Abstract
Dietary fat is a macronutrient comprised of many different lipids and fatty acids some of which are essential nutrients. The fatty acid classes are saturated (SFA), monounsaturated (MUFA), polyunsaturated (PUFA) (omega-6 and omega-3 fatty acids), and trans (TFA). Unsaturated fatty acids typically exist in the cis configuration and differ structurally based on chain length and the number of carbon-to-carbon double bonds. Unsaturated fatty acids also exist in trans isomer configurations, which occur as the result of partial hydrogenation (via industrial synthesis or by naturally occurring biohydrogenation in ruminant animals). The different fatty acid classes have varying effects on lipids and lipoproteins that affect risk of cardiovascular disease (CVD). All TFA increase CVD risk, and, as a result, industrially produced TFA have been banned in the US food supply. SFA increase low-density lipoprotein-cholesterol (LDL-C) and increase CVD risk. Replacement of SFA with unsaturated fatty acids or carbohydrates (preferably whole grains) reduces LDL-C and CVD risk. Dietary guidelines recommend a healthy dietary pattern with <10% total calories from SFA, which should be achieved by replacing SFA with unsaturated fat or carbohydrate from whole grains. The fat content of the diet will vary based on the replacement macronutrient for SFA.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Fatty acids (FAs) differ by the structure of their hydrocarbon chain containing no double bonds (saturated, SFA), one double bond (monounsaturated, MUFA), or multiple double bonds (polyunsaturated, PUFA).
-
Essential fatty acids (EFA) cannot be synthesized by human beings. These are PUFA (omega-6 and omega-3 fatty acids) and must be consumed in the diet or taken as a supplement. These fatty acids decrease risk of heart disease and other chronic conditions.
-
Some foods contain trans-fatty acids (TFA), naturally occurring and industrially produced. The process of partial hydrogenation of unsaturated fatty acids (PHOs) creates TFA. TFA increases risk of heart disease.
-
Most SFA increase low-density lipoprotein-cholesterol (LDL-C), a causal factor for atherosclerotic cardiovascular disease.
-
When MUFA and PUFA replace SFA in the diet, lipids/lipoproteins are improved, which reduces the risk of CVD.
-
Recommended healthy eating patterns are low in SFA and higher in unsaturated fat and/or carbohydrate from whole grains, although will vary in total fat based on the macronutrient substituted for SFA. Importantly, a healthy eating pattern can be individualized to accommodate dietary preferences as a strategy to promote adherence.
Introduction
The Internet is littered with misinformation about macronutrients, foods, and diets. This has created many misconceptions about dietary fat and how it impacts health. In addition, there is much confusion about including foods containing fat in healthy diets. Many patients obtain their health information from non-evidence-based sources and are misinformed about dietary recommendations, in general, and guidelines for fat intake. Typical questions healthcare professionals ask about dietary fats are as follows:
-
What are the bad fats?
-
What are the good fats?
-
Can a very low-fat diet be healthy?
-
Can a high-fat diet be healthy?
Types of Fat
General Characteristics
Fatty acids (FAs) are organic molecules composed of a carboxyl group, methyl group, and a hydrocarbon chain of varying lengths. FAs can be saturated (-CH2-CH2-), monounsaturated (-CH2-CH=CH-CH2-), and polyunsaturated containing more than one double bond. The carbon-to-carbon bonds are in the cis-formation (almost always), but food processing can create carbon-to-carbon bonds in the trans-formation. Saturated (SFA), monounsaturated (MUFA), and polyunsaturated (PUFA) fatty acids are present in foods primarily as triglycerides.
Saturated Fatty Acids
Dietary sources of SFA include red meat, full-fat dairy products, fish, poultry, and all fats and oils, with tropical oils (coconut and palm and palm kernel) being the highest. SFA are solid at room temperature. The structural features of SFA are important for maintaining the structure/function of plasma membranes and lipid bilayers. Common SFA found in foods are stearic (18:0), palmitic (16:0), myristic (14:0), and lauric (12:0) acid, with palmitic acid being the major SFA in the Western diet.
