Abstract
With recent advances in technology, the surgical management of distal femur fractures has significantly improved. The use of locked plating technology with minimally invasive or less invasive surgical techniques is now a commonly preferred surgical management. Ultimately, treatment centers around the anatomic restoration of articular surface, functional alignment of articular unit to shaft with restoration of length, and alignment and rotation with the ultimate goal of early range of motion and mobilization. This chapter will focus on indications for plate and screw fixation of distal femur fractures, choice of implants based on fracture classification, various surgical approaches, and the postoperative care and follow-up.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Indications for Plate and Screw Fixation of Distal Femur Fractures
Distal femur fractures make up <1% of all fractures and approximately 3–6% of femoral fractures [1]. Patients who sustain such fractures have a primarily unimodal distribution. A small number of patients are young individuals who sustain accidental high-energy trauma. However, the primary group is elderly patients, usually female with poor bone stock and multiple medical comorbidities following low-energy mechanisms of injury [2].
Following this injury, goals of treatment are threefold: (1) anatomic restoration of articular surface; (2) functional restoration of the articular unit to shaft restoring length, alignment, and rotation; and (3) stable fixation to allow for early range of motion and mobilization [1, 3]. In the vast majority of patients, this means surgical intervention is indicated. Other treatment options may be indicated in nonoperative candidate patients, patients with non-displaced fractures, non-ambulatory patients, or patients with spinal cord injury. However, even in these patients, nonoperative management has been shown to lead to increased risk of stiffness, decubitus ulcers, wound complications, pulmonary complications, deep vein thrombosis, and deconditioning as compared to operative management [1, 4, 5].
Open reduction with plate and screw fixation of distal femur fractures has been shown in many studies to come with a high risk of wound and healing complications; this lead to the introduction and subsequent popularity of the retrograde femoral nail [6,7,8,9]. However, more recent advancements in locked plating technologies with minimally invasive or less invasive surgical techniques have led many to reconsider indications for plate and screw fixation of these types of fractures [9].
When considering the use of plate and screw fixation for distal femur fracture stabilization, a few factors must be taken into account: anatomy/geometry of the fracture, desired immediate postoperative activity level, previously placed hardware, and surgeon ability/familiarity with equipment and techniques [4].
A distinct advantage of locked plating fixation over intramedullary device utilization is the ability to adequately address very distal fractures of the femur. Locked plating devices allow for fragment-specific fixation in, and reduction of, intra-articular distal femur fractures such as in the case of AO/OTA 33-C3 fractures still amenable to fixation. Locking plates also allow one to provide a stable construct for extremely distal fractures, something that is difficult to provide with IM devices [10]. When a fracture is more proximal and anatomic reduction of fracture fragments is not necessary for optimal functional outcomes, this advantage is lost over intramedullary fixation techniques.
Plate and screw fixation of distal femur fractures have historically been too weak a construct to have the mechanical strength to bear the full weight of a patient, especially those with osteoporosis/osteopenia [11, 12]. All patients treated with such devices would consequently then be restricted to toe touch or non-weight-bearing on the operative extremity [11,12,13]. This was a marked disadvantage as compared to intramedullary nails or acute total knee arthroplasties performed for these fractures. However, newer plate and screw technologies are made of materials durable enough to potentially allow patients to bear weight immediately following operative fixation [13].
In the case of periprosthetic distal femur fractures, previously implanted hardware must be taken into consideration when choosing a stabilization technique [14]. In the case of total knee prosthesis, many femoral implants do not have an “open box” or sufficiently large enough opening to allow for access to the medullary canal through the prosthesis, while others have stemmed hardware which have already occupied the same space [14]. Techniques have been described in which the opening in the prosthesis is widened using a diamond-tipped burr to allow for supracondylar nail entry or an antegrade nail is utilized for fractures >8 cm superior to the femoral condyles [15, 16], although newer nail designs allow their use in fractures more distal. Some hip arthroplasty stems may also prohibit intramedullary fixation of such fractures. If the knee prosthesis is loose as in the case of Rorabeck III fractures, revision TKA is the appropriate choice for fixation [14, 17]. In cases other than those described previously, plate and screw fixation vs revision of arthroplasty hardware are the options remaining [14].
Surgeon skill and familiarity with the surgical technique has a significantly larger effect of outcomes after plate and screw fixation of distal femur fractures as compared to intramedullary nail fixation [18]. It has been shown that the low-volume surgeon has comparable success rates with intramedullary nailing of distal femur fractures as compared to higher-volume surgeons with greater experience [19]. However, in the case of minimally invasive locked plating fixation of distal femur fractures, surgeon experience has a major moderating factor on patient outcomes [19]. Patients treated by less experienced surgeons have more variable and overall worse outcomes when compared to highly experienced surgeons using the same systems for treatment of similar fractures [20].
7.2 Choice of Implants for the Plate and Screw Fixation of Distal Femur Fractures
As discussed above, the nature—or classification—of the fracture at the distal femur will help guide the choice of fixation. For intra-articular fracture components, absolute stability with anatomic reduction of articular fragments is paramount, followed by applying absolute versus relative stability principles to the extra-articular fracture components depending on the fracture patterns [21]. Conventional plating, fixed-angle plates with or without additional screw fixation, and locked plate fixation are three major options [19, 22]:
7.2.1 Conventional Plate Fixation
Despite many technological advances in plate and screw engineering, there remain some fracture geometries, like simple medial condyle fractures and Hoffa fragments, which are best managed via interfragmentary compression screws supplemented with a plate and screws in a position where they provide neutralization or a buttress function (Fig. 7.1).
7.2.2 Fixed-Angle Plate Fixation
As implied by the name, fixed-angle plates are implants that are “precontoured” with a constant angle between the plate blade or screw designed to fit the anatomy of the distal femur [4, 23] (Fig. 7.2). In most cases, they are used for simple fractures with metaphyseal comminution, extra-articular fractures, fractures in the supracondylar/intercondylar region, or fractures involving only one femoral condyle [4, 21,22,23]. With the advent of fixed-angle plates, there is a significant improvement in the success of treatment of distal femur fractures [19].
There are two main variants of the fixed-angle plate, the blade plate, and the dynamic condylar screw/compression plate. Blade plates are stable, rigid, and fixed-angle constructs that provide compression at the site of fractures [4, 23]. One of the most commonly used blade plates is the 95° plate [19, 22]. Given the shape of the plate, once inserted laterally, it will provide medial compression due to the valgus nature of the femur’s articular surface [23]. In order to be effective, the blade must be positioned approximately 2 cm proximal to the femoral joint line along the diaphyseal axis of the femur and over the anterior half of the femoral condyles [23]. Although a very good fixation device, there are disadvantages to its use, particularly in osteoporotic bone or cyclic stress loading situations, and due to the extensive surgical exposure required for insertion and less than optimal ability to address coronal plane fracture lines [4, 23]. From the blade plate design, dynamic condylar screw/compression plates (DCS) evolved with ability to provide epiphyseal lag screw fixation for fracture compression, particularly when there are intercondylar fracture lines [4, 23] (Fig. 7.3). The advantage was the less-extensive exposure needed and easier insertion technique [4, 23]. However, disadvantages are similar to the blade plate in terms of cyclic stress loading tolerance [4].
7.2.3 Locked Plate Fixation
As designs evolved in plate fixation, the use of minimally invasive techniques became more popular. Within distal femur fracture fixation, this led to the use of precontoured locked plates [4, 24]. An advantage of locked plate fixation is that constructs provide improved stability, which is particularly important when addressing osteoporotic bone (Fig. 7.4). Specifically, by locking the screw directly on the plate, the stability of the construct becomes independent of the interaction between the bone and the plate—a feature of fixed-angle devices [23]. Not only does this improve stability but also spares the devitalization of periosteum beneath the plate [19, 23]. Locked plates tend to have a precontoured design so as to allow reduction during insertion; in other words, the plate can be used as a reduction tool in the form of a mold [19, 23]. Additional advantages of novel locked plate designs are their ability to be inserted open or via minimally invasive approaches, all dependent on fracture pattern, degree of articular involvement, and experience of the surgeon [23]. Generally, longer plates are preferred so as to distribute stress and strain over long lengths of fixation constructs [19, 23]. Nevertheless, as in fixed-angle devices, plate placement is of utmost importance, with locked plates ideally placed parallel to the bone cortex and close to bone on AP view and aligned on lateral views with the intramedullary femoral canal [19, 23].
It is important to note that modern plating techniques have developed the ability to combine fixed-angle device features with locked plating advantages, thus creating hybrid constructs [19, 23]. By locking certain screw holes and utilizing nonlocking screws in others, a hybrid fixation with advantages of both constructs can be achieved to dial in appropriate stability to fractures based on bone quality and fixation construct [23]. Additionally, by using same plates, one can provide improved mechanical performance under torsional loads, particularly when using polyaxial locked screw fixation [19, 23].
7.3 Surgical Approaches to the Distal Femur for Plate and Screw Fixation
There are three main surgical approaches available for the insertion of plates for distal femur fracture fixation: (1) lateral, (2) medial, and (3) posterior approach [1, 4, 21, 25]. Some surgeons describe an anterior approach, which is usually a medial or lateral parapatellar approach and is discussed in the respective medial or lateral sections. Of note, minimally invasive submuscular approaches are also possible and are generally modifications of the above approaches.
7.3.1 Lateral Approach
A majority of distal femur fractures are addressed utilizing the lateral approach, usually combined with a lateral parapatellar arthrotomy (Fig. 7.1). This approach is particularly helpful if there is involvement of the articular surface and for the application of most plate constructs [1, 4, 21]. The approach involves the split of the iliotibial (IT) band in line with the skin incision, and the internervous plane between the vastus lateralis muscle and the lateral intermuscular septum overlaying the hamstring muscles [1, 25]. The vastus lateralis is elevated anteriorly which reveals the distal femur [1]; however, care should be taken with this maneuver, as the profunda femoris perforators lie in the region depending on the extent of proximal dissection. Perforators should be tied off carefully prior to continuing dissection. The minimally invasive modification generally involves an incision over the anterior half of the lateral femoral condyle in line with Gerdy’s tubercle over the joint line and through the IT band. If the incision is performed about the epicondyle, little vastus lateralis should be encountered, which is retracted anteriorly to expose the lateral aspect of the distal femur.
7.3.2 Medial Approach
The medial approach should be strongly considered for the plating of fractures on the medial femoral condyle [21]. The interval is between the vastus medialis and sartorius muscles (Fig. 7.1). Vastus medialis is elevated and sartorius is generally retracted posteriorly to reveal the adductor magnus muscle and its insertion to the adductor tubercle. Adductor magnus can then be retracted posteriