Abstract
Treatment decisions and prognostic expectations for bladder cancer rely on accurate pathologic staging. Pathologic staging of bladder cancers is performed on tissue obtained after radical cystectomy and utilizes the American Joint Committee on Cancer (AJCC) staging system. The eighth edition of the AJCC staging manual has been published and implemented in January 2018 to update staging criteria for bladder cancer, with several critical changes and clarifications. This chapter will discuss the AJCC eighth edition with emphasis on the selected changes and/or clarifications. Diagnostic pitfalls and controversial issues in staging and substaging of bladder cancer will be also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Bladder cancer is one of the major causes of cancer morbidity and mortality in men, accounting for an estimated 80,470 new cases and 17,670 cancer deaths in the United States in 2019 [1]. Among many prognostic determinants, pathologic stage is the most crucial factor in risk stratification, management, and surveillance follow-up for bladder cancer [2,3,4,5,6]. As with other hollow visceral organs, bladder tumor (T) stage categories are defined by the depth of invasion (extent of wall invasion). However, assigning pT stage category is sometimes problematic due to regional and individual histoanatomic variation. An ideal and uniform staging system would permit accurate reflection of the natural history of cancer, the extent of disease spread, the stratification of prognostic groups and comparison of therapeutic interventions among different hospitals. Staging guidelines from the International Union Against Cancer (UICC) were released in 2016 [7, 8], and on January 1, 2018, utilization of the eighth edition of the AJCC staging manual was implemented [9]. However, the UICC failed to incorporate new data considered in the new eighth edition of AJCC, and there are many differences between the staging recommendations of recent UICC and AJCC staging systems. Thus, this chapter will discuss the current staging recommendations of the AJCC staging manual eighth edition.
Stage pT0 Carcinoma
Stage pT0 carcinoma is assigned when there is no evidence of residual urothelial carcinoma in the cystectomy specimen, according to the eighth AJCC staging system [9]. The incidence of stage pT0 carcinoma is approximately 10% [10,11,12,13,14,15]. Recently, the incidence of pT0 carcinoma has been increasing due to the use of neoadjuvant chemotherapy [16,17,18]. The presence of variant histology is associated with a decreased rate of complete pathologic response (ypT0) [19]. The clinical outcome of patients with ypT0 carcinoma is variable. The 5-year recurrence-free, cancer-specific, and overall survival rates were 84%, 88% and 84%, respectively [11]. In one study, the presence of lymphovascular invasion and concomitant carcinoma in situ in the transurethral resection (TUR) specimen were the only significant prognostic factors associated with shorter overall survival and recurrence-free survival in patients with ypT0 carcinoma [11]. The incidence of lymph node metastasis of patients with ypT0 carcinoma was 3–7% [12, 14].
Stage pTa Carcinoma
There are two types of noninvasive carcinomas with one pTa and the other with pTis. Stage pTa carcinoma is defined as noninvasive papillary carcinoma that lacks invasion, according to the eighth AJCC staging system [9]. pTa carcinoma should be distinguished from pT1 carcinoma by the absence of lamina propria or submucosal invasion.
Stage pTis Carcinoma
Stage pTis carcinoma is assigned when urothelial carcinoma in situ without stromal invasion is present in the cystectomy specimen, according to the eighth AJCC staging system (Fig. 18.1) [9]. pTis carcinoma is often associated with concurrent invasive urothelial carcinoma, but it can be present alone in about 10% of cystectomy specimens [20].
Stage pT1 Carcinoma
pT1 carcinoma is defined when a tumor invades the lamina propria/submucosa but not the proper muscle layer, according to the eighth AJCC staging system [9].
Topographic Variation of the Lamina Propria (Submucosa, Submucosal Connective Tissue Layer)
The lamina propria/submucosa (LP/SM) is composed predominantly of loose connective tissue stroma with a collection of thin smooth muscle fibers, vascular plexuses, nerves, and occasional adipose tissue between the mucosa and muscularis propria (MP) layer [21]. In the bladder, LP and SM are interchangeably used; however, the proper designation of LP and SM is available when muscularis mucosae (MM) is present: LP is the layer above MM, and SM is the layer below MM. Therefore, the proper term in the bladder is submucosal connective layer over LP or SM. In this chapter the term LP is used. The LP depth is more pronounced at the dome (0.98–3.07 mm), similar at the anterior, posterior, and lateral walls and relatively thinner at the bladder neck and trigone (0.46–1.58 mm) (Fig. 18.2) [21]. The mean tumor depth of pT1 carcinoma is 1.1–1.5 mm (range, 0.1–5 mm) [22, 23].
The MM in the urinary bladder LP layer was first described by Dixon and Gosling [24] in 1983, and Ro et al. later underlined its importance in the pathologic staging of bladder cancer [25]. The MM is usually at about the mid- to upper LP and forms a discernible layer in up to 40% of cystectomy specimens, varying by region but more common in the dome (75%) and less common in the trigone (~10%) [21]. Typically, the MM forms individual or small groups of slender and wavy fascicles or wispy fibers with (a) dispersed/scattered (71%), (b) discontinuous/interrupted (20%), or (c) continuous (3%) muscle layers (Fig. 18.3) [25]. The MM also has a focal to rarely extensive hyperplastic appearance with two recognizable patterns of aggregates of hyperplastic MM with haphazard outlines and hyperplastic compact MM with parallel muscle fibers and a regular outline arranged singly or in small groups that sometimes mimics the muscularis propria (MP) (Fig. 18.4) [21]. Hyperplastic MM is relatively more common in the dome and less frequent in the trigone [21]. Awareness of these occasional hyperplastic MM patterns and distributions of hyperplastic MM is crucial to avoid overstaging of bladder cancer.
The muscularis mucosae shows a variable hyperplastic appearance ranging from focal to rarely extensive with two discernible patterns: (a) haphazardly arranged hyperplastic muscularis mucosae with irregular outlines and (b) hyperplastic compact muscularis mucosae with parallel muscle fibers and regular outline arranged singly or in small groups. This pattern of the muscularis mucosae should be distinguished from the muscularis propria, especially in transurethral resection specimens
Adipose tissue within the LP is seen in about 50% of cystectomy specimens and typically located at the deep aspect near the superficial border of the MP (Fig. 18.5) [21, 26]. It is more often focal (35%), mostly situated in the dome (32%), and rare in the trigone (5%) [21]. Considering the high frequency of adipose tissue within the LP, care should be taken to avoid misinterpretation of pT1 carcinoma as perivesical soft tissue involvement (pT3 carcinoma) in TUR specimens to prevent inappropriate aggressive treatment.
Adipose tissue within the lamina propria. Adipose tissue is seen in the deep aspect of the lamina propria, which faces the superficial border of the muscularis propria. The presence of adipose tissue can be often misinterpreted as perivesical soft tissue in transurethral resection specimens, resulting in unnecessary overtreatment
Substaging of pT1 Bladder Carcinoma
A reproducible, easy-to-use, and accurate substaging system is essential to stratify pT1 carcinomas into prognostically distinct subgroups. There are two main approaches: histoanatomic and micrometric substaging. Histoanatomic substaging using the MM and/or vascular plexus as histologic landmarks is the most studied approach for pT1 carcinomas. Both two-tiered and three-tiered systems have been utilized. However, the size and distribution of the MM varies depending on anatomical location. Micrometric substaging of pT1 carcinoma involves measuring the depth of invasion from the mucosal basement membrane using an ocular micrometer with different linear cut-offs. However, the LP depth varies depending on location. The eighth edition of the AJCC staging manual recommends subcategorization of pT1, but no specific methods have been endorsed yet [9], and pT1 substages are not currently recommended to officially implement to use.
Histoanatomical Substaging
This method uses the MM and/or vascular plexus as landmarks to divide the extent of LP invasion [27,28,29,30]. The MM is usually at about the mid- to upper LP and disperses or forms a discernable layer as a discontinuous or infrequently near-continuous layer in only about 40% of cystectomy sections [21]. In cases that lack the MM, the vascular plexus has been proposed as a surrogate, because it is typically situated at about the same level of the accompanying MM. However, the location of the vascular plexus sporadically varies from the suburothelial to the deep LP region, being above, below, and/or at the plane of the MM [21]. Therefore, some cases cannot be properly staged using this method because of absent or incomplete MM and variable locations of the vascular plexus either above or below the MM [21].
