Abstract
The second leading cause of mortality in the world is cardiovascular disease (CVD), causing 17 million deaths in 2013. CVD disproportionately affects low- and middle-income countries (LMIC), which account for 80% of these deaths. The use of ultrasound technology has been a mainstay in the medical field for formal diagnostic purposes for years and has recently received increased interest for point-of-care diagnostics and procedural guidance. Transesophageal echocardiography (TEE) is routinely used for diagnosis and monitoring during cardiac surgery, and transthoracic echocardiography (TTE) is increasingly used as a point-of-care diagnostic modality both in the perioperative setting and in critically ill patients. In recent years, there has been emergence of portable ultrasound devices that offer many of the functionalities of traditional ultrasound machines. These handheld portable ultrasound devices have been shown to be very effective as a diagnostic modality and are a promising technology for increasing adoption of ultrasound use in LMIC. Significant training and expertise is required to achieve a level of expertise needed to perform and interpret an echocardiographic examination. Traditional training with direct supervision of an experienced and certified practitioner is not practical for widespread adoption of echocardiography in LMIC. There is a range of simulators available in the market for replicating a TTE and TEE exams. These simulators give learners the added benefit of familiarizing themselves with echocardiography before application in a patient care setting. A variety of simulators are available in the market across various price points, each with its own benefits and limitations, from static simulation to 2D and 3D imaging, as well as AR capability. It is possible to develop curriculums that include simulators as part of the teaching to train learners in echocardiography. Such technology increases the number of possibilities for future applications and may help in the early diagnosis of deadly diseases such as RHD and CVD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anesthesia
- Cardiac surgery
- Curriculum
- Echocardiography
- Imaging
- Low-income countries
- Middle-income countries
- Simulators
- Training
- Technology
1 Introduction
The second leading cause of mortality in the world is cardiovascular disease (CVD), causing 17 million deaths in 2013. CVD disproportionately affects low- and middle-income countries (LMIC), which account for 80% of these deaths [1, 2]. Atherosclerotic diseases, including ischemic heart disease and stroke, are principal causes of death in Latin America, Eastern Europe, South Asia, East Asia, and North Africa and the Middle East [3,4,5,6,7,8]. Non-atherosclerotic diseases including rheumatic heart disease (RHD) and non-ischemic cardiomyopathy (NICM) are very prevalent in Southeast Asia and parts of South Asia [4, 9, 10]. RHD is a preventable disease that affects up to 40 million people worldwide [11]. It is endemic in impoverished children and young adults. Early diagnostic imaging is imperative in diagnosing and managing RHD and NICM, especially to prevent the deadly long-term consequences. The World Health Organization (WHO) published a report in 1998 that said 60% of the world does not have access to any diagnostic radiological services [12], however, even if imaging is available in many LMICs, marked disparities exist in utilization of such imaging and access is provided on a fee-for-service basis [2]. More than half of the installed equipment is not utilized due to a lack of maintenance or trained users. New paradigms must be developed to train healthcare providers in ultrasound imaging, especially for early detection of these morbid conditions, as training for and availability of technicians is nearly non-existent in LMICs [13].
The following is a discussion of the technology, availability, and utility as well as applicable content of simulation for training providers in LMIC to appropriately use transesophageal echocardiography (TEE) and transthoracic echocardiography (TTE) for diagnosis, treatment, and guidance during procedures while treating their patients.
