Abstract
Whenever possible, treatment of humerus diaphyseal fractures should be conservative. In the event of failure of such treatment or in fractures with surgical criteria, the current trend is to perform minimally invasive plate osteosynthesis. Other surgical options are closed reduction and intramedullary nail fixation and open reduction and internal fixation with plate. Numerous studies have not demonstrated the superiority of any of them, pointing out as the main disadvantage of open reduction the wide approach required jeopardizing the radial nerve and, for intramedullary nailing, the possible tendon injury and functional impairment of the shoulder. When surgical treatment is required, it is advisable to place plates percutaneously in these fractures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Fractures of the proximal humerus account for 1%–5% of all fractures [1], with an incidence of 13–14 cases per 100,000 population and a bimodal distribution, with a peak in young adults aged 20–30 years related to high-energy trauma and another in the elderly due to falls from their own height and lower-energy trauma associated with osteoporosis [1, 2].
There are several treatment options for this type of fracture, with controversy in the current literature and much variability in surgeon preferences [3].
8.2 Anatomy
To understand how these fractures behave and to establish the basis for their treatment, it is important to know certain anatomy details of the humeral diaphysis and its vasculonervous relationships.
The humeral diaphysis extends from the surgical neck of the proximal humerus [4] or superior border of the pectoralis major insertion [5] to the epicondyles or supracondylar crest [4, 5]. This is cylindrical in its proximal half and then becomes triangular, with three surfaces—anterolateral, anteromedial, and posterior [4, 5]—and a narrower diameter, which is important to take into account in the case of intramedullary fixations. Most of the vascularization of the humeral diaphysis arrives via a nutritional artery along the anteromedial border between the insertion of the coracobrachialis and anterior brachial muscles [4].
There are important and close vasculonervous relationships and structures to be considered, which can be injured by both the fracture itself and iatrogenically either by manipulations or in its surgical management. The humeral diaphysis has certain areas that the surgeon must know how to recognize because they are key points in these vasculonervous relationships. The deltoid tuberosity is a slight V-shaped bony outgrowth on the anterolateral surface where, as its name indicates, the deltoid muscle inserts [4]. This fact is important because, in diaphyseal fractures of the proximal third of the humerus below the deltoid V, the deltoid tends to pull on the proximal end and displaces it. Another important landmark is the radial groove that develops posteriorly at the insertion of the lateral belly of the triceps and extends distally and laterally and houses the radial nerve along with the brachial artery [4].
The vasculonervous structures in relation to the humeral diaphysis are the brachial artery and axillary nerve in the most proximal part and the radial, ulnar, median, and lateral antebrachial cutaneous nerves, sensory branches of the musculocutaneous nerve, in the most distal part. Special mention should be made of the radial nerve, the most commonly injured structure in this type of fractures, and the lateral antebrachial cutaneous nerve, present in the anterior mid-distal third approach.
The radial nerve is the main structure that can be affected in diaphyseal fractures of the humerus, with a reported rate of injury of 7–17% [6], which can be primary or iatrogenic. Iatrogenic injury rates in the literature range around 7%, but rates of up to 32% have been reported in some series [7, 8]. It is therefore important to have a good knowledge of the pathway and relationships of this nerve. It comes from the posterior fascicle of the brachial plexus, from nerve fibers coming from the spinal roots C5, C6, C7, and C8. It passes through the anterior aspect of the subscapularis muscle, descends medially along with the brachial artery, then separates from it, passes posteriorly between 18.1 and 20.7 cm proximal to the medial epicondyle, and enters the torsion canal [9, 10]. It leaves the latter between 10.1 and 14.8 cm proximal to the lateral epicondyle and crosses the lateral intermuscular septum of the arm to pass into the anterior compartment between 7.5 and 10 cm proximal to the elbow joint [11], an important anatomical relationship due to the possible injury of this nerve in Holstein Lewis fractures [12].
The lateral antebrachial cutaneous nerve is a terminal branch of the musculocutaneous nerve, which, after innervating the biceps and anterior brachial muscles, becomes superficial crossing the bicipital aponeurosis innervating the cutaneous region of the radial border of the forearm.
It is important to know the anatomy and relationships of these structures to avoid injury during surgical approaches. As we have said, the structure with the highest rate of injury in these fractures, both primary and iatrogenic, is the radial nerve, which we will make special mention of throughout this chapter.
8.3 Classification of Diaphyseal Humeral Fractures
Fractures of the humeral diaphysis can be defined according to location (proximal to the pectoralis major insertion, between the pectoralis major and deltoid insertions, or below the deltoid insertion) [5], fracture morphology (transverse, oblique, spiroid), angulation, displacement, and comminution or whether the fracture is open or closed. The most commonly used classification for open fractures is the Gustilo classification [13].
According to the fracture pattern, the most commonly used classification is that of the AO/OTA (Arbeitsgemeinschaft für Osteosynthesefragen (AO)/Orthopaedic Trauma Association (OTA) [14], which classifies fractures into 3 types—type A (simple fractures 63.3%), type B (wedge or butterfly wing fractures), and type C (complex comminuted fractures)—and then subdivides them into three distinct patterns according to the magnitude of comminution. Interobserver agreement for the 3 fracture types and for the 9 fracture groups was moderate (κ = 0.46 and κ = 0.48, respectively) [14].
There are also eponyms to describe certain fracture patterns, such as the Holstein-Lewis fracture, described in 1963 [15], an extra-articular spiroid displaced fracture of the distal third of humerus, where the proximal peak of the distal fragment deviates laterally, thus resulting in a high rate of radial involvement, since at that level this nerve crosses the lateral intermuscular septum to pass into the anterior compartment. It constitutes 7.5% of all humeral diaphyseal fractures [8, 12] (Fig. 8.1).
8.4 Initial Patient Assessment
During the anamnesis, the mechanism of injury should be ascertained; a fall from its own height with low-energy trauma indicates possible bone fragility, whether previously diagnosed or not. A high-energy trauma should warn us about possible associated injuries, both vasculonervous lesions at the fracture level and possible associated injuries.
In the physical examination, we will find pain, functional impairment, swelling, and frequent deformity at arm level. It will be necessary to verify a correct state of soft tissues and to rule out wounds that turn the injury into an open fracture.
It is essential to perform and record in the clinical history an initial neurovascular evaluation before any manipulation or surgical intervention and, again after them, paying special attention to the radial nerve, the most frequently injured, by checking the ability to extend the wrist and fingers. We will also check the ulnar nerve by means of Froment’s sign and the median nerve by means of the extension of the first finger. The axillary nerve should be examined by means of the sensitivity in the deltoid area since the functional impotence due to the same fracture prevents us from abducting the arm. Finally, it is important to check the radial and ulnar pulses to rule out the involvement of the brachial artery.
A simple radiography in two projections will generally be sufficient for a correct diagnosis and characterization of the injury, including the adjacent joints, elbow, and shoulder. Other tests such as magnetic resonance imaging (MRI) or CT scan are reserved for a second time to evaluate possible lesions of the rotator cuff or other associated shoulder structures or consolidation delays, respectively.
The initial treatment will be immobilization by means of a hanging cast or U-splint. We would opt for an external fixator in open fractures with significant exposure (Gustilo III) where we consider that primary closure and definitive treatment is not possible or in the case of polytraumatized patients with injuries at other levels for damage control.
