Abstract
Over the last 15 years, the cardiological scenario has greatly changed: the increase in cardio-surgery centers and the refinement of surgical techniques have made it possible to carry out a greater number of operations with a progressive increase in children who adopt adulthood. About 85% of newborns with congenital heart disease reach that age. These patients with an entrance today in an estimated group in Italy of more than 100,000 adult subjects each year of at least 2000 patients.
It is therefore a completely new population of subjects, towards which it is necessary to structure a recovery or conditioning path, starting from the already existing dedicated cardiological rehabilitation guidelines, adapting them and adopting them to the patient suffering from congenital heart disease.
Reviews of the literature are relating to the activity of safety and validity of physics in GUCH patients.
Small improvements are highlighted in cardiorespiratory capacity, physical activity carried out independently, and in the quality of life of the patients compared to the control group. There were no serious adverse effects related to rehabilitation and set physical activity interventions. These observations support the proposition that physical activity and exercise are safe and the benefits outweigh the potential risk.
Physical exercise is therefore proposed as an ideal preventive and therapeutic means, as it is physiological, effective, safe, and at low cost.
It is necessary to look for the most appropriate tests to be performed in the immediate postoperative period, to break away from the old concept of only the recovery of Activity Day Living. All these allow a new form of “Accelerated Rehabilitation.” This is the challenge.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The World Health Organization (WHO) has defined Rehabilitation Cardiology (CR) as a multifactorial, active, and dynamic process, which aims to promote clinical stability, reduce disabilities resulting from the disease, and support the maintenance and the resumption of an active role in society, with the aim of reducing the risk of subsequent cardiovascular events, improving the quality of life and having an overall positive impact on survival. The role of Rehabilitation Cardiology has evolved a lot in the last 20 years. The first programs were developed in the 1960s–1970s following confirmation of the benefits of early mobilization during prolonged hospitalization after a coronary event.
Exercise was the main component of these programs which were essentially offered to patients who survived an uncomplicated myocardial infarction and started physical activity generally very late after the acute episode. In the years, the indications for cardiological rehabilitation have undergone important changes. The programs have also been successfully proposed to post-heart attack patients with complications or after coronary artery bypass grafting or coronary angioplasty. Finally, also as a consequence of the progressive aging of the population, the number of elderly people undergoing cardiological rehabilitation has increased considerably, many of them suffering from severe coronary artery disease, serious comorbidities, and dysautonomias. In the meantime, even the cardiological scenario of reference of our specific one has strongly changed: the increase in cardiac surgery centers and the refinement of medical-surgical techniques have made it possible to carry out a greater number of interventions with a progressive increase in children reaching adulthood. About 85% of newborns with congenital heart disease reach adulthood. These patients now constitute an estimated group in Italy of more than 100,000 subjects with at least 2000 patients entering adulthood every year.
It is therefore a completely new population of subjects, towards whom it is necessary to structure a dedicated recovery path starting from the already existing cardiological rehabilitation guidelines, adapting and perfecting them to the patient suffering from congenital heart disease. Undergoing cardiac surgery in childhood leads to a reduction in expectations, which naturally translates into a lower willingness of the patients themselves to assume an active lifestyle. The result is that the low physical activity of GUCH patients increases their predisposition to cardiovascular disease proportionally more than the general population [1].
Although the scientific literature is now full of confirmations about the benefits of physical exercise, not only in the healthy subject but also and above all in the heart disease, the recommendations issued to ACHD patients by specialized health structures do not appear adequate due to excessive fear and protection by healthcare professionals [2]. We must not forget that in people with congenital heart disease, the cardiorespiratory capacity is lower and deteriorates faster than in healthy people [3]. This has significant implications as cardiorespiratory capacity has been associated with increased mortality and morbidity [4].
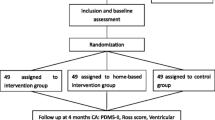
In support of the safety and goodness of physical activity in ACHDs, the recent Cochrane review is cited, which quantitatively analyzes the effects of physical activity in people with congenital heart disease [5]. This review collects randomized controlled trials that compare the following:
-
Any type of rehabilitation intervention and general physical activity, intended as the promotion of physical activity, physical training, and training of the respiratory system, with a control group “without physical activity”.
-
Which include all individuals with a diagnosis of congenital heart disease, regardless of age or previous medical interventions.
-
With a median duration of surgery of 12 weeks.
The primary outcomes of the review were as follows:
-
Cardiorespiratory capacity assessed on the basis of the oxygen peak with cardiopulmonary test on a cycle ergometer.
-
The health-related quality of life determined by the HRQoL validated questionnaire.
-
Objective measures of physical activity carried out by the patient during the day measured with a device supported by an app for continuous monitoring of movement.
Although the review highlights only small improvements in cardiorespiratory capacity, self-employed physical activity, and HRQoL of patients compared to the control group, there were no serious negative effects related to rehabilitation interventions and set physical activity. These observations support the proposition that physical activity and exercise are safe and the benefits outweigh the potential risk.
Physical exercise is therefore proposed as an ideal preventive and therapeutic means, as it is physiological, effective, safe, and at low cost.
It is fundamental to define the rational principles and the ways in which to prescribe physical activity in individual heart diseases and therefore what is the right “dose” and the correct “modality” of exercise to be recommended.
To achieve a 20% reduction in mortality, an exercise intensity is required that leads to an energy consumption of approximately 4200 kJ per week (equal to 30 mins of physical exercise per day for at least 4–5 days per week). The greatest risk reduction is achieved with moderate intensity exercise, equivalent to 3–5 h of brisk walking, 2–3 h of jogging, or 1–2 h of running per week [6].
In analogy to what happens for a drug, in order to correctly prescribe physical activity to a sedentary, healthy, or cardiopathic subject, one must know the physiology and pathophysiology of the different types of physical exercise and sport, with particular regard to acute cardiovascular effects and chronic that they involve. For this reason, the various physical and sports activities, in relation to the responses of the cardiovascular system, have been classified by the experts of the COCIS (Cardiological Committee for Fitness for Competitive Sport) starting from the following essential physiological and pathophysiological concepts:
-
1.
The cardiovascular effort can be constant over time, as in prolonged aerobic activities, or intermittent.
-
2.
The cardio-circulatory effort primarily depends on the intensity of the effort, which in turn is proportional to the metabolic demands of the muscles involved. A simple measure of metabolic intensity is the MET or Metabolic Equivalent, which expresses the amount of oxygen consumed at rest (sitting silently on a chair), equal to approximately 3.5 ml of O2/kg/min corresponding to 1.2 kcal/min for a person of 70 kg.
Compared to the calculation of the METs, an effort involving an expenditure of around 3 METS is considered of light intensity, of moderate intensity when the metabolic expenditure is between 3 and 6 METS, and of medium to high intensity when the effort involves an energy expenditure exceeding 6 METS.
-
3.
The hemodynamic response to exertion is significantly influenced by the type of exercise. In activities where the technical gesture is cyclic, for example, in walking or pedaling, the muscle strength used is generally not high. These are aerobic activities in which the muscles, when the intensity of the effort is mild to moderate (<50–60% of the maximum), mainly use the energy released by the lipids, while for higher-intensity levels, the preferential substrate is represented by carbohydrates (glycogen). From a cardiovascular point of view, they are characterized by an increase in heart rate proportional to the intensity of exertion and a prevalent peripheral vasodilation with modest or no increase in mean arterial pressure. In power activities, on the other hand, the muscles use phosphocreatine as an energy source and only part of the carbohydrates through anaerobic glycolysis, with the production of lactic acid. In this type of exercise, the cardiocirculatory response is characterized by an important elevation of the mean arterial pressure due to the increase in peripheral vascular resistance, which, although of short duration, can be harmful in hypertensive patients and patients with pathologies of the aorta.
-
4.
In terms of cardiovascular risk, the intensity of the exercise is a key factor. In fact, up to an intensity not exceeding 70–75% of the maximum, the regular practice of physical exercise is able to induce beneficial effects on the body and the cardiovascular system, without a significant increase in risk.
The incentive to a regular practice of physical exercise intended as a promotion and maintenance of health in subjects affected by congenital heart disease finds a specific application in childhood and adolescence not only for the important psychological and social aspects but also for the irreplaceable educational and training role.
