Abstract
Finite element models (FEM) have been a breakthrough in the field of medicine for a wide variety of applications. They have been used, for example, for predicting the behaviour of many biological structures, as well as to foresee the possible outcomes of some types of operations. One of the basic problems when modelling biological structures is finding a way to determine the initial geometric parameters with a sufficient degree of precision, so that the results are representative. In the case of computational models used for the study of corneal biomechanics, the knowledge of initial conditions defined in a finite element model become critical, since they represent the in-vivo state of the biological structure by means of a computer simulation. There is a lack of consensus among the investigations carried out to date regarding whether the initial status in the FEM models should be considered or not. In this research work, two approaches that aim to determine the geometry of the in-vivo state of the cornea with mild keratoconus have been compared: the so-called stress-free geometry on the one side, and the initial tension state on the other side. The results obtained allow comparisons between them, and validate both approaches when they are used to obtain corneal geometry in initial stress-free conditions for a FEM model when incipient keratoconus.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The cornea is a fundamental part of the human eye. It is a complex, heterogeneous, aspherical and thin tissue, which is part of the anterior part of the eye, and it is in contact with the outside environment in one of its areas. In a conventional scenario, without the presence of pathological alterations, both the anterior and posterior parts of the cornea present a very particular morphology, derived from the balance between stresses and deformations, which generate a very stable geometric surface. This geometry can be structured in-vivo by corneal tomographers [1].
In the early 1990s, following the publication of the first case of iatrogenic ectasia, a rising interest in biomechanical modelling emerged, aiming to use it to predict, by means of a numerical model developed by the Finite Element Method (FEM), the response of the cornea to various situations, such as pathological surgeries and non-surgical treatments, whether they were invasive or not [2].
The reliability of these behavioral models depends on both the fixed geometry of the cornea and the goodness of fit to the reality of the parameters that define the composition of the material at both microscopic and macroscopic levels [3]. Therefore, it would be of the highest interest determining the stress-free geometric state in the initial FEM model for incipient keratoconus.
The first works in the field of biomechanics considered asymmetric two-dimensional geometric models [4, 5]. Later approximations to corneal geometry were based on the use of different optical models, and different approaches to the basic geometry of the cornea could be adopted depending on the model being considered. In all cases, the objective is to obtain a model capable of representing the essential characteristics of the mean cornea, i.e., using as an approximation to the corneal surface a model based on a conical or biconical surface plus a residue, the so-called Navarro model [6]. However, these models do not register true specific geometry of the patient, and therefore they do not capture the defining structural irregularities of each patient, and those that are inherent to corneal pathologies.
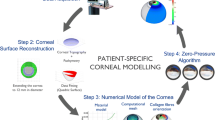
In addition, our research group has introduced the concept of “patient-specific geometry”, that consists in the development of a patient-specific 3D model that can effectively record the characteristic geometrical alterations of corneal pathologies. This model has been validated for the both the detection and diagnosis of corneal ectasia. The 3D model has recently been used for the first time in a FEM model for the characterization of corneal biomechanics [7].
As mentioned above, the reliability of the numerical simulation models used for the study of corneal biomechanics depends on the initial conditions defined in the FEM model, since they are responsible for representing the in-vivo state of the biological structure using a computer simulation. Among the investigations to date, there are differences as to whether or not to consider the initial state in the FEM models.
In this research work two approaches are compared to determine the geometry of the in-vivo state of the cornea with incipient keratoconus according to the Amsler-Krumeich classification [1], the so-called stress-free geometry and the initial stress state.
2 Materials and Methods
2.1 Participants
This study involved 12 patients aged between 19 and 61 years (38% men, 72% women).
All patients were selected, according to the Amsler-Krumiech grading, basing on the level of myopia, central keratometry, minimum pachymetry and the presence of other signs such as scars or steepening.
Inclusion criteria were: patients diagnosed as having Grade I KC eyes (up to – 5D astigmatism, ≤48D values of central mean keratometry, lack of scarring and eccentrical localized steepening).
The exclusion criteria were the following: any previous eye surgery in clinical history, ocular surface inflammation, moderate to severe dry eye or other active ocular comorbidity, or use of contact lenses within the four weeks prior to the first visit.
The participants signed an informed consent to participate in the clinical study that was carried out according to the ethical standards agreed by the Declaration of Helsinki (7th revision, October 2013, Fortaleza, Brazil).
The patients were part of the Iberia Biobank (Universidad Miguel Hernández de Elche, OFTARED-ISCIII). The study was approved by the UPCT ethics committee (CEI21_001).