8.5 Treatment
The treatment of these fractures can be classified as conservative or surgical, the latter being an open reduction and internal fixation by means of a plate or a closed reduction and internal fixation by means of an intramedullary nail. In recent years, percutaneously placed plates have also been increasingly used.
As early as 1977, Sarmiento described good results with conservative treatment [15], which have been corroborated by numerous studies by the same author and others [16, 17]. For many surgeons, it is still considered the gold standard treatment. However, there has been a growing trend toward surgical management of these fractures, despite the lack of evidence in the literature on its superiority over orthopedic treatment. A study analyzing the Finland National Hospital Discharge Registry showed an increase in surgical treatment in the last two decades, doubling in men and almost tripling in women [18].
8.5.1 Conservative Treatment
As we have said, this is a treatment option with good results described decades ago [15,16,17, 19]. Before Sarmiento’s description of functional immobilization, rigid immobilizations involving the shoulder and elbow (brachial splints, U-splints, hanging casts, Velpeau bandages) were used, which caused joint stiffness of the shoulder and elbow. In addition, it was also observed that functional rather than rigid immobilization created a larger and stronger callus [20].
Conservative treatment is performed sequentially. Initially, the fracture is immobilized in a hanging cast or U-splint for one to 2 weeks [15]. After this period, the immobilization is replaced by a prefabricated functional brace that can be adapted to the patient’s arm by means of straps and can be tightened over the weeks as the swelling goes down. This system is based on external compression of the fracture through the musculature and other soft tissues, achieving good control of angulation and rotation, although not so much of the shortening, which depends more on the initial pattern of the fracture. Thanks to this system, the patient will be able to mobilize the elbow and shoulder according to tolerance to avoid stiffness [21]. To control the possible secondary displacement of the fracture, a control X-ray should be taken at 1 week of evolution and then serial X-rays every 2 weeks until the treatment is completed, which will last between 10 and 12 weeks on average [1].
Consolidation rates of between 77.4 and 100% have been described. Sarmiento published in 2000 a large series of 620 patients treated in this way with a nonunion rate of less than 2% in closed fractures and 6% in open fractures. Furthermore, this consolidation was achieved in 87% with less than 16 degrees of varus angulation and less than 16 degrees of anterior angulation [17]. Since then, numerous studies have been published confirming these good results.
In addition, in some studies, certain fracture patterns were observed to have worse healing rates with conservative treatment. Koch published a series of 67 fractures in 2002, with 87% healing in an average period of 10 weeks. Of the 9 cases of nonunions that required surgery, 6 were single-trait transverse fractures [16]. Rutgers published in 2006 a series of 49 patients with 44 of them (90%) consolidating. Of the five that did not consolidate, four were proximal third [19]. Ekholm published in 2006 a series of 78 patients with 90% consolidation after conservative treatment. The majority of nonunions, with a nonunion rate of 20%, were single-stroke fractures (type A of the AO classification) in the proximal third. He also reflected that functional outcomes were good in patients in whom the fracture consolidated with conservative treatment from the beginning but worse in those who required surgery for nonunion, even if consolidation was finally achieved, so this author recommended assessing a surgical treatment from the beginning for simple fractures of the proximal third, due to a higher risk of nonunion [22]. Ali published in 2015 a series of 138 fractures, with a consolidation rate of 83%, observing worse rates also in proximal third fractures and better rates in comminuted fractures than in simpler traces, being more specifically oblique proximal third fractures the ones with the lowest union rate [23]. These results are reflected in Table 8.1 [16, 17, 19, 22, 23].
Papsoulis conducted a literature review in 2021 with 16 case series and two comparative studies and observed a 94.5% healing rate in a mean time of 10.7 weeks, also observing a higher rate of nonunion in single-trace fractures (type A) in the proximal third [24]. It is suggested that the cause of this fact may rely on the action of the deltoid and pectoralis major displacing the proximal fragment and producing a muscular interposition in the fracture line. The same conclusion was reached by Ring et al. in their 2007 study [25]. They studied 32 patients with nonunions after orthopedic treatment of diaphyseal fractures of the humerus, 17 of which were in the proximal humerus, 14 in the middle third, and 1 in the distal third. Twenty-seven fractures had an oblique or simple spiral trace.
Regarding residual angulation, Klenerman described a sagittal angulation of 20° and a varus angulation of 30° as tolerable for good function as early as 1966 [26]. Since then, these parameters have been accepted. A valgus of 30°, a malrotation of 15°, and a maximum shortening of 3 cm have also been established as tolerable [27].
Therefore, conservative treatment of humerus diaphyseal fractures is a good option, with high healing rates and good functional results even with significant angulations. However, we know that certain fracture patterns, mainly single and proximal third traces, specifically a long oblique proximal third trace, probably due to muscle traction, have a higher risk of nonunion, and we could consider surgical treatment from the beginning (Fig. 8.2).
However, there are still absolute indications for surgery [13], which can be classified into several causes, summarized in Table 8.2:
-
Because of non-tolerance to conservative treatment: obese patients, with poor pain control with immobilization or who simply refuse this type of treatment, since there is evidence that, for optimal conservative treatment, the patient must be satisfied with this method [22].
-
By fracture pattern: whether adequate angulation cannot be obtained by functional immobilization or whether secondary displacement occurs after this treatment. Close follow-up by serial radiographs is therefore important. As mentioned above, the accepted angulation values are 30° of varus or valgus, 20° of anterior angulation, 15° of malrotation, and 3 cm of shortening [26, 27]. We would also opt for surgical treatment if the fracture has intra-articular extension, which would bring us closer to the plate option. Finally, if it is a floating elbow or in case of a pathological fracture due to metastasis, we would consider pin fixation. A polytraumatized patient or bilateral fractures would be a relative indication for surgery.
-
Due to poor condition of soft tissues: open Gustilo type III fractures, burns, or extensive abrasions requiring frequent dressing.
-
Associated vascular lesions that need to be surgically repaired, since fracture fixation, preferably rigid fixation with a plate, would be indicated to protect the anastomosis [1].
-
Brachial plexus injuries: in these cases, high rates of nonunion have been observed in conservative treatment with functional plaster, due to poor muscle tone, not achieving adequate compression. In addition, this situation delays rehabilitation [28].
Regarding primary radial nerve involvement, it is not currently considered by itself a criterion for surgery. The literature has described high (73–95%) and similar rates of nerve recovery with both expectant management and early surgical revision, so it has been advised to avoid surgical indication from the outset [29,30,31,32]. However, other authors disagree and have created decision algorithms when facing radial palsy. The recommendation is to perform an electromyogram between week 3 and 4 and week 6 and week 12. Progressive reinnervation should be observed, although full recovery may take 6–12 months. If at week 12 there is no recovery, some authors suggest surgical revision of the nerve. For other authors, this date may be extended to the 4th–sixth month [33]. In the case of fractures with radial symptoms that require surgical treatment for another reason (described in Table 8.1), it is recommended that a revision of the radial nerve be performed at the same time. The osteosynthesis method of choice in these cases would be the plate, since there is a possibility of the nerve being in the fracture site and getting injured during intramedullary nail insertion [33].
