Abstract
Obstructive sleep apnea (OSA) is a heterogeneous disease with many physiological implications. OSA is associated with a great diversity of diseases, with which it shares common and very often bidirectional pathophysiological mechanisms, leading to significantly negative implications on morbidity and mortality. In these patients, underdiagnosis of OSA is high. Concerning cardiorespiratory comorbidities, several studies have assessed the usefulness of simplified screening tests for OSA in patients with hypertension, COPD, heart failure, atrial fibrillation, stroke, morbid obesity, and in hospitalized elders.
The key question is whether there is any benefit in the screening for the existence of OSA in patients with comorbidities. In this regard, there are few studies evaluating the performance of the various diagnostic procedures in patients at high risk for OSA. The purpose of this chapter is to review the existing literature about diagnosis in those diseases with a high risk for OSA, with special reference to artificial intelligence-related methods.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Obstructive sleep apnea
- Comorbidities
- Diagnosis
- Polysomnography
- Respiratory event
- Sleep staging
- Home sleep apnea testing
- Screening
- Decision support system
- Artificial intelligence
- Machine learning
1 Introduction
Obstructive sleep apnea (OSA) is a chronic, complex, and heterogeneous respiratory disease of high prevalence in the general population, with important health consequences. OSA is associated with a great diversity of diseases. In the clinical evaluation of these patients cardiorespiratory, cerebrovascular, and metabolic comorbidities potentially linked with OSA should be investigated (Bonsignore et al., 2019; Marin-Oto et al., 2019). It shares common and very often bidirectional pathophysiological mechanisms, which have significant implications on morbidity and mortality. The most frequent comorbidities are found in the vascular field, respiratory or metabolic among others. Associated diseases vary according to sex, being more frequent in patients with a higher severity of OSA.
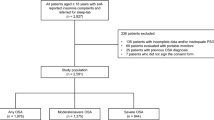
Table 4.1 shows the most frequent comorbidities in which screening studies have been performed due to the high possibility of presenting OSA. In these patients, underdiagnosis of OSA is high. There are many reasons for this, including the fact that these patients often do not present with daytime sleepiness or the usual symptoms of OSA. Moreover, the symptoms of the disease themselves often mask the presence of OSA. Added to this is the fact that there is little diagnostic suspicion on the part of the physician (Costa et al., 2015). Hence the importance of early diagnosis in order to initiate treatment as soon as possible. In most of these comorbidities, the treatment of OSA is a therapeutic objective in itself, as it acts as a risk factor.
The key question is whether there is any benefit in the screening for the existence of OSA in patients with comorbidities. Currently, there are not enough studies to establish the existence of a benefit in the general asymptomatic population (Jonas et al., 2017; Rosen et al., 2017). Given the high frequency of OSA in these diseases with the possible benefit of treatment, the need for diagnostic studies in these patients can be assumed. However, some authors advocate the need to confirm the benefits of treatment through randomized studies, especially in relation to CPAP treatment, as a step prior to the need for screening (Sanchez-de-la-Torre et al., 2021, Kee et al., 2018). Moreover, there are few studies evaluating the performance of the various diagnostic procedures in patients at high risk for OSA (Treptow et al., 2015).
Table 4.2 summarizes the main approaches to the abbreviated diagnosis of OSA in the presence of comorbidities using simplified tools. Among the level IV procedures, pulse oximetry has been one of the most exhaustively studied biological signals for screening. Table 4.3 shows the characteristics of the main approaches to OSA diagnosis in patient with comorbidities based on the analysis of pulse oximetry. Biomedical signal processing techniques and artificial intelligence-based tools have hardly been applied to evaluate their usefulness in the group of diseases where there is a high risk of associated OSA.
The purpose of this chapter is to review the existing knowledge regarding diagnosis in those diseases with a high risk for OSA, with special reference to artificial intelligence-related methods.
2 Chronic Obstructive Pulmonary Disease (COPD)
Both COPD and OSA are two very prevalent diseases in the general population, which are associated with high morbidity, especially in the area of cardiovascular disease. Their association has been widely described in the literature. Both diseases are characterized by low-grade inflammation (Zamarrón et al., 2008). Their association increases morbimortality and the costs associated with them, which makes it necessary to maintain an integral vision of the patient, being able to identify both diseases early and optimize their control (Jelic, 2008). The use of CPAP in these patients has been shown to reduce mortality (Marin et al., 2010).
Despite the high prevalence of its association, nocturnal polysomnography is not routinely recommended in COPD patients. In the same regard, spirometry is not routinely performed in clinical practice in patients with OSA.
As in the rest of the comorbidities, the diagnosis of OSA is often underestimated even though these patients often present symptomatology in relation to sleep quality. Gunduz found in his study that 58% of patients with COPD and no symptoms had OSA (Gunduz et al., 2018).
Nocturnal polysomnography would be indicated in patients with COPD in the presence of excessive daytime sleepiness, observed nocturnal apneas, morning headache as well as if cor pulmonale or polycythemia is present (McNicholas, 2017). Similarly, the presence of clinical deterioration disproportionate to pulmonary function, with the presence of excessive daytime sleepiness, polycythemia, or pulmonary hypertension with a baseline PaO2 greater than 60 mmHg point to the diagnosis of OSA. Recently, the American Thoracic Society in its clinical guidelines on non-invasive ventilation in patients with COPD and chronic hypercapnic respiratory failure recommends that before starting ventilation it is necessary to perform an OSA screening using the STOP-BANG questionnaire (Macrea et al., 2020).
The most optimal method of diagnosing OSA in these patients is not determined (Malhotra et al., 2018). Very different clinical questionnaires have been used for the prediction of OSA in COPD patients: Epworth, STOP-BANG, Berlin Questionnaire, and Sleep Apnea Clinical Score. Most of them include small population sizes, presenting poor performance with high sensitivity and moderate specificity.
Thus, in a study carried out in a Chinese population using the Berlin and STOP-BANG questionnaires, the sensitivity and specificity achieved was similar to that obtained in patients without COPD (Wu et al., 2020), although greater diagnostic accuracy was obtained in patients with less pulmonary involvement measured in terms of forced expiratory volume in 1 second (FEV1) or forced vital capacity (FVC). Xiong et al., compared the diagnostic performance of various questionnaires in 335 patients with COPD and OSA, finding that the questionnaire with the best performance was the Berlin questionnaire (Xiong et al., 2019). Particularly, for an AHI >15 events/h, they obtained a sensitivity of 77.6%, and a specificity of 55% and an area under the receiver operating characteristics curve (AUC) equal to 0.737. The specificity was higher in patients with severe OSA.
Arsian et al., in a comparative study of the usefulness of various questionnaires (Berlin, STOP-BANG and Epworth) in patients with suspected OSA, evaluated the impact of various comorbidities in 1003 patients, finding that the STOP-BANG showed the highest sensitivity and the highest PPV (97% and 91.4%, respectively) (Arsian et al., 2020). The STOP-BANG showed high sensitivity in the group of patients with comorbidities (hypertension, diabetes mellitus, coronary artery disease, COPD, asthma), while notably lower values of specificity were reached with respect to the group without comorbidity (Arsian et al., 2020).
Other authors have evaluated the symptoms of OSA themselves in the development of other predictive models. Thus, the study by Soler et al. does not show that clinical features such as male sex, body mass index (BMI), or neck circumference are relevant in the prediction of OSA in these patients (Soler et al., 2017) Other authors, such as Faria et al., were interested in a new predictive model called Sleep Apnea Clinical Score and randomly applied it to 24 patients with COPD referred to PSG, in order to assess both the BQ and the Epworth sleepiness scale. They reported that their predictive model had a better diagnostic performance, with an AUC of 0.82, higher than that obtained by the other questionnaires. In addition, a sensitivity close to 60% was obtained, although in this study the STOP-BANG was not included (Faria et al., 2015).
There are very few studies that evaluated the usefulness of respiratory polygraphy in patients with COPD. Oliveira et al., in one of the first studies in this regard, evaluated the usefulness of a respiratory polygraphy (Stardust) in patients with COPD (Oliveira et al., 2012). The study was initially performed in 72 patients, in GOLD stages II and III, but due to difficulties during enrollment, finally only 26 patients were included, which implied the presence of a high failure rate. The intra-class correlation coefficient (ICC) between the AHI derived from the respiratory polygraphy and that from standard PSG was 0.61 (0.28–0.8) in the hospital setting and 0.47 (0.11–0.72) at the patient’s home. Graphical analysis showed a tendency to overestimate the AHI in mild cases and underestimate it in the more severe ones. The authors conclude that there is insufficient significant evidence to support the use of this diagnostic procedure in these subgroups of patients.
