Abstract
Anesthesia machine provides control of patient’s gas exchange. Anesthesia machine reduces the pressure of desired gases to a safe level. The anesthesia machine can be divided into three parts as high, intermediate, and low pressure systems. The high pressure system includes cylinders and pressure regulators. The intermediate pressure system starts from pressure regulators and continues to the flow control valves. The low pressure system contains the flowmeter tubes, vaporizers, unidirectional valves, and components up to the common gas outlet. Modern anesthesia machines have many safety equipment to minimize the risk of hypoxic gas mixture. Vaporizers are the devices which convert liquid anesthetics into vapor and deliver volatile anesthetics to the breathing circuit. Sodalyme and barolyme are the most commonly used absorbents to eliminate CO2. Ventilators are classified as single-circuit and double-circuit systems according to the movement mechanism. Modern ventilators are timed and electronically controlled. Breathing systems are classified as open, semi-open, semi-closed, and closed systems. There is no anesthetic gas reservoir balloon in open systems. It is used with insufflation by open drop or mask method. Semi-open systems are flow-controlled, valve-free, and non-rebreathing systems. There are types as Mapleson A, B, C, D, E, and F. Semi-closed breathing systems are the most commonly used breathing system in adults and older children. In closed systems, the entire volume of expiratory gas returns to the patient after CO2 is absorbed. Today, modern devices with increased safety are used for different patient types.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Anesthesia machine provides the control of patient’s gas exchange. In addition, anesthesia maintenance is carried out by applying inhalation anesthetics. Morton identified ether in 1846. In 1912, Gwathwey described continue flow anesthetic machine. Then, Boyle modification was reported in 1917. Anesthesia machine reduces the pressure of desired gases to a safe level. Volatile anesthetics are vaporized into the final gas mixture. It controls the flow of oxygen and nitrous oxide. Positive pressure ventilation is provided by anesthesia machine. The risk of delivering hypoxic gas mixture to a patient is avoided.
8.2 Basic Components of Anesthesia Machine (Figs. 8.1 and 8.2)
-
Gas supply.
-
Flowmeter.
-
Vaporizers.
-
Breathing circuits.
-
Ventilator.
-
Scavenging System.
-
Monitors.
The anesthesia machine can be divided into three parts as high, intermediate, and low pressure systems. The high pressure system includes cylinders and pressure regulators. Oxygen pressure is kept between 2200 and 45 psig. Nitrous oxide (N2O) pressure ranges from 750 to 45 psig. The high pressure system provides more constant and proper gas transport to the flowmeter.
The intermediate pressure system starts from pressure regulators and continues to the flow control valves. The pressure of gas supplied from cylinder to the anesthesia machine is 45 psig, while the approximate pipeline pressure is about 50–55 psig. The anesthesia machine receives medical gases from piping network and cylinders. The cylinders are generally used as a back-up supply in case of pipeline failure.
8.2.1 Oxygen Flush Valve
It is located in the intermediate pressure system with 45–60 psig pressure. It allows the delivery of 35–75 L/min of 100% oxygen flow to breathing circuit. Malfunction of oxygen flush valve may result in barotrauma or awareness during anesthesia. It dilutes the anesthetic agent concentrations.
The hose attachment to the anesthesia machine is specific for each supplied gas. Connectors have safety features such as non-interchangeable screw thread (NIST). Moreover, there are different universal colored flexible hoses for each gas to prevent incorrect connection.
The low pressure system contains the flowmeter tubes, vaporizers, unidirectional valves, and components up to the common gas outlet. The low pressure section is the section distal to the flow control valves. Flowmeter and flow control valves separate intermediate and low pressure systems. Flowmeter regulates the amount of gas that will pass into the low pressure system.
The unidirectional valves prevent gas flow back to the vaporizer during positive pressure ventilation. The tubes have an antistatic coating on both surfaces, preventing the effect of static electricity. There could be electronic flowmeters in the low pressure system as well. There are electronic flowmeters in modern anesthesia machines. In these machines, the data are displayed graphically or numerically on the screen.