2 Ultrasound
The use of ultrasound technology has been a mainstay in the medical field for formal diagnostic purposes for years but has recently received increased interest for point-of-care diagnostics and procedural guidance [14]. This increased interest is becoming formalized in medical training in the United States as multiple specialties incorporate curriculum changes to teach ultrasound techniques in residency programs. Surface ultrasound is regularly used to guide placement of peripheral and central intravenous lines, regional blocks and as a non-invasive monitor of cardio-pulmonary function. TEE is routinely used for diagnosis and monitoring during cardiac surgery, and TTE is increasingly used as a point-of-care diagnostic modality both in the perioperative setting and in critically ill patients. Initially, TEE was only used to capture images in patients who had suboptimal echo windows during TTE. However, the importance of TEE has increased considerably and has become an indispensable tool during cardiac valve surgery and in the diagnosis and management of life-threatening hemodynamic instability [15, 16]. In 1985, the WHO published a report concluding that there are “very real advantages to be gained from the use” of ultrasound for imaging in developing countries by noting its potential for “improved patient management and care of the individual” [17]. Despite the time that has passed, there has not been widespread adoption of echocardiography in LMIC. Training and skill are important barriers to adoption that can, at least partially, be overcome with robust simulation programs.
2.1 Point of Care Ultrasound (POCUS)
In recent years, there has been emergence of portable ultrasound devices that offer many of the functionalities of traditional ultrasound machines [18]. These devices can be used to perform a TTE and come with a portable display unit and probe that be used any time. These devices have a rugged design that can be easier to maintain compared to larger ultrasound workstations. Clinicians can carry around these portable devices very easily and incorporate this technology into their initial assessment and physical examination of a patient [19], and they are relatively less expensive than traditional ultrasound systems. Telecommunication over cloud-based platforms is also possible with these devices, allowing for remote peer evaluation and viewing of locally captured images. Manufacturers such as SonoQue (Yorba Linda, CA); Philips (Amsterdam, The Netherlands); TENS Pros (St. Louis, MO); and Butterfly Network, Inc (Guilford, CT) (Fig. 19.1) offer this functionality. Some limitations of these portable devices still exist—such as overheating with continuous use—but these devices can assist in performing a focused examination to identify acute pathologies, even if the image quality might be inferior to standalone ultrasound machines.
These handheld portable ultrasound devices have been shown to be very effective as a diagnostic modality. Studies have shown that these devices can be used to diagnose left ventricular hypertrophy and can then be used as an indicator for starting anti-hypertensive regimen [20]. RHD can also be screened through POCUS and multiple studies have shown it to be superior as a screening tool compared to cardiac auscultation alone [21,22,23]. POCUS has also been shown to have high diagnostic accuracy compared to comprehensive echocardiograms when evaluating ejection fraction, valvular regurgitation and wall motion according to two studies from Brazil [24, 25].
These advances in technology, and the demonstrated utility that comes with it, will lead to increased adoption and utilization of echocardiography in LMIC but require robust training and operator expertise prior to widespread use in clinical care.
2.2 Training
The WHO Ultrasound Manual states that in order to reliably interpret ultrasound scans, a physician requires at least 6 months of full-time training at a recognized academic center. They should also have at least 2–3 years of healthcare training [26]. The vast majority of personnel performing ultrasound scans in LMICs do not meet the abovementioned criteria to practice ultrasonography and have little or no formal training [13].
Significant training and expertise are required to achieve a level of expertise needed to perform and interpret an echocardiographic examination. Traditionally, training is performed under direct supervision of an experienced and certified practitioner. The learner is expected to appreciate the normal anatomic cardiac structures, and then differentiate the abnormal structures. The anatomy of heart must be learned from both the perspectives of TTE and TEE. The learner must familiarize themself with these alternative image orientations and mentally visualize the three-dimensional image of the heart from multiple two-dimensional image planes. Vertical and oblique plane imaging can make this very challenging. Following mastery of normal and abnormal anatomy, the learner is then taught to assess ventricular and valvular function. This formalized training is only available in major academic centers during dedicated fellowship training [27]. There is significant variation in exposure to ultrasound education for learners, and proficiency in POCUS is not a compulsory milestone [28]. Introducing ultrasound courses focused specifically on POCUS as part of the curriculum, however, is feasible and helps the learners improve their cognitive and technical skills. Training to perform an adequate TEE exam requires a substantial learning curve and multiple sessions to be fully competent. Use of simulators is a clear measure that can be implemented to help bridge this gap. Incorporating simulators as part of echocardiography training can suitably supplement the existing training methods to develop the necessary skills for performing echocardiography.