These problems may cause concern about the feasibility of pT1 substaging. However, many studies have applied histoanatomical staging in pT1 carcinomas in relation to the MM and/or vascular plexus using either the three-tiered [above (T1a), into (T1b), and below (T1c)] or a two-tiered [above and into (T1a) and below (T1b)] approach, and substaging was feasible in 43–100% (median, 93%) of the tumors [22, 23, 27, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56].
Micrometric Substaging
Substaging pT1 carcinoma can also be carried out by measuring the depth of invasion using an ocular micrometer, and measurement of the depth of invasion from the mucosal basement membrane in biopsy specimens correlates well with the final pathologic stage at cystectomy [57, 58]. The most studied method uses a 0.5 mm (1 high power field) cut-off to divide pT1 into pT1m (microinvasive) and pT1e (extensive) [28, 56, 59]. In contrast to the histoanatomical method, micrometric pT1 substaging using a 0.5 mm cut-off was feasible in all (100%) tumors studied [29, 34, 35, 55, 56, 59]. Other studies have also proposed different cut-offs to divide pT1, including 1 mm, 1.5 mm, 3 mm, and 6 mm [22, 23, 29, 35]. Several studies have also suggested that measuring the aggregate linear length of invasive carcinoma in TUR fragments is a superior quantification approach for pT1 substaging [60, 61].
Microinvasive Carcinoma
Microinvasive carcinoma was originally defined as tumor extending up to 5 mm from the basement membrane (Fig. 18.6) [62]. Since then, several criteria has been proposed to define microinvasive carcinoma, and the cut-off has been lowered to the proposed 0.5 mm [59]. Alternatively, Lopez-Beltran et al. suggested using 20 infiltrating tumor cells within the LP as the cut-off rather than a linear measurement [63]. The 0.5 mm cut-off is currently proposed in pT1 substaging because it has been shown to be widely attainable and correlates with outcome in the majority of studies [29, 34, 35, 55, 56, 59]. Lawless et al. compared tumors with stalk-only invasion, base-focal invasion, and base-extensive invasion and suggested that patients with base-extensive invasion had worse prognosis [64]. They proposed that the site as well as the extent of the LP invasion matters in patient stratification for risk of progression [64].
Diagnostic Pitfalls
Factors in Superficially or Focally Invasive pT1 Carcinomas
Because pT1 carcinomas often invade the LP as single cells or irregularly shaped small nests, the identification of pT1 carcinoma can be sometimes challenging when problems are encountered such as improper tissue embedding (tangential cut or poor orientation), procedural artifacts (thermal injury or cautery artifact), or tumoral responses (obscuring due to inflammation) [65].
Bland Cytology and von Brunn Nests
Some variant histology such as nested variants show deceptively bland cytology, and florid von Brunn nests mimic invasion (Fig. 18.7) [65]. Tumor cells involving von Brunn nests either by pagetoid spread or direct extension from the adjacent tumor can be confusing and especially problematic when the involved von Brunn nests are distorted by inflammation or cautery artifact [66]. True LP invasion can be distinguished from pseudoinvasion of von Brunn nests by identifying the smooth linear contour of the basement membrane (Fig. 18.8).
Helpful Histological Features in Identifying Invasive Carcinoma
Histological features that can be helpful in identification of LP invasion include identifying single cells or irregularly shaped small nests, absence of parallel arrays of thin-walled vessels that often line the basement membrane of noninvasive nests, presence of retraction artifacts, stromal reaction, and paradoxical maturation, where invasive tumor cells obtain abundant eosinophilic cytoplasm [66]. Retraction is a helpful clue, but it sometimes mimics lymphovascular invasion, which can be distinguished from true lymphovascular invasion using immunohistochemical stains (CD34, CD31, and D2–40) [66, 67]. A stromal reaction may be helpful in identifying invasion but is not always present [68]. It may be hypocellular with myxoid background, cellular with spindle-shaped fibroblasts and variable collagenization, pseudosarcomatous, desmoplastic, or inflammatory (Fig. 18.9) [66, 67].
Diverse stromal reaction seen in urothelial carcinomas. (a) Tumor cells infiltrate into hypocellular and loose stroma with a myxoid background. (b) Tumor cells are surrounded by cellular stroma composed of an admixture of spindle-shaped fibroblasts and variable collagenization. (c) Tumor cells are intermingled with fibrous stroma containing atypical spindle cells and lacking overt malignant histological features (i.e., increased mitotic activity, necrosis). (d) Tumor cells infiltrate in cords and single cells with abundant fibrous stroma. (e) Tumor cells are embedded in a rich inflammatory stroma with variable inflammatory cells, including lymphocytes, plasma cells, neutrophils, and eosinophils
Early Cystectomy
Proper muscle invasion in TUR specimens is the major indication for more aggressive treatment (radical cystectomy with bilateral pelvic lymphadenectomy, neoadjuvant chemotherapy or chemoradiation). However, early radical cystectomy can be considered when pT1 carcinoma is associated with other high-risk features such as concurrent carcinoma in situ, multiple or large tumor size (>3 cm), and repeated pT1 on re-TUR and variant histologies, particularly for micropapillary carcinoma [3, 5].
Stage pT2 Carcinoma
Stage pT2 carcinoma is defined as tumor extending into the MP. The urinary bladder MP serves as a key anatomic landmark in the evaluation of depth of invasion and is most often the critical intersection between conservative and aggressive treatment. Diagnosing pT2 carcinomas in TUR specimens is essential for aggressive treatment, including radical cystectomy. Therefore, distinction between the MM and MP invasion is mandatory. The MP layer is composed predominantly of smooth muscle bundles, fibroconnective tissue, adipose tissue, and vessels in between the muscle bundles. A definite pT2 carcinoma is defined by infiltration into MP muscle bundles, but tumors situated in between MP muscle bundles within the MP layer are also typically staged as pT2 carcinoma [6].
Helpful Morphologic Features in Diagnosing pT2 Carcinoma
Hyperplastic MM
The MM is occasionally hyperplastic and could mimic the MP, obscuring pT1/pT2 [21, 28]. Helpful morphologic clues for the MM include thin and slender muscle bundles, superficial location, nonjuxtaposition to adipose tissue, closeness to the surface epithelium, or association with the vascular plexus [28].
LP-Inner MP Boundary and MP-Perivesical Boundary
The inner boundary of the MP can be irregular due to disconnected muscle bundles that vary in size. Therefore, the principle of defining the LP-inner MP boundary (junction of pT1 vs. pT2) is not clear. Traditionally, the outermost extent of the MP was considered the boundary distinguishing the outer MP from perivesical tissue. However, the criteria defining the outer boundary of the MP is unclear due to no clear defined boundary and aggregates of adipose tissue randomly separating MP bundles without a clear demarcation line and is different among expert pathologists. It is reasonable to follow the common approach in defining the outer MP-perivesical tissue boundary [28, 69]. A common criterion in defining the inner and outer boundary of the MP can be used. In a recent study, three general methods were reviewed by expert genitourinary pathologists without consensus, although one method (multiple boundary lines between variable outer bands of the MP) resulted in the highest level of interobserver reproducibility [69].
Staging pT2 Carcinoma in TUR Specimens
Definite pT2 carcinoma can be diagnosed by identifying tumor infiltrating into MP muscle bundles. Therefore, MP presence is considered a surrogate marker for good TUR quality [70,71,72,73]. In contrast to cystectomy specimens, the clear line of demarcation of the LP-inner MP boundary cannot be drawn in TUR specimens, where tissue fragmentation is common. Therefore, the diagnosis of pT2 carcinoma in TUR specimens is generally recommended to be restricted to cases where definite muscle invasion is present (Fig. 18.10). However, the MP can be often fractured and separated by carcinomas into small muscle bundles, masquerading pT1 carcinoma invading into the MM. Diagnosis of pT2 carcinoma is preferred when invasive carcinoma nests are surrounded by MP muscle bundles or invasive carcinoma nests are surrounding an MP muscle bundle, even without direct MP muscle invasion (Fig. 18.11) [6]. The diagnosis of pT3 carcinoma in TUR specimens is generally not recommended, because adipose tissue in the MP layer may be mistakenly considered to be perivesical adipose tissue (Fig. 18.12), complicating the distinction between pT2b and pT3a disease.