8.2.2 Fail-Safe Systems
Fail-safe systems prevent the delivery of a hypoxic mixture of gas to the patient. These systems include pneumatic and electronic alarm devices. When the oxygen pressure drops below a limit set by the manufacturer, it gives an alarm within 5 seconds. This is called 2000 ASTM F1850–00 standard. In addition, the oxygen concentration in the common gas outlet should not be below 19%. Modern anesthesia machines have many safety equipment. The aim is to minimize the risk of hypoxic gas mixture. Fail-safe system is present in all gas lines except oxygen. When oxygen pressure drops, other gases are either completely shut down or their ratio is reduced in proportion to oxygen. Datex-Ohmeda machines feature pressure sensor shut off valve. It works on the off-or-on principle. North American Drager machines have oxygen failure protection device (OFPD), which shuts off nitrous oxide or allows its proportional flow.
8.2.3 Safety Systems to Prevent Hypoxic Gas Mixture
There is oxygen/nitrous oxide ratio controller in Datex-Ohmeda Link 25 system. The oxygen gear is connected to nitrous oxide gear. When oxygen flow decreases, nitrous oxide flow is directly reduced. This arrangement helps to ensure a minimum oxygen concentration of 25%. The disadvantage of proportional systems is that their sensors are not oxygen specific. This poses a risk of incorrect gas connections. Therefore; it is necessary to use an oxygen analyzer.
8.2.4 Causes of Flowmeter Malfunction
-
They could provide wrong measurements because of debris in the flow tube, static electricity or sticking inside the tube.
-
Scales may be mixed.
8.2.5 Vaporizers
Vaporizers are the devices which convert liquid anesthetics into vapor and deliver volatile anesthetics to the breathing circuit. Vapor pressure is not affected by atmospheric pressure; it only depends on the characteristics of the volatile agent and the temperature. A liquid’s boiling point is the temperature at which its vapor pressure is equal to the atmospheric pressure. Boiling points at 760 mmHg are 22.5 for desflurane, 48.5 for isoflurane, 50.2 for halothane, 56.5 for enflurane, and 58.5 for sevoflurane. All modern vaporizers are agent specific. They are capable of delivering a constant concentration of the agent regardless of temperature changes or flow through the vaporizer.
Electrically heated special vaporizers must be utilized for desflurane because it boils at room temperature. According to the working principle of agent-specific variable by-pass vaporizers, anesthetic gas mixture passes through the vaporizing chamber. The gas flow directed to the vaporizing chamber is saturated with liquid anesthetic agent. These vaporizers are agent specific. In flow over vaporizers, the carrier gas passes over the inhalation agent in vaporizing chamber.
8.2.6 Factors Affecting the Vaporizer Output
Flow rate, temperature and characteristics of the volatile agent affect on vaporizer output. The characteristics of the carrier gas are also effective.
8.2.7 Points to Pay Attention in Vaporizers
-
Filling vaporizers with the incorrect anesthetics.
-
Contamination.
-
Excessive tilting of vaporizers.
-
Overfilling.
-
Insufficient filling.
-
Filling with multiple agents.
-
Leaks.
8.3 Carbon Dioxide (CO2) Elimination
The exhaled CO2 is chemically bound with granules consisting of alkaline metal and earth metal hydroxides. Sodalyme and barolyme are the most commonly used absorbents. 100 g sodalyme absorbs 26 L CO2. On the other hand, 100 g barolyme absorbs 18 L of CO2. When the color change reaches 60–70%, the absorbent is replaced (Table 8.1).
When sodalyme and sevoflurane are combined, Compound A and formaldehyde are formed. Carbon monoxide formation increases with desflurane. New absorbents significantly reduce Compound A formation with Sevoflurane use. Spherasorb does not contain KOH and Amsorb does not contain NaOH and KOH.