3 Role of Simulators
There is a range of simulators available in the market for replicating a TTE and TEE exams. These simulators give learners the added benefit of familiarizing themselves with echocardiography before application in a patient care setting. These simulators also give the learners the chance to practice multiple times without any time or patient safety constraints, which allows for individualized training and evaluation of competency. Simulators have high fidelity and help learners feel as if the procedure is being performed on humans due to anatomically accurate simulations and images. When choosing a simulator, one must consider price, hardware and software requirements, and capabilities. These simulators can then be integrated and adopted by an institution as part of a curriculum.
Below is a discussion of different simulators available in the market and how these can help medical professionals obtain essential echocardiography skills.
4 Static Simulation
There are simulators available in the markets that allow static simulation of the heart to perform a TTE or TEE. One such model available in the market called The Blue Phantom Model (CAE Healthcare) is designed to be compatible with ultrasound and aids in teaching echocardiography skills to learners [29]. It is made of durable rubber that is echogenic to allow for easy visualization using any ultrasound system with an appropriate transducer. The rubber is designed with a convex contour to allow realistic scanning and cannulation to more accurately mimic human tissue. The interior of the Blue Phantom Model houses an anatomically accurate heart model with precise corresponding atria, ventricles, appendages and vessels. This heart model can also be clearly seen with an identical translucent copy of the Blue Phantom Model. The total dimensions of the model are 10.5 × 5.3 × 5.7 inches. It features two ports: one of the ports is connected to tubing with a stopper that is used for filling and emptying fluid for to simulate pericardial effusions. The company produces a specific fluid called Red Ultrasound Refill Solution (BRS180-Red; CAE Healthcare) to replicate pericardial effusion that can be purchased separately. The second port is used to insert a TEE probe. The model also allows for actual needle punctures to be performed to better train for pericardial effusion drainage (Fig. 19.2).
4.1 Workflow
Learners are required to follow the same steps to acquire images from the Blue Phantom Model, as they would for standard ultrasound machines. This includes:
-
1.
Connecting an ultrasound machine to a power source.
-
2.
Initializing the probe and having the system ready for starting echocardiography.
-
3.
Entering “patient information” on the ultrasound machine.
-
4.
Inserting the TEE probe through the port in model with adequate lubrication.
-
5.
Positioning the probe at the upper esophageal, midesophageal, transgastric and deep transgastric windows accordingly.
-
6.
Visualize the image.
-
7.
This model allows for adjustment of depth, gain, harmonics, compression, and zoom on the ultrasound system for better image optimization.
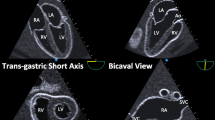
The TEE image in the Blue Phantom Model is visualized as a static image, devoid of any motion, with appropriately positioned intra-cardiac chambers and valves. The walls of the heart have appropriate thickness with well-defined endocardial and epicardial borders. The vena cavae, ascending aorta, and pulmonary artery can also be visualized. This simulator also allows the learners to practice various three-dimensional (3D) imaging modes in real time. All the images that are captured can be stored and reviewed (Fig. 19.3).
4.2 Limitations
The most significant limitation of the Blue Phantom Model is that it is static and it does not allow flow information to be visualized; therefore real valve motion and doppler flow profiled cannot be generated. The image quality is also not consistent throughout different TEE views. The variability could be due to differences in probe position and contact, use of lubricant material, or due to the orientation of the model in the gel suspension. However, by using more lubricant gel at the time of probe insertion and filling the pericardial cavity beforehand does improve the image quality.
