Abstract
Autism spectrum disorder is a heterogeneous neurodevelopmental disorder characterized by repetitive patterns of behavior and deficits in social communication that affects approximately 1 in 45 adults. Many members of this population receive psychotropic medication, typically to reduce challenging responses or to treat comorbid psychiatric conditions, such as depression, anxiety, and attention-deficit/hyperactivity disorder. The scientific literature that supports this practice is neither large nor high quality and does not provide compelling support for the use of any medication for any purpose in this population. It leaves many important questions unanswered. We do not know, for instance, whether age modulates drug effects in people with autism spectrum disorder or whether autism spectrum disorder alters the effects of drugs. We also know very little about the long-term effects of psychotropic medications or about the effects of drug combinations, which is commonly prescribed. Despite the limitation of the literate, it is important to recognize that most studies report positive results, and it is clear that some adults with autism spectrum disorder derive significant benefit from psychotropic medications. Appropriate use of such drugs requires caregivers to ensure that (a) the goals of treatment are clear and in the client’s best interest, (b) treatment decisions are made on the basis of real drug effects, and (c) drug therapy is flexible and integrated with non-pharmacological interventions. If these provisions are met, psychotropic drugs can be a powerful tool for improving the lives of adults with autism.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Autism spectrum disorder (ASD) is a heterogeneous neurodevelopmental disorder characterized by restrictive, repetitive patterns of behavior and deficits in social communication and social interaction (American Psychiatric Association, 2013). ASD is common – data from the Autism and Developmental Disabilities Monitoring Network indicated that in 2016, 1 in 54 children met the criteria for being diagnosed with ASD (Maenner et al., 2020). It is also a persistent, lifelong disorder. As with everyone, the behavior of people with autism changes over the course of their lives, so do the challenges they face.
Physicians often prescribe psychotropic drugs – medications intended to improve mood, cognitive status, or overt behavior – to help people with ASD meet these challenges. Two medications, the antipsychotics aripiprazole (Abilify) and risperidone (Risperdal), are approved by the US Food and Drug Administration (FDA) for treating “irritability” in young people (6–17 years of age) with ASD and are widely used for this purpose. Other psychotropic medications are also commonly prescribed for members of this population. The effectiveness of psychotropic medications as a treatment for young people with ASD has generated substantial interest among researchers and scholars. As an example, VanDerwall et al. (2021) recently reviewed the effects of aripiprazole in people with ASD. They found 14 relevant studies and 12 review articles that summarized the research findings.
Although VanDerwall et al. (2021) included studies regardless of the age of participants, the oldest participant in any study was 22 years of age, and most involved only children and adolescents. Given the absence of relevant information, VanDerwall and colleagues emphasized that it is impossible to determine whether age modulates the effects of aripiprazole in people with ASD or to reach data-based conclusions about the effects of the drug in older members of this population.
The tendency of researchers to not include adult participants with ASD in drug research is not limited to studies of aripiprazole. Poling et al. (2017) recently summarized the effects of psychotropic drugs in people with ASD. In describing the limitations of the published research, they wrote: “The effects of psychotropic drugs in people [with ASD] past young adulthood remain to be determined” (Poling et al., 2017, p. 464). In making this point, they referred to a review by Dove et al. (2012), who examined eight studies that examined the effects of psychotropic medications in 13- to 30-year-old people with ASD. Four of the studies were of fair quality and four were of low quality. The scarcity of studies and the lack of good quality studies indicate a clear need for more, and better, drug research involving adults with ASD, because members of this population often receive psychotropic drugs.
Given the relative scarcity of research examining the effects of psychotropic drugs in adults with ASD, it is no surprise that many reviews of the psychopharmacology of ASD pay little or no attention to adults. Table 17.1 lists 28 reviews published since 2010 with the drug(s), target symptoms, and age range considered. Half of them considered research involving adults. None of their authors, except for VanDerwall et al. (2021), suggested that age influences the effects of psychotropic drugs in people with ASD.
It may well be that results obtained with children and adolescents with ASD generalize to older people. Even if this is so, the available research has serious limitations. Beginning with Greiner’s (1958) plea for good quality studies, researchers have pointed out that drug studies involving people with developmental disabilities, including ASD, often are poorly controlled and of limited scope (e.g., Gadow & Poling, 1986; Matson et al., 2000; Sprague & Werry, 1971).
In Poling et al.’s (2017) review of psychotropic medications for people with ASD, they described several limitations of the available research and explained the significance of these limitations. Those limitations are relevant to what is known about drug effects in all people with ASD, including adults. We list them below, with occasional comments pointing out particular relevance to adults. Please see Poling et al. for detailed, general discussion.
-
1.
There are no long-term studies of the value or adverse effects of drug treatments . By the time a person with ASD is 50 years of age, that individual may well have received a psychotropic drug every day for three or four decades, but nothing is known about the costs and benefits of such extended exposure.
-
2.
The probability of gender differences in drug effects has been largely ignored. It is interesting that Jobski et al. (2017) found that the sex of adults with ASD did not predict overall psychotropic drug use, but there was a difference in the kinds of drugs most often prescribed for men and women. Men more often received antipsychotics and medications identified to treat attention-deficit/hyperactivity disorder (ADHD) than women, whereas women were more likely to be treated with antidepressants and anxiolytics than were men. The factors responsible for this difference merit investigation.
-
3.
Very little is known about the effects of polypharmacy .
-
4.
Drug treatments are rarely compared to other treatments. Few drug versus drug comparisons have appeared. Comparisons of drug versus nondrug treatments are even rarer.
-
5.
The effects of combinations of psychotropic medications and non-pharmacological interventions are largely unknown.
-
6.
Measures of desired and side effects are often weak. As evidence, Brugha et al. (2015) reviewed studies that supposedly examined the effects of various interventions on the core symptoms of ASD in adults, including 19 drug studies. They found that measures were inconsistent and often inappropriate, noting: “Use of outcome measures varied with frequent use of non-standardized assessment, very little use of measures designed specifically for individuals with ASD or of instruments focusing on core ASD deficits, such as communication or social functioning” (Brugha et al., 2015, p. 99).
-
7.
Data analysis is often weak. In many studies with adults, the clinical significance of drug-induced changes is not considered. Rather, statistical significance revealed via an inferential statistic is the sole evidence of the supposed value of the medication.
-
8.
The possibility of bias affecting findings is high in many studies. Research funded by the manufacturers of psychotropic drugs raises this possibility.
-
9.
Predictors of positive responses to drugs have not been isolated. When data for individual adults with ASD are reported, there are individual differences in the effects of a medication, but the variables responsible for the differences are unknown. For example, McDougle et al. (1998) examined the effects of risperidone on the severe aggression of 14 adults with ASD. Eight responded favorably to the drug; six did not. The reason for the difference was unclear.
Despite these limitations, Poling et al. (2017) concluded that research supports three conclusions. They are as follows:
-
1.
A wide range of medications have been evaluated inadequately. Very few drugs have been studied in multiple, well-controlled trials using valid outcome measures. This poses a huge problem for physicians searching for evidence-based pharmacological interventions to benefit people with ASD. Huete et al. (2014) clearly described the problem they face: “…psychiatrists are challenged with basing their understanding of medication utility on a less that optimal body of research and more often on case study reports, and sometimes must refer to reported results and clinical trials of medications used in the general population for similar symptoms to guide their decision” (p. 736).
-
2.
Antipsychotic drugs often reduce challenging behaviors in children and adolescents. As noted, risperidone and aripiprazole are FDA-approved for this purpose (i.e., treating “irritability”). This is de facto evidence that a panel of experts deemed the data providing evidence of their value compelling.
-
3.
No drug significantly improves the core symptoms of autism. Although a well-tolerated medication that produced such an effect would revolutionize the treatment of people with ASD, such a drug is yet to appear.
