Abstract
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease that affects 0.5 to 1% of the human population. Gene expression profiling studies of tissues from RA patients showed marked variation in gene expression profiles that allowed identifying distinct molecular disease mechanisms involved in RA pathology. The relative contribution of the different mechanisms may vary among patients and in different stages of the disease. Thus, the broad goals of expression profiling in RA are the improvement of understanding of the pathogenic mechanisms underlying RA, the identification of disease subsets and new drug targets, and the assessment of disease activity, such as responsiveness to therapy, overall disease severity, and organ-specific risk, and development of new diagnostic tests. Genetic and environmental factors contribute to the development of this disease and numerous studies have indicated the participation of the major histocompatibility complex (MHC) class II alleles and non-MHC genes. Therefore, identification of the major roles of the participating cells and of candidate genes has been an important subject of study to the understanding of RA pathogenesis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Rheumatoid arthritis (RA)
- Chronic inflammatory autoimmune disease
- Major histocompatibility complex (MHC)
- Activated T and B lymphocytes
- Synoviocytes
- Anti-cyclic citrullinated peptide antibodies (ACPA)
- RNA transcripts
- Arthritis experimental models
- Adjuvants
- Proteoglycan
- Type II collagen
- Collagen-induced arthritis (CIA)
- Articular joint
- Transgenic mice
- Chronic inflammatory erosive polyarthritis
- Microarray
- Transcriptomic analysis
- RNA sequencing
- Loci
- Quantitative trait loci
- Pristine
- GWAS
- AIRmax
- AIRmin
- miRNAs
- mRNA-miRNA interaction
1 Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease that affects 0.5 to 1% of the human population. RA is a complex pathology characterized by systemic chronic inflammation with the accumulation into synovium and periarticular spaces of activated T and B lymphocytes, innate immune cells such as neutrophils, mast cells, dendritic cells, natural killer cells, and macrophages, and endothelial cells. Rheumatoid fibroblast-like synoviocytes, which exhibit invasive characteristics and synovial macrophages with proinflammatory properties are crucial for the progression of arthritis causing proliferation of synovial membranes and the formation of the invasive pannus that erodes cartilage and bone. In human patients the clinical signs of RA are largely heterogeneous, but the disease is considered to be autoimmune (You et al. 2014). RA heterogeneity is demonstrated by the presence of distinct autoantibody specificities, such as antibodies against immunoglobulins, the rheumatoid factor (RF), and anti-cyclic citrullinated peptide antibodies (ACPA) in the serum, the differential responsiveness to treatment, and by the variability in clinical signs (Silman and Pearson 2002). The precise etiology of RA remains poorly understood, but the main symptoms are chronic synovitis, joint erosion, and several immune abnormalities in both the innate and adaptive compartments.
Given the complexity of RA, systems biology approaches designed to give a general view of different aspects of the disease are required to better understand the basis of arthritis. Oligonucleotide-based microarray technology for global gene expression profiling has arisen as a powerful tool to investigate the molecular complexity and pathogenesis of arthritis and other complex pathologies. This genomic or transcriptomic method combined with postgenomic techniques provides an opportunity to monitor the complex interactions between genes and environment, the regulation of genes and of RNA transcripts, and the proteins that constitute the basis for the etiology or progression of the diseases (Jarvis and Frank 2010).
Gene expression profiling studies of tissues from RA patients showed marked variation in gene expression profiles that allowed to identify distinct molecular disease mechanisms involved in RA pathology (Baechler et al. 2006). The relative contribution of the different mechanisms may vary among patients and in different stages of the disease. Thus, the broad goals of expression profiling in RA are the improvement of understanding of the pathogenic mechanisms underlying RA, the identification of disease subsets and new drug targets, and the assessment of disease activity, such as responsiveness to therapy, overall disease severity, and organ-specific risk, and development of new diagnostic tests (Teixeira et al. 2009).
Genetic and environmental factors contribute to the development of this disease. Numerous studies have indicated the participation of the major histocompatibility complex (MHC) class II alleles and non-MHC genes, such as the solute carrier family 11a member 1—SLC11A1 (formerly named NRAMP1- Natural resistance-associated macrophage protein 1) related to macrophage activation (Runstadler et al. 2005). Identification of the major roles of the participating cells and of candidate genes has been an important subject of study to the understanding of RA pathogenesis (Kurko et al. 2013).
2 Experimental Models of Rheumatoid Arthritis
The initial or preclinical stages of RA are difficult to be studied in humans but numerous arthritis experimental models have been developed which are valuable tools for in-depth investigation of pathogenic pathways that are involved in the several phases of the disease (Kobezda et al. 2014). Regarding ethical procedures, in these models the animals can be submitted to immunizations with arthritogenic substances or antigens, to cell transfer or depletion, to phenotypic selective crosses, to genetic manipulations for the production of transgenic or knockout individuals, etc. Most importantly, these models have been useful for the candidacy of targets for preventive or therapeutic strategies (Asquith et al. 2009).
Several studies have used different animal models for arthritis, generally induced by the injection of adjuvants (AIA), proteoglycan (PGIA), type II collagen (CIA), or pristane (PIA) (Kannan et al. 2005).
Collagen-induced arthritis (CIA). Type II collagen (CII) is expressed exclusively in the articular joint. Although the relationship between anti-CII immunity and human rheumatoid arthritis (RA) has been studied for a long time, definitive conclusions have not been established. CII, as an autoantigen, has been studied extensively in small animal models, such as mice and rats, and the collagen-induced arthritis (CIA) model has increased our understanding of the pathogenesis of human RA (Cho et al. 2007). The disease is class II MHC restricted but mouse strains with permissive haplotypes vary in their susceptibility to CIA. Arthritis development is associated with B and T lymphocyte responses and the generation of anticollagen antibodies and T-cells.
Collagen antibody-induced arthritis (CAIA) in mice has demonstrated the role of humoral immunity in arthritis development. It has been useful for the identification of collagen epitopes for the generation of arthritogenic antibody cocktails that represent humoral autoimmunity in RA. The disease is characterized by macrophage and polymorphonuclear cell infiltration and no T- and B-cell involvement and is non-MHC class II restricted (Hirose and Tanaka 2011).
Proteoglycan-induced arthritis (PGIA) is based on the immunization of mice with human cartilage-derived proteoglycans, which induces the development of severe polyarthritis and spondylitis (Glant et al. 2003).