5 Live TEE Simulation
Simulators designed for training of TEE and TTE have simplified the teaching of the complex process of echocardiography. One such simulator, called the HeartWorks Simulator, was developed at Heart Hospital in London UK, in collaboration with a graphics animation company (Glassworks, London, UK). The simulator comes with an external mannequin and a realistic TEE probe that learners can use to accurately visualize the anatomically correct model of the heart [27]. As the learners manipulate the probe, a digital image of the heart and the probe is displayed automatically on the computer screen in real time to give the learners an accurate understanding of their anatomic orientation. The internal and external anatomy of the heart is displayed. A Microsoft Windows based computer (Redmond, WA) with a suitable graphics card and adequate processing power and memory, is connected to the mannequin and the TEE probe via a standard USB port. The TEE probe allows for anteflexion, retroflexion, and left and right tilt with controls that mimic modern TEE probes. The mannequin houses the positioning sensors for the TEE probe for orientation in relation to the digital heart (Fig. 19.4).
5.1 Modes
This simulator comes with a number of modes that can help in teaching basics of echocardiography and anatomy. “Camera mode” allows the user to change the viewing angle of the heart through mouse control, allowing for a better understanding of the internal anatomy of the heart. The “Manipulator mode” allows the user to keep the camera angle constant, but the slice plane can be changed from multiple perspectives and angles. The “TEE mode” allows for a complete TEE exam to simulated by using the TEE probe, complete with the controls to anteflex and retroflex the probe, as well as advance and withdraw the probe in the mannequin. The digital probe on the computer screen automatically reproduces the probe manipulations, and at the same time, a three-dimensional (3D) image is generated in real time on the computer to give perspective to the learner and improve their skills. The teacher observing can assist the learner accordingly. The software on the computer also has the ability to digitally remove certain cardiac tissues according to the users’ interest and focus. The anatomic structures can be easily highlighted and linked to explanations via text (Figs. 19.5 and 19.6).
5.2 Limitations
The biggest limitation of this simulator is that it is expensive, and the initial cost may inhibit a more common uptake of this technology. It is available in varying configurations, however, which may reduce the cost. The simulator also does not allow Doppler functionality and the graphics and videos are not able to be saved for future reference.
6 3D TEE Simulator
A 3D-TEE simulator offers accurate views of cardiac physiologic and pathologic cardiac anatomy, while also providing real-time volumetric scanning, allowing learners to practice both qualitatively and quantitatively.
One such simulator is the Vimedix TEE/TTE simulator (CAE Healthcare, Montreal, Canada) that is capable of both 2D and 3D echocardiography. A computer is connected via standard USB port to a mannequin that includes a standard TEE probe, capable of all maneuvers of a standard probe. This mannequin houses the positioning sensors to allow the orientation of the TEE probe in relation to the digital heart. The mannequin is also capable of working with a TTE probe (Fig. 19.7).
This simulator is equipped with multiple modes that can help in teaching basics of 3D echocardiography and anatomy. The simulator is capable of a wide array of standard 3D echocardiography technology, including live narrow and wide sector imaging, single beat full volume imaging, orthogonal biplane imaging, multiplanar reconstruction from 3D datasets. This allows for the learner to familiarize themselves with the “knobology” and anatomy specific to 3D echocardiography. This is an expensive simulator that needs a large physical space to house the unit and it needs regular upkeep for maintenance. These limitations, as well as the advanced nature of 3D echocardiography, currently limit its applicability for LMICs.
7 Augmented Reality (AR)
Augmented Reality (AR) is an immersive technology that adds an artificial layer of computer-generated information over an actual real-world image, most commonly done through a headset. AR helps improve situational awareness and understanding by greatly enhancing spatial orientation [30]. It is most commonly used in the gaming industry or in the military, but its use is also increasing in the healthcare sector as it has shown promise. Healthcare related applications include visualization of subcutaneous veins, treatment of psychiatric disorders, displaying patient data using a head-mounted display during surgery, task training and procedure planning adjuncts.
