Abstract
Reoperative hypospadias surgery is often complicated by the general lack of healthy tissue for urethroplasty and skin coverage. The penile skin that is present is typically scarred and has a variable and poorly defined blood supply. Each case is different and demands individualized evaluation and care. Reoperation is delayed at least 6 months after the last repair, in order to maximize tissue healing and vascularity. Earlier attempts at definitive repair are often fraught with more complications. Common post hypospadias repair complications are urethrocutaneous fistula, urethral diverticulum, persistent chordee, and urethral stricture. A procedure using “wide” exposure may be required to correct what appears to be a small problem. Successful reconstruction of such refractory, postsurgical strictures, requires the whole surgical armamentarium, namely, vascularized onlay flaps, buccal mucosal grafts, and planned-staged procedures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Summary
Reoperative hypospadias surgery is often complicated by the general lack of healthy tissue for urethroplasty and skin coverage. The penile skin that is present is typically scarred and has a variable and poorly defined blood supply. Each case is different and demands individualized evaluation and care. Reoperation is delayed at least 6 months after the last repair, in order to maximize tissue healing and vascularity. Earlier attempts at definitive repair are often fraught with more complications. Common post hypospadias repair complications are urethrocutaneous fistula, urethral diverticulum, persistent chordee, and urethral stricture. A procedure using “wide” exposure may be required to correct what appears to be a small problem. Successful reconstruction of such refractory, postsurgical strictures, requires the whole surgical armamentarium, namely, vascularized onlay flaps, buccal mucosal grafts, and planned-staged procedures.
Introduction
Current hypospadias techniques set a high standard for functional and cosmetic outcomes. A slit-like meatus in an orthotopic position on a conical glans is the goal. This should be achieved with a single operation in patients with a glandular hypospadias. Success is greater than 95 % in boys with a distal hypospadias. In large series, complication rates after proximal hypospadias repair can be as high as 30–40 %. The complications are lower if the urethral plate is preserved and may be lowest if the repair solely utilizes the urethral plate and not vascular or grafted preputial skin [1–4]. Regardless of meatal position the complication rate is highest and approaches 100 % in some series of primary hypospadias repair in postpubertal males [5, 6].
The most important factor that impacts reoperative hypospadias is the presence of healthy tissue that is needed for urethroplasty and skin coverage. There is usually a paucity of penile skin that is scarred and has a variable and poorly defined blood supply. Natural tissue planes often are disrupted, and dissection may damage the blood supply to the penile skin. Each case requires individual evaluation and managemvent based upon sound plastic surgical principles. Every attempt should be made to review the previous operative notes.
There are no randomized trials assessing the efficacy of testosterone administration prior to primary or reoperative hypospadias surgery. There are reports showing both increased and decreased complication rates after preoperative administration of testosterone [7, 8]. There is evidence that the microvasculature of preputial skin in hypospadias patients is lower than in normal controls [9]. It is unknown if testosterone improves vascularity, but there is some evidence in the plastic surgery literature that androgens may inhibit wound healing while estrogens may decrease inflammation and promote healing [10].
In general, reoperative surgery should be delayed at least 6 months after the last repair to eliminate any residual inflammation and allow complete healing. Time allows in growth of new blood supply to relocated penile skin. Earlier attempts at definitive repair may actually create a more significant complication. The glansplasty is the key to a normal postoperative appearance, so urethrocutaneous fistulae, diverticula, or urethral strictures in the presence of a normal glandular urethra may be technically easier and more successfully repaired than cases where postoperative disruption of the glansplasty has occurred.
Surgical Complications
Urethrocutaneous Fistula
When a fistula is identified, the urethra and meatus are examined under anesthesia prior to making any incisions. I like to observe the urinary stream prior to manipulating the urethra. Crede recapitulates urination and helps assess for meatal stenosis (Fig. 27.1). The urethra is calibrated with bougie-a-boule. I perform this after crede because the bougies can easily dilate a very soft stricture. This also assesses for any urethral irregularity. Depending upon the age of the patient and the previous surgical technique used, urethroscopy may be indicated to exclude urethral hair or encrustations that would complicate the fistula closure. The urethra is pressurized with saline or water through a catheter to confirm the location and number of fistulae.
We pass a small lacrimal duct probe through the fistula tract and out the urethral meatus. This step helps to define the tract and identifies the exact point of communication with the urethra. Lidocaine with epinephrine is infiltrated around the fistula site. Electrocautery is rarely if ever required during these cases and should be discouraged.