Pristane-induced arthritis (PIA) has proven to be a valuable experimental model for inflammatory RA. The natural saturated terpenoid alkane 2,4,6,10-tetramethyl pentadecane induces an acute inflammation followed by a chronic relapsing phase. The reaction is T-cell dependent with edema and articular infiltration of mononuclear and polymorphonuclear cells (Potter and Wax 1981).
There are also genetically manipulated models that develop RA spontaneously. For example, transgenic mice overexpressing human TNF-α develop chronic inflammatory erosive polyarthritis (Li and Schwarz 2003). This model highlights the importance of TNF-α in cytokine network in RA. Another example is the IL1 receptor antagonist-deficient mouse that develops inflammatory arthritis mediated by a polarized TH17 response (van den Berg 2009; Lubberts et al. 2005).
In experimental models, microarray analysis should optimally be carried out in isolated populations of cells. New methods have emerged for transcriptomic analysis that are based on single cell RNA sequencing and high-resolution spatial transcriptomic technology. Although they still have limitations, the methods allow the analysis of the subpopulations of cells that make up the tissue and their location (Reviewed in Carr et al. 2020). However, in complex diseases such as RA there is extensive tissue damage with the contribution of several cell types. Hence the analysis of rodent whole ankle joints or of footpads, which comprise heterogeneous cell types, has given a global view of differential gene expression during the several phases of arthritis onset and development. Differential expression of genes encoding tissue repair factors, signal transduction molecules, transcription factors, and DNA repair enzymes, as well as cell cycle regulators have been observed in multiple microarray experiments. An interesting observation in these experiments is the transcriptome map of the differentially expressed genes; in different models of arthritis there is a functional grouping of dysregulated genes forming clusters in the chromosomes. Examples are the MHC class I and class II gene clusters, known to affect susceptibility to a variety of autoimmune diseases and the chemoattractant gene clusters such as CC or CXC chemokine ligands and receptors, which mediate infiltration of leukocytes into synovial tissue, a hallmark of RA (Fujikado et al. 2006). Some studies attempt to link differentially expressed genes into interactive regulatory networks (Silva et al. 2009). This approach is quite powerful to identify new targets for therapy by looking at the network structures, the places (genes) with the highest connectivity in which disruption would have a larger impact.
3 Loci Regulating Inflammatory Arthritis
The identification of the loci influencing inflammatory arthritis in animal models is important for parallel genetic studies in humans. The individual genetic constitution of experimental animals involving major histocompatibility complex (MHC) or non-MHC genes has been associated with variations in rheumatoid arthritis susceptibility. In mice or rats, genome-wide linkage studies with DNA polymorphism markers, such as microsatellites or single nucleotide polymorphisms (SNPs), have been carried out using intercross progenies of resistant and susceptible strains. These studies, in which environmental effects and genetic backgrounds are controlled, have been useful for the study of the genetic basis of RA (Ibrahim and Yu 2006).
Several QTLs (Quantitative Trait Loci) were identified in different models of experimental arthritis. The first locus controlling pristane-induced arthritis (PIA) detected in mice was Prtia1 on chromosome 3, in an intercross population from mice selected for high and low antibody production (Jensen et al. 2006). QTL was also mapped in other arthritis models such as those induced by Borrelia burgdorferi (Roper et al. 2001), PGIA (Glant et al. 2004), and collagen (Adarichev et al. 2003). Nonoverlapping sets of QTLs were identified, generating a heterogeneous picture of risk alleles (Besenyei et al. 2012; Kurko et al. 2013). The results evidence the genetic heterogeneity in the control of the different stages and phenotypes of the disease. Table 12.1 presents some relevant coincident susceptibility QTLs in rheumatoid arthritis, according to GWAS studies carried out in mice and humans.
Numerous RA QTLs have been mapped but few of the associated polymorphisms were identified in protein-coding regions of genes causing changes in protein structure or function. This suggests that polymorphisms in noncoding regions which might affect gene expression largely contribute to variations in RA susceptibility. In this way, transcriptome technology can also be used to detect genetic polymorphisms that regulate gene expression levels.
4 Combining Transcriptome and Genome Screening to Identify Genes That Control Arthritis
The two genomic approaches, that is, transcriptome and genome screening (GWAS), have been combined in studies where the locations of differently expressed genes during RA are compared with those mapping at QTLs for arthritis, for immune or inflammatory responses, or for other autoimmune diseases (Yu et al. 2007). The approach has been useful to candidate genes inside the QTLs. The coincidence of chromosomal locations of genes in QTLs in different model systems with the locations of the corresponding human orthologue is a good indicator of their implication in RA control.
Furthermore, the modulation of common genes during RA, irrespective of etiology and of species indicates the importance of these mediators in the pathogenesis of arthritis. For example, the augmented expression of chemokines and receptors, which recruit neutrophils or naïve and memory T cells to inflammatory sites, is very important to disease progression. Chemokines and ligands are found in the synovial tissue of patients with RA; proinflammatory cytokines and their cognate receptors, such as IL-1β, IL-1RI, TNF-α R, IL-6Rα, IL-2Rγ, and IL-17R, are upregulated in several RA models as well as in arthritis patients; IL-1β induces serum amyloid A3 (Saa3) and the matrix metalloproteinases Mmp-3 and Mmp-9 that are also upregulated in several models. High upregulation in runt-related transcription factor 1 (RUNX1) and a group of transporter genes such as solute carrier 11 family A1 (Slc11a1, formerly Nramp1) is also a common feature in RA models. In synthesis, a remarkable feature that originated from numerous transcriptome or genomic studies of arthritis has been the demonstration of gene expression signatures associated with inflammation. The results evidence that besides being an antigen-driven event there is an important interplay between innate and adaptive immunity systems in the etiology of RA (Jarvis and Frank 2010).
5 A Model to Study Inflammatory Rheumatoid Arthritis: AIRmax and AIRmin Phenotypically Selected Mouse Lines
Heterogeneous mice selected for maximal (AIRmax) or minimal (AIRmin) acute inflammatory reaction appeared to be useful models for studying the mechanisms involved in rheumatoid arthritis susceptibility (Vigar et al. 2000).
