Abstract
Staging is an important step in the management of bladder cancer as it guides treatment options and surveillance protocols. Accurate staging is highly dependent on diagnostic capabilities and surgical biopsy/resection techniques. Cystoscopy is the mainstay of bladder cancer workup with urine cytology and cystoscopic enhancement serving as adjuncts to cancer detection. After tumor identification, transurethral resection is done to obtain tissue. Recently, newer resection techniques and laser energies have been used to optimize detrusor muscle in the specimen for more accurate staging. To this end, a second-look resection is still recommended in high-risk patients. An important part of clinical staging is obtaining cross-sectional imaging. Classically, CT scan has been used though there may be a role for MRI and PET scan in certain cases. Staging follows the standard TNM classification system and the most recent WHO grading system. Subsequent risk stratification is assigned based on tumor characteristics. Risk tables can provide clinicians and patients with estimates for disease recurrence and progression and further guide surveillance strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Urothelial carcinoma
- Bladder cancer
- Staging
- Muscle-invasive
- Non-muscle-invasive
- Re-resection
- Recurrence
- Progression
- Risk tables
Introduction
After establishing a diagnosis of bladder cancer, practitioners must stage cancer in order to guide treatment. Staging is divided into pathologic and clinical staging. As the name suggests, pathologic staging relies on tumor histopathology from surgery or biopsy while clinical staging considers pre-surgical imaging and physical examination. Accurate staging guides both treatment decisions and prognostic discussions for patients. This is imperative in bladder cancer as staging may determine the need for radical cystectomy versus a bladder-sparing option. This chapter reviews staging considerations for bladder cancer from initial diagnosis to surveillance protocols.
Diagnosis
A variety of tools exist for diagnosing bladder cancer including cystoscopy, urine cytology, and transurethral resection of bladder tumor (TURBT)). Cystoscopy is the mainstay in the workup of suspected bladder cancer. While it is more invasive than a voided urine test, flexible cystoscopy is frequently and easily done in the office. Urine cytology can be used on its own or as an adjunct to cystoscopy. A positive urine cytology signals malignancy anywhere along the urinary tract, and in the absence of upper tract pathology or grossly visible bladder tumor, the patient requires bladder mapping biopsies and prostatic urethral biopsy [1]. A negative urine cytology, however, does not exclude bladder cancer. Urine cytology is more sensitive for higher-grade tumors (84% for HG versus 16% for LG tumors), while detection of carcinoma in situ (CIS)) is variable (82–100%) [2, 3]. If office cystoscopy demonstrates a bladder tumor, the patient should proceed to the operating room for TURBT or cold-cup biopsy to obtain pathologic diagnosis.
Urinary biomarkers are less established in this diagnostic paradigm (see Chap. 11). The most studied in bladder cancer is a nuclear matrix protein, NMP-22, levels of which are up to 20 times higher in malignant cells than normal cells [4]. A commercial ELISA is available that quantifies NMP-22 levels in the urine. Sensitivities for NMP-22 range from 69% to 90% and roughly 75% with CIS [4]. Other urinary biomarkers exist as well, and while most have increased sensitivity to bladder cancer when compared to urine cytology, it is at the cost of lower specificity [1, 2]. Ultimately, no urine test can replace cystoscopy for initial visual diagnosis.
Staging Modalities
TURBT
The gold standard for diagnosis of bladder cancer is with transurethral resection of bladder tumor (TURBT). TURBT is diagnostic, and in the case of non-muscle-invasive bladder cancer (NMIBC), it can be therapeutic as well. Optimizing staging accuracy is largely dependent on providing the best specimen for pathologists and performing a bimanual exam to assess for the palpable or “fixed” local extent of disease. A full discussion of the TURBT is beyond the scope of this chapter, but here, we will focus on particular variables (cystoscopy enhancements, resection methods) that may influence staging.
Cystoscopy Enhancements
Standard cystoscopy uses white light to identify tumors, and this can be enhanced with the use of blue-light (BLC) or narrowband imaging (NBI). Each has its own advantages and disadvantages as reflected in Table 4.1 (see also Chap. 9). Most tumors are visualized with white light cystoscopy (WLC) although smaller tumors and CIS can be missed. Also referred to as Cysview, or fluorescence cystoscopy, BLC relies on the biochemical synthesis of photoactive porphyrins (PAPs) from intravesically instilled hexaminolevulinate hydrochloride (HAL). These PAPs preferentially accumulate in mitotically active cells like in bladder cancer and can be seen as red or pink under blue light (wavelengths 360–450 nm). In contrast, NBI relies on image enhancement rather than a biochemical pathway. It employs two specific bandwidths, blue (415 nm) and green (540 nm), that are strongly absorbed by hemoglobin in superficial tissues. As a result, highly vascularized tissues, like cancer cells, will absorb these wavelengths more and appear distinct from surrounding, less vascularized normal tissue. Compared with stand-alone WLC , the concomitant use of BLC or NBI has been shown to have higher tumor detection rates on initial TURBT [5, 6], and their use can reduce recurrence rates [7].