The principles of fistula closure include dissection of the tract flush with the urethra, excision of unhealthy tissues, an inverting watertight closure, and placement of one or more barrier layers between the urethra and the skin [11]. A dartos-based subcutaneous pedicle flap can usually be advanced to cover the fistula closure, although tunica vaginalis may be used in more complex cases [12, 13].
Small fistulae on the penile shaft can be circumscribed and excised flush with the urethra. However, subcoronal or glandular fistulae may require a more extensive dissection because of a paucity of healthy adjacent tissues. In these cases, a takedown of the glansplasty may be required to facilitate fistula excision. A distal urethroplasty can then be performed, followed by interposition of a dartos pedicle and reapproximation of the glans wings. Simple fistula closures without meatal reconstruction rarely require a postoperative catheter, but when distal edema may increase urethral voiding pressure, a catheter or urethral stent is preferable.
Urethral Diverticulum
Diverticular formation after hypospadias surgery may be indicative of urethral meatal stenosis but, in most cases, calibration reveals no evidence of narrowing. Children may present with dysuria (urethritis), a urinary tract infection, or post-void dribbling. Occasionally ballooning of the ventral aspect of the phallus is presenting observation (Fig. 27.2a). If the child presents with a febrile UTI, a cystogram can be attempted but often the catheter cannot be easily manipulated across the proximal aspect of the urethroplasty (Fig. 27.2b). Repair is most accurately performed after degloving the ventral phallus. A feeding tube is passed transurethrally and the diverticulum is distended with saline (Fig. 27.2c). This distension facilitates dissection by defining the appropriate plane between the diverticulum and skin while sparing the blood supply to the urethra. The diverticulum is opened in the ventral midline along its entire length (Fig. 27.2d). Calipers are used to mark the appropriate urethral width (10–12 mm in a prepubertal male (Fig. 27.2e) and 20–24 French postpubertal) on the dorsal urethral wall. Redundant epithelium is sharply excised while sparing the subcutaneous blood supply. The urethra is closed with a running and interrupted inverting suture line. The redundant subcutaneous tissue is an excellent covering layer and can be approximated over the urethroplasty in a pant-over-vest fashion. Because of the length of the closure, catheter drainage is advisable (Fig. 27.2f).
Large urethral diverticulum after onlay island flap hypospadias repair. (a) Marked ventral ballooning noted during urination, (b) he presented with a febrile UTI and a retrograde urethrogram confirms a large diverticulum. The catheter could not be advanced into the bladder, (c) the diverticulum is distended and a midline incision is made over the diverticulum, (d) squamous epithelial debris is noted inside the diverticulum once it is opened, (e) in a prepubertal male, a 12-mm strip of mucosa is marked for the urethroplasty. The redundant epithelium can be sharply excised with preservation of the underlying vascular tissue that provides an excellent barrier layer to prevent subsequent fistula formation, (f) appearance of the phallus immediately after urethroplasty and skin closure
Repair of a urethral diverticulum using plication has been reported [14]. This approach, however, does not remove the redundant mucosa, and since absorbable sutures are used, the diverticulum might recur. Definitive excision and urethroplasty are recommended to eliminate potential long-term concerns.
Urethral Stricture
Stenosis of the urethral meatus is the most common site of narrowing after hypospadias repair. This can occasionally be corrected with either a dorsal or ventral urethral meatoplasty. A midline incision is made across the narrowing and carried deep into the glans tissues. The edges are reapproximated in Heineke-Mikulicz fashion using 7-0 absorbable sutures. A dorsal meatoplasty sometimes causes dimpling of the dorsal glans and can affect the direction of the urinary stream. A ventral meatoplasty may effectively improve the urinary stream, but this may result in a coronal opening (megameatus).
At times it is difficult to ascertain if the narrowing is at the meatal level or extends more proximally. Because of patient age (anxiety for invasive testing) and the history of penile surgery, we often do not obtain a urethrogram prior to reoperation, but as part of informed consent, parents need to understand that a more extensive procedure may be required. In boys with a history of urinary tract infections after hypospadias repair, a urethrogram or cystogram is advisable (Fig. 27.3). If a longer distal stricture is identified, then this needs to be marsupialized and corrected with either a vascularized flap or grafting. With a distal stricture there is high likelihood that biopsy will show balanitis xerotica obliterans. In these cases the use of local tissues should be avoided as they are similarly affected by this pathology.
Strictures in the midportion of a urethroplasty are actually very uncommon. Narrowing of the proximal junction between the reconstructed and native urethra is more common. These are often diaphanous narrowings that are amenable to an attempt at optical urethrotomy, although the long-term success is less than 50 % [15].