AIRmax and AIRmin mice were produced by bidirectional selection, starting from a highly polymorphic population (F0) derived from the intercrossing of eight inbred mouse strains (Fig. 12.1). The selection phenotypes chosen were localized leukocyte influx and exudated plasma proteins 24 h after the subcutaneous injection of polyacrylamide beads (Biogel), a nonantigenic, insoluble, and chemically inert substance (Ibanez et al. 1992). The progressive divergence of the AIRmax and AIRmin lines during successive generations of selective breeding reached 20- and 2.5-fold differences in leukocyte infiltration and exudated protein concentrations respectively. These differences resulted from the accumulation of alleles in quantitative trait loci endowed with opposite and additive effects on the inflammatory response. Inbreeding was avoided for selective breeding, and as such AIRmax and AIRmin mice are outbred mice that maintain a heterogeneous genetic background but are homozygous in acute inflammation modifier loci. Analysis of the selective processes indicated that the AIR phenotype is regulated by at least 11 QTLs (Biozzi et al. 1998).
Pristane-induced arthritis (PIA) has proven to be a valuable experimental model for inflammatory RA for its delayed onset, chronicity, and independence from xenoantigen administration. Thus, arthritis ensues from a sensitization over time and pristane has been described to improve autoimmunity by the activation of the immune response against cross-reactive microbiota antigens (Patten et al. 2004). AIRmax mice are extremely susceptible whereas AIRmin mice are resistant to PIA (Fig. 12.2a). The incidence of PIA in AIRmax mice was similar to that of inbred DBA/1 and BALB/c mice although with higher severity. The incidence and severity were more intense than in the CBA/Igb model because 15 to 25% of these mice develop inflammation of the ankle and wrist joints approximately 200 days after pristane injection. PIA is accompanied by markedly elevated humoral agalactosyl IgG levels mediated by IL6 production (Thompson et al. 1992) and CD4+ T cell (Th)-dependent (Stasiuk et al. 1997) immune responses to mycobacterial 65-kDa heat shock protein (hsp65). Moreover, the protection against PIA is mediated by Th2-associated cytokines produced after hsp65 preimmunization (Thompson et al. 1998; Thompson et al. 1990). In contrast to the immune response profile observed in inbred mice, high IgG1 anti-hsp65 levels were observed in susceptible AIRmax mice, whereas IgG2a was the predominant isotype in the resistant AIRmin mice. Additionally, it was shown that IL-4, IL-6, and TNF secreting splenic cells were significantly more abundant in AIRmax than in AIRmin animals. IFNg-producing cells, on the other hand, increased only in AIRmin mice. Specific pathogen-free susceptible mice do not develop this disease, but when transferred to a conventional environment, they reacquire arthritis susceptibility, indicating the involvement of environmental factors in PIA (Thompson and Elson 1993).
The results in the AIRmax and AIRmin PIA model, when compared to those obtained in inbred mice, evidence the interference of genetic background in the mechanisms underlying arthritis susceptibility and severity. Interaction of arthritis controlling genes with heterogeneous genetic backgrounds and variability in gut microbiota might contribute to the variable signs of arthritis occurring in humans.
The transporter gene Solute carrier 11 family a1 ( Slc11a1) has been described in mice as a major modulator of susceptibility to infectious diseases and is expressed in macrophages and neutrophils. Slc11a1 is pleiotropic, interfering with macrophage activation, oxidative and nitrosamine bursts, TNF, IFNg, and IL-1 production, and the expression of MHC class II molecules. In mice, the mutation corresponding to the Slc11a1 S allele associated with susceptibility determines a gly169asp substitution resulting in a nonfunctional protein that promotes an accumulation of ions inside the phagosome of macrophages that favors pathogen replication (Vidal et al. 1992). In the experiment for the production of AIRmax and AIRmin mouse lines, the frequency of the Slc11a1 S allele was 25% in the founder population (F0), but shifted to 60% in AIRmin and to 9% in AIRmax after 30 generations of selective breeding. The results suggest that these changes in allele frequencies were the result of the selection process for acute inflammatory response (Araujo et al. 1998).
The effect of the Slc11a1 R and S alleles during PIA development was studied in AIRmax and AIRmin mice that were rendered homozygous for the Slc11a1 alleles by genotype-assisted breeding (Fig. 12.2b). AIRmax mice homozygous for the S allele (AIRmaxSS) were significantly more susceptible (80% incidence) to RA than AIRmaxRR mice (30% incidence) evidencing the influence of this polymorphism in RA (Peters et al. 2007). The involvement of this gene in this study as well as in other murine arthritis models constituted the basis for the study of Slc11a1 involvement in human RA. In fact, several authors reported linkage of SLC11A1 alleles to human RA probably associated with a polymorphic repeat in the RUNX1-containing promoter region of the gene (Ates et al. 2009).
6 Mapping of QTL Controlling PIA in AIRmax and AIRmin Mice
A genome-wide linkage study was carried out in a large F2 population of intercrossed AIRmax and AIRmin F2(AIRmax x AIRmin) mice through linkage analysis of PIA severity phenotype with a panel of SNPs. Two new PIA QTLs ( Prtia 2 and Prtia3) were mapped on chromosomes 5 and 8, respectively, and three suggestive QTLs were detected on chromosomes 7, 17, and 19 (De Franco et al. 2014). In this same F2(AIRmax x AIRmin) population, loci that regulate the intensity of the acute inflammatory response were mapped on chromosomes 5, 7, 8, and 17, which overlap the QTLs that controls PIA severity, suggesting common regulations (Vorraro et al. 2010; Galvan et al. 2011). Co-located chromosome 5 QTLs controlling arthritis severity and humoral responses during B. burgdorferi infection were identified in the F2 intercross of C3H/HeNCr and C57BL/6NCr mice (Weis et al. 1999), suggesting the involvement of the chemokine Cxcl9 gene , which maps to the QTL peak in this model (Ma et al. 2009).
In order to candidate genes within the QTL detected in the AIRmax and AIRmin model, transcriptome studies were performed using tissues or cells from normal or arthritic individuals. In this model, the total number of up- and downregulated genes in each line was distinct, as can be seen in Fig. 12.3. More genes were modulated in AIRmax than in AIRmin mice, although a gene ontology analysis revealed an overrepresentation of genes related to inflammatory reaction and chemotaxis biological themes in both lines (Fig. 12.4). Global gene expression analysis indicated 419 differentially expressed genes between AIRmax and AIRmin mice. Figs. 12.5 and 12.6 show genes differentially expressed on chromosomes 5 and 8 respectively. Several genes related to inflammation, cell adhesion, and chemotaxis could be observed on chromosome 5, while tissue antigens, cell differentiation, hemeoxigenase, and scavenger receptor genes were observed on chromosome 8 (De Franco et al. 2014).
