Abstract
Sleep is commonly impaired during peripartum due to anatomical, endocrinological, physiological, psychological, behavioral, socioeconomic, and cultural factors. Cumulative evidence suggests that disrupted sleep in pregnancy is linked to negative gestational and birth outcomes, including an increased risk of peripartum psychopathology. Disturbed sleep has been associated with the emergence of new depressive symptoms in pregnancy and postpartum and may be the final common pathway in the development of postpartum psychotic episodes. Most importantly, sleep disturbances during peripartum have linked to an increased suicidal risk. Maternal sleep patterns in pregnancy may also entrain infant sleep patterns, which can in turn lead to disrupted maternal postpartum sleep. Sleep in the perinatal period has been considered a family issue with potential short-term and the long-term consequences on the mental health of the whole family, in particular modifying a child’s vulnerability to mental health across the lifespan. In this framework, assessing and treating sleep disturbances during peripartum should be a priority in clinical practice. It might reduce the risk for postpartum psychopathology and prevent short-term/long-term consequences on the whole family’s mental health. Alternatively, modulation of sleep–wake patterns could offer relief to women in whom symptoms of these disorders have already developed. In this chapter, pregnancy-related changes in sleep physiology and the most frequent sleep disturbances in peripartum are discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Sleep is an important regulatory psychophysiological behavior in life, influencing mood, emotion regulation, and impulse behavior, which are key mediators of stress adjustments commonly needed in the perinatal period [1]. Consistently, sleep problems are recognized as a major risk factor for mental health and health problems in general [2, 3], while sleep is commonly impaired during peripartum [1, 4,5,6,7]. Women’s sleep during pregnancy and postpartum is altered by anatomical, endocrinological, physiological, psychological, behavioral, socioeconomic, and cultural factors [6].
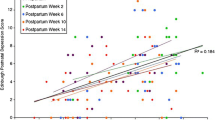
These changes have the potential to affect sleep duration, sleep quality, sleep pattern, and breathing during sleep, hence predisposing pregnant women to sleep disturbances during peripartum [1, 4,5,6,7]. In fact, evidence clearly shows that peripartum sleep disruption is reported by most women. Most common problems during all three trimesters include short sleep duration, poor sleep quality, and insomnia [1, 4,5,6,7], which tend to persist and worsen during postpartum [8], but also nightmares, sleep-disordered breathing, and restless legs syndrome [6, 7]. Cumulative evidence suggests that disrupted sleep in pregnancy has been linked to negative gestational and birth outcomes [9], emergency cesarean section [10], and gestational diabetes [11]. Most importantly, insomnia and poor sleep quality during peripartum have been found to be prospective risk factors for peripartum psychopathology, including mood disorders, postpartum blues, and psychosis. In particular, disturbed sleep has been considered a risk factor for unipolar and bipolar depression during the prenatal and postpartum periods [1, 4, 12, 13]. Disturbed sleep has been associated with the emergence of new depressive symptoms in pregnancy, such that sleep disturbances in early pregnancy predict depressive symptoms in late pregnancy. Similarly, sleep disturbances in late pregnancy assessed both objectively and subjectively have been shown to independently predict symptoms of postpartum depression [1, 4, 12, 13]. In addition, potentially, sleep disruption during pregnancy may mediate the relation between postpartum blues and increased risk of postpartum depression [14]. Sharma et al. (2003) [15] have discussed that sleep loss/disruption may be the final common pathway in the development of postpartum psychotic episodes. Most importantly, sleep disturbances during peripartum have been linked to an increased suicidal risk [16, 17].
Maternal sleep patterns in pregnancy may also entrain infant sleep patterns, such that disrupted maternal sleep in pregnancy is associated with worse infant sleep, which can in turn lead to disrupted maternal postpartum sleep [8, 18]. Sleep in the perinatal period has been considered a family issue with potential short-term consequences on child and whole family mental health and, in the long-term, modifying child’s vulnerability to mental health during adult life [1, 18].
In this framework, assessing and treating sleep disturbances during peripartum should be a priority in clinical practice. It might reduce the risk for postpartum psychopathology and prevent short-term/long-term consequences on the whole family’s mental health. Alternatively, modulation of sleep–wake patterns could offer relief to women in whom symptoms of these disorders have already developed. In this chapter, pregnancy-related changes in sleep physiology and the most frequent sleep disturbances in peripartum are discussed.
2 Pregnancy-Related Changes in Sleep Physiology
Pregnancy is a physiological condition characterized by profound biological changes, which have a significant influence on sleep [6, 7]. The typically increased secretion of several hormones across pregnancy considerably affects both the circadian and homeostatic components of sleep regulation, leading to modifications of sleep architecture [6, 14]. Pregnancy causes changes in melatonin and cortisol as well as gonadal steroids such as estrogen and progesterone and pituitary hormones such as gonadotropins, prolactin, and growth hormone, and these changes may affect sleep [6]. In human studies, nonrapid eye movement sleep (NREM) has been shown to be enhanced by progesterone and prolactin, while rapid eye movement sleep (REM) is decreased by progesterone and increased by estrogens. In particular, progesterone has sleep-inducing action on brain gamma-aminobutyric acid (GABA) receptors, producing a soporific effect and a significant increase in nonrapid eye movement (NREM) sleep. This effect may partly explain daytime sleepiness and fatigue in the first trimester when progesterone is steadily rising. The increased respiratory rate caused by progesterone may protect the airway from occlusion, protecting from SDB. Indeed, the thermogenic effect of progesterone elevates core body temperature, and its inhibitory effect on smooth muscle (including gastrointestinal tract, ureters, and bladder) indirectly influences sleep and favors more awakenings during the night with low sleep quality disturbances [6, 19, 20]. Estrogen secreted by the placenta increases significantly during pregnancy, reaching peak levels before birth and declining thereafter. Estrogen has excitatory effects on the nervous system and selectively decreases REM sleep, its concentration during pregnancy causes vasodilation, and women typically experience nasal congestion that might contribute to SDB. Estrogen also stimulates prolactin production and suppresses dopamine release, contributing to RLS disturbances [6, 19, 20]. Oxytocin peaks during the night, promoting uterine contractions, might lead to sleep fragmentation. Cortisol and growth hormone levels are also elevated, affecting sleep quality and inducing daytime sleepiness [6, 7]. Melatonin, which is the major regulator of circadian rhythms, is secreted by the pineal gland and is activated by darkness and suppressed by light; melatonin levels increase in the third trimester. Melatonin synergizes with oxytocin to promote the birth process. Altered rhythm or low levels of melatonin secretion, which is related to sleep disturbances, might potentially result in some pregnancy complications and in pregnancy psychopathology (for an overview, see Izci-Balserak et al. 2017, Kay-Stacey et al. 2017) [19, 20]. Besides hormones, other factors that are essential to maintain a healthy pregnancy may contribute to sleep disruption during pregnancy, such as gastroesophageal reflux, affecting up to 75% of pregnant women, nocturnal micturition, due to an increase in overnight sodium excretion, anatomical changes related to the growing uterus, and increased body weight [6, 19, 20]. Moreover, iron and folate deficiency may play a role in the occurrence of sleep-related movement disorders in pregnant women [6, 19, 20].
With the physical and hormonal adaptations in pregnancy, changes in sleep are common, from 66% to 97% of women [19, 20]. During the first trimester, women experience daytime sleepiness and fatigue and report more frequent naps, an increase in total sleep time (TST), longer sleep onset latency, and more wake time after sleep onset (WASO). Overall sleep quality, sleep duration, and deep sleep decrease in this period. Hormones are responsible for fatigue and daytime sleepiness, morning sickness, waking with nausea, increased urinary frequency, physical discomforts such as back pain, and mood changes, which may all contribute to sleep disturbances in this period [19, 20]. Psychosocial stressors, if in the case of first-time or unplanned pregnancies, might also contribute to sleep disturbances in this first trimester [4, 19, 20]. In the second trimester, most women report less fatigue and less wake time after sleep onset (WASO) compared to the first one, with an average of more than 7 h per night in the second trimester likely due to the stabilization of hormone levels. By the end of the second trimester, however, the number of awakenings increases. Accordingly, women may experience disturbed sleep because of the onset of snoring, heartburn, irregular uterine contractions, fetal movements, or leg cramps [4, 19, 20]. Vivid dreams and pain in the back, neck, and joints were additional reasons for sleep disruption during the second trimester. The majority, from 75% to 98%, of women report sleep disturbances during the third trimester of pregnancy with high WASO and increased light sleep and reduction in deep sleep [1, 4, 19, 20]. Nocturnal sleep time is lower than the first two trimesters, with more frequent and longer daytime naps. Physical changes associated with a rapidly growing uterus, urinary frequency, general physical discomfort (backache), heartburn, and leg cramps, in addition to hormonal fluctuations, are the main causes of sleep disturbances in the third trimester. Fetal movements, shortness of breath, vivid dreams/nightmares associated with labor/delivery, the health of the fetus, and pregnancy complications also contribute to disturbing sleep during the night during the third trimester. During childbirth, pain, anxiety, uterine contractions, long labor, and administration of medications all affect sleep and result in sleep loss and low sleep quality during labor and immediately after delivery. In summary, each trimester may lead to disrupting sleep. Pregnant women have more light sleep and less deep sleep (i.e., slow-wave sleep), owing to nocturnal awakenings [1, 4, 19, 20].