What is required of the patient is to perform a certain amount of physical work in order to obtain with the lowest possible risk, an improvement in quality of life. To this end, a correct prescription of physical activity should combine two fundamental points:
-
Meet the expectations of reintegration into active life and sports.
-
Choose a physical activity and sport capable of providing benefits on the psychological and physical level with a risk of complications in the short and long term reasonably negligible or at least equal to the expected benefits.
The 2013 COCIS protocols [7, 8] devoted an entire chapter to competitive fitness criteria in the various types of congenital heart disease. Summarizing the general characters to prescribe any physical activity or sport in a child, adolescent, or young adult with congenital heart disease is necessary:
-
A precise diagnostic framing of the pathology of the definition of its severity.
-
A reasonable prediction of the possible evolution of the heart disease and of the possible impact on it of the chosen physical and sports activity.
-
The evaluation of the functional capacity of the subject, through stress tests, or better still through a cardiopulmonary test.
There is no formula for adapting the program to each individual patient. Each subject differs in physical condition and consequences of the disease, with possible sequelae (pump dysfunction ischemia arrhythmias) that make it even more necessary and even more challenging to customize the work protocol. For this purpose, it is essential, when planning the program, to consider the following elements.
-
Age.
-
Sex.
-
Risk class and associated pathologies.
-
Musculoskeletal situation.
-
Current drug therapy, particularly for drugs that may interfere with exercise response.
-
Exercise testing if available.
-
Previous exercise habits and exercise enjoyment.
-
Understanding of how the program is executed.
Prescribing an exercise program should take these four factors into account:
-
1.
FREQUENCY (F) of sessions per week
-
2.
INTENSITY (I) the amount of absolute energy expenditure during the sessions
-
3.
TYPE (T) the modality of execution
-
4.
TIME (T) the duration of the single session
-
1.
Frequency: As has already been amply reiterated, there is no one-size-fits-all. In general, the frequency of execution of the exercise program is daily, especially during the first phases of rehabilitation, and tri-weekly at home.
-
2.
Intensity: The intensity of the activity must be such as to produce an increase in physical training in proportion to the degree of tolerance to the effort and the period of time in which the immobilization determined by the acute event has lasted. The intensity of the exercise must therefore be personalized and put in relation with the duration: in fact, similar results, in terms of increase of functional capacity, can be obtained with prolonged periods at low intensity and vice versa.
Since it is not always possible to measure the patient’s VO2max, the maximum heart rate reached in the cardiopulmonary test or through an exercise test is used as a reference parameter. For the evaluation of the training intensity, the heart rate range within which to carry out the program under safe conditions (TargetHeart Rate or THR) is calculated according to:
-
The percentage of the maximum heart rate reached; if the recommendations of the American Heart Association are followed, the training is performed keeping the heart rate between 50 and 80% of the maximum rate reached; in the practice of our centers, this percentage is instead 70–85%.
-
The Karvonen formula. This method of calculation leads to a heavier program than the previous one and therefore should be reserved for uncomplicated subjects with good adaptation to the effort.
It is important to educate the patient so that he recognizes his own response to the effort by means of simple methods of self-evaluation. The most commonly used method is the measurement of pulse beats both at maximum effort and in the first minutes of recovery immediately after the interruption of exercise. Widely used is the fatigue perception scale codified by Borg (or similar like OMNI) and validated by numerous studies. In association can also be used the Borg scale of dyspnea.
-
-
3.
Type: The mode of carrying out the rehabilitation and training program can be interval training or endurance training. Intermittent exercise (interval), which can be performed both free-body and with equipment, alternates periods of work at a predetermined intensity with phases of recovery with no or very light work. The application of the workload for short periods of time determines an adaptation to the effort that is useful in the most deconditioned patients or in the elderly who do not tolerate the application of a continuous workload in the first training sessions.
The general principle of all free-body programs is to mobilize the major muscle groups, with various repetitions for a duration of 1–3 mins per exercise and with increasing commitment. It should be emphasized that there is no such thing as exercise “for the heart patient,” but calisthenics, free body, or small apparatus can be used, provided that the criteria set out in the quantification of intensity are followed.