Resection Method
The method of resection is just as important as identifying areas to resect. There is no standardized approach, but most resect any exophytic component followed by the resection of the base and circumferential margins of up to 1 cm [8, 9]. Separately sending resection tissue as superficial and deep specimen can help better define the muscle layer. There are two methods of resection: conventional or en bloc. In the conventional approach, all visible tumor is resected piece by piece with loop electrocautery until detrusor fibers are seen to ensure muscle is captured in the specimen. This method splits the tumor as resection is underway. While this is the most widely used approach, it is not without its faults. Conventional TURBT (cTURBT)) works directly against the basic oncologic principle to not break up the tumor. Fragmented tumor risks seeding malignant cells for reimplantation in the bladder. The greatest criticism of conventional TURBT, however, is the high percentage of understaging. An absence of detrusor muscle (DM) in a submitted tumor is the main reason for this with studies reporting up to 56% of tumors without DM [10]. Understaging has been shown to lead to worse recurrence-free survival (RFS) rates in patients with NMIBC, and it risks inadequate treatment of muscle-invasive disease. The importance of a “second look” cannot be overstated for accurate staging, and will be discussed further in the chapter.
In contrast to cTURBT, en bloc resection (EBR) is a newer surgical technique with the goal of removing the bladder tumor in one piece without compromising tissue quality or safety. EBR has been found to greatly increase the likelihood of detrusor muscle (DM) being present with studies reporting 97–100% of DM) in specimen [11, 12]. Multiple studies have found EBR to have lower risks of bladder perforation, less operative time, and possibly less chance of tumor seeding and reimplantation due to resection of the tumor as a whole [9, 11, 12]. However, this method is not always practical, and cases must be appropriately selected (Table 4.2). Due to the increasing interest globally in EBR, the European Association of Urology (EAU) devised an International Consensus statement [9]. Tumor size can be the major limitation, with 3 cm being the cutoff in most studies. A modified approach can still be done for tumors above this cutoff. Also, if en bloc resection is successfully performed but the specimen is too large to be removed from the bladder as one piece, the tumor can be divided into a few pieces. Surgeons can feasibly do EBR for multiple sites though operative time would increase depending on the total number of tumors. As always, bladder dome tumors are more technically difficult to resect, regardless of resection method , and should be done cautiously. Some tips for successful resection include making a circumferential marking around the tumor before resection, ensuring the mark is at least 5 mm from any other tumor, and incising at the level of the detrusor muscle. If using a laser, a fan-shaped incision can be made through the bladder wall to expose the base. Surgeons can then take advantage of the resulting hydrodissection lifting the incised tumor to aid in resection [12]. Also, additional biopsies or resection of the tumor base is not necessary if EBR is done correctly since muscle should be included with the initial specimen [9].
Conventional TURBT remains the mainstay for remains the mainstay for diagnosis of bladder cancer. It has the advantage of being able to resect irrespective of tumor size. EBR is a feasible and safe alternative that can provide improved specimen quality with higher rates of DM. Smaller and fewer tumors and those farther from the dome are more advantageous for EBR. Bladder tumors that do not fit these parameters can still be resected via a modified approach to optimize DM in the specimen.
Influence of Energy Type
There are two main energy sources for TURBT: electric and laser (Table 4.3). Conventional TURBT uses electrical energy (monopolar or bipolar), while en bloc resection can be done with either type. There is not agreement in the literature on whether monopolar or bipolar energy has greater DM rates in specimen. In a prospective, randomized controlled trial (RCT) by Teoh et al., bipolar TURBT had superior DM sampling compared with monopolar TURBT (84.6 vs 67.7, p = 0.025) [13]. An earlier RCT by Venaktramani et al. did not find a difference [14]. There is consensus though that thermal injury is problematic with electrocautery. It can damage surrounding normal tissues and render tumor specimen poor quality. Carbonization effects from monopolar energy cause resected tumor to adhere to the loop yielding significant artifact from charred tumor [15]. In one series, cautery artifact (monopolar or bipolar) was found to understage urothelial cancer from initial TURBT by up to 6% for large tumors [16]. This is an inherent risk with electrical energy though it may be less with bipolar [14, 15, 17]. Aside from cautery artifact, incomplete resection is another cause for understaging with cTURBT. Electrocautery was initially thought to be the reason for this; however, monopolar energy has been used successfully with EBR to render whole specimen with high rates of DM present. Initial studies used a modified loop, usually a J-shaped electrode fashioned from a loop [11, 18]. More recent studies have shown feasibility of monopolar and bipolar EBR without modification of the conventional loop electrode [11, 19]. These studies report near 100% of DM in EBR specimen compared to lower percentages (54%) with cTURBT [19].
Laser energy can also be used to treat bladder tumors. Laser vaporization has been shown to be both a safe and feasible alternative to cTURBT for treating NMIBC [15, 20]. Successful en bloc resection has been performed with holmium, thulium, and green light lasers. The high-power tissue vaporization potential of these lasers allows for excellent hemostasis. Their use for treatment of bladder cancer, however, was initially limited given the concern that vaporization does not provide adequate specimen for diagnosis. Xishuang et al. found it more difficult to obtain intact tumor for precise TNM staging when doing Holmium en bloc resection (Hol-EBR) versus cTURBT. Smaller tumors, especially those 5 mm or less in diameter, may be most prone to vaporization effects [15]. Leaving a margin (anywhere from 2 to 20 mm around the tumor base) when resecting can minimize the risk of inadequate specimen [15, 21, 22]. He et al. was able to lessen this risk by using a front-firing rather than a side-firing green light laser [12]. Specimen can be further kept intact by using lower power settings. With green light laser, for instance, the standard 80–120 W power used for BPH procedures is not needed, and 30 W power is adequate [12, 15]. The concern for serosal injury is less with thulium lasers than with holmium and green light. Thulium lasers, also known as 2-micron continuous-wave laser systems, evaporate tissues continuously and do not generate pressure waves. As a result, the laser affects tissues only within 2 mm in front of the fiber tip, and cleaner resection cuts are achieved [22, 23]. Muto et al. found detrusor muscle to be present in all bladder tumor specimen resected with thulium laser in a prospective study on Thulium EBR [24]. An advantage of laser energy is that it does not activate the obturator nerve reflex as much as electroresection. Compared with cTURBT, studies using r Hol-EBR and Thul-EBR have not reported cases of activating the obturator nerve reflex and thus mitigating the risk of bladder perforation [15, 21,22,23, 25].