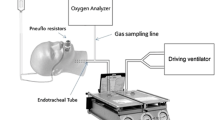
8.3.1 Ventilators
Ventilators are classified as single-circuit and double-circuit systems according to the movement mechanism. Modern ventilators are timed and electronically controlled. In a double-circuit ventilator, the driving gas activates the pneumatic system that pushes the bellows. Oxygen or a mixture of oxygen and air are used as pressurized gas. Single-circuit ventilators have special electrically driven motors. They can work more precisely and computer-controlled. This type of ventilator requires no driving gas. An ascending bellows is safer. When the fresh gas flow is cut off, the ascending bellow will collapse; it prevents breathing of hypoxic gas mixture.
8.3.2 Ventilation Modes
In order to provide optimum mechanical ventilation, the pressure, volume, and flow parameters on the ventilator should be adjusted in accordance with the patient’s respiratory system. Modes of mechanical ventilation can be classified according to the control of tidal volume. In this regard, volume controlled and pressure controlled modes are available. Volume controlled modes include Continuous mandatory ventilation (VC-CMV), Synchronized intermittent mandatory ventilation (VC-SIMV), and Autoflow. On the other side pressure controlled modes are Continuous mandatory ventilation (PC-CMV), Synchronized intermittent mandatory ventilation (PC-SIMV), Pressure control with volume guarantee (PC-CMV-VG), Pressure support ventilation (PC-PSV), Biphasic positive airway pressure (PC-BIPAP), and Airway Pressure Release Ventilation (PC-APRV). In VC-CMV, there is a constant flow. Peak inspiratory pressure varies according to lung mechanics. In both VC-SIMV and PC-SIMV, the mandatory breaths are synchronized with the patients’ breathing effort.
8.3.3 Scavenging System
It consists of two parts: active and passive. In the passive system, gases are discharged with their own pressure. The positive pressure valve is sufficient. In the active system, there is a connection to the hospital’s vacuum system. The negative pressure reducing valve protects against the negative pressure of the vacuum system. The positive pressure reducing valve protects against the positive pressure caused by clogged replaceable hoses.
The scavenging system extends the anesthesia circuit. Obstruction in the circuit may occur. In case of obstruction, excessive positive pressure is applied to the respiratory tract, which may cause barotrauma.
8.3.4 Alarm Systems in Anesthesia Machine
There are several safety features in anesthesia machines. These are connected with alarm systems. Oxygen pressure failure system works as a standard to activate an audible alarm when oxygen pressure falls below a safe threshold. The oxygen failure safety system detects failure on pressure and provides an alarm to warn the low level of oxygen. Integral monitor alarms are other types for patient safety.
8.3.5 Monitors of Anesthesia Machine
The monitors provide valuable information about ventilation, oxygenation, hemodynamic parameters, and temperature. Ventilation monitoring includes pulse oximeter, end tidal carbon dioxide measurement, and respiratory rate analysis. Electrocardiogram (ECG), non-invasive and invasive blood pressure monitoring give information about circulation.
8.4 Anesthesia Machine Calibration and Checklist
8.4.1 Anesthesia Machine Calibration
Today, modern anesthesia machines are different than simple pneumatic devices. Anesthesia workstation is consist of vital electrical, electronic, and mechanical components such as computer equipped microprocessors. Therefore, their complex structure makes the calibration, maintenance, and cleaning more complicated. The calibration includes the physical and electrical components of workstation, oxygen supply and the monitor, flowmeters, ventilators vaporizers, and panel connectors. The calibration of oxygen sensor should be performed with both 21% and 100% oxygen. The control of anesthesia device and related equipment should include routine maintenance and calibrations by authorized services. Weekly maintenance and daily checks should be performed by nurse anesthetists or anesthesiologists. It is mostly applied as checklists and should be checked at appropriate time intervals.
8.4.2 Checklist
The American Society of Anesthesiologists (ASA) issued a pre-anesthetic checkout procedure in 2008 as a guide. The items are presented in Table 8.2.