Ibrahim and collaborators investigated the gene expression profiles of inflamed paws in DBA/1 inbred mice using a similar approach for collagen-induced arthritis (Ibrahim et al. 2002). In their work, inflammation resulted in increased gene expression of matrix metalloproteinases, and immune-related extracellular matrix and cell-adhesion molecules, as well as molecules involved in cell division and transcription, in a manner very similar to the AIRmax/AIRmin model. However, the total number of differentially expressed genes involved in the inbred mice model (223) was lower than in our model (419), suggesting that the heterogeneous background of AIRmax and AIRmin mice permitted a larger genome involvement in this phenotype. Among the differentially expressed genes, inflammatory and chemokine genes on chromosome 5 and macrophage scavenger receptor 1 ( Msr1) and hemeoxigenase 1 ( Hmox1) genes on chromosome 8 appear to be the major candidates.
Chemokines are involved in leukocyte recruitment to inflammatory sites, such as synovial tissue in rheumatoid arthritis (RA). However, they may also be homeostatic as these functions often overlap (Ibrahim et al. 2001). Chemokines have essential roles in the recruitment and activation of leucocyte subsets within tissue microenvironments, and stromal cells actively contribute to these networks. Macrophages play a central role in the pathogenesis of rheumatoid arthritis (RA), which is marked by an imbalance of inflammatory and anti-inflammatory macrophages in RA synovium. Although the polarization and heterogeneity of macrophages in RA have not been fully elucidated, the identities of macrophages in RA can potentially be defined by their products, including costimulatory molecules, scavenger receptors, cytokines/chemokines and their receptors, and transcription factors (Li et al. 2012). It has been demonstrated that inappropriate constitutive chemokine expression contributes to the persistence of inflammation by actively blocking its resolution (Filer et al. 2008). This was also observed in urethane-induced lung carcinogenesis, where transcriptome analysis revealed that the genes involved in transendothelial migration and chemokine-cell adhesion were differently expressed in normal lungs of susceptible AIRmin and resistant AIRmax mice (De Franco et al. 2010), suggesting important roles for these phenotypes in chronic diseases.
7 MicroRNA and Arthritis
Several studies have demonstrated the involvement of small RNAs, known as miRNAs in the development of RA. MiRNAs are a class of small, noncoding, RNA molecules with approximately 21 nucleotides in length that can regulate gene expression by reducing the ability of specific mRNAs to direct the synthesis of their encoded proteins (Krol et al. 2010). They likely participate in most developmental and physiologic processes, with involvement in, but not limited to, cell proliferation and differentiation, regulation of lipid metabolism, and modulation of insulin secretion. The importance of miRNA-mediated regulation of gene expression for the prevention of autoimmunity and maintenance of normal immune system functions has been described (Wittmann and Jäck 2011). Studies in humans have detected altered miRNA expression in RA patients when compared to controls or osteoarthritis patients (Pauley et al. 2008; Kobayashi et al. 2008; Stanczyk et al. 2008). MiRNAs can be detected in body fluids without invasive procedures, and thus may be used as prognostic or diagnostic biomarkers for specific conditions, such as rheumatic diseases (Ceribelli et al. 2012).
In the PIA model, pristane injection modulated several genes in the peritoneal cells of AIRmax and AIRmin lines in both time points analyzed. This modulation was more widespread in AIRmax mice, with about twice the number of modulated genes than the AIRmin line (2025 vs 1043). This difference reflects mainly the number of downregulated genes, which was five-fold higher in AIRmax animals (704 vs 131). In previous microarray analyses using the paws of these animals, the AIRmax line also showed five-fold more downregulated genes than AIRmin and two-fold more upregulated genes (De Franco et al. 2014). The same gene expression profile was also observed in the subcutaneous tissue of these lines after Biogel injection (Fernandes et al. 2016). Although different tissues and stimuli have been analyzed, these results indicate that the selective pressure during phenotypic selection acted in general inflammatory regulation mechanisms.
MiRNA expressions after pristane injection were also distinct in AIRmax and AIRmin mice. At 120 days, 184 miRNAs were upregulated and 12 downregulated exclusively in AIRmax animals. That regulation was similar (189 up- and 12 downregulated) at 170 days. In contrast, the AIRmin line upregulated 15 and 10 miRNAs at 120 and 170 days respectively; no downregulated miRNA was detected. The higher number of downregulated genes observed in AIRmax mice may be a consequence of the upregulation of miRNAs in their peritoneal cells.
Most of the up- or downregulated miRNAs have not been ascribed roles in experimental or human arthritis development. Instead, many of those miRNAs are described in terms of their roles in suppressing or inducing several types of malignant tumors, although many have been shown to be involved in the regulation of important biological processes in the development of autoimmune diseases such as inflammation. We therefore sought to identify important pathways in which those miRNAs participated and which could explain their modulation in our model – eventually leading to the identification of new arthritis-related miRNAs in experimentally induced arthritis.
MiR-132-3p was the most upregulated miRNA in the susceptible mouse line in microarrays and qRT-PCR (106- and seven-fold higher at 120 days, and 67- and 4.5-fold higher at 170 days respectively). Expression of that miRNA has been found to increase in the peripheral blood mononuclear cells (PBMCs) of rheumatoid arthritis patients (Kobayashi et al. 2008). In that study, one of the patients with the active disease showed unaltered levels of that and other miRNAs related to the disease after two months of treatment with methotrexate. Those results indicate that the high expressions of miRNAs in that patient were related to unresponsiveness to the treatment. MiR-132-3p may therefore play a key role in systemic conditions related to joint inflammation, which would explain its high expression in the peritoneum of susceptible AIRmax animals. MiR-132 is specifically induced in Th17 cells and acts as a proinflammatory mediator increasing osteoclastogenesis through the downregulation of COX2. In in vivo, articular knockdown of MiR-132 in murine arthritis models reduces the number of osteoclasts in the joints (Donate et al. 2021).
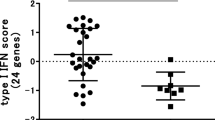
MiR-132-3p and miR-212-3p are members of the same family (located on chromosome 11 in mice) that forms the miR-212/132 cluster, and they have similar seed sequences. That cluster, induced by the activation of AhR in inflammatory bowel disease, was able to promote an inflammatory response by inducing the Th17 response and suppressing IL-10 production (Chinen et al. 2015). The Il10 gene was downregulated in peritoneal cells in AIRmax mice, indicating that there may be an indirect regulation of the expression of that cytokine by those miRNAs (Fernandes et al. 2018). IL-10 is an important anti-inflammatory cytokine that inhibits proinflammatory mediator production and lymphocyte proliferation, thus playing a protective role in autoimmune diseases. IL-10 has been shown to contribute to the prevention of arthritic inflammation in macrophages during collagen-induced arthritis development (Chen et al. 2017). That gene can be regulated by different miRNAs, including miR-27b-3p, which is highly upregulated in that line (Fig. 12.7).
mRNA-miRNA interaction network. (a) miRNAs upregulated in AIRmax mice and their interaction with predicted target genes; (b) miRNAs upregulated AIRmin mice and their interaction with predicted target genes. Red = upregulated genes; green = downregulated genes. The interaction network was built with Cytoscape 3.4.0.
Cd69 and S1pr1 (specifically targeted by 106a-5p, 25-3p, and 20b-5p miRNAs) were downregulated in AIRmax mice (Fig. 12.7). CD69 is a leukocyte receptor induced in lymphocytes and macrophages after activation. Sancho et al. 2003 demonstrated that CD69−/− and CD69 +/− mice had an exacerbated form of collagen-induced arthritis (CIA) when compared to controls and that CD69 was capable of inducing TGF-β2 synthesis. TGF-β2 is an anti-inflammatory cytokine, and null mutations in that gene can lead to severe inflammatory disorders; that gene regulates the production of inflammatory cytokines and has protective effects in the CIA model (Sancho et al. 2003; Brandes et al. 1991). Tgfb2 was the most downregulated gene in the AIRmax line (40-fold), while CD69 was approximately six-fold downregulated. The S1pr1 gene, on the other hand, affects the differentiation of osteoblasts (Sato et al. 2012). The inhibition of osteoblast differentiation contributes to bone loss in RA as well as to a decreased healing ability of those lesions (Baum and Gravallese 2016).
The expressions of miR-181b-5p and Il6 were shown to be inversely correlated following stimulation with LPS, and Il6 is a direct target of miR-181b-5p (Zhang et al. 2015), demonstrating the critical role of the posttranscriptional control of IL-6 by miR-181b-5p in endotoxin tolerance. The expressions of miR-181b-5p and Il6 were also inversely correlated in susceptible AIRmax mice. Although Il6 did not appear as a target for miR-181b-5p in our interaction network (which considered at least 3 different algorithms), the data from the TargetScan database (which is widely used in the literature to predict miRNA-RNA interactions) indicated that gene as a possible target of miR-181b-5p. An important role of IL-6 has been reported in the in vitro inhibition of osteoclast progenitors mediated by the disruption of RANK signaling (Yoshitake et al. 2008). Osteoclasts are required for articular bone resorption and are responsible for bone erosion in RA (Baum and Gravallese 2016; Lin et al. 2015). The unbalanced expression of the genes that promote osteoclatogenesis and inhibit osteoblast differentiation may represent a mechanism for the stimulation of bone erosion and increased disease severity in AIRmax animals. Histological analyses of the AIRmax paws did, in fact, show bone loss in addition to the destruction of cartilage (Correa et al. 2017).
Soto et al. 2008 compared the gene expression profiles of the rat collagen-induced arthritis model (CIA) with human RA (using paw and knee synovial tissue respectively). Comparing the DEGs in our model with the model used by Soto, we observed that two genes upregulated in AIRmax mice (Mmp13 and Gpsm3) were also upregulated in CIA rats.
The MMP13 and GPSM3 genes play significant roles in rheumatoid arthritis in humans, and GPSM3 has been associated with the risk of developing autoimmune diseases. Polymorphisms associated with decreased transcription have been inversely correlated with the risk of developing arthritis. The reduced expression of GPSM3 was observed to prevent neutrophil migration mediated by LTB4 (leukotriene B4) and CXCL8 to arthritic joints (Gall et al. 2016). Additionally, mice deficient for Gpsm3 were protected from arthritis induced by anticollagen antibodies, with reduced CCL2- and CX3CL1-mediated migration of myeloid cells (Giguère et al. 2013). Gpsm3 is located on chromosome 17 in mice, where a suggestive QTL for experimental arthritis was detected in our model (De Franco et al. 2014). The miRanda database identified Gpsm3 as a predicted target of miRNA-151-5p, which is downregulated in AIRmax mice. Since the interaction was only predicted by the database, it was not considered in our results, although the high expression of Gpsm3 as a consequence of the downregulation of miRNA-151-3p should not be completely ruled out.
MMP-13 (or collagenase-3) hydrolyzes type 2 collagen and may favor the destruction of cartilage in arthritic joints. In rheumatoid arthritis, IL-1β and TNF-α produced by macrophages in the connective tissue stimulate the production of that MMP by articular chondrocytes (Vincenti and Brinckerhoff 2002). Additionally, a key role has been attributed to some genetic loci encoding metalloproteinases in bone destruction. The expression of MMP-13 increased ten-fold in AIRmax mice but remained unaltered in pristane-treated AIRmin animals. Vonk and coworkers (Vonk et al. 2014) looked for different miRNAs expressed in healthy and osteoarthritis (OA) patients and found that miRNA-148a levels in healthy subjects were approximately ten-fold higher than those seen in patients with the disease. Transfection of miR-148a-3p into cells of OA patients resulted in decreased MMP-13 expression (which had increased in those patients), suggesting that this miRNA may play a protective role in OA, with a consequent reduction in cartilage destruction.
In a second analysis, Soto et al. 2008 identified 30 differentially expressed genes when comparing RA patients and healthy controls. Of those 30 genes, Pde3b, Tgfb2, and Fam120c were downregulated in both RA patients and AIRmax mice; Tgfb2 showed a significant protective effect in arthritis models as discussed above.