Unsaturated Fatty Acids
Dietary sources of MUFA and PUFA are mainly plant-based, although they are also present in animal sources. MUFA are found in many plant foods such as nuts, seeds, and liquid oils, as well as animal foods, such as meats, dairy products, and eggs. The most common MUFA is oleic acid (18:1, n-9). Foods rich in PUFA are safflower, corn, and soybean oils as well as nuts and fish/seafood. The most common PUFA are linoleic acid (18:2, n-6) and alpha-linolenic acid (18:3, n-3). Longer-chain PUFA, i.e., eicosapentaenoic acid (EPA [20:5, n-3]) and docosahexaenoic acid (DHA [22:6, n-3]), are present in lesser amounts in the diet. Unlike SFA, MUFA and PUFA are liquid at room temperature. Essential fatty acids are linoleic acid (an omega-6, or n-6, fatty acid) and alpha-linolenic acid (an omega-3, or n-3, fatty acid).
N-6 and N-3 Fatty Acids
The classification of either n-3 or n-6 is based on the first double bond being on the 3rd (n-3) or 6th (n-6) carbon from the methyl terminus. The common long-chain n-3 FAs are EPA and DHA. The most abundant n-6 FA is linoleic acid (LA) and the most prevalent n-3 fatty acid is alpha-linolenic acid (ALA).
N-3 and n-6 FAs have many health benefits (see Dietary fat and health). Fish and shellfish, particularly fatty cold-water species, are rich in EPA and DHA (salmon, albacore tuna, mackerel, and oysters). Fish oil supplements are a source of EPA and DHA. Non-animal sources of DHA and EPA are seaweed and algae. ALA is found primarily in plant-based foods like walnuts, flaxseeds, and chia seeds as well as canola oil and soybean oil. Sources of LA are nuts, seeds, and most vegetable/liquid oils.
Sterols, Stanols, and Cholesterol
Sterols , also referred to as steroid alcohols, are comprised of a four-ring steroid structure, a double bond, and one or more hydroxyl groups [1]. Stanols are nearly identical, but the four-ring steroid structure is saturated. The majority of cholesterol in the body is synthesized in the liver and is an integral component of plasma membranes as well as steroid hormones (i.e., testosterone and estrogen) and cholecalciferol (vitamin D) synthesis. Cholesterol is found in animal foods like eggs, shrimp and other shellfish, and organ meats. Phytosterols (both sterols and stanols) are found in plant cell membranes. Structurally similar to cholesterol, they block the absorption of dietary cholesterol in the intestine.
Trans-Fatty Acids
Most unsaturated fatty acids (UFA) occur naturally in the cis configuration, but some trans-fatty acids (TFA) are formed by biohydrogenation in ruminant animals. TFA are also produced by partial hydrogenation of vegetable oils. This creates a trans isomer that solidifies the vegetable oil at room temperature. This process prevents PUFA oxidation that increases the shelf life of processed foods. In response to the many adverse health effects of TFA, the FDA banned adding partially hydrogenated oils (PHOs) (that contain TFA) to any processed foods after June 2018 (see Dietary fat and health).
Triacylglycerols
Triacylglycerols (TAGs) or triglycerides are comprised of a glycerol backbone with three FAs (SFA, MUFA, or PUFA) attached via ester bonds [1]. TAGs make up approximately 95% of dietary fat [1]. During fat digestion lingual, gastric, and pancreatic lipases cleave the FA into diacylglycerols or monoacylglycerols for absorption into the enterocyte. These can be repackaged into TAGs and assembled into chylomicrons for transport in the plasma to target tissues such as the muscle and adipose tissue where they can be metabolized or stored.
Circulating Lipoproteins
Lipoproteins transport the bulk of dietary lipids through the circulation to target tissues. The hydrophobic core of lipoproteins contains triglycerides and cholesteryl esters, and the outer bilayer membrane is made up of phospholipids, free cholesterol, and protein molecules (apolipoproteins), with the different lipoprotein classes having one or more apolipoproteins. Lipoprotein classes are defined by their density, size, and characteristic constituent apolipoprotein(s). The key lipid constituents that affect CVD risk are TAG and cholesterol, which are transported in the plasma principally in chylomicrons and very low-density lipoproteins (specifically TAG), and LDL and HDL (specifically cholesterol). An elevated TAG level increases risk for CVD, and elevated cholesterol carried in LDL increases CVD risk whereas a high HDL-C decreases risk.