For the same aim, Chang et al. evaluated 90 patients diagnosed with COPD with a high probability of OSA who underwent home polygraphy (NoxT3) followed by a one-week in-hospital polysomnographic and polygraphic recording (Chang et al., 2019). The home study showed good agreement with the AHI and the rest of the studies, especially in the most severe cases. The authors reported 95% sensitivity, 78% specificity, 88% positive predictive value (PPV), and 89% negative predictive value (NPV) compared to PSG, with a kappa coefficient of 0.746 for an AHI >5 events/h. The failure rate was 5.6%. The CT90 obtained was higher in polygraphic recordings, both at home and in the hospital. The authors highlight the usefulness of these systems in patients with COPD, whose results are similar to those obtained in patients without comorbidity. Additionally, they reported similar results between manual and automatic analyses. The same equipment has been used for this purpose in the presence of various comorbidities: psychiatric diseases, stroke, ischemic heart disease, chronic kidney disease, and others, obtaining an underestimation of severity in each of the groups of diseases, finding a greater dispersion in relation to the concordance of NOX-T3 and polysomnography (To et al., 2021).
The usefulness of peripheral arterial tonometry in patients with COPD versus polysomnography was evaluated by Holmedahl et al. in 16 patients with COPD (Holmedahl et al., 2019). Concerning sleep staging, they obtained an accuracy of 63% and an agreement of 0.418 kappa, while an ICC of 0.957 (CI95% 0.878–0.985) was reached for the AHI estimation task. It is noticeable that the concordance was lower than that previously obtained in control patients and OSA (lower specificity). However, the accuracy for AHI was adequate. One of the limitations of the study was the small sample size, as well as its inability to differentiate between central and obstructive apneas.
Jen et al. evaluated the usefulness of the WatchPAT system with respect to polysomnography in 33 patients diagnosed with COPD (Jen et al., 2020). WatchPAT is a new device that records the peripheral arterial tone (PAT), heart rate, oximetry, actigraphy, position, snoring, and chest movements. It shows good agreement with the AHI, unaffected by the severity of lung function. The WatchPAT system overestimated total sleep and REM sleep time. The agreement with polysomnography was 78.8%, with an overestimation of the AHI in 18.2% of the cases, concluding that the WatchPAT is a good alternative test in patients with COPD for a severe-to-moderate degree of OSA. In patients with an AHI >15 events/h, they obtained a sensitivity of 92.3% and a specificity of 65%. A cut-off point of 20 events/h allowed for the same degree of severity, a sensitivity of 76.9%, and a specificity of 90%. Its main difficulty lies when the events are very close in time.
The role of nocturnal oximetry as an aid in the diagnosis of OSA in patients with COPD presents important limitations, because of the desaturations linked to COPD that these patients present during sleep. However, it has the advantage of being easy to access, being one of the tools most widely used as a screening test in patients with suspected of OSA. (Del Campo et al., 2018). Therefore, the design and validation of automated techniques for OSA detection based on unsupervised oximetry at home is justified in the context of COPD patients, which can benefit from an early therapy by means of CPAP.
One of the first approaches to the diagnostic utility of nocturnal oximetry in the diagnosis of OSA in patients with respiratory diseases was performed by Pépin et al. (1991). These authors attempted to evaluate the diagnostic behavior of the delta index in different respiratory diseases. The number of COPD patients included in the study was notably small (only eight subjects), which significantly limits the generalizability of their results. The value of the delta index obtained in patients with COPD was very low compared to other respiratory diseases also analyzed in the study, although they obtained a high and more balanced sensitivity-specificity pair.
Scott et al. sought to develop a strategy to interpret nocturnal pulse oximetry and evaluate its ability to detect OSA in patients with stage 3 and 4 COPD (Scott et al., 2014). Consecutive COPD patients referred for simultaneous oximetry and polysomnography were studied. Patients were diagnosed with OSA if the polysomnographic AHI was >15 events/h. These criteria consisted of visually identifying oximetry “events” (sustained desaturation ≥4% in 1 hour time scale), “patterns” (≥ 3 similar desaturation cycles/15 minutes time scale), and the automated oxygen desaturation index (ODI). AUC, sensitivity, specificity, and accuracy were computed. Of the 59 patients (27 males), 31 had OSA (53%). Among these 59 patients, 35 were correctly identified as having OSA corresponding to an accuracy of 59%, with a sensitivity and specificity of 59% and 60%, respectively. The AUC was 0.57 (CI95%: 0.55 to 0.59). Using a computerized software for scoring desaturation events (hypoxemia ≥4% for ≥10 s) and using a cutoff of ≥15 events/h (of sleep time) for diagnostic criteria, the sensitivity was 60%, the specificity 63%, and the AUC was 0.64 (CI95% 0.62–0.66) (Scott et al., 2014). Interpretation of pulse oximetry tracing was of modest diagnostic value in identifying OSA in patients with moderate to severe COPD.
Lajoie et al., within the INOX clinical trial (multicenter, randomized, double-blind, placebo-controlled trial of nocturnal oxygen therapy in patients with COPD and nocturnal oxygen desaturation), performed a polysomnography on those desaturating patients who presented a cyclic desaturation pattern suggestive of OSA, confirming the existence of OSA in 50% of the patients and concluding that the oximetry tracing is not useful (Lajoie et al., 2020). However, the study was performed in a small sample population and with particular constraints.
In one of the few existing studies applying machine learning techniques, Andrés et al. evaluated the usefulness of an automated diagnostic algorithm for OSA diagnosis in COPD patients based on nocturnal oximetry. They extracted statistical, spectral, and nonlinear characteristics from the oximetry signal, which fed a regression multilayer perceptron (MLP) artificial neural network aimed at estimating the AHI, both in the hospital and at home (Andrés-Blanco et al., 2017). The algorithm was validated in patients with and without COPD. A high ICC was obtained both in the hospital (0.937 vs. 0.936) and at the patient’s home (0.731 vs. 0.788). For an AHI >15 events/h, the algorithm reached 87.3% and 86.8% accuracy in patients with and without COPD in the supervised hospital setting, respectively, while it reached 78.2% and 75% at home. It is concluded that an algorithm based on a MLP neural network model can be a good, simplified test in patients with moderate-to-severe OSA regardless of the presence of associated COPD.
Another area of interest, given the implications between OSA and the different comorbidities, is the diagnosis of these conditions in patients referred for OSA (Bar et al., 2021). This is the case of Levy et al., who tried to identify the presence of COPD using nocturnal oximetry in patients undergoing diagnostic PSG due to clinical suspicion of OSA on the basis that very often these patients are underdiagnosed (Levy et al., 2021). The study was performed in 350 patients, 70 of whom had COPD. Clinical and oximetric characteristics were used as input to the automated algorithm. Both logistic regression and random forest were assessed for this task. The random forest model obtained an AUC of 0.94 and a F1 score of 0.89.
COPD, like other respiratory comorbidities, may need continuous monitoring of CO2. Often the presence of hypoventilation is not easily evidenced in these patients. The measurement of CO2 in exhaled air (end-tidal CO2) has become a reliable diagnostic method to assess the presence of hypoventilation during sleep in these patients (Mayer et al., 2017).
3 Cardiovascular Diseases
Several studies have shown the existence of a high prevalence of OSA in patients with cardiovascular disease, estimated at 40–60%, although the prevalence varies depending on the type of cardiovascular disease. Despite this, as in the rest of the comorbidities, OSA is very often underdiagnosed (Costa et al., 2015), mainly because these patients do not present the usual symptoms. Given the high prevalence of OSA in cardiovascular diseases together with the benefits of treatment, it is useful to design and assess abbreviated tests for these patients (McEvoy et al., 2016).
A recent scientific statement by the American Heart Association regarding OSA and cardiovascular disease (Yeghiazarians et al., 2021) recommends the following indications for screening for OSA: resistant/poorly controlled hypertension, pulmonary hypertension, and recurrent atrial fibrillation after cardioversion or ablation. Screening for the presence of symptoms was recommended as well in the following situations: heart failure, tachy-brady syndrome, sick sinus syndrome, ventricular tachycardia, survivors of sudden cardiac death, and stroke. Likewise, as future research directions and areas of research, it should be highlighted the use of artificial intelligence and machine learning for the processing and identification of actionable data in OSA patients and the development of personalized therapies (Gutierrez-Tobal et al., 2019).
3.1 Atrial Fibrillation
Atrial fibrillation is one of the most prevalent arrhythmias in the general population. It is highly frequent in patients with OSA (Traaen et al., 2020), both in men and women, with a prevalence ranging from 49% to 62%. Both entities share common pathophysiological mechanisms of a complex nature. It is accepted that treatment with CPAP can reduce recurrences of these episodes, especially in patients with episodes of paroxysmal atrial fibrillation, although most of these studies are observational (Youssef et al., 2018). It is important to know that atrial fibrillation is currently a common reason for consultation in sleep units, which demands further analysis.