8.5.2 Intramedullary Nailing
In comparison with open fixation with a plate, intramedullary fixation provides greater respect for the soft tissues and periosteal circulation, thus improving the biological environment for the repair of the fracture [1, 4]. In addition, being an intramedullary implant, it is aligned with the loading axis of the humerus, contributing to a better load distribution and more resistance to bending. It would be the implant of choice in cases of pathological fractures or bifocal fractures [1, 4].
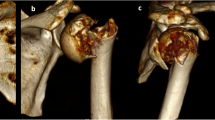
Its main drawback would be residual pain and functional impairment of the shoulder in anterograde nails, the most commonly used, due to damage to the cuff in the hypovascular area near its insertion or subacromial occupation by protrusion of the material [34, 35]. For this reason, modifications in the entry point have been considered to try to minimize damage to the cuff insertion, making it more medial, more lateral, through the Neviaser portal or through the rotator interval [36,37,38,39]. It is also important to perform a good reduction, even if it is not direct as in plate placement. In oblique proximal traces, which are displaced by the action of the deltoid and pectoralis, a mini-open may be necessary to start introducing the nail with the fracture already reduced by a clamp or cerclage, in order to avoid possible nonunion of these traces, which is also greater in conservative treatment (Figs. 8.3 and 8.4).
As for retrograde nails, which are less commonly used, there is a risk of supracondylar humerus fracture during placement, as well as elbow joint stiffness and heterotopic calcifications, although they would prevent rotator cuff damage [40, 41]. In addition, they have shown similar results in terms of consolidation and complications with respect to the antegrade ones. However, they are less used probably due to their technical difficulty at the insertion point, requiring an oval entry area of several centimeters to avoid producing iatrogenic fracture of the anterior cortex of the humerus.
8.5.2.1 Results
The union rates are high, similar to conservative treatment, between 85% and 100%; the results are reflected in Table 8.3 [34, 42,43,44,45,46,47]. In contrast, high rates of residual pain and functional impairment of the shoulder have been reported, ranging from 6% to 100% in some series [48]. The longest published series [34] retrospectively reviewed 99 patients treated with intramedullary nailing, 54 antegrade, and 45 retrograde. A 97% consolidation rate was observed, 3 cases of radial paresis after surgery, which recovered spontaneously. Regarding shoulder function, measured by the Constant scale, 91.3% showed excellent function and 5.4% good. Elbow function, using the Mayo Elbow Score, was excellent in 81.5% and good in 14.1%. All patients with shoulder function deficits corresponded to antegrade nails, and all those with elbow function deficits corresponded to retrograde nails.
8.5.3 Internal Fixation with Plate
In the case of opting for surgical treatment, the indications for a plate instead of a nail would be the need for an arterial repair taking advantage of the same approach and thus achieving a rigid fixation that protects the anastomosis [49] and the articular extension, either distal or proximal, of the fracture, since an anatomical reduction would then be required (Fig. 8.5). As previously mentioned, radial involvement in a fracture with surgical treatment criteria for another reason would make us more inclined to opt for a plate as a method of osteosynthesis associated with radial exploration, since there is a likelihood that the nerve is trapped in the fracture site and can be injured during the intramedullary nail insertion [33].
8.5.3.1 Surgical Approaches
For the proximal and middle third, the anterolateral approach is commonly used, a prolongation of the shoulder deltopectoral approach that goes down the lateral area of the biceps, displaces it medially, and goes deeper through the brachialis muscle, between its middle and lateral thirds, taking advantage of the double innervation of this muscle. In fact, some authors have proposed a new division of this muscle into two independent fascicles [50]. The only vasculonervous structure to be taken into account at this level is the lateral antebrachial cutaneous nerve, a sensory branch of the musculocutaneous nerve, which is located between the biceps and the brachialis. This approach allows a large exposure of the diaphysis in the middle and proximal thirds.
For the distal third, the most commonly used approach is the posterior approach, which can expose both the diaphysis and the elbow in case of intra-articular extension. In addition, a good exposure of the radial nerve is also achieved at proximal level, when it is located posteriorly, in the torsion canal, being able to place a plate under it if the fracture extends more proximally. Deep planes are accessed through the triceps fibers by separating them longitudinally or through lateral and medial paratricipital windows, thus avoiding injury to the muscle belly. Gerwin published an anatomical study on 10 specimens where three types of posterior approach were performed [51]. Through triceps-splitting, 15.4 +/− 0.8 cm of humerus was exposed, from the epicondyle proximally, where the radial nerve crosses the posterior part of the humerus, seeing a total of 55% of the humerus. A second modification also mobilizes the radial nerve toward proximal and visualizes 6 cm more of the humerus toward proximal, 76% of the humerus. Finally, the third variant is the modified posterior approach, where the radial nerve was located in the distal and lateral area of the humerus and the triceps was retracted medially, being able to expose 26.2 ± 0.4 cm of the humeral diaphysis from the epicondyle to the proximal, 94% of the humerus. Clinical studies have also shown good results with the latter approach, emphasizing the large exposure achieved [52].
Other authors have proposed less used approaches such as the medial approach, although reserved only for the middle third, neither proximal nor distal, demonstrating the same results as with the anterolateral approach and proposing it as a more aesthetic alternative to the latter [53]. There are also groups that have used neurostimulators in their approaches to avoid radial injury [3].
8.5.3.2 Type and Placement of Plates
Following the principles of AO, the plates, generally of large fragments, can be arranged to give compression to the fracture, as neutralization plates of an interfragmentary compression with one or more screws or as bridging plates. This arrangement will depend on the fracture trace. In a simple trace, direct reduction and interfragmentary compression can be applied by plate in short transverse or oblique traces and by interferential screws plus neutralization plate in longer spiroid or oblique traces. In a comminuted fracture, a bridging plate assembly would be best option [54]. Regarding locked or unlocked screws, no significant differences in bending or torsional strength have been reported in cases with good bone quality [55], unlike in osteoporotic models [56], where locked plates would be beneficial. In cases of bone defects due to severe comminution, a shortening of the humerus, acceptable up to 3–4 cm, can be considered, despite the possible residual muscle weakness.
As for the use of double plates, there are several biomechanical and more recently clinical studies that support their use because they provide greater stability [57,58,59,60,61], so they could be useful for fractures where intraoperatively satisfactory stability is not achieved. It is also possible to associate a small fragment, reconstruction, or third shank plate as initial fixation to maintain the reduction and then place the large fragment plate.
8.5.3.3 Results
Consolidation rates vary between 87% and 96% with a mean consolidation time of 12 weeks; figures are very similar to conservative treatment and nailing. The results are summarized in Table 8.4 [42,43,44,45,46,47]. Regarding radial nerve injury, a study of 261 fractures treated by open reduction and internal fixation showed an injury rate of 12.2%, finding no differences in fracture location or type of approach [62]. In one study, these were significantly related to surgeon experience and not to fracture location or fracture pattern [63]. Most of these palsies recover spontaneously [64].