In fairness, we must point out that some experts are more optimistic in their appraisal of the research literature than are Poling et al. (2017). Ethical and practical restrictions, coupled with very limited funding, make it difficult to conduct well-controlled research involving people with ASD. The results of limited, poorly controlled studies are often all that is available for assessing the value of pharmacological interventions, and experts differ in their willingness to accept the results of such studies. They also differ with respect to the criteria they apply when evaluating whether a study supports meaningful results. This is fine. Anyone interested in the psychopharmacology of ASD should contact multiple sources, such as the reviews listed in Table 17.1, and view all conclusions – including ours – with due skepticism. With that caution in mind, and an overview of the psychopharmacology of ASD as background, we now turn our attention specifically to adults.
Prevalence of Psychotropic Drug Use in Adults with Autism
A small number of studies have examined the prevalence of psychotropic drug use in adults with ASD. Prevalence rates differ substantially across studies, but, overall, their findings suggest that more than half of the members of this population are prescribed at least one psychotropic drug at a given point in time. Jobski et al. (2017) provided a systematic review of the use of psychotropic drugs in patients with ASD and reported a median prevalence level of 41.9% for 21 surveys that primarily involved children. They reported a median prevalence of 61.5% for six surveys that primarily involved adults.
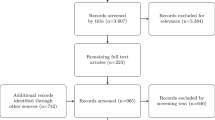
We conducted a literature search to find articles reporting prevalence rates that were published after the review by Jobski et al. (2017). We searched four databases (i.e., Cochrane Library, PubMed, Scopus, and Web of Science) using the terms “Autism Spectrum Disorder” AND “Adult” AND “Psychotropic drug.” This search produced 114 results. Two of us perused each article, selecting those that reported the prevalence of psychotropic drug use among adults with ASD. Five articles, listed in Table 17.2, reported prevalence. The median prevalence was 59%, with a range of 39–90%. These findings are comparable to the results of the studies summarized by Jobski et al.
In general, the probability that a person with ASD will receive at least one psychoactive drug increases with age, the presence of psychiatric comorbidity, the presence of concomitant intellectual disability (ID), and the occurrence of severe challenging behavior. These factors also appear to increase the probability of polypharmacy. Polypharmacy, which we define as the concurrent administration of two or more psychotropic medications (some researchers require three or more medications), is common when adults with ASD are considered. Jobski et al. (2017) reported a median polypharmacy level of 21.5% in studies primarily including children and 40.6% in those focusing on adults. We examined the articles revealed by our literature search to find those that reported the prevalence of polypharmacy. Seven, listed in Table 17.3, did so. The median prevalence of polypharmacy was 33%, slightly lower than that reported by Jobski et al. with a range of 19–75%.
Psychiatric Comorbidity and Autism in Adulthood
Many children and adolescents with ASD hurt themselves, damage property, have temper tantrums, and do other things that reduce the quality of their lives, limit their freedom and independence, and pose problems for caregivers (Matson & Rivet, 2008; Matson et al., 2011; Minshawi et al., 2014; Summers et al., 2017). Medical professionals frequently view such responses as indications of “irritability,” and both aripiprazole and risperidone are FDA-approved for treating irritability in children and adolescents with ASD. “Irritability” is not a disease, and the responses it comprises are often learned operant behavior that often can be treated effectively with non-pharmacological interventions (Poling et al., 2017). Nonetheless, the kinds of behavioral excesses comprised by “irritability” often persist into and sometimes develop during adulthood (Matson & Rivet, 2008).
Studies show that a substantial minority of adults with ASD engage in one or more forms of challenging behavior, including stereotypies, self-injury, temper tantrums, elopement, property destruction, and physical aggression (Matson et al., 2011). The likelihood of such behavior occurring increases when ID accompanies ASD and as ASD severity increases. Psychotropic medications are commonly prescribed to reduce such behaviors (Matson et al., 2011) in adults, as well as in children and adolescents, with ASD.
Psychotropic medications also are widely used to treat psychiatric comorbidities that accompany ASD. There is a substantial level of co-occurring psychiatric disorders in children and adolescents with ASD. It is not clear how comorbidities change across the lifetime, but psychiatric comorbidities are common in adults with ASD (Buck et al., 2014; Esler et al., 2019). Conditions that often occur in combination with ASD in adults are ADHD, mood disorders, and anxiety disorders (e.g., Hofvander et al., 2009; Joshi et al., 2013).
Psychiatric diagnosis is fraught with difficulty regardless of the population being diagnosed, but it is especially hard in people with ASD. This is because symptoms of ASD may overlap with symptoms of other disorders (e.g., ADHD, obsessive compulsive disorder [OCD]) and the communication impairments characteristic of ASD may limit the information (e.g., about thoughts and feelings) available to diagnosticians (Esler et al., 2019). The presence of ID can further challenge diagnosticians. Nonetheless, as noted, when adults with ASD experience problems involving their mood, cognitive status, or overt behavior, those problems often lead to a psychiatric diagnosis.
Psychotropic medications are the primary tool that psychiatrists and other physicians have available for helping people who have problems involving their mood, cognitive status, or overt behavior. Psychiatric diagnosis helps them to choose appropriate medications. If, for example, someone is diagnosed with major depressive disorder (American Psychiatric Association, 2013), a physician is almost certain to prescribe a drug that is FDA-approved for treating depression. More than 20 such medications are available. The choice of a medication is based upon an individual physician’s knowledge of and experience with individual drugs, including their side effects and specific indications and contraindications for their use.
Once a drug is selected, the physician selects a starting dose, which is often at the bottom of the suggested therapeutic range. The patient takes the drug for a sufficient period for it to have an effect, and then the severity of depression is assessed and compared to the level evident before treatment started. Standardized measures of severity, such as the Beck’s Depression Inventory (Bech et al., 1996), should be used, but clinical judgment and patient self-report are also important and in some cases are used alone. If no significant improvement is evident, the physician is likely to adjust the dose upward. If, again, no gain is evident, the physician is likely to try another antidepressant. This process is typically continued until, ideally, an effective medication is found or it becomes clear that the patient is not going to benefit from a single FDA-approved antidepressant. At that point, some physicians will try a drug that is not FDA-approved, which is an off-label application. Off-label prescribing is an accepted medical practice and is justified when there is sound evidence that the drug is likely to be beneficial.
As examples of an off-label application of a psychotropic drug, both aripiprazole and risperidone are approved to treat irritability in young people (6–17 years of age) with ASD. If a physician sees evidence of irritability in a 20-year-old person with ASD – and the evidence would be the occurrence of challenging behavior – it would be reasonable for the physician to prescribe one of these drugs off-label.
When no single drug produces the desired effect, some physicians will add a second drug to the treatment regimen, so the patient is simultaneously prescribed two psychotropic medications to treat the same condition, depression in our example, which is one form of polypharmacy. Simultaneously prescribing two or more drugs to treat two or more psychiatric conditions, such as a tricyclic antidepressant to treat depression and an antipsychotic to treat schizophrenia, is another form. Decisions regarding the continuation or modification of multi-drug regimens, like those concerning single drugs, should be made based on valid and reliable measures of the conditions being treated. Given the time and resource constraints faced by most practicing physicians, this is easier said than done.
People who come to physicians having problems with mood, cognitive status, or overt behavior, and their advocates when present, want and need help. Drugs are the main tools that physicians can use to help these people. Given this dynamic, patients and advocates are apt to encourage physicians to prescribe drugs, to keep searching for effective medications when initial attempts fail, and to not throw in the towel. Persistence is a virtue, and there is no doubt that psychotropic drugs benefit many patients, including adults with ASD. But with any treatment modality, it is all too easy to be convinced that an intervention, such as an antidepressant drug, is beneficial, when it is not actually changing the patient in the desired way.