Chylomicrons are produced postprandially in the intestine as a vehicle for dietary fat absorption and transport. The peripheral tissues (cardiac, skeletal, adipose, etc.) remove TAGs from chylomicrons resulting in chylomicron remnants (CR), which are taken up by the liver [2]. Hepatocytes produce TAG-rich very-low-density lipoproteins (VLDL), which contain Apo B-100 as their main structural apolipoprotein. VLDL transports TAGs to target tissues for storage and energy utilization. VLDL are converted to cholesteryl ester-rich intermediate-density lipoproteins (IDL) and low-density lipoproteins (i.e., LDL-C) via hydrolysis of triglycerides by lipoprotein lipase and hepatic lipase. IDL and LDL are smaller than VLDL and have a greater proportion of cholesterol and protein because TAGs have been removed by peripheral tissues.
Low-density lipoprotein cholesterol (LDL-C) is the primary transporter of cholesterol in the body, and its major structural apolipoprotein is Apo B-100, the ligand for hepatic LDL receptor-mediated LDL clearance. LDL particles range in size and density, which affect their function. All LDL-C are atherogenic; however, the LDL particle size affects the susceptibility and likelihood of the particle becoming trapped in the arterial wall [3]. Compared to larger LDL particles, small-dense LDL particles bind more avidly to glycosaminoglycans in the artery wall where they are taken up into the subintimal space and are more likely to be trapped. All LDL particles that are trapped in the artery wall release cholesterol and promote atherogenesis. Despite more small, dense LDL being trapped, more cholesterol is released by each larger LDL particle (despite fewer being trapped). Thus, large and small LDL particles cause similar vessel wall injury because large LDL particles release more cholesterol per particle, while small LDL particles contain less cholesterol and more particles are trapped so the net atherogenic effects are equal. Small-dense LDL particles are potentially more susceptible to oxidation, and oxidized LDL-C may bind to scavenger receptors on macrophages thereby promoting atherosclerosis [2, 4]. Therefore, all LDL-C (i.e., all LDL regardless of particle size) are considered to be an independent causal risk factor for coronary artery disease [5].
High-density lipoprotein-cholesterol (HDL-C) is also comprised of cholesterol and phospholipids and the main structural protein is Apo A-1. HDL particles have several anti-atherogenic properties. Most notably, HDL particles remove cholesterol from cells and tissues and deliver it to the liver for excretion by two different pathways. First, through a process of reverse cholesterol transport, HDL removes cholesterol from macrophages thereby preventing foam cell formation and atherogenesis. Another pathway of cholesterol transport to the liver by HDL is via its cholesteryl ester exchange for TAG from VLDL and LDL by cholesteryl ester transfer protein (CETP) followed by receptor-mediated hepatic LDL (and cholesteryl ester) uptake. Other anti-atherogenic properties of HDL include reducing inflammation, LDL oxidation, and thrombosis formation (by inhibiting coagulation factors), as well as inducing endothelium-dependent vasodilation [6].
There is a robust evidence base from epidemiological studies, clinical trials, animal studies, and in vitro experiments that HDL-C is cardioprotective and is inversely associated with cardiovascular morbidity and mortality [5, 7]. However, there is some evidence that not all HDL particles confer protection against CVD. HDL is a heterogeneous particle; subspecies contain apolipoprotein E and or apolipoprotein CIII. Interestingly, HDL particles that contain apolipoprotein E promote reverse cholesterol transport, whereas the presence of apolipoprotein C III abolishes these effects [8]. Further research is needed to understand which HDL particles confer the greatest benefits against CVD and how these can be increased with lifestyle and pharmacologic interventions. To date, the CETP inhibitor drugs that have increased HDL-C markedly have not demonstrated cardiovascular benefits without side effects. Therefore , despite considerable initial promise, CETP inhibition provides insufficient cardiovascular benefit for routine use [9].
Non-high-density lipoprotein-cholesterol (non-HDL-C) is calculated by subtracting serum HDL-C from total cholesterol and is an estimate of all cholesterol and triglycerides present in chylomicrons, CR, VLDL, IDL, and LDL-C [10]. Thus, non-HDL-C includes all atherogenic cholesterol in contrast to LDL-C measurement, which only accounts for the cholesterol contained in the LDL particles (roughly 75% of cholesterol carried by non-HDL-C). Moreover, LDL-C is usually calculated, not directly measured, and therefore may not provide the most accurate measure of atherogenic cholesterol. Finally, non-HDL-C is more strongly associated with ASCVD risk compared to LDL-C [11].
