Abstract
Monitoring cerebral blood flow velocity via transcranial doppler (TCD) can also be applied to measure the brain’s vascular reactivity. Cerebral autoregulation (CA) is the ability of the brain’s blood vessels to constrict or dilate to adapt to variations in mean arterial blood pressure (MAP) to maintain a stable cerebral perfusion pressure.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Background
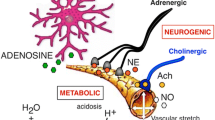
Monitoring cerebral blood flow velocity via transcranial doppler (TCD) can also be applied to measure the brain’s vasculature reactivity. Cerebral autoregulation (CA) is the ability of the brain’s blood vessels to constrict or dilate to adapt to variations in mean arterial blood pressure (MAP) to maintain a stable cerebral perfusion pressure.
TCD is widely used to monitor cerebral blood flow velocity and cerebral autoregulation, assuming that the monitored vessel diameter does not change (steady state) during the monitoring period. If this assumption holds true, we can apply the volumetric flow rate definition where cerebral blood flow equals cerebral blood flow velocity. TCD is able to insonate the largest intracranial arteries and the circle of Willis. The most common monitored artery in CA is the middle cerebral artery.
Continuous monitoring of CA with TCD has more advantages over static measurements as it does not require any intervention to change the MAP. It relies on spontaneous variations of slow waves to measure CA. Healthy adults exhibit slow wave oscillations of cerebral blood volume, cerebral blood flow and tissue oxygenation in the frequency of 0.004–0.05 Hz; these slow waves occur in the setting of normal physiologic functions such as breathing and variations in neuronal and cerebrovascular tone [1]. These slow waves are recorded with TCD.
Monitoring cerebral autoregulation with TCD can be helpful in prognostication for unfavorable clinical outcomes and mortality [2] in patients who suffer aneurysmal subarachnoid hemorrhage (aSAH) [3], traumatic brain injury (TBI) [4, 5], large artery vessel occlusion [6], intracerebral hemorrhage (ICH) [7], and patients undergoing cardiac bypass [8].
Cerebral autoregulation can also be applied to optimizing blood pressure management by delineating the cerebral autoregulatory curve and optimal MAP. By delineating the lower and upper limit of CA we can target the MAP or cerebral perfusion pressure to prevent hypoperfusion leading to cerebral ischemia and hyperperfusion leading to cerebral edema and worsening intracranial hypertension. This can facilitate precision medicine by individualizing blood pressure goals with the hope of preventing secondary injury, decreasing mortality and disability [9,10,11]. In a nested randomized controlled trial, patients undergoing cardiac bypass were monitored with TCD to determine the lower limit of CA. The group that was assigned to keep a MAP above the lower limit of CA determined by TCD during cardiac bypass had a lower incidence of postoperative delirium [12]. Individualized blood pressure management during cardiac bypass has also been shown to lead to improved cognitive function and better memory testing in a randomized clinical trial [13]. The objective of these trials is to target personalized blood pressure goals to prevent mainly hypoperfusion leading to increased risk for kidney disease, cognitive impairment and stroke [8, 11, 14, 15].
Step by Step Using Analog Hemodynamic Monitors (Fig. 1)
Equipment
-
Analog hemodynamic monitor
-
ADC converter (converts analog to digital signals)
-
TCD machine with headset
-
Laptop
-
Autoregulation software
-
Cables connecting hemodynamic monitor to ADC converter
Example of robotic transcranial Doppler (rTCD) bedside setup for multimodal monitoring. (Panel a) High level analog output (HLO) ports used to stream data from patient monitor to analog-to-digital convertor (ADC). (Panel b) Multimodal monitoring of a traumatic brain injury patient including rTCD probe and headband. (Panel c) Typical rTCD tracing of right middle cerebral artery (MCA). (Panel d) Laptop compiling and recording time-locked multimodal data streams. (*Figure is a color adaptation from Zeiler et al. Acta Neurochir (Wien). 2018; 160 (11): 2149–57 (with permission from corresponding author))
Requirements
-
Arterial catheter for continuous MAP monitoring
Steps
-
1.
Connect the ADC converter to the hemodynamic monitor
-
2.
Connect the ADC converter to laptop through USB cord
-
3.
Connect TCD machine to laptop through USB cord
-
4.
Turn on TCD monitor and find the bilateral MCA’s signals on the monitored patient using the head-set
-
5.
Turn on laptop
-
6.
Open autoregulation software (software that runs automatic correlations between MAP and cerebral blood flow velocity)
-
(a)
Enter patient identifiers
-
(b)
Select autoregulation profile
-
(c)
Test connections, make sure the analog signals from hemodynamic monitor are connected to the correct channels on the ADC converter
-
(d)
Click start to begin recording
-
(a)
-
7.
When finished, click “stop”, and then click “save” before exiting the program.
-
8.
Open the file and start analyzing the file. See Fig. 2 showing a monitoring period with the index of CA derived from the correlation between cerebral blood flow velocity and MAP, Mx (mean velocity index). When the index approaches 0 and is <0.45 this indicates intact autoregulation, when the index approaches 1 and is ≥0.45 there is impaired autoregulation.
Example of 30 minute recording of continuous monitoring of cerebral autoregulation monitoring with TCD. 51-year old with high grade aneurysmal subarachnoid hemorrhage who underwent CA monitoring with TCD upon admission to the neurocritical care unit. In the top panel ABP (mean arterial blood pressure) and left (L) and right (R) middle cerebral artery velocities (MCAvel) are displayed. In the two bottom panels, the CA index derived from TCD, Mx (mean velocity index) is displayed. Mx is <0.45 during the monitoring period indicating intact cerebral autoregulation
Step by Step with Digital Hemodynamic Monitors
Equipment
-
Digital hemodynamic monitor
-
TCD machine with headset
-
Laptop
-
Autoregulation software
-
Cables connecting hemodynamic monitor and TCD monitor to laptop
Requirements
-
Arterial catheter for continuous MAP monitoring
Steps
-
1.