Thompson (2007) provides an insightful discussion of why parents of children with ASD often persist with useless treatments. He notes that the absence of viable alternative treatments, the failure of prior treatments, the presence of small treatment effects, and the failure to systematically measure the problem the treatment is intended to solve are contributing factors. These same factors can influence the decisions that adults with ASD make about the treatments they receive. In many cases, however, such decisions will not be made by the adult with ASD but rather by legal guardians. They, too, are apt to be influenced by factors other than the actual effects of the intervention.
In some cases, there is compelling evidence that a given drug is widely effective in treating a diagnosed condition, so that a physician can treat the disorder with substantial confidence that the treatment will be effective. When drugs are FDA-approved for a particular indication, a panel of experts at the Center for Drug Evaluation and Research agrees that there is sufficient scientific evidence to conclude that the drug is safe and effective for a given use. This is not to say that everyone treated with the drug will derive significant benefits or that the drug is free of adverse effects, but only that the drug’s health benefits outweigh its known risks in a given population (US Food and Drug Administration, 2019).
Many drugs currently are FDA-approved for treating named psychiatric disorders in adults, and it is reasonable to assume that they are appropriate for treating adults with ASD diagnosed with these disorders. But two considerations call this assumption into question. One is the imprecision of psychiatric diagnosis, especially when applied to people with ASD. Obsessive-compulsive disorder (OCD) diagnosed in an adult with ASD is not necessarily the same condition as OCD in another adult with respect to manifestations and underlying cause. The other is that the presence of ASD might alter sensitivity to pharmacological interventions. The drug trials upon which FDA approval is based typically do not include people with ASD, and it is not given that the effects observed in other people will generalize to people with ASD. Of course, it is possible that the effects of psychotropic drugs do not differ as a function of the presence or absence of ASD and that psychiatric diagnosis in adults with ASD is accurate enough to not constitute a challenge. The only way to evaluate these possibilities is to consult the research literature and determine what is known about the effects of psychotropic drugs in adults with ASD.
Research Findings
Taylor (2016) provided an exhaustive review of studies examining the effects of psychotropic medications in adults with ASD that were published in the English language between 1985 and 2015. Taylor found and summarized 43 studies. As she classified the drugs, 13 studies examined selective serotonin reuptake inhibitors (i.e., fluoxetine 4, fluvoxamine 2, sertraline 2), two examined the tricyclic antidepressant clomipramine, two examined the serotonin norepinephrine inhibitor venlafaxine, one examined the norepinephrine reuptake inhibitor atomoxetine, one examined the benzodiazepine lorazepam, one examined the azapirone buspirone, one examined the anticonvulsant divalproex sodium, and one examined the psychostimulant methylphenidate. Miscellaneous agents were examined in six studies (i.e., naltrexone 3, clonidine 2, propranolol 1). Antipsychotic drugs were examined in 14 studies (i.e., aripiprazole 5, risperidone 4, clozapine 2, haloperidol 1, lithium 1, paliperidone 1, quetiapine 1).
Taylor (2016) provided information about the research designs of all studies she examined. Randomized between-groups, placebo-controlled studies enrolling a large number of participants, often termed “clinical trials,” are typically considered to be the “gold standard” in clinical psychopharmacology, with a pharmacological intervention considered as “evidence-based” when two (or more) such studies demonstrated its value (Reichow et al., 2008). The faith placed in such studies is so great, in fact, that some reviews of drug effects in people with ASD only consider them and exclude other research designs (e.g., Hirsch & Pringsheim, 2016; Maneeton et al., 2018).
There are good reasons for the scarcity of large-N, well-controlled studies of drug effects in adults with autism. Such studies are expensive and there is no ready source of funding. Practical and ethical considerations make such studies difficult to conduct and limit the range of tenable outcome measures. It is hard to access large numbers of adults with ASD, for (unlike, for instance, young people with ASD in school settings) they do not necessarily meet in sizeable groups. They are a protected group, which rightly causes Human Subjects Review Boards to look very carefully at research protocols involving them. Many adults with ASD receive one or more psychotropic medication, which may confound research involving other medications. Finally, limited access to and limited human resources for data collection prevent collecting detailed behavior data for large numbers of participants, especially over long periods of time.
Although not widely accepted in medicine, well-controlled small-N within-subject experiments can yield meaningful information about drug effects. Recognizing this, Reichow et al. (2008) developed a rubric that allows within-subject (which they term “single subject”) research designs to be considered in evaluating the evidence base for a particular application of an intervention. Applying the rubric categorizes an intervention as an established evidenced-based practice (EBP), a promising EBP, or not an EBP.
Taylor (2016) applied the rubric developed by Reichou et al. (2008) to determine the status of various psychotropic drugs as EBPs for targeted outcomes in adults with ASD. She concluded that two drugs, risperidone and fluoxetine, are promising EBPs in this population. To be considered a promising EBP as defined by Reichou et al., a drug can be shown to be effective in at least three single-subject studies of at least adequate research report strength meeting the following criteria: (1) conducted by at least two different research teams, (2) conducted in at least two different locations, and (3) total sample size of at least nine different participants across studies. A drug can also be deemed a promising EBP if it is shown to be effective in at least two group experimental design studies of at least adequate research report strength (the studies can be conducted by the same research team in the same location). More rigorous criteria must be met for a drug to be considered as an EBP.
With respect to specific applications for adults with ASD, Taylor (2016) concluded that “only two medications, risperidone and fluoxetine, met Reichow et al.’s (2008) criteria for promising evidence based interventions for reducing irritability and repetitive behaviour associated with ASD in adults” (p. 71). To examine whether studies published after her review elevate any drugs as an established EBP for adults with ASD, we examined all of the articles revealed by our literature search, described previously, and by a search of Google Scholar. Although research examining several drugs appeared, they were not sufficient to elevate any medication to the status of an established EBP. Published studies varied greatly in several respects, and we saw no evidence of a consistent and concerted effort to examine the effects of a particular medication on a significant outcome measure. To provide evidence of the broad and varied range of studies we examined, overviews of nine of them follow.
In 2016, Carminati et al. conducted a randomized, double-blind, placebo-controlled study to investigate the effectiveness of venlafaxine in treating behavioral disorders (i.e., irritability, hyperactivity/noncompliance, overall clinical performance) in 13 adults with ASD. Scores on the Aberrant Behavior Checklist and the Behavior Problems Inventory were the primary dependent variables. This study failed to provide clear evidence of a beneficial effect of venlafaxine, although the authors worked hard to find, via statistical analysis, a beneficial effect of the drug.
Joshi et al. (2016) evaluated memantine hydrochloride for the treatment of core social and cognitive deficits in 18 adults with high-functioning ASD using a prospective, 12-week, open-label trial. They found that memantine treatment significantly reduced scores on the Social Responsiveness Scale-Adult Research Version and Clinical Global Impression-Improvement subscale measures of autism severity. Moreover, the treatment led to significant improvement in ADHD and anxiety symptom severity, nonverbal communication, executive function, and neuropsychological assessment scores. The drug was well-tolerated by participants and was not associated with any serious adverse events. However, the design of the study is inadequate to support strong conclusions.
In a brief report, Olincy et al. (2016) utilized a double-blind placebo-controlled cross-over study to examine the effects of an investigational receptor-specific partial agonist drug (DMXB-A) on the inhibitory functions of the alpha7-nicotinic receptor gene (CHRNA7), in two adults with ASD. Abnormalities in this gene (i.e., CHRNA7) are common among individuals with ASD. They found that DMXB-A altered the biomarker for receptor activity and increased attention, as evidenced by self-reports and scores on the Attention Scale on the Repeatable Battery for the Assessment of Neuropsychological Status.
