Abstract
Different scenarios embrace radiological imaging and colonic diverticula, including asymptomatic (diverticulosis) and symptomatic patients (acute diverticulitis, follow-up of acute diverticulitis, chronic diverticulitis). The role of imaging is in evolution; the role of computed tomography (CT) is validated and is widely supported by evidence in the case of acute diverticulitis, but this is not the case for acute diverticulitis follow-up or with symptoms related to diverticula without acute inflammation. In these settings, computed tomography colonography (CTC) is gaining consensus as the preferred radiological test.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Acute Diverticulitis
The evaluation of patients with acute diverticulitis includes medical history, physical examination, and laboratory testing, but cross-sectional imaging often plays a pivotal role in verifying the diagnosis. In fact, clinical suspicion of acute diverticulitis alone is correct in only 40–65% [1, 2], especially in patients with no previous diagnosis of diverticulosis. Different radiological tests can be applied for the diagnosis of acute diverticulitis, including ultrasound, computed tomography (CT), and magnetic resonance (MR) imaging. CT colonography (CTC) and double-contrast barium enema (DCBE) are contraindicated in the setting of suspected acute diverticulitis.
Conventional CT has a high sensitivity and specificity in the diagnosis of acute diverticulitis [2] and is generally considered by most to be the preferred front-line radiological test for evaluating patients with suspected acute diverticulitis.
The strengths of CT examination include its reproducibility, operator independence, wide availability, and high accuracy for diagnosing acute disease [2, 3]. CT allows for a comprehensive evaluation, including the grading of severity and detection of complications that affect therapeutic management.
Two meta-analyses [2, 3] have reported that ultrasound may have comparable accuracy in the evaluation of acute diverticulitis, although these data may be somewhat biased, and certain European scientific societies guidelines [1, 4,5,6] propose ultrasound as the first-line examination. This test is safe, low-cost, widely available, and easily accessible within the emergency department. Another advantage of ultrasound is the ability to correlate imaging findings with the region of greatest tenderness in real time. The relative disadvantages of ultrasound include operator dependence, difficulties in evaluation of the distal sigmoid colon, especially in obese patients, and a lower accuracy for abscess identification. Moreover, a severity classification cannot be assessed by ultrasound [7].
Currently, MR imaging does not play an important role in the workup of patients with suspected acute diverticulitis, but it can be considered in selected cases, such as pregnant women. Although there are some advantages compared with other radiological tests (e.g., lack of ionizing radiation exposure and high intrinsic contrast resolution), MR availability in the emergency department is currently limited in most hospital settings. Moreover, to date, there is relatively little evidence regarding the accuracy of MR for acute diverticulitis, limited to small select patient cohorts [8, 9].
Both CTC and DCBE are contraindicated in patients with acute diverticulitis, adding no additional useful information to conventional CT evaluation for acute management. Since both examinations include active colonic distention with either room air or carbon dioxide, there is at least a theoretical concern for extension of the typical microperforation associated with acute diverticulitis to more frank perforation and peritonitis. DCBE in particular is an obsolete test and should be abandoned, regardless of the clinical scenario. This test has a lower accuracy than CTC and optical colonoscopy for colorectal evaluation [10], is associated with higher ionizing radiation exposure [11], and is less acceptable for patients [12]. On occasion, findings of unsuspected mild acute or subacute diverticulitis may be encountered at CTC in patients with only minimal or no apparent symptoms.
1.1 CT Protocol
There has been some controversy over the appropriate CT protocol regarding the use of oral, rectal, and intravenous contrast agents. In general, the use of intravenous contrast should be encouraged in cases of suspected complicated disease to confirm the severity of the event and better diagnose complications such as abscesses and fistulas.
In cases of massive diverticular bleeding, it may not be possible to identify the source by colonoscopy, and angiographic or surgical therapy may be necessary [13,14,15].
Given the delay associated with bowel preparation and the difficulty of endoscopic visualization in the setting of large-volume hemorrhage, CT angiography has seen an increasing role in the initial workup of acute lower GI bleeding [16,17,18]. CT provides more information regarding localization and potential structural causes for the bleeding.