Turn on TCD monitor and find the bilateral MCA signals on the monitored patient using the headset
-
2.
Connect TCD monitor to laptop via USB port
-
3.
Connect hemodynamic monitor to laptop via USB port
-
4.
Turn on laptop
-
5.
Open autoregulation software (software that runs automatic correlations between MAP and cerebral blood flow velocity)
-
(a)
Enter patient identifiers
-
(b)
Select monitoring profile
-
(c)
Test connections
-
(d)
Click “start” to begin recording
-
(a)
-
6.
When finished, click “stop”, and then click “save” before exiting the program
-
7.
Open file to start analyzing
Limitations
The assumption that the vessel caliber does not change during the monitoring period is a big limitation. If an instantaneous change occurs with a narrowing or dilation of the blood vessel, there will be a significant change in velocity which may not be proportional to the change in flow. Secondly, continuous monitoring with 2-MHz ultrasonic waves through the temporal bone (energy used for diagnostic ultrasonography) is known to be sufficient to enhance thrombolysis [16], so caution should be taken when monitoring patients with or at risk of intracranial bleeding. Lastly, movement artifact is always problematic especially in patients who are not sedated.
References
Lee JK, Kibler KK, Benni PB, Easley RB, Czosnyka M, Smielewski P, et al. Cerebrovascular reactivity measured by near-infrared spectroscopy. Stroke. 2009;40(5):1820–6.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin R, Ziai W, Healy R, Thompson R, et al. Predictors of outcome with cerebral autoregulation monitoring: a systematic review and meta-analysis. Crit Care Med. 2017;45(4):695–704.
Barth M, Woitzik J, Weiss C, Muench E, Diepers M, Schmiedek P, et al. Correlation of clinical outcome with pressure-, oxygen-, and flow-related indices of cerebrovascular reactivity in patients following aneurysmal SAH. Neurocrit Care. 2010;12(2):234–43.
Czosnyka M, Smielewski P, Kirkpatrick P, Menon DK, Pickard JD. Monitoring of cerebral autoregulation in head-injured patients. Stroke. 1996;27(10):1829–34.
Czosnyka M, Smielewski P, Piechnik S, Schmidt EA, Seeley H, al-Rawi P, et al. Continuous assessment of cerebral autoregulation–clinical verification of the method in head injured patients. Acta Neurochir Suppl. 2000;76:483–4.
Reinhard M, Rutsch S, Lambeck J, Wihler C, Czosnyka M, Weiller C, et al. Dynamic cerebral autoregulation associates with infarct size and outcome after ischemic stroke. Acta Neurol Scand. 2012;125(3):156–62.
Reinhard M, Neunhoeffer F, Gerds TA, Niesen WD, Buttler KJ, Timmer J, et al. Secondary decline of cerebral autoregulation is associated with worse outcome after intracerebral hemorrhage. Intensive Care Med. 2010;36(2):264–71.
Ono M, Joshi B, Brady K, Easley RB, Zheng Y, Brown C, et al. Risks for impaired cerebral autoregulation during cardiopulmonary bypass and postoperative stroke. Br J Anaesth. 2012;109(3):391–8.
Rivera-Lara L, Zorrilla-Vaca A, Geocadin RG, Healy RJ, Ziai W, Mirski MA. Cerebral autoregulation-oriented therapy at the bedside: a comprehensive review. Anesthesiology. 2017;126(6):1187–99.
Aries MJ, Czosnyka M, Budohoski KP, Steiner LA, Lavinio A, Kolias AG, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40(8):2456–63.
Ono M, Brady K, Easley RB, Brown C, Kraut M, Gottesman RF, et al. Duration and magnitude of blood pressure below cerebral autoregulation threshold during cardiopulmonary bypass is associated with major morbidity and operative mortality. J Thorac Cardiovasc Surg. 2014;147(1):483–9.
Brown CH, Neufeld KJ, Tian J, Probert J, LaFlam A, Max L, et al. Effect of targeting mean arterial pressure during cardiopulmonary bypass by monitoring cerebral autoregulation on postsurgical delirium among older patients: a nested randomized clinical trial. JAMA Surg. 2019;154(9):819–26.
Hogue CW, Brown CH, Hori D, Ono M, Nomura Y, Balmert LC, et al. Personalized blood pressure management during cardiac surgery with cerebral autoregulation monitoring: a randomized trial. Semin Thorac Cardiovasc Surg. 2021;33(2):429–38.
Ono M, Arnaoutakis GJ, Fine DM, Brady K, Easley RB, Zheng Y, et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med. 2013;41(2):464–71.
Ono M, Arnaoutakis G, Fine D, Brady K, Easley R, Zheng Y, et al. Blood pressure excursions below the cerebral autoregulation threshold during cardiac surgery are associated with acute kidney injury. Crit Care Med. 2012;41(2):464–71.
Alexandrov AV, Molina CA, Grotta JC, Garami Z, Ford SR, Alvarez-Sabin J, et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med. 2004;351(21):2170–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rivera-Lara, L., Zeiler, F.A. (2022). Continuous Cerebral Autoregulation Monitoring Using TCD. In: Ziai, W.C., Cornwell, C.L. (eds) Neurovascular Sonography . Springer, Cham. https://doi.org/10.1007/978-3-030-96893-9_16
Download citation
DOI: https://doi.org/10.1007/978-3-030-96893-9_16
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-96892-2
Online ISBN: 978-3-030-96893-9
eBook Packages: MedicineMedicine (R0)