemic injection. This is shown for the IVT EXODEPT/tretazicar treatment of implanted BT474 human HER2+ tumors in mice (Fig. 7).

Source (Forterre et al. 2020). Reproduced by permission of the corresponding author and the Journal
In vivo effectiveness of systemic IVT EXODEPTs + tretazicar. Implanted orthotopic human HER2+ BC tumor volumes in mice, as measured by caliper. The treatment likely killed the tumor—see text for further information.
CB1954 was used at its safe dose (determined in its phases I/II clinical trials; see above) and a total of 2.8 × 107 mRNA copies were delivered per mouse via IVT-EXODEPTs. In mice receiving this treatment, there was minimal growth of the tumor and it ceased by day 8 with no growth resumption over the next 21 days; the experiment was stopped on the 29th day in conformance with the approved animal use protocol. As the last dose was on day 7, it is reasonable to conclude that the treatment had killed the tumor. Untargeted, but mRNA-loaded, EVs also caused significant arrest of the xenograft growth but some 50% less than with the EXODEPTs. This illustrates the facts that EVs can be effective because of the enhanced permeability retention (EPR) effect, but that for full effectiveness they need to be directed. Untreated controls sowed vigorous tumor growth. It should be noted that nearly three orders of magnitude fewer IVT-EXODEPTs were as effective in treating the cancer as the pXPort/HchrR6 mRNA plasmid-EXODEPTs described above; this was ascribed mainly to the limitation imposed on the latter by the need for the plasmid to enter the nucleus of the producer cells for mRNA generation (Forterre et al. 2020).
Trastuzumab and similar drugs are effective in treating the HER2+ cancer because they interact with the HER2 receptor and inhibit its signaling. The EXODEPTs displaying the anti-HER2 receptor scFv may have been effective, at least in part, for the same reason. This, however, was not the case, because administration of directed EVs (displaying the scFv) not containing HchrR6 mRNA had no effect on tumor growth (Forterre et al. 2020).
EVs temporarily colonize organs like pancreas, spleen, and liver, and the ML39 scFv of the EXODEPTs might also have recognized mouse ErbbB2-expressing normal cells and by delivering the mRNA might have enabled them to activate the CB-1954. This would have caused general injury besides treating the cancer. However, a comprehensive investigation of organ histopathology (namely of liver, spleen, kidney, lung, heart, and the brain), hematology, and serum chemistry indicated no deleterious effects. Thus, the therapy was cancer curative without side effects (Forterre et al. 2020).
The above studies were conducted in immune-deficient mice. The authors are planning to extend them to immune-competent FVB/NJ mice. These contain an oncogenic form of human HER2—HER2Δ16 (Turpin et al. 2016)—resulting in spontaneous development of HER2+ BC (inducible by Dox). The therapy discussed above (Forterre et al. 2020; Wang et al. 2018) includes elements of human origin, viz. the C1-C2 lactadherin domain and the anti-HER2 scFv, ML39. An immune response to these, while possibly deleterious can, however, bolster the therapy instead. There was no off-target toxicity of the regimen, as discussed, indicating that the EXODEPT location was confined to the tumor. Thus, the immune rejection of these human elements of EXODEPTs might, by being directed to the tumor, further promote its eradication. HER2 tumor ablation evokes a strong anti-HER2 immune response (Milani et al. 2014), which too can reinforce the therapy.
A recent study involving an innovative chimeric protein to concomitantly activate two prodrugs, ganciclovir and tretazicar, has been reported (Kanada et al. 2019). The genes encoding the activating enzymes were cloned into minicircles (miniaturized plasmids, which are more efficient in gene delivery than the parent plasmid). Injection of the two prodrugs and 5.5 × 109 minicircle plasmids encoding the hybrid gene directly into breast cancer xenografts in mice resulted in 54% killing of the tumor. With EV-mediated mRNA gene delivery in the EXODEPT approach mentioned above, over two orders of magnitude fewer gene copies sufficed to kill the tumor despite systemic administration and the use of only one prodrug. This may be because DNA for gene delivery is less efficacious in cancer treatment than mRNA, as discussed above.
4.2.3 CD47
This is an abundant EV surface protein, and as opposed to PS, which needs to be masked to prevent EV phagocytosis, CD47 suppresses phagocytosis, and so a strategy opposite to that described for C1C2 fusions was followed that increased CD47 expression on the EVs (Yang et al. 2020). EVs containing the PTEN mRNA generated, as described above, were made to display increased CD47 fused to glioma targeting peptides (‘Exo-T’ EVs). Exo-Ts had increased circulation time and were specifically taken up by U87 and GL261 cells. Their use in orthotopic PTEN-deficient glioma mouse model inhibited tumor growth and resulted in increased survival.
4.3 Improving EVs for Clinical Use
A major step needed for this is scaling up of EV production. The electrical pulse method described above is a step in this direction. Among other approaches being pursued are placing cells in a nitrogen cavitation vessel under pressure (350–400 psi) and its quick release to disrupt the cells. This generates large numbers of what are referred to as ‘NC EVs.’ These EVs significantly attenuated acute lung inflammation (Gao et al. 2017). Another method involves the use of sulfhydryl blocking reagents, such as formaldehyde and a reducing agent such as dithiothreitol during EV production; it generated in one hour the amount of EVs that conventional methods (e.g., differential centrifugation) take 12 h to produce (Li et al. 2017) (https://patents.google.com/patent/WO2018102608A1/en). Increasing intracellular calcium also resulted in increased EV release (Savina et al. 2003), and it has been reported that incubation of liposomes with cells enhanced EV secretion several fold (Emam et al. 2018).
Other needed measures are: 1. To standardize EV engineering protocols. 2. To prevent rapid clearance of EVs from circulation to permit effective binding to the targeted cells. The use of CD47 fusions discussed above is conducive to this. The need for high residence time in circulation can be decreased by display on the EVs of high affinity directing molecules that can bind to the target rapidly after systemic injection; the use of the EVHB protein (see above, Fig. 6) is an example of this. 3. Avoiding potential immunogenicity. As discussed, being natural means of biomolecule exchange, this may not be a major problem with EVs. Further, their localization to the tumor can direct any anti-EV immune response against the tumor, reinforcing the therapeutic effect (see above). And finally, the use of stem cell EVs and those made from patients’ own, e.g., DCs is unlikely to evoke an immune response.
5 Conclusion
Directed, systemically administered mRNA-based gene delivery has the potential of revolutionizing therapy of disease like cancer and others. Both LNPs and EVs are highly promising vehicles for such delivery, each with its own unique advantages.
Abbreviations
- 18PA:
-
1,2-Dioleoyl-sn-glycero-3-phosphate
- ARCAs:
-
Anti-reverse cap analogs
- ApoE:
-
Apolipoprotein E
- APEs:
-
Ionizable amino-polyesters
- CNOB:
-
6-Chloro-9-nitro-5-oxo-5H-benzo[a]phenoxazine
- CB1954/tretazicar:
-
5-(Aziridine-1-yl)-2,4-dinitrobenzamide
- DC:
-
Dendritic cells
- DSB:
-
Double-stranded break
- EVs:
-
Extracellular membrane vesicles
- GDEPT:
-
Gene-directed enzyme prodrug therapy
- HEK293:
-
Human kidney embryo 293 cells
- IVT:
-
In vitro Synthesized mRNA
- IRES:
-
Internal ribosome entry site
- ITG:
-
Integrin
- LDL:
-
Low-density lipoprotein
- let7a:
-
Let-7ainordertodeliverlet-7a
- LNP:
-
Lipid nanoparticles
- m7G:
-
Me-m7GpppG
- MCHB:
-
9-Amino-6-chloro-5H-benzo[a]phenoxazine-5-one
- MPNQ:
-
5-(Aziridine-1-yl)–2,4-N-acetoxy-2-nitrobenzamide
- NTPs:
-
Nucleotide triphosphates
- PEG:
-
Polyethylene glycol
- PS:
-
Phosphatidylserine
- ROP:
-
Ring-opening polymerization
- SORT:
-
Selective organ targeting
- TTR:
-
Transthyretin protein
- UTR:
-
Untranslated region
References