Many miRNAs are over- or underexpressed in autoimmune diseases such as SLE (Liang and Shen 2012; Amarilyo and La Cava 2012) and rheumatoid arthritis (RA) (Ceribelli et al. 2011), and investigators have reported that miR-146a is altered in those diseases (Ceribelli et al. 2012). Interestingly, expression of miR-146a was higher in AIRmax than in AIRmin control mice 120 days after pristane injection. Increased expression of miRNA-146a has been well documented in the PBMCs of arthritic patients. That microRNA has two known targets: Traf6 (TNF receptor-associated factor 6) and Irak1 (interleukin-1 receptor-associated kinase 1) , both of which stimulate TNF-α production (Shrivastava and Pandey 2013). The expression of those molecules were unaltered in those patients, suggesting that increased miRNA-146a levels were unable to regulate TRAF6/IRAK. Therefore, it is not exactly known how the high expression of that miRNA is related to the increased levels of TNF-α in RA (Ceribelli et al. 2011).
8 Concluding Remarks
Recent advances in the field of genetics have dramatically changed our understanding of autoimmune disease. Candidate gene and, more recently, genome-wide association (GWA) and linkage studies have led to an explosion in the number of loci and pathways known to contribute to autoimmune phenotypes, confirming a major role for the MHC region and, more recently, identifying risk loci involving both the innate and adaptive immune responses. However, most regions found through GWA scans have yet to isolate the association to the causal allele(s) responsible for conferring disease risk. A role for rare variants (allele frequencies of <1%) has begun to emerge. The study of the abundant long intergenic noncoding RNAs and of small interfering RNA (microRNAs) has also become a powerful tool to understand the mechanisms that modulate the gene expression profiles in RA and other autoimmune diseases (Jarvis and Frank 2010; Donate et al. 2013). Future research will also use next generation sequencing (NGS) technology to comprehensively evaluate the human genome for risk variants. Whole transcriptome sequencing (e.g., RNA-Seq), which combines gene expression, sequence, and splice variant analysis, will provide much more detailed gene expression data. Despite its high incidence and severe phenotype, RA still has no cure in spite of many efforts to produce effective therapy treatments. Further studies should therefore be carried out to better understand the functions and mechanisms of miRNAs in the immune system and in arthritis development. The AIRmax and AIRmin lines constitute interesting tools for mapping inflammatory disease modifying genes and miRNAs, in addition to being a valid animal model for the human disease in respect to similar gene pathways and miRNAs. Our studies have been demonstrated that those lines have distinct gene and miRNA expression profiles, which may be partly responsible for their different phenotypes. Regardless of the current or future technology, the versatility of murine models will continue to be required to advance our understanding of human diseases.
References
Adarichev VA, Valdez JC, Bardos T et al (2003) Combined autoimmune models of arthritis reveal shared and independent qualitative (binary) and quantitative trait loci. J Immunol 170(5):2283–2292
Amarilyo G, La Cava A (2012) miRNA in systemic lupus erythematosus. Clin Immunol 144(1):26–31
Araujo LM, Ribeiro OG, Siqueira M et al (1998) Innate resistance to infection by intracellular bacterial pathogens differs in mice selected for maximal or minimal acute inflammatory response. Eur J Immunol 28(9):2913–2920
Asquith DL, Miller AM, Mcinnes IB et al (2009) Animal models of rheumatoid arthritis. Eur J Immunol 39(8):2040–2044
Ates O, Dalyan L, Musellim B et al (2009) NRAMP1 (SLC11A1) gene polymorphisms that correlate with autoimmune versus infectious disease susceptibility in tuberculosis and rheumatoid arthritis. Int J Immunogenet 36(1):15–19
Baechler EC, Batliwalla FM, Reed AM et al (2006) Gene expression profiling in human autoimmunity. Immunol Rev 210:120–137
Besenyei T, Kadar A, Tryniszewska B et al (2012) Non-MHC risk alleles in rheumatoid arthritis and in the syntenic chromosome regions of corresponding animal models. Clin Dev Immunol. https://doi.org/10.1155/2012/284751
Baum R, Gravallese EM (2016) Bone as a target organ in rheumatic disease: impact on osteoclasts and osteoblasts. Clin Rev Allergy Immunol 51(1):1–15
Biozzi G, Ribeiro OG, Saran A et al (1998) Effect of genetic modification of acute inflammatory responsiveness on tumorigenesis in the mouse. Carcinogenesis 19(2):337–346
Brandes ME, Allen JB, Ogawa Y et al (1991) Transforming Growth Factor Beta 1 suppresses acute and chronic arthritis in experimental animals. J Clin Invest 87(3):1108–1113
Carr HL, Turner JD, Major T, Scheel-Toellner D, Filer A (2020) New developments in transcriptomic analysis of synovial tissue. Front Med 7:21. https://doi.org/10.3389/fmed.2020.00021
Ceribelli A, Ma N, Satoh M et al (2011) MicroRNAs in rheumatoid arthritis. FEBS Lett 585(23):3667–3674
Ceribelli A, Satoh M, Chan EK (2012) microRNAs and autoimmunity. Curr Opin Immunol 24(6):686–691
Chen S, Chen B, Wen Z et al (2017) Il-33/st2-mediated inflammation in macrophages is directly abrogated by Il-10 during rheumatoid arthritis. Oncotarget 8(20):32407–324018
Chinen I, Nakahama T, Kimura A et al (2015) the aryl hydrocarbon receptor/microrna-212/132 axis in t cells regulates il-10 production to maintain intestinal homeostasis. Int Immunol 27(8):405–415
Cho YG, Cho ML, Min SY et al (2007) Type II collagen autoimmunity in a mouse model of human rheumatoid arthritis. Autoimmun Rev 7(1):65–70
Correa MA, Canhamero T, Borrego A et al (2017) Slc11a1 (Nramp-1) gene modulates immune-inflammation genes in macrophages during pristane-induced arthritis in mice. Inflamm Res 66:969–980