Dietary Fat and Health
Dietary fat, one of the three macronutrients, is necessary for survival. The composition of our dietary fat has specific effects on circulating lipoproteins . Different FAs can be associated with both health benefits and adverse health outcomes. Specific FAs elicit changes in circulating lipids/lipoproteins, and long-term consumption of certain FAs increases risk of developing cardiometabolic diseases. Diets containing a greater percentage of SFA are associated with increased risk of CVD, diabetes, obesity, metabolic syndrome, and non-alcoholic fatty liver disease [12,13,14]; unsaturated fatty acids, in contrast, confer many health benefits.
When MUFA/PUFA are substituted for SFA, improvements in lipids/lipoproteins and vascular health are observed [14]. A diet containing a greater proportion, or ratio, of MUFA/PUFA:SFA is associated with reduced risk of CHD, metabolic syndrome, and hyperglycemia [15]. Additionally, n-3 PUFA, notably, marine-derived n-3 PUFA, have unique cardioprotective benefits, which has led to extensive research and the development of pharmaceuticals to treat specific diseases.
Trans-Fatty Acids
Although there were concerns about the negative health consequences of TFA in the 1980s, it was not until 1990 that Mensink and Katan reported that TFA increased LDL-C and decreased HDL-C in healthy subjects [16]. A subsequent meta-analysis of 12 controlled trials confirmed these findings reporting adverse effects of TFA on both LDL-C and HDL-C, thereby increasing risk of CHD [17].
The pooled relative risk from two observational studies showed a 2% increase in calories from TFA was associated with a 23% increased incidence of CHD [17]. A more recent dose-response meta-analysis of cohort studies estimated that the risk of CVD was increased 16% for each 2% increase in daily energy from TFA [18]. Collectively, the epidemiological and clinical research showing that TFA increased CHD risk led first to food labeling guidelines by the Food and Drug Administration, then removal of the Generally Recognized as Safe (GRAS) status for partially hydrogenated oils, and finally a ban on their addition to foods [19]. In the United States, consumption of TFA significantly decreased from 2.6% of total energy in the 1990s to 1.1% of total energy in the late 2000s, and serum TFA levels declined more than 50% from 2000 to 2009 [20, 21].
SFA/MUFA/PUFA
Current guidelines recommend consuming <10% of calories from SFA due to their adverse effects on lipoproteins (from clinical trial evidence) and associations with CVD (from epidemiological studies) [22, 23]. The 2020 Dietary Guidelines Advisory Committee concluded that there is strong evidence to support the replacement of SFA with PUFA based on consistent findings demonstrating risk reduction for both CHD events and CVD mortality [24]. Clinical trials assessing the effects of SFA on serum lipoproteins consistently show increases in LDL-C and HDL-C [25, 26]. Over the last few decades, epidemiological studies evaluating the relationship between dietary SFA and cardiometabolic health have reported inconsistent findings, which are largely explained by the statistical methods used and whether the replacement macronutrient was considered [27].
An epidemiological study beginning in the late 1950s showed a positive relationship between dietary SFA and heart disease leading to the hypothesis that SFA causes cardiovascular disease [28]. Zhu and colleagues conducted a dose-response meta-analysis on dietary FA and CVD in cohort studies and determined SFA intake was not associated with CVD [18]. However, this analysis only examined the relationship between SFA and CVD without assessing the replacement nutrient for SFA, which was likely refined carbohydrates (CHO) based on data about usual American consumption patterns. In a prospective cohort analysis, of over 126,000 US adults followed for up to 32 years, isocaloric replacement of 5% of energy from SFA with either PUFA (predominate dietary source is n-6) or MUFA was associated with a reduction in risk of total mortality by 27% and 13%, respectively. Similarly, replacing 5% of energy with unsaturated fatty acids (both PUFA and MUFA) reduced CVD mortality by 20% [29]. In addition, replacement of 5% of energy from SFA with whole grain CHO, MUFA , or PUFA was associated with a 9, 15, and 25% reduced risk of CHD, respectively [30].
In alignment with epidemiological findings, a recent Cochrane systematic review of 15 clinical studies, including over 59,000 participants, found that lowering SFA intake, regardless of the replacement macronutrient (PUFA, MUFA , or CHO), reduced combined cardiovascular events (cardiovascular death, cardiovascular morbidity, and unplanned cardiovascular interventions) risk by 21% [31]. However, there was not a significantly lower risk of all-cause mortality, cardiovascular mortality, or any of the secondary outcomes; findings are likely explained by the lack of statistical power due to the insufficient number of events and relatively short duration of follow-up.
Clinical trial evidence demonstrates that replacing SFA with MUFA, PUFA , or CHO significantly reduces LDL-C. Replacing 1% of dietary energy from SFA with the same percentage of energy from PUFA, MUFA, and CHO is estimated to lower LDL-C by 2.1, 1.6, and 1.3 mg/dL, respectively [32]. Whole grain CHO sources lower LDL-C more than refined grains [33]. A meta-analysis of randomized controlled trials showed that replacing SFA with whole grains, compared to refined grains, led to a greater reduction (3.5 mg/dL) in LDL-C [34].
Full-fat dairy products are a rich source of SFA with dairy fat being comprised of nearly 60% SFA (an 8-ounce glass of whole milk contains 8 g fat and 5 g is SFA). Dairy fat-derived SFA may not have the same effect on circulating lipoproteins as other animal-based SFA. Observational data suggest that dairy fat containing SFA is not associated with increased risk of CVD [35]. However, macronutrient replacement analyses show that CVD risk is reduced when MUFA , PUFA , and whole grains are consumed in place of dairy fat-derived SFA. Interestingly, a meta-analysis of three cohorts estimated that the replacement of 5% energy from dairy fat with equal energy from other animal fat increased CVD risk by 6% [35]. Dairy fat-derived SFA increased LDL-C less than other animal fats containing SFA; however, dairy fat-derived SFA are more atherogenic than UFA [35, 36]. The findings described here indicate that dairy fats pose some risk of CVD, but this is less than that associated with other animal fats containing SFA . For that reason, it is recommended that intake of dairy foods should be fat-free, low-fat dairy products.
N-3 Fatty Acids (ALA, EPA, and DHA)
Large, randomized controlled trials of prescription EPA + DHA and/or EPA (840–4000 mg/day) show reduced risk of CVD in healthy individuals and those with diabetes or elevated triglycerides (135–499 mg/dL) [37]. Two trials, VITAL and ASCEND, evaluated EPA + DHA for primary prevention of CVD and did not find a significant reduction in the primary endpoints (combination of coronary and ischemic outcomes). It is important to note, however, that in the VITAL trial, 460 mg of EPA + 380 mg DHA significantly reduced fatal (50%) and nonfatal heart attacks (28%) and in the ASCEND trial, 465 mg of EPA + 375 mg DHA resulted in a 19% reduction in CVD death, each of these being secondary endpoints [38, 39]. In VITAL, individuals consuming 1 ½ servings of fish per week at baseline had a 19% reduction in major cardiovascular events, while those with a baseline fish consumption greater than 1 ½ servings/week did not have a significant reduction in cardiovascular events [38]. The REDUCE-IT trial evaluated 4 g/day (2 g two times/day) of a purified form of EPA (icosapent ethyl) for secondary prevention of CVD in statin-treated individuals with elevated triglycerides. There was a 25% reduction in the primary endpoint, a composite of unstable angina, nonfatal stroke, nonfatal heart attack, and CV death, compared to the placebo group [40]. A recent meta-analysis of 13 trials (including VITAL, ASCEND, and REDUCE-IT) found a dose-response effect of marine-based n-3 on reducing risk of total CVD, CVD death, myocardial infarction, and total CHD [41]. Collectively , these studies demonstrate the importance of the n-3 fatty acids, EPA + DHA, for primary prevention of CHD and underscore the need to increase intake of these fatty acids in the population. There are also important benefits of a prescription dose of icosapent ethyl for secondary prevention of CVD, excluding stroke.
The 2020–2025 Dietary Guidelines for Americans recommend consuming 8 ounces of seafood per week, which provides approximately 250 mg EPA+DHA/day [23, 42]. The AHA recommends 1 to 2 servings (3.5 oz/sv) of fish per week, with emphasis on fatty fish [42]. If recommendations for n-3 intake cannot be achieved from food sources , an over-the-counter supplement may be considered in consultation with a healthcare provider. Over-the-counter supplements are not regulated by the Food and Drug Administration but are typically safe although sometimes the quantity of EPA/DHA in the product falls short of what is listed on the label.
Observational studies demonstrate a moderately lower risk for CVD with increased alpha-linolenic acid (ALA) consumption, but the relationship is not as consistent or strong as for EPA and DHA [43]. However, a meta-analysis of five cohort studies estimated that a 1 g/day increase in ALA was associated with a 10% reduction in CHD death, and a systematic review of RCTs reported that a higher intake of ALA was associated with a 5–9% reduction in CVD, although this was nonsignificant [43, 44].
Dietary Patterns
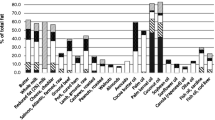
The focus of this chapter is on the effects of individual FAs and FA classes on circulating lipoproteins as well as overall health. However, foods contain a mixture of different fatty acids in varying proportions and generally have a predominant fatty acid class. As such, the focus of current dietary recommendations is on food-based healthy eating patterns. The 2020–2025 Dietary Guidelines for Americans recommend a healthy US style, a healthy Mediterranean style, and a healthy vegetarian/vegan style eating pattern [23]. In addition, the Dietary Approaches to Stop Hypertension (DASH) eating pattern also is recommended by many health organizations [45]. These dietary patterns are all low in SFA (<10% kcal), sodium, and added sugars and emphasize fruits, vegetables, nuts, seeds, legumes, whole grains, plant protein or lean/low-fat unprocessed animal protein, and liquid oils. In addition, these dietary patterns limit SFA by including MUFA/PUFA or fiber-rich whole grain CHO foods in place of food sources of SFA thereby affecting the total fat content of the diet. Although the total fat content of these dietary patterns can vary depending on the replacement macronutrient, they nonetheless align with the current dietary reference intake (DRI) for total fat (20–35% of total calories).
The fat content of many commonly consumed dietary patterns exists on a spectrum ranging from very-low fat (Ornish diet: <10% of total calories), low fat (10–20% of total calories), moderate fat (20–35% of total calories), and high/higher-fat (35–70% of total calories) to very-high fat (keto diet: >70% of calories from fat) diets. The topic of how low-carbohydrate diets influence plasma lipid profiles is discussed in further detail in Chap. 18. Clinical trials of these dietary patterns show that the effects on lipids/lipoproteins generally reflect their fatty acid profile (see Dietary fat and health). The effects of fatty acids on lipids and lipoproteins are due to their quantitative contribution on an energy basis in the diet. The key is for SFA to be low, and as total fat increases in the diet, the emphasis should be on unsaturated fat. As a result, all healthy dietary patterns, defined as meeting nutrient and food-based recommendations, provide <10% of calories from SFA, regardless of total fat content. Therefore, healthy lower-fat diets are higher in fiber-rich whole grain CHO, while healthy higher-fat diets are higher in MUFA and PUFA.
Summary
Healthy eating patterns meet food-based dietary guidelines, achieve nutrient adequacy, and meet recommendations for SFA (<10% of calories), sodium, and added sugars. A healthy eating pattern can vary in total fat, which depends largely on the differences in the amounts of unsaturated fatty acids and CHO that are substituted for SFA. The evidence that supports recommendations for SFA is based on the well-documented adverse effects of SFA on LDL-C and CVD risk and beneficial effects of unsaturated fats and CHO from whole grains. The core precept of contemporary dietary guidance specific to fatty acids is to replace SFA with PUFA, MUFA, or CHO (from whole grains) to decrease CVD risk.
References
Gropper SS, Smith JL. Advanced nutrition and human metabolism. Boston: Cengage Learning; 2012.
Cooper AD. Hepatic uptake of chylomicron remnants. J Lipid Res. 1997;38:2173–92.
Sniderman AD, Thanassoulis G, Glavinovic T, Navar AM, Pencina M, Catapano A, Ference BA. Apolipoprotein B particles and cardiovascular disease: a narrative review. JAMA Cardiol. 2019;4:1287–95.
Fan J, Liu Y, Yin S, Chen N, Bai X, Ke Q, Shen J, Xia M. Small dense LDL cholesterol is associated with metabolic syndrome traits independently of obesity and inflammation. Nutr Metab (Lond). 2019;16:7.