The resistance training or continuous (endurance) is the most widely used because it allows the maximum increase in aerobic capacity, are traditionally preferred activities with a dynamic component carried out by cycle ergometers, ergometers or treadmills. Even in these cases, it is possible to provide exercises with weights and/or equipment, designed to determine an increase in muscle power. The rationale for integrating aerobic exercise with strength training derives from the observation that most human activities are characterized by both static and dynamic muscle work, in addition to contributing to work and social life activities. Strength work in the cardiopathic patient is not addressed to the development of hypertrophy and fast strength but must be aimed at the search of resistant strength with exercises, as we will see later, of low intensity, numerous repetitions and longer recovery times between series.
The mode of execution is related to the availability of equipment and risk stratification of patients: tendentially, patients at low risk and with a good tolerance to effort, after the first 2 weeks of aerobic training, can gradually begin a strengthening work with weights.
-
4.
Time: During the first phases of rehabilitation, the single training session is generally set at around 30 mins, while in the later phases and especially in home maintenance programs, the session can last up to an hour. The single session is generally organized in 10′ of warm-up, 40′ of actual training, and 10′ of fatigue or recovery. Longer periods of exercise are not warranted. The overall duration of the training program must be planned according to the objectives set for each patient: the standard protocols of the main cardiology centers in Italy and abroad provide for a minimum of 12 sessions to a maximum of 40 sessions, in periods between 2 and 8 weeks.
The progressive increase of the workload is a function of numerous variables that make it difficult to standardize a protocol. The simplest and most direct reference to regulate the progression of the program is the heart rate: the improvement of the response to the effort corresponds to a smaller increase in HR per equivalent load. This allows you to increase the workload until the target heart rate is within the set range.
Placing in a graph on the y-axis the trend of the heart rate during the rehabilitation or training session and on the x-axis the progressive increase in intensity or time of the single work session, it is possible to monitor the improvements of the cardiovascular system obtained and then customize the physical activity program.
Basically, the more the slope of the resulting line is reduced, the more the subject is trained; moreover, the greater is the cardiovascular adaptation to the effort, the lower will be the HR at the same load intensity.
The safety of physical training and the timing of initiating the rehabilitation program in the ACHD patient are a controversial topic.
Although the ability to perform prognostic stratification is now far more thorough, allowing the degree of risk of the patient to be established with sufficient sensitivity to minimize the risks potentially induced by exertion, the diversity and complexity of ACHD patients make the conclusions of the literature on the incidence of major complications during rehabilitation scarcely indicative.
On the topic of safety, attention is drawn to the following observations:
-
It is necessary to consider multiple parameters of the response to exertion: linearity of cardiac frequency progression, body pressure (BP) behavior, ECG recovery phase, and patient’s perception of fatigue.
-
It is advisable to follow carefully the adaptation to the effort in the initial sessions of the program, in which the physical deconditioning or the difficulty in learning the pattern of execution of the exercise can determine an abnormal increase in heart rate (HR) and BP.
-
It is recommended to adapt the modalities and the type of exercise to the physical capacities and motor aptitudes of the subject, up to a total customization of the program.
-
It is necessary to be able to count on a staff (rehabilitation therapists, physiatrists, cardiologists, cardiac surgeons) specifically trained and updated and able to recognize those situations that require the immediate suspension of exercise (e.g., appearance of angina or complex arrhythmias), while in the case of subjective sensation of fatigue or exceeding the CF of training is sufficient to reduce the workload or lengthen the recovery time between exercises.
-
What has been stated above outlines the basis for the design and execution of a standard protocol of physical activity for cardiac patients and for heart patients.
The rehabilitation program is part of a therapeutic intervention whose main objective is to improve the quality of life, the subject’s perception of his own state of health, independently of the actual clinical conditions. The resumption of motor activity and the consolidation of a better tolerance to effort obtained through training play a decisive role in maintaining a condition as close as possible to the “state of health,” and this is all, the more important, the more precarious the physical, psychological, or social situation of the patient. It is therefore understandable that rehabilitation, and physical exercise as the central expression of the program, has a privileged position for the categories of patients most compromised, and therefore at greater risk of poor quality of life, which until a few years ago were excluded from rehabilitation itself because they were considered at high risk.
In practice, Cardiac Rehabilitation should take place in stages.