De Franco M, Colombo F, Galvan A et al (2010) Transcriptome of normal lung distinguishes mouse lines with different susceptibility to inflammation and to lung tumorigenesis. Cancer Lett 294(2):187–194
De Franco M, Peters LC, Correa MA et al (2014) Pristane-induced arthritis loci interact with the Slc11a1 gene to determine susceptibility in mice selected for high inflammation. PLoS One 9(2):e88302
Donate PB, Fornari TA, Macedo C et al (2013) T cell post-transcriptional miRNA-mRNA interaction networks identify targets associated with susceptibility/resistance to collagen-induced arthritis. PLoS One 8(1):e54803
Donate PB, Alves de Lima K, Peres RS, et al (2021) Cigarette smoke induces miR-132 in Th17 cells that enhance osteoclastogenesis in inflammatory arthritis. Proc Natl Acad Sci USA 5;118(1):e2017120118
Fernandes JG, Canhamero T, Borrego A, et al (2016) Distinct gene expression profiles provoked by polyacrylamide beads (Biogel) during chronic and acute inflammation in mice selected for maximal and minimal inflammatory responses. Inflamm Res 2016;65(4):313–323
Fernandes JG, Borrego A, Jensen JR et al (2018) miRNA Expression and Interaction with Genes Involved in Susceptibility to Pristane-Induced Arthritis. J Immunol Res Dec 16:1928405. https://doi.org/10.1155/2018/1928405
Filer A, Raza K, Salmon M et al (2008) The role of chemokines in leucocyte-stromal interactions in rheumatoid arthritis. Front Biosci 13:2674–2685
Fujikado N, Saijo S, Iwakura Y (2006) Identification of arthritis-related gene clusters by microarray analysis of two independent mouse models for rheumatoid arthritis. Arthritis Res Ther 8(4):100–125
Gall BJ, Schroer AB, Gross JD et al (2016) Reduction of Gpsm3 expression skin to the arthritis-protective SNP rs204989 differentially affects migration in a neutrophil model. Genes Immun 17(6):321–327
Galvan A, Vorraro F, Cabrera W et al (2011) Association study by genetic clustering detects multiple inflammatory response loci in non-inbred mice. Genes Immun 12(5):390–394
Giguère PM, Billard MJ, Laroche G et al (2013) G-protein signaling modulator-3, a gene linked to autoimmune diseases, regulates monocyte function and its deficiency protects from inflammatory arthritis. Mol Immunol 54(2):193–198
Glant TT, Finnegan A, Mikecz K (2003) Proteoglycan-induced arthritis: immune regulation, cellular mechanisms, and genetics. Crit Rev Immunol 23(3):199–250
Glant TT, Adarichev VA, Nesterovitch AB et al (2004) Disease-associated qualitative and quantitative trait loci in proteoglycan-induced arthritis and collagen-induced arthritis. Am J Med Sci 327(4):188–195
Hirose J, Tanaka S (2011) Animal models for bone and joint disease. CIA, CAIA model. Clin Calcium 21(2):253–259
Ibanez OM, Stiffel C, Ribeiro OG et al (1992) Genetics of nonspecific immunity: I. Bidirectional selective breeding of lines of mice endowed with maximal or minimal inflammatory responsiveness. Eur J Immunol 22(10):2555–2563
Ibrahim SM, Yu X (2006) Dissecting the genetic basis of rheumatoid arthritis in mouse models. Curr Pharm Des 12(29):3753–3759
Ibrahim SM, Mix E, Bottcher T et al (2001) Gene expression profiling of the nervous system in murine experimental autoimmune encephalomyelitis. Brain 124:1927–1938
Ibrahim SM, Koczan D, Thiesen HJ (2002) Gene-expression profile of collagen-induced arthritis. J Autoimmun 18(2):159–167
Jarvis JN, Frank MB (2010) Functional genomics and rheumatoid arthritis: where have we been and where should we go? Genome Med 2(7):44–59
Jensen JR, Peters LC, Borrego A et al (2006) Involvement of antibody production quantitative trait loci in the susceptibility to pristane-induced arthritis in the mouse. Genes Immun 7(1):44–50
Kannan K, Ortmann RA, Kimpel D (2005) Animal models of rheumatoid arthritis and their relevance to human disease. Pathophysiology 12(3):167–181
Kobayashi T, Lu J, Cobb BS et al (2008) Dicer-dependent pathways regulate chondrocyte proliferation and differentiation. Proc Natl Acad Sci U S A 105(6):1949–1954
Kobezda T, Ghassemi-Nejad S, Mikecz K et al (2014) Of mice and men: how animal models advance our understanding of T-cell function in RA. Nat Rev Rheumatol 10(3):160–170
Krol J, Loedige I, Filipowicz W (2010) The widespread regulation of microrna biogenesis, function and decay. Nat Rev Genet 11(9):597–610
Kurko J, Besenyei T, Laki J et al (2013) Genetics of rheumatoid arthritis—a comprehensive review. Clin Rev Allergy Immunol 45(2):170–179
Li P, Schwarz EM (2003) The TNF-alpha transgenic mouse model of inflammatory arthritis. Springer Semin Immunopathol 25(1):19–33
Li J, Hsu HC, Mountz JD (2012) Managing macrophages in rheumatoid arthritis by reform or removal. Curr Rheumatol Rep 14(5):445–454
Liang D, Shen N (2012) MicroRNA involvement in lupus: the beginning of a new tale. Curr Opin Rheumatol 24(5):489–498
Lin L, Yee SW, Kim RB et al (2015) Slc transporters as therapeutic targets: emerging opportunities. Nat Rev Drug Discov 14(8):543–560
Lubberts E, Koenders MI, Van Den Berg WB (2005) The role of T-cell interleukin-17 in conducting destructive arthritis: lessons from animal models. Arthritis Res Ther 7(1):29–37
Ma Y, Miller JC, Crandall H et al (2009) Interval-specific congenic lines reveal quantitative trait Loci with penetrant lyme arthritis phenotypes on chromosomes 5, 11, and 12. Infect Immun 77(8):3302–3311
Pauley KM, Satoh M, Chan AL et al (2008) Upregulated mir-146a expression in peripheral blood mononuclear cells from rheumatoid arthritis patients. Arthritis Res Ther 10(4):r101
Patten C, Bush K, Rioja I et al (2004) Characterization of pristane-induced arthritis, a murine model of chronic disease: response to antirheumatic agents, expression of joint cytokines, and immunopathology. Arthritis Rheum 50(10):3334–3345