AR can also be applied to echocardiographic imaging modalities such as TTE and TEE. Typically, the person performing a TTE or TEE has to undergo extensive training to understand the cardiac imaging that is presented as a two-dimensional (2D) cross-section via ultrasound technology. The operator is then expected to construct a mental picture of a 3D image of the anatomy for orientation. AR can be used instead to supplement the generated ultrasound image by overlaying the corresponding virtual anatomic perspective. This can be done, for example, by using an AR Headset such as Hololens (Microsoft, Redmond, WA) alongside a Vimedix TEE/TTE simulator (CAE Healthcare, Montreal, Canada). This has the potential to improve training and orientation for learners and reduce their learning curve to perform a TEE/TTE. Such kind of technology can then be incorporated as part of future didactics and custom tutorials for the learners to improve their understanding of the procedure.
7.1 Limitations
There are, however, limitations to AR Technology. The technology is nascent and, therefore can be expensive to buy and maintain, and these simulators have cross-compatibility issues to overcome. The AR headset has limited battery life with a limited field of view and prolonged use of an AR headset can also be associated with neck muscle fatigue.
8 Curricula for Application of Simulation Technology
In order to fully utilize the benefits of the aforementioned simulators, it is important to incorporate this technology to existing teaching curriculums in academic centers that focus on teaching the necessary skills in performing a TEE or TTE, in an effective and systematic manner. One study demonstrated a curriculum that integrated simulators to teach trainees over a period of four weeks [31]. This curriculum included multiple approaches to teaching, with clearly defined objectives for learning and instantaneous feedback for improvement. The first part of the curriculum was focused on topic specific web-based teaching modules orienting the learners on the fundamentals of echocardiography, probe positioning and orientation, and the visualization of different structures of the heart, such as right ventricle and tricuspid valve, aortic valve, mitral valve, left ventricle systolic function and wall motion assessment. This is done via various online lectures, quizzes, and practice exercises, primarily through visual learning. Learners could access this content at their own convenience at any time to appropriately cover the didactic materials, and a test is taken before and after undergoing these web-based modules to assess its effectiveness and measure the knowledge acquisition. The second part of the curriculum focused on teaching the learners through the TEE simulator, with sessions taking place two times a week. Expert attending physicians gave tutorials to the learners and then they were encouraged to reciprocate the skills obtained by practicing hands-on on the simulators. Instant feedback was then provided to the learners to correct their mistakes and improve proficiency. As part of this section of training, the facilitators also held focused discussions on review of real-world cases and scenarios in order to increase contextualization with clinical relevance (Fig. 19.8). This study, among others, demonstrates the effectiveness of simulation technology for learners in an academic setting. The curricula proposed could be easily adapted to suit practitioners in LMIC. The short period of time, web-based modules and online assessment lend themselves particularly well to remote or asynchronous teaching techniques. These advantages may serve to improve participation for learners from disparate geographical areas.
9 Future Applications
Multiple studies have shown the effectiveness of using simulators to teach echocardiography skills to learners, specifically TEE. All these studies have shown promising results by demonstrating that learners did better after undergoing simulator-based training compared to others who did not train on simulators before being tested [31,32,33]. It is possible to develop and implement a curriculum to teach echocardiography that is web-and-simulation-based, which could encourage more widespread adoption. Studies have also shown that learners who underwent simulation-based teaching, with no prior knowledge of echocardiography, performed significantly better than learners who underwent traditional didactic-based teaching or those who underwent hands-on training in the operating room. AR can be used to teach learners at multiple different sites at the same time. A single instructor can demonstrate the necessary skills using a simulator and then also evaluate and assess learners performing the same skills at remote locations, allowing greater outreach for teaching [30].
Measuring the time or number of errors in performing a task, is traditionally the basis on which successful completion of a task is assessed. It is possible to create integrated curriculum based on hands-on sessions on simulators and objectively assess echocardiography skills using hand motion metrics, including the number of rapid movements or transitions and the total length travelled by the TEE probe. This kinematic data can then be used to assess expertise [34]. These studies showed significant improvement in technical skills of learners who underwent simulation-based educational curriculum by analyzing the novice learners’ technical proficiency and comparing to an expert board-certified echocardiographer. Such objective analysis can also aid in identifying participants who need further training to improve their skills.
Echocardiography based teaching aimed at LMIC can use such technology available in the market with a perspective of significant upfront investment, but a very high return of investment in the future, as such technology can greatly help in training personnel in LMIC.
