Abstract
Continued clinical experience shows that no single type of urethroplasty is uniformly applicable to all types of hypospadias. Surgeons involved in hypospadias treatment should be able to offer a variety of technical solutions to the gamut of anatomical variations usually encountered. Surgeons who master one technique of repair or who plan to operate only on distal hypospadias are not acting in their patients’ best interests. This chapter evaluates the role of different flaps and grafts in the management of hypospadias.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Flaps
Flaps used in hypospadias repair may be meatal-based , e.g.,:
-
Mathieu
-
Mustardé and Barcat (Chap. 21)
-
“Slit-like adjusted Mathieu” (SLAM, Chap. 22)
-
Koyanagi (Chap. 36)
-
Yoke (Chap. 37)
-
“Chordee excision and distal urethroplasty” (CEDU, Chap. 33)
-
“Lateral-based onlay flap” (LABO, Chap. 30)
or urethral plate-based
Common pedicled flaps are usually based on preputial vessels and include Hodgson’s/Perovic flap (Chap. 38), onlay island flap (Chap. 31), transverse preputial island flap (Chap. 34), and Asopa’s double-faced island flap (Chap. 35).
Vascularized fascial flaps have also become popular as a protective intermediate layer (Chap. 43). They help to provide a protective intermediate layer and minimize complications. Common examples are tunica vaginalis flap, preputial subcutaneous flap, and dartos flap. The routine use of these vascularized fascial flaps has significantly improved the results of hypospadias repair and reduced the incidence of complications to less than 5% in distal hypospadias repair [1, 2].
Additionally flaps can be used for corporal straightening (Chap. 8). In hypospadias cases with deep corpus cavernosum-based chordee, an epithelial covered flap can cover the corporal defect that is achieved by the transverse cut to correct corporal chordee [3].
2 Grafts
Grafts commonly used in hypospadias repair include preputial skin (full thickness or partial thickness), post-auricular Wolffian graft (PAWG) (full thickness), abdominal skin (full-thickness or dermal grafts following chordee excision), bladder mucosa, and oral mucosa (buccal or labial) (Chaps. 39 and 40).
3 Flaps Versus Grafts
In Chap. 16, the basic principles, advantages, and disadvantages of flaps and grafts were discussed. A simple practical maxim was mentioned:
“A graft is a non-living tissue that you try to bring to life and a flap is a living tissue that you try not to bring to death.”
This is perhaps somewhat biased but nevertheless conforms to the basic principles of plastic surgery.
Duckett believed that flap repair has an advantage over grafts since the normal blood supply to the tissues is intact [4]. This again conforms to plastic surgery principles.
The known advantage of flaps compared to grafts is the intact blood supply which results in a better survivability. Another important advantage is that flaps are unlikely to contract or scar. The published disadvantage is a higher rate of diverticulum formation compared to grafts, and it requires experience to plan the flap properly and maintain good blood supply.
The advantages of grafts compared to flaps are the lower rate of diverticulum formation and its availability when there is little local healthy tissues available and the relatively easy gathering and availability even in circumcised redo cases. The main disadvantages of grafts are failure of graft take, scarring or contracture and shrinkage even after a few years, and failure of graft to grow as the penis grows.
In a controversial debate of flaps versus grafts, Cendron stated that a flap in an experienced surgeon’s hands
On the other hand, Snodgrass reported that he had better outcome using buccal mucosal grafts in proximal hypospadias as compared with flaps [6]. It is clear that the surgeon’s experience plays an important role in the outcome.
Several studies evaluated the results of different techniques. However, in an excellent study, Powell et al. compared the results of flaps and grafts in the management of proximal hypospadias [7]. In this retrospective investigation, they reviewed the records of 142 patients who had undergone proximal hypospadias repair between 1981 and 1997. The techniques used in the repair were transverse preputial island flaps used as a tube or onlay and preputial skin grafts used as a tube or onlay. One surgeon operated on 93 patients (65%). Tube urethroplasty was the routine technique in the earlier years of the study (1980s), and onlay was the preferred technique in later years (1990s). Two-thirds of the study group (95 patients) had the repair performed using grafts. Two-thirds of the grafts were done as a tube (61 vs. 34 patients). In the flap group (47 patients), 27 patients had a tube flap and 20 had an onlay flap. The authors concluded that there was no significant difference in the complication rates of flaps and grafts used to repair proximal hypospadias. However, in the graft group, there was a significantly higher proximal stricture rate when a tube rather than an onlay was used. The study also raised a very important issue, namely, that a significant number of complications (67%) presented more than 1 year after surgery.
Since then there has been no prospective investigation with a large sample group directly comparing flaps to grafts.
Table 52.1 shows the complication rate of tubed flaps and tubed grafts in different series, while Table 52.2 shows the complication rate of onlay repairs. The data in the two tables permit no definite conclusions. The retrospective studies were reported at different times, and different suture materials and suture techniques were used. The surgeons had different levels of experience, and selection criteria may have differed. Also, the follow-up period varied from one study to another.