Vice versa, some authors [19, 20] suggested that the unenhanced CT examination alone is an accurate and valuable tool for triaging patients older than 75 years, presenting to the emergency department with nontraumatic acute abdominal pain.
In our experience, neither an oral nor a rectal contrast is truly necessary, whereas visceral obesity and, in particular, a high amount of pericolic fat is beneficial in visualizing the typical findings (i.e., perifocal stranding; inflamed diverticula; abscesses) of this acute event.
1.2 Typical CT Findings and Severity Classifications
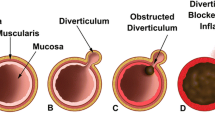
The diagnosis of acute diverticulitis can be directly made on the basis of localized bowel wall thickening that is centered on an inflamed diverticulum, with surrounding peridiverticular inflammation of pericolonic fat (Fig. 14.1). As diverticulitis is primarily an extraluminal disease, cross-sectional imaging holds a distinct advantage over luminal studies. Covered or free perforations can be rapidly and reliably diagnosed by the direct detection of air inclusions outside the intestinal lumen (Fig. 14.2), often associated with mesenteric fasciae thickening and free fluid. In case of severe disease, contrast-enhanced CT is an accurate test for diagnosing both parietal and peridiverticular abscesses (Fig. 14.3). When abscesses are present, CT is also useful for guiding abscess drainage, particularly in cases in which collections are small and located in regions difficult to assess [21].
Uncomplicated acute sigmoid diverticulitis in a 51-year-old woman with LLQ pain. (a) Unenhanced CT image showing inflamed sigmoid diverticula (arrow head) with extraluminal inflammatory changes surrounding the diverticula with thickening of the mesenteric fascia (arrows). (b) Contrast-enhanced CT image confirms uncomplicated acute sigmoid diverticulitis with an inflamed sigmoid diverticulum (arrow head), pericolonic fat stranding, and thickening of the mesenteric fascia (arrow); no abscess was present
Complicated acute sigmoid diverticulitis in a 50-year-old man with LLQ pain. (a) Contrast-enhanced axial CT image showing air inclusions outside the sigmoid colon lumen (arrow head) in a patient with sigmoid colon acute diverticulitis with evidence of extraluminal inflammatory changes surrounding the sigmoid diverticula. (b) Contrast-enhanced coronal CT image confirms complicated acute sigmoid diverticulitis with an inflamed sigmoid diverticulum (arrow), pericolonic fat stranding, and thickening of the mesenteric fascia (arrows); free perforations can be diagnosed by the direct detection of air inclusions outside the sigmoid colon and in the upper left quadrant (arrow heads)
Complicated acute sigmoid diverticulitis in a 56-year-old man diagnosed by contrast-enhanced CT examination. (a) Unenhanced axial CT image showing sigmoid diverticula with fat stranding and thickening of the mesenteric fascia. (b) Contrast-enhanced axial CT image showing intraparietal abscess (arrow head), not clearly visualizable at an unenhanced scan
CT evaluation is valuable for its appraisal of disease severity, which impacts therapeutic management.
There are many classifications of disease severity based on CT [6, 22,23,24,25] and none has been demonstrated to be clearly superior to the other. Among these, the modified version of the Hinchey classification has been used in several clinical trials and it is the most used in clinical practice.
This classification and that recently proposed by the WSES acute diverticulitis working group [25] strive to divide patients into two main categories, namely, uncomplicated and complicated acute diverticulitis.
In uncomplicated cases, the CT findings are generally limited to the phlegmonous reaction of the pericolonic fat tissue (Fig. 14.4a), whereas complicated features include peridiverticular abscess (Fig. 14.4b), significant pneumoperitoneum (Fig. 14.5), and diffuse peritonitis. Moreover, the CT grading of acute diverticulitis has prognostic significance in terms of disease recurrence after an initial episode of acute disease [26].