10 Conclusion
Proficiency in echocardiography is essential to correctly diagnose cardiovascular diseases. With the increased use and availability of ultrasound devices and machines, it is imperative that training modalities keep pace with technical advancements. This could lead to early diagnosis of deadly diseases such as RHD and other CVD and aid in the care of critically ill patients through proliferation of POCUS. A variety of simulators are available in the market across various price points, each with its own benefits and limitations, from static simulation to 2D and 3D imaging, as well as AR capability. It is possible to develop curricula that include simulators to train learners in echocardiography. Previously developed curricula have shown to improve cognitive and technical skills in echocardiography and may serve as the basis for more widespread adoption of echocardiography in LMIC.
Abbreviations
- 2D:
-
Two-dimensional
- 3D:
-
Three-dimensional
- AI:
-
Artificial Intelligence
- AR:
-
Augmented Reality
- CVD:
-
Cardiovascular Disease
- LMIC:
-
Low and Middle Income Countries
- NICM:
-
Non-ischemic cardiomyopathy
- OR:
-
Operating room
- POCUS:
-
Point of Care Ultrasound
- RHD:
-
Rheumatic Heart Disease
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
- WHO:
-
World Health Organization
References
Bowry ADK, Lewey J, Dugani SB, Choudhry NK. The burden of cardiovascular disease in low- and middle-income countries: epidemiology and management. Can J Cardiol. 2015;31(9):1151–9.
Vedanthan R, Choi BG, Baber U, Narula J, Fuster V. Bioimaging and subclinical cardiovascular disease in low- and middle-income countries. J Cardiovasc Transl Res. 2014;7(8):701–10.
Moran A. East Asia. Glob Heart. 2014;9(1):53–8.
Moran A. South Asia. Glob Heart. 2014;9(1):65–70.
Moran A. Central Europe. Glob Heart. 2014;9(1):71–6.
Moran A. Eastern Europe & Central Asia. Glob Heart. 2014;9(1):77–82.
Moran A. North Africa & Middle East. Glob Heart. 2014;9(1):17–22.
Moran A. Latin America & Caribbean. Glob Heart. 2014;9(1):35–40.
Moran A. Sub-Saharan Africa. Glob Heart. 2014;9(1):23–8.
Moran A. Southeast Asia. Glob Heart. 2014;9(1):59–64.
Peters F, Karthikeyan G, Abrams J, Muhwava L, Zühlke L. Rheumatic heart disease: current status of diagnosis and therapy. Cardiovasc Diagn Ther. 2020;10(2):305–15.
Who study group on training in diagnostic ultrasound: essentials PaS, world health organization. In: Training in diagnostic ultrasound: essentials, principles and standards: report of a WHO study group. Geneva: World Health Organization;1998.
LaGrone LN, Sadasivam V, Kushner AL, Groen RS. A review of training opportunities for ultrasonography in low and middle income countries. Trop Med Int Health. 2012;17(7):808–19.
Training in perioperative echocardiography. Time to think outside the box. J Am Soc Echocardiogr. 2016;29(7):A28–9.
Mahmood F, Christie A, Matyal R. Transesophageal echocardiography and noncardiac surgery. Semin Cardiothorac Vasc Anesth. 2008;12(4):265–89.
Practice guidelines for perioperative transesophageal echocardiography. A report by the American society of anesthesiologists and the society of cardiovascular anesthesiologists task force on transesophageal echocardiography. Anesthesiology. 1996;84(4):986–1006.
Countries WHOSGotFUoNITiD, world health organization. In:Future use of new imaging technologies in developing countries : report of a WHO scientific group [meeting held in Geneva from 24 September to 1 October 1984]. Geneva: World Health Organization;1985.
Becker DM, Tafoya CA, Becker SL, Kruger GH, Tafoya MJ, Becker TK. The use of portable ultrasound devices in low- and middle-income countries: a systematic review of the literature. Trop Med Int Health. 2016;21(3):294–311.