Distinguishing between hypertrophic muscularis mucosae and muscularis propria can be problematic in transurethral resection specimens. (a) Tumor cell nests infiltrate into hypertrophic muscularis mucosae composed of thin and slender smooth muscle fibers (pT1). (b) Tumor cell nests invade into aggregates of thick muscular bundles (pT2)
Staging pT2 carcinoma in transurethral resection specimens. The diagnosis of pT2 urothelial carcinoma is favored when tumor cells surround some muscle bundles of the muscularis propria (a) or tumor cells are surrounded by muscle bundles of the muscularis propria (b) in transurethral resection specimens
Substaging of pT2 Bladder Carcinoma
pT2 carcinoma is subdivided into tumor extending into the superficial (i.e., inner half) MP (pT2a) and tumor extending into the deep (i.e., outer half) MP (pT2b). The clinical implication of this substaging is still uncertain [66], although several recent large studies have shown the clinical utility of this approach [74,75,76,77]. Using the middle of the MP as the cut-off seems to be profitable in pT2 substaging [67]. However, this substage is not recommended on TUR specimens.
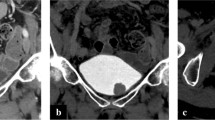
Stage pT3 Carcinoma
pT3 carcinoma is defined by tumor extending into perivesical soft tissue. The outer boundary of the MP is not well delineated, confounding the distinction between T2b and T3a carcinomas. However, distinguishing pT2b from pT3a disease is critical, because pT3 disease is usually treated with adjuvant chemotherapy [69, 78, 79]. Subclassification of muscle invasive tumors (>pT2) should be made only in cystectomy specimens. It is usually not feasible to document pT3a carcinoma in biopsy or TUR specimens because the outer MP boundary is irregular, with discontinuous MP muscle bundles separated by adipose tissue or fibroconnective tissue [26].
The MP outer boundary is irregular due to discrete muscle bundles that vary in size. Therefore, the clear line of demarcation of the outer MP boundary (junction of pT2b vs. pT3a) cannot be delineated, and the criteria of definition vary among expert pathologists. In an interobserver study tasked to assign stage on equivocal cases, three categories for delineating the outer MP boundary were used as follows: (1) drawing a straight horizontal line using the outermost MP bundle edges as reference for the MP-perivesical tissue boundary, (2) drawing multiple discontinuous lines between the outermost MP bundle edges, and (3) making a curved line along every outermost MP muscle bundle edges. The most commonly used approach was by interconnecting the outermost MP bundles edges with multiple straight lines [69]. The presence of lymphovascular invasion alone in perivesical soft tissue should not be considered pT3a, although this is not mentioned in the eighth edition of AJCC TNM staging manual [9, 67].
Substaging of pT3 Bladder Carcinoma
pT3 carcinoma is subdivided further into pT3a (i.e., microscopic invasion of perivesical soft tissue) and pT3b (i.e., macroscopic invasion of perivesical soft tissue). To date, pT3 substaging counts entirely on meticulous gross examination of perivesical soft tissue. Even in a tertiary institution, the presence or absence of macroscopic perivesical soft tissue involvement was not documented in 17% of pT3 cystectomy specimens [80]. Moreover, there is considerable debate about the prognostic significance of pT3 substaging [81,82,83,84,85,86]. However, it was adopted for use in the AJCC 2010 system [87]. An alternative approach has also been proposed to subdivide pT3 by measuring the depth of invasion into the perivesical soft tissue from the base of the MP (>4.5 mm) [88], but this approach remains to be clarified due to inconsistency in defining the MP base (outer boundary of the MP) [69].
Stage pT4 Carcinoma
pT4 carcinoma is defined as extravesical tumor directly invading adjacent organs or structures and is subcategorized into pT4a (direct invasion into the prostatic stroma, uterus, or vagina) and pT4b (direct invasion into the pelvic or abdominal wall) [9]. Overall, 11.7–19.2% and 1.9–4.4% of patients with radical cystectomy harbor pT4a or pT4b disease, respectively, according to recent studies [89, 90].
Substaging of pT4 Bladder Carcinoma
Prostatic Stromal Invasion
Prostatic stromal invasion by bladder cancer may occur by transmural extravesical, transmural bladder neck, and superficially intraurethral invasion [91,92,93]. Among these routes, transmural direct invasion of the prostatic stroma through extravesical fat or the bladder neck merits classification as pT4a. However, the third pathway of invasion of the prostate, superficially intraurethral invasion, has been a matter of debate. Cases with superficially intraurethral invasion of the prostatic stroma are not as aggressive as a true pattern of transmural invasion [92, 94,95,96,97,98]. Thus, the prior 2010 AJCC staging manual excluded intraurethral spread from pT4a [87], and Patel et al. validated this revision by showing that cases with subepithelial prostatic stromal invasion had more favorable outcomes compared to transmural pT4a disease [99]. Because of the ambiguity of defining prostatic stromal invasion in the previous AJCC staging manual [87], the new eighth edition AJCC staging manual clarified that intraurethral spread of urothelial carcinoma with prostatic stromal invasion should be assigned as pT2 according to urethral cancer staging and not bladder cancer staging, and the bladder tumor should be staged separately per bladder cancer staging [9]. Therefore, providing two separate pT stages is advocated. In cases of prostatic TUR specimens, rendering a definite pT stage is not recommended. In the absence of direct prostatic stromal invasion, explanatory comments should be given and the tumor staged at least as pT2 unless otherwise specified.
Seminal Vesicle Invasion
Seminal vesicle invasion may occur via direct bladder transmural perivesical soft tissue or intraepithelial extension from the prostate, and both have similarly poor prognosis (Fig. 18.13) [100]. However, the significance of seminal vesicle invasion through an intraurethral prostatic route is uncertain [101]. Direct seminal vesicle invasion is staged as pT4 according to the current eighth AJCC staging manual, but there is no further subclassification [9]. Studies demonstrate that seminal vesicle invasion has a more unfavorable effect on survival than prostatic stromal invasion alone and argue a prognosis comparable with pT4b tumor [100, 102, 103].
Gynecological Tract Invasion
Direct invasion of the uterus or vagina by bladder cancer is regarded as stage pT4a (Fig. 18.14) [9], and the incidence is relatively rare (3–6% of female cystectomy specimens) compared to prostatic stromal invasion (7–38% of male cystoprostatectomy specimens) [91,92,93,94,95,96,97, 104,105,106,107,108,109,110]. The involvement of urothelial carcinoma in the female gynecological tract either via pagetoid or metastatic spread would not be considered stage pT4a [9].
Pelvic or Abdominal Wall Invasion
Direct invasion of urinary bladder carcinoma into the pelvic or abdominal wall is assigned as stage pT4b [9]. Stage pT4b is uncommon due to the limited number of patients with this stage disease, constituting only 1.9–4.4% of all patients with radical cystectomy [89, 90].
Regional Nodal Staging (N Staging)
In the AJCC staging manual eighth edition, regional nodal staging in bladder cancer is determined by the number and location of positive lymph nodes, not by the number and size of positive lymph nodes [9]. In the previous edition, regional lymph nodes included the obturator, iliac (internal and external), sacral (lateral and sacral promontory), and common iliac lymph nodes [87]. In the current AJCC staging manual, perivesical lymph nodes are included as formal regional lymph nodes [9]. Regional nodal staging is classified as follows: (1) lymph nodes cannot be assessed (pNX); no lymph node metastasis (pN0); single regional lymph node metastasis in the true pelvis (pN1); multiple regional lymph node metastasis in the true pelvis (pN2); and metastasis to common iliac lymph nodes (pN3) [9]. Although reporting perinodal extension is not included in the AJCC staging manual eighth edition, it is recommended to report the presence or absence of extranodal extension as well as the total number of lymph nodes examined [9]. However, the minimum number of lymph nodes necessary to determine adequate pN staging has not been clarified yet for bladder cancer.
M Staging
Stage pM1 was previously designated for both non-regional lymph node metastasis and distant non-lymph node metastasis (Fig. 18.15) [87]. However, stage pM1 is now subdivided into non-regional lymph node metastasis (pM1a) and distant non-lymph node metastasis (pM1b) in the AJCC staging manual eighth edition [9] because patients with non-regional lymph node metastasis (pM1a) have a better clinical outcome than patients with distant non-lymph node metastasis (pM1b) [111].