Phase 1 applies to hospitalized patients, often with a combination of low- to medium-intensity exercise, stress management techniques, and risk factor education programs. The program in this phase aims to ensure that the patient is discharged with the best possible physical and psychological conditions, with all possible information on a healthy lifestyle.
Phase 2, in which the exercise program is further individualized in terms of intensity, duration, frequency, type, and progression, as well as constant monitoring, is aimed at returning to social and professional activities. In some situations, cardiovascular rehabilitation can be performed on an outpatient basis.
Advantages of outpatient rehabilitation:
-
Recovery in the usual environment.
-
Involvement of the family in lifestyle adjustments.
-
Assumption of greater self-responsibility without the fixed rules of a hospital.
-
Ability to perform regular physical activity in a family environment.
-
Disadvantages of outpatient rehabilitation:
-
Danger of reexposing oneself too soon to professional and social stress.
-
Less rigorous surveillance, so this type of rehabilitation is not for everyone.
In a rehabilitation center, the patient is assisted individually by the interdisciplinary team. The most important element is the physical activity program appropriate to the patient’s efficiency.
Advantages of rehabilitation with permanence:
-
No professional or domestic stressful situations.
-
Global assistance.
-
Thanks to continuous surveillance, more demanding physical activities are possible.
Disadvantages of rehabilitation with permanence:
-
Separation from family and the usual environment for a few weeks.
-
Less involvement of the family in lifestyle adjustments.
-
The rules of the rehabilitation center with permanence reduce self-responsibility.
Phase 3 may or may not follow the previous one. Improving the physical condition is the main goal as well as improving the quality of life.
Phase 4, following long-term programs, has the main objective of increasing and maintaining physical fitness. Activities are not necessarily controlled, and sufficient time should be available for maintaining the exercise program and preference for recreational sports activities.
REHABILITATION does not mean “letting oneself be assisted,” but actively dealing with the experience with the disease, hospitalization, and learning what is good for the body.
2 Phases 1 and 2
Cardiac rehabilitation programs aim at the physical, social, and psychological improvement of individuals, and studies show the reduction of anxiety and depression [9]. During immediate postoperative hospitalization (Phase 1), physiotherapy aims to avoid the negative effects of prolonged bed restraint, stimulates a quick return to daily activities, maintains functional capacity, develops patient confidence, reduces psychological impact, maximizes the chances of early discharge, and provides the foundation for a home program [10].
In Italy, the majority of congenital patients, after surgery, do not have access to cardio-specialist rehabilitation courses. This is mainly due to an excess of protection and uncertainty about how to carry out such rehabilitation, which in turn translates into an encouragement to a sedentary lifestyle, and to the further uncertainty about what physical activity and at what intensity it should be recommended.
The cardiopulmonary stress test (CPT) represents the gold standard for a correct drafting of the Individual Rehabilitation Project with specific target intensity.
But in the immediate postoperative period, the limitations given by sternotomy and restrictive respiratory dysfunction make it impossible to use a CPT because it would in any case be interrupted prematurely.
Added to this was the impossibility of being able to perform it during the COVID emergency, a circumstance that however allowed us to reconsider some evaluation methods [11].
To evaluate the functional capacity of each individual patient, stratify it in a correct training profile and create a targeted intervention in the absence of a CPT, some physical performance tests (field tests) can be used.
Among the most used we mention:
-
Six-minute walking test (6MWT) [12], a test that is not strictly standardized as it is influenced by the patient’s cooperation and by the level of encouragement (which takes place every 60 seconds) and requires a lot of space (corridor length). It has a moderate correlation with the VO2 peak. It can underestimate the performance in patients with a moderate level of cardiovascular fitness. It can be a valid alternative to CPT in more compromised patients.
-
Incremental shuttle walk test (ISWT) [12]. The patient is asked to walk along a 10-m path marked by cones at the pace defined by an acoustic signal that increases the pace every minute. The patient, unlike the 6MWT, is not encouraged and ends when the cone is not reached or when symptoms occur. Being an incremental test, it correlates better to peak VO2 than 6MWT. Producing a cardiovascular response more similar to CPT, it is a valid alternative for assessing exercise tolerance.
-
Step test [13,14,15]. One needs only a step or another solid surface as well as a method of counting time and tracking steps.