OSA is considered a modifiable risk factor by most clinical guidelines, recommending its screening in a broad sense (Calkins et al., 2017), although it is not clearly specified how and when the sleep study should be indicated. The European Cardiology Society recommends screening for OSA in patients with asymptomatic AF before initiating rhythm control treatment such as catheter ablation (Hindricks et al., 2021), although its implementation in clinical practice is not established. For other authors, screening would be justified in patients with AF if the patient had an episode of stroke or suffer from recurrent arrhythmias (Marulanda-Londoño & Chaturvedi, 2017). In this regard, there is great interest in determining the most optimal option for diagnosing these patients (Kadhim et al., 2020), as well as optimizing their diagnosis and treatment, given that very often there is a lack of coordination between cardiologists and sleep units (Desteghe et al., 2021).
OSA is frequently underdiagnosed in patients with AF. As with other comorbidities, it is always necessary to ask patients about symptoms related to sleep-disordered breathing. Several questionnaires have been used for screening (BQ, STOP-BANG, Non-OSA), although these questionnaires have not been validated in this population (Genta et al., 2017; Mohammadieh et al., 2021), being considered of little value as a screening method as they have a low negative predictive value and a low specificity (Ranjan, 2020). A main limitation is the absence of somnolence in these patients, so that the application of the Epworth test will provide a low sensitivity. The Berlin questionnaire shows high sensitivity (86–100%) but lower specificity (30–89%). In 579 patients with AF, Traaen et al. reported a sensitivity of 84% and specificity of 45% using the STOP-BANG, with respiratory polygraphy as a diagnostic method (Traaen, 2020). The authors attributed the lower performance to the lack of drowsiness reported by these patients.
In one of the few comparative studies, May et al. evaluated the efficacy of these questionnaires in patients with atrial fibrillation with respect to a control group, with polysomnography being the reference method (May et al., 2020). They included 150 patients in each of the groups. The authors assessed the Epworth, STOP-BANG, BQ, and NoSAS questionnaires, as well as a new model based on snoring, age, neck circumference, and BMI. In both groups, the clinical questionnaires showed worse performance in patients with AF, except for the STOP-BANG. Thus, in the presence of AF they obtained an AUC of 0.75 (CI95% 0.66–0.86) and 0.79 using the NoSAS, for an AHI> 15 events/h as cutoff for clinical diagnosis. The inclusion in the model of clinical variables such as neck circumference, BMI, snoring, and age improves the results obtained by the STOP-BANG. The model reached a sensitivity of 45% and a specificity of 97% for an AHI> 15 events/h. The inclusion of physiological variables such as heart rate or left atrial volume did not improve the performance of model.
Starkey et al. tried to evaluate the usefulness of the Berlin and NoSAS questionnaires, as well as a technique called acoustic pharyngometry, in 188 patients using the ApneaLink as a diagnostic method (Starkey et al., 2021). They concluded that the questionnaires were not useful to predict OSA in these patients. With the same purpose, Delesie et al. evaluated the usefulness of these questionnaires in 100 patients referred to study for atrial fibrillation, to whom a polysomnographic study was performed (Delesie et al., 2021). None of them showed sufficient discriminative ability (OSA50, BQ, STOP-BANG, MOODS, SACS, and Epworth), with an AUC <0.70 in the detection of severe OSA. In these patients, Abumuamar et al. also found that these questionnaires present low specificity (Abumuamar et al., 2018).
With respect to the use of respiratory polygraphy, its diagnostic accuracy is not as clearly established as in studies performed with oximetry, which makes it necessary to search for accurate and validated techniques (Hendricks, 2020). Thus, Linz et al. performed in-hospital polysomnography independent of clinical suspicion in 439 patients, subsequently obtaining the oximetry signal from the PSG (Linz et al., 2018). The prevalence of severe-to-moderate OSA was 33.9%. The authors evaluated the performance of the desaturation index using a new automatic algorithm that takes into account resaturation after desaturation in order to increase specificity. For AHI >15 events/h, they found an AUC of 0.951(0.929–0.972), while 0.932 was reached for an AHI >30 events/h. With a desaturation index cutoff point of 4.1, they obtained a sensitivity of 91% and a specificity of 83% for an AHI >15 events/h, thus being useful to rule out the disease, showing a negative predictive value of 95%.
Mohammadieh et al. evaluated the usefulness of various clinical questionnaires and the value of the oximetry tracing extracted from a respiratory polygraph (apnea-link) performed at the patient’s home in a series of 98 patients referred for AF (Mohammadieh et al., 2021). In this study, the ODI showed excellent diagnostic accuracy for an AHI >5 events/h, with an AUC of 0.874. Similarly, using the automated scoring tool, the ApneaLink reached 0.925 AUC for moderate and 0.925 AUC for severe OSA.
In a multicenter study, Tauman et al. evaluated the usefulness of automatic analysis with WatchPAT versus PSG in 101 patients with AF (Tauman et al., 2020). He obtained a good correlation, as well as 88% sensitivity and 63% specificity, with 0.89 PPV and an AUC of 0.85 for a cutoff of AHI >15 events/h. A kappa agreement of 0.42 was obtained with respect to sleep phases, being higher in the absence of AF episodes during the night. There were no significant differences neither in relation to the persistence or not of episodes of AF during the night nor concerning medication.
In these patients, the use of new generation implanted pacemakers has been used to assess the presence of OSA by incorporating a respiratory monitoring algorithm, although one of its drawbacks is the inability to assess the duration of apneas. A recent meta-analysis evaluated 5 cohort studies using the measurement derived from transthoracic impedance provided by various electronic devices and Holters, in order to assess its usefulness in screening for OSA (Wyckmans et al., 2021), being of particular interest in patients with severe OSA. In the same regard, Gonçalves et al. achieved a diagnosis of 62% in 81 patients who underwent pacemaker implantation, reporting an AUC 0.76 and a sensitivity of 78% (Gonçalves et al., 2019). Algorithms implemented in implanted defibrillators (apnea scan system) have also been used for this aim. Thus, in 25 patients with AF, Defaye et al. obtained an ICC of 0.67 (CI 95% 0.39–0.84) with respect to polysomnography. For a cut-off point of 30 events/h, they obtained a sensitivity of 100% and a specificity of 80% (Defaye et al., 2019).
This type of device has also proven usefulness in monitoring AF patients, especially those for whom OSA is not evident in the first study. An example of monitoring is the non-contact biomotion radar sensor (SleepMinder™; ResMed) that allows monitoring over long periods of time and has been used in the evaluation of patients with atrial fibrillation or in patients with heart failure.
3.2 Chronic Ischemic Heart Disease
In chronic ischemic heart disease, clinical questionnaires do not accurately predict the presence of OSA in the patients. Szymanski et al. used a model for the identification of risk factors in the development of OSA based on clinical parameters. In their model, they use logistic regression based on clinical and echocardiographic data from patients who have suffered an acute myocardial infarction (Szymanski et al., 2015). Their model takes into account left ventricular diastolic diameter, interventricular septal thickness, diagnosis of hypertension, BMI, and diastolic pressure, all of which are independent risk factors for a high risk of OSA, reaching 0.87 AUC.
3.3 Chronic Heart Failure
OSA is highly prevalent in patients with heart failure, estimated at 47–76%. It is accepted that the association between OSA and heart failure has implications in the prognosis of the disease (Valika & Costanzo 2017), being frequent in the presence of both central and obstructive apneas. Various societies such as the American College of Cardiology (ACC), the American Heart Association (AHA), and the Heart Failure Society of America have pointed out in their respective guidelines the importance of diagnosing the existence of a sleep-disordered breathing and initiating the correct treatment in these patients (Yancy et al., 2017). Screening in these types of patients has been performed in two contexts: in the stable phase or during hospital admission because of an exacerbation, the latter being considered a good opportunity, although the performance of screening methods in these patients is widely debated (Series, 2015).
The Epworth sleepiness scale, Stop-Bang, and the Berlin questionnaire have been used as the main screening questionnaires. Parisot et al. proposed a clinical scale in which age, BMI, the New York Heart Association (NYHA) scale, and sex are combined to help identify OSA in patients with heart failure using multivariate logistic regression (Parisot et al., 2015). For an AHI ≥ 5 events/h, they obtained 78.9% sensitivity, 61.5% specificity, and an AUC of 0.73.
Type III polygraphs have been shown to be useful in these subjects, both in patients hospitalized for exacerbation and in chronic forms. In one of the first studies, Quintana-Gallego et al. evaluated the usefulness of home polygraphy in 75 patients with heart failure who underwent hospital polysomnography and respiratory polygraphy in a randomized way over a period of 30 days (Quintana-Gallego et al., 2004). For an AHI cutoff point >5 events/h, the diagnostic accuracy was 78.6%, while for an AHI>15 events/h the sensitivity was 68.4% and the specificity 94.6%. On the other hand, respiratory polygraphy was able to detect the presence of both central and obstructive apneas (Quintana-Gallego et al., 2004).