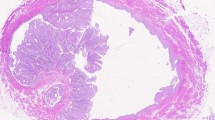
Staging of Bladder Carcinoma Arising in a Diverticulum
The AJCC staging manual eighth edition provides formal recommendations regarding tumors arising in a diverticulum (Fig. 18.16). Most bladder diverticula are acquired and lack an MP layer [112]. Thus, the tumor moves directly from pT1 carcinoma into pT3 carcinoma without invading the MP [112,113,114,115,116,117]. The AJCC staging manual eighth edition advises skipping the pT2 stage [9].
Urothelial carcinoma arising from a diverticulum of the urinary bladder. The diverticulum, a mucosal outpouching without a muscle layer, is in direct contact with perivesical soft tissue in the deep portion. Infiltrating urothelial carcinoma that developed in a diverticulum invades into subepithelial connective tissue. Squamous metaplasia is noted in the non-tumoral epithelium within the diverticulum
In conclusion, this chapter provides a comprehensive review with regard to bladder cancer staging including a reliable substaging method of each stage based on histoanatomic characteristics. In addition, confounding factors or diagnostic pitfalls in the staging of bladder cancer were discussed. The accurate staging is crucial to determine the prognosis and the prompt treatment option of bladder cancer patients. This chapter will offer a standardized guideline for bladder cancer staging to reduce disagreement in staging among pathologists and to define the optimal treatment for bladder cancer patients.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. https://doi.org/10.3322/caac.21551.
Alfred Witjes J, Lebret T, Comperat EM, Cowan NC, De Santis M, Bruins HM, Hernandez V, Espinos EL, Dunn J, Rouanne M, Neuzillet Y, Veskimae E, van der Heijden AG, Gakis G, Ribal MJ. Updated 2016 EAU guidelines on muscle-invasive and metastatic bladder Cancer. Eur Urol. 2017;71(3):462–75. https://doi.org/10.1016/j.eururo.2016.06.020.
Babjuk M, Bohle A, Burger M, Capoun O, Cohen D, Comperat EM, Hernandez V, Kaasinen E, Palou J, Roupret M, van Rhijn BW, Shariat SF, Soukup V, Sylvester RJ, Zigeuner R. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2016. Eur Urol. 2017;71(3):447–61. https://doi.org/10.1016/j.eururo.2016.05.041.
Chang SS, Bochner BH, Chou R, Dreicer R, Kamat AM, Lerner SP, Lotan Y, Meeks JJ, Michalski JM, Morgan TM, Quale DZ, Rosenberg JE, Zietman AL, Holzbeierlein JM. Treatment of non-metastatic muscle-invasive bladder cancer: AUA/ASCO/ASTRO/SUO guideline. J Urol. 2017;198(3):552–9. https://doi.org/10.1016/j.juro.2017.04.086.
Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, Pruthi R, Quale DZ, Ritch CR, Seigne JD, Skinner EC, Smith ND, McKiernan JM. Diagnosis and treatment of non-muscle invasive bladder Cancer: AUA/SUO guideline. J Urol. 2016;196(4):1021–9. https://doi.org/10.1016/j.juro.2016.06.049.
Gallan AJ, Choy B, Paner GP. Contemporary grading and staging of urothelial neoplasms of the urinary bladder: new concepts and approaches to challenging scenarios. Surg Pathol Clin. 2018;11(4):775–95. https://doi.org/10.1016/j.path.2018.07.006.
Brierley JGM, Wittekind C. TNM classification of malignant tumours. 8th ed. Chichester: John Wiley & Sons Inc; 2017.
Delahunt B, Egevad L, Samaratunga H, Varma M, Verrill C, Cheville J, Kristiansen G, Corbishley C, Berney DM. UICC drops the ball in the 8th edition TNM staging of urological cancers. Histopathology. 2017;71(1):5–11. https://doi.org/10.1111/his.13200.
Amin MBES, Greene FL, et al. AJCC cancer staging manual. 8th ed. Chicago: Springer; 2016.
Dalbagni G, Genega E, Hashibe M, Zhang ZF, Russo P, Herr H, Reuter V. Cystectomy for bladder cancer: a contemporary series. J Urol. 2001;165(4):1111–6.
Kassouf W, Spiess PE, Brown GA, Munsell MF, Grossman HB, Siefker-Radtke A, Dinney CP, Kamat AM. P0 stage at radical cystectomy for bladder cancer is associated with improved outcome independent of traditional clinical risk factors. Eur Urol. 2007;52(3):769–74. https://doi.org/10.1016/j.eururo.2007.03.086.
Palapattu GS, Shariat SF, Karakiewicz PI, Bastian PJ, Rogers CG, Amiel G, Lotan Y, Vazina A, Gupta A, Sagalowsky AI, Lerner SP, Schoenberg MP. Cancer specific outcomes in patients with pT0 disease following radical cystectomy. J Urol. 2006;175(5):1645–9.; discussion 1649. https://doi.org/10.1016/s0022-5347(05)00995-x.
Thrasher JB, Frazier HA, Robertson JE, Paulson DF. Does of stage pT0 cystectomy specimen confer a survival advantage in patients with minimally invasive bladder cancer? J Urol. 1994;152(2 Pt 1):393–6. https://doi.org/10.1016/s0022-5347(17)32746-5.
Volkmer BG, Kuefer R, Bartsch G Jr, Straub M, de Petriconi R, Gschwend JE, Hautmann RE. Effect of a pT0 cystectomy specimen without neoadjuvant therapy on survival. Cancer. 2005;104(11):2384–91. https://doi.org/10.1002/cncr.21475.
Yiou R, Patard JJ, Benhard H, Abbou CC, Chopin DK. Outcome of radical cystectomy for bladder cancer according to the disease type at presentation. BJU Int. 2002;89(4):374–8. https://doi.org/10.1046/j.1464-4096.2001.001020.x.
Kim HS, Jeong CW, Kwak C, Kim HH, Ku JH. Pathological T0 following cisplatin-based neoadjuvant chemotherapy for muscle-invasive bladder cancer: a network meta-analysis. Clin Cancer Res. 2016;22(5):1086–94. https://doi.org/10.1158/1078-0432.Ccr-15-1208.
Lavery HJ, Stensland KD, Niegisch G, Albers P, Droller MJ. Pathological T0 following radical cystectomy with or without neoadjuvant chemotherapy: a useful surrogate. J Urol. 2014;191(4):898–906. https://doi.org/10.1016/j.juro.2013.10.142.
Petrelli F, Coinu A, Cabiddu M, Ghilardi M, Vavassori I, Barni S. Correlation of pathologic complete response with survival after neoadjuvant chemotherapy in bladder cancer treated with cystectomy: a meta-analysis. Eur Urol. 2014;65(2):350–7. https://doi.org/10.1016/j.eururo.2013.06.049.
Pokuri VK, Syed JR, Yang Z, Field EP, Cyriac S, Pili R, Levine EG, Azabdaftari G, Trump DL, Guru K, George S. Predictors of complete pathologic response (pT0) to neoadjuvant chemotherapy in muscle-invasive bladder carcinoma. Clin Genitourin Cancer. 2016;14(1):e59–65. https://doi.org/10.1016/j.clgc.2015.09.013.
Shariat SF, Karakiewicz PI, Palapattu GS, Lotan Y, Rogers CG, Amiel GE, Vazina A, Gupta A, Bastian PJ, Sagalowsky AI, Schoenberg MP, Lerner SP. Outcomes of radical cystectomy for transitional cell carcinoma of the bladder: a contemporary series from the bladder Cancer research consortium. J Urol. 2006;176(6 Pt 1):2414–22.; discussion 2422. https://doi.org/10.1016/j.juro.2006.08.004.
Paner GP, Ro JY, Wojcik EM, Venkataraman G, Datta MW, Amin MB. Further characterization of the muscle layers and lamina propria of the urinary bladder by systematic histologic mapping: implications for pathologic staging of invasive urothelial carcinoma. Am J Surg Pathol. 2007;31(9):1420–9. https://doi.org/10.1097/PAS.0b013e3180588283.