2.2 Anisotropic Properties of the Cornea
Since the last century, it is well known that the human cornea is formed by a complex grouping of structured collagen fibres, that are interwoven, in a very precise way, within a matrix [2]. From a numerical point of view, the effect of considering a fibre-reinforced continuum is important, and that is why most studies in this field consider anisotropic models for their analysis. In general, there is agreement on the distribution of collagen fibres in the most important components of the human eye:
-
The cornea has two preferential directions: nasal-temporal and upper-lower
-
Limbo presents a preferential direction: circumferential
-
The sclera, for numerical purposes, is considered as an isotropic material.
2.3 Material Parameters
Through experimental test, mechanical behavior of any type of material can be characterized, an experimental study on corneal biomechanics with few test is a poorly conditioned problem [8, 9].
However, some studies promoted by some authors present a sufficient set of data to perform the study of mechanical characterization of the cornea, in our study we have considered a hyperelastic anisotropic material with incompressible behavior [10].
2.4 Meshing
To optimize the time required for calculations, as well as the quality of the solution, the right mesh size should be found. For such problems, it has been found that the mesh size based on a minimum of 4 elements thick and 6 to model the dynamic fluid coupling [10].
Finally, for the mesh the total number of elements is 1024 and 6138 nodes. The type of element used for the analysis has been SOLID186.
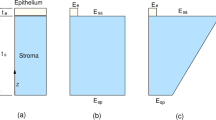
2.5 Displacement Method
This method allows obtaining the stress-free geometry by means of an iterative process, in which that geometry is firstly assumed, and then intraocular pressure is applied. The resulting geometry is compared to the geometry measured with the topographer until the difference between them two is below a certain fixed threshold.
This technique was initially proposed by A. Pandolfi and G.A. Holzapfel [11] and was later modified by Elsheikh et al. [12] basing on a loop-like iterative process. Initially, the cornea is under the influence of the intraocular pressure (IOP), being \({X}_{0}\) the coordinates of the nodes of the stressed mesh. After applying pressure equal to the IOP, the material is deformed, moving the coordinates a quantity \(u\):
so, it can be affirmed that
The process begins by assuming that the coordinates in the first iteration \({x}_{1}\), are equal to the deformed configuration, and applying a pressure equal to the PIO it can be determined the displacement field in iteration 1, \({u}_{1}\), with which can be calculated the coordinates of the deformed geometry, \({x}_{1}\) according to Eq. (3):
An overall measure of error could be estimated from the vector standard of differences between the deformed coordinates after the application of the IOP and the initial configuration, as shown in Eq. (4):
Finally, the material coordinates can be updated with the iteration in Eq. (5):
The process will end when, in iteration k, \({e}_{\mathrm{k}}\) error is
being \(\varepsilon \) a preset value between orders 10–6 and 10–9 (Fig. 1).
2.6 Pre-stress Method
The pre-stress method does not allow calculating stress-free geometry by itself. It looks for the initial pre-stress of the tissue that makes deformation almost null when the intraocular pressure is applied, and therefore the resulting geometry practically coincides with the one of the topographer. If only that stress is considered as a load once calculated, stress-free geometry can be obtained.
This methodology was proposed by E. Lanchares in 2018 [13], and is based on finding the stresses to which the cornea is subjected when the IOP is present.
The ultimate goal is to determine what is the stress field that makes nodal shifts null or, in other words, find the stress field that balances the IOP.
The algorithm of this implementation is based on solving the static problem as many times as necessary for the displacement field to be overridden.
To do this, assuming that the iterator is in iteration k > 0, then this iteration will have as inputs the following parameters:
-
The initial iteration mesh
-
The assigned IOP (about 15 mmHg)
-
The stress field solution for iteration k−1
When k = 0, the only entry will be the assigned IOP, given an initial mesh.
The natural trend is that this algorithm converges after about 20 iterations (Fig. 2).
2.7 Statistical Analysis
The statistical analysis of the outcomes obtained was performed using the software SPSS version 15.0 for Windows (SPSS, Chicago, IL). Normality of all data distributions was confirmed by means of the Kolmogorov–Smirnov test. Then, parametric statistics was always applied. Differences between X, Y and Z positions calculated with the displacement and pre-stress methods for the different point evaluated were analyzed using the paired Student t test. All statistical tests were two-tailed, and p-values less than 0.05 were considered statistically significant.
3 Results
Table 1 summarizes the results of the comparison of the simulations obtained with the two methods of simulation, displacement and pre-stress, in the keratoconus cornea grade I. As shown, significant differences between methods were only detected in the Z position of points on the anterior corneal surface (p = 0.004).