De Vries et al. used the ApneaLink device in 90 patients with stable chronic heart failure, using home polysomnography as a reference (De Vries et al., 2015). These authors obtained an ICC of 0.85 (0.78–0.90) with a kappa coefficient of 0.59 for classification into the common degrees of OSA severity using automated scoring with ApneLink. For an AHI >15 events/h, the sensitivity obtained was 92.9% and the specificity 91.9%. In this study, the AHI was overestimated in more than two-thirds by the portable device, considering its usefulness just to rule out the disease (De Vries et al., 2015).
Araujo et al. used the ApneaLink in 35 patients with heart failure, simultaneously performing a PSG as reference (Araujo et al., 2018). Using a cutoff of AHI >15 events/h, they obtained a sensitivity of 83.3%, specificity of 91.3%, accuracy of 88.6%, and 0.93 AUC. For values above AHI >20 events/h, automated scoring with the ApneaLink showed a trend towards underestimate. The authors found greater efficacy in patients with more severe OSA (Araujo et al., 2018).
Similarly, Aurora et al. evaluated the usefulness of this portable sleep monitoring in 57 patients admitted for heart failure. They reported a significant performance, with 95.8% sensitivity and 80% specificity, obtaining better results in relation to central apneas (Aurora et al., 2018).
Li et al. used a type 3 equipment to identify the different respiratory events in 84 patients admitted for exacerbation of heart failure. For an AHI >5 events/h, they reported a sensitivity of 86.7%, specificity of 76.5%, and a PPV of 92.9%. The equipment used was able to identify both obstructive and central apneas, as well as Cheyne-Stokes respiration (Li et al., 2021).
Sharma et al. performed a prospective study in a population composed of 105 patients admitted for heart failure who underwent simultaneous high-resolution oximetry and respiratory polygraphy (ApneaLink) as a reference method (Sharma et al., 2017). The presence of OSA was confirmed in 87% of the sample. For an ODI of 5 events/h, the sensitivity was 89.8%, specificity 50%, and accuracy 83%. In patients with an AHI >30 events/h, sensitivity remained high and specificity increased to 87.6%. However, saturation values differed between methods, probably due to the use of different oximeters (Sharma et al., 2017).
Central sleep apneas are frequent in patients with heart failure, and there are hardly any studies that evaluate the usefulness of simplified diagnostic approaches in this type of apneas. Thus, polysomnography continues to be the reference diagnostic method in this context. However, it is advisable for this type of equipment to use inductive plethysmography bands for the detection of respiratory effort. Within the simplified procedures, such as ApneaLink, an algorithm for Cheyne-Stokes breathing detection using the flow cannula is available. Using this algorithm, the recognition of this respiratory pattern achieved a sensitivity of 87% and a specificity of 94% (Weinreich et al., 2009). These same authors used spectral entropy to automatically detect this pattern (Weinreich et al., 2008). Similarly, the usefulness of detecting the presence of Cheyne-Stokes respiration by means of neural networks based on the spectral analysis of oximetry has been described, obtaining also a high performance. Using respiratory polygraphy, Li et al. obtained a sensitivity of 94.6% for the detection of Cheyne-Stokes respiration (Li et al., 2021).
In its initial design, the WatchPAT system did not have the possibility of identifying the presence of central apneas, an aspect of particular importance in diseases such as heart failure, where patients may present central sleep apnea. This device currently has a specific module for the identification of central apneas. Accordingly, in a recent multicenter study performed in 11 centers that included 84 patients with heart failure and/or atrial fibrillation, correlations higher than 0.8 were reached for both AHI and central AHI, obtaining in the latter case 67% sensitivity, 100% specificity, 100% PPV, and 94.7% NPV for an AHI >15 events/h, with a kappa index of 0.77 (Pillar et al., 2020).
Concerning the use of machine learning approaches, artificial neural networks have been applied to identify certain respiratory patterns, such as the presence of Cheyne-Stokes respiration, using a probabilistic neural network based on spectral analysis, oximetric indices, and the delta index (El-Solh et al., 2003; Weinreich et al., 2008).
4 Cerebrovascular Diseases
In a systematic review by Dong et al., an overall prevalence of OSA in patients with cerebrovascular disease was found to be 61.9% (Dong et al., 2018). In this framework, OSA is considered an independent risk factor for stroke. Treatment with CPAP reduces the risk of suffering a stroke episode, as well as having a beneficial effect on sleepiness, quality of life, and blood pressure control. However, its efficacy on the occurrence of new events is in doubt, as the researchers of the SAVE study found no evidence of a reduction in events including stroke episodes (McEvoy et al., 2016).
The high prevalence and possible treatment implications in these patients (Seiler et al., 2019) have led various scientific societies, such as the American Heart Association-American Stroke Association, to publish secondary stroke prevention guidelines in order to recommend that patients with ischemic stroke or transient ischemic attack (TIA) should consider an OSA assessment for diagnosis (Kleindorfer et al., 2021). However, these recommendations have hardly been implemented in clinical practice or accepted by all societies (Warner et al., 2019). In a study involving a total of 1000 patients, only 17% were offered a sleep test (Brown et al., 2020) and were hardly asked about symptoms related to OSA within the first 3 months. Unfortunately, the guidelines on this subject have not changed significantly. This emphasizes the need for randomized studies to ascertain the benefits of CPAP in these types of patients.
The study of the association between sleep apnea and stroke has been carried out both at the hospital level in the acute phase (Huhtakangas et al., 2019) and in the follow-up of these patients, although in the latter case the prevalence of OSA may be overestimated.
Clinical questionnaires have not been shown to be useful as screening methods in patients who have had a stroke (Sico et al., 2017; Takala et al., 2018), since they have moderate sensitivity and low specificity. Other authors even question the need for a pretest questionnaire given the high pretest probability of OSA in patients with cerebrovascular disease.
Several questionnaires have been used in these types of patients, mainly the Berlin and the Stop-Bang questionnaires (Boulos et al., 2016; Senaratna et al., 2017). Some authors have proposed modifications to the Stop-Bang questionnaire (Boulos et al., 2019) to increase its diagnostic performance, removing the neck circumference item due to its low impact in these patients, and incorporating oxygen saturation values, either ODI4% or presenting an oxyhemoglobin saturation < 88%, which added one point to the questionnaire. For their study, Boulos et al. used either polysomnography or the ApneaLink at home in 231 patients. For an AHI >15 events/h and a cutoff point of 3 desaturations, they obtained a sensitivity of 98.5%, but a very low specificity of 23%, although the diagnostic performance was superior to that of the questionnaire. This is a consequence of the absence of somnolence and obesity in these patients.
Katzan et al. retrospectively assessed a modification of the Stop-Bang questionnaire in patients who had previously undergone the questionnaire and polysomnography (Katzan et al., 2016). In 208 patients, they created six logistic regression-based predictive models, obtaining better results with the use of continuous variables than with dichotomous variables as in the STOP-BANG. The authors found high sensitivity in all the automated models, while low specificity. The proposed model was able to detect 14% more patients with OSA.
Similarly, the development of predictive models based on logistic regression has been attempted by other authors (Siarnick et al., 2021). Thus, Siarnik et al. included clinical and echocardiographic characteristics, such as BMI, diastolic dysfunction, and history of wake-up stroke onset, as input variables to a model, which was applied to 120 stroke patients. The proposed model reached a sensitivity of 82.9%, a specificity of 71.9%, and an AUC of 0.81 in patients with severe-to-moderate OSA. The performance was lower for central apneas (Siarnick et al., 2021).
Sico et al. developed a new model (sleep inventory) based on symptoms and anthropometric measurements, using home polysomnography as a reference (Sico et al., 2017). This model achieved an AUC of 0.73, failing to classify 25% of patients. It reached high sensitivity and very low specificity both in development and validation stages.
Respiratory polygraphy is a good alternative to polysomnography in these patients (Boulos et al., 2021; Bravata et al., 2017; Saletu et al., 2018), although it is necessary to select the appropriate diagnostic procedure. Using the SOMNOcheck polygraph for detecting moderate-to-severe OSA, Kepplinger et al. found a sensitivity of 94.7% in 61 patients with mild ischemic accidents (Kepplinger et al., 2013). Similarly, in the context of a rehabilitation unit, Saletu et al. only studied those patients who presented a positive result in the polygraphy, so he eventually assessed 33 patients, reporting a good concordance in the Bland-Altman plot (Saletu et al., 2018).
Boulos et al. conducted a comparative study in 250 post-stroke patients randomized to home study versus PSG (Boulos et al., 2021), although 94 patients were included in the group of home sleep apnea test and 71 in the polysomnography group. They found a higher prevalence of OSA in the group of patients who underwent a home study, with a higher proportion of patients with CPAP being more cost-effective.