Peters LC, Jensen JR, Borrego A et al (2007) Slc11a1 (formerly NRAMP1) gene modulates both acute inflammatory reactions and pristane-induced arthritis in mice. Genes Immun 8(1):51–56
Potter M, Wax JS (1981) Genetics of susceptibility to pristane-induced plasmacytomas in BALB/ cAn: reduced susceptibility in BALB/cJ with a brief description of pristane-induced arthritis. J Immunol 127(4):1591–1595
Roper RJ, Weis JJ, Mccracken BA et al (2001) Genetic control of susceptibility to experimental Lyme arthritis is polygenic and exhibits consistent linkage to multiple loci on chromosome 5 in four independent mouse crosses. Genes Immun 2(7):388–397
Runstadler JA, Saila H, Savolainen A et al (2005) Association of SLC11A1 (NRAMP1) with persistent oligoarticular and polyarticular rheumatoid factor-negative juvenile idiopathic arthritis in Finnish patients: haplotype analysis in Finnish families. Arthritis Rheum 52(1):247–256
Sancho D, Gómez M, Viedma F et al (2003) CD69 downregulates autoimmune reactivity through active transforming growth factor-beta production in collagen-induced arthritis. J Clin Invest 112(6):872–882
Sato C, Iwasaki T, Kitano S et al (2012) Sphingosine 1-phosphate receptor activation enhances bmp-2-induced osteoblast differentiation. Biochem Biophys Res Commun 423(1):200–205
Silman AJ, Pearson JE (2002) Epidemiology and genetics of rheumatoid arthritis. Arthritis Res 4(Suppl 3):S265–S272
Silva GL, Junta CM, Sakamoto-Hojo ET et al (2009) Genetic susceptibility loci in rheumatoid arthritis establish transcriptional regulatory networks with other genes. Ann N Y Acad Sci 1173:521–537
Shrivastava AK, Pandey A (2013) Inflammation and rheumatoid arthritis. J Physiol Biochem 69(2):335–347
Soto H, Hevezi P, Roth RB et al (2008) Gene array analysis comparison between rat collagen-induced arthritis and human rheumatoid arthritis. Scand J Immunol 68(1):43–57
Stanczyk J, Pedrioli DM, Brentano F et al (2008) Altered expression of microRNA in synovial fibroblasts and synovial tissue in rheumatoid arthritis. Arthritis Rheum 58(4):1001–1009
Stasiuk LM, Ghoraishian M, Elson CJ et al (1997) Pristane-induced arthritis is CD4+ T-cell dependent. Immunology 90(1):81–86
Teixeira VH, Olaso R, Martin-Magniette ML et al (2009) Transcriptome analysis describing new immunity and defense genes in peripheral blood mononuclear cells of rheumatoid arthritis patients. PLoS One 4(8):e6803
Thompson SJ, Elson CJ (1993) Susceptibility to pristane-induced arthritis is altered with changes in bowel flora. Immunol Lett 36(2):227–231
Thompson SJ, Rook GA, Brealey RJ et al (1990) Autoimmune reactions to heat-shock proteins in pristane-induced arthritis. Eur J Immunol 20(11):2479–2484
Thompson SJ, Hitsumoto Y, Zhang YW et al (1992) Agalactosyl IgG in pristane-induced arthritis. Pregnancy affects the incidence and severity of arthritis and the glycosylation status of IgG. Clin Exp Immunol 89(3):434–438
Thompson SJ, Francis JN, Siew LK et al (1998) An immunodominant epitope from mycobacterial 65-kDa heat shock protein protects against pristane-induced arthritis. J Immunol 160(9):4628–4634
Van Den Berg WB (2009) Lessons from animal models of arthritis over the past decade. Arthritis Res Ther 11(5):250–259
Vidal SM, Epstein DJ, Malo D et al (1992) Identification and mapping of six microdissected genomic DNA probes to the proximal region of mouse chromosome 1. Genomics 14(1):32–37
Vincenti MP, Brinckerhoff CE (2002) Transcriptional regulation of collagenase (Mmp-1, Mmp-13) genes in arthritis: integration of complex signaling pathways for the recruitment of gene-specific transcription factors. Arthritis Res 4(3):157–164
Vigar ND, Cabrera WH, Araujo LM et al (2000) Pristane-induced arthritis in mice selected for maximal or minimal acute inflammatory reaction. Eur J Immunol 30(2):431–437
Vonk LA, Kragten AH, Dhert WJ et al (2014) Overexpression of Hsa-Mir-148a promotes cartilage production and inhibits cartilage degradation by osteoarthritic chondrocytes. Osteoarthr Cartil 22(1):145–153
Vorraro F, Galvan A, Cabrera WH et al (2010) Genetic control of IL-1 beta production and inflammatory response by the mouse Irm1 locus. J Immunol 185(3):1616–1621
Weis JJ, Mccracken BA, Ma Y et al (1999) Identification of quantitative trait loci governing arthritis severity and humoral responses in the murine model of Lyme disease. J Immunol 162(2):948–956
Wittmann J, Jäck HM (2011) MicroRNAs in rheumatoid arthritis: midget rnas with a giant impact. Ann Rheum Dis 70(suppl 1):i92–i96
Yoshitake F, Itoh S, Narita H et al (2008) Interleukin-6 directly inhibits osteoclast differentiation by suppressing receptor activator of nf-kappab signaling pathways. J Biol Chem 283(17):11535–11540
You S, Yoo SA, Choi S et al (2014) Identification of key regulators for the migration and invasion of rheumatoid synoviocytes through a systems approach. Proc Natl Acad Sci U S A 111(1):550–555
Yu X, Bauer K, Koczan D et al (2007) Combining global genome and transcriptome approaches to identify the candidate genes of small-effect quantitative trait loci in collagen-induced arthritis. Arthritis Res Ther 9(1):3–17
Zhang W, Shen X, Xie L et al (2015) MicroRNA-181b regulates endotoxin tolerance by targeting il-6 in macrophage raw264.7 cells. J Inflamm 12:18. https://doi.org/10.1186/s12950-015-0061-8
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ibañez, O.M., Jensen, J.R., De Franco, M. (2022). Transcriptome Profiling in Experimental Inflammatory Arthritis. In: Passos, G.A. (eds) Transcriptomics in Health and Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-87821-4_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-87821-4_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87820-7
Online ISBN: 978-3-030-87821-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)