Examples of uncomplicated and complicated acute diverticulitis. (a) Contrast-enhanced axial CT image in a 60-year-old man showing mild acute diverticulitis with an inflamed sigmoid diverticulum with fat stranding (arrow heads). (b) Contrast-enhanced axial CT image in a 48-year-old man showing complicated acute diverticulitis with a large peridiverticular abscess (arrows) adjacent to the sigmoid diverticula
Complicated acute sigmoid diverticulitis in a 73-year-old man with a large abscess and pneumoperitoneum due to perforation of an inflamed sigmoid diverticulum. Laparoscopic surgery confirmed sigmoid perforation in the presence of acute diverticulitis and purulent peritonitis-treated Hartmann sigmoid colon surgical resection. (a) Contrast-enhanced axial CT image showing significant pneumoperitoneum (arrows). (b) Contrast-enhanced axial CT image showing free air (arrow) adjacent to the inflamed sigmoid diverticula
1.3 Differential Diagnosis
In addition to being highly accurate for acute diverticulitis itself, CT is also the most accurate test for diagnosing alternative conditions [27, 28] (Fig. 14.6). Several studies have described characteristic CT features differentiating diverticular disease from CRC [29, 30], but, in some cases, findings overlap and the differential diagnosis remains challenging. In our opinion, this difficulty can explain data obtained from two large trials [31, 32], describing a higher 1-year CRC risk for patients recovering from an acute episode of diverticulitis.
Descending colon nonspecific acute colitis mimicking acute diverticulitis in a 77-year-old man with COVID-19 infection. (a) Unenhanced axial CT image showing circumferential descending colon wall thickening (arrows) with fat stranding and thickening of the left anterior renal fascia. (b) Unenhanced axial CT image showing circumferential distal descending colon wall thickening (arrows) with fat stranding and thickening of the left anterior renal fascia. No diverticula are present
2 Chronic Diverticular Disease
In contrast to acute diverticulitis, the role of imaging in the follow-up of acute diverticulitis is in evolution and still subject to debate.
In this setting, the evidence is in favor of computed tomography colonography (CTC) as a preferred radiological test, suggesting a complementary role of CTC and colonoscopy [33, 34].
Regardless of the specific scenario, radiologists are first requested to confirm the diagnosis of diverticular disease, ruling out other diseases and in particular a superimposed CRC.
CTC is able to depict the test number and site of diverticula [35], morphology of the diverticula necks (Fig. 14.7), less common disease-related findings such as focal or diffuse wall thickening (Fig. 14.8), and sigmoid colon stenosis (Fig. 14.9) [36,37,38], better than others. Moreover, CTC is highly accurate for diagnosing complications (abscesses and fistulas), which represent a validated indication for elective surgery; fistulas in particular could be overlooked by conventional abdominal CT performed at the time of an acute event (Fig. 14.10).
Examples of wall thickening associated with sigmoid colon diverticula. (a) Axial CTC image showing mild sigmoid colon wall thickening (arrow heads) in the presence of sigmoid diverticula. These are typical findings of chronic diverticular disease. (b) Axial CTC image showing eccentric focal sigmoid colon wall thickening (arrow) in the presence of sigmoid diverticula. The benign nature of this finding has been confirmed at conventional colonoscopy
A 49-year-old man with marked sigmoid colon wall thickening and lumen stenosis after recovering from acute diverticulitis. (a) Double-contrast barium enema like-view CTC image showing sigmoid colon with severe lumen stenosis and sigmoid diverticula. (b) Axial 2D supine CTC image showing marked sigmoid colon wall thickening with severe lumen stenosis, in the presence of sigmoid diverticula
A 49-year-old man with a double enteroenteric fistula in chronic diverticular inflammation. (a) Axial CTC image showing sigmoid colon wall thickening of both the distal ileum and the sigmoid colon with adjacent fat stranding. (b, c) Coronal CTC images demonstrating the two sigmoid colon–ileum fistulae (arrow) and sigmoid colon wall thickening. The patient underwent CTC elective surgery with confirmation of two sigmoid colon–ileum fistulae in chronic diverticular disease
The advantage of CTC over colonoscopy in evaluating patients with diverticular disease relies on its minor invasiveness; even if diverticular disease is the first leading reason for a non-well-distended colonic tract at CTC [39], this test is always complete, different from colonoscopy. A high-quality CTC examination can be performed even in case of severe stenosis [34, 38], allowing adequate accuracy in diagnosing proximal colonic polyps and CRCs [40, 41].