Pathogenetic mechanisms behind these associations have been postulated but remain to be proven [1, 4, 6, 19, 20]. The placenta has been proposed as a potential target organ in mediating adverse pregnancy outcomes in relation to sleep disturbances. For example, evidence of placental hypoxia and alterations in placenta-secreted markers have been shown in sleep disordered breathing (SDB) during pregnancy. It is biologically plausible that other sleep disturbances may affect placental function as well, given associations of sleep deprivation with similar placenta-mediated outcomes. The hypothalamic–pituitary–adrenal axis has been postulated to play a potential role in the association between SDB and gestational diabetes. Other potential mechanisms include an enhanced inflammatory profile, endothelial dysfunction, and oxidative stress but remain to be proven. The allostatic load hypothesis has also been proposed, suggesting that chronic sleep loss is both a precipitant of stress and a consequence of it and may lead to the “overload” of the stress system, which may account for adverse pregnancy outcomes. In summary, sleep is significantly disturbed in pregnancy, and sleep disruptions might have significant implications on perinatal health outcomes. Future research needs to focus on understanding the pathogenesis of these associations and examining the impact of sleep-targeted interventions on perinatal outcomes [1, 4, 6, 19, 20].
3 Pregnancy-Related Most Frequent Sleep Disturbances
3.1 Insomnia: Epidemiological and Clinical Characteristic During Peripartum
Chronic insomnia, also currently referred to as “insomnia disorder,” now has similar diagnostic criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [21] and in other sleep manuals. Insomnia disorder is now considered a 24-h sleep–wake disorder [21] characterized by nocturnal and diurnal symptoms. Insomnia can be episodic, lasting for a period within 1 month or between 1 month–3 months, or persistent, lasting longer than 3 months; transient-episodic forms tend, in the majority of the cases, to chronicity.
Insomnia is defined as difficulty initiating or maintaining sleep, early-morning awakening, or nonrestorative sleep associated with daytime consequences such as fatigue, irritability, and lack of concentration [21]. It is the most frequent sleep disturbance, affecting almost one-third of the general population [22, 23]. Frequency, severity, and pattern of insomnia can vary during pregnancy, with insomnia affecting >50% of pregnant women and reaching 80% during the third trimester. Insomnia symptoms increase in the first 6 months after childbirth with a total nocturnal sleep time of less than 6 h, and almost 10% of women develop an insomnia disorder in the long term [1, 4, 6, 19, 20].
The evolving models of chronic insomnia according to neurobiological, neurophysiological, cognitive, behavioral, or other perspectives [24] made the evaluation of insomnia progressively more complex. Although details of current models are beyond the scope of this chapter, concepts are critical for insomnia evaluation. The most heuristic model of insomnia is the diathesis-stress model, commonly known as the “3-P” model, describing predisposing, precipitating, and perpetuating factors relevant to the development and maintenance of insomnia (for an overview, see Palagini et al. 2020) [23]. Predisposing factors include genetic, physiological, or psychological diatheses that confer differential susceptibility to individuals in response to stress. Precipitating factors include physiological, environmental, or psychological stressors interacting with predisposing factors to produce acute symptoms. Perpetuating factors, especially behavioral, cognitive, and environmental factors, intervene in the perpetuation of insomnia. Hormonal and physical factors during pregnancy act as predisposing factors while maladaptive sleep behaviors and coping strategies such as napping, spending more time in bed, or increasing caffeine intake can perpetuate insomnia. Other risk factors for insomnia in pregnancy include age older than 30 years, nulliparity, single motherhood, preeclampsia or pregnancy-induced hypertension, prepregnancy affective disorders, perinatal depression, and environmental factors such as noise from other children or bed partners. Emotional distress related to pregnancy might be considered a precipitating factor per se, especially in the first trimester [1, 4, 6, 19, 20]. Weight gain and obesity contribute to sleep-onset or maintenance insomnia and SDB, favoring multiple awakenings during the night.
Decades of research into the cause of chronic insomnia have identified hyperarousal as a key factor [25] with increased levels of physiological, cognitive, and emotional levels of arousal in insomnia. The hyperarousal has been hypothesized to interact with unhelpful cognitive beliefs and negative behaviors contributing to the perpetuation of insomnia [26]. It is commonly seen in pregnancy as a higher body temperature and metabolic rate, with increased secretion of cortisol. The allostatic load hypothesis has been proposed and suggested that sleep loss is both a precipitant of stress as well as a consequence of it and by leading to a stress “overload” may account for adverse pregnancy outcomes, including peripartum psychopathology [4].
4 Evaluation of Insomnia During Peripartum
Insomnia evaluation needs a careful patient history and examination addressing sleep and waking functions as well as common medical, psychiatric, and medication/substance-related comorbidities. International guidelines suggest evaluating insomnia symptoms firstly using the Consensus Sleep Diary for at least 1/2 weeks to assess the insomnia day-to-day variability [23, 27]. In addition, the administration of questionnaires and survey instruments has been suggested to assess outcomes and guide treatment: the Insomnia Severity Index (ISI) [24] and the Epworth Sleepiness Scale (ESS) [28] are the questionnaires that have been suggested for the evaluation of insomnia and of its daytime consequences [23, 27]. The Insomnia Symptom Questionnaire was validated among pregnant women; therefore, it can be used as a reasonable screening tool for insomnia during pregnancy [29].
5 Management of Insomnia During Peripartum
Timely assessment and appropriate management are essential to prevent potential adverse pregnancy outcomes and the reoccurrence of chronic insomnia. It is of importance to know that many pregnant women do not seek treatment for insomnia because they either think it will naturally resolve after birth or wish to avoid medication owing to concerns about adverse effects on the fetus [20]. Therefore, it seems of utmost importance to clinically assess and manage sleep disruption from the beginning of pregnancy.
For chronic insomnia, cognitive behavioral therapy for insomnia (CBT-I) is the internationally considered first-line treatment [23, 30, 31]. Cognitive behavioral therapy for insomnia usually consists of behavioral strategies including psychoeducation/sleep hygiene, relaxation training, stimulus control therapy, sleep restriction therapy, and cognitive strategies such as sleep/related cognitive restructuring. In the context of CBT-I, psychoeducation typically includes the so-called “sleep hygiene rules” about health practices and environmental factors (e.g., light, noise, temperature) that may promote or disrupt sleep. Relaxation therapy is aimed at reducing somatic tension or intrusive thoughts at bedtime. Behavioral strategies include sleep restriction and stimulus control therapies; sleep restriction is a method designed to curtail the time in bed to the actual amount of sleep being achieved, and stimulus control therapy is a set of behavioral instructions designed to re-associate the bed/bedroom with sleep and to re-establish a consistent sleep–wake schedule. A recent systematic review pointed out a severe lack of knowledge on effective clinical interventions for insomnia during pregnancy [32]. The review selected 16 studies including in total 1252 expecting mothers. Four studies evaluated cognitive behavioral interventions for insomnia, one study pharmacotherapy, one study acupuncture, three studies mindfulness or yoga, five studies relaxation techniques, and two studies herbal medication. Of those, only six were randomized controlled trials. Although some preliminary support for clinically assessing insomnia during pregnancy is reported, the lack of evidence is severe. Specifically, preliminary support was evidenced for cognitive behavioral interventions for insomnia, which was also found to be the preferred therapy for pregnant women [33]. Furthermore, so far, no specific adaptation of the standard cognitive-behavioral therapy for insomnia protocol for pregnant women has been developed, but improving sleep hygiene, using relaxation, mindfulness techniques and yoga, and implementation of lifestyle modifications such as regular exercise have been used and suggested in pregnancy [32].