Huhtakangas et al. assessed the feasibility of OSA screening in the acute phase of ischemic stroke using automatically and manually scored cardiorespiratory polygraphy (Huhtakangas et al., 2019). A diagnosis of OSA was confirmed in 111 (59.3%) out of 187 subjects. Automated scoring properly identified respiratory events. A high agreement was obtained (ICC = 0.869), being inferior for central and mixed apneas.
In a multicenter, prospective study conducted in 1330 patients who presented an ischemic stroke, Brown et al. found a prevalence of 67%. They used machine learning algorithms to build different models for automated diagnosis (Random Forests, Boosted Regression Models, XGBoost, Deep Learning and Stacked Ensembles) (Brown et al., 2019). One of the limitations of the study is that the reference test is the ApneaLink. For an AHI >10 events/h and by means of a Random Forest approach, they reached an AUC of 0.75, correctly classifying 72.5% of the validation samples. Superior performance was achieved compared to that obtained with a logistic regression and the rest of the algorithms assessed, but the gain was small, showing AUC ranging 0.68–0.73. The most important variables in the model were neck circumference, BMI, waist circumference, age, NIHSS, and pre-stroke daytime sleepiness (Brown et al., 2019).
Oximetry has been widely used in these patients. In patients recovering from stroke, ODI4% provided a sensitivity of 77% and a specificity of 100% in patients with moderate-to-severe OSA (Aaronson et al., 2012). In the same regard, Lin et al. studied 254 patients undergoing an ApneaLink study, showing that an ODI <5 ruled out the disease and an ODI >5 confirmed moderate-to-severe OSA for an RDI >15 events/h, with a specificity of 96.4% (Lin et al., 2018). However, they did not perform polysomnography as reference standard.
Siarnick et al. evaluated the usefulness of pulse oximetry in 420 patients with acute stroke (Siarnik et al., 2020). A control polysomnography was conducted, although the proportion of patients performing both tests was low. With an ODI-based cutoff point of 15.3, the authors found a sensitivity of 90.5%, specificity of 75% for moderate-to-severe OSA, correctly classifying 81.6% with an AUC of 0.86 (CI95% 0.76–0.97) (Siarnik et al., 2020).
Boulos et al. extracted the oximetry from either the PSG or the ApneaLink in 231 patients who had a stroke in the previous year (Boulos et al., 2016). The STOP-BANG was performed as abbreviated test as well. A score < 3 achieved the highest sensitivity, while 4 led to the highest specificity. They included in the STOP-BANG questionnaire certain oximetric values, improving the performance of this tool, being capable of identifying both high- and low-risk patients. It is important to note that the authors removed the neck circumference item from the questionnaire (Boulos et al., 2016).
Although deep learning techniques have been applied in the field of sleep-disordered breathing (Vaquerizo-Villar et al., 2021), they have been scarcely used in patients with additional comorbidities. Bernardini et al. proposed an algorithm based on ECG and saturation monitoring obtained from unselected patients, to which they applied a convolutional-based deep-learning framework to detect apneas events (Bernardini et al., 2021). The authors validated their algorithm in 30 patients using in-laboratory polysomnograpy as reference.
Leino et al. used the oximetric recording as input to an algorithm also based on a convolutional neural network and they assessed its usefulness as a screening test for OSA in patients with cerebrovascular disease (Leino et al., 2021). The algorithm was previously developed in patients without cerebrovascular disease, while the authors proposed to assess its generalizability in these types of patients. The design group was composed of 1379 oximetry recordings obtained by means of a home polygraph (Embletta) and validated in 77 patients admitted for ischemic stroke or TIA who underwent a polygraph study, as well as in 394 patients with suspected OSA. A 4% drop in hypopneas was used instead of the common 3% decrease. The deep-learning model was trained to estimate the respiratory event index (REI). The agreement was close to 80% in the classification by degree of severity, although it was higher in the suspected OSA group. Errors in REI estimation appeared in apneas without desaturation. The main inconvenience is that central apneas, which are frequent in these patients, are not estimated. The ICC was 0.982 in patients with OSA and 0.972 in cerebrovascular disease patients, being the sensitivity and specificity high in both groups and in all degrees of severity. A correct classification of the categories was obtained in 88.3% and 77.9%, although the accuracy was better in the OSA suspicion group for a cutoff point of AHI >15 events/h. The sensitivity was 97.3% and the specificity 98.6% in the first group, while 92.3% sensitivity and 96.1% specificity were achieved in the second group.
Capnography monitoring has been used as a screening method for OSA in stroke patients. Dziewas et al. (2005) found a significant correlation between the AHI estimated from capnography and that derived from respiratory polygraphy. Assessing a population composed of patients with an AHI >15 events/h and using a cutoff point of 5 events/h for the estimated AHI from capnography, they achieved 100% positive predictive value, 86% negative predictive value, 87% sensitivity, and 100% specificity. Nevertheless, a trend to overestimation was observed.
All these studies have great heterogeneity in terms of design and timing of the disease, while the post-stroke data underestimate the true prevalence.
5 Diabetes
OSA is frequently associated with type 2 diabetes mellitus. It is estimated that 55%–85% of patients with this type of diabetes have also concomitant OSA (Tahrani et al., 2015). Several studies have shown that OSA contributes to the presence of glucose intolerance and the development of insulin resistance, hindering its control and leading to the appearance of vascular complications (Lindberg et al., 2012). The influence of CPAP treatment on glucose metabolism is not well known. The studies found in the literature report contradictory findings, although better results are linked with long-term therapy. Currently, there is a lack of evidence concerning the potential benefit of screening for OSA in these patients. Nevertheless, it is accepted to perform a diagnostic test in those patients showing symptoms (Donovan et al., 2017), although the most appropriate diagnosis method is not clearly established. In one of the few studies in this context, Chen et al. analyze the diagnostic ability of nocturnal oximetry derived from standard PSG along with other clinical variables in 440 patients with diabetes. The authors report a high diagnostic accuracy (AUC 0.94) for an ODI >5 events/h, with a sensitivity of 92% and a specificity of 73%, while for an ODI >25 events/h the sensitivity was 93% and the specificity 85% (Chen et al., 2021). Kurinami et al. (2018) analyze body composition data obtained via electrical bioimpedance of 186 patients with decompensated type 2 diabetes mellitus who required admission. They obtained an AUC of 0.70, with a great imbalance in the sensitivity-specificity pair (27.1% vs. 90.5%). In addition, the presence of OSAS was confirmed using a conservative diagnostic threshold (RDI >19 events/h). The use of clinical questionnaires (STOP-BANG, Berlin) shows no difference among them in terms of performance, being their overall diagnostic capacity suboptimal.
References
Aaronson, J. A., van Bezeij, T., van den Aardweg, J. G., van Bennekom, C. A. M., & Hofman, W. F. (2012). Diagnostic accuracy of nocturnal oximetry for detection of sleep apnea syndrome in stroke rehabilitation. Stroke, 43, 2491–2493.
Abumuamar, A. M., Dorian, P., Newman, D., & Shapiro, C. M. (2018). The Stop-Bang questionnaire shows an insufficient specificity for detecting obstructive sleep apnea in patients with atrial fibrillation. Journal of Sleep Research, 27, 1–7.
Andrés-Blanco, A. M., Alvarez, D., Crespo, A., Arroyo, A., Cerezo, A., Gutierrez Tobal, G., et al. (2017). Assessment of automated analysis of portable oximetry as a screening test for moderate-to-severe sleep apnea in patients with chronic obstructive pulmonary disease. PLoS One, 12(11), e0188094.
Araujo, I., Marques, F., Andre, S., Araujo, M., Marques, S., Ferreira, R., et al. (2018). Diagnosis of sleep apnea in patients with stable chronic heart failure using a portable sleep test diagnostic device. Sleep & Breathing, 22(3), 749–755.
Arsian, B. O., Hosgor, Z. Z., & Orman, M. N. (2020). Which screening questionnaire is best for predicting obstructive sleep apnea in the sleep clinic population considering age, gender, and comorbidities? Turkish Thoracic Journal, 21(6), 383–389.
Aurora, R. N., Patil, S. P., & Punjabi, N. M. (2018). Portable sleep monitoring for diagnosing sleep apnea in hospitalized patients with heart failure. Chest, 154(1), 91–98.
Bar, N., Sobel, J. A., Penzel, T., Shamay, Y., & Bejar, J. (2021). From sleep medicine to medicine during sleep. A clinical perspective. Physiological Measurement, 42, 044006.
Bernardini, A., Brunello, A., Gigli, G. L., Montanari, A., & Saccomanno, N. (2021). AIOSA: An approach to the automatic identification of obstructive sleep apnea events based on deep learning. Artificial Intelligence in Medicine, 118, 102133.