This fact has a tremendous clinical impact if we consider the risk of advanced adenoma related to patients recovering from acute diverticulitis [42]. In particular, patients with severe stenosis caused by diverticular disease and responsive to an incomplete colonoscopy could have a significant delay in the diagnosis of proximal colon lesions (Fig. 14.11).
Positive CTC examination in a 57-year-old-man recovering from acute diverticulitis, with incomplete colonoscopy. (a, b) 2D axial CTC image (A) and 3D colon map (B) showing severe luminal narrowing associated with diverticula at the distal sigmoid colon, explaining the incomplete colonoscopy. (c) 3D endoluminal CTC view showing a nonpolypoid lesion in the transverse colon. (d, e) Axial 2D (D) and 3D endoluminal (E) CTC views showing a 20 mm pedunculated polyp in the ascending colon. (f) 3D endoluminal (H) CTC view showing a 7 mm sessile polyp in the transverse colon. The patient underwent subtotal colectomy; the pathology confirmed the presence of three right colon lesions revealing as tubular adenoma. In particular, the larger one contained high-grade dysplasia
Even if the literature concerning the use of CTC in the follow-up of patients recovering from an episode of acute diverticulitis is not yet robust enough, no complications have been reported and in particular no cases of perforation have ever been described [34, 43].
For patients recovering from an episode of acute diverticulitis, CTC should be carried out at least 3 or 4 months after the acute event to reduce both the risk of perforation and because of the likelihood of a residual acute inflammatory component.
2.1 CTC Protocol
It may be advisable to slightly modify the standard CTC protocol in the setting of a known complicated diverticular disease. For example, it can be useful to perform the CTC examination with an IV contrast in the presence of severe wall thickening and luminal stenosis, when the differential diagnosis between diverticular disease and CRC is more relevant. Another scenario generally requiring an IV contrast is when there is potential concern for a diverticular complication such as abscesses or fistulas. Evaluation with soft tissue windowing improves the assessment for these complications over the standard CTC polyp window. In patients with severe diverticular disease, an additional third scan in the right lateral decubitus position (after supine and prone) can be valuable for confirming the severity of both luminal stenosis and wall thickening, avoiding errors caused by colon spasms [43,44,45]. To achieve the best distention of the sigmoid colon, which is most commonly involved in diverticular disease, the right lateral decubitus position is generally obtained for gravitational reasons. Moreover, a lateral decubitus position is much more comfortable and feasible for obese and otherwise debilitated patients [45].
To optimize distention of the entire colon, which is critical for a high-quality examination, automated carbon dioxide insufflation is preferred [46]. In addition, a spasmolytic agent may help optimize distention as well. Taylor et al. [47] demonstrated significantly improved distention using hyoscine butylbromide as a hypotonic drug in CTC, given that it is especially useful in patients with diverticulosis. Carbon dioxide insufflation with an automatic device is preferable when evaluating patients with diverticular disease because of the continuous low pressure and reproducible distention. When using room air, the risk of perforation is increased due to the high-pressure values that can be achieved. If the patient has only recently recovered from acute diverticulitis, it may be reasonable to scan the entire abdomen and pelvis before initiating insufflation. If the pre-insufflation scan shows signs suggesting persistent acute diverticulitis, active colonic distention should be aborted (Fig. 14.12).
Unsuspected persistent complication from diverticulitis detected at CTC. (a) 2D axial CT image taken before carbon dioxide insufflation in a patient with a recent episode of diverticulitis showing air bubbles (arrows) around the sigmoid colon related to perforation and ongoing inflammation. Thus, the scheduled CTC was not performed and the patient was referred for therapeutic management. (b) 2D sagittal CTC image confirms the presence of air bubbles (arrows) around the sigmoid colon due to recent covered perforation
2.2 Diverticular Disease Severity Score Based on CT Colonography
Wall thickening and lumen stenosis are the two CTC features that need to be investigated to describe the severity of the disease in follow-up, and, recently, a diverticular disease severity score (DDSS) based on CTC findings has been proposed [43]. The score is based on the varying degrees of these two CTC findings, i.e., wall thickening and lumen stenosis, and consists of four grades (DDSS 1–4). In the case of DDSS grade 4 (Fig. 14.13), where marked wall thickening is associated with severe luminal stenosis, surgical options should be considered. In practice, the simultaneous presence of severe stenosis and the inability to exclude CRC are both potential indications for surgery [48]. Moreover, this validated CTC-based DDSS score is a good predictor of chronic inflammation and fibrosis [49] and seems to have prognostic value in the follow-up of acute diverticulitis [50].