Wright J, Noriega O, Ho H. The application of hand-held ultrasound scanner in teaching of telemedicine and rural medicine. Donald Sch J Ultrasound Obstet & Gynecol. 2014;8:87–91.
Kobal SL, Czer LSC, Czer PC, Feldsher Z, Hamilton R, Siegel RJ. Making an impossible mission possible. Chest. 2004;125(1):293–6.
Godown J, Lu JC, Beaton A, et al. Handheld echocardiography versus auscultation for detection of rheumatic heart disease. Pediatrics. 2015;135(4):e939-944.
Lu JC, Sable C, Ensing GJ, et al. Simplified rheumatic heart disease screening criteria for handheld echocardiography. J Am Soc Echocardiogr. 2015;28(4):463–9.
Beaton A, Aliku T, Okello E, et al. The utility of handheld echocardiography for early diagnosis of rheumatic heart disease. J Am Soc Echocardiogr. 2014;27(1):42–9.
Siqueira VN, Mancuso FJ, Campos O, De Paola AA, Carvalho AC, Moises VA. Training program for cardiology residents to perform focused cardiac ultrasound examination with portable device. Echocardiography. 2015;32(10):1455–62.
Tsutsui JM, Maciel RR, Costa JM, Andrade JL, Ramires JF, Mathias W Jr. Hand-carried ultrasound performed at bedside in cardiology inpatient setting—a comparative study with comprehensive echocardiography. Cardiovasc Ultrasound. 2004;2:24.
Buscarini E, Lutz H, Mirk P. World health organization, world federation for ultrasound in medicine and B. In: Elisabetta B, Harald L, Paoletta M, editors. Manual of diagnostic ultrasound, 2nd ed. Geneva: World Health Organization;2013.
Bose R, Matyal R, Panzica P, et al. Transesophageal echocardiography simulator: a new learning tool. J Cardiothorac Vasc Anesth. 2009;23(4):544–8.
Education ACfGM. ACGME program requirements for graduate medical education in anesthesiology;2019.
Mahboobi S, Mahmood F, Bortman J, et al. Simulator-based training of workflow in echocardiography. J Cardiothorac Vasc Anesth. 2019;33(6):1533–9.
Mahmood F, Mahmood E, Dorfman RG, et al. Augmented Reality and Ultrasound Education: Initial Experience. J Cardiothorac Vasc Anesth. 2018;32(3):1363–7.
Mitchell JD, Mahmood F, Bose R, Hess PE, Wong V, Matyal R. Novel, multimodal approach for basic transesophageal echocardiographic teaching. J Cardiothorac Vasc Anesth. 2014;28(3):800–9.
Weber U, Zapletal B, Base E, Hambrusch M, Ristl R, Mora B. Resident performance in basic perioperative transesophageal echocardiography: comparing 3 teaching methods in a randomized controlled trial. Med (Balt). 2019;98(36):e17072.
Bose RR, Matyal R, Warraich HJ, et al. Utility of a transesophageal echocardiographic simulator as a teaching tool. J Cardiothorac Vasc Anesth. 2011;25(2):212–5.
Matyal R, Mitchell JD, Hess PE, et al. Simulator-based transesophageal echocardiographic training with motion analysis: a curriculum-based approach. Anesthesiology. 2014;121(2):389–99.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Quraishi, I., Mahmood, F., Khabbaz, K., Kpodonu, J., Robitaille, M.J. (2022). Utility of Simulation in Transthoracic and Transesophageal Echocardiogram-Based Training of a Cardiovascular Workforce in Low and Middle-Income Countries (LMIC). In: Kpodonu, J. (eds) Global Cardiac Surgery Capacity Development in Low and Middle Income Countries. Sustainable Development Goals Series. Springer, Cham. https://doi.org/10.1007/978-3-030-83864-5_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-83864-5_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-83863-8
Online ISBN: 978-3-030-83864-5
eBook Packages: MedicineMedicine (R0)