-
Gait speed test (GST) [16]. It accesses an individual’s functional mobility. It is simple to perform, and it requests minimal space, equipment, and time.
-
Sit to stand (STS) [16]. It is a way to access in individual’s legs strength and endurance by having them stand up from a sitting position repeatedly over the course of the seconds of the test.
-
Short physical performance battery (SPPB) [17], a short battery of tests to evaluate the functional capabilities essential for the autonomy and performance of the lower limbs.
-
Time up and go (TUG) [18]. It is the time that an individual uses to stand up from a sitting position, walking for 3 meters, turning of 180°, come back, and sit down.
Some test batteries were developed and validated as correlations of the underlying fitness domains, while others were developed and validated as predictors of disability and hospitalization. Making them requires little space, equipment, and costs; they can be administered by nonmedical personnel with minimal training. They are considered extremely safe in patients with clinical conditions to compensate.
The most used are excellent screenings of functional limits associated with a worse state of health.
They help in assessing the functional status of patients, especially at certain points in their medical history.
3 Exercise Prescription
The general principles of exercise prescription apply to adults of all ages. The relative adaptations to exercise and the rate of improvement of the components of physical fitness are important for maintaining health, functional capacity, and mitigating many of the physiological changes associated with congenital heart disease.
Low aerobic capacity, muscle weakness, and deconditioning are more common in this type of patient, and therefore the prescription should include aerobic, muscle-strength-endurance, and flexibility exercises. They may also benefit from specific neuromotor exercises to improve balance, agility, and proprioceptive training (Tai Chi Chuan), in addition to the other components of health-related fitness. Age should never be a barrier because positive improvements are possible at any age.
Physical exercise DOSE is defined as the total sum of energy expended, determined by the intensity, frequency, and duration of the activity performed. The MET is the most used unit of measurement which, multiplied by the duration and frequency of the exercise, provides the total sum of the energy expended. This is one of the most popular ways to identify the “dose.” But in reality, it does not take into account individual variability, such as the different subjective effort between a trained patient and a deconditioned one. It is therefore difficult to identify a volume of physical activity that can be standardized for each individual person.
For performing adults, moderate-intensity and vigorous-intensity exercises are defined as such compared to METs, with moderate-intensity activities defined as 3–5 and vigorous-intensity activities such as ≥6 METs. Conversely, for more deconditioned adults, activities should be defined in relation to physical fitness in the context of a perception scale of physical exertion (Borg or OMNI). Moderate intensity exercise should produce a minimal increase in heart rate (HR) and breathing, while one of vigorous intensity should produce a large increase in HR and breathing.
Considerations that should be made to maximize the effective development of an exercise program in deconditioned patients are:
-
Increase muscle strength before you are physiologically able to engage in aerobic training.
-
Intensity and duration of exercise should be mild at the beginning.
-
The progression of the exercise should be personalized and adapted to tolerance and preferences; a conservative approach may be necessary for patients who are severely deconditioned or physically limited.
-
If the clinical conditions prevent activity at the minimum recommended amount, the exercise must be performed “within tolerance.”
-
The initial load should be light (<3 MET), and the workload increases in the order of 0.5–1 MET.
It is desirable, after a correct stratification of patients, to apply the principle of “accelerated rehabilitation” and to start physical conditioning as soon as possible. Patients already deconditioned in the preoperative period or those who have undergone longer surgical times will hardly be able to tolerate training times longer than 10 mins in the immediate postoperative period: in these cases, it is useful to divide the treatment into at least two daily sessions. Once hemodynamic stability has been reached, the patient must be guided to use a pedal mini bike to be performed in the room even without supervision in order to create a “training volume effect” during the day.
Subsequently, the stepper (10–20 cm high step), a low-cost and easily transportable tool, usable in supervision, allows an infinite range of training and combinations of exercises. Initially performed slowly and for a few repetitions, it retrains strength, balance capacity, and, over the course of the days, it can be combined with numerous other exercises before and after the climb. The patient must be able at discharge to climb the stairs to return home. It is a tool that can also be used at home.
During training, in the absence of CPT performed, the rate of ascent of the heart rate must always be monitored, and with what progression, it is increased. Peripheral saturation control oxygen, blood pressure, Borg scale dyspnea (0–10), and perceived exertion (6–20) or alternatively Omni scale [19] are always monitored.