Only significant correlations of the differences in X (r = −0.288, p = 0.030) and Z (r = −0.254, p = 0.046) coordinates calculated with the displacement and pre-stress methods on the posterior corneal surface in the keratoconus grade I eye were found with the distance of location of the point evaluated (Fig. 3).
Maximum difference reached 7.32 microns per point (anterior surface). Mean value of total difference between inverse geometries calculated between methods 2.88 (standard deviation 2.00 microns).
Maximum difference reached 7.90 microns per point (posterior surface). Mean value of total difference between inverse geometries calculated between methods 0.04 (standard deviation 0.03 microns).
4 Discussion
In the field of modelling and numerical simulation of corneal biomechanics, the main objective is usually predicting the response of this structure in several different situations, whether they are invasive or non-invasive. Works can be found in the scientific literature presenting applications related with the behavior of the cornea in a healthy scenario [14], the analysis of its behavior before an ocular surgery [11], corneal structural alterations induced by physical phenomena, such as tonometry for the measurement of IOP [15], the evaluation of structural alterations before pathologies such as keratoconus [16], or even their incorporation into the biomechanical assessment of visual acuity optic models after a treatment. For all these applications, a real geometrical model of the corneal architecture must be developed, including both its anterior and posterior surfaces [1].
In a physiological state, when a biological structure is captured in-vivo, as it is the case of the cornea, it is subjected to a series of internal and external forces that force it to acquire a specific geometry, as a result of an equilibrium between them. In the case of the cornea, it is the IOP and the atmospheric pressure the ones which are balanced to generate the patient-specific geometry captured by the corneal tomographs [1].
There are discrepancies among current investigators regarding whether initial status should be considered or not. The general rule is that the problem of conditions is not mentioned, however, there are certain works that do contemplate it. To take into account the in-vivo state of the cornea two approaches can be observed: the stress-free geometry or the displacement method [11] and the initial tension state or pre-stress method [13].
Both methods present significant differences with respect to the coordinates of height Z or point of maximum curvature on the anterior surface, especially in the paracentral region, coinciding these results with those obtained by other authors on 3D models [17, 18].
With respect to the posterior face, there are no differences between both methods for the Cartesian coordinates (X, Y, Z), this behavior is aligned with the mean values of the total differences obtained between both methods for the inverse geometry, that is just 0.04 ± 0.03 microns.
With respect to the displacement method, the main advantage is that it allows to obtain the inverse geometry directly, and then the real IOP can be applied for each patient to obtain its physiological geometry (Fig. 4). Another feature of this method is that it can be implemented in any FEM code, so it does not depend on the material or the type of geometry.
With respect to the pre-stress method, it presents an important limitation, consisting in the fact that it does not allow to calculate the stress-free geometry by itself, but it carries one more step (Fig. 2) to obtain such geometry. The method allows to obtain the tension field that balances the IOP or, in other words, the stress field that makes the nodal displacements null, and consequently it entails a greater computational cost. Then, inverse geometry can be obtained from this point.
5 Conclusion
Due to the non-linearity of corneal tissues and the exponential character of the behavior curve, failure to include residual stresses or not from the stress-free geometric model in computational numeric models can lead to calculation errors.
In this study we compared two methods to obtain stress-free or inverse geometry for corneas with incipient keratoconus. Both methodologies are valid to obtain the free geometry for these pathological corneas, but the displacement method is an inverse method more agile and with lower computational cost.
References
Cavas-Martínez, F., De la Cruz Sánchez, E., Nieto Martínez, J., Fernández Cañavate, F.J., Fernández-Pacheco, D.G.: Corneal topography in keratoconus: state of the art. Eye Vis. (London, England) 3(5) (2016). https://doi.org/10.1186/s40662-016-0036-8
Ma, J., Wang, Y., Wei, P., Jhanji, V.: Biomechanics and structure of the cornea: implications and association with corneal disorders. Surv. Ophthalmol. 63, 851–861 (2018). https://doi.org/10.1016/j.survophthal.2018.05.004
Kling, S., Hafezi, F.: Corneal biomechanics - a review. Ophthalmic Physiol. Opt. J. Br. Coll. Ophthalmic Opt. (Optom.) 37, 240–252 (2017). https://doi.org/10.1111/opo.12345
Bryant, M.R., McDonnell, P.J.: Constitutive laws for biomechanical modeling of refractive surgery. J. Biomech. Eng. 118, 473–481 (1996). https://doi.org/10.1115/1.2796033
Buzard, K.A.: Introduction to biomechanics of the cornea. Refract. Corneal Surg. 8, 127–138 (1992)
Navarro, R., González, L., Hernández, J.L.: Optics of the average normal cornea from general and canonical representations of its surface topography. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 23, 219–232 (2006). https://doi.org/10.1364/josaa.23.000219
Gómez, C., Piñero, D.P., Paredes, M., Alió, J.L., Cavas, F.: Iterative methods for the biomechanical evaluation of corneal response. A case study in the measurement phase. Appl. Sci. 11, 10819 (2021)
Ariza-Gracia, M., Ortillés, Á., Cristóbal, J., Rodríguez Matas, J.F., Calvo, B.: A numerical-experimental protocol to characterize corneal tissue with an application to predict astigmatic keratotomy surgery. J. Mech. Behav. Biomed. Mater. 74, 304–314 (2017). https://doi.org/10.1016/j.jmbbm.2017.06.017
Ariza-Gracia, M.Á., Zurita, J., Piñero, D.P., Calvo, B., Rodríguez-Matas, J.F.: Automatized patient-specific methodology for numerical determination of biomechanical corneal response. Ann. Biomed. Eng. 44(5), 1753–1772 (2015). https://doi.org/10.1007/s10439-015-1426-0
Pandolfi, A.: Cornea modelling. Eye Vis. (London, England) 7, 2 (2020). https://doi.org/10.1186/s40662-019-0166-x
Pandolfi, A., Holzapfel, G.A.: Three-dimensional modeling and computational analysis of the human cornea considering distributed collagen fibril orientations. J. Biomech. Eng. 130, 061006 (2008). https://doi.org/10.1115/1.2982251
Elsheikh, A., Whitford, C., Hamarashid, R., Kassem, W., Joda, A., Büchler, P.: Stress free configuration of the human eye. Med. Eng. Phys. 35, 211–216 (2013). https://doi.org/10.1016/j.medengphy.2012.09.006
Lanchares, E., Calvo, B., Cristóbal, J.A., Doblaré, M.: Finite element simulation of arcuates for astigmatism correction. J. Biomech. 41, 797–805 (2008). https://doi.org/10.1016/j.jbiomech.2007.11.010
Alastrué, V., Calvo, B., Peña, E., Doblaré, M.: Biomechanical modeling of refractive corneal surgery. J. Biomech. Eng. 128, 150–160 (2006). https://doi.org/10.1115/1.2132368
Elsheikh, A., Wang, D., Kotecha, A., Brown, M., Garway-Heath, D.: Evaluation of Goldmann applanation tonometry using a nonlinear finite element ocular model. Ann. Biomed. Eng. 34, 1628–1640 (2006). https://doi.org/10.1007/s10439-006-9191-8
Navarro, R., Palos, F., Lanchares, E., Calvo, B., Cristóbal, J.A.: Lower- and higher-order aberrations predicted by an optomechanical model of arcuate keratotomy for astigmatism. J. Cataract Refract. Surg. 35, 158–165 (2009). https://doi.org/10.1016/j.jcrs.2008.09.015
Alifa, R., Piñero, D., Velázquez, J., Alió Del Barrio, J.L., Cavas, F., Alió, J.L.: Changes in the 3D corneal structure and morphogeometric properties in keratoconus after corneal collagen crosslinking. Diagnostics (Basel, Switzerland) 10, 397 (2020). https://doi.org/10.3390/diagnostics10060397
Toprak, I., Cavas, F., Velázquez, J.S., Alió Del Barrio, J.L., Alió, J.L.: Three-dimensional morphogeometric and volumetric characterization of cornea in pediatric patients with early keratoconus. Am. J. Ophthalmol. 222, 102–111 (2021). https://doi.org/10.1016/j.ajo.2020.09.031
Funding
This publication was carried out within the framework of the project “Desarrollo y validación de un nuevo concepto de caracterización biomecánica-morfofuncional de la córnea” reference number DTS21/00103. This Project has been funded by Instituto de Salud Carlos III (ISCIII) and cofunded by the European Union.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this paper
Cite this paper
Cavas, F., Gómez, C., Velázquez, J.S., Piñero, D., Sáez-Gutiérrez, F.L., Alió, J. (2022). Adaptative Modelling of the Corneal Architecture in a Free-of-Stress State in Incipient Keratoconus. In: Rojas, I., Valenzuela, O., Rojas, F., Herrera, L.J., Ortuño, F. (eds) Bioinformatics and Biomedical Engineering. IWBBIO 2022. Lecture Notes in Computer Science(), vol 13346. Springer, Cham. https://doi.org/10.1007/978-3-031-07704-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-07704-3_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07703-6
Online ISBN: 978-3-031-07704-3
eBook Packages: Computer ScienceComputer Science (R0)