Brimo F, Wu C, Zeizafoun N, Tanguay S, Aprikian A, Mansure JJ, Kassouf W. Prognostic factors in T1 bladder urothelial carcinoma: the value of recording millimetric depth of invasion, diameter of invasive carcinoma, and muscularis mucosa invasion. Hum Pathol. 2013;44(1):95–102. https://doi.org/10.1016/j.humpath.2012.04.020.
Cheng L, Neumann RM, Weaver AL, Spotts BE, Bostwick DG. Predicting cancer progression in patients with stage T1 bladder carcinoma. J Clin Oncol Off J Am Soc Clin Oncol. 1999;17(10):3182–7. https://doi.org/10.1200/jco.1999.17.10.3182.
Dixon JS, Gosling JA. Histology and fine structure of the muscularis mucosae of the human urinary bladder. J Anat. 1983;136(Pt 2):265–71.
Ro JY, Ayala AG, el-Naggar A (1987) Muscularis mucosa of urinary bladder. Importance for staging and treatment. Am J Surg Pathol 11(9):668–673. https://doi.org/10.1097/00000478-198709000-00002.
Philip AT, Amin MB, Tamboli P, Lee TJ, Hill CE, Ro JY. Intravesical adipose tissue: a quantitative study of its presence and location with implications for therapy and prognosis. Am J Surg Pathol. 2000;24(9):1286–90. https://doi.org/10.1097/00000478-200009000-00013.
Orsola A, Werner L, de Torres I, Martin-Doyle W, Raventos CX, Lozano F, Mullane SA, Leow JJ, Barletta JA, Bellmunt J, Morote J. Reexamining treatment of high-grade T1 bladder cancer according to depth of lamina propria invasion: a prospective trial of 200 patients. Br J Cancer. 2015;112(3):468–74. https://doi.org/10.1038/bjc.2014.633.
Paner GP, Montironi R, Amin MB. Challenges in pathologic staging of bladder cancer: proposals for fresh approaches of assessing pathologic stage in light of recent studies and observations pertaining to bladder Histoanatomic variances. Adv Anat Pathol. 2017;24(3):113–27. https://doi.org/10.1097/pap.0000000000000152.
Patriarca C, Hurle R, Moschini M, Freschi M, Colombo P, Colecchia M, Ferrari L, Guazzoni G, Conti A, Conti G, Luciano R, Magnani T, Colombo R. Usefulness of pT1 substaging in papillary urothelial bladder carcinoma. Diagn Pathol. 2016;11:6. https://doi.org/10.1186/s13000-016-0466-6.
Roupret M, Seisen T, Comperat E, Larre S, Mazerolles C, Gobet F, Fetissof F, Fromont G, Safsaf A, d’Arcier BF, Celhay O, Validire P, Rozet F, Irani J, Soulie M, Pfister C. Prognostic interest in discriminating muscularis mucosa invasion (T1a vs T1b) in nonmuscle invasive bladder carcinoma: French national multicenter study with central pathology review. J Urol. 2013;189(6):2069–76. https://doi.org/10.1016/j.juro.2012.11.120.
Andius P, Johansson SL, Holmang S. Prognostic factors in stage T1 bladder cancer: tumor pattern (solid or papillary) and vascular invasion more important than depth of invasion. Urology. 2007;70(4):758–62. https://doi.org/10.1016/j.urology.2007.06.638.
Angulo JC, Lopez JI, Grignon DJ, Sanchez-Chapado M. Muscularis mucosa differentiates two populations with different prognosis in stage T1 bladder cancer. Urology. 1995;45(1):47–53. https://doi.org/10.1016/s0090-4295(95)96490-8.
Bernardini S, Billerey C, Martin M, Adessi GL, Wallerand H, Bittard H. The predictive value of muscularis mucosae invasion and p53 over expression on progression of stage T1 bladder carcinoma. J Urol. 2001;165(1):42–6.; discussion 46. https://doi.org/10.1097/00005392-200101000-00011.
Bertz S, Denzinger S, Otto W, Wieland WF, Stoehr R, Hofstaedter F, Hartmann A. Substaging by estimating the size of invasive tumour can improve risk stratification in pT1 urothelial bladder cancer-evaluation of a large hospital-based single-Centre series. Histopathology. 2011;59(4):722–32. https://doi.org/10.1111/j.1365-2559.2011.03989.x.
Chang WC, Chang YH, Pan CC. Prognostic significance in substaging of T1 urinary bladder urothelial carcinoma on transurethral resection. Am J Surg Pathol. 2012;36(3):454–61. https://doi.org/10.1097/PAS.0b013e31823dafd3.
Faivre d’Arcier B, Celhay O, Safsaf A, Zairi A, Pfister C, Soulie M, Rozet F, Roupret M, Fromont G, Mazerolles C, Gobet F, Fetissof F, Irani J. T1 bladder carcinoma: prognostic value of the muscularis mucosae invasion (T1a/T1b). A multicenter study by the French urological association (CCAFU). Prog Urol. 2010;20(6):440–9. https://doi.org/10.1016/j.purol.2010.02.002.
Fransen van de Putte EE, Behrendt MA, Pigot GL, van der Kwast TH, van Rhijn BW. Prognostic significance of substage and WHO classification systems in T1 urothelial carcinoma of the bladder. Curr Opin Urol. 2015;25(5):427–35. https://doi.org/10.1097/mou.0000000000000202.
Hasui Y, Osada Y, Kitada S, Nishi S. Significance of invasion to the muscularis mucosae on the progression of superficial bladder cancer. Urology. 1994;43(6):782–6. https://doi.org/10.1016/0090-4295(94)90134-1.
Hermann GG, Horn T, Steven K. The influence of the level of lamina propria invasion and the prevalence of p53 nuclear accumulation on survival in stage T1 transitional cell bladder cancer. J Urol. 1998;159(1):91–4. https://doi.org/10.1016/s0022-5347(01)64021-7.
Holmang S, Hedelin H, Anderstrom C, Holmberg E, Johansson SL. The importance of the depth of invasion in stage T1 bladder carcinoma: a prospective cohort study. J Urol. 1997;157(3):800–3.; discussion 804. https://doi.org/10.1016/s0022-5347(01)65044-4.
Kondylis FI, Demirci S, Ladaga L, Kolm P, Schellhammer PF. Outcomes after intravesical bacillus Calmette-Guerin are not affected by substaging of high grade T1 transitional cell carcinoma. J Urol. 2000;163(4):1120–3.
Lee JY, Joo HJ, Cho DS, Kim SI, Ahn HS, Kim SJ. Prognostic significance of substaging according to the depth of Lamina Propria invasion in primary T1 transitional cell carcinoma of the bladder. Korean J Urol. 2012;53(5):317–23. https://doi.org/10.4111/kju.2012.53.5.317.
Mhawech-Fauceglia P, Fischer G, Alvarez V Jr, Ahmed A, Herrmann FR. Predicting outcome in minimally invasive (T1a and T1b) urothelial bladder carcinoma using a panel of biomarkers: a high throughput tissue microarray analysis. BJU Int. 2007;100(5):1182–7. https://doi.org/10.1111/j.1464-410X.2007.07090.x.
Nguyen-Huu Y, Delorme G, Lillaz J, Bedgedjian I, Le Ray-Ferrieres I, Chabannes E, Bernardini S, Guichard G, Bittard H, Kleinclauss F. Muscularis mucosae invasion: prognostic factor for intravesical BCG immunotherapy failure for T1 bladder carcinoma. Prog Urol. 2012;22(5):284–90. https://doi.org/10.1016/j.purol.2011.10.002.
Olsson H, Hultman P, Rosell J, Jahnson S. Population-based study on prognostic factors for recurrence and progression in primary stage T1 bladder tumours. Scand J Urol. 2013;47(3):188–95. https://doi.org/10.3109/00365599.2012.719539.
Orsola A, Cecchini L, Raventos CX, Trilla E, Planas J, Landolfi S, de Torres I, Morote J. Risk factors for positive findings in patients with high-grade T1 bladder cancer treated with transurethral resection of bladder tumour (TUR) and bacille Calmette-Guerin therapy and the decision for a repeat TUR. BJU Int. 2010;105(2):202–7. https://doi.org/10.1111/j.1464-410X.2009.08694.x.