Persistent Chordee
Persistent penile curvature may be a result of ventral skin tethering, corporal disproportion, and urethral foreshortening [16–18]. Historically, the urethral plate was divided to correct penile curvature. However, in the 1990s, Duckett and others popularized the concept of corporal disproportion as the primary etiology of penile curvature [8]. Histological evaluation of the urethral plate usually reveals healthy spongy tissue that clinically is very elastic.
Curvature may recur years after the initial hypospadias repair even when corporoplasty (plication and/or ventral grafting) was used to successfully correct chordee at the first surgery (Fig. 27.4). There are no good data showing whether or not free graft urethroplasties are at greater risk for recurrence of curvature when compared with vascularized flaps or primary plate tubularizations. However, a urethral graft with some fibrosis is less likely to grow in concert with the rest of the phallus at puberty. Even if the urethral plate was not previously divided because of a normal appearance, it is possible that the primary surgeon did not appreciate its contribution to curvature.
Recurrent penile curvature in a 12-year-old boy. He is 11 years s/p dorsal plication and tubularized incised plate hypospadias repair. In this case there is marked corporal disproportion and a staged correction is likely required with first stage-ventral lengthening (dermal grafts or parallel relaxing incisions) and buccal graft Second stage-urethroplasty
At reoperation, an artificial erection is induced intraoperatively. The urethra is inspected to determine whether it is supple or a “bowstring” (indicative of fibrosis). When urethral tethering is suspected, then the urethra should be transected and fibrous tissue resected. A repeat erection after transection may show persistent curvature in up to 50 % of cases, indicating coexisting corporal disproportion. Either ventral dermal grafting or dorsal plications can be used to correct the curvature in these cases. In cases where the urethra is normal, then a primarily dorsal approach to correction is indicated. In some cases, prior dorsal plications may have disrupted, but it is also possible that the intrinsically disproportionate corporal growth pattern persisted at puberty.
Complex Reoperative Hypospadias Techniques
Urethral Plate Retubularization
Tubularized incised plate (TIP) hypospadias repair was introduced in 1994 and is the operation of choice for distal hypospadias repair in many centers. There is good evidence that the preserved urethral plate can be used in reoperative hypospadias [2, 20–23]. Extensive experience with the primary procedure is helpful when assessing the quality of the urethral plate. If the plate appears supple without scarring or evidence of a prior incision, then tubularization is reasonable. The complication rate with tubularization of the plate in secondary operations is similar to the rate when used in primary repairs (Table 27.1).
Previous surgery that involved incision of the urethral plate might alter the blood supply and decrease the success of a second tubularization. In addition, a failed TIP may be indicative of an intrinsic abnormality with the plate and spongiosum that precludes a second attempt at urethroplasty using the same technique. Because of these factors, there has been reluctance to perform a repeat TIP, although literature reports show that a repeat TIP does not appear to be associated with a higher complication rate in experienced hands (Table 27.1).
The plate can always be incised at the time of reoperation. If it is apparent after the incision that fibrosis is present that precludes a healthy tension-free urethral closure, adjacent genital tissues or a free graft can be utilized. Incision of the plate does not burn a bridge and exclude other operative approaches [24].
The most common complication with retubularization is fistula formation, so the use of a barrier flap is very important in these reoperative cases. If a circumcision was not performed at the time of the prior hypospadias repair, a dartos subcutaneous is available for neourethral coverage. Otherwise, adjacent ventral dartos or tunica vaginalis flaps are useful barriers.
Adjacent Genital Tissues
If the urethral plate is not suitable for retubularization, then the use of vascularized adjacent genital tissues may be possible (Fig. 27.5 [3, 17, 25–30]). Local flaps may be preferable to grafts because the former do not rely upon the reestablishment of vascularity. Care must be taken when harvesting the flap in the presence of scarring from multiple prior procedures. Both meatal-based and dartos pedicle flaps can be used for the urethroplasty, but ventral blood supply is often more highly compromised than tissues that are laterally or dorsally positioned. Scrotal skin is often well vascularized, but it is usually hair bearing and is associated with a high incidence of future urethral complications.
As noted in Table 27.2, an additional procedure will likely be required in at least 25 % of patients when a vascularized flap is used for the urethroplasty. This complication rate is clearly higher than the outcomes when flaps are used in a primary repair. The penile skin adjacent to the meatus is often not well vascularized at the hinge of the flip-flap. If this technique is utilized, the dartos pedicle from the prior Byars’ flap is preserved as the blood supply for the ventral flap.
Although skin is usually available, there is a significant incidence of postoperative fistulae, strictures, and glansplasty breakdown when adjacent skin is used for repeat hypospadias repairs. Some authors express concern that the glansplasty and meatal appearance are abnormal after flap urethroplasty, but with appropriate glans wing dissection, an orthotopic vertical meatal opening can be achieved. The limiting factor for a normal-appearing glans is the degree of glans scarring and contraction after the prior repairs.
Extragenital Tissues
Frequently, a paucity of genital tissue is available in reoperative hypospadias. A skin graft urethroplasty using either squamous [4, 17, 31–33], transitional (bladder mucosa [34–36]), or pseudostratified (buccal mucosa [22, 33, 37–41]) is then required. Most hypospadias surgeons are somewhat uncomfortable with this approach because they are now trained in primary repairs that consist of either primary plate tubularization or vascularized flaps.
Grafts can be approached with a one- or two-stage operation. A graft must establish vascularity to survive. In reoperations, this neovascularity comes from the scarred recipient bed. Graft take is theoretically more reliable in a staged approach because the corporal bodies are likely healthier than the shaft skin that would be important in supplying blood to the ventral aspect of an onlay or tube graft. If a tube graft is used, a tunneled placement may cause less disruption to the ventral blood supply.
Bracka uses a staged grafting technique for most primary hypospadias, and this same technique is very useful in reoperative repairs [4]. During the first operation, the scarred urethral plate and unhealthy ventral tissue are excised. The graft is secured to the corporal bodies from the proximal urethral opening to the tip of the glans. The graft can be quilted onto the corporal bodies and a gentle compression dressing that immobilizes the graft. This prevents hematoma formation and the shear forces that inhibit the development of blood supply. Graft take can be assessed before a second tubularization at least 6 months later.
A staged approach may give a better cosmetic result to the patient [4, 22, 41]. When a hypospadias repair fails, the glans wings often contract, and there is not sufficient width or mobility to achieve an orthotopic meatus after the second procedure. Glandular scarring can be excised, and the graft can be interposed between the corporal bodies to give a deep groove for subsequent glansplasty and distal urethroplasty.
A barrier layer is required and this can be challenging when there is a paucity of local skin. A tunica vaginalis or subcutaneous scrotal flap has an excellent blood supply and can usually be mobilized to give a barrier layer (Fig. 27.5). The use of small intestinal submucosa has been described but in some series did not inhibit fistula formation, and there was the subjective assessment of increased fibrosis ventrally.
Squamous Epithelium
Nonhair-bearing squamous epithelium has historically been the graft material of choice. Bracka uses the inner preputial skin for staged repairs, but the prepuce is frequently unavailable in reoperative cases [4]. Single-stage skin graft urethroplasty in these cases has a 30–50 % failure rate with complete graft loss in up to 25 % of cases. A split thickness technique has been described but the grafted area is usually very small, so meshing may not be required to achieve coverage [31, 32].
Bladder Mucosal Graft
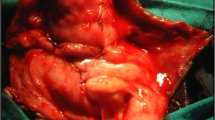
Bladder mucosal urethral replacement was popularized in the middle of the 1980s. Penile dissection and correction of chordee is completed before harvesting of the bladder mucosa. A Pfannenstiel incision is used to harvest the bladder. Distending the bladder and sharply excising the muscle giving the typical “blue-domed cyst” appearance of the bulging mucosa best performs this. The bladder mucosa is very thin and difficult to handle.
Urethral meatal prolapse is a unique complication with bladder mucosa urethroplasty. The exposed transitional epithelium becomes sticky and hypertrophic [35]. Construction of a 20-French urethral meatus, prolonged catheter drainage, anchoring of graft to the corporal bodies, and a distal skin graft may reduce this complication. A greater than 75–85 % success rate has been described when bladder mucosa is utilized for urethral replacement. Certainly transitional epithelium is a natural choice for urethral replacement since it is normally exposed to urine. The need for the lower abdominal incision has led to the use of other graft materials.
Buccal Mucosal Graft
Buccal mucosa is a thick epithelium with good tensile strength and a very vascular submucosal plexus that favors graft take [37]. The thickness aids in dissection and subsequent manipulation of the graft material. The buccal mucosa can be harvested from either the inner cheek or lip. The harvest minimizes fat and avoids dissection into muscle. There may be a little bit less morbidity if the donor site is closed, but many surgeons allow the site to heal by secondary intention. In the early 1990s, there were several reports of short-term success with single-stage buccal mucosal grafts in complex urethroplasty. Surprisingly, tube grafts seemed to do better than onlays, but the overall complication rate was as much as 60 % with long-term follow-up [40].
Buccal graft urethroplasty using the staged technique described by Bracka has improved outcomes when compared with single-stage buccal repairs [22, 41]. In this technique, the initial graft take is probably better because it is dependent only upon the corporal bodies and not upon the previously operated ventral skin. The ability to inspect the graft prior to retubularization allows regrafting when clinically indicated. This likely decreases the development of urethral strictures (Fig. 27.6). In a recent series [22] first-stage graft revision was required for graft contraction or loss in 10 % of patients. A urethroplasty complication occurred in 17 of 45 (38 %) patients after the second stage. The complication rate did not seem to be related to patient age, number of prior surgeries, or location of the meatus. Glans dehiscence occurred in one-third of patients when a cheek graft was used and 0 of 17 when a lip graft was utilized. The authors hypothesize that the inner lip buccal mucosa is thinner and facilitates a tension-free glansplasty.
Buccal mucosal graft. (a) Coronal meatus (glans dehiscence) after tubularized incised plate hypospadias repair, (b) a deep, clefted incision is made in the glans midline and buccal mucosa is sutured/quilted directly onto the corporal bodies, (c) a compression dressing consisting of xeroform gauze and horizontal mattress nylon sutures is left in place for 1 week. Depending upon patient age the urine is diverted with either a urethral catheter or a suprapubic tube, (d) normal appearance with fibrinous exudate at the time of dressing removal, (e) appearance of buccal graft 6 months after primary graft
Critics of staged procedures correctly note that some patients did not require two additional surgeries. Dorsal grafting (inlay) of an attenuated yet supple plate and “primary” urethroplasty has been described as part of a single-stage repair. In a small series this approach was successful in 11/13 (85 %) patients [22]. The decision to proceed with this approach requires an appropriate assessment of the recipient bed.
A summary of our treatment algorithm for complex reoperative hypospadias repair (glans dehiscence, diverticulum, urethral stricture) is detailed in Fig. 27.7. This algorithm is different than that proposed by Snodgrass et al. [22] who does not see a role for vascularized flaps in reoperative hypospadias.
Postpubertal and Adult Complications
Adult hypospadias surgery is associated with a much greater complication rate even in de novo cases [5, 6]. Even though the techniques are similar, there are clear differences in wound healing, infections, and overall success rate. A number of steps may be taken to reduce the risk of complications in adults. All adults presenting for hypospadias repair should have a urine culture with directed treatment for positive cultures. Chronically infected or hair-bearing tissue should be removed at the time of surgery.
A postoperative suprapubic diversion may be beneficial from both a comfort and healing standpoint. A urethral catheter has a tendency to pull on the phallus, and this can be very uncomfortable in the postoperative period. This distal tension may also disrupt the glansplasty.
The adult “cripple” has an abnormal meatus, a scarred glans, curvature that is either intrinsic or related to ventral urethral contraction, an absent foreskin, and very thin or scarred ventral shaft skin that is usually adherent to the underlying urethra [42]. Any future surgery is complicated because well-vascularized skin is not available for flaps and the lack of a good vascular bed hinders the success of free grafts. If redundant tissue is present, it can be rearranged during a first stage and subsequently tubularized. Care should be taken to avoid the use of hair-bearing skin (Fig. 27.8).
A retrograde reveals distal tortuosity, stricture, and mild diverticular formation after prior hypospadias surgery (a). The phallus is degloved and the ventral urethra is opened. The tissue is rearranged distally, advanced into a deep glans cleft, and allowed to heal in preparation for a second stage (b). Six months later, there is a nice supple template available for tubularization and glansplasty (c–e). Although this was the result of inlay of vascular tissue, this is also the appearance after a free graft when adjacent genital skin is not available (Courtesy of S.B. Brandes)
Strictures often develop long after an apparently successful hypospadias repair. This may be secondary to failed growth at puberty, but Bracka suggests that balanitis xerotica obliterans is causative in at least 30 % of late hypospadias failures and strictures [43]. In these cases, a skin graft is doomed to failure, and buccal mucosa should be used as the graft material.
Surgical experience is a key to success, and ideally the extent of the problem can be determined preoperatively. Abnormalities of only the distal shaft and glans are more readily corrected than cases where the entire urethra needs to be replaced. In theory, even in reoperative cases, the glans (spongiosum) has excellent blood supply. If there is minimal glans injury, a deep cut into the ventrum gives an excellent vascular bed for a free graft.
If the urethral abnormality extends proximal to the glans, then the region between the glans and the more proximal normal spongiosum is at risk for recurrent fistula, stricture, or complete breakdown. A planned-staged procedure is preferable in these cases. The advantages of a staged repair are more reliable and secure graft revascularization. In addition, one can observe graft take or contraction prior to completing the secondary tubularization.
The phallus should be degloved and all ventral fibrotic tissues should be sharply excised. If curvature persists, then dorsal plications are usually performed. If the phallus is foreshortened and ventral grafting is performed, then a third operation will be required because a graft will not survive when placed on another graft. Snodgrass has described multiple transverse “feathered cuts” in the ventral corporal bodies at the time of a first-stage buccal mucosal graft. This is successful only if the graft is aggressively quilted to eliminate hematomas under the graft and improve the take.
After the curvature is corrected, the entirety of the denuded tunica albuginea is grafted (Fig. 27.6). The results of this procedure are assessed 6 months later for adequacy of graft take, depth of the glans cleft, and suppleness of the surrounding tissues. Tubularization of the urethra is completed only if these are satisfactory. A tunica vaginalis flap is usually available to cover this urethroplasty.
Urethral Hair
Urethral hair is an annoying complication that occurs when hair-bearing skin is inadvertently incorporated into a urethroplasty. Infections, calculi, and trichobezoar (hair ball) may result (Fig. 27.9). Obviously, the use of nonhair-bearing skin flaps or free grafts is preferable. Preemptive depilation of hair-bearing skin has been described, but electrocoagulation of the dermal papillae is usually ineffective because of poor depth of penetration. The Nd:YAG laser has 4- to 5-mm penetration and destroys hair follicles more effectively.
However, if hair-bearing skin has been previously used, eradication and prevention of recurrence is very important. When isolated hair is identified, endoscopic removal with laser coagulation of the base may be effective. When hair growth is more abundant, a urethrotomy should be performed. One has to decide whether the urethral segment needs to be replaced with a nonhair-bearing graft (in a staged fashion) or if the hair can be removed and the segment effectively depilated. If the segment then it should be closely followed for regrowth and chemical depilation can be attempted using reducing agents that break the cross-linkage disulfide bonds in keratin [44].
Editorial Comment
I often joke that when I see an adult patient with urethral stricture who comes to the office with his parents, I can always accurately guess that he is a “hypospadias cripple.” Strictures in the hypospadias cripple are difficult to treat, in particular because of the psychological baggage and number of years that the patient and his family have suffered. Early in my surgical career, I was often overly aggressive and tried to manage adult hypospadias cripple patients with one-stage repairs. While surgically complex and elegant looking and often requiring the use of a combination of grafts and flaps, the failure was exceedingly high. After prior failed hypospadias repair, one-stage penile skin flaps typically fail, because the blood supply is often compromised (especially flap vascularity) and disrupted from prior surgical mobilization and the penile skin is scarred.
I have evolved my surgeries for hypospadias cripples to a staged approach of buccal grafts followed by a 2nd or 3rd stage to tabularize 6–12 months later. To prevent urethrocutaneous fistula formation, I typically interpose a tunica vaginalis flap at the final stage. The key is to keep the penis on stretch when tabularizing the plate and while mobilizing the tunica vaginalis to the external ring (if not mobilized enough, with erection, the testes will be pulled up into the high scrotum or groin). Barbagli recently reported his experience with 1,176 hypospadias cripples. Highlighting the complexity and difficulty of reconstruction such adult patients, they required a median of 3 operations for repair, with 10 % requiring more than 5 operations. Success rates for the staged approach in adults range from 67 to 86 %. My general personal surgical experience with hypospadias cripples has been at the lower end of the range – with roughly a 30 % complication rate – whether it be restricture, diverticulum, post-void dribbling, chordee, or urethrocutaneous fistula.
At the second (or third) stage, where we tubularize the urethra, if the plate is a little narrow (<3 cm), I will place an inlay buccal graft in the Asopa technique. As per the Dennis Browne principle, the primary purpose of the urethral Foley, if to act as a scaffold to promote epithelization, and not really for urinary drainage. I place a 12 F Foley for the urethra, in order to prevent ischemic compression of the mucosa and to promote periurethral gland drainage (glands of Littré). I plug the urethral Foley and keep the SP to gravity, as I have had many patients with just a urethral Foley who accidently pulled or slept on the catheter, resulting in disruption of the suture line, resulting in an iatrogenic subcoronal hypospadias.
Occasionally, the hypospadias adult patient presents with a urethral stricture well away from the prior surgical site – such as in the bulbar urethra. For such strictures, I typically have shied away from stricture and primary anastomosis repairs, as the collateral and bipedal blood flow to the penile urethra is often poor. As the hypospadias-constructed penile urethra is often nothing more than a skin tube, rather than a vascular corpus spongiosum, there is deficient vascularity supplied from perforators and circumflex arteries. I am concerned that transecting the urethra as in an EPA will lead to ischemia of the distal urethra/spongiosum. For such bulbar strictures, I prefer to perform an onlay buccal graft. For distal bulb strictures, I place the graft dorsal and for the mid- and proximal bulb strictures, I place the graft ventral. See the algorithm in Fig. 27.10 – it is a nice summary of the general surgical strategy for the hypospadias cripple and a little more detailed than the one supplied in the above chapter.
Algorithm for the surgical management of the adult with failed hypospadias reconstruction (From Myers et al. [45])
—Steven B. Brandes
References
Baskin LS, Duckett JW, Ueoka K, et al. Changing concepts of hypospadias curvature lead to more onlay island flap procedures. J Urol. 1994;151:191–6.
El-Sherbiny MT, Hafez AT, Dawaba MS, et al. Comprehensive analysis of tubularized incised-plate urethroplasty in primary and re-operative hypospadias. BJU Int. 2004;93:1057–61.
Zargooshi J. Tube-onlay-tube tunica vaginalis flap for proximal primary and reoperative adult hypospadias. J Urol. 2004;171:224–8.
Bracka A. A versatile two-stage hypospadias repair. Br J Plast Surg. 1995;48:345–52.
Hensle TW, Tennenbaum SY, Reiley EA, Pollard J. Hypospadias repairs in adults: adventures and misadventures. J Urol. 2001;165:77–9.
Ching CB, Wood HM, Ross JH, Gao T, Angermeier KW. The Cleveland Clinic experience with adult patient undergoing hypospadias repair; their presentation and a new classification system. BJU Int. 2011;107:1142–6.
Gorduza DB, Gay CL, Silva EDM, Demède D, Hameury F, Berthiller J, Mure P-Y, Mouriquand PD. Does androgen stimulation prior to hypospadias surgery increase the rate of healing complications? – A preliminary report. J Pediatr Urology. 2011;7:158.
Snodgrass W, Cost N, Nakonezny PA, Bush N. Analysis of risk factors for glans dehiscence after tubularized incised plate hypospadias repair. J Urol. 2011;185:1845–9.
Cağrı Savaş M, Kapucuoğlu N, Gürsoy K, Başpınar S. The microvessel density of the hypospadiac prepuce in children. J Pediatr Urology. 2011;7:162–5.
Gilliver SC, Ashworth JJ, Ashcroft GS. The hormonal regulation of cutaneous wound healing. Clin Dermatol. 2007;25:56–62.
Waterman BJ, Renschelt T, Cartwright PC, et al. Variables in successful repair of urethrocutaneous fistula after hypospadias surgery. J Urol. 2002;168:726–30.
Churchill BM, Van Savage JG, Khoury AE, McLorie GA. The dartos flap as an adjunct in preventing urethrocutaneous fistulas in repeat hypospadias surgery. J Urol. 1996;156:2047–9.
Landau EH, Gofrit ON, Meretyk S, et al. Outcome analysis of tunica vaginalis flap for the correction of recurrent urethrocutaneous fistula in children. J Urol. 2003;170:1596–9.
Heaton BW, Snow BW, Cartwright PC. Repair of urethral diverticulum by placation. Urology. 1994;44:749–52.
Husmann DA, Rathbun SR. Long-term followup of visual internal urethrotomy for management of short (less than 1 cm) penile urethral strictures following hypospadias repair. J Urol. 2006;176:1738–41.
Vandersteen DR, Husmann DA. Late onset recurrent penile chordee after successful correction at hypospadias repair. J Urol. 1998;160:1131–3.
Secrest CL, Jordan GH, Winslow BH, et al. Repair of complications of hypospadias surgery. J Urol. 1993;150:1415–8.
Soylet Y, Gundogdu G, Yesildag E, Emir H. Hypospadias reoperations. Eur J Pediatr Surg. 2004;14:188–92.
Borer JG, Bauer SB, Peters CA, et al. Tubularized incised plate urethroplasty: expanded use in primary and repeat surgery for hypospadias. J Urol. 2001;165:581–5.
Shanberg AM, Sanderson K, Duel B. Re-operative hypospadias repair using the Snodgrass incised plate urethroplasty. BJU Int. 2001;87:544–7.