8.4.3 Checking the Oxygen Cylinder
Oxygen can be dangerous if not used correctly. Therefore, the check of the cylinder has a vital importance for both patients and health care workers. As oxygen may cause explotion and burns, the safety guidelines should be followed. First, the pressure gauge is checked to prevent the lack of oxygen. Then, the gauge should be checked when the valve is turned on. Afterwards the flowmeter is adjusted. Connections to oxygen delivery devices and oxygen cylinders should be checked for leakage at least once monthly.
8.5 Breathing Systems
8.5.1 Classification
-
Open systems.
-
Semi-open systems.
-
Semi-closed systems.
-
Closed systems.
There is no anesthetic gas reservoir balloon in open systems. There is no rebreathing of exhaled gases. These systems are simple and cheap. No breathing resistance occurs. It is used with insufflation by open drop or mask method.
Semi-open systems are flow-controlled, valve-free, and non-rebreathing systems. There are types as Mapleson A, B, C, D, E, and F. The Mapleson circuits are simple, lightweight, and easy to clean. There is low breathing resistance. The disadvantages are that they require high flow rate, there is high heat and moisture loss and there is excessive anesthetic agent mixing into the operating room air.
Mapleson A is named as Magill circuit. It requires very high fresh gas flow to prevent rebreathing in controlled ventilation. Mapleson C is named as Waters’ “to and fro” circuit. Mapleson D is Bain circuit. Mapleson E is called as Ayre’s T-piece. Mapleson F is Jackson modification. The disadvantage is that it requires high fresh gas flow and waste gas excretion is not sufficient. Advantages are minimal dead space, minimal resistance to breathing, and economy during controlled ventilation.
Bain circuit has coaxial modification. There is fresh gas inlet tubing inside breathing tube. Exhalation occurs via outer tube. During spontaneous ventilation, a fresh gas flow of 200–300 mL/kg/min is required for normocarbia. On the other side, during controlled ventilation, a fresh gas flow of 70 mL/kg/min is needed to prevent rebreathing. The advantages of Bain circuit are that it retains heat and humidity. The disadvantages are unnoticed disconnection, the possibility of kinking of inlet tubing, high flow requirement, and increase in physiological dead space.
Sorting by advantages in spontaneous ventilation is like A > D > C > B; in controlled ventilation it is like D > B > C > A.
8.5.2 Semi-Closed Breathing Systems
It is the most commonly used breathing system in adults and older children. There is CO2 absorbent. Their disadvantage is that they are large, less potable, and more complex. Resistance is higher in spontaneous ventilation due to valves. Humidity is minimized when the fresh gas flow >5 L/min. Bacteria filter is required. Its advantages are low cost, protection of humidity and heat, reduction in environmental pollution, increased rebreathing with the decrease of fresh gas flow, and very low levels of fresh gas flow.
8.5.3 Closed Breathing Systems
If the fresh gas volume delivered into the system is exactly equal to the amount received by the patient in a certain period of time, this system is called a closed system. The entire volume of expiratory gas returns to the patient after CO2 is absorbed. Maintaining sufficient gas volume in the system is ensured by the fact that excess gas discharge valve is closed and no leak from the system is present. Closed breathing systems have some hazards such as giving 02 in unknown and insufficient concentrations and administration of potent anesthetic inhalation agent at unknown and excessively high concentrations.
8.6 Conclusion
As a result, anesthesia administration started with open systems using ether. Today, modern devices with increased safety are being used and they address different patient types. Mastering the components of these devices, which play a critical role in anesthesia practice, is crucial for physicians working in this field.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Saracoglu, K.T., Cimenoglu, B., Demirhan, R., Saracoglu, A., Tanirgan, G. (2022). Anesthesia Machines and Anesthetic Breathing System. In: Shallik, N.A., Ismail, A., Al Hariri, O. (eds) Improving Anesthesia Technical Staff’s Skills. Springer, Cham. https://doi.org/10.1007/978-3-030-88849-7_8
Download citation
DOI: https://doi.org/10.1007/978-3-030-88849-7_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-88848-0
Online ISBN: 978-3-030-88849-7
eBook Packages: MedicineMedicine (R0)