CTC examination in a 66-year-old-woman with recurrent diverticulitis (DDSS 4). (a, b) Axial 2D image (a) and sagittal 2D CTC image (b) showing marked sigmoid wall thickening (arrows) and luminal narrowing associated with diverticula in the setting of sigmoid diverticular disease, classified as DDSS 4. The patient underwent elective surgery, and the pathology revealed diverticular disease with acute and chronic inflammation
2.3 Differential Diagnosis Between Diverticular Disease and Colorectal Cancer
In patients with diverticular disease, it can be challenging to recognize a superimposed colorectal cancer (CRC), but these two entities are both relatively common in elderly patients and can therefore coexist. This differential diagnosis is particularly tricky in cases of marked wall thickening and severe luminal stenosis from diverticular disease. Some authors [36, 37] have described a number of CTC findings as being useful in differentiating these two disease entities. Of these various findings, the absence of diverticula in the affected segment and the presence of a shoulder phenomenon are the two most important findings for CRC (Fig. 14.14). Other CTC signs in favor of cancer include shorter length with straightening of the involved segment, the absence of mesenteric fascia thickening, the presence of distorted folds, and the presence of prominent local lymph nodes.
Sigmoid diverticular disease versus cancer at CTC. (a) 2D axial CTC image in a 59-year-old-woman showing focal sigmoid wall thickening with severe luminal narrowing, shoulder formation (arrow), and diverticula adjacent to, but not within, the affected segment. The patient underwent a same-day colonoscopy with biopsies, and CRC diagnosis was confirmed. The pathology after surgery revealed adenocarcinoma (pT3N2b). (b) 2D axial CTC image showing circumferential segmental wall thickening and luminal narrowing of the sigmoid colon associated with multiple diverticula (arrow). The presence of diverticula is a key factor for excluding cancer. This was a diverticular stricture
Lips et al. [37] described a prevalence of about 4–5% of their population where findings of advanced diverticular disease versus CRC are present. We believe that this prevalence could be substantially higher in some settings, including those patients recovering from a prior episode of acute diverticulitis with CTC. The above-mentioned criteria are useful for ruling out CRC, but sometimes the CTC findings will overlap. In these selected cases, referral to optical colonoscopy or flexible sigmoidoscopy may be necessary to allow for direct mucosal evaluation and biopsy. In other cases, the surgical option may be indicated regardless of the underlying cause.
2.4 Preoperative Surgical Information
There are a variety of treatment options for patients with chronic diverticular disease, leading to some controversy in the surgical guidelines [48]. In particular, new surgical guidelines [51,52,53] recommend a more conservative and case-by-case approach, taking into account multiple factors, including patient age, patient’ s comorbidities (i.e., immune status), number of recurrent episodes of acute diverticulitis, the presence of complications, and patient preferences. Before elective surgery, surgeons could benefit from detailed anatomic information regarding the entire colon, and CTC, in our opinion, represents the test of choice for providing this. In this regard, CTC is clearly superior to both optical colonoscopy and the barium enema. In particular, CTC provides detailed information on colon anatomy, total number and distribution of diverticula (Fig. 14.15), and the degree of wall thickening and luminal stenosis. Surgical treatment is often considered when CTC detects unsuspected complications, such as abscess or fistula. CTC can also guide clinicians and surgeons when the appropriate therapeutic management is uncertain. For example, CTC diagnosis of unsuspected severe luminal stenosis could be a key factor in deciding on a surgical option. The surgical approach is generally laparoscopic, and surgeons could benefit from information about the vascular map derived from CTC (Fig. 14.16) [54, 55]. Of course, to obtain this level of detail requires a contrast-enhanced CTC protocol, adding an arterial contrast phase to the standard portal venous phase. In general, the initial position (e.g., prone) is obtained prior to the IV contrast, allowing for assessment of enhancement.
Examples of a different distribution of diverticula in two patients who are candidates for elective surgery. (a) 3D computed tomography colonographic color map. The image shows diverticula limited to the sigmoid colon. (b) 3D computed tomography colonographic color map. The image shows diverticula spread in the whole colon
Examples of a vascular 3D map provided by CT colonography. (a) 2D axial CTC image showing multiple diverticula limited to the sigmoid colon. (b) 3D-fused image demonstrating the sigmoid arteries (SAs) branching from the left colic artery (LCA) and the accessory left colic artery (ALCA) branching from the middle colic artery (MCA). LCA and SAs run anteriorly to the inferior mesenteric vein
References
Andeweg CS, Mulder IM, Felt-Bersma RJ, et al. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg. 2013;30:278–92.
Lameris W, van Randen A, Bipat S, et al. Graded compression ultrasonography and computed tomography in acute colonic diverticulitis: meta-analysis of test accuracy. Eur Radiol. 2008;18:2498–511.
Liljegren G, Chabok A, Wickbom M, et al. Acute colonic diverticulitis: a systematic review of diagnostic accuracy. Colorectal Dis. 2007;9:480–8.
Fozard JB, Armitage NC, Schofield JB, et al. ACPGBI position statement on elective resection for diverticulitis. Color Dis. 2011;13(suppl 3):1–11.
Nederlandse Vereniging voor Heelkunde. Richtlijn “Diagnostiek en behandeling acute diverticulitis van het colon” (Dutch Society of Surgery. Guideline “Diagnosis and Treatment of Acute Colonic Diverticulitis”). 2012. http://heelkunde.nl/uploads/mu/22/mu22HtlbEpr-SLLyAdT5nQ/NVvH-richtlijn-Acute-diverticulitis-van-het-colon-2012.pdf. Accessed June 2013.
Schreyer AG, Layer G. S2k guidelines for diverticular disease and diverticulitis: diagnosis, classification, and therapy for the radiologist. Fortschr Röntgenstr. 2015;187:676–84.
Schultz JK, Azhar N, Binda GA, et al. European Society of Coloproctology: guidelines for the management of diverticular disease of the colon. Color Dis. 2020;22(Suppl 2):5–28. https://doi.org/10.1111/codi.15140. Epub 2020 Jul 7
Oh KY, Gilfeather M, Kennedy A, et al. Limited abdominal MRI in the evaluation of acute right upper quadrant pain. Abdom Imaging. 2003;28:643–51.
Heverhagen JT, Sitter H, Zielke A, et al. Prospective evaluation of the value of magnetic resonance imaging in suspected acute sigmoid diverticulitis. Dis Colon Rectum. 2008;51:1810–5.
Halligan S, Wooldrage K, Dadswell E, Kralj-Hans I, von Wagner C, et al. Computed tomographic colonography versus barium enema for diagnosis of colorectal cancer or large polyps in symptomatic patients (SIGGAR): a multicentre randomised trial. Lancet. 2013;381(9873):1185–93. https://doi.org/10.1016/S0140-6736(12)62124-2. Epub 2013 Feb 14
Neri E, Faggioni L, Cerri F, Turini F, Angeli S, et al. CT colonography versus double-contrast barium enema for screening of colorectal cancer: comparison of radiation burden. Abdom Imaging. 2010;35(5):596–601. https://doi.org/10.1007/s00261-009-9568-x. Epub 2009 Sep 24
Stevenson G. Colon imaging in radiology departments in 2008: goodbye to the routine double contrast barium enema. Can Assoc Radiol J. 2008;59(4):174–82.
Jensen DM, Machicado GA, Jutabha R, et al. Urgent colonoscopy for the diagnosis and treatment of severe diverticular haemorrhage. N Engl J Med. 2000;342:78–82.
Bloomfeld RS, Rockey DC, Shetzline MA. Endoscopic therapy of an acute diverticula hemorrhage. Am J Gastroenterol. 2001;96:2367–72.
Smoot RL, Gostout CJ, Rajan E, et al. Is early colonoscopy after admission for acute diverticular bleeding needed? Am J Gastroenterol. 2003;98:1996–9.
Hizaya K, Miura N, Matsumoto T, Iida M. Colonic diverticular bleeding: precise localization and successful management by a combination of CT angiography and interventional radiology. Abdom Imaging. 2009;34:777–9.