If nonpharmacologic therapies have failed for moderate insomnia during pregnancy, antihistamines like doxylamine or diphenhydramine (histamine H1 receptor antagonists) are categorized as possible but unlikely to harm the fetus. Based on animal and human studies, these drugs are not expected to be teratogenic. There are, however, some concerns with first-trimester use and minor birth defects. Breastfeeding is not recommended, but no reports of adverse effects exist in the medical literature [19, 20]. If a patient’s insomnia is more severe, then treatment with a sedating antidepressant or sedative-hypnotic may be considered. However, there are limited safety data on the sedative hypnotics during pregnancy. Zolpidem, with no known teratogenicity but with potentials of low birth weight and preterm delivery, need futher studies to be suggested. This drug is indeed considered safe in breastfeeding by the American Academy of Pediatrics [34]. Most other sedative hypnotics should be avoided or used with extreme caution in pregnancy. The available human data suggest no teratogenicity with zopiclone or eszopiclone, but there have been reports of withdrawal in infants after birth with chronic maternal use. Safety in breastfeeding has not been established. Sedating antidepressants such as tricyclic antidepressants (TCAs) might be better alternatives when patients have comorbid depression with insomnia. Based on case reports and on animal and human studies, the two antidepressants amitriptyline and trazodone are not expected to be teratogenic. Low-dose benzodiazepines (i.e., lorazepam) might also be considered if a patient also has issues with anxiety; however, caution must be used due to the potential risk for withdrawal and toxicity for the infant postpartum as well as an increased risk of cleft palate. For pregnant women with extreme sleep, mood, or anxiety symptoms, the benefits of using low-dose benzodiazepines may outweigh these reported concerns; however, the lowest effective dose should be prescribed to lower the risk of withdrawal and toxicity in infants postpartum [20]. Occasional use seems to be compatible with breastfeeding [34]. Finally, ramelteon, a melatonin receptor agonist, is associated with teratogenicity, but no human data on either pregnancy or breastfeeding are available [34]. Alternative therapies, herbal or dietary supplements, such as chamomile tea, lavender pillows, or acupuncture, are also used as sleep aids, but controlled studies are needed to assess the benefits and risks to fetal and maternal health [32].
6 Sleep Disordered Breathing (SDB): Epidemiological and Clinical Characteristic During Peripartum
Sleep disordered breathing (SDB) includes the spectrum of snoring, upper airway resistance syndrome and obstructive sleep apnea (OSA), and hypopnea syndrome. It is a breathing-related sleep disorder characterized by repeated episodes of apnea (cessation of breathing) or hypopnea (decrease in the flow of breathing accompanied by oxygen desaturation) secondary to obstruction of airflow in the upper airway [20]. The estimated prevalence in pregnant women has been reported to be higher than the general population, and it is reported to be between 10% and 25%. Normal physiological and hormonal changes in pregnancy, including weight gain, edema, and diaphragmatic displacement secondary to enlarging uterus, can contribute to breathing-related sleep difficulties. In addition, higher circulating levels of estrogen cause edema of mucous membranes, which can lead to nasal congestion and pharyngeal constriction, another cause of breathing-related sleep disorders. On the other hand, progesterone stimulates the ventilatory drive and increases the electromyographic activity of the upper airway dilator muscle. Progesterone’s stimulating properties enhance the responsiveness of the upper airway dilator muscles to chemical stimuli during sleep. This effect of progesterone theoretically protects against the development of SDB. Sleeping in the lateral position and the reduction in the time spent in REM sleep in late pregnancy are both protective against apneic and hypopneic events [19, 20].
7 Evaluation of SDB During Peripartum
Clinical manifestations of SDB during pregnancy include snoring and symptoms of daytime hypersomnolence, which can be evaluated with the Epworth Sleepiness Scale (ESS). A score of >10 is indicative of pathological hypersomnolence. SDB during pregnancy represents a risk factor for adverse pregnancy outcomes [6]. Therefore, it is of particular importance to evaluate and treat SDB during pregnancy.
8 Management of SDB in Pregnancy
Although no recommendations exist for the pregnant population specifically, it has been considered reasonable to follow those same guidelines in pregnancy [19, 20].
The decision to treat pregnant women with SDB should probably be made the same way as in the nonpregnant population [19, 20]. A particular concern regards fetal well-being in women with recurrent episodes of intermittent apnea and potential intermittent desaturations and hypoventilation. Continuous positive airway pressure (CPAP) is the preferred method of treatment of SDB in the general population and helps treat over 90% of patients with OSA. Although there is a theoretical concern regarding an increased risk of aspiration in pregnancy with the use of CPAP, it has been shown to be well tolerated in pregnancy and does not seem to be associated with a higher risk of complications in this population [19, 20]. CPAP pressures may have to be titrated during the course of pregnancy because of weight gain, but the required increase in pressures may only be 1–2 cm. CPAP therapy has been shown to improve hemodynamic parameters nocturnal cardiac output on the treatment night in patients with preeclampsia. Although the studies mentioned above involve only a small number of subjects, they are supportive of a potential hemodynamic benefit to the use of CPAP therapy in patients with preeclampsia. Other therapies for OSAs include oral appliances that have a well-documented benefit in eliminating apneas in patients with mild to moderate disease. The effect of this therapy on patients with severe disease is less well documented. Although not all sleep apnea cases will resolve postpartum, those that do persist in the postpartum period may need a different CPAP prescription following weight loss. Given that a supine position could worsen OSA in about half of the general population, lateral-recumbent or head-elevated positions are recommended. It is possible that pregnant patients may also have position-dependent OSA, so positional therapy could be an alternative that is less invasive than CPAP. Positional therapy includes wearing something around one’s waist or back (i.e., tennis balls or foam in a backpack or fanny pack) as well as newer devices, such as sleep-position trainers, that incorporate vibrations while a patient is in a supine position that continues until the patient changes position [19, 20].
9 Restless Legs Syndrome (RLS): Epidemiological and Clinical Characteristics During Peripartum
Restless legs syndrome (RLS) is characterized by an unpleasant leg sensation that causes an almost irresistible urge to move the legs [21]. A diagnosis of RLS is established when four clinical features are present: (1) the urge to move the legs; (2) the urge is worse when the patient is sedentary; (3) the abnormal sensation in the legs or the urge to move improves or resolves when the movement of the legs occurs; and (4) the symptoms have a circadian pattern and get worse during the evening or night [19, 20].
RLS occurs more frequently in pregnancy than in the general population and is reported in as many as 27% of pregnant women. RLS is considered a dysfunction of dopamine within the nigrostriatal circuit, but when RLS is associated with pregnancy, this syndrome is related to iron deficiency anemia, folate deficiency, advanced renal disease, and peripheral neuropathy. Other theories in pregnancy include iron deficiency and dopamine insufficiency as well as hormonal causes related to progesterone and prolactin. RLS is often under-diagnosed during pregnancy also because symptoms can be similar to leg cramps that are quite common in pregnancy. Untreated RLS increases the risk of depressed mood, and RLS-related sleep deprivation is linked to adverse effects like prolonged labor, heightened pain perception and discomfort during labor, higher rates of C-section, preterm labor, and elevated inflammatory cytokine. Therefore, it is of importance to evaluate RLS during pregnancy [19, 20].
10 Evaluation of RLS During Peripartum
A sleep history that includes the diagnostic criteria of RLS can help with an accurate diagnosis. History of RLS in a previous pregnancy and in the nonpregnant state, family history, multiparity, anemia, low folate level, low iron level, and high estrogen level are associated with an increased risk of RLS during pregnancy [20]. Specific questionnaires may help in the diagnosis such as the Restless Legs Syndrome Rating Scale that was developed by the International Restless Legs Syndrome Study Group (IRLSSG) to assess the severity of a patient’s RLS symptoms [35]. It consists of 10 questions and has been commonly used to assess RLS in pregnant women.
11 Management of RLS During Peripartum
First, managing the symptoms of RLS should begin with a nonpharmacological approach, including mental alerting activities, abstinence from caffeine, and removal of drugs known to aggravate RLS such as antidepressants, neuroleptics, anti-emetics, and sedating antihistamines. If the above approach does not reduce the symptoms of RLS, then a pharmacological approach should be considered for further management. When treating RLS during pregnancy, the physician must consider the effect of medication on the fetus, especially the possibility of congenital malformations. Controlled studies of RLS during pregnancy have been limited. As a result, most evidence of therapeutic results come from reported cases or small case series. The medications that were studied include iron supplementation, dopaminergic agents, benzodiazepines, opioids, and anti-epileptic agents [19, 20].
Treatment of RLS in pregnancy aims at identifying iron or folate deficiency and replenishing the stores. Although the mainstay of therapy for this syndrome is monotherapy with levodopa and dopaminergic agents, levodopa has been associated with adverse pregnancy outcomes in experimental animals after high-dose treatment. Safety in human pregnancies has not been established, despite case reports in humans describing no evidence of abnormal embryological or fetal development [19, 20].
There are no data to support the safety of pramipexole or ropinirole use in pregnancy. Benzodiazepine, in particular clonazepam, may potentially be used to treat RLS during pregnancy as adjunct treatment, and there is no evidence that it causes an increased rate of major malformations; however, the incidence of minor congenital malformations including cleft lip and palate is more frequent with benzodiazepine use. Due to the risks of congenital malformations and neonatal abstinence syndrome, opioids should be avoided for treating the symptoms of RLS during pregnancy if possible. Anti-epileptic agents should be considered the last choice for treating RLS during pregnancy. Gabapentin, carbamazepine, and oxcarbazepine may be reasonable choices due to their lower rates of teratogenicity [19, 20].
12 Nightmare and Bad Dreams During Peripartum
Women during their first pregnancy experience frequently pregnancy-related dreams [36]. An higher frequency of disturbing dreams has been described in pregnant women compared to nonpregnant women. Research indicated that pregnancy-related worries like loss, danger to the fetus/baby, or giving birth to a deformed baby also occurred in dreams during pregnancy. The number of these negatively toned dreams correlated with daytime depressive mood and trait anxiety; i.e., the dreams including pregnancy-related worries also reflect the daytime worries of pregnant women. Nightmares are defined as well-remembered dreams that usually involve a threat to survival, security, or physical integrity and, thus, represent an extreme form of negatively toned dreams. About 40–50% of pregnant women experience nightmares, at least about 6–10% of pregnant women reported severe nightmares related to fear of childbirth with dream recall higher than once per week. The findings clearly indicated a heightened nightmare frequency in pregnant women in their last trimester. If a substantial number of pregnant women suffer from nightmare disorders, it would be very interesting to learn whether short-term interventions like imagery rehearsal therapy, which have been shown to be very effective in different samples, are also beneficial for pregnant women with nightmares. Imagery rehearsal therapy is based on principles of cognitive therapy and encompasses three steps: confrontation (recording the dream), coping (imagining a new, more satisfying dream ending), and rehearsal (imagining the new coping strategy once a day for 5–10 min over 2 weeks) [36].
References
Baglioni C, Tang NK, Johann AF, Altena E, Bramante A, Riemann D, et al. Insomnia and poor sleep quality during peripartum: a family issue with potential long term consequences on mental health. J Matern Fetal Neonatal Med. 2020;2:1–9. https://doi.org/10.1080/14767058.2020.1854718.
Palagini L, Bruno RM, Gemignani A, Baglioni C, Ghiadoni L, Riemann D. Sleep loss and hypertension: a systematic review. Curr Pharm Des. 2013;19(13):2409–19. https://doi.org/10.2174/1381612811319130009.
Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. 2019;43:96–105. https://doi.org/10.1016/j.smrv.2018.10.006.
Palagini L, Gemignani A, Banti S, Manconi M, Mauri M, Riemann D. Chronic sleep loss during pregnancy as a determinant of stress: impact on pregnancy outcome. Sleep Med. 2014;15(8):853–9. https://doi.org/10.1016/j.sleep.2014.02.013.
Mindell JA, Cook RA, Nikolovski J. Sleep patterns and sleep disturbances across pregnancy. Sleep Med. 2015;16(4):483–8. https://doi.org/10.1016/j.sleep.2014.12.006.
Pengo MF, Won CH, Bourjeily G. Sleep in women across the life span. Chest. 2018;154(1):196–206. https://doi.org/10.1016/j.chest.2018.04.005.
Garbazza C, Hackethal S, Riccardi S, Cajochen C, Cicolin A, D’Agostino A, et al. Polysomnographic features of pregnancy: a systematic review. Sleep Med Rev. 2020;50:101249. https://doi.org/10.1016/j.smrv.2019.101249.
Meltzer LJ, Montgomery-Downs HE. Sleep in the family. Pediatr Clin N Am. 2011;58(3):765–74. https://doi.org/10.1016/j.pcl.2011.03.010.
Okun ML, Schetter CD, Glynn LM. Glynn LM. Poor sleep quality is associated with preterm birth. Sleep 2011;34(11):1493–1498. doi: https://doi.org/10.5665/sleep.1384.
Paine SJ, Signal TL, Sweeney B, Priston M, Muller D, Smith A, et al. Maternal sleep disturbances in late pregnancy and the association with emergency caesarean section: a prospective cohort study. Sleep Health. 2020;6(1):65–70. https://doi.org/10.1016/j.sleh.2019.11.004.
Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. https://doi.org/10.1016/j.smrv.2015.10.002.
Tomfohr LM, Buliga E, Letourneau NL, Campbell TS, Giesbrecht GF. Trajectories of sleep quality and associations with mood during the perinatal period. Sleep. 2015;38(8):1237–45. https://doi.org/10.5665/sleep.4900.
Emamian F, Khazaie H, Okun ML, Tahmasian M, Sepehry AA. Link between insomnia and perinatal depressive symptoms: a metaanalysis. J Sleep Res. 2019;28(6):e12858. https://doi.org/10.1111/jsr.12858.
Ross LE, Murray BJ, Steiner M. Sleep and perinatal mood disorders: a critical review. J Psychiatry Neurosci. 2005;30(4):247–56.
Sharma V, Mazmanian D. Sleep loss and postpartum psychosis. Bipolar Disord. 2003;5:98–105. https://doi.org/10.1034/j.1399-5618.2003.00015.x.
Palagini L, Cipollone G, Masci I, Novi M, Caruso D, Kalmbach DA, et al. Stress-related sleep reactivity is associated with insomnia, psychopathology and suicidality in pregnant women: preliminary results. Sleep Med. 2019;56:145–50. https://doi.org/10.1016/j.sleep.2019.01.009.
Kalmbach DA, Cheng P, Ong JC, Ciesla JA, Kingsberg SA, Sangha R, et al. Depression and suicidal ideation in pregnancy: exploring relationships with insomnia, short sleep, and nocturnal rumination. Sleep Med. 2020;65:62–73. https://doi.org/10.1016/j.sleep.2019.07.010.
Mindell JA, Leichman ES, DuMond C, Sadeh A. Sleep and social-emotional development in infants and toddlers. J Clin Child Adolesc Psychol. 2017;46(2):236–46. https://doi.org/10.1080/15374416.2016.1188701.
Izci-Balserak B, Lee KA. Sleep and sleep disorders associated with pregnancy. In: Kryger M, Roth T, Dement W, editors. Principles and practice of sleep medicine. 6th ed. Philadelphia, PA: Saunders; 2017. p. 1525–39.
Kay-Stacey M, Attarian HP. Managing sleep disorders during pregnancy. Gender Genome. 2017;1:34–45. https://doi.org/10.1089/gg.2016.0006.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Arlington, VA: American Psychiatric Publishing; 2013.
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26:675–700. https://doi.org/10.1111/jsr.12594.
Palagini L, Manni R, Aguglia E, Amore M, Brugnoli R, Girardi P, et al. Expert opinions and consensus recommendations for the evaluation and management of insomnia in clinical practice: joint statements of five Italian scientific societies. Front Psychiatry. 2020;11:558. https://doi.org/10.3389/fpsyt.2020.00558.
Morin CM. Insomnia: psychological assessment and management. New York: Guilford Press; 1993.
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31. https://doi.org/10.1016/j.smrv.2009.04.002.
Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14(5):547–58. https://doi.org/10.1016/S1474-4422(15)00021-6.
Carney CE, Buysse DJ, Ancoli-Israel S, Edinger J, Krystal AD, Lichstein KL, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35:287–302. https://doi.org/10.5665/sleep.1642.
Johns MW. A new method of measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540. https://doi.org/10.1093/sleep/14.6.540.
Okun ML, Kravitz HM, Sowers MF, Moul DE, Buysse DJ, Hall M. Psychometric evaluation of the insomnia symptom questionnaire: a self-report measure to identify chronic insomnia. J Clin Sleep Med. 2009;5:41–51.
Baglioni C, Altena E, Bjorvatn B, Blom K, Bothelius K, Devoto A, et al. The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29(2):e12967. https://doi.org/10.1111/jsr.12967.
Baglioni C, Bostanova Z, Bacaro V, Benz F, Hertenstein E, Spiegelhalder K, et al. A systematic review and network meta-analysis of randomized controlled trials evaluating the evidence base of melatonin, light exposure, exercise, and complementary and alternative medicine for patients with insomnia disorder. J Clin Med. 2020;9(6):1949. https://doi.org/10.3390/jcm9061949.
Bacaro V, Benz F, Pappaccogli A, De Bartolo P, Johann AF, Palagini L, et al. Interventions for sleep problems during pregnancy: a systematic review. Sleep Med Rev. 2020;50:101234. https://doi.org/10.1016/j.smrv.2019.101234.
Sedov ID, Goodman SH, Tomfohr-Madsen LM. Insomnia treatment preferences during pregnancy. J Obstet Gynecol Neonat Nurs. 2017;46(3):e95–e104. https://doi.org/10.1016/j.jogn.2017.01.005.
Oyiengo D, Louis M, Hott B, Bourjeily G. Sleep disorders in pregnancy. Clin Chest Med. 2014;35:571–87. https://doi.org/10.1016/j.ccm.2014.06.012.
The International Restless Legs Syndrome Study Group. Validation of the international restless legs syndrome study group rating scale for restless legs syndrome. Sleep Med. 2003;4(2):121–32. https://doi.org/10.1016/s1389-9457(02)00258-7.
Schredl M, Gilles M, Wolf I, Peus V, Scharnholz B, Sütterlin M, et al. Nightmare frequency in last trimester of pregnancy. BMC Pregnancy Childbirth. 2016;16(1):346. https://doi.org/10.1186/s12884-016-1147-x.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Palagini, L., Massa, L., Riemann, D. (2022). Sleep Disorders and Peripartum. In: Percudani, M., Bramante, A., Brenna, V., Pariante, C. (eds) Key Topics in Perinatal Mental Health. Springer, Cham. https://doi.org/10.1007/978-3-030-91832-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-91832-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91831-6
Online ISBN: 978-3-030-91832-3
eBook Packages: MedicineMedicine (R0)