Umbricht et al. (2017) conducted a randomized, double-blind, placebo-controlled cross-over study, assessing the effects of a single dose of arginine vasopressin receptor 1A antagonist (RG7713) on eye tracking, behavioral and clinical measures of social cognition and communication, and safety and tolerability, in 19 adult males with ASD. Statistically significant effects were limited to improved eye tracking, providing preliminary evidence of a positive effect of RG7713 on social cognition.
In 2017, Quintana and colleagues conducted a randomized controlled trial that examined the effects of two doses of oxytocin administered using a novel Breath Powered intranasal delivery device. Seventeen male adults with ASD participated in the study. They received a randomized sequence of single-dose sessions which consisted of eight international units (IU) oxytocin, 24 IU oxytocin, or placebo, before completing four social-cognitive tasks. The primary outcome measure of “overt emotion salience” found a significant effect, with eight IU of oxytocin increasing overt emotion salience compared to placebo. However, there was no significant increase after 24 IU of oxytocin treatment. No significant effects were found in the remaining measures (reading the mind in the eyes task performance, emotional dot probe, and face morphing). It is not clear how overt emotion salience relates to the core symptoms of ASD, to challenging behavior, or to any psychiatric disorder.
Yamasue et al. (2018) examined the effects of intranasal oxytocin on the core social symptoms of ASD using a randomized clinical trial. One hundred and six adult males with ASD were assigned to either a placebo group or a treatment group. The treatment group received 481 units per day of intranasal oxytocin for a total of 6 weeks. No between-group differences were found on the Autism Diagnostic Observation Schedule reciprocity measure, as both the treatment and placebo groups saw a reduction in scores. Some secondary measures such as the Autism Diagnostic Observation Schedule repetitive behavior measure and the duration of gaze fixation on socially relevant regions were better in the treatment group, but others were not. The frequency of adverse events did not differ between groups. Yamasue et al. concluded that continuous intranasal oxytocin treatment, as administered in the study, could not be recommended as a treatment for the core social symptoms of high-functioning ASD in adult men. However, they did add that there was some evidence that oxytocin could be useful in treating repetitive behavior.
In 2018, Danforth et al. examined the feasibility and safety of 3,4-methylenedioxymethamphetamine (MDMA)-assisted psychotherapy on reduction of social fear and avoidance, characteristics that are common among people with ASD. They conducted a blinded, placebo-controlled pilot study, with 12 adults with ASD who displayed a marked to severe level of anxiety. Danforth et al. found statistical improvement in Liebowitz Social Anxiety Scale scores from baseline to 1 month post-intervention, for the MDMA group, as well as from baseline to the 6-month follow-up.
In 2019, Ballester and colleagues assessed the effectiveness and tolerability of agomelatine as a treatment for sleep problems in adults with both ASD and ID. They conducted a randomized controlled trial with 23 individuals between the ages of 23 and 47 years old, 87% of which were male and all presenting with insomnia symptoms prior to the start of the study. The primary measure was total sleep time, as measured by ambulatory circadian monitoring. Agomelatine treatment was effective in treating insomnia and circadian rhythm sleep problems in the targeted participants, with only mild and transient adverse events. Although not a core symptom of ASD, a challenging behavior, or a psychiatric disorder, sleep disturbance is common in people with ASD and can contribute to other problems, making the results of this study noteworthy.
Bolognani et al. (2019) also used a randomized, double-blind, placebo-controlled study to investigate the effects of balovaptan on the core symptoms of ASD (i.e., socialization and communication deficits), in 223 adult males with ASD. They observed no significant difference in the primary efficacy measure (i.e., Social Responsiveness Scale, second edition). However, balovaptan was associated with improvement in scores on the Vineland-II Adaptive Behavior Scale. Balovaptan is of particular interest because it was developed by Roche specifically as a treatment for ASD. As reported by Fierce Biotech (n.d.-b), animal research suggested that balovaptan, a vasopressin 1a receptor antagonist, could help neurons communicate, an action that might target the core symptoms of ASD. Initial results were promising, but that promise was not realized in a phase 3 clinical trial, which was abandoned early, along with the drug. This pattern of results resembles that observed previously with oxytocin, another neuropeptide.
Finally, Joshi et al. (2020) assessed the short-term tolerability and efficacy of liquid formulation extended-release methylphenidate (MPH-ER) for the treatment of adults with comorbid ADHD and high-functioning ASD. During a 6-week, open-label trial with 15 adults between the ages of 20 and 29 years old (80% male), MPH-ER was administered using a flexible titration schedule. Results indicated that short-term MPH-ER treatment was effective, with a significant improvement in ADHD severity. MPH-ER was also described as well-tolerated, although adverse effects of headache, insomnia, anxiety, and decreased appetite were experienced by 13 of 15 participants. Methylphenidate has been repeatedly shown to be effective in reducing indications of ADHD in other populations, and this study suggests that its values extend to adults with ASD. Unfortunately, the design of the study does not support strong conclusions.
Conclusions
More than four dozen studies of the effects of psychotropic drugs in people with ASD have included adult participants. These studies have examined several different drugs, representing all of the major classes of psychotropic medications and experimental compounds. Unfortunately, the design of most studies renders their results suggestive, but not compelling. There are, however, some points that the research supports. After examining what is known regarding the use of psychotropic drugs to benefit adults with ASD, we reached seven conclusions.
Many Adults with ASD Are Prescribed One or More Psychotropic Drugs
Prevalence values differ substantially across studies, but it is clear that many, perhaps most, adults with ASD receive at least one psychotropic medication and a substantial proportion of medicated individuals receive two or more drugs. The widespread use of such medications suggests that they produce substantial benefits. Critics of psychopharmacology point out that those benefits could take the form of profits for the people who manage or invest in big pharma, the representatives who market psychotropic drugs to physicians, and the physicians who prescribe them.
There is no doubt that the pharmacological industry markets drugs aggressively, sometimes inappropriately, and generates enormous profits. It is not uncommon for new drugs to be introduced with enormous fanfare only to subsequently fall from grace. Aripiprazole is a case in point (VanDerwall et al., 2021). There is reason to be skeptical of big pharma, but we are convinced that the vast majority of physicians are committed to the well-being of their patients and would not consistently prescribe drugs they knew to be useless, let alone harmful. Moreover, research supports the value of some such drugs.
Beneficial Effects Are Reported in Most Studies
In most, but not all, of the drug studies involving adult participants with ASD reviewed by Taylor (2016), and in the subsequent studies we analyzed, some evidence of benefit was provided. This held, regardless of the drug class or specific drug evaluated, the design of the experiment or the outcome measure used. It is fair to state that, at present, there is insufficient evidence to support the use of any drug for any indication in an adult with ASD as an established EBP. But it is unfair to claim that there is no evidence that medications produce beneficial effects; there is such evidence. Moreover, many drugs are FDA-approved for specific indications in the adult population at large. If these indications, namely, psychiatric comorbidities, are present in adults with ASD, their use with these adults is appropriate. But, as noted previously, accurately diagnosing psychiatric disorders in adults with ASD is difficult, especially in individuals with comorbid ID. In addition, it is unclear whether the presence of ASD modulates the effects of psychotropic medications. Given this state of affairs, one can never be confident that a given medication will benefit an adult with ASD who receives it. Careful monitoring of desired and adverse drug effects is the quintessence of appropriate psychotropic drug treatments. This is an important point to which we will return.
There Is No Evidence That Age Influences Drug Effects in People with ASD
Most reviews of the pharmacological treatment of people with ASD emphasize findings with children and adolescents, although some of them include studies with adults. Table 17.1 lists 28 reviews published since 2010. Readers seeking detailed information about the pharmacological treatment of people with ASD should consult these reviews. Given the focus of the present chapter, it is interesting that their authors do not indicate that age modulates the clinical value of psychotropic medications. Although they vary in how strongly they endorse the use of pharmacological interventions for people with ASD, these authors generally agree that there are substantial limitations in the research base, that aripiprazole and risperidone are often useful for reducing challenging behavior, and that medications should be used with caution because of their potential side effects.
As we noted in another review (Poling et al., 2017), however, there are no systematic comparisons of the effects of psychotropic drugs across age groups. Many studies that include adults also include younger people but fail to disaggregate the data as a function of age. Had such disaggregation occurred and a large enough number of patients of different ages been studied, an effect of age might have been revealed. The effects of age also could be examined by comparing drug effects in similar studies that used different age groups, but such studies do not exist. The limited information that is available suggests that age does not strongly influence how people with ASD respond to psychotropic medications, but support for this proposition is decidedly weak. Almost nothing is known about the effects of psychotropic medication in elderly people with ASD. Given the issues associated with geriatric psychopharmacology in the general population (Meyers & Jeste, 2010), this is unfortunate.
It Is Not Clear Whether ASD Modulates the Effects of Psychotropic Drugs
It is not clear because compelling comparisons of the effects of the same doses of drugs on the same outcome measures in similar-aged adults with and without ASD have not appeared. Functional and structural brain characteristics that differ between people who are and who are not diagnosed with ASD underpin the behavioral differences responsible for the diagnosis. As Thompson (2007) points out, “Collectively, the available evidence suggests that the symptoms of ASDs can be traced to dysfunctions in specific brain areas, primarily the amygdala, prefrontal and parietal motor areas (minor neurons), orbitofrontal cortex, fusiform face area, cingulate, basal ganglia, and the two primary speech areas” (p. 37). It is logical to expect these dysfunctions to qualitatively or quantitatively alter the effects of psychotropic drugs and research examining this possibility is merited.
Researchers have made significant progress in determining the genetic and neurochemical mechanisms responsible for ASD (see Crespi, 2019; Marotta et al., 2020). Knowledge of the biological mechanisms responsible for the core symptoms of ASD, as well as the psychiatric disorders and challenging behavior that frequently accompany ASD, might well provide a logical rational basis for pharmacological interventions. Work in this direction is ongoing (Crespi, 2019).
It is noteworthy that two companies, Novartis and Sangamo, recently inked a $75,000,000 deal to work jointly to develop targeted drugs for treating ASD, with up to an additional $720,000,000 available to Sangamo across 3 years if milestones are met (Fierce Biotech, n.d.-a). The two companies will partner to use Sanomo’s proprietary genome regulation technology to alter activity in three genes believed to be involved in ASD and ID. Success is far from a given, but, should it occur, it would fundamentally alter the way medications for ASD are designed, their mechanism of action, and, ideally, their benefits for recipients.
All psychotropic drugs can produce side effects, although the nature, likelihood, potential severity, and reversibility of these untoward effects differ across medications. It is possible that the neurological dysfunctions responsible for ASD alter the likelihood and the severity of some medications, although whether this occurs has not been determined.
More, and Better, Research Is Needed
There is much of importance regarding the effects of psychotropic drugs in people with ASD, regardless of their age, that has not been adequately examined. Additional, well-controlled research in several areas is obviously needed. But, as we have also noted, conducting research involving participants with ASD is difficult, and there is little funding to support it. Small-N repeated measures experimental designs, although not generally accepted in medicine, can yield valuable important information about the effects of psychotropic medications (Poling et al., 2010; Weeden et al., 2010). Adopting this approach to research would make it easier to conduct drug studies involving adults with ASD. But it is essential that small-N studies, like traditional clinical trials, be well-controlled, with sound experimental designs, double-blinds, placebo controls, and appropriate outcome measures. Few such studies have occurred and this approach does not appear to be gaining favor.
For the foreseeable future, people with ASD and their caregivers who are seeking benefit from psychotropic drugs can know all there is to know about these medications and still lack important information regarding risks and benefits. The same is true of the physicians who prescribe such medications. Nonetheless, it is clearly evident that, when used appropriately, psychotropic medications significantly benefit many adults with ASD. The key phrase here is “when used appropriately.”
EBP for an Individual Constitutes Appropriate Drug Use
We have suggested elsewhere (e.g., Poling, 1994; Poling & Ehrhardt, 1999; Weeden et al., 2010) that the essence of appropriate use of psychotropic drugs entails the following:
-
1.
Ensuring that the goals of treatment are clear and in the client’s best interest.
-
2.
Ensuring that treatment decisions are made on the basis of real drug effects.
-
3.
Ensuring that drug therapy is flexible and integrated with non-pharmacological interventions.
In pursuing these objectives, practitioners are behaving in a manner consistent with best practice guidelines. Table 17.4 provides a list of such guidelines, slightly modified from the recommendations of the American Academy of Child and Adolescent Psychiatry (Walkup et al., 2009) for the appropriate use of psychotropic medications in children. Age and the presence of ASD do not alter the fundamentals of appropriate medication use. Following the guidelines listed in Table 17.4 goes far in ensuring that psychotropic medications are used appropriately in adults with ASD.
These guidelines are based on the use of EBPs. Appropriate use of EBPs involves three steps for each individual to be treated. First, the condition to be treated is quantified, which may, but need not, involve assigning a diagnostic label. Second, an intervention, such as a psychotropic medication, for which there is good scientific evidence to support its value in treating that condition, is selected. Third, the effects of that intervention, both desired and adverse, are evaluated in the treated individual, and decisions about subsequent treatment are based on the results of this evaluation.
The third step is the most important one. If it can be shown that receiving a psychotropic medication clearly improves the quality of life of an adult with ASD, then that medication is, for that person, an EBP and, put simply, a good thing. Unfortunately, in everyday situations, it is often hard to adequately determine whether a drug is producing either desired or significant adverse effects. It is generally assumed that neurotypical adults can, in consultation with their physicians, make sound judgments about how a psychotropic medication is affecting them and rationally choose whether to continue, alter, or terminate treatment. Some adults with ASD have the capacity to do likewise, but others do not. In the latter case, special care should be taken to ensure that decisions are based on actual, rather than hoped-for, beneficial effects, a point Thomas Greiner (1958) made more than 40 years ago, when he noted that, when it came to psychotropic medication, children and developmentally disabled people require special protections. Physicians alone are rarely in a position to collect the data needed to fully profile the effects of a psychotropic medication, and it is wise to enlist members of other professions, such as behavior analysts, to assist (see Weeden et al., 2010).
Of course, non-pharmacological alternatives have been shown to be of value for treating challenging behaviors and psychiatric comorbidities, and the doctrine of least restrictive alternatives suggests that they deserve consideration prior to drug treatment. But in many cases, such treatments are not available or have been tried and failed. Psychotropic medications can play a valuable role in the lives of adults with ASD. Because of the risks they pose, they are best used at the lowest dose and for the shortest time possible, but that by no means makes them bad. To borrow a metaphor from Travis Thompson (2007) categorizing psychotropic drugs as “bad” or “good” is as foolish as doing the same for rain. Clearly, both depend on the situation. Rain is bad in the midst of a flood, a blessing in a drought. A psychotropic drug that causes tardive dyskinesia and changes nothing for the better is bad; a drug that relieves suffering is good. Psychotropic drugs are powerful tools that need to be used with care and caution. When they are, they can greatly benefit adults with ASD. Providing psychiatrists and other physicians with appropriate training regarding ASD and the effects of psychotropic drugs in this population, including strategies for evaluating drug effects, would go far in making this happen. Fostering in caregivers and advocates a skeptical, but not cynical, perspective on the use of psychotropic drugs would do the same. If this chapter has helped to foster such an attitude in you, the reader, then our goal in writing is met, and we are pleased.