Orsola A, Trias I, Raventos CX, Espanol I, Cecchini L, Bucar S, Salinas D, Orsola I. Initial high-grade T1 urothelial cell carcinoma: feasibility and prognostic significance of lamina propria invasion microstaging (T1a/b/c) in BCG-treated and BCG-non-treated patients. Eur Urol. 2005;48(2):231–8.; discussion 238. https://doi.org/10.1016/j.eururo.2005.04.013.
Palou J, Sylvester RJ, Faba OR, Parada R, Pena JA, Algaba F, Villavicencio H. Female gender and carcinoma in situ in the prostatic urethra are prognostic factors for recurrence, progression, and disease-specific mortality in T1G3 bladder cancer patients treated with bacillus Calmette-Guerin. Eur Urol. 2012;62(1):118–25. https://doi.org/10.1016/j.eururo.2011.10.029.
Patschan O, Sjodahl G, Chebil G, Lovgren K, Lauss M, Gudjonsson S, Kollberg P, Eriksson P, Aine M, Mansson W, Ferno M, Liedberg F, Hoglund M. A molecular pathologic framework for risk stratification of stage T1 urothelial carcinoma. Eur Urol. 2015;68(5):824–32.; discussion 835-826. https://doi.org/10.1016/j.eururo.2015.02.021.
Platz CE, Cohen MB, Jones MP, Olson DB, Lynch CF. Is microstaging of early invasive cancer of the urinary bladder possible or useful? Modern pathology: an official journal of the United States and canadian academy of pathology. Inc. 1996;9(11):1035–9.
Shariat SF, Weizer AZ, Green A, Laucirica R, Frolov A, Wheeler TM, Lerner SP. Prognostic value of P53 nuclear accumulation and histopathologic features in T1 transitional cell carcinoma of the urinary bladder. Urology. 2000;56(5):735–40. https://doi.org/10.1016/s0090-4295(00)00756-1.
Smits G, Schaafsma E, Kiemeney L, Caris C, Debruyne F, Witjes JA. Microstaging of pT1 transitional cell carcinoma of the bladder: identification of subgroups with distinct risks of progression. Urology. 1998;52(6):1009–13.; discussion 1013-1004. https://doi.org/10.1016/s0090-4295(98)00374-4.
Soukup V, Duskova J, Pesl M, Capoun O, Feherova Z, Zamecnik L, Hanus T, Babjuk M. The prognostic value of T1 bladder cancer substaging: a single institution retrospective study. Urol Int. 2014;92(2):150–6. https://doi.org/10.1159/000355358.
Sozen S, Akbal C, Sokmensuer C, Ekici S, Ozen H. Microstaging of pT1 transitional cell carcinoma of the bladder. Does it really differentiate two populations with different prognoses? (pT1 subcategory). Urol Int. 2002;69(3):200–6. https://doi.org/10.1159/000063941.
De Marco V, Cerruto MA, D’Elia C, Brunelli M, Otte O, Minja A, Luchini C, Novella G, Cavalleri S, Martignoni G, Artibani W. Prognostic role of substaging in T1G3 transitional cell carcinoma of the urinary bladder. Mol Clin Oncol. 2014;2(4):575–80. https://doi.org/10.3892/mco.2014.290.
van Rhijn BW, van der Kwast TH, Alkhateeb SS, Fleshner NE, van Leenders GJ, Bostrom PJ, van der Aa MN, Kakiashvili DM, Bangma CH, Jewett MA, Zlotta AR. A new and highly prognostic system to discern T1 bladder cancer substage. Eur Urol. 2012;61(2):378–84. https://doi.org/10.1016/j.eururo.2011.10.026.
Cheng L, Weaver AL, Bostwick DG. Predicting extravesical extension of bladder carcinoma: a novel method based on micrometer measurement of the depth of invasion in transurethral resection specimens. Urology. 2000;55(5):668–72. https://doi.org/10.1016/s0090-4295(99)00595-6.
Cheng L, Weaver AL, Neumann RM, Scherer BG, Bostwick DG. Substaging of T1 bladder carcinoma based on the depth of invasion as measured by micrometer: a new proposal. Cancer. 1999;86(6):1035–43. https://doi.org/10.1002/(sici)1097-0142(19990915)86:6<1035::aid-cncr20>3.0.co;2-d.
van der Aa MN, van Leenders GJ, Steyerberg EW, van Rhijn BW, Jobsis AC, Zwarthoff EC, van der Kwast TH. A new system for substaging pT1 papillary bladder cancer: a prognostic evaluation. Hum Pathol. 2005;36(9):981–6. https://doi.org/10.1016/j.humpath.2005.06.017.
Hu Z, Mudaliar K, Quek ML, Paner GP, Barkan GA. Measuring the dimension of invasive component in pT1 urothelial carcinoma in transurethral resection specimens can predict time to recurrence. Ann Diagn Pathol. 2014;18(2):49–52. https://doi.org/10.1016/j.anndiagpath.2013.11.002.
Leivo MZ, Sahoo D, Hamilton Z, Mirsadraei L, Shabaik A, Parsons JK, Kader AK, Derweesh I, Kane C, Hansel DE. Analysis of T1 bladder cancer on biopsy and transurethral resection specimens: comparison and ranking of T1 quantification approaches to predict progression to Muscularis Propria invasion. Am J Surg Pathol. 2018;42(1):e1–e10. https://doi.org/10.1097/pas.0000000000000964.
Farrow GM, Utz DC, Rife CC. Morphological and clinical observations of patients with early bladder cancer treated with total cystectomy. Cancer Res. 1976;36(7 pt 2):2495–501.
Lopez-Beltran A, Cheng L, Andersson L, Brausi M, de Matteis A, Montironi R, Sesterhenn I, van det Kwast KT, Mazerolles C. Preneoplastic non-papillary lesions and conditions of the urinary bladder: an update based on the Ancona international consultation. Virchows Arch. 2002;440(1):3–11. https://doi.org/10.1007/s00428-001-0577-6.
Lawless M, Gulati R, Tretiakova M. Stalk versus base invasion in pT1 papillary cancers of the bladder: improved substaging system predicting the risk of progression. Histopathology. 2017;71(3):406–14. https://doi.org/10.1111/his.13247.
Lopez-Beltran A, Cheng L. Stage pT1 bladder carcinoma: diagnostic criteria, pitfalls and prognostic significance. Pathology. 2003;35(6):484–91. https://doi.org/10.1080/00313020310001619127.
Cheng L, Montironi R, Davidson DD, Lopez-Beltran A. Staging and reporting of urothelial carcinoma of the urinary bladder. Mod Pathol 2009;22 Suppl 2:S70–95. https://doi.org/10.1038/modpathol.2009.1.
Magers MJ, Lopez-Beltran A, Montironi R, Williamson SR, Kaimakliotis HZ, Cheng L. Staging of bladder cancer. Histopathology. 2019;74(1):112–34. https://doi.org/10.1111/his.13734.
Jimenez RE, Keane TE, Hardy HT, Amin MB. pT1 urothelial carcinoma of the bladder: criteria for diagnosis, pitfalls, and clinical implications. Adv Anat Pathol. 2000;7(1):13–25.
Ananthanarayanan V, Pan Y, Tretiakova M, Amin MB, Cheng L, Epstein JI, Grignon DJ, Hansel DE, Jimenez RE, McKenney JK, Montironi R, Oliva E, Osunkoya AO, Rao P, Reuter VE, Ro JY, Shen SS, Srigley JR, Tsuzuki T, Yao JL, Antic T, Haber M, Taxy JB, Paner GP. Influence of histologic criteria and confounding factors in staging equivocal cases for microscopic perivesical tissue invasion (pT3a): an interobserver study among genitourinary pathologists. Am J Surg Pathol. 2014;38(2):167–75. https://doi.org/10.1097/pas.0000000000000096.
Huang J, Fu J, Zhan H, Xie K, Liu B, Yang F, Lu Y, Zhou X. Analysis of the absence of the detrusor muscle in initial transurethral resected specimens and the presence of residual tumor tissue. Urol Int. 2012;89(3):319–25. https://doi.org/10.1159/000341103.
Mariappan P, Finney SM, Head E, Somani BK, Zachou A, Smith G, Mishriki SF, N’Dow J, Grigor KM. Good quality white-light transurethral resection of bladder tumours (GQ-WLTURBT) with experienced surgeons performing complete resections and obtaining detrusor muscle reduces early recurrence in new non-muscle-invasive bladder cancer: validation across time and place and recommendation for benchmarking. BJU Int. 2012;109(11):1666–73. https://doi.org/10.1111/j.1464-410X.2011.10571.x.
Mariappan P, Zachou A, Grigor KM. Detrusor muscle in the first, apparently complete transurethral resection of bladder tumour specimen is a surrogate marker of resection quality, predicts risk of early recurrence, and is dependent on operator experience. Eur Urol. 2010;57(5):843–9. https://doi.org/10.1016/j.eururo.2009.05.047.
Shoshany O, Mano R, Margel D, Baniel J, Yossepowitch O. Presence of detrusor muscle in bladder tumor specimens--predictors and effect on outcome as a measure of resection quality. Urol Oncol. 2014;32(1):40.e17-22. https://doi.org/10.1016/j.urolonc.2013.04.009.
Gakis G, Schilling D, Renninger M, Seibold J, Sievert KD, Stenzl A. Comparison of the new American joint committee on cancer substratification in node-negative pT2 urothelial carcinoma of the bladder: analysis of patient outcomes in a contemporary series. BJU Int. 2011;107(6):919–23. https://doi.org/10.1111/j.1464-410X.2010.09548.x.
Ghoneim MA, Abdel-Latif M, el-Mekresh M, Abol-Enein H, Mosbah A, Ashamallah A, el-Baz MA. Radical cystectomy for carcinoma of the bladder: 2,720 consecutive cases 5 years later. J Urol. 2008;180(1):121–7. https://doi.org/10.1016/j.juro.2008.03.024.
Sonpavde G, Khan MM, Svatek RS, Lee R, Novara G, Tilki D, Lerner SP, Amiel GE, Skinner E, Karakiewicz PI, Bastian PJ, Kassouf W, Fritsche HM, Izawa JI, Ficarra V, Dinney CP, Lotan Y, Fradet Y, Shariat SF. Prognostic risk stratification of pathological stage T2N0 bladder cancer after radical cystectomy. BJU Int. 2011;108(5):687–92. https://doi.org/10.1111/j.1464-410X.2010.09902.x.
Tilki D, Reich O, Karakiewicz PI, Novara G, Kassouf W, Ergun S, Fradet Y, Ficarra V, Sonpavde G, Stief CG, Skinner E, Svatek RS, Lotan Y, Sagalowsky AI, Shariat SF. Validation of the AJCC TNM substaging of pT2 bladder cancer: deep muscle invasion is associated with significantly worse outcome. Eur Urol. 2010;58(1):112–7. https://doi.org/10.1016/j.eururo.2010.01.015.
Milowsky MI, Rumble RB, Booth CM, Gilligan T, Eapen LJ, Hauke RJ, Boumansour P, Lee CT. Guideline on muscle-invasive and metastatic bladder cancer (European Association of Urology guideline): American society of clinical oncology clinical practice guideline endorsement. J Clin Oncol Off J Am Soc Clin Oncol. 2016;34(16):1945–52. https://doi.org/10.1200/jco.2015.65.9797.
Witjes JA, Comperat E, Cowan NC, De Santis M, Gakis G, Lebret T, Ribal MJ, Van der Heijden AG, Sherif A. EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol. 2014;65(4):778–92. https://doi.org/10.1016/j.eururo.2013.11.046.
Tretter EM, Ebel JJ, Pohar KS, Zynger DL. Does the gross prosector impact pT3 subclassification or lymph node counts in bladder cancer? Hum Pathol. 2017;61:190–8. https://doi.org/10.1016/j.humpath.2016.12.009.
Boudreaux KJ Jr, Chang SS, Lowrance WT, Rumohr JA, Barocas DA, Cookson MS, Smith JA Jr, Clark PE. Comparison of American joint committee on Cancer pathologic stage T3a versus T3b urothelial carcinoma: analysis of patient outcomes. Cancer. 2009;115(4):770–5. https://doi.org/10.1002/cncr.24110.
Quek ML, Stein JP, Clark PE, Daneshmand S, Miranda G, Cai J, Groshen S, Cote RJ, Lieskovsky G, Quinn DI, Skinner DG. Microscopic and gross extravesical extension in pathological staging of bladder cancer. J Urol. 2004;171(2 Pt 1):640–5. https://doi.org/10.1097/01.ju.0000108664.39035.51.
Quek ML, Stein JP, Clark PE, Daneshmand S, Miranda G, Cai J, Groshen S, Lieskovsky G, Quinn DI, Raghavan D, Skinner DG. Natural history of surgically treated bladder carcinoma with extravesical tumor extension. Cancer. 2003;98(5):955–61. https://doi.org/10.1002/cncr.11569.
Scosyrev E, Yao J, Messing E. Microscopic invasion of perivesical fat by urothelial carcinoma: implications for prognosis and pathology practice. Urology. 2010;76(4):908–13.; discussion 914. https://doi.org/10.1016/j.urology.2010.02.073.
Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, Skinner E, Bochner B, Thangathurai D, Mikhail M, Raghavan D, Skinner DG. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1,054 patients. J Clin Oncol Off J Am Soc Clin Oncol. 2001;19(3):666–75. https://doi.org/10.1200/jco.2001.19.3.666.
Tilki D, Svatek RS, Karakiewicz PI, Novara G, Seitz M, Sonpavde G, Gupta A, Kassouf W, Fradet Y, Ficarra V, Skinner E, Lotan Y, Sagalowsky AI, Stief CG, Reich O, Shariat SF. pT3 substaging is a prognostic indicator for lymph node negative urothelial carcinoma of the bladder. J Urol. 2010;184(2):470–4. https://doi.org/10.1016/j.juro.2010.04.007.
Edge SBBD, Compton CC. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Zarei S, Frank I, Boorjian SA, Thompson RH, Kim S, Weight C, Tarrell R, Thapa P, Cheville JC. Prognostic significance of measured depth of invasion of urothelial carcinoma of the bladder compared to the 2010 American joint committee on Cancer pT2 and pT3 classifications. J Urol. 2012;188(5):1706–11. https://doi.org/10.1016/j.juro.2012.07.035.
Moschini M, Zamboni S, Mattei A, Baumeister P, Di Bona C, Cornelius J, Shariat SF, Freschi M, Zaffuto E, Salonia A, Montorsi F, Briganti A, Colombo R, Gallina A. Radical cystectomy in pathological T4a and T4b bladder cancer patients: is there any space for sub stratification? Urol Int. 2019;102(3):269–76. https://doi.org/10.1159/000493899.
Tilki D, Svatek RS, Karakiewicz PI, Isbarn H, Reich O, Kassouf W, Fradet Y, Novara G, Fritsche HM, Bastian PJ, Izawa JI, Stief CG, Ficarra V, Lerner SP, Schoenberg M, Dinney CP, Skinner E, Lotan Y, Sagalowsky AI, Shariat SF. Characteristics and outcomes of patients with pT4 urothelial carcinoma at radical cystectomy: a retrospective international study of 583 patients. J Urol. 2010;183(1):87–93. https://doi.org/10.1016/j.juro.2009.08.145.
Donat SM, Genega EM, Herr HW, Reuter VE. Mechanisms of prostatic stromal invasion in patients with bladder cancer: clinical significance. J Urol. 2001;165(4):1117–20.
Esrig D, Freeman JA, Elmajian DA, Stein JP, Chen SC, Groshen S, Simoneau A, Skinner EC, Lieskovsky G, Boyd SD, Cote RJ, Skinner DG. Transitional cell carcinoma involving the prostate with a proposed staging classification for stromal invasion. J Urol. 1996;156(3):1071–6.
Montironi R, Cheng L, Mazzucchelli R, Scarpelli M, Kirkali Z, Montorsi F, Lopez-Beltran A. Critical evaluation of the prostate from cystoprostatectomies for bladder cancer: insights from a complete sampling with the whole mount technique. Eur Urol. 2009;55(6):1305–9. https://doi.org/10.1016/j.eururo.2008.10.032.
Ayyathurai R, Gomez P, Luongo T, Soloway MS, Manoharan M. Prostatic involvement by urothelial carcinoma of the bladder: clinicopathological features and outcome after radical cystectomy. BJU Int. 2007;100(5):1021–5. https://doi.org/10.1111/j.1464-410X.2007.07171.x.