Regarding the attitude to radial paresis after surgical treatment, i.e., considered iatrogenic, there has classically been controversy between maintaining a wait-and-see attitude as in primary paresis or performing an early surgical revision. In a study of 707 surgically treated diaphyseal fractures of the humerus, 46 radial palsies were observed, in no case having been recorded during the operation of obvious radial lesions. Thirty-nine had been treated with plate, three with intramedullary nail, and four with Ender nails. Five cases were surgically revised, in none of which a macroscopic radial lesion was found. All cases recovered spontaneously in an average of 15 weeks. Therefore, these authors advocate a wait-and-see attitude unless there is any suspicion of injury, for example, by a loss of reduction or mobilization of the material in the post-surgical radiological control [65]. In a 2019 review, the authors observed a similar radial recovery pattern in primary and secondary paresis and observed no advantage to early surgical exploration [66]. In another recent review, they also recommend a wait-and-see approach unless there is an obvious suspicion of injury at surgery [67].
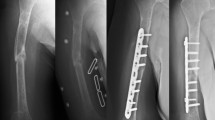
8.5.3.4 MIPO (Minimally Invasive Plate Osteosynthesis) Technique
Minimally invasive plating has grown in recent years. In 2002, Fernandez Dell’Oca introduced the idea of helical implants for several types of fractures, including humerus diaphyseal fractures, presenting two cases with good results [68]. A helical conformation placed the proximal part of the plate in the lateral zone, while the distal zone remained in the anterior zone, avoiding the radial nerve. Livani published in 2004 his series of 15 patients with diaphyseal fractures treated by this technique where he described the percutaneous placement of a large fragment plate in the anterior zone of the humerus, a safe area in terms of vasculonervous structures and also flat, so it was not necessary to conform the plate, as proposed by Fernandez Dell’Oca, whose placement in the lateral zone of the humerus of his preconformed plate put the axillary nerve at risk [69]. The proximal approach involved a 3–5 cm anterolateral mini-approach between the biceps on one side and the deltoid and cephalic vein on the other. The distal approach was also made about 3–5 cm along the lateral aspect of the biceps, more deeply crossing the brachialis muscle and leaving the musculocutaneous nerve medially and the radial nerve laterally, which are the two nerves that supply this muscle, thus going through an interneural plane. A submuscular and extraperiosteal tunneling was then performed connecting the two approaches. The plate was introduced from proximal to distal, taking special care to place the plate medial to the long portion of the biceps and not trapping it. The plate was then fixed to the proximal fragment with 3 screws, followed by an indirect reduction of the distal fragment on the plate. Once verified by radioscopy, the distal fixation is performed with three more screws. In the case of very distal fractures, he opted to curve the end zone of the plate anteriorly and place it in the anterior zone of the lateral column, in this case performing the Kocher approach in this distal area [69]. From this point on, increasing series with similar surgical technique and good results continued to be published [70,71,72,73,74,75,76,77,78,79,80,81,82], and since then dozens of comparative studies, reviews, and several recent meta-analyses have been published showing excellent results compared to conventional open reduction, with less radial nerve injury rate, less bleeding, less surgical time, and even less nonunions. When compared to intramedullary nail fixation, better functional shoulder scales have been reported [83,84,85,86] (Table 8.5). The MIPO seem to correspond to the current trend as opposed to the wide approaches previously described (Fig. 8.6).
(a–c) Comminuted diaphyseal humerus fracture (a). Closed reduction and fixation with straight plate using MIPO (minimally invasive plate osteosynthesis) technique (b). Surgical mini-approaches: proximal anterolateral and distal Kocher (c). Images provided by Dr. Miquel Videla, Traumatology and Orthogeriatrics Unit, Hospital Moisés Broggi
A cadaveric study in 2005 already described this method as very safe regarding the radial nerve. When sliding the plate through the anterior zone, it remained in the distal zone between 2 and 4.9 mm from the radial nerve in full supination and between 0 and 3 in pronation, so it is recommended to keep the arm in supination during percutaneous sliding of the plate [71]. Caution should also be taken to avoid tensioning the lateral area of the distal approach with Hohman-type spreaders to avoid radial paresis. The surgical technique and the confirmation of the safety of vasculonervous structures are maintained to this day. There are authors who consider radial paresis as a contraindication to perform a percutaneous technique, but others such as Livani already in 2005 published a small series of six patients with distal humerus fractures and radial paresis where he performed a percutaneous technique but through a distal Kocher approach, locating the radial nerve and introducing the plate from distal to proximal. All patients recovered from paresis [72].
More recently, the idea of helical implants for diaphyseal fractures with metaphyseal or proximal articular extension has been taken up again, either because there is insufficient space for an anterior plate placement proximally or because an associated articular reduction is needed. García-Virto et al. have recently published a series of 15 patients with fractures of this type where osteosynthesis was performed using the MIPO technique with preconformed helical plates. In the proximal area, a lateral transdeltoid mini-approach of 3–5 cm is performed, and in the distal area the anterior approach is similar to the anterior placement of straight plates. The helical plate is introduced from proximal to distal taking special care with the axillary nerve. They had one case of nonunion, with no radial paresis and good to excellent functional results [87] (Fig. 8.7).
(a–c) Diaphyseal fracture of the proximal humerus with insufficient space in the proximal fragment for placement of an anterior plate (a). Closed reduction and fixation with precontoured helical plate using MIPO (minimally invasive plate osteosynthesis) technique (b). Excellent functional result (c). Images provided by Dr. Miquel Videla, Traumatology and Orthogeriatrics Unit, Hospital Moisés Broggi
This technique offers a middle ground between ORIF and intramedullary nailing, incorporating benefits of both. From the nail, minimally invasive surgery provides greater respect for the soft tissues and relative stability, thus obtaining a more biological fixation but avoiding damage to the cuff at its entry point, such as the plate. It also reduces radial nerve injuries, more frequently observed in open reductions and internal fixations with plate.
8.5.4 External Fixator
Generally, treatment with an external fixator is reserved for damage control in polytraumatized patients and for open fractures with a large defect (Gustilo III). In cases where definitive surgical treatment cannot be carried out after placement, either because of the general condition of the patient or because of the poor condition of the soft tissues, there are studies that describe good results using this method as definitive treatment [88]. It is important to be familiar with the anatomy and the changing situation of the radial nerve along the humerus to avoid injuring it with the pins [89].
8.6 Comparison of Treatment Options
Regarding the choice between conservative or surgical treatment, a 2012 Cochrane review could not conclude whether surgical treatment was better or worse than conservative treatment [90]. In 2015, another systematic review continued to state that there was no level 1 evidence in the literature on the management of these fractures [91]. A 2019 systematic review reflects that conservative treatment has better consolidation rates (6.3% nonunions versus 17.6%), with lower rates of complications such as iatrogenic radial injury or infection. Radiological malunion rates were higher in conservative treatment but did not correlate with worse functional outcomes [2]. In contrast, another systematic review with meta-analysis in 2020 showed a lower rate of nonunion in surgical treatment but a higher rate of infection, with no differences in malunion or nerve injury. Therefore, it does not seem to be a superiority of surgical treatment over conservative management, as long as there are no absolute indications for the latter (no tolerance to conservative treatment, inadequate reduction, intra-articular extension, floating elbow, metastasis, open Gustilo III fractures, brachial plexus lesions, vascular lesion).
As for the option of plate or nail if surgical treatment is chosen, this has been a matter of debate for decades, even when non-locked intramedullary implants were used. A 1995 study by Rodríguez-Merchán compared the use of plates with Hackethal nails in 40 patients with diaphyseal humerus fractures, finding no differences in healing and complication rates. He also proposed a classification for functional outcomes after treatment of these fractures [92].
In more recent literature and after many comparative studies, a 2010 meta-analysis of four randomized studies (n = 203 patients) reflected that there were no significant differences between both treatments in the rates of complications, nonunions, infection, radial palsy, or need for reintervention, although authors acknowledged there was heterogeneity in the studies, small samples, and certain methodological limitations [93]. A 2013 meta-analysis of 10 randomized controlled studies (n = 429 patients) found no differences in nonunion, delayed consolidation, radial paresis, or implant failure. In contrast, there were differences favoring the plate use in subacromial impingement, although the increased need for reinterventions for this reason was unclear [94]. A recent 2021 meta-analysis of 18 observational studies (n = 4906 patients) and 10 randomized controlled studies (n = 525 patients) showed no differences in consolidation rates, quality of life, and upper limb functional scales. A higher rate of reoperation was observed in the intramedullary nail group, most frequently for symptoms of subacromial impingement. There were lower rates of temporary radial paresis in the intramedullary nail group, although all but one case recovered spontaneously in both groups. Consolidation time was somewhat shorter in the intramedullary nail group (slight difference of 1.9 weeks), with lower infection rates and shorter operative time. All these differences, although significant, were small and advocate that both treatments achieve good results [48].
As for minimally invasive plating, developing in recent years, studies seem to point to it as the best option not only superior to ORIF but also to intramedullary nailing. A dozen of meta-analyses in the last 5 years report a statistically significant difference in favor of the MIPO technique in terms of consolidation rate, radial paresis, bleeding, operative time, and shoulder pain (Table 8.5).
8.7 Conclusions
After several decades of controversy in the literature on the treatment of diaphyseal fractures of the humerus, it can now be stated that whenever there are no contraindications, conservative treatment should be chosen, paying special attention to the need for close clinical and radiological follow-up and the patient’s compliance and tolerance of this treatment. This mode of treatment is carried out sequentially, first with a hanging cast or U-splint immobilization, to be replaced in 1 or 2 weeks by a custom-made prefabricated brace, achieving a functional immobilization with early mobilization of the shoulder and elbow. Special attention should be paid to a fracture pattern: proximal third oblique line, in which higher rates of nonunion have been demonstrated, and surgical treatment can then be chosen at the outset.
In the case of deciding for surgical treatment, in fractures with metaphyseal or articular extension or in the case of vascular lesions in need of repair, we would opt for a plate, and, in bifocal or pathological fractures, we would opt for a nail. In all other cases, both treatments seem equally effective, with residual shoulder pain being the major disadvantage of the intramedullary nail, so special care should be taken to ensure that the material does not protrude into the subacromial space and try to minimize damage to the cuff at the point of entry. A more recent and superior treatment option to the previous ones are the plates placed in a minimally invasive way, its main limitation being the need for a learning curve, which once overcome seems to make this treatment the one of choice in case of deciding for a surgical treatment.
Regarding the most frequent complication, radial paresis, whether primary or iatrogenic, there seems to be general agreement that most of them have a spontaneous recovery, and therefore we should maintain an expectant attitude and not consider an early surgical revision unless there is a high suspicion of a clear lesion.
References
Gallusser N, Barimani B, Vauclair F. Humeral shaft fractures. EFORT Open Rev. 2021;6:24–34.
Sargeant HW, Farrow L, Barker S, Kumar K. Operative versus non-operative treatment of humeral shaft fractures: a systematic review. Shoulder Elbow. 2020;12:229–42.
Gulcek M, Gamli M. Anterior humeral approach with nerve stimulator. J Orthop Surg (Hong Kong). 2018;26:2309499018803002.
Updegrove GF, Mourad W, Abboud JA. Humeral shaft fractures. J Shoulder Elb Surg. 2018;27:e87–97.
Browner BD, Jupiter JB, Levine AM, Trafton PG, Krettek C, editors. Skeletal trauma basic science, management, and reconstruction, vol. 1 & 2. 4th ed. Philadelphia: Saunders Elsevier; 2009. ISBN: 978-1416022206.
Bishop J, Ring D. Management of radial nerve palsy associated with humeral shaft fracture: a decision analysis model. J Hand Surg Am. 2009;34(6):991–6.e1. https://doi.org/10.1016/j.jhsa.2008.12.029. Epub 2009 Apr 10.
Claessen FM, Peters RM, Verbeek DO, Helfet DL, Ring D. Factors associated with radial nerve palsy after operative treatment of diaphyseal humeral shaft fractures. J Shoulder Elb Surg. 2015;24(11):e307–11. https://doi.org/10.1016/j.jse.2015.07.012. Epub 2015 Sep 2.
Hak DJ. Radial nerve palsy associated with humeral shaft fractures. Orthopedics. 2009;32(2):111.
Guse TR, Ostrum RF. The surgical anatomy of the radial nerve around the humerus. Clin Orthop Relat Res. 1995;320:149–53.
Zlotolow DA, Catalano LW, Barron OA, Glickel SZ. Surgical exposures of the humerus. J Am Acad Orthop Surg. 2006;14:754–65.
McCann PA, Smith GC, Clark D, Amirfeyz R. The tricipital aponeurosis—a reliable soft tissue landmark for humeral plating. Hand Surg. 2015;20(1):53–8. https://doi.org/10.1142/S0218810415500070.
Holstein A, Lewis GM. Fractures of the humerus with radial-nerve paralysis. J Bone Joint Surg Am. 1963;45:1382–8.
Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24(8):742–6. https://doi.org/10.1097/00005373-198408000-00009.
Mahabier KC, Van Lieshout EM, Van Der Schaaf BC, Roukema GR, Punt BJ, Verhofstad MH, et al. Reliability and reproducibility of the OTA/AO classification for humeral shaft fractures. J Orthop Trauma. 2017;31:e75–80.
Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG. Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am. 1977;59(5):596–601.
Koch PP, Gross DF, Gerber C. The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elb Surg. 2002;11(2):143–50. https://doi.org/10.1067/mse.2002.121634.
Sarmiento A, Zagorski JB, Zych GA, Latta LL, Capps CA. Functional bracing for the treatment of fractures of the humeral diaphysis. J Bone Joint Surg Am. 2000;82(4):478–86. https://doi.org/10.2106/00004623-200004000-00003.
Huttunen TT, Kannus P, Lepola V, Pihlajamäki H, Mattila VM. Surgical treatment of humeral-shaft fractures: a register-based study in Finland between 1987 and 2009. Injury. 2012;43(10):1704–8. https://doi.org/10.1016/j.injury.2012.06.011. Epub 2012 Jul 6.
Rutgers M, Ring D. Treatment of diaphyseal fractures of the humerus using a functional brace. J Orthop Trauma. 2006;20(9):597–601. https://doi.org/10.1097/01.bot.0000249423.48074.82.