Special Staging Circumstances: Diverticulae
Bladder diverticula present a unique staging challenge . They account for just 1% of all bladder cancers [26]. The majority of intra-diverticular bladder tumors (IDBTs) in adults are acquired, which means they lack true muscularis propria. Per the 2017 American Joint Committee on Cancer (AJCC) recommendations, stage T2 is omitted with IBDTs to avoid confusion since there is no muscle layer, [26, 27]. Normally, specimen quality is judged based on the presence of detrusor muscle, but this is lost with IDBTs. Previous studies have noted a dense fibroconnective band that demarcates the boundary between the lamina propria and perivesical fat [26, 28]. Invasion beyond this thick band has been suggested to be at least stage T3 [28]. Given that tumors can more easily extend from the lamina propria to the perivesical fat in a diverticulum, obtaining adequate specimen is especially important for staging [29]. This may be challenging with the increased risk of bladder perforation in a thin-walled diverticulum or difficulty passing an endoscope through a narrow diverticulum stalk.
Bimanual Exam
An exam under anesthesia can provide important information about the patient’s clinical stage and tumor resectability and should be done before and after TURBT. Factors that suggest locally advanced disease include a fixed mass (cT4b), invasion of adjacent structures (cT4a), and the presence of a large residual mass after TURBT (cT3b) [30]. While these are clinically useful benchmarks, results of the bimanual exam are not always accurate with one study reporting clinical overstaging in 11% and understaging in 33% of cases (total of 44% discordance) [31].
Accuracy of Staging: Importance of Repeat TURBT
As noted above, a single TURBT may provide inaccurate staging information. Most important is the risk for understaging, as this risks undertreatment of aggressive disease. Further, any intravesical therapy is most efficacious after complete tumor resection. A repeat resection is helpful in two ways: it eliminates any residual tumor at the operative site and allows for more accurate staging.
There is significant evidence supporting this practice. Herr and Donat from Memorial Sloan Kettering (MSK) showed high rates of residual tumor in patients referred after outside TURBT (74%), and there were significant rates of upstaging in both Ta (15%) and T1 (30%) tumors [32, 33]. Of note, this benefit did not extend to patients with low-grade disease at initial resection. These results were confirmed in a systematic review by Cumberbatch et al., which noted residual tumor in up to 70% of repeat resections and upstaging in up to 8% of Ta and 32% of T1 tumors [34]. This is true even for experienced clinicians. An MSK series of re-resection of T1 tumors in which initial resection was done at their center found persistent T1 tumor in 25% of patients [35].
Appropriate staging as above improves patient selection for appropriate therapies, whether it be intravesical adjunctive therapies or radical cystectomy. This improvement in patient selection translates into improved patient outcomes. A prospective trial by Divrik et al. showed that patients undergoing repeat TUR had improved recurrence-free and progression-free survival [36]. Further, repeat TURBT has demonstrated improved outcomes after BCG therapy. In both cases, it appears that repeat TURBT allowed for the full eradication of tumor and appropriate patient selection, which improved patient outcomes after therapy [37].
American Urological Association (AUA) Guidelines recommend repeat resection if there is incomplete resection at the initial TURBT or if there is T1 disease at initial resection. These same guidelines suggest consideration of repeat TURBT for high-risk , high-grade Ta tumors [30]. NCCN guidelines suggest similarly, adding a strong consideration for repeat TURBT in high-grade tumors if no detrusor muscle was present in the initial specimen [38]. This addition by the NCCN guidelines reflects the presence of detrusor muscle in the specimen as a proxy for adequacy/quality of initial TURBT. Indeed, several studies have shown decreased rates of understaging in patients with detrusor muscle in the primary specimen [10, 39]. The timing of the repeat TURBT has been debated in the literature, but most advocate for a time period of 4–6 weeks after initial TURBT. A retrospective study of high-risk NMIBC looking at the timing of re-resection showed decreased recurrence-free and progression-free survival in patients with repeat resection >42 after the initial resection [40].
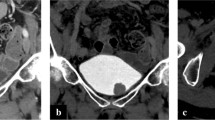
Imaging
Imaging studies are an important component of the staging workup for both NMIBC and MIBC (see also Chap. 5). With any newly diagnosed bladder tumor, it is recommended to obtain cross-sectional imaging prior to planned OR for TURBT. This imaging should assess the upper urinary collecting system. Traditionally, this has been accomplished with triphasic CT scan, combining a non-contrast, arterial, and delayed (excretory) phase imaging. However, in some cases, such as allergy to CT contrast dye or compromised renal function, practitioners may choose to use triphasic MR imaging or retrograde urography at the time of cystoscopy in combination with non-contrast CT or ultrasound. Often, this has been completed previously if the patient’s initial presentation was for gross or microscopic hematuria.