Abu Lila AS, Kiwada H, Ishida T (2013a) The accelerated blood clearance (ABC) phenomenon: clinical challenge and approaches to manage. J Control Release 172:38–47
Abu Lila AS, Nawata K, Shimizu T et al (2013b) Use of polyglycerol (PG), instead of polyethylene glycol (PEG), prevents induction of the accelerated blood clearance phenomenon against long-circulating liposomes upon repeated administration. Int J Pharm 456:235–242
Adibzadeh S, Fardaei M, Takhshid MA et al (2019) Enhancing stability of destabilized green fluorescent protein using chimeric mRNA containing human beta-globin 5′ and 3′ untranslated regions. Avicenna J Med Biotechnol 11:112–117
Alvarez-Erviti L, Seow Y, Yin H et al (2011) Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat Biotechnol 29:341–345
Barak Y, Nov Y, Ackerley DF et al (2008) Enzyme improvement in the absence of structural knowledge: a novel statistical approach. ISME J 2:171–179
Barak Y, Thorne SH, Ackerley DF et al (2006) New enzyme for reductive cancer chemotherapy, YieF, and its improvement by directed evolution (research support, N.I.H., extramural, research support, Non-U.S. gov’t, research support, U.S. gov’t, non-P.H.S.). Mol Cancer Ther 5:97–103
Bolukbasi MF, Mizrak A, Ozdener GB et al (2012) miR-1289 and “Zipcode”-like sequence enrich mRNAs in Microvesicles. Mol Ther Nucleic Acids 1:e10
Cameron D, Piccart-Gebhart MJ, Gelber RD et al (2017) 11 years’ follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive early breast cancer: final analysis of the HERceptin adjuvant (HERA) trial. Lancet 389:1195–1205
Capasso D, Del Gatto A, Comegna D et al (2020) Selective targeting of alphavbeta5 integrin in HepG2 cell line by RGDechi15D peptide. Molecules 25:4298
Cheng C, Convertine AJ, Stayton PS et al (2012) Multifunctional triblock copolymers for intracellular messenger RNA delivery. Biomaterials 33:6868–6876
Cheng Q, Wei T, Farbiak L et al (2020) Selective organ targeting (SORT) nanoparticles for tissue-specific mRNA delivery and CRISPR-Cas gene editing. Nat Nanotechnol 15:313–320
Daijogo S, Semler BL (2011) Mechanistic intersections between picornavirus translation and RNA replication. Adv Virus Res 80:1–24
Dammes N, Peer D (2020) Paving the road for RNA therapeutics. Trends Pharmacol Sci 41:755–775
Dudjak LA (1992) Cancer metastasis. Semin Oncol Nurs 8:40–50
Emam SE, Ando H, Abu Lila AS et al (2018) A novel strategy to increase the yield of exosomes (extracellular vesicles) for an expansion of basic research. Biol Pharm Bull 41:733–742
Filho OM, Viale G, Stein S et al (2021) Impact of HER2 heterogeneity on treatment response of early-stage HER2-positive breast cancer: phase II neoadjuvant clinical trial of T-DM1 combined with Pertuzumab. Cancer Discov 11:2474–2487
Forterre AV, Wang JH, Delcayre A et al (2020) Extracellular vesicle-mediated in vitro transcribed mRNA delivery for treatment of HER2(+) breast cancer xenografts in mice by prodrug CB1954 without general toxicity. Mol Cancer Ther 19:858–867
Freund I, Eigenbrod T, Helm M et al (2019) RNA modifications modulate activation of innate toll-like receptors. Genes (basel) 10:92
Gallie DR (2001) Cap-independent translation conferred by the 5’ leader of tobacco etch virus is eukaryotic initiation factor 4G dependent. J Virol 75:12141–12152
Gao J, Wang S, Wang Z (2017) High yield, scalable and remotely drug-loaded neutrophil-derived extracellular vesicles (EVs) for anti-inflammation therapy. Biomaterial 135:62–73
Gillmore JD, Gane E, Taubel J et al (2021) CRISPR-Cas9 in vivo gene editing for transthyretin amyloidosis. N Engl J Med 385:493–502
Holtkamp S, Kreiter S, Selmi A et al (2006) Modification of antigen-encoding RNA increases stability, translational efficacy, and T-cell stimulatory capacity of dendritic cells. Blood 108:4009–4017
Hou X, Zaks T, Langer R et al (2021) Lipid nanoparticles for mRNA delivery. Nat Rev Mater 1–17
Hung ME, Leonard JN (2016) A platform for actively loading cargo RNA to elucidate limiting steps in EV-mediated delivery. J Extracell Vesicles 5:31027
Jayasinghe MK, Tan M, Peng B et al (2021) New approaches in extracellular vesicle engineering for improving the efficacy of anti-cancer therapies. Semin Cancer Biol 74:62–78
Kanada M, Bachmann MH, Hardy JW et al (2015) Differential fates of biomolecules delivered to target cells via extracellular vesicles. Proc Natl Acad Sci USA 112:E1433-1442
Kanada M, Kim BD, Hardy JW et al (2019) Microvesicle-mediated delivery of minicircle DNA results in effective gene-directed enzyme prodrug cancer therapy. Mol Cancer Ther 18:2331–2342
Khan MA, Yumak H, Goss DJ (2009) Kinetic mechanism for the binding of eIF4F and tobacco etch virus internal ribosome entry site RNA: effects of eIF4B and poly(A)-binding protein. J Biol Chem 284:35461–35470
Kojima R, Bojar D, Rizzi G et al (2018) Designer exosomes produced by implanted cells intracerebrally deliver therapeutic cargo for Parkinson’s disease treatment. Nat Commun 9:1305
Kong SM, Costa DF, Jagielska A et al (2021) Stiffness of targeted layer-by-layer nanoparticles impacts elimination half-life, tumor accumulation, and tumor penetration. Proc Natl Acad Sci USA 118:e2104826118
Kooijmans SA, Aleza CG, Roffler SR et al (2016) Display of GPI-anchored anti-EGFR nanobodies on extracellular vesicles promotes tumour cell targeting. J Extracell Vesicles 5:31053
Kowalski PS, Rudra A, Miao L et al (2019) Delivering the messenger: advances in technologies for therapeutic mRNA delivery. Mol Ther 27:710–728
Kowalski PS, Capasso Palmiero U, Huang Y et al (2018) Ionizable amino-polyesters synthesized via ring opening polymerization of tertiary amino-alcohols for tissue selective mRNA delivery. Adv Mater e1801151
Lee BC, Kang I, Yu KR (2021) Therapeutic features and updated clinical trials of mesenchymal stem cell (MSC)-derived exosomes. J Clin Med 10:711
Li HY, Chen Z, Ho LW et al (2017) Oligonucleotide-conjugated nanoparticles for targeted drug delivery via scavenger receptors class A: an in vitro assessment for proof-of-concept. Int J Pharm 532:647–655
Milani A, Sangiolo D, Aglietta M et al (2014) Recent advances in the development of breast cancer vaccines. Breast Cancer (dove Med Press) 6:159–168
Ohno S, Takanashi M, Sudo K et al (2013) Systemically injected exosomes targeted to EGFR deliver antitumor microRNA to breast cancer cells. Mol Ther 21:185–191
Okumura K, Nakase M, Inui M et al (2008) Bax mRNA therapy using cationic liposomes for human malignant melanoma. J Gene Med 10:910–917
Patel P, Young JG, Mautner V et al (2009) A phase I/II clinical trial in localized prostate cancer of an adenovirus expressing nitroreductase with CB1954 [correction of CB1984]. Mol Ther 17:1292–1299
Pitt JM, Andre F, Amigorena S et al (2016) Dendritic cell-derived exosomes for cancer therapy (research support, non-U.S. gov’t review). J Clin Invest 126:1224–1232
Rautio J, Kumpulainen H, Heimbach T et al (2008) Prodrugs: design and clinical applications. Nat Rev Drug Discov 7:255–270
Rosenblum D, Gutkin A, Kedmi R et al (2020). CRISPR-Cas9 genome editing using targeted lipid nanoparticles for cancer therapy. Sci Adv 6: eabc9450
Russell JE, Liebhaber SA (1996) The stability of human beta-globin mRNA is dependent on structural determinants positioned within its 3′ untranslated region. Blood 87:5314–5323
Sahin U, Kariko K, Tureci O (2014) mRNA-based therapeutics–developing a new class of drugs. Nat Rev Drug Discov 13:759–780
Savina A, Furlan M, Vidal M et al (2003) Exosome release is regulated by a calcium-dependent mechanism in K562 cells. J Biol Chem 278:20083–20090
Sedic M, Senn JJ, Lynn A et al (2018) Safety evaluation of lipid nanoparticle-formulated modified mRNA in the sprague-dawley rat and cynomolgus monkey. Vet Pathol 55:341–354