Rüedi T, Moshfegh A, Pfeiffer KM, Allgöwer M. Fresh fractures of the shaft of the humerus—conservative or operative treatment? Reconstr Surg Traumatol 1974;14:65–74
Sarmiento A, Horowitch A, Aboulafia A, Vangsness CT Jr. Functional bracing for comminuted extra-articular fractures of the distal third of the humerus. J Bone Joint Surg Br. 1990;72(2):283–7. https://doi.org/10.1302/0301-620X.72B2.2312570. Erratum in: J Bone Joint Surg Br 1990 Jul;72(4):752.
Ekholm R, Tidermark J, Törnkvist H, Adami J, Ponzer S. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma. 2006;20(9):591–6. https://doi.org/10.1097/01.bot.0000246466.01287.04.
Ali E, Griffiths D, Obi N, Tytherleigh-Strong G, Van Rensburg L. Nonoperative treatment of humeral shaft fractures revisited. J Shoulder Elb Surg. 2015;24(2):210–4. https://doi.org/10.1016/j.jse.2014.05.009. Epub 2014 Aug 1.
Papasoulis E, Drosos GI, Ververidis AN, Verettas DA. Functional bracing of humeral shaft fractures. A review of clinical studies. Injury. 2010;41(7):e21–7. https://doi.org/10.1016/j.injury.2009.05.004. Epub 2009 Jun 11.
Ring D, Chin K, Taghinia AH, Jupiter JB. Nonunion after functional brace treatment of diaphyseal humerus fractures. J Trauma. 2007;62(5):1157–8. https://doi.org/10.1097/01.ta.0000222719.52619.2c.
Klenerman L. Fractures of the shaft of the humerus. J Bone Joint Surg Br. 1966;48(1):105–11.
Shields E, Sundem L, Childs S, Maceroli M, Humphrey C, Ketz JP, Soles G, Gorczyca JT. The impact of residual angulation on patient reported functional outcome scores after non-operative treatment for humeral shaft fractures. Injury. 2016;47(4):914–8. https://doi.org/10.1016/j.injury.2015.12.014. Epub 2015 Dec 23.
Brien WW, Gellman H, Becker V, Garland DE, Waters RL, Wiss DA. Management of fractures of the humerus in patients who have an injury of the ipsilateral brachial plexus. J Bone Joint Surg Am. 1990;72(8):1208–10.
Ekholm R, Ponzer S, Törnkvist H, Adami J, Tidermark J. The Holstein-Lewis humeral shaft fracture: aspects of radial nerve injury, primary treatment, and outcome. J Orthop Trauma. 2008;22(10):693–7. https://doi.org/10.1097/BOT.0b013e31818915bf.
Shao YC, Harwood P, Grotz MR, Limb D, Giannoudis PV. Radial nerve palsy associated with fractures of the shaft of the humerus: a systematic review. J Bone Joint Surg Br. 2005;87(12):1647–52. https://doi.org/10.1302/0301-620X.87B12.16132.
Pollock FH, Drake D, Bovill EG, Day L, Trafton PG. Treatment of radial neuropathy associated with fractures of the humerus. J Bone Joint Surg Am. 1981;63(2):239–43.
Bumbasirević M, Lesić A, Bumbasirević V, Cobeljić G, Milosević I, Atkinson HD. The management of humeral shaft fractures with associated radial nerve palsy: a review of 117 cases. Arch Orthop Trauma Surg. 2010;130(4):519–22. https://doi.org/10.1007/s00402-009-0951-4. Epub 2009 Aug 11.
Rocchi M, Tarallo L, Mugnai R, Adani R. Humerus shaft fracture complicated by radial nerve palsy: is surgical exploration necessary? Musculoskelet Surg. 2016;100(Suppl 1):53–60. https://doi.org/10.1007/s12306-016-0414-3. Epub 2016 Nov 30.
Rommens PM, Kuechle R, Bord T, Lewens T, Engelmann R, Blum J. Humeral nailing revisited. Injury. 2008;39(12):1319–28. https://doi.org/10.1016/j.injury.2008.01.014. Epub 2008 Apr 15.
Jang Y, Kempton LB, Mckinley TO, Sorkin AT. Insertion-related pain with intramedullary nailing. Injury. 2017;48(Suppl 1):S18–21. https://doi.org/10.1016/j.injury.2017.04.029. Epub 2017 May 5.
Christ AB, Gausden EB, Warner SJ, Nellestein AM, Thacher RR, Lorich DG. Rotator cuff-sparing approach for antegrade humeral nailing with biceps tenodesis: a technical trick with clinical implications. J Orthop Trauma. 2017;31(2):e60–5. https://doi.org/10.1097/BOT.0000000000000684.
Park JY, Pandher DS, Chun JY, Md ST. Antegrade humeral nailing through the rotator cuff interval: a new entry portal. J Orthop Trauma. 2008;22(6):419–25. https://doi.org/10.1097/BOT.0b013e318173f751.
Dimakopoulos P, Papadopoulos AX, Papas M, Panagopoulos A, Lambiris E. Modified extra rotator-cuff entry point in antegrade humeral nailing. Arch Orthop Trauma Surg. 2005;125(1):27–32. https://doi.org/10.1007/s00402-004-0757-3. Epub 2004 Nov 3.
Tanaka Y, Gotani H, Sasaki K, Yoshimura T, Yagi H. Evaluation of intramedullary nail fixation via the Neviaser portal for proximal humerus fracture. J Clin Orthop Trauma. 2019;10(3):474–9. https://doi.org/10.1016/j.jcot.2019.02.007. Epub 2019 Feb 8.
Rommens PM, Blum J, Runkel M. Retrograde nailing of humeral shaft fractures. Clin Orthop Relat Res. 1998;350:26–39.
Rommens PM, Verbruggen J, Broos PL. Retrograde locked nailing of humeral shaft fractures. A review of 39 patients. J Bone Joint Surg Br. 1995;77(1):84–9.
Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2009;17(2):139–41. https://doi.org/10.1177/230949900901700202.
Singisetti K, Ambedkar M. Nailing versus plating in humerus shaft fractures: a prospective comparative study. Int Orthop. 2010;34(4):571–6. https://doi.org/10.1007/s00264-009-0813-2. Epub 2009 Jun 9.
Changulani M, Jain UK, Keswani T. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study. Int Orthop. 2007;31(3):391–5. https://doi.org/10.1007/s00264-006-0200-1. Epub 2006 Aug 10.
Benegas E, Ferreira Neto AA, Gracitelli ME, Malavolta EA, Assunção JH, Prada Fde S, Bolliger Neto R, Mattar R Jr. Shoulder function after surgical treatment of displaced fractures of the humeral shaft: a randomized trial comparing antegrade intramedullary nailing with minimally invasive plate osteosynthesis. J Shoulder Elb Surg. 2014;23(6):767–74. https://doi.org/10.1016/j.jse.2014.02.010. Epub 2014 Apr 24.
McCormack RG, Brien D, Buckley RE, McKee MD, Powell J, Schemitsch EH. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82(3):336–9. https://doi.org/10.1302/0301-620x.82b3.9675.
Chapman JR, Henley MB, Agel J, Benca PJ. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma. 2000;14(3):162–6. https://doi.org/10.1097/00005131-200003000-00002.
Beeres FJP, van Veelen N, Houwert RM, Link BC, Heng M, Knobe M, Groenwold RHH, Babst R, van de Wall BJM. Open plate fixation versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2021; https://doi.org/10.1007/s00068-021-01728-7. Epub ahead of print.