Knoedler JJ, Boorjian SA, Tollefson MK, Cheville JC, Thapa P, Tarrell RF, Frank I. Urothelial carcinoma involving the prostate: the association of revised tumour stage and coexistent bladder cancer with survival after radical cystectomy. BJU Int. 2014;114(6):832–6. https://doi.org/10.1111/bju.12486.
Njinou Ngninkeu B, Lorge F, Moulin P, Jamart J, Van Cangh PJ. Transitional cell carcinoma involving the prostate: a clinicopathological retrospective study of 76 cases. J Urol. 2003;169(1):149–52. https://doi.org/10.1097/01.ju.0000042810.43380.36.
Pagano F, Bassi P, Ferrante GL, Piazza N, Abatangelo G, Pappagallo GL, Garbeglio A. Is stage pT4a (D1) reliable in assessing transitional cell carcinoma involvement of the prostate in patients with a concurrent bladder cancer? A necessary distinction for contiguous or noncontiguous involvement. J Urol. 1996;155(1):244–7.
Vallo S, Gilfrich C, Burger M, Volkmer B, Boehm K, Rink M, Chun FK, Roghmann F, Novotny V, Mani J, Brisuda A, Mayr R, Stredele R, Noldus J, Schnabel M, May M, Fritsche HM, Pycha A, Martini T, Wirth M, Roigas J, Bastian PJ, Nuhn P, Dahlem R, Haferkamp A, Fisch M, Aziz A. Comparative analysis of the effect of prostatic invasion patterns on cancer-specific mortality after radical cystectomy in pT4a urothelial carcinoma of the bladder. Urol Oncol. 2016;34(10):432.e431-438. https://doi.org/10.1016/j.urolonc.2016.05.008.
Patel AR, Cohn JA, Abd El Latif A, Miocinovic R, Steinberg GD, Paner GP, Hansel DE. Validation of new AJCC exclusion criteria for subepithelial prostatic stromal invasion from pT4a bladder urothelial carcinoma. J Urol. 2013;189(1):53–8. https://doi.org/10.1016/j.juro.2012.09.006.
Daneshmand S, Stein JP, Lesser T, Quek ML, Nichols PW, Miranda G, Cai J, Groshen S, Skinner EC, Skinner DG. Prognosis of seminal vesicle involvement by transitional cell carcinoma of the bladder. J Urol. 2004;172(1):81–4. https://doi.org/10.1097/01.ju.0000132131.64727.ff.
Murphy WM, Crissman JD, Johansson SL, Ayala AG. Recommendations for the reporting of urinary bladder specimens that contain bladder neoplasms. Mod Pathol. 1996;9(7):796–8.
May M, Brookman-May S, Burger M, Gilfrich C, Fritsche HM, Rink M, Chun F, Fisch M, Roghmann F, Noldus J, Mayr R, Pycha A, Novotny V, Wirth M, Vallo S, Haferkamp A, Roigas J, Brisuda A, Stredele R, Volkmer B, Dechet C, Schnabel M, Denzinger S, Stief CG, Bastian PJ, Aziz A. Concomitant seminal vesicle invasion in pT4a urothelial carcinoma of the bladder with contiguous prostatic infiltration is an adverse prognosticator for cancer-specific survival after radical cystectomy. Ann Surg Oncol. 2014;21(12):4034–40. https://doi.org/10.1245/s10434-014-3827-y.
You D, Kim SC, Jeong IG, Hong JH, Ro JY, Ahn H, Kim CS. Urothelial carcinoma of the bladder with seminal vesicle invasion: prognostic significance. BJU Int. 2010;106(11):1657–61. https://doi.org/10.1111/j.1464-410X.2010.09494.x.
Ali-El-Dein B, Abdel-Latif M, Mosbah A, Eraky I, Shaaban AA, Taha NM, Ghoneim MA. Secondary malignant involvement of gynecologic organs in radical cystectomy specimens in women: is it mandatory to remove these organs routinely? J Urol. 2004;172(3):885–7. https://doi.org/10.1097/01.ju.0000133986.29257.bf.
Barocas DA, Patel SG, Chang SS, Clark PE, Smith JA Jr, Cookson MS. Outcomes of patients undergoing radical cystoprostatectomy for bladder cancer with prostatic involvement on final pathology. BJU Int. 2009;104(8):1091–7. https://doi.org/10.1111/j.1464-410X.2009.08558.x.
Chen ME, Pisters LL, Malpica A, Pettaway CA, Dinney CP. Risk of urethral, vaginal and cervical involvement in patients undergoing radical cystectomy for bladder cancer: results of a contemporary cystectomy series from M.D. Anderson Cancer Center. J Urol. 1997;157(6):2120–3.
Groutz A, Gillon G, Konichezky M, Shimonov M, Winkler H, Livne PM, Baniel J. Involvement of internal genitalia in female patients undergoing radical cystectomy for bladder cancer: a clinicopathologic study of 37 cases. Int J Gynecol Cancer. 1999;9(4):302–6. https://doi.org/10.1046/j.1525-1438.1999.99039.x.
Salem H, El-Mazny A. A clinicopathologic study of gynecologic organ involvement at radical cystectomy for bladder cancer. Int J Gynaecol Obstet. 2011;115(2):188–90. https://doi.org/10.1016/j.ijgo.2011.05.026.
Shen SS, Lerner SP, Muezzinoglu B, Truong LD, Amiel G, Wheeler TM. Prostatic involvement by transitional cell carcinoma in patients with bladder cancer and its prognostic significance. Hum Pathol. 2006;37(6):726–34. https://doi.org/10.1016/j.humpath.2006.01.027.
Varkarakis IM, Pinggera G, Antoniou N, Constantinides K, Chrisofos M, Deliveliotis C. Pathological review of internal genitalia after anterior exenteration for bladder cancer in women. Evaluating risk factors for female organ involvement. Int Urol Nephrol. 2007;39(4):1015–21. https://doi.org/10.1007/s11255-006-9158-6.
Galsky MD, Moshier E, Krege S, Lin CC, Hahn N, Ecke T, Sonpavde G, Godbold J, Oh WK, Bamias A. Nomogram for predicting survival in patients with unresectable and/or metastatic urothelial cancer who are treated with cisplatin-based chemotherapy. Cancer. 2013;119(16):3012–9. https://doi.org/10.1002/cncr.28146.
Hansel DE, Paner GP, Nese N, Amin MB. Limited smoothelin expression within the muscularis mucosae: validation in bladder diverticula. Hum Pathol. 2011;42(11):1770–6. https://doi.org/10.1016/j.humpath.2011.02.022.
Golijanin D, Yossepowitch O, Beck SD, Sogani P, Dalbagni G. Carcinoma in a bladder diverticulum: presentation and treatment outcome. J Urol. 2003;170(5):1761–4. https://doi.org/10.1097/01.ju.0000091800.15071.52.
Hu B, Satkunasivam R, Schuckman A, Miranda G, Cai J, Daneshmand S. Urothelial carcinoma in bladder diverticula: outcomes after radical cystectomy. World J Urol. 2015;33(10):1397–402. https://doi.org/10.1007/s00345-014-1472-5.
Idrees MT, Alexander RE, Kum JB, Cheng L. The spectrum of histopathologic findings in vesical diverticulum: implications for pathogenesis and staging. Hum Pathol. 2013;44(7):1223–32. https://doi.org/10.1016/j.humpath.2012.11.005.
Tamas EF, Stephenson AJ, Campbell SC, Montague DK, Trusty DC, Hansel DE. Histopathologic features and clinical outcomes in 71 cases of bladder diverticula. Arch Pathol Lab Med. 2009;133(5):791–6. https://doi.org/10.1043/1543-2165-133.5.791.
Walker NF, Gan C, Olsburgh J, Khan MS. Diagnosis and management of intradiverticular bladder tumours. Nat Rev Urol. 2014;11(7):383–90. https://doi.org/10.1038/nrurol.2014.131.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Choi, E., Park, S., Ro, J.Y. (2021). AJCC Staging of Bladder Cancers. In: Zhou, H., Guo, C.C., Ro, J.Y. (eds) Urinary Bladder Pathology. Springer, Cham. https://doi.org/10.1007/978-3-030-71509-0_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-71509-0_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-71508-3
Online ISBN: 978-3-030-71509-0
eBook Packages: MedicineMedicine (R0)