Abstract
The early detection of the clinical expressions of septic arthritis is fundamental to start adequate therapeutic interventions before the development of irreversible articular and tendinous damage. In this perspective, imaging techniques and particularly ultrasound (US) are important tools to demonstrate the joint and musculoskeletal damage, and to help in the diagnosis and follow-up of the disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In general, infectious arthritis is classified as pyogenic (septic) or nonpyogenic. Septic arthritis is a serious type of joint infection and may represent a direct invasion of joint space by various microorganisms, most commonly caused by bacteria. Nonpyogenic infective arthritis tends to be less aggressive and has a more chronic course, with causative organisms including Mycobacterium tuberculosis, fungi, viruses, and spirochetes.
Arthritis can develop indirectly as a result of hematogenous seeding or extension from a contiguous focus of infection. Bacterial arthritis can also arise following direct introduction, can be accidental from penetrating trauma (also from human or animal bite or from a fingernail wound), or can be iatrogenic by intra-articular injection. Joint surgery has increasingly been a source of bacterial arthritis, particularly following knee and hip arthroplasty.
Septic arthritis can be theoretically caused by any bacterium; however the most common etiological agent of all septic arthritis cases is Staphylococcus aureus, which causes a destructive form of acute arthritis, representing a real medical emergency. Patients with a history of intravenous drug abuse, elderly, or immunocompromised people display a higher prevalence of infection by gram-negative organisms. The most common gram-negative organisms are Pseudomonas aeruginosa and Escherichia coli.
Infants and older adults are more likely to develop septic arthritis. The knees are most commonly affected, but septic arthritis can also affect the hips, shoulders, and other joints. Typically, septic arthritis affects one large joint, such as the knee or hip, and only one. Less frequently, septic arthritis can affect multiple joints simultaneously.
The infection can quickly and severely injure the cartilage and bone within the joint, so prompt diagnosis and antibiotic treatment are crucial, also to prevent permanent damage to the joint. An acute onset of monoarticular joint pain, joint swelling by effusion, erythema, heat, and impaired range of movement, with fever and chills, should raise suspicion of sepsis. Clinical evaluation, laboratory workup, and joint fluid aspiration are the primary means of diagnosing septic arthritis. The role of imaging is to confirm the diagnosis and establish the presence and severity of joint damage.
2 Diagnostic Imaging
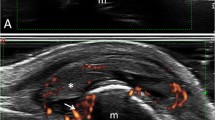
Conventional radiograph still remains as the initial imaging approach, but it has low sensitivity and specificity for acute infection. In early stages the simple radiograph can be normal and this does not rule out infection. With further development of the conditions, the typical radiological picture shows severe osteoporosis, destruction of joint cartilages with joint space narrowing, and serious damage to bones. Therefore, X-ray allows to identify late stages of the disease, when bone tissue is already damaged, and it is no more useful for therapeutic decision-making. Early recognition of the presence of intra-articular effusion in affected joint is the primary objective of diagnostic imaging, because the absence of a joint effusion essentially excludes septic arthritis. Both ultrasound and MRI can detect a joint effusion; however ultrasound is preferred for its accessibility and patient acceptance. However MRI and bone scintigraphy may be warranted to rule out adjacent osteomyelitis. Therefore, when the diagnosis of septic arthritis is presumed, ultrasonography may be mostly beneficial not only for a diagnostic confirmation, but also for simultaneous, ultrasound-guided arthrocentesis with aspiration of the purulent effusion. Ultrasonography is more sensitive for detecting effusions, particularly in challenging joints, such as the hip. This ability is especially useful in the early diagnosis of newborn septic arthritis, because of the frequent paucity of clinical signs and symptoms in these patients. Usually, when a joint effusion is found, sonography alone cannot distinguish with certainty between septic arthritis and other types of synovitis. In fact, septic arthritis demonstrates great variability in ultrasound presentation, depending on the patient age, etiological agent, evolutionary stage, and affected joint. The ultrasound appearance can range from mild echogenic articular effusion to joint destruction (Figs. 17.1 and 17.2a–e).
Long-standing rheumatoid arthritis and osteomyelitis. Hot and swollen ankle for 4 weeks in a 68-year-old male, who underwent ankle arthrodesis 5 years before. Conventional radiography (a, b). Images acquired using different projections. The arrows and the arrowheads indicate the parts of the screw displayed in the ultrasound images. Radiographic detail (c): note soft-tissue swelling around the tibia (empty arrows), related to septic infiltrate. Ultrasound (d, e). Note the septic fluid collection (*) surrounding both screw extremities [i.e., the head (arrow) and the tip (arrowhead)] and appearing as an inhomogeneous area characterized by hyperechoic spots of different size and shape distributed in a less echogenic fluid material. t tibia, tp tibialis posterior tendon (Images courtesy of MD Cipolletta E, Ancona)
In pediatric age, septic arthritis is relatively frequent, most commonly involving the hip joint, and can have potentially serious consequences, being considered a medical emergency. Prompt diagnosis is of paramount importance to avoid a disastrous outcome, which can lead to joint destruction when the therapy is delayed or inadequate. A classic clinical presentation of septic arthritis is a sudden onset of the pain and joint discomfort (frequently at hip), and the presence of Kocher criteria (non-weight-bearing status on the affected side; fever >38.5°; erythrocyte sedimentation rate (ESR) >40 mm/h; increase in serum white blood cell (WBC) count >12,000/mm3). But sometimes distinguishing septic arthritis from transient synovitis or other types of arthritis of the hip in a limping child could be challenging. In fact, in the early stage of disease their clinical presentation could be similar but treatment and prognosis are very different. In these cases, although they are unable to provide diagnostic certainty, some echographic features may help to distinguish septic arthritis from other different types. For example, the echogenicity of exudate is usually anechoic and homogeneous in transient arthritis while in septic arthritis it often shows a cloudy and inhomogeneous aspect (Figs. 17.3a, b, and 17.4a–c). Synovium thickening is generally present in juvenile idiopathic arthritis (for hypertrophy), moderate in septic arthritis (for edema), and minimally evident or absent in transient arthritis. As a rule, synovial hyperemia is present at power Doppler evaluation in septic arthritis and juvenile idiopathic arthritis, while it is generally least or absent in transient arthritis.
(a, b) Septic arthritis of the hip in a limping 3-year-old child with mild hip pain. (a) Longitudinal US scan reveals a small effusion with inhomogeneous echogenicity and synovial thickening. Metaphyseal bone erosion is present (large white arrow). (b) X-ray in the same patient confirms the soft-tissue swelling around the involved joint, suggestive of effusion (empty white arrows) and bone erosion (small white arrow)
(a–c) Transient synovitis in a 5-year-old child with similar clinical presentation to that of the patient in Fig. 17.2. (a) Frontal radiograph shows capsular swelling (empty white arrows). (b) US detects increased capsule-to-bone distance (calipers) related to joint effusion and to synovial thickening (*). (c) Power Doppler US demonstrates absence of intrasynovial increased flow
However, we must remember that septic arthritis is a great mimic. Therefore, even if the echographic evaluation reveals a monoarticular and homogeneously anechoic effusion, and a minimal synovial thickening without hypervascularity, arthrocentesis is still mandatory if the clinical and laboratory results evoke septic involvement. Conversely, septic arthritis must always be excluded even in situations where the clinical presentation is atypical. In this way, sonography can play a useful role in differential diagnosis. In doubt, a precise and unmistakable diagnosis is only possible through arthrocentesis and isolation of the bacterium.
Further Readings
Chin TWY, Tse KS. Clinical and radiological differentiation of septic arthritis and transient synovitis of the hip. Hong Kong J Radiol. 2017;20:41–6.
Goldenberg DL. Septic arthritis. Lancet. 1998;351:197–202.
Gordon JE, Huang M, Dobbs M, et al. Causes of false-negative ultrasound scans in the diagnosis of septic arthritis of the hip in children. J Pediatr Orthop. 2002;22:312–6.
Marchal GJ, Van Holsbeeck MT, Raes M, et al. Transient synovitis of the hip in children: role of US. Radiology. 1987;162:825–8.
Martino F, Silvestri E, Grassi W, Garlaschi G. Musculoskeletal sonography. Springer: Milan, Berlin, Heidelberg, New York; 2006.
Merino R, de Inocencio J, Garcia-Consuegra J. Differentiation between transient synovitis of the hip with clinical and ultrasound criteria. An Pediatr (Barc). 2010;73(4):189–93.
Nguyen A, Kan JH, Bisset G, Rosenfeld S. Kocher criteria revisited in the era of MRI: how often does the Kocher criteria identify underlying osteomyelitis? J Pediatr Orthop. 2017;37(2):e114–9.
Ryan MJ, Kavanagh R, Wall PG, Hazleman BL. Bacterial joint infections in England and Wales: analysis of bacterial isolates over a four year period. Br J Rheumatol. 1997;36:370–3.
Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002;15(4):527–44.
Strouse PJ, DiPietro MA, Adler RS. Pediatric hip effusions: evaluation with power Doppler sonography. Radiology. 1998;206:731–5.
Taylor-Robinson D, Keat A. Septic and aseptic arthritis: a continuum? Baillieres Best Pract Res Clin Rheumatol. 1999;13:179–92.
Zamzam MM. The role of ultrasound in differentiating septic arthritis from transient synovitis of the hip in children. J Pediatr Orthop. 2006;15:418–22.
Zieger MM, Dörr U, Schulz RD. Ultrasonography of hip joint effusions. Skelet Radiol. 1987;16:607–11.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Muda, A., Martino, F. (2022). Septic Arthritis. In: Martino, F., Silvestri, E., Orlandi, D. (eds) Musculoskeletal Ultrasound in Orthopedic and Rheumatic disease in Adults. Springer, Cham. https://doi.org/10.1007/978-3-030-91202-4_17
Download citation
DOI: https://doi.org/10.1007/978-3-030-91202-4_17
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91201-7
Online ISBN: 978-3-030-91202-4
eBook Packages: MedicineMedicine (R0)