Marques LR, Diniz TA, Antunes BM, Rossi FE, Caperuto EC, Lira FS, Gonçalves DC. Reverse cholesterol transport: molecular mechanisms and the non-medical approach to enhance HDL cholesterol. Front Physiol. 2018;9:526.
Linton MF, Yancey PG, Davies SS, Jerome WG, Linton EF, Song WL, et al. The role of lipids and lipoproteins in atherosclerosis. Endotext. MDText. com, Inc; 2019.
Ali KM, Wonnerth A, Huber K, Wojta J. Cardiovascular disease risk reduction by raising HDL cholesterol–current therapies and future opportunities. Br J Pharmacol. 2012;167:1177–94.
Morton AM, Koch M, Mendivil CO, Furtado JD, Tjønneland A, Overvad K, et al. Apolipoproteins E and CIII interact to regulate HDL metabolism and coronary heart disease risk. JCI Insight. 2018;3:e98045.
Armitage J, Holmes MV, Preiss D. Cholesteryl ester transfer protein inhibition for preventing cardiovascular events: JACC review topic of the week. J Am Coll Cardiol. 2019;73:477–87.
Liu J, Sempos C, Donahue RP, Dorn J, Trevisan M, Grundy SM. Joint distribution of non-HDL and LDL cholesterol and coronary heart disease risk prediction among individuals with and without diabetes. Diabetes Care. 2005;28:1916–21.
Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 1-full report. J Clin Lipidol. 2015;9:129–69.
Raatz SK, Conrad Z, Johnson LK, Picklo MJ, Jahns L. Relationship of the reported intakes of fat and fatty acids to body weight in US adults. Nutrients. 2017;9:438.
Luukkonen PK, Sädevirta S, Zhou Y, Kayser B, Ali A, Ahonen L, et al. Saturated fat is more metabolically harmful for the human liver than unsaturated fat or simple sugars. Diabetes Care. 2018;41:1732–9.
Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136:e1–23.
Julibert A, del Bibiloni MM, Bouzas C, Martínez-González MÁ, Salas-Salvadó J, Corella D, et al. Total and subtypes of dietary fat intake and its association with components of the metabolic syndrome in a Mediterranean population at high cardiovascular risk. Nutrients. 2019;11:1493.
Mensink RP, Katan MB. Effect of dietary trans fatty acids on high-density and low-density lipoprotein cholesterol levels in healthy subjects. N Engl J Med. 1990;323:439–45.
Mozaffarian D, Katan MB, Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and cardiovascular disease. N Engl J Med. 2006;354:1601–13.
Zhu Y, Bo Y, Liu Y. Dietary total fat, fatty acids intake, and risk of cardiovascular disease: a dose-response meta-analysis of cohort studies. Lipids Health Dis. 2019;18:91.
Li C. Global surveillance of trans-fatty acids. Prev Chronic Dis. 2019;16:E147.
Vesper HW, Kuiper HC, Mirel LB, Johnson CL, Pirkle JL. Levels of plasma trans-fatty acids in non-Hispanic white adults in the United States in 2000 and 2009. JAMA. 2012;307:562–3.
Wanders AJ, Zock PL, Brouwer IA. Trans fat intake and its dietary sources in general populations worldwide: a systematic review. Nutrients. 2017;9:840.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;74:e177–232.
U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020-2025. 9th Edition. December 2020. Available at DietaryGuidelines.gov.
Snetselaar L, Bailey R, Sabate J, Van Horn L. 2020 Dietary Guidelines Advisory Committee: Dietary Fats and Seafood Subcommittee. 2020.
Baum SJ, Kris-Etherton PM, Willett WC, Lichtenstein AH, Rudel LL, Maki KC, et al. Fatty acids in cardiovascular health and disease: a comprehensive update. J Clin Lipidol. 2012;6:216–34.
Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Saturated fatty acids and risk of coronary heart disease: modulation by replacement nutrients. Curr Atheroscler Rep. 2010;12:384–90.
Siri-Tarino PW, Sun Q, Hu FB, Krauss RM. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J Clin Nutr. 2010;91:535–46.
Keys A. Coronary heart disease in seven countries. Circulation. 1970;41:186–95.
Wang DD, Li Y, Chiuve SE, Stampfer MJ, Manson JE, Rimm EB, et al. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176:1134–45.
Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, et al. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol. 2015;66:1538–48.
Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2020 May 19;5(5):CD011737. https://doi.org/10.1002/14651858.CD011737.pub2.
Mensink RP. Effects of saturated fatty acids on serum lipids and lipoproteins: a systematic review and regression analysis. Geneva: World Health Organization; 2016.
Kris-Etherton PM, Petersen K, Van Horn L. Convincing evidence supports reducing saturated fat to decrease cardiovascular disease risk. BMJ Nutr Prev Heal. 2018;1:23–6.
Hollænder PLB, Ross AB, Kristensen M. Whole-grain and blood lipid changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr. 2015;102:556–72.
Chen M, Li Y, Sun Q, Pan A, Manson JE, Rexrode KM, et al. Dairy fat and risk of cardiovascular disease in 3 cohorts of US adults. Am J Clin Nutr. 2016;104:1209–17.
Kris-Etherton PM, Krauss RM. Public health guidelines should recommend reducing saturated fat consumption as much as possible: YES. Am J Clin Nutr. 2020 July;112(1):13–8.
Kris-Etherton PM, Richter CK, Bowen KJ, Skulas-Ray AC, Jackson KH, Petersen KS, Harris WS. Recent clinical trials shed new light on the cardiovascular benefits of omega-3 fatty acids. Methodist Debakey Cardiovasc J. 2019;15:171.
Manson JE, Cook NR, Lee IM, Christen W, Bassuk SS, Mora S, et al. Marine n-3 fatty acids and prevention of cardiovascular disease and cancer. N Engl J Med. 2019;380:23–32.
ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379:1529–39.
Bhatt DL, Steg PG, Miller M, Brinton EA, Jacobson TA, Ketchum SB, et al. Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med. 2019;380:11–22.
Hu Y, Hu FB, Manson JE. Marine omega-3 supplementation and cardiovascular disease: an updated meta-analysis of 13 randomized controlled trials involving 127 477 participants. J Am Heart Assoc. 2019;8:e013543.
Rimm EB, Appel LJ, Chiuve SE, Djoussé L, Engler MB, Kris-Etherton PM, et al. Seafood long-chain n-3 polyunsaturated fatty acids and cardiovascular disease: a science advisory from the American Heart Association. Circulation. 2018;138:e35–47.
Pan A, Chen M, Chowdhury R, Wu JHY, Sun Q, Campos H, et al. α-Linolenic acid and risk of cardiovascular disease: a systematic review and meta-analysis. Am J Clin Nutr. 2012;96:1262–73.
Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2020 Feb 29;3(2):CD003177.
Appel L, Moore T, Obarzanek E, Vollmer W, Svetkey L, Sacks F, Bray G, et al. A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med. 1997;336:1117–24.
Suggested Further Readings
Eckel RH, Jakicic JM, Ard JD, de Jesus JM, Miller NH, Hubbard VS, et al. AHA/ACC guideline on lifestyle management to reduce cardiovascular risk. J Am Coll Cardiol. 2014;63(25 Part B):2960–84.
Hooper L, Martin N, Abdelhamid A, Smith GD. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2020, Issue 5. Art. No.: CD011737.
Jacobson Terry A, Maki KC, Orringer CE, Jones PH, Kris-Etherton PM, Sikand G, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 2. J Clin Lipidol. 2015;9:S1–S122.e1.
Lichtenstein AH, Appel LJ, Vadiveloo M, Hu FB, Kris-Etherton PM, Rebholz CM, et al. American Heart Association Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; and Stroke Council. 2021 Dietary Guidance to Improve Cardiovascular Health: A Scientific Statement From the American Heart Association. Circulation. 2021 Nov 2:CIR0000000000001031.
Sacks FM, Lichtenstein AHWJHY, Appel LJ, Creager MA, Kris-Etherton PM, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136:e1–e23.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sapp, P.A., Petersen, K.S., Kris-Etherton, P.M. (2022). Dietary Fat: The Good, the Bad, and What Is Best?. In: Wilson, T., Temple, N.J., Bray, G.A. (eds) Nutrition Guide for Physicians and Related Healthcare Professions. Nutrition and Health. Humana, Cham. https://doi.org/10.1007/978-3-030-82515-7_29
Download citation
DOI: https://doi.org/10.1007/978-3-030-82515-7_29
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-82514-0
Online ISBN: 978-3-030-82515-7
eBook Packages: MedicineMedicine (R0)