Loffroy R, Multidetector CT. Angiography for the detection of colonic diverticular bleeding: when, how, and why? Dig Dis Sci. 2013;58:1822–4.
Nagata N, Niikura R, Aoki T, Moriyasu S, Sakurai T, et al. Role of urgent contrast-enhanced multidetector computed tomography for acute lower gastrointestinal bleeding in patients undergoing early colonoscopy. J Gastroenterol. 2015;50:1162–72.
Barat M, Paisant A, Calame P, et al. Unenhanced CT for clinical triage of elderly patients presenting to the emergency department with acute abdominal pain. Diagn Interv Imaging. 2019;100:709–19.
Millet I, Sebbane M, Molinari N, et al. Systematic unenhanced CT for acute abdominal symptoms in th elderly patients improves both emergency deprtment diagnosis and prompt clinical management. Eur Radiol. 2017;27:868–77.
Expert panel on gastrointestinal imaging, Galgano SJ, MM MN, Peterson CM, et al. ACR appropriateness criteria left lower quadrant pain suspected diverticulitis. J Am Coll Radiol. 2019;16:S141–9.
Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109.
Klarenbeek BR, de Korte N, van der Peet DL, Cuesta MA. Review of current classifications for diverticular disease and a traslation into clinical practice. Int J Color Dis. 2012;27:207–14.
Tursi A, Brandimarte G, Di Mario F, Andreoli A, Annunziata ML, et al. Development and validation of an endoscopic classification of diverticular disease of the colon: the DICA classification. Dig Dis. 2015;33(1):68–76. https://doi.org/10.1159/000366039. Epub 2014 Dec 17
Sartelli A, Moore FA, Ansaloni L, Di Saverio S, Coccolini F, et al. A proposal for a CT driven classification of left colon acute diverticulitis. World J Emerg Surg. 2015;10:3.
Ambrosetti P. Value of CT for acute left-colonic diverticulitis: the Surgeon’s view. Dig Dis. 2012;30:51–5.
Stoker J, van Randen A, Lameris W, Boermeester MA. Imaging patients with acute abdominal pain. Radiology. 2009;253:31–46.
van Randen A, Lameris W, Nio CY, et al. Inter-observer agreement for abdominal CT in unselected patients with acute abdominal pain. Eur Radiol. 2009;19:1394–407.
Chintapalli KN, Chopra S, Ghiatas AA, et al. Diverticulitis versus colon cancer: differentiation with helical CT findings. Radiology. 1999;210:429–35.
Shen SH, Chen JD, Tiu CM, et al. Differentiating colonic diverticulitis from colon cancer: the value of computed tomography in the emergency setting. J Chin Med Assoc. 2005;68:411–8.
Granlund J, Svensson T, Granath F, et al. Diverticular disease and the risk of colon cancer: a population based case-control study. Aliment Pharmacol Ther. 2011;34:675–81.
Huang WY, Lin CC, Jen YM, et al. Association between colonic diverticular disease and colorectal cancer: a nationwide population-based study. Clin Gastroenterol Hepatol. 2014;12:1288–94.
Flor N, Maconi G, Cornalba GP, Pickhardt PJ. The current role of radiologic and endoscopic imaging in diagnosis and foloow-up of colonic diverticular disease. AJR Am J Roentgenol. 2016;207:15–24.
Hjern F, Jonas E, Holmstrom B, Josephson T, Mellgren A, Johansson C. CT colonography versus colonoscopy in the follow-up of patients after diverticulitis. A prospective, comparative study. Clin Radiol. 2007;62:645–50.
De Cecco CN, Ciolina M, Annibale B, et al. Prevalence and distribution of colonic diverticula assessed with CT colonography. Eur Radiol. 2016;26(3):639–45. https://doi.org/10.1007/s00330-015-3866-1. Epub 2015 Jun 24
Gryspeerdt S, Lefere P. Chronic diverticulitis vs. colorectal cancer: findings on CT colonography. Abdom Imaging. 2012;37(6):1101–9. https://doi.org/10.1007/s00261-012-9858-6.
Lips LM, Cremers PT, Pickhardt PJ, Cremers SE, Janssen-Heijnen ML, de Witte MT, Simons PC. Sigmoid cancer versus chronic diverticular disease: differentiating features at CT colonography. Radiology. 2015;275(1):127–35. https://doi.org/10.1148/radiol.14132829. Epub 2014 Nov 26
Flor N, Rigamonti P, Di Leo G, et al. Technical quality of CT colonography in relation with diverticular disease. Eur J Radiol. 2012;81(3):e250–4.
Pichkardt PJ, Kim D. CT colonography. Pitfalls in interpretation. Radiol Clin N Am. 2013;51:69–88.
Sanford M, Pickhardt PJ. Diagnostic performance of primary 3-dimensional computed tomography colonography in the setting of colonic diverticular disease. Clin Gastroenterol Hepatol. 2006;4:1039–47.
Flor N, Sardanelli F, Pickhardt PJ. Diagnostic accuracy of CT colonography for the detection of polyps in the diverticular disease. Scand J Gastroenterol. 2014;49(3):383–4.
Theranian S, Klinge M, Saul M, et al. Prevalence of colorectal cancer and advanced adenoma in patients with acute diverticulitis: implications for follow-up colonoscopy. Clin Endosc. 2020;91:634–40.
Flor N, Rigamonti P, Pisani Ceretti A, et al. Diverticular disease severity score based on CT colonography. Eur Radiol. 2013;23(10):2723–9.
Buchach CM, Kim DH, Pickhardt PJ. Performing an additional decubitus series at CT colonography. Abdom Imaging. 2011;36(5):538–44. https://doi.org/10.1007/s00261-010-9666-9.
Pickhardt PJ, Bakke J, Kuo J, Robbins JB, Lubner MG, del Rio AM, Kim DH. Volumetric analysis of colonic distention according to patient position at CT colonography: diagnostic value of the right lateral decubitus series. AJR Am J Roentgenol. 2014;203:W623–8.
Shinners TJ, Pickhardt PJ, Taylor AJ, Jones DA, Olsen CH. Patient-controlled room air insufflation versus automated carbon dioxide delivery for CT colonography. AJR Am J Roentgenol. 2006;186:1491–6.
Taylor SA, Halligan S, Goh V, Morley S, Bassett P, Atkin W, Bartram CI. Optimizing colonic distention for multi-detector row CT colonography: effect of hyoscine butylbromide and rectal balloon catheter. Radiology. 2003;229(1):99–108.
Köhler L, Sauerland S, Neugebauer R, et al. Diagnosis and treatment of diverticular disease. Results of a consensus development conference. Surg Endosc. 1999;13(4):430–6.
Flor N, Pickhardt PJ, Maconi G, et al. CT colonography followed by elective surgery in patients with acute diverticulitis: a radiological-pathological correlation study. Abdom Radiol (NY). 2021;46:491–7.
Flor N, Maconi G, Sardanelli S, et al. Prognostic value of the diverticular disease severity score based on CT colonography: follow-up in patients recovering from acute diverticulitis. Acad Radiol. 2015;22:1503–9.
Hall J, Hardiman K, Lee S, et al. The american society of colon and rectal surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum. 2020;63:728–47.
Sartelli A, Weber DG, Kluger Y, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emer Surg. 2020;15:32.
Francis NK, Sylla P, Abou-Khalil M, et al. EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc. 2019;33:2726–41.
Matsuki M, Okuda J, Kanazawa S, Kanamoto T, Inada Y, Tatsugami F, et al. Virtual CT colectomy by three-dimensional imaging using multidetector-row CT for laparoscopic colorectal surgery. Abdom Imaging. 2005;30:698–707.
Flor N, Campari A, Ravelli A, Lombardi MA, Pisani Ceretti A, et al. Vascular map combined with CT Colonography for evaluating candidates for laparoscopic colorectal surgery. Korean J Radiol. 2015;16:821–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Flor, N., Innamorati, S., Pickhardt, P. (2022). Radiology. In: Tursi, A., Bafutto, M., Brandimarte, G., Chaves de Oliveira, E. (eds) Colonic Diverticular Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-93761-4_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-93761-4_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-93760-7
Online ISBN: 978-3-030-93761-4
eBook Packages: MedicineMedicine (R0)