There are other factors that need to be addressed when comparing flaps and grafts. These factors include single- or two-stage repair, the ease or difficulty of flap or graft preparation, the required period of hospitalization, the duration and degree of mobilization, the method of urinary diversion, if needed, the comfort of the child (e.g., hip spica in case of grafts [32]), and the degree of inconvenience to the family.
Generally speaking a hypospadiologist should be capable of performing both techniques to provide the optimal care for the hypospadias patients. This can be seen in various publications. An example would be de Mattos e Silva et al., where the team describes a retrospective analysis in 184 proximal hypospadias cases [33]. An onlay flap urethroplasty was chosen for primary cases with a healthy urethral plate. In redo cases with missing foreskin, a buccal mucosa graft was gathered and in the most severe cases the Koyanagi repair was chosen. With these limitations in mind, the complication rates seem rather even between the techniques.
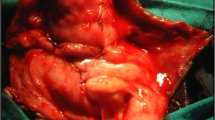
Grafts are not only used to reconstruct new urethra; sometimes, skin grafts are needed to cover the penis. Sources for skin graft to cover the penis include the lower abdominal crease, post-auricular skin, and even the groin at the junction of lower abdomen and thigh (Figs. 52.2 and 52.3).
(a–d) A child with buried penis who underwent improper circumcision. (a) Only the glans can be seen but the rest of the penis is hidden in the abdomen. (b) After mobilization, the penis looks normal in size but there is lack of skin to cover it. A large skin graft was taken from the groin to cover the skin defect. (c) After covering the skin defect and before closing the donor area at the groin. (d) After complete healing of the wound (courtesy of Prof. Ibrahim Ulman)
Further prospective multicenter studies involving a large number of patients using standardized operation techniques and suturing techniques and materials, with a follow-up period of at least 5 years are needed to permit definite conclusions.
Abbreviations
- CEDU:
-
Chordee excision and distal urethroplasty
- LABO:
-
Lateral-based onlay flap
- PAWG:
-
Post-auricular Wolffian Graft
- SLAM:
-
Slit-like adjusted Mathieu
- TIP:
-
Tubularized incised plate
References
Snow BW. Use of tunica vaginalis to prevent fistulas in hypospadias surgery. J Urol. 1986;136:861–3.
Snow BW, Cartwright PC, Unger K. Tunica vaginalis blanket wrap to prevent urethrocutaneous fistula: an 8-year experience. J Urol. 1995; https://doi.org/10.1097/00005392-199502000-00061.
Braga LHP, Pippi Salle JL, Dave S, Bagli DJ, Lorenzo AJ, Khoury AE. Outcome analysis of severe chordee correction using tunica vaginalis as a flap in boys with proximal hypospadias. J Urol. 2007; https://doi.org/10.1016/j.juro.2007.03.166.
Duckett JW. The island flap technique for hypospadias repair. Urol Clin North Am. 1981;8:503–11.
Cendron M. Flap versus graft 2-stage repair of severe hypospadias with chordee. J Urol. 2015; https://doi.org/10.1016/j.juro.2014.12.064.
Snodgrass WT. Flap versus graft 2-stage repair of severe hypospadias with chordee. J Urol. 2015; https://doi.org/10.1016/j.juro.2014.12.063.
Powell CR, Mcaleer I, Alagiri M, Kaplan GW. Comparison of flaps versus grafts in proximal hypospadias surgery. J Urol. 2000; https://doi.org/10.1016/S0022-5347(05)67762-2.
Monfort G, Jean P, Lacoste M. Correction des hypospadias posterieurs en un temps par lambeau pedicule transversal (intervention de Duckett). A propos de 50 observations. Chir Pediatr. 1983;24:71.
Hendren WH, Crooks KK. Tubed free skin graft for construction of male urethra. J Urol. 1980; https://doi.org/10.1016/S0022-5347(17)56163-7.
Bondonny JM, Barthaburu D, Vergnes P. L’hypospadias balanique et penien les elements de la malformation: implications therapeutiques et resultats. A partir de l’etude de cent trente-cinq dossiers. Ann Urol. 1984;18:21–7.
De Sy WA, Oosterlinck W. One-stage Hypospadias repair by free full-thickness skin graft and island flap techniques. Urol Clin North Am. 1981; https://doi.org/10.1016/s0094-0143(21)01305-7.
Barraza MA, Roth DR, Terry WJ, Livne PM, Gonzales ET. One-stage reconstruction of moderately severe hypospadias. J Urol. 1987; https://doi.org/10.1016/S0022-5347(17)44186-3.
Redman JF. Experience with 60 consecutive hypospadias repairs using the Horton-Devine techniques. J Urol. 1983; https://doi.org/10.1016/S0022-5347(17)51948-5.