4 Phases 3 and 4
The reduced physical performance resulting from a sedentary lifestyle represents one of the most important negative predictors for the state of health: in fact, poor tolerance to effort is associated with a significant increase in mortality.
In the first two phases, in the absence of contraindications, the objectives include “preparing” the patient to tolerate an aerobic training [20, 21] with a training phase lasting at least 20–30 mins. Considered the minimum level recommended by the guidelines, each program should be customized so that each patient does not only perform the type of physical activity preferred but that the modalities are those that are best suited to his degree of physical performance. It is useful to create structured protocols calibrated on the patient’s level of availability, designed to help practice physical activity in daily life. Goals should be attainable and quantifiable by the patient himself, reinforcing successes and preventing dropouts. The message that must be conveyed is that physical activity must be promoted and must have the same importance as any other therapeutic treatment, and, to be effective, it must be done regularly throughout life.
The physical activity of aerobic resistance (endurance training), of light or moderate intensity (150 mins per week), can be divided into five weekly sessions of 30 mins and can be added to the activities of daily life if lasting more than 10 mins.
As for muscle strength training, when indicated, it can be trained two times a week, associated with aerobic activity, with 8–10 exercises for the main muscle groups in the number of 8–12 repetitions per exercise. These exercises should be performed without tearing and without holding breath to avoid pressure spikes.
Create groups of physical activity, associations between patients, forums on the Internet, applications, or anything that the construction of a “network” can give as an aid to the execution and continuation of the physical conditioning program.
In the third millennium, it would be desirable to create digital media, for the optimization of the prescription, the control of the activities carried out, and the timely resolution of any critical issues. The development of applications that can be easily downloaded on a telephone or computer would allow the patient not only to have indications on the type of training to be performed, but interacting with it could obtain instant variations on the workloads and the type of exercises to be performed, as well as see the objectives achieved and above all, by creating a feedback with the interdisciplinary pool that follows him, perform “remotely” (perhaps in supervision with video call) the functional tests used during the hospital stay. It should be remembered that various hospitals during 2020–2021 were forced to use this method to follow the changes in the clinical and fitness conditions of COVID patients previously undergoing physiotherapy during hospitalization after weeks [22, 23].
References
Gierat-Haponiuk K, Haponiuk I, Jaworski R, Chojnicki M, Szalewska D, Leszczyńska K, et al. Physical activity in patients with grown-up congenital heart defects after comprehensive cardiac rehabilitation. Kardiochir Torakochirurgia Pol. 2014;4:452–8.
Williams CA, Gowing L, Horn R, Stuart AG. A survey of exercise advice and recommendations in United Kingdom paediatric cardiac clinics. Cardiol Young. 2017;27(5):951–6.
Amedro P, Gavotto A, Guillaumont S, Bertet H, Vincenti M, De La Villeon G, et al. Cardiopulmonary fitness in children with congenital heart diseases versus healthy children. Heart. 2018;104(12):1026–36.
Udholm S, Aldweib N, Hjortdal VE, Veldtman GR. Prognostic power of cardiopulmonary exercise testing in Fontan patients: a systematic review. Open Heart. 2018;5(1):e000812.
Williams CA, Wadey C, Pieles G, Stuart G, Taylor RS, Long L. Physical activity interventions for people with congenital heart disease. In: Cochrane Heart Group, editor. Cochrane Database of Systematic Reviews [Internet]; 2020. [cited 2022 Feb 1];2021(5). Available from: http://doi.wiley.com/10.1002/14651858.CD013400.pub2.
Sesso HD, Paffenbarger RS, Lee I-M. Physical activity and coronary heart disease in men: the Harvard alumni health study. Circulation. 2000;102(9):975–80.
Biffi A, Delise P, Zeppilli P, Giada F, Pelliccia A, Penco M, et al. Italian Cardiological guidelines for sports eligibility in athletes with heart disease: part 1. J Cardiovasc Med. 2013;14(7):477–99.
Delise P, Guiducci U, Zeppilli P, D’Andrea L, Proto C, Bettini R, et al. Cardiological guidelines for competitive sports eligibility. Ital Heart J. 2005;6(8):661–702.