Obtaining this imaging is beneficial in several ways. If pathology is noted on this imaging, then the practitioner may choose to bypass the office cystoscopy and proceed directly to the operating room. Also, if upper tract findings are noted, they may be evaluated and addressed at the time of the TURBT. Further imaging is dependent on pathology noted after resection. In both NMIBC and MIBC, imaging of the upper tracts must be performed as above if not done previously. If MIBC is noted, addition of chest imaging (CT or X-ray) should be performed, and consideration for bone imaging should be given if the patient has concerning symptoms.
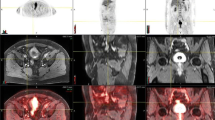
The use of MRI has become more common by practitioners given its useful soft tissue discrimination. Much work is underway to use MRI as a potential discriminator of muscle-invasive disease. Vesical Imaging-Reporting and Data System (VI-RADS) has been recently created to give a standardized reporting platform for clinicians [41]. While the study is still ongoing, there is hope MRI will provide a noninvasive method to assess muscle invasion or determine treatment response. Some initial data suggests the ability to determine between NMIBC and MIBC states, and further literature on the subject will provide more useful guidance as to the best use of this imaging [42]. Studies in the United Kingdom that are using mpMRI as a means of triaging patients with definitive muscle-invasive disease to immediate RC are underway (BladderPath Study).
The use of positron emission tomography (PET) may) be useful in the staging workup for bladder cancer (see also Chap. 7). Classically, the use of this modality has been limited, given that urinary excretion of tracer obscures assessment of the primary or upper tract tumors. However, some have advocated the use of this for assessment of lymph node metastases in MIBC. Dason et al. compared preoperative PET imaging to pathologic node metastases at the time of radical cystectomy and found PET imaging to be most useful in the setting of clinically enlarged nodes on cross-sectional imaging [43]. The most appropriate use of PET imaging as well as the most useful tracer is still undetermined.
Staging
Current TNM Staging
Staging for bladder cancers follows the tumor, node, metastasis (TNM) system (Table 4.4).
Historical Considerations and Updates
In 1973, the World Health Organization (WHO) published its initial grading system for urothelial carcinomas based on cell differentiation. A more uniform system was adopted in 2004 (updated in 2016) that eliminated the heterogenous Grade 2 (G2) category. Figure 4.1 shows the shift in grading and result of the reclassification on each category. A systematic review did not find the 2004/2016 system outperformed the 1973 one in predicting recurrence and progression [45]. In fact, the 1973 groupings may more accurately predict recurrence and progression for pT1 tumors. In tumors classified as T1HG, Pelluchhi et al. found a higher recurrence (68% vs 50%) and progression rate (28% vs 9%) in the Grade 3 (G3) over G2 tumors, respectively [46].
WHO grading of NMIBC in 1973 versus 2004/2016 [47] . *PUNLMP papillary urothelial neoplasm of low malignant potential
Risk Stratification Schema
The creation of risk categories is helpful for counseling and surveillance. The AUA and EAU have separate but similar guidelines on this. The AUA stratifies risk into three categories (Table 4.5). Unique to the AUA risk table is the reclassification of intermediate-risk patients to high risk if they fail BCG treatment with the thought that these patients likely harbor more aggressive disease with increased risk for progression [30]. The EAU further subcategorizes high-risk patients into those with the highest risk [1]. This group includes tumors that are T1HG with concomitant bladder or prostatic urethra CIS, multiple and/or large T1HG and/or recurrent T1HG disease, variant histology, or lymphovascular invasion. Along with assigning a clinical stage, clinicians should designate each tumor recurrence or occurrence as low, intermediate, or high risk.
Current EAU NMIBC guidelines recommend using EORTC risk tables to determine a patients’ risk to recur or progress after undergoing TUR. The tables are the result of a combined analysis of 2596 patients who underwent different prophylactic treatments after TUR of Ta-T1 bladder cancer with or without CIS. Each patient was assigned a total score (0–23) based on the presence or absence of certain factors influencing recurrence and progression. Higher scores indicate a worse prognosis (Table 4.6) [48]. Patients were then placed into one of four groups that related total score to 1- and 5-year recurrence and progression percentages (Table 4.7) [48]. Limitations of this study should be noted though. Specifically, no patients underwent second-look TUR or maintenance BCG, and only 78% received intravesical therapy [48]. Nowadays, many patients with high-risk disease undergo re-resection and maintenance BCG, which both independently reduce recurrence and progression [40, 49, 50].
The Spanish urologic oncology group (CUETO) subsequently performed external validation of the EORTC model. In their study, all patients had NMIBC treated with 12 intravesical instillations of BCG over 5–6 months [51]. They found that EORTC tables overestimated the risk of progression in high-risk patients and risk of recurrence overall after BCG. In the EORTC study, high-risk patients had a 61% and 78% chance to recur at 1 and 5 years compared with 26–30% and ~50% in the CUETO group, respectively [48, 51]. Chance of progression in EORTC high-risk patients was 17% and 45% at 1 and 5 years versus the 14% and 34% seen in the comparative CUETO patients [48, 51]. These reduced risks are likely due to treatment with BCG which has been shown to lessen recurrences and progression to MIBC [49, 50]. Notably, study populations were slightly different, with more G3 T1 tumors and CIS seen in the CUETO series.