Paryavi E, Pensy RA, Higgins TF, Chia B, Eglseder WA. Salvage of upper extremities with humeral fracture and associated brachial artery injury. Injury. 2014;45(12):1870–5. https://doi.org/10.1016/j.injury.2014.08.038.
Chang AC, Ha NB, Sagar C, Bain GI, Leonello DT. The modified anterolateral approach to the humerus. J Orthop Surg (Hong Kong). 2019;27(3):2309499019865954. https://doi.org/10.1177/2309499019865954.
Gerwin M, Hotchkiss RN, Weiland AJ. Alternative operative exposures of the posterior aspect of the humeral diaphysis with reference to the radial nerve. J Bone Joint Surg Am. 1996;78(11):1690–5. https://doi.org/10.2106/00004623-199611000-00008.
Páramo-Díaz P, Arroyo-Hernández M, Rodríguez Vega V, Aroca-Peinado M, León-Baltasar JL, Caba-Doussoux P. Surgical treatment of extra-articular distal-third diaphyseal fractures of the humerus using a modified posterior approach and an extra-articular plate. Rev Esp Cir Ortop Traumatol. 2017;61(6):404–11. https://doi.org/10.1016/j.recot.2017.07.001. English, Spanish. Epub 2017 Sep 7.
Lu S, Wu J, Xu S, Fu B, Dong J, Yang Y, Wang G, Xin M, Li Q, He TC, Wang F, Zhou D. Medial approach to treat humeral mid-shaft fractures: a retrospective study. J Orthop Surg Res. 2016;11:32. https://doi.org/10.1186/s13018-016-0366-1.
Rellán I, Gallucci GL, Donndorff AG, De Carli P, Zaidenberg EE, Richard MJ, Boretto JG. Time until union in absolute vs. relative stability MIPO plating in simple humeral shaft fractures. Eur J Orthop Surg Traumatol. 2021; https://doi.org/10.1007/s00590-021-02920-6. Epub ahead of print.
O’Toole RV, Andersen RC, Vesnovsky O, Alexander M, Topoleski LD, Nascone JW, Sciadini MF, Turen C, Eglseder WA Jr. Are locking screws advantageous with plate fixation of humeral shaft fractures? A biomechanical analysis of synthetic and cadaveric bone. J Orthop Trauma. 2008;22(10):709–15. https://doi.org/10.1097/BOT.0b013e31818df8cb.
Gardner MJ, Griffith MH, Demetrakopoulos D, Brophy RH, Grose A, Helfet DL, Lorich DG. Hybrid locked plating of osteoporotic fractures of the humerus. J Bone Joint Surg Am. 2006;88(9):1962–7. https://doi.org/10.2106/JBJS.E.00893.
Karakasli A, Basci O, Ertem F, Sekik E, Havitcioglu H. Dual plating for fixation of humeral shaft fractures: a mechanical comparison of various combinations of plate lengths. Acta Orthop Traumatol Turc. 2016;50(4):432–6. https://doi.org/10.1016/j.aott.2016.07.002. Epub 2016 Jul 29.
Kosmopoulos V, Nana AD. Dual plating of humeral shaft fractures: orthogonal plates biomechanically outperform side-by-side plates. Clin Orthop Relat Res. 2014;472(4):1310–7. https://doi.org/10.1007/s11999-013-3379-7. Epub 2013 Nov 12.
Seo JB, Heo K, Yang JH, Yoo JS. Clinical outcomes of dual 3.5-mm locking compression plate fixation for humeral shaft fractures: comparison with single 4.5-mm locking compression plate fixation. J Orthop Surg (Hong Kong). 2019;27(2):2309499019839608. https://doi.org/10.1177/2309499019839608.
Sharaby M, Elhawary A. A simple technique for double plating of extraarticular distal humeral shaft fractures. Acta Orthop Belg. 2012;78(6):708–13.
Lee JK, Choi YS, Sim YS, Choi DS, Han SH. Dual plate fixation on distal third diaphyseal fracture of the humerus. Int Orthop. 2017;41(8):1655–61. https://doi.org/10.1007/s00264-016-3355-4. Epub 2016 Dec 1.
Streufert BD, Eaford I, Sellers TR, Christensen JT, Maxson B, Infante A, Shah AR, Watson DT, Sanders RW, Mir HR. Iatrogenic nerve palsy occurs with anterior and posterior approaches for humeral shaft fixation. J Orthop Trauma. 2020;34(3):163–8. https://doi.org/10.1097/BOT.0000000000001658.
Lee WY, Shin HD, Kim KC, Cha SM, Jeon YS. Relationship between incidence of postoperative radial nerve palsy and surgical experience in the treatment of humeral shaft fractures through a posterior triceps splitting approach: a retrospective study. Acta Orthop Traumatol Turc. 2021;55(4):338–43. https://doi.org/10.5152/j.aott.2021.20415.
Chang G, Ilyas AM. Radial nerve palsy after humeral shaft fractures: the case for early exploration and a new classification to guide treatment and prognosis. Hand Clin. 2018;34(1):105–12. https://doi.org/10.1016/j.hcl.2017.09.011.
Wang JP, Shen WJ, Chen WM, Huang CK, Shen YS, Chen TH. Iatrogenic radial nerve palsy after operative management of humeral shaft fractures. J Trauma. 2009;66(3):800–3. https://doi.org/10.1097/TA.0b013e31816142cf.
Vaishya R, Kandel IS, Agarwal AK, Vijay V, Vaish A, Acharya K. Is early exploration of secondary radial nerve injury in patients with humerus shaft fracture justified? J Clin Orthop Trauma. 2019;10(3):535–40. https://doi.org/10.1016/j.jcot.2018.11.002. Epub 2018 Nov 9.
Hegeman EM, Polmear M, Scanaliato JP, Nesti L, Dunn JC. Incidence and management of radial nerve palsies in humeral shaft fractures: a systematic review. Cureus. 2020;12(11):e11490. https://doi.org/10.7759/cureus.11490.
Fernández Dell’Oca AA. The principle of helical implants. Unusual ideas worth considering. Injury. 2002;33(Suppl 1):SA1–27. https://doi.org/10.1016/s0020-1383(02)00064-5.
Livani B, Belangero WD. Bridging plate osteosynthesis of humeral shaft fractures. Injury. 2004;35(6):587–95. https://doi.org/10.1016/j.injury.2003.12.003.
van de Wall BJM, Baumgärtner R, Houwert RM, Link BC, Heng M, Knobe M, Groenwold RHH, Babst R, Beeres FJP. MIPO versus nailing for humeral shaft fractures: a meta-analysis and systematic review of randomised clinical trials and observational studies. Eur J Trauma Emerg Surg. 2021; https://doi.org/10.1007/s00068-020-01585-w. Epub ahead of print.
Apivatthakakul T, Arpornchayanon O, Bavornratanavech S. Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury. 2005;36(4):530–8. https://doi.org/10.1016/j.injury.2004.05.036.
Livani B, Belangero WD, Castro de Medeiros R. Fractures of the distal third of the humerus with palsy of the radial nerve: management using minimally-invasive percutaneous plate osteosynthesis. J Bone Joint Surg Br. 2006;88(12):1625–8. https://doi.org/10.1302/0301-620X.88B12.17924.
Zhiquan A, Bingfang Z, Yeming W, Chi Z, Peiyan H. Minimally invasive plating osteosynthesis (MIPO) of middle and distal third humeral shaft fractures. J Orthop Trauma. 2007;21(9):628–33. https://doi.org/10.1097/BOT.0b013e31815928c2.
Apivatthakakul T, Phornphutkul C, Laohapoonrungsee A, Sirirungruangsarn Y. Less invasive plate osteosynthesis in humeral shaft fractures. Oper Orthop Traumatol. 2009;21(6):602–13. https://doi.org/10.1007/s00064-009-2008-9.
Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010;24(4):212–6. https://doi.org/10.1097/BOT.0b013e3181c2fe49.
Concha JM, Sandoval A, Streubel PN. Minimally invasive plate osteosynthesis for humeral shaft fractures: are results reproducible? Int Orthop. 2010;34(8):1297–305. https://doi.org/10.1007/s00264-009-0893-z. Epub 2009 Oct 21.
Lee HJ, Oh CW, Oh JK, Apivatthakakul T, Kim JW, Yoon JP, Lee DJ, Jung JW. Minimally invasive plate osteosynthesis for humeral shaft fracture: a reproducible technique with the assistance of an external fixator. Arch Orthop Trauma Surg 2013;133(5):649–657. doi: https://doi.org/10.1007/s00402-013-1708-7. Epub 2013 Mar 5.
Giordano M, Giordano V, Gameiro VS, Belangero W, Livani B, Giannoudis PV, Krettek C. Anterior minimally invasive plating osteosynthesis technique (MIPO) for humeral shaft fractures: an anatomical study of neuromuscular structures at risk. Eur J Orthop Surg Traumatol. 2021;31(3):449–58. https://doi.org/10.1007/s00590-020-02792-2. Epub 2020 Sep 14.
Shin SJ, Sohn HS, Do NH. Minimally invasive plate osteosynthesis of humeral shaft fractures: a technique to aid fracture reduction and minimize complications. J Orthop Trauma. 2012;26(10):585–9. https://doi.org/10.1097/BOT.0b013e318254895f.
López-Arévalo R, de Llano-Temboury AQ, Serrano-Montilla J, de Llano-Giménez EQ, Fernández-Medina JM. Treatment of diaphyseal humeral fractures with the minimally invasive percutaneous plate (MIPPO) technique: a cadaveric study and clinical results. J Orthop Trauma. 2011;25(5):294–9. https://doi.org/10.1097/BOT.0b013e3181f98421.
Ziran BH, Kinney RC, Smith WR, Peacher G. Sub-muscular plating of the humerus: an emerging technique. Injury. 2010;41(10):1047–52. https://doi.org/10.1016/j.injury.2010.04.021.
Ziran BH, Belangero W, Livani B, Pesantez R. Percutaneous plating of the humerus with locked plating: technique and case report. J Trauma. 2007;63(1):205–10. https://doi.org/10.1097/01.ta.0000231870.11908.3e.
Tetsworth K, Hohmann E, Glatt V. Minimally invasive plate osteosynthesis of humeral shaft fractures: current state of the art. J Am Acad Orthop Surg. 2018;26(18):652–61. https://doi.org/10.5435/JAAOS-D-17-00238.
Hohmann E, Glatt V, Tetsworth K. Minimally invasive plating versus either open reduction and plate fixation or intramedullary nailing of humeral shaft fractures: a systematic review and meta-analysis of randomized controlled trials. J Shoulder Elb Surg. 2016;25(10):1634–42. https://doi.org/10.1016/j.jse.2016.05.014. Epub 2016 Aug 10.
Keshav K, Baghel A, Kumar V, Neradi D, Kaustubh K, Mishra P. Is minimally invasive plating osteosynthesis better than conventional open plating for humeral shaft fractures? A systematic review and meta-analysis of comparative studies. Indian J Orthop. 2021;55(Suppl 2):283–303. https://doi.org/10.1007/s43465-021-00413-6.
Beeres FJ, Diwersi N, Houwert MR, Link BC, Heng M, Knobe M, Groenwold RH, Frima H, Babst R, van de Wall BJ. ORIF versus MIPO for humeral shaft fractures: a meta-analysis and systematic review of randomized clinical trials and observational studies. Injury. 2021;52(4):653–63. https://doi.org/10.1016/j.injury.2020.11.016. Epub 2020 Nov 6.
García-Virto V, Santiago-Maniega S, Llorente-Peris A, Simón-Pérez C, Álvarez-Ramos BA, García-Florez L, Aguado HJ. MIPO helical pre-contoured plates in diaphyseal humeral fractures with proximal extension. Surgical technique and results. Injury. 2021;52(Suppl 4):S125–30. https://doi.org/10.1016/j.injury.2021.01.049. Epub 2021 Feb 13.
Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011;6:CD005959. https://doi.org/10.1002/14651858.CD005959.pub2.
Gausepohl T, Koebke J, Pennig D, Hobrecker S, Mader K. The anatomical base of unilateral external fixation in the upper limb. Injury. 2000;31(Suppl 1):11–20. https://doi.org/10.1016/s0020-1383(99)00258-2.
Gosler MW, Testroote M, Morrenhof JW, Janzing HM. Surgical versus non-surgical interventions for treating humeral shaft fractures in adults. Cochrane Database Syst Rev. 2012;1:CD008832. https://doi.org/10.1002/14651858.CD008832.pub2.
Clement ND. Management of humeral shaft fractures; non-operative versus operative. Arch Trauma Res. 2015;4(2):e28013. https://doi.org/10.5812/atr.28013v2.
Rodríguez-Merchán EC. Compression plating versus hackethal nailing in closed humeral shaft fractures failing nonoperative reduction. J Orthop Trauma. 1995;9(3):194–7. https://doi.org/10.1097/00005131-199506000-00003.
Heineman DJ, Poolman RW, Nork SE, Ponsen KJ, Bhandari M. Plate fixation or intramedullary fixation of humeral shaft fractures. Acta Orthop. 2010;81(2):216–23. https://doi.org/10.3109/17453671003635884. Erratum in: Acta Orthop 2010;81(5):647.
Ouyang H, Xiong J, Xiang P, Cui Z, Chen L, Yu B. Plate versus intramedullary nail fixation in the treatment of humeral shaft fractures: an updated meta-analysis. J Shoulder Elb Surg. 2013;22(3):387–95. https://doi.org/10.1016/j.jse.2012.06.007. Epub 2012 Sep 1.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Gálvez-Sirvent, E., Ibarzabal-Gil, A., Rodríguez-Merchán, E.C. (2022). Humeral Shaft Fixation in Adults: Plate Fixation, Intramedullary Nail, or Nonoperative?. In: Rodríguez-Merchán, E.C., Moreno-Garcìa, A. (eds) Controversies in Orthopedic Surgery of The Upper Limb . Springer, Cham. https://doi.org/10.1007/978-3-031-04907-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-031-04907-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-04906-4
Online ISBN: 978-3-031-04907-1
eBook Packages: MedicineMedicine (R0)