Sauvage P, Rougeron G, Bientz J, Cuvelier G. L’utilisation du lambeau preputial transverse pedicule dans la chirurgie de l’hypospadias. Chir Pediatr. 1987;28.
Shapiro SR. Complications of hypospadias repair. J Urol. 1984; https://doi.org/10.1016/S0022-5347(17)50475-9.
Harris DL, Jeffery RS. One-stage repair of hypospadias using split preputial flaps (Harris): the first 100 patients treated. Br J Urol. 1989; https://doi.org/10.1111/j.1464-410X.1989.tb05227.x.
Vyas PR, Roth DR, Perlmutter AD. Experience with free grafts in urethral reconstruction. J Urol. 1987; https://doi.org/10.1016/S0022-5347(17)44071-7.
Hollowell JG, Keating MA, Snyder HM, Duckett JW. Preservation of the urethral plate in hypospadias repair: extended applications and further experience with the onlay island flap urethroplasty. J Urol. 1990; https://doi.org/10.1016/s0022-5347(17)39878-6.
Rober PE, Perlmutter AD, Reitelman C. Experience with 81, 1-stage hypospadias/chordee repairs with free graft urethroplasties. J Urol. 1990;144:526–9.
Rickwood AMK, Anderson PAM. One-stage hypospadias repair: experience of 367 cases. Br J Urol. 1991; https://doi.org/10.1111/j.1464-410X.1991.tb15171.x.
Johal NS, Nitkunan T, O’Malley K, Cuckow PM. The two-stage repair for severe primary hypospadias. Eur Urol. 2006; https://doi.org/10.1016/j.eururo.2006.01.002.
Kass EJ, Bolong D. Single stage hypospadias reconstruction without fistula. J Urol. 1990; https://doi.org/10.1016/s0022-5347(17)39510-1.
Obara K, Hoshii T, Hoshino S, Yamana K, Anraku T, Maruyama R, Kuroki H, Ishizaki F, Yamazaki H, Tomita Y. Free tube graft urethroplasty for repair of hypospadias. Urol Int. 2020; https://doi.org/10.1159/000504146.
Wacksman J. Use of the Hodgson XX (modified Asopa) procedure to correct hypospadias with chordee: surgical technique and results. J Urol. 1986; https://doi.org/10.1016/S0022-5347(17)45309-2.
Badawy H, Orabi S, Hanno A, Abdelhamid H. Posterior hypospadias: evaluation of a paradigm shift from single to staged repair. J Pediatr Urol. 2018; https://doi.org/10.1016/j.jpurol.2017.07.007.
Seleim HM, Morsi H, Elbarbary MM. Neo-yoke repair for severe hypospadias: a simple modification for better outcome. J Pediatr Urol. 2017; https://doi.org/10.1016/j.jpurol.2016.11.016.
Liao AY, Smith GHH. Urethrocutaneous fistulae after hypospadias repair: when do they occur? J Paediatr Child Health. 2016; https://doi.org/10.1111/jpc.13102.
Hadidi AT. Perineal hypospadias: back to the future chordee Excision & Distal Urethroplasty. J Pediatr Urol. 2018; https://doi.org/10.1016/j.jpurol.2018.08.014.
Elder JS, Duckett JW, Snyder HM. Onlay island flap in the repair of mid and distal penile hypospadias without chordee. J Urol. 1987; https://doi.org/10.1016/S0022-5347(17)43152-1.
Baskin LS, Duckett JW, Ueoka K, Seibold J, Snyder HM. Changing concepts of hypospadias curvature lead to more onlay island flap procedures. J Urol. 1994; https://doi.org/10.1016/S0022-5347(17)34915-7.
Hadidi AT. Proximal hypospadias with small flat glans: the lateral-based onlay flap technique. J Pediatr Surg. 2012; https://doi.org/10.1016/j.jpedsurg.2012.06.027.
Cilento BG, Stock JA, Kaplan GW. Pantaloon spica cast: an effective method for postoperative immobilization after free graft hypospadias repair. J Urol. 1997; https://doi.org/10.1016/S0022-5347(01)64892-4.
de Mattos e Silva E, Gorduza DB, Catti M, Valmalle AF, Demède D, Hameury F, Pierre-Yves M, Mouriquand P. Outcome of severe hypospadias repair using three different techniques. J Pediatr Urol. 2009; https://doi.org/10.1016/j.jpurol.2008.12.010.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sennert, M., Hadidi, A.T. (2022). Flaps Versus Grafts. In: Hadidi, A.T. (eds) Hypospadias Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-94248-9_52
Download citation
DOI: https://doi.org/10.1007/978-3-030-94248-9_52
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-94247-2
Online ISBN: 978-3-030-94248-9
eBook Packages: MedicineMedicine (R0)