Surveillance Protocols
Non-muscle-Invasive Disease
The goal of surveillance in NMIBC is to detect high-grade recurrence and progression to MIBC as early as possible after the initial treatment in order to optimize patient outcomes. Low-grade tumors rarely progress, so early detection is less essential. In contrast, intermediate-/high-grade tumors progress more frequently, so timely detection is key as diagnostic delays can be life-threatening. Overall, there is a lack of robust randomized trial data comparing different surveillance strategies to suggest one over the other. The EORTC and CUETO risk stratification models provide a starting point that can be adapted based on each patient’s individual risk.
Cystoscopy remains the standard for surveillance follow-up. As with diagnosis, urine cytology should be used as an adjunct. Currently, no urinary biomarkers, cytology, or imaging studies can replace the ability to carefully inspect the patient’s entire bladder. Visualization allows the clinician to ensure the previous resection was complete and look for new tumor. The first cystoscopy after TURBT (and any adjuvant therapies) is generally recommended to be done at 3–4 months. Multiple studies have found recurrence at 3 months to be an important predictor of future recurrences and progression to MIBC [52, 53]. This is especially important for TaT1 tumors or CIS, which are independent risk factors for progression [52, 53]. The AUA defines three surveillance strategies after a negative first cystoscopy [30]:
-
Low risk – Next cystoscopy at 6–9 months and then annually
-
Intermediate risk – Next cystoscopy and cytology at 3–6 months for 2 years, 6–12 months for years 3 and 4, and then annually
-
High risk – Next cystoscopy and cytology every 3–4 months for 2 years, 6 months for years 3 and 4, and then annually
The less frequent surveillance for low-risk disease is supported by a historical study by Olsen & Genster et al., the only RCT on follow-up in NMIBC. Though the study was small, it showed no difference in recurrence, progression, or survival between more or less frequent follow-up for low-risk NMIBC (every 3 months versus 6 months) [54]. In a retrospective study, Shroeck et al. similarly found that among patients with Ta disease, low-intensity surveillance (≤5 cystoscopies over 2 years) was not associated with increased risk of disease progression to T1/T2 or death from bladder cancer when compared with high-intensity surveillance [55]. Furthermore, frequent cystoscopies (>3 in 2 years) among the low-risk NMIBC group are associated with twice as many TURs without a decrease disease progression or death [56]. Both AUA and EAU guidelines suggest discontinuing surveillance of low-risk patients after 5 years if disease-free due to the limited recurrences and muscle progression noted past this point [1, 30]. In a study by Matsumoto et al., 14.9% of patients who had undergone TURBT for NMIBC had any recurrence after a disease-free interval of 5 years, and none were in patients with low-grade Ta [57]. Recurrence past 5 years is not uncommon but those at low risk likely do not require lifelong follow-up. Further, active surveillance with urine cytology appears to be a safe approach for small, recurrent, low-grade Ta tumors [58]. This may be especially beneficial in elderly patients.
The duration of follow-up is less clear for patients with intermediate- or high-risk disease. The EAU recommends life-long follow-up, while the AUA recommends shared decision-making after 5 years of being disease-free [1, 30]. Both groups agree intermediate- and high-risk patients should have upper tract imaging periodically (every 1 or 2 years) [1, 30]. In an observational study of 1529 patients with NMIBC, Millán-Rodríguez et al. found an increasing incidence of UUT with increasing risk group (low risk: 0.6%, intermediate: 1.8%, high: 4.1%) [59]. Aside from higher-risk groups, having multiple recurrent superficial bladder tumors has been found to be another predictor for the development of upper urinary tract tumors (UUT) [59].
Recurrence After BCG
Despite several additional intravesical therapies available on the market, BCG remains the standard of care for patients with high-grade NMIBC and CIS. While BCG has been shown to reduce both recurrence and progression, a number of patients will experience treatment failure. In order to characterize the diverse situations in which this can occur, the International Bladder Cancer Group (IBCG) has a standardized classification of BCG failure into four different categories: refractory, relapsing, intolerant, and unresponsive [60].
-
Refractory: persistent high-grade disease at 6 months despite adequate BCG treatment
-
Relapsing: recurrent high-grade disease after previously achieving disease-free state at 6 months after adequate BCG (or last exposure)
-
Intolerant: disease persists due to inability to receive adequate BCG because of toxicity
-
Unresponsive: includes patients with BCG refractory or relapsing (within 6 months of last BCG) disease
There are a few points to emphasize regarding the above classification. First, the impetus for waiting 6 months prior to classification as BCG-refractory stems from the knowledge that a significant proportion of patients will respond to a second course of BCG [61]. Second, the designation of BCG-unresponsive disease (BCG refractory or relapsing within 6 months) should denote to the practitioner that further BCG is unlikely to be efficacious.
Conclusion
The spectrum of potential treatments for newly diagnosed bladder cancer is quite broad, spanning from close observation for low-grade lesions to radical surgery in the context of muscle-invasive disease. Selection of the appropriate treatment first involves obtaining accurate staging. Through the use of quality bladder resection, physical examination, and imaging, the practitioner can accurately determine the appropriate stage, weigh prognostic risk, and evaluate available treatment options.
References
Babjuk M, Oosterlinck W, Sylvester R. Guidelines on non-muscle invasive bladder cancer (TaT1 and CIS)- limited update march 2020. 2011. Eur Urol [Internet]. 2013;(March):1–42.
Têtu B. Diagnosis of urothelial carcinoma from urine. Mod Pathol. 2009;22(October 2008):S53–9.
Yafi FA, Brimo F, Steinberg J, Aprikian AG, Tanguay S, Kassouf W. Prospective analysis of sensitivity and specificity of urinary cytology and other urinary biomarkers for bladder cancer. Urol Oncol Semin Orig Investig. 2015;33(2):66.e25–31.
Pincus MR, Brandt-Rauf PW, Bluth MH, Bowne WB. Oncoproteins and early tumor detection [Internet]. In: Twenty Thi. Henry’s clinical diagnosis and management by laboratory methods. Elsevier Inc.; 2011. 1452–1459 p.. Available from: https://doi.org/10.1016/B978-0-323-29568-0.00075-9.
Kim SB, Yoon SG, Tae J, Kim JY, Shim JS, Kang SG, et al. Detection and recurrence rate of transurethral resection of bladder tumors by narrow-band imaging: prospective, randomized comparison with white light cystoscopy. Investig Clin Urol. 2018;59(2):98–105.
Mowatt G, N’Dow J, Vale L, Nabi G, Boachie C, Cook JA, et al. Photodynamic diagnosis of bladder cancer compared with white light cystoscopy: systematic review and meta-analysis. Int J Technol Assess Health Care. 2011;27(1):3–10.
Geavlete B, Multescu R, Georgescu D, Jecu M, Stanescu F, Geavlete P. Treatment changes and long-term recurrence rates after hexaminolevulinate (HAL) fluorescence cystoscopy: does it really make a difference in patients with non-muscle-invasive bladder cancer (NMIBC)? BJU Int. 2012;109(4):549–56.
Zhang JH, Gill BA, Wilkins L, Ramkumar RR, Shoskes DA. Systemic comorbidity burden using the ACTIONS phenotype predicts urologic medication discontinuation following transurethral resection of the prostate. Urology. 2019;127:91.
Teoh JYC, MacLennan S, Chan VWS, Miki J, Lee HY, Chiong E, et al. An international collaborative consensus statement on En bloc resection of bladder tumour incorporating two systematic reviews, a two-round delphi survey, and a consensus meeting. Eur Urol [Internet]. 2020;78(4):546–69. Available from: https://doi.org/10.1016/j.eururo.2020.04.059.
Herr H. The value of a seond transurethral resection in evaluating patients with bladder tumors. J Urol. 1999;162(1):74–6.
Kramer MW, Rassweiler JJ, Klein J, Martov A, Baykov N, Lusuardi L, et al. En bloc resection of urothelium carcinoma of the bladder (EBRUC): a European multicenter study to compare safety, efficacy, and outcome of laser and electrical en bloc transurethral resection of bladder tumor. World J Urol. 2015;33(12):1937–43.
He D, Fan J, Wu K, Wang X, Wu D, Li L, et al. Novel green-light KTP laser en bloc enucleation for nonmuscle-invasive bladder cancer: technique and initial clinical experience. J Endourol. 2014;28(8):975–9.
Teoh JYC, Chan ESY, Yip SY, Tam HM, Chiu PKF, Yee CH, et al. Comparison of detrusor muscle sampling rate in monopolar and bipolar transurethral resection of bladder tumor: a randomized trial. Ann Surg Oncol. 2017;24(5):1428–34.
Venkatramani V, Panda A, Manojkumar R, Kekre NS. Monopolar versus bipolar transurethral resection of bladder tumors: a single center, parallel arm, randomized, controlled trial. J Urol [Internet]. 2014;191(6):1703–7. Available from: https://doi.org/10.1016/j.juro.2013.12.004.
Xishuang S, Deyong Y, Xiangyu C, Tao J, Quanlin L, Hongwei G, et al. Comparing the safety and efficiency of conventional monopolar, plasmakinetic, and holmium laser transurethral resection of primary non-muscle invasive bladder cancer. J Endourol. 2010;24(1):69–73.
Truong M, Liang L, Kukreja J, O’Brien J, Jean-Gilles J, Messing E. Cautery artifact understages urothelial cancer at initial transurethral resection of large bladder tumours. Can Urol Assoc J. 2017;11(5):E203–6.
Del Rosso A, Pace G, Masciovecchio S, Saldutto P, Galatioto GP, Vicentini C. Plasmakinetic bipolar versus monopolar transurethral resection of non-muscle invasive bladder cancer: a single center randomized controlled trial. Int J Urol. 2013;20(4):399–403.
Ukai R, Hashimoto K, Iwasa T, Nakayama H. Transurethral resection in one piece (TURBO) is an accurate tool for pathological staging of bladder tumor. Int J Urol. 2010;17(8):708–14.
Zhang KY, Xing JC, Li W, Wu Z, Chen B, Bai DY. A novel transurethral resection technique for superficial bladder tumor: retrograde en bloc resection. World J Surg Oncol. 2017;15(1):1–7.
Tao W, Yang D, Shan Y, Xue B, Sun C, Zang Y, et al. Safety and efficacy of 120w high performance system greenlight laser vaporization for non-muscle-invasive bladder cancer. J Xray Sci Technol. 2013;21(2):309–16.
D’Souza N, Verma A. Holmium laser transurethral resection of bladder tumor: our experience. Urol Ann. 2016;8(4):439–43.
Liu H, Wu J, Xue S, Zhang Q, Ruan Y, Sun X, et al. Comparison of the safety and efficacy of conventional monopolar and 2-micron laser transurethral resection in the management of multiple nonmuscle-invasive bladder cancer. J Int Med Res. 2013;41(4):984–92.
Chen X, Liao J, Chen L, Qiu S, Mo C, Mao X, et al. En bloc transurethral resection with 2-micron continuous-wave laser for primary non-muscle-invasive bladder cancer: a randomized controlled trial. World J Urol [Internet]. 2015;33(7):989–95. Available from: https://doi.org/10.1007/s00345-014-1342-1.
Muto G, Collura D, Giacobbe A, D’Urso L, Muto GL, Demarchi A, et al. Thulium:yttrium-aluminum-garnet laser for en bloc resection of bladder cancer: clinical and histopathologic advantages. Urology [Internet]. 2014;83(4):851–5. Available from: https://doi.org/10.1016/j.urology.2013.12.022.
Kramer MW, Altieri V, Hurle R, Lusuardi L, Merseburger AS, Rassweiler J, et al. Current evidence of transurethral En-bloc resection of nonmuscle invasive bladder cancer. Eur Urol Focus [Internet]. 2017;3(6):567–76. Available from: https://doi.org/10.1016/j.euf.2016.12.004.
Idrees MT, Alexander RE, Kum JB, Cheng L. The spectrum of histopathologic findings in vesical diverticulum: implications for pathogenesis and staging. Hum Pathol [Internet]. 2013;44(7):1223–32. Available from: https://doi.org/10.1016/j.humpath.2012.11.005.
Bochner B, DE H, Efstathiou JA, et al. Urinary bladder. In: Springer, editor. AJCC cancer staging manual. 8th ed. Chicago; 2017. p. 757–65.
Tamas EF, Stephenson AJ, Campbell SC, Montague DK, Trusty DC, Hansel DE. Histopathologic features and clinical outcomes in 71 cases of bladder diverticula. Springer. Arch Pathol Lab Med. 2009;133(5):791–6.
Walker NF, Gan C, Olsburgh J, Khan MS. Diagnosis and management of intradiverticular bladder tumours. Nat Rev Urol. 2014;11(7):383–90.
Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, et al. American Urological Association ( AUA )/ Society of Urologic Oncology ( SUO ) guideline diagnosis and treatment of non-muscle invasive bladder cancer: AUA / SUO guideline 2016, Amended 2020. 2020;(May):1–45.
Ploeg M, Kiemeney LALM, Smits GA, Vergunst H, Viddeleer AC, Geboers ADH, et al. Discrepancy between clinical staging through bimanual palpation and pathological staging after cystectomy. Urol Oncol Semin Orig Investig [Internet]. 2012;30(3):247–51. Available from: https://doi.org/10.1016/j.urolonc.2009.12.020.
Herr HW. Role of re-resection in non-muscle-invasive bladder cancer. ScientificWorldJournal. 2011;11:283–8.
Herr HW, Donat SM. Quality control in transurethral resection of bladder tumours. BJU Int. 2008;102(9B):1242–6.
Cumberbatch MGK, Foerster B, Catto JWF, Kamat AM, Kassouf W, Jubber I, et al. Repeat transurethral resection in non–muscle-invasive bladder cancer: a systematic review [Figure presented]. Eur Urol [Internet]. 2018;73(6):925–33. Available from: https://doi.org/10.1016/j.eururo.2018.02.014.
Dalbagni G, Herr HW, Reuter VE. Impact of a second transurethral resection on the staging of T1 bladder cancer. Urology. 2002;60(5):822–4.
Divrik RT, Ahin AF, Yildirim Ü, Altok M, Zorlu F. Impact of routine second transurethral resection on the long-term outcome of patients with newly diagnosed pT1 urothelial carcinoma with respect to recurrence, progression rate, and disease-specific survival: a prospective randomised clinical trial. Eur Urol. 2010;58(2):185–90.
Sfakianos JP, Kim PH, Hakimi AA, Herr HW. The effect of restaging transurethral resection on recurrence and progression rates in patients with nonmuscle invasive bladder cancer treated with intravesical bacillus Calmette-Guérin. J Urol. 2014;191(2):341–5.
Flaig TW, Spiess PE, Agarwal N, Bangs R, Boorjian SA, Buyyounouski MK, et al. Bladder cancer, version 3.2020, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2020;18(3):329–54.
Dutta SC, Smith JA Jr, Shappell SB, Coffey CS, Chang SS, Cookson MS. Clinical under staging of high risk nonmuscle invasive urothelial carcinoma treated with radical cystectomy. J Urol. 2001;166(2):490–3.
Baltaci S, Bozlu M, Yildirim A, Gökçe MI, Tinay I, Aslan G, et al. Significance of the interval between first and second transurethral resection on recurrence and progression rates in patients with high-risk non-muscle-invasive bladder cancer treated with maintenance intravesical Bacillus Calmette-Guérin. BJU Int. 2015;116(5):721–6.
Panebianco V, Narumi Y, Altun E, Bochner BH, Jason A, Hafeez S, et al. Multiparametric magnetic resonance imaging for bladder cancer: development of VI-RADS. Eur Urol. 2019;74(3):294–306.
Makboul M, Farghaly S, AbDelkawI IF. Multiparametric MRI in differentiation between muscle invasive and non-muscle invasive urinary bladder cancer with vesical imaging reporting and data system (VI-RADS) application. Br J Radiol. 2020;93(1109):20200025.
Dason S, Wong NC, Donahue TF, Meier A, Zheng J, Mannelli L, et al. Utility of routine preoperative 18F-fluorodeoxyglucose positron emission tomography/computerized tomography in identifying pathological lymph node metastases at radical cystectomy. J Urol. 2020;204(2):254–9.
Brierley JD, et al. TNM classification of malignant tumors. 8th. In: UICC international union against cancer. 8th ed. Oxford; 2017.
Soukup V, Čapoun O, Cohen D, Hernández V, Babjuk M, Burger M, et al. Prognostic performance and reproducibility of the 1973 and 2004/2016 World Health Organization grading classification systems in non–muscle-invasive bladder cancer: a European Association of Urology Non-muscle Invasive Bladder Cancer Guidelines Panel Syst. Eur Urol. 2017;72(5):801–13.
Pellucchi F, Freschi M, Moschini M, Rocchini L, Maccagnano C, Nazareno S, et al. Oncological predictive value of the 2004 World Health Organisation grading classification in primary T1 non-muscle-invasive bladder cancer. A step forward or back? BJU Int. 2015;115(2):267–73.
MacLennan GT, Kirkali Z, Cheng L. Histologic grading of noninvasive papillary urothelial neoplasms. Eur Urol. 2007;51(4):889–98.
Sylvester RJ, Van Der Meijden APM, Oosterlinck W, Witjes JA, Bouffioux C, Denis L, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol. 2006;49(3):466–77.
Böhle A, Jocham D, Bock P. Intravesical bacillus Calmette-Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. J Urol. 2003;169(1):90–5.
Sylvester RJ, van der MEIJDEN AP, Lamm DL. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. J Urol. 2002;168(5):1964–70.
Fernandez-Gomez J, Madero R, Solsona E, Unda M, Martinez-Piñeiro L, Ojea A, et al. The EORTC tables overestimate the risk of recurrence and progression in patients with non-muscle-invasive bladder cancer treated with bacillus Calmette-Guérin: external validation of the EORTC risk tables. Eur Urol. 2011;60(3):423–30.
Soukup V, Babjuk M, Bellmunt J, Dalbagni G, Giannarini G, Hakenberg OW, et al. Follow-up after surgical treatment of bladder cancer: a critical analysis of the literature. Eur Urol. 2012;62(2):290–302.
Palou J, Rodríguez-Rubio F, Millán F, Algaba F, Rodríguez-Faba O, Huguet J, et al. Recurrence at three months and high-grade recurrence as prognostic factor of progression in multivariate analysis of T1G2 bladder tumors. Urology [Internet]. 2009;73(6):1313–7. Available from: https://doi.org/10.1016/j.urology.2008.12.047.
Olsen L, Genster H. Prolonging follow-up intervals for non-invasive bladder tumors: a randomized controlled trial. Scand J Urol Nephrol Suppl. 1995;172(33):6.
Rezaee ME, Lynch KE, Li Z, MacKenzie TA, Seigne JD, Robertson DJ, et al. The impact of low-versus high-intensity surveillance cystoscopy on surgical care and cancer outcomes in patients with high-risk non-muscle-invasive bladder cancer (NMIBC). PLoS One [Internet]. 2020;15(3):1–13. Available from: https://doi.org/10.1371/journal.pone.0230417.
Schroeck FR, Lynch KE, Li Z, Todd A, Sirovich B, Goodney PP. U. S. Department of Veterans Affairs. 2020;125(18):3147–54.
Matsumoto K, Kikuchi E, Horiguchi Y, Tanaka N, Miyajima A, Nakagawa K, et al. Late recurrence and progression in non-muscle-invasive bladder cancers after 5-year tumor-free periods. Urology [Internet]. 2010;75(6):1385–90. Available from: https://doi.org/10.1016/j.urology.2009.09.088.
Matulay JT, Soloway M, Witjes JA, Buckley R, Persad R, Lamm DL, et al. Risk-adapted management of low-grade bladder tumours: recommendations from the International Bladder Cancer Group (IBCG). BJU Int. 2020;125(4):497–505.
Millán-Rodríguez F, Chéchile-Toniolo G, Salvador-Bayarri J, Huguet-Pérez J, Vicente-Rodríguez J. Upper urinary tract tumors after primary superficial bladder tumors: prognostic factors and risk groups. J Urol. 2000;164(4):1183–7.
Kamat AM, Sylvester RJ, Bohle A, Palou J, Lamm DL, Brausi M, et al. Definitions, end points, and clinical trial designs for non–muscle-invasive bladder cancer: recommendations from the international bladder cancer group. J Clin Oncol. 2016;34:1935–43.
Sylvester RJ, Van Der Meijden A, Witjes JA, Jakse G, Nonomura N, Cheng C, et al. High-grade Ta urothelial carcinoma and carcinoma in situ of the bladder. Urology. 2005;66(6 Suppl 1):90–107.
Disclosures
None of the authors have any relevant disclosures or conflicts of interest to report.
Funding Sources
None
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ramkumar, R.R., Haywood, S.C. (2021). Staging of Bladder Cancer. In: Bjurlin, M.A., Matulewicz, R.S. (eds) Comprehensive Diagnostic Approach to Bladder Cancer. Springer, Cham. https://doi.org/10.1007/978-3-030-82048-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-82048-0_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-82047-3
Online ISBN: 978-3-030-82048-0
eBook Packages: MedicineMedicine (R0)