Boulos, M. I., Colelli, D. R., Vaccarino, S. R., Kamra, E., Murray, B. J., & Swartz, R. H. (2019). Using a modified version of the "STOP-BANG" questionnaire and nocturnal oxygen desaturation to predict obstructive sleep apnea after stroke or TIA. Sleep Medicine, 56, 177–183.
Boulos, M. I., Kamra, M., Colelli, D. R., Kirolos, N., Gladstone, D., Boyle, K., et al. (2021). SLEEP SMART (Sleep Apnea Screening Using Mobile Ambulatory Recorders After TIA/Stroke): A randomized controlled trial. Stroke, 53, 710.
Boulos, M. I., Wan, A., Im, J., Elias, S., Frankul, F., & Atalla, M. (2016). Identifying obstructive sleep apnea after stroke/TIA: Evaluating four simple screening tools. Sleep Medicine, 21, 133–139.
Bonsignore, M. R., Baiamonte, P., Mazzuca, E., Castrogiobavvi, A., & Marrone, O. (2019). Obstructive sleep apnea and comorbidities: A dangerous liaison. Multidisciplinary Respiratory Medicine, 14, 8.
Bravata, D. M., McClain, V., Austin, C., Ferguson, J., Burrus, N., Miech, E. J., et al. (2017). Diagnosing and managing sleep apnea in patients with chronic cerebrovascular disease: A randomized trial of a home-based strategy. Sleep & Breathing, 21, 713–725.
Brown, D. L., He, K., Kim, S., Hsu, C.-W., Case, E., Chervin, R. D., et al. (2020). Prediction of sleep-disordered breathing after stroke. Sleep Medicine, 75, 1–6.
Brown, D. L., Jiang, X., Li, C., Case, E., Sozener, C. B., Chervin, R. D., et al. (2019). Sleep apnea screening is uncommon after stroke. Sleep Medicine, 59, 90.
Calkins, H., Hindricks, G., Cappato, R., Kim, Y. H., Saad, E. S., Aguinaga, L., et al. (2017). 2017 HRS/EHRA/ECAS/ APHRS/SOLAECE expert consensus statement on catheter and sugical ablation of atrial fibrillation. Heart Rhythm, 14(10), e275–e244.
Costa, L. E., Uchoa, C. H. G., Harmon, R. R., Bortolotto, L. A., LorenFiho, G., & Drager, L. F. (2015). Potential underdiagnosis of obstructive sleep apnea in the cardiology outpatient setting. Heart, 101(16), 1288–1292.
Chang, Y., Xu, L., Han, F., Keenan, B. T., Kneeland-Szanto, E., Zhang, R., et al. (2019). Validation of the Nox-T3 portable monitor for diagnosis of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. Journal of Clinical Sleep Medicine, 15(4), 587–596.
Chen, L., Tang, W., Wang, C., Chen, D., Gao, Y., Ma, W., et al. (2021). Diagnostic accuracy of oxygen desaturation index for sleep-disordered breathing in patients with diabetes. Frontiers in Endocrinology, 12, 598470.
Del Campo, F., Crespo, A., Cerezo-Hernández, A., Gutiérrez-Tobal, G. C., Hornero, R., & Álvarez, D. (2018). Oximetry use in obstructive sleep apnea. Expert Review of Respiratory Medicine, 12(8), 665–681.
Defaye, P., Mendelson, M., Tamisier, R., Jacon, P., Venier, S., Arnold, N., et al. (2019). Validation of an apnea and hypopnea detection algorithm implemented in implantable cardioverter defibrillators. The AIRLESS study. Scientific Reports, 9, 9597.
Delesie, M., Knaepen, L., Hendrikcs, B., Huygen, L., Verbraeken, J., Weytjens, K., et al. (2021). The value of screening questionnaires/scoring scales for obstructive sleep apnoea in patients with atrial fibrillation. Archives of Cardiovascular Diseases. https://doi.org/10.1016/j.acvd.2021.08.002
Desteghe, L., Hendricks, J. M. L., Heidbuchel, H., Potpara, T. S., Lee, G. A., & Linz, D. (2021). Obstructive sleep apnoea testing and management in atrial fibrillation patients: A joint survey by the European heart rhythm association (EHRA) and the Association of Cardiovascular Nurses and Allied Professions (ACNAP). Europace, 23(10), 1667–1674.
De Vries, G. E., Van der Wal, H. H., Kerstjens, H. A. M., Van Deursen, V. M., Stegenga, B., Van Veldhuisen, D. J., et al. (2015). Validity and predictive value of portable two channel sleep screening tool in the identification of sleep apnea in patients with heart failure. Journal of Cardiac Failure, 21, 848–855.
Dong, R., Dong, Z., Liu, H., Shi, F., & Du, J. (2018). Prevalence, risk factors, outcomes, and treatment of obstructive sleep apnea in patients with cerebrovascular disease: A systematic review. Journal of Stroke and Cerebrovascular Diseases, 27(6), 1471–1480.
Donovan, L. M., Rueschman, M., Weng, M., Basu, N., Dudley, K. A., Bakker, J. P., et al. (2017). Effectiveness of an obstructive sleep apnea screening and treatment program in patients with type 2 diabetes. Diabetes Research and Clinical Practice, 134, 145–152.
Dziewas, R., Hopmann, B., Humpert, M., Böntert, M., Dittrich, R., Lüdemann, P., et al. (2005). Capnography screening for sleep apnea in patients with acute stroke. Neurological Research, 27, 83–87.
El-Solh, A. A., Magalang, U. J., Mador, M. J., Dmochowski, J., Veeramachaneni, S., Saberi, A., et al. (2003). The utility of neural network in the diagnosis of Cheyne-stokes respiration. Journal of Medical Engineering & Technology, 27, 54–58.
Faria, A. C., da Costa, C. H., & Rufino, R. (2015). Sleep apnea clinical score, Berlin questionnaire, or Epworth sleepiness scale: Which is the best obstructive sleep apnea predictor in patients with COPD? International Journal of General Medicine, 8, 275–281.
Genta, P. R., Drager, L. F., & Lorenzi-Filho, G. (2017). Screening for obstructivesleep apnea in patients with atrial fibrillation. Sleep Medicine Clinics, 12, 99–105.
Gonçalves, I. S., Agostinho, J. R., Silva, G., Guimarães, T., Bernardes, A., Santos, I., et al. (2019). Accuracy and utility of a pacemaker respiratory monitoring algorithm for the detection of obstructive sleep apnea in patients with atrial fibrillation. Sleep Medicine, 61, 88–94.
Gunduz, C., Basoglu, O. K., & Tasbakan, M. S. (2018). Prevalence of overlap syndrome in chronic obstructive pulmonary disease patients without sleep apnea symptoms. The Clinical Respiratory Journal, 12(1), 105–112.
Gutierrez-Tobal, G. C., Alvarez, D., Crespo, A., Del Campo, F., & Hornero, R. (2019). Evaluation of machine-learning approaches to estimate sleep apnea severity from at-home oximetry recordings. IEEE Journal of Biomedical and Health Informatics, 23(2), 882–892.
Hendricks, J. M. (2020). Screening for obstructive sleep apnoea in patients with atrial fibrillation: Much more than a screening tool alone. IJC Heart Vasc, 31, 100655.
Hindricks, G., Potpara, T., Dagres, N., Arbelo, E., Bax, J. J., Blomström, C., et al. (2021). 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). European Heart Journal, 42, 373–498.
Holmedahl, N. H., Fjeldstad, O. M., Engan, H., Saxvig, I. W., & Gronli, J. (2019). Validation of peripheral arterial tonometry as tool for sleep assessment in chronic obstructive pulmonary disease. Scientific Reports, 9, 19392.
Huhtakangas, J. K., Huhtakangas, J., Bloigu, R., & Saaresranta, T. (2019). Unattended sleep study in screening for sleep apnea in the acute phase of ischemic stroke. Sleep Medicine, 65, 121–126.
Jelic, S. (2008). Diagnostic and therapeutic approach to coexistent chronic obstructive pulmonary disease and obstructive sleep apnea. International Journal of COPD, 3, 269–275.
Jen, R., Orr, J. E., DeYoung, P., Smales, E., Malhotra, A., & Owens, R. L. (2020). Accuracy of WatchPAT for the diagnosis of obstructive sleep apnea in patients with chronic obstructive pulmonary disease. COPD, 17(1), 34–39.
Jonas, D. E., Amick, H. R., Feltner, C., Weber, R. P., Arvanitis, M., Stine, A., et al. (2017). Screening for obstructive sleep apnea in adults: An evidence review for the US preventive services task force: Evidence synthesis no. 146. Agency for Healthcare Research and Quality. AHRQ publication 14–05216-EF-1.
Kadhim, K., Lau, D. H., & Sandres, P. (2020). Sleep apnea in atrial fibrillation highly prevalent, highly relevant, but most patients are not somnolent. Int J Cardiol Heart Vasc, 26, 100463.
Katzan, I. L., Thompson, N. R., Uchino, K., & Foldvary-Schaefer, N. (2016). A screening tool for obstructive sleep apnea in cerebrovascular patients. Sleep Medicine, 21, 70–76.
Kleindorfer, D. O., Towfighi, A., Chaturvedi, S., Cockroft, K. M., Gutierrez, J., Lombardi-Hill, D., et al. (2021). 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline from the American Heart Association/American Stroke Association. Stroke, 52(7), e364–e467.
Kee, K, Dixon, J, Shaw, J, Vulikh, E, Schlaich, M, Kaye, D. M., et al. (2018). Comparison of commonly used questionnaires to identify obstructive sleep apnea in a high-risk population. J Clin Sleep Med. 14(12):2057–2064.
Kepplinger, J., Barlinn, K., & Albright, K. (2013). Early sleep apnea screening on a stroke unit is feasible in patients with acute cerebral ischemia. Journal of Neurology, 260, 1343–1350.
Kurinami, N., Sugiyamaa, S., Ijima, H., Yoshida, A., Hieshima, K., Miyamoto, F., et al. (2018). Clinical usefulness of the body muscle-to-fat ratio for screening obstructive sleep apnea syndrome in patients with inadequately controlled type 2 diabetes mellitus. Diab Res Clin Pract, 143, 134–139.
Leino, A., Nikkonen, S., Kainulainen, S., Korkalainen, H., Töyräs, J., Myllymaa, S., et al. (2021). Neural network analysis of nocturnal SpO2 signal enables easy screening of sleep apnea in patients with acute cerebrovascular disease. Sleep Medicine, 79, 71–78.
Lajoie, A., Series, F., Bernard, S., Bernard, E., Egea-SantaOlalla, C. J., Abad Fernandez, A., et al. (2020). Reliability of home nocturnal oximetry in the diagnosis of overlap syndrome in COPD. Respiration, 99(2), 132–139.
Levy, J., Alvarez, D., Rosemberg, A. A., Alexandrovich, A., del Campo, F., & Behar, J. (2021). Digital oximetry biomarkers for assessing respiratory functions: Standards of measurement, physiological interpretation, and clinical use. Npg Digital Medicine, 4, 1–14.
Li, S., Xu, L., Dong, X., Zhang, X., Keenan, B. T., Hang, F., et al. (2021). Home sleep apnea testing of adults with chronic heart failure. Journal of Clinical Sleep Medicine, 17(7), 1453–1463.
Lin, S. H., Branson, C., Park, L., Leung, J., Doshi, N., & Auerbach, S. H. (2018). Oximetry as an accurate tool for identifying moderate to severe sleep apnea in patients with acute stroke. Journal of Clinical Sleep Medicine, 14(12), 2065–2073.
Lindberg, E., Theorell-Haglow, J., Svensson, M., Gislason, T., Berne, C., & Janson, C. (2012). Sleep apnea and glucose metabolism: A long-term follow-up in a community-based sample. Chest, 142, 935–942.
Linz, D., Kadhim, K., Brooks, A. G., Elliot, A. D., Hendricks, J. M., Lau, D. H., et al. (2018). Diagnostic accuracy of overnight oximetry for the diagnosis of sleep-disordered breathing in atrial fibrillation patients.Int. Journal of Cardiology, 272, 155–161.
Macrea, M., Oczkowski, S., Rochwerg, B., Branson, R. D., Celli, B., Coleman, M., et al. (2020). Long-term noninvasive ventilation in chronic stable hypercapnic chronic obstructive pulmonary disease. An official American Thoracic Society clinical practice guideline. American Journal of Respiratory and Critical Care Medicine, 202(4), e74–e87.
Marin-Oto, M., Vicente, E. E., & Marin, J. M. (2019). Lon term management of obstructive sleep apnea and its comorbidities. Multidisciplinary Respiratory Medicine, 14, 21.
Marin, J. M., Soriano, J. B., Carrizo, S. J., Boldova, A., & Celli, B. R. (2010). Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea. The overlap syndrome. American Journal of Respiratory and Critical Care Medicine, 182, 325–331.
Marulanda-Londoño, E., & Chaturvedi, S. (2017). The interplay between obstructive sleep apnea and atrial fibrillation. Frontiers in Neurology, 8, 668.
Mayer, G., Schwalmstadt-Treysa, M. A., Regensburg, B. B., et al. (2017). S3-guideline non-restorative sleep / sleep disorders – Chapter “sleep related breathing disorders”. Somnologie, 20(Suppl 2), S97–S180.
McEvoy, R. D., Antic, N. A., Heeley, E., Luo, Y., Ou, Q., Zhang, X., et al. (2016). CPAP for prevention of cardiovascular events in obstructive sleep apnea. The New England Journal of Medicine, 375, 919–931.
McNicholas, W. T. (2017). COPD-OSA overlap syndrome: Evolving evidence regarding epidemiology, clinical consequences, and management. Chest, 152(6), 1318–1326.
Malhotra, A., Schwartz, A. R., Schneider, H., Owens, R. L., DeYoung, P., Han, M. K., et al. (2018). ATS assembly on sleep and respiratory neurobiology. Research priorities in pathophysiology for sleep-disordered breathing in patients with chronic obstructive pulmonary dis-ease. An Official American Thoracic Society Research Statement. American Journal of Respiratory and Critical Care Medicine, 197(3), 289–299.
May, A. M., Wang, L., Kwon, D. H., Van Wagoner, D. R., Chung, M. K., Dalton, J. E., & Mehra, R. (2020). Sleep apnea screening instrument evaluation and novel model development and validation in the paroxysmal atrial fibrillation population. IJC Heart & Vasculature, 31, 100624.
Mohammadieh, A. M., Sutherland, K., Kanagaratnam, L. B., Whalley, D. W., Gillett, M. J., & Cistulli, P. A. (2021). Clinical screening tools for obstructive sleep apnea in a population with atrial fibrillation: A diagnostic accuracy trial. Journal of Clinical Sleep Medicine, 17(5), 1015–1024.
Oliveira, M. G., Nery, L. E., Santos-Silva, R., Sartori, D. E., Alonso, F. F., Togeiro, S. M., et al. (2012). Is portable monitoring accurate in the diagnosis of obstructive sleep apnea syndrome in chronic pulmonary obstructive disease? Sleep Medicine, 13, 1033–1038.
Parisot, J., Damy, T., Gellen, B., Covali-Noroc, A., Bodez, D., Rappeneau, S., et al. (2015). Sleep-disordered breathing in chronic heart failure: Development and validation of a clinical screening score. Sleep Medicine, 16(9), 1094–1101.
Pépin, J. L., Lévy, P., Lepaulle, B., & Guilleminault, C. (1991). Does oximetry contribute to the detection of apneic events? Mathematical processing of the SaO2 signal. Chest, 99, 1151–1157.
Pillar, G., Berall, M., Berry, R., Etzioni, T., Shrater, N., & Hwang, D. (2020). Detecting central sleep apnea in adult patients using WatchPAT— A multicenter validation study. Sleep & Breathing, 24, 387–398.
Quintana-Gallego, E., Villa-Gil, M., Carmona-Bernal, C., Botebol-Benhamou, G., Martínez-Martínez, A., Sánchez-Armengol, A., et al. (2004). Home respiratory polygraphy for diagnosis of sleep-disordered breathing in heart failure. The European Respiratory Journal, 24(3), 443–448.
Ranjan, R. (2020). Is it time to screen all patients for sleep apnea before atrial fibrillation ablation? Journal of the American College of Cardiology, 6(12), 1507–1508.
Rosen, I. M., Kirsch, D. B., Chervin, R. D., Carden, K. A., Ramar, K., Aurora, R. N., et al. (2017). American Academy of sleep medicine Board of Directors. Clinical use of a home sleep apnea test: An American Academy of sleep medicine position statement. Journal of Clinical Sleep Medicine, 13(10), 1205–1207.
Saletu, M., Kotzian, S., Schwarzinger, A., Haider, S., Spatt, J., & Saletu, B. (2018). Home sleep apnea testing is a feasible and accurate method to diagnose obstructive sleep apnea in stroke patients during in-hospital rehabilitation. Journal of Clinical Sleep Medicine, 14, 1495–1501.
Sanchez-de-la-Torre, M., Lee, C.-H., & Barbé, F. (2021). Obstructive sleep apnea and atrial fibrillation: We need to go step by step. Journal of Clinical Sleep Medicine, 17(5), 869–870.
Scott, A. S., Baltzan, M. A., & Wolkove, N. (2014). Examination of pulse oximetry tracings to detect obstructive sleep apnea in patients with advanced chronic obstructive pulmonary disease. Canadian Respiratory Journal, 21, 171–175.