Sharif F, Shoul A, Janati M, Kojuri J, Zare N. The effect of cardiac rehabilitation on anxiety and depression in patients undergoing cardiac bypass graft surgery in Iran. BMC Cardiovasc Disord. 2012;12(1):40.
de Regenga M. Fisioterapia em Cardiologia: da Unidade de Terapia Intensiva à Reabilitação. São Paulo: Roca SaúdeProfissional.
Holland AE, Malaguti C, Hoffman M, Lahham A, Burge AT, Dowman L, et al. Home-based or remote exercise testing in chronic respiratory disease, during the COVID-19 pandemic and beyond: A rapid review. Chron Respir Dis. 2020;17:147997312095241.
Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428–46.
de Andrade CHS, Cianci RG, Malaguti C, Dal CS. The use of step tests for the assessment of exercise capacity in healthy subjects and in patients with chronic lung disease. J braspneumol. 2012;38(1):116–24.
Balfour-Lynn IM, Prasad SA, Laverty A, Whitehead BF, Dinwiddie R. A step in the right direction: assessing exercise tolerance in cystic fibrosis. Pediatr Pulmonol. 1998;25(4):278–84.
Shitrit D, Rusanov V, Peled N, Amital A, Fuks L, Kramer MR. The 15-step oximetry test: a reliable tool to identify candidates for lung transplantation among patients with idiopathic pulmonary fibrosis. J Heart Lung Transplant. 2009;28(4):328–33.
Puthoff ML, Saskowski D. Reliability and responsiveness of gait speed, five times sit to stand, and hand grip strength for patients in cardiac rehabilitation. Cardiopulm Phys Ther J. 2013;24(1):31–7.
Puthoff ML. Outcome measures in cardiopulmonary physical therapy: short physical performance battery. Cardiopulm Phys Ther J. 2008;19(1):17–22.
Nordin E, Lindelöf N, Rosendahl E, Jensen J, Lundin-Olsson L. Prognostic validity of the timed up-and-go test, a modified get-up-and-go test, staff’s global judgement and fall history in evaluating fall risk in residential care facilities. Age Ageing. 2008;37(4):442–8.
Haile L, Gallagher MJ, Robertson R. Perceived exertion laboratory manual: from standard practice to contemporary application [Internet]. New York, NY: Springer; 2015. [cited 2022 Feb 1]. Available from: http://springerlink.bibliotecabuap.elogim.com/10.1007/978-1-4939-1917-8
Doyle MP, Indraratna P, Tardo DT, Peeceeyen SC, Peoples GE. Safety and efficacy of aerobic exercise commence dearly after cardiac surgery: a systematic review and meta-analysis. Eur J Prev Cardiolog. 2019;26(1):36–45.
Duppen N, Etnel JR, Spaans L, Takken T. Van denBerg-Emons RJ, Boersma E, et al. does exercise training improve cardiopulmonary fitness and daily physical activity in children and young adults with corrected tetralogy of Fallot or Fontan circulation? A randomized controlled trial. Am Heart J. 2015;170(3):606–14.
Turquetto ALR, dos Santos MR, Agostinho DR, Sayegh ALC, de Souza FR, Amato LP, et al. Aerobic exercise and inspiratory muscle training increase functional capacity in patients with univentricular physiology after Fontan operation: a randomized controlled trial. Int J Cardiol. 2021;330:50–8.
Houchen-Wolloff L, Daynes E, Watt A, Chaplin E, Gardiner N, Singh S. Which functional outcome measures can we use as a surrogate for exercise capacity during remote cardiopulmonary rehabilitation assessments? A rapid narrative review. ERJ Open Res. 2020;6(4):00526–2020.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Baroni, B., Girelli, D. (2022). Rehabilitation’s Point Break: Changing for Improving. In: Flocco, S.F., Habibi, H., Dellafiore, F., Sillman, C. (eds) Guide for Advanced Nursing Care of the Adult with Congenital Heart Disease. Springer, Cham. https://doi.org/10.1007/978-3-031-07598-8_14
Download citation
DOI: https://doi.org/10.1007/978-3-031-07598-8_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07597-1
Online ISBN: 978-3-031-07598-8
eBook Packages: MedicineMedicine (R0)