Shibamoto Y, Streffer C (1991) Estimation of the dividing fraction and potential doubling time of tumors using cytochalasin B. Cancer Re 51:5134–5138
Steinle H, Behring A, Schlensak C et al (2017) Concise review: application of in vitro transcribed messenger RNA for cellular engineering and reprogramming: progress and challenges. Stem Cells 35:68–79
Thorne SH, Barak Y, Liang W et al (2009) CNOB/ChrR6, a new prodrug enzyme cancer chemotherapy. Mol Cancer Ther 8:333–341
Tian Y, Li S, Song J et al (2014) A doxorubicin delivery platform using engineered natural membrane vesicle exosomes for targeted tumor therapy. Biomaterials 35:2383–2390
Turpin J, Ling C, Crosby EJ et al (2016) The ErbB2DeltaEx16 splice variant is a major oncogenic driver in breast cancer that promotes a pro-metastatic tumor microenvironment. Oncogene 35:6053–6064
Veerman RE, Teeuwen L, Czarnewski P et al (2021) Molecular evaluation of five different isolation methods for extracellular vesicles reveals different clinical applicability and subcellular origin. J Extracell Vesicles 10:e12128
Vogel AB, Lambert L, Kinnear E et al (2018) Self-amplifying RNA vaccines give equivalent protection against influenza to mRNA vaccines but at much lower doses. Mol Ther 26:446–455
Wahlgren J, De LKT, Brisslert M et al (2012) Plasma exosomes can deliver exogenous short interfering RNA to monocytes and lymphocytes. Nucleic Acids Res 40:e130
Wang JH, Endsley AN, Green CE et al (2016) Utilizing native fluorescence imaging, modeling and simulation to examine pharmacokinetics and therapeutic regimen of a novel anticancer prodrug (Research Support, N.I.H., Extramural). BMC Cancer 16:524
Wang JH, Forterre AV, Zhao J et al (2018) Anti-HER2 scFv-directed extracellular vesicle-mediated mRNA-based gene delivery inhibits growth of HER2-positive human breast tumor xenografts by prodrug activation. Mol Cancer Ther 17:1133–1142
Weissman D, Ni H, Scales D et al (2000) HIV gag mRNA transfection of dendritic cells (DC) delivers encoded antigen to MHC class I and II molecules, causes DC maturation, and induces a potent human in vitro primary immune response. J Immunol 165:4710–4717
Wesselhoeft RA, Kowalski PS, Parker-Hale FC et al (2019) RNA circularization diminishes immunogenicity and can extend translation duration in vivo. Mol Cell 74(508–520):e504
Wojtczak BA, Sikorski PJ, Fac-Dabrowska K et al (2018) 5’-phosphorothiolate dinucleotide cap analogues: reagents for messenger RNA modification and potent small-molecular inhibitors of decapping enzymes. J Am Chem Soc 140:5987–5999
Yang Z, Shi J, Xie J et al (2020) Large-scale generation of functional mRNA-encapsulating exosomes via cellular nanoporation. Nat Biomed Eng 4:69–83
Yang Z, Shi J, Xie J et al (2021) Author correction: large-scale generation of functional mRNA-encapsulating exosomes via cellular nanoporation. Nat Biomed Eng 5:944–945
Yu M, Levine SJ (2011) Toll-like receptor, RIG-I-like receptors and the NLRP3 inflammasome: key modulators of innate immune responses to double-stranded RNA viruses. Cytokine Growth Factor Rev 22:63–72
Zhu X, Badawi M, Pomeroy S et al (2017) Comprehensive toxicity and immunogenicity studies reveal minimal effects in mice following sustained dosing of extracellular vesicles derived from HEK293T cells. J Extracell Vesicles 6:1324730
Zou S, Scarfo K, Nantz MH et al (2010) Lipid-mediated delivery of RNA is more efficient than delivery of DNA in non-dividing cells. Int J Pharm 389:232–243
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Matin, A.C., Forterre, A. (2022). Medical Use of mRNA-Based Directed Gene Delivery. In: Jurga, S., Barciszewski, J. (eds) Messenger RNA Therapeutics. RNA Technologies, vol 13. Springer, Cham. https://doi.org/10.1007/978-3-031-08415-7_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-08415-7_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-08414-0
Online ISBN: 978-3-031-08415-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)