Seiler, A., Camilo, M., Korostovtseva, L., Haynes, A. G., Brill, A. K., Horvath, T., et al. (2019). Prevalence of sleep disordered breathing after stroke and TIA. A meta-analysis. Neurology, 92, e648–e654.
Series, F. (2015). Should all congestive heart failure patients have a routine sleep apnea screening? Pro. Canadian Journal of Cardiology, 31, 935–939.
Senaratna, C. V., Perret, J. L., Matheson, M. C., Lodge, C. J., Lowe, A. J., Cassim, R., et al. (2017). Validity of the Berlin questionnaire in detecting obstructive sleep apnea: A systematic review and meta-analysis. Sleep Medicine Reviews, 36, 116–124.
Sharma, S., Mather, P. J., Chowdhury, A., Gupta, S., Mukhtar, U., & Willes, L. (2017). Sleep overnight monitoring for apnea in patients hospitalized with heart failure (SOMA-HF study). Journal of Clinical Sleep Medicine, 13(10), 1185–1190.
Siarnick, P., Jurik, M., Klobučníkováa, K., Kollár, B., Pirošováb, M., Malik, M., et al. (2021). Sleep apnea prediction in acute ischemic stroke (SLAPS score): A derivation study. Sleep Medicine, 77, 23–28.
Siarnik, P., Jurík, M., Veverka, J., Klobučníkováa, K., Kollár, B., Turcani, P., et al. (2020). Pulse oximetric routine examination of sleep apnea in acute stroke (PRESS). Sleep Medicine, 73, 208–212.
Sico, J., Yaggi, H., Ofner, S., Cocato, J., Austin, C. H., Fergurson, J., et al. (2017). Development, validation, and assessment of an ischemic stroke or transient ischemic attack-specific prediction tool for obstructive sleep apnea. Journal of Stroke and Cerebrovascular Diseases, 26, 1745–1754.
Soler, X., Liao, S. Y., Marin, J. M., Lorenzi-Filho, G., Jen, R., DeYoung, P., et al. (2017). Age, gender, neck circumference, and Epworth sleepiness scale do not predict obstructive sleep apnea (OSA) in moderate to severe chronic obstructive pulmonary disease (COPD): The challenge to predict OSA in advanced COPD. PLoS One, 12(5), e0177289.
Starkey, S. Y., Jonasson, D. R., Alexis, S., Su, S., Johal, R., Sweeney, P., et al. (2021). Screening for obstructive sleep apnea in an atrial fibrillation population: What’s the best test? CJC Open, 3, 442–449.
Szymanski, F. M., Platek, A. E., & Filipiak, K. J. (2015). Is obstructive sleep apnea associated with the risk of ischemic stroke in patients with atrial fibrillation? International Journal of Cardiology, 2015(184), 481–482.
Tahrani, A. A. (2015). Obstructive sleep Apnoea and vascular disease in patients with type 2 diabetes. Eur Endocrinol, 11(2), 81–89.
Takala, M., Puustinen, J., Rauhala, E., et al. (2018). Pre-screening of sleep-disordered breathing after stroke: A systematic review. Brain and Behavior: A Cognitive Neuroscience Perspective, 8, e01146.
Tauman, R., Berall, M., Berry, R., Etzioni, T., Shrater, N., Hwang, D., et al. (2020). Watch-PAT is useful in the diagnosis of sleep apnea in patients with atrial fibrillation. Nat Sci Sleep, 12, 1115–1121.
To KW, Chan TO, Chan WC, Choo KL, Hui DSC. (2021) Using a portable monitoring device for diagnosing obstructive sleep apnea in patients with multiple coexisting medical illnesses. Clin Respir J. 15(10):1104–1112.
Traaen, G. M., Overland, B., Aakeroy, L., Hunt, T. E., Bendz, C., Sande, L., et al. (2020). Prevalence, risk factors, and type of sleep apnea in patients with paroxysmal atrial fibrillation. Int J Cardiol Heart Vasc, 26, 100463.
Treptow, E., Oliveira, M. G., Moreira, G. A., Togeiro, S., Nery, L. E., Tufyk, S., et al. (2015). Update on the use of portable monitoring system for the diagnosis of sleep apnea in specific population. World J Respirol., 5(1), 17–27.
Valika, A., Costanzo, M. R. (2017). Sleep-disordered breathing during congestive heart failure: To intervene or not to intervene? Cardiac Failure Review, 3(2), 134–139.
Vaquerizo-Villar, F., Álvarez, D., Kheirandish-Gozal, L., Gutiérrez-Tobal, G. C., Barroso-García, V., Santamaría-Vázquez, E., del Campo, F., Gozal, D., & Hornero, R. (2021). A convolutional neural network architecture to enhance oximetry ability to diagnose pediatric obstructive sleep apnea. IEEE Journal of Biomedical and Health Informatics, 25(8), 2906–2916.
Warner, J. J., Harrington, R. A., Sacco, R. L., et al. (2019). Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke. Stroke, 50, 3331–3332.
Weinreich, G., Armitstead, J., Töpfer, V., Wang, Y. M., Wang, Y., & Teschler, H. (2009). Validation of apnea link as screening device for Cheyne-stokes respiration. Sleep, 32(4), 553–557.
Weinreich, G., Armitstead, J., & Teschler, H. (2008). Pattern recognition of obstructive sleep apnoea and Cheyne-stokes respiration. Physiological Measurement, 29, 869–878.
Wyckmans, M., Tukanov, S., Winters, R., Stinissen, R., Vermeulen, H., Dendale, P., et al. (2021). Pacemaker guide screening for severe sleep apnea, a possible option for patients with atrial fibrillation. A systematic review and meta-analysis. Pacing and Clinical Electrophysiology, 44(8), 1421–1431.
Wu, Q., Xie, L., Li, W., Xiang, G., Hu, W., Jiang, H., et al. (2020). Pulmonary function influences the performance of Berlin Questionnaire, modified Berlin Questionnaire, and STOP-Bang score for screening obstructive sleep apnea in subjects with chronic obstructive pulmonary disease. International Journal of COPD, 15, 1207–1216.
Xiong, M., Hu, W., Dong, M., Wang, M., Chen, J., Xiong, H., et al. (2019). The screening value of ESS, SACS, BQ, and SBQ on obstructive sleep apnea in patients with chronic obstructive pulmonary disease. International Journal of COPD, 14, 2497–2505.
Yancy, C. W., Jessup, M., Bozkurt, B., Butler, B., Casey, D. E., Jr., Colvin, M. M., et al. (2017). 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the Heart Failure Society of America. Coll Cardiol, 70(6), 776–803.
Yeghiazarians, J. H., Tietjens, J. R., Redline, S., Brown, D. L., El-Sherif, N., et al. (2021). Obstructive sleep apnea and cardiovascular disease: A scientific statement from the American Heart Association. Circulation, 144(3), e56–e67.
Youssef, I., Kamran, H., Yacoub, M., Patel, N., Goulbourne, C., Kumar, S., et al. (2018). Obstructive sleep apnea as a risk factor for atrial fibrillation: A meta-analysis. J Sleep Disord Ther., 7(1), 1000282.
Zamarrón, C., García, V., Morete, E., & del Campo, F. (2008). Association of chronic obstructive pulmonary diseases and obstructive sleep apnea consequences. International Journal of COPD, 3(4), 1–12.
Acknowledgments
This work was supported in part by “Ministerio de Ciencia e Innovación-Agencia Estatal de Investigación” and “European Regional Development Fund (FEDER)” under Projects PID2020-115468RB-I00 and RTC-2017-6516-1, in part by “Sociedad Española de Neumología y Cirugía Torácica (SEPAR)” under project 649/2018, by “Sociedad Española de Sueño (SES)” under project “Beca de Investigación SES 2019”, and in part by “Centro de Investigación Biomédica en Red en Bioingeniería, Biomateriales y Nanomedicina, (CIBER-BBN), Spain” through “Instituto de Salud Carlos III” co-funded with FEDER funds. The work of Daniel Álvarez was supported by a “Ramón y Cajal” grant (RYC2019-028566-I) from the “Ministerio de Ciencia e Innovación – Agencia Estatal de Inves-tigación” co-funded by the European Social Fund.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
del Campo, F., Arroyo, C.A., Zamarrón, C., Álvarez, D. (2022). Diagnosis of Obstructive Sleep Apnea in Patients with Associated Comorbidity. In: Penzel, T., Hornero, R. (eds) Advances in the Diagnosis and Treatment of Sleep Apnea . Advances in Experimental Medicine and Biology, vol 1384. Springer, Cham. https://doi.org/10.1007/978-3-031-06413-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-031-06413-5_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-06412-8
Online ISBN: 978-3-031-06413-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)