Yang SSD, Chen SC, Hsieh CH, Chen YT. Re-operative snodgrass procedure. J Urol. 2001;166:2342–5.
Snodgrass WT, Bush N, Cost N. Algorithm for comprehensive approach to hypospadias reoperation using 3 techniques. J Urol. 2009;182:2885–92.
Cakan M, Yalcinkaya F, Demirel F, et al. The midterm success rates of tubularized incised plate urethroplasty in reoperative patients with distal or midpenile hypospadias. Pediatr Surg Int. 2005;21:973–6.
Hayes MD, Malone PS. The use of dorsal buccal mucosal graft with urethral plate incision (Snodgrass) for hypospadias salvage. BJU Int. 1999;84:508–9.
Jayanthi VR, McLorie GA, Khoury AE, Churchill BM. Can previously relocated penile skin be successfully used for salvage hypospadias repair? J Urol. 1994;152:740–3.
Teague JL, Roth DR, Gonzales ET. Repair of hypospadias complications using the meatal based flap urethroplasty. J Urol. 1994;151:470–2.
Emir L, Erol D. Mathieu urethroplasty as a salvage procedure: 20-year experience. J Urol. 2003;169:2325–7.
Emir L, Bermiyanoglu C, Erol D. Onlay island flap urethroplasty: a comparative analysis of primary versus reoperative cases. Urology. 2003;61:216–9.
Simmons B, Cain MP, Casale A, et al. Repair of hypospadias complications using the previously utilized urethral plate. Urology. 1999;54:724–6.
Soutis M, Papandreou E, Mavridis G, Keramidas D. Multiple failed urethroplasties: definitive repair with the Duckett island-flap technique. J Pediatr Surg. 2003;38:1633–6.
Ehrlich RM, Alter G. Split-thickness skin graft urethroplasty and tunica vaginalis flaps for failed hypospadias repairs. J Urol. 1996;155:131–4.
Schreiter F, Noll F. Mesh graft urethroplasty using split thickness graft or foreskin. J Urol. 1989;142:1223–6.
Amukele SA, Stock JA, Hanna MK. Management and outcome of complex hypospadias repairs. J Urol. 2005;174:1540–3.
Koyle MA, Ehrlich RM. The bladder mucosal graft for urethral reconstruction. J Urol. 1987;138:1093–5.
Ransley PG, Duffy PG, Oesch IL, et al. The use of bladder mucosa and combined bladder mucosa/preputial skin grafts for urethral reconstruction. J Urol. 1987;138:1096–8.
Decter RM, Roth DR, Gonzales ET. Hypospadias repair by bladder mucosal graft: an initial report. J Urol. 1988;40:1256–8.
Duckett JW, Coplen D, Ewalt D, Baskin LS. Buccal mucosal urethral replacement. J Urol. 1995;153:1660–3.
Li L-C, Zhang X, Zhou S-W, et al. Experience with repair of hypospadias using bladder mucosa in adolescents and adults. J Urol. 1995;153:1117–9.
Ahmed S, Gough DCS. Buccal mucosal graft for secondary hypospadias repair and urethral replacement. Br J Urol. 1997;80:328–30.
Metro MJ, Wu H-Y, Snyder HM, et al. Buccal mucosal grafts: lessons learned from an 8-year experience. J Urol. 2001;166:1459–61.
Snodgrass W, Elmore J. Initial experience with staged buccal graft (Bracka) hypospadias reoperations. J Urol. 2004;172:1720–4.
Barbagli G, De Angelis M, Palminteri E, aLazzeri M. Failed hypospadias repair presenting in adults. Eur Urol. 2006;49:887–95.
Depasqualie I, Park AJ, Bracka A. The treatment of balanitis xerotica obliterans. BJU Int. 2000;86:459–65.
Singh I, Hemal AK. Recurrent urethral hairball and stone in a hypospadiac: management and prevention. J Endourol. 2001;15:645–7.
Myers JB, McAninch JW, Erikson BA, Breyer BN. Treatment of adults with complications from previous hypospadias surgery. J Urol. 2012;188:459–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Coplen, D.E. (2014). Reoperative Hypospadias Surgery and Management of Complications. In: Brandes, S., Morey, A. (eds) Advanced Male Urethral and Genital Reconstructive Surgery. Current Clinical Urology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4614-7708-2_27
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7708-2_27
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4614-7707-5
Online ISBN: 978-1-4614-7708-2
eBook Packages: MedicineMedicine (R0)