References
Aman, M. G., Smith, T., Arnold, L. E., Corbett-Dick, P., Tumuluru, R., Hollway, J. A., Hyman, S. L., Mendoza-Burchamm, M., Pan, X., Mruzek, D. W., Lecavalier, L., Levato, L., Silverman, L. B., & Handen, B. (2014). A review of atomoxetine effects in young people with developmental disabilities. Research in Developmental Disabilities, 35, 1412–1424. https://doi.org/10.1016/j.ridd.2014.03.006
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author.
Axmon, A., Kristensson, J., Ahlström, G., & Midlöv, P. (2017). Use of antipsychotics, benzodiazepine derivatives, and dementia medication among older people with intellectual disability and/or autism spectrum disorder and dementia. Research in Developmental Disabilities, 62, 50–57. https://doi.org/10.1016/j.ridd.2017.01.001
Ballester, P., Martínez, M. J., Inda, M. D., Javaloyes, A., Richdale, A. L., Muriel, J., Belda, C., Toral, N., Morales, D., Fernández, E., & Peiró, A. M. (2019). Evaluation of agomelatine for the treatment of sleep problems in adults with autism spectrum disorder and co-morbid intellectual disability. Journal of psychopharmacology (Oxford, England), 33, 1395–1406. https://doi.org/10.1177/0269881119864968
Baribeau, D. A., & Anagnostou, E. (2013). Social communication is an emerging target for pharmacotherapy in autism spectrum disorder – A review of the literature for potential agents. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 23, 20–30.
Bartram, L. A., Lozano, J., & Coury, D. L. (2019). Aripiprazole for treating irritability associated with autism spectrum disorders. Expert Opinion on Pharmacotherapy, 20, 1421–1427. https://doi.org/10.1080/14656566.2019.1626825
Bech, P., Hamilton, M., & Zung, W. W. K. (1996). The Bech, Hamilton, and Zung Scales for mood disorders: Screening and listening (2nd ed.). Springer.
Bolognani, F., Del Valle Rubido, M., Squassante, L., Wandel, C., Derks, M., Murtagh, L., Sevigny, J., Khwaja, O., Umbricht, D., & Fontoura, P. (2019). A phase 2 clinical trial of a vasopressin V1a receptor antagonist shows improved adaptive behaviors in men with autism spectrum disorder. Science Translational Medicine, 11, eaat 7838. https://doi.org/10.1126/scitranslmed.aat7838
Brugha, T. S., Doos, L., Tempier, A., Einfeld, S., & Howlin, P. (2015). Outcome measures in intervention trials for adults with autism spectrum disorders: A systematic review of assessments of core autism features and associated emotional and behavioural problems. Internal Journal of Measures in Psychiatric Research, 24, 99–115. https://doi.org/10.1002/mpr.1466
Buck, T. R., Viskochil, J., Farley, M., Coon, H., McMahon, W. M., Morgan, J., & Bilder, D. A. (2014). Psychiatric comorbidity and medication use in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 3063–3071. https://doi.org/10.1007/s10803-014-2170-2
Carminati, G. G., Gerber, F., Darbellay, B., Kosel, M. M., Deriaz, N., Chabert, J., Fathi, M., Bertschy, G., Ferrero, F., & Carminati, F. (2016). Using venlafaxine to treat behavioral disorders in patients with autism spectrum disorder. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 65, 85–95. https://doi.org/10.1016/j.pnpbp.2015.09.002
Ching, H., & Pringsheim, T. (2012). Aripiprazole for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews, 5. https://doi.org/10.1002/14651858.CD009043.pub2
Crespi, J. (2019). Comparative psychopharmacology of autism and psychotic-affective disorders suggests new targets for treatment. Evolution, Medicine, and Public Health, 1, 149–168. https://doi.org/10.1093/emph/eoz022
Cvejic, R. C., Arnold, S. R. C., Foley, K., & Trollor, J. N. (2018). Neuropsychiatric profile and psychotropic medication use in adults with autism spectrum disorder: Results from the Australian Longitudinal Study of Adults with Autism. BJPsych Open, 4, 461–466. https://doi.org/10.1192/bjo.2018.64
Danforth, A. L., Grob, C. S., Struble, C., Feduccia, A. A., Walker, N., Jerome, L., Yazar-Klosinski, B., & Emerson, A. (2018). Reduction in social anxiety after MDMA-assisted psychotherapy with autistic adults: A randomized, double-blind, placebo-controlled pilot study. Psychopharmacology, 235, 3137–3148. https://doi.org/10.1007/s00213-018-5010-9
Dove, D., Warren, Z., McPheeters, M. L., Taylor, J. L., Sathe, N. A., & Veenstra-Vander Weele, J. (2012). Medications for adolescents and young adults with autism spectrum disorders: A systematic review. Pediatrics, 130, 717–726. https://doi.org/10.1542/peds.2012-0683
Doyle, C. A., & McDougle, C. J. (2012). Pharmacologic treatments for the behavioral symptoms associated with autism spectrum disorders across the lifespan. Dialogues in Clinical Neuroscience, 14, 263–279. https://doi.org/10.31887/DCNS.2012.14.3/cdoyle
Elbe, D., & Lalani, Z. (2012). Review of the pharmacotherapy of irritability of autism. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 21, 130–146.
Esler, A., Hewitt, A., Hall-Lande, J., Pettingell, S. L., & Houseworth, J. (2019). Psychotropic medication use for adults with autism spectrum disorder who receive services and supports through adults developmental disability services in the United States. Journal of Autism and Developmental Disorders, 49, 2291–2303. https://doi.org/10.1007/s10803-019-03903-7
Espadas, C., Ballester, P., Londoño, A. C., Almenara, S., Aguilar, V., Belda, C., Pérez, E., & Peiró, A. M. (2020). Multimorbidity and psychotropic polypharmacy among participants with autism spectrum disorder with intellectual disability. Psychiatry Research, 292. https://doi.org/10.1016/j.psychres.2020.113321
Farmer, C. A., & Aman, M. G. (2011). Aripiprazole for the treatment of irritability associated with autism. Expert Opinion on Pharmacotherapy, 12, 635–640. https://doi.org/10.1517/14656566.2011.557661
Fierce Biotech. (n.d.-a). Novartis, Sangamo team up on genetic meds for autism in $75M deal. Downloaded March 2, 2021 from https://www.fiercebiotech.com/biotech/novartis-sangamo-team-up-genetic-meds-for-autism-75m-deal
Fierce Biotech. (n.d.-b). Special reports: 2 Balovaptan. Downloaded March 23, 2021 from https://www.fiercebiotech.com/special-report/2-balovaptan-2020-s-top-10-clinical-trial-flops
Frye, R. E., Rossignol, D., Casanova, M. F., Brown, G. L., Martin, V., Edelson, S., Coben, R., Lewine, J., Slattery, J. C., Lau, C., Hardy, P., Fatemi, S. H., Folsom, T. D., MacFabe, D., & Adams, J. B. (2013). A review of traditional and novel treatments for seizures in autism spectrum disorder: Findings from a systematic review and expert panel. Frontiers in Public Health. https://doi.org/10.3389/fpubh.2013.00031
Fung, L. K., Chahal, L., Libove, R. A., Bivas, R., & Hardan, A. (2012). A retrospective review of the effectiveness of aripiprazole in the treatment of sensory abnormalities in autism. Journal of Child and Adolescent Psychopharmacology, 22, 245–248. https://doi.org/10.1089/cap.2010.0103
Fusar-Poli, L., Brondino, N., Rocchetti, M., Petrosino, B., Arillotta, D., Damiani, S., Provenzani, U., Petrosino, C., Aguglia, E., & Pierluigi, P. (2019). Prevalence and predictors of psychotropic medication use in adolescents and adults with autism spectrum disorder in Italy: A cross-sectional study. Psychiatry Research, 276, 203–209. https://doi.org/10.1016/j.psychres.2019.04.013
Gadow, K., & Poling, A. (1986). Methodological issues in human psychopharmacology. JAI Press.
Ghanizadeh, A. (2012). Atomoxetine for treating ADHD symptoms in autism: A systematic review. Journal of Attention Disorders, 17, 635–640. https://doi.org/10.1177/1087054712443154
Ghanizadeh, A., Tordjman, S., & Jaafari, N. (2015). Aripiprazole for treating irritability in children & adolescents with autism: A systematic review. Indian Journal of Medical Research, 142, 269–275. https://doi.org/10.4103/0971-5916.166584
Greiner, T. (1958). Problems in methodology in research with drugs. American Journal of Mental Deficiency, 64, 346–352.
Guénolé, F., Godbout, R., Nicolas, A., Franco, P., Claustrat, B., & Baleyte, J. M. (2011). Melatonin for disordered sleep in individuals with autism spectrum disorders: Systematic review and discussion. Sleep Medicine Reviews, 15, 379–387. https://doi.org/10.1016/j.smrv.2011.02.001
Hirsch, L. E., & Pringsheim, T. (2016). Aripiprazole for autism spectrum disorders (ASD). Cochrane Database of Systematic Reviews, 6. https://doi.org/10.1002/14651858.CD009043.pub3
Hofvander, B., Delorme, R., Chaste, P., Nyden, A., Wentz, E., Stahlberg, O., Herbrecht, E., Stopin, A., Anckarsater, H., Gillberg, C., Rastam, M., & Leboyer, M. (2009). Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry, 9, 35. https://doi.org/10.1186/1471-244X-9-35
Huete, J., Schmidt, J., & Lopez-Arvizu, D. (2014). Behavioral disorders in young children with autism spectrum disorder. In J. Tarbox, D. R. Dixon, P. Sturmey, & J. L. Matson (Eds.), Handbook of early intervention for autism spectrum disorders (pp. 717–752). Springer.
Jenabi, E., Ataei, S., & Bashirian, S. (2019). Evaluation of drug interventions for the treatment of sleep disorders in children with autism spectrum disorders: A systematic review. Korean Journal of Pediatrics, 62, 405–409. https://doi.org/10.3345/kjp.2019.00668
Jobski, K., Höfer, J., Hoffmann, F., & Bachmann, C. (2017). Use of psychotropic drugs in patients with autism spectrum disorders: A systematic review. Acta Psychiatrica Scandinavica, 135, 8–28. https://doi.org/10.1111/acps.12644
Joshi, G., Wozniak, J., Petty, C., Martelon, M. K., Friend, R., Bolfek, A., Kotte, A., Stevens, J., Furtak, S. L., Bourgeois, M., Caruso, J., Caron, A., & Biederman, J. (2013). Psychiatric comorbidity and functioning in a clinically referred population of adults with autism spectrum disorders: A comparative study. Journal of Autism and Developmental Disorders, 43, 1314–1325. https://doi.org/10.1007/s10803-012-1679-5
Joshi, G., Wozniak, J., Faraone, S. V., Fried, R., Chan, J., Furtak, S., Grimsley, E., Conroy, K., Kilcullen, J. R., Woodworth, K. Y., & Biederman, J. (2016). A prospective open-label trial of memantine hydrochloride for the treatment of social deficits in intellectually capable adults with autism spectrum disorder. Journal of Clinical Psychopharmacology, 36, 262–271. https://doi.org/10.1097/jcp.0000000000000499
Joshi, G., DiSalvo, M., Wozniak, J., Ceranoglu, T. A., Yule, A., Surman, C., Fried, R., Galdo, M., Hoskova, B., Belser, A., & Biederman, J. (2020). A prospective open-label trial of long-acting liquid methylphenidate for the treatment of attention deficit/hyperactivity disorder in intellectually capable adults with autism spectrum disorder. The World Journal of Biological Psychiatry, 21, 274–290. https://doi.org/10.1080/15622975.2019.1679392
Krishnaswami, S., McPheeters, M., & Veenstra-Vaderweele, J. (2011). A systematic review of secretin with children with autism spectrum disorders. Pediatrics, 127, 1322–1325. https://doi.org/10.1542/peds.2011-0428
Maenner, M. J., Shaw, K. A., Baio, J., Washington, A., Patrick, M., DiRienzo, M., … Dietz, P. M. (2020). Prevalence of autism spectrum disorder among children aged 8 years – Autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveillance Summaries, 69, 1–12. https://doi.org/10.15585/mmwr.ss6904a1
Maneeton, N., Maneeton, B., Putthisri, S., Suttajit, S., Likhitsathian, S., & Srisurapanoont, M. (2018). Aripiprazole in acute treatment of children and adolescents with autism spectrum disorder: A systematic review and meta-analysis. Neuropsychiatric Disease and Treatment, 14, 3063–3072. https://doi.org/10.2147/ndt.s174622
Marotta, R., Risoleo, M. C., Messina, G., Parisi, L., Carotenuto, M., Vetri, L., & Roccella, M. (2020). The neurochemistry of autism. Brain Sciences, 10(3), 63. https://doi.org/10.3390/brainsci10030163
Matson, J. L., & Rivet, T. T. (2008). Characteristics of challenging behaviours in adults with autistic disorder, PDD-NOS, and intellectual disability. Journal of Intellectual and Developmental Disability, 33, 323–329. https://doi.org/10.1080/13668250802492600
Matson, J. L., Bamburg, J. W., Mayville, E. A., Pinkston, J., Bielecki, J., Kuhn, D., Smalls, Y., & Logan, J. R. (2000). Psychopharmacology and mental retardation: A 10 year review (1990-1999). Research in Developmental Disabilities, 21, 263–296. https://doi.org/10.1016/s0891-4222(00)00042-1
Matson, J. L., Sipes, M., Fodstad, J. C., & Fitzgerald, M. E. (2011). Issues in the management of challenging behaviours of adults with autism spectrum disorders. CNS Drugs, 25, 597–606. https://doi.org/10.2165/11591700-000000000-00000
McDougle, C. J., Holmes, J. O., Carlson, R. C., et al. (1998). A double-blind placebo-controlled study of risperidone in adults with autistic disorder and other pervasive developmental disorders. Archives of General Psychiatry, 55, 633–641. https://doi.org/10.1001/archpsyc.55.7.633
McPheeters, M. L., Warren, Z., Sathe, N., Bruzek, J. L., Krishnaswami, S., Jerome, R. N., & Veenstra-Vanderwheele, J. (2011). A systematic review of medical treatments for children with autism spectrum disorder. Pediatrics, 127, 1312–1321. https://doi.org/10.1542/peds.2011-0427
Meyers, B. S., & Jeste, D. V. (2010). Geriatric psychopharmacology: Evolution of a discipline. The Journal of Clinical Psychiatry, 71, 1416–1424. https://doi.org/10.4088/jcp.10r06485gry
Minshawi, N. F., Hurwitz, S., Fodstad, J. C., Biebl, S., Morriss, D. H., & McDougle, C. J. (2014). The association between self-injurious behaviors and autism spectrum disorders. Psychology Research and Behavior Management, 7, 125–136. https://doi.org/10.2147/PRBM.S44635
Mohiuddin, S., & Ghaziuddin, M. (2013). Psychopharmacology of autism spectrum disorders: A selective review. Autism, 17, 645–654. https://doi.org/10.1177/1362361312453776
Nylander, L., Axmon, A., Björne, P., Ahlström, G., & Gillberg, C. (2018). Older adults with autism spectrum disorders in Sweden: A register study of diagnoses, psychiatric care utilization and psychotropic medication of 601 individuals. Journal of Autism and Developmental Disorders, 48, 3076–3085. https://doi.org/10.1007/s10803-018-3567-0
Olincy, A., Blakeley-Smith, A., Johnson, L., Kem, W. R., & Freedman, R. (2016). Brief report: Initial trial of alpha 7-nicotinic receptor stimulation in two adult patients with autism spectrum disorder. Journal of Autism and Developmental Disorders, 46, 3812–2817. https://doi.org/10.1007/s10803-016-2890-6
Poling, A. (1994). Pharmacological treatment of behavioral problems in people with mental retardation: Some ethical considerations. In L. J. Hayes, G. J. Hayes, S. C. Moore, & P. M. Ghezzi (Eds.), Ethical issues in developmental disabilities (pp. 149–177). Context Press.
Poling, A., & Ehrhardt, K. (1999). Applied behavior analysis, social validation, and the psychopharmacology of mental retardation. Mental Retardation and Developmental Disabilities Research Reviews, 5, 342–347. https://doi.org/10.1002/(SICI)1098-2779(1999)5:4%3C342::AID-MRDD12%3E3.0.CO;2-7
Poling, A., Ehrhardt, K., Wood, A., & Bowerman, R. (2010). Psychopharmacology and behavior analysis in autism treatment. In E. A. Mayville & J. A. Mulick (Eds.), Behavioral foundations of effective autism treatment (pp. 257–275). Sloan.
Poling, A., Ehrhardt, K., & Li, A. (2017). Psychotropic medications as treatments for people with autism spectrum disorders. In J. Matson (Ed.), Handbook of treatments for autism spectrum disorder (pp. 459–471). Springer.
Preti, A., Melis, M., Siddi, S., Vellante, M., Doneddu, G., & Fadda, R. (2014). Oxytocin and autism: A systematic review of randomized controlled trials. Journal of Child and Adolescent Psychopharmacology, 24, 54–68. https://doi.org/10.1089/cap.2013.0040
Quintana, D. S., Westlye, L. T., Hope, S., Nærland, T., Elvsåshagen, T., Dørum, E., Rustan, Ø., Valstad, M., Rezvaya, L., Lishaugen, H., Stensønes, E., Yaqub, S., Smerud, K. T., Mahmoud, R. A., Djupesland, P. G., & Andreassen, O. A. (2017). Dose-dependent social-cognitive effects of intranasal oxytocin delivered with novel breath powered device in adults with autism spectrum disorder: A randomized placebo-controlled double-blind crossover trial. Translational Psychiatry, 7, E1136. https://doi.org/10.1038/tp.2017.103
Reichow, B., Volkmar, F. R., & Cicchetti, D. V. (2008). Development of the evaluative method for evaluating and determining evidence-based practices in autism. Journal of Autism and Developmental Disorders, 38, 1311–1319. https://doi.org/10.1007/s10803-007-0517-7
Reichow, B., Volkmar, F. R., & Bloch, M. H. (2013). Systematic review and meta-analysis of pharmacological treatment of the symptoms of attention-deficit/hyperactivity disorder in children with pervasive developmental disorders. Journal of Autism and Developmental Disorders, 43, 2435–2441. https://doi.org/10.1007/s10803-013-1793-z
Rizzo, R., & Pavone, P. (2016). Aripiprazole for the treatment of irritability and aggression in children and adolescents affected by autism spectrum disorders. Expert Review of Neurotherapeutics, 16, 867–874. https://doi.org/10.1080/14737175.2016.1211007
Rossignol, D. A., & Frye, R. E. (2014). The use of medications approved for Alzheimer’s disease in autism spectrum disorder: A systematic review. Frontiers in Pediatrics, 2, 1–8. https://doi.org/10.3389/2Ffped.2014.00087
Roy, A., Roy, M., Deb, S., Unwin, G., & Roy, A. (2015). Are opioid antagonists effective in attenuating the core symptoms of autism spectrum conditions in children: A systematic review. Journal of Intellectual Disability Research, 59, 293–306. https://doi.org/10.1111/jir.12122
Siegel, M., & Beaulieu, A. A. (2012). Psychotropic medications in children with autism spectrum disorders: A systematic review and synthesis for evidence-based practice. Journal of Autism and Developmental Disorders, 42, 1592–1605. https://doi.org/10.1007/s10803-011-1399-2
Sprague, R. L., & Werry, J. L. (1971). Methodology of psychopharmacological studies with the retarded. In N. R. Ellis (Ed.), International review of research in mental retardation (Vol. 5, pp. 147–219). Academic Press.
Summers, J., Shahrami, A., Cali, S., D’Mello, C., Kako, M., Palikucin-Reljin, A., Savage, M., Shaw, O., & Lunsky, Y. (2017). Self-injury in autism spectrum disorder and intellectual disability: Exploring the role of reactivity to pain and sensory input. Brain Sciences, 7, 140. https://doi.org/10.3390/brainsci7110140
Taylor, L. R. (2016). Psychopharmacologic intervention for adults with autism spectrum disorder: A systematic literature review. Research in Autism Spectrum Disorders, 25, 58–75. https://doi.org/10.1016/j.rasd.2016.01.011
Thompson, T. (2007). Making sense of autism. Paul H. Brookes.
U.S. Food and Drug Administration. (2019). Development and approval process: Drugs.
Umbricht, D., Del Valle Rubido, M., Hollander, E., McCracken, J. T., Shic, F., Scahill, L., Noeldeke, J., Boak, L., Khwaja, O., Squassante, L., Grundschober, C., Kletzl, H., & Fontoura, P. (2017). A single dose, randomized, controlled proof-of-mechanism study of a novel vasopressin 1a receptor antagonist (RG7713) in high-functioning adults with autism spectrum disorder. Neuropsychopharmacology, 42, 1924. https://doi.org/10.1038/npp.2016.232
VanDerwall, R., Rotta, K., Ehrhardt, K., & Poling, A. (2021). Using aripiprazole to benefit people with autism spectrum disorder: A critical appraisal. Advances in Neurodevelopmental Disorders, 5, 1–10. https://doi.org/10.1007/s41252-020-00190-7
Vohra, R., Madhavan, S., Sambamoorthi, U., StPeter, C., Poe, S., Dwibedi, N., & Ajmera, M. (2016). Prescription drug use and polypharmacy among Medicaid-enrolled adults with autism: A retrospective cross-sectional analysis. Drugs – Real World Outcomes, 3, 409–425. https://doi.org/10.1007/s40801-016-0096-z
Walkup, J., & the Work Group of Quality Issues. (2009). Practice parameter on the use of psychotropic medication in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 961–973. https://doi.org/10.1097/chi.0b013e3181ae0a08
Weeden, M., Ehrhardt, K., & Poling, A. (2010). Psychotropic drug treatments for people with autism and other developmental disabilities: A primer for practicing behavior analysts. Behavior Analysis in Practice, 3, 4–12. https://doi.org/10.1007/2FBF03391753
Yamasue, H., Okada, T., Munesue, T., Juroda, M., Fujioka, T., Uno, Y., Matsumoto, K., Kuwabara, H., Mori, D., Okamoto, Y., Yoshimura, Y., Kawakubo, Y., Arioka, Y., Kojima, M., Yuhi, T., Owada, K., Yassin, W., Kushima, I., Benner, S., … Kosak, H. (2018). Effect of intranasal oxytocin on the core social symptoms of autism spectrum disorder: A randomized clinical trial. Molecular Psychiatry, 25, 1849–1858. https://doi.org/10.1038/s41380-018-0097-2
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rotta, K., VanDerwall, R., Ehrhardt, K., Poling, A. (2022). Pharmacological Interventions for Adults with Autism Spectrum Disorder. In: Leaf, J.B., Cihon, J.H., Ferguson, J.L., Gerhardt, P.F. (eds) Handbook of Quality of Life for Individuals with Autism Spectrum Disorder. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-030-98507-3_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-98507-3_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-98506-6
Online ISBN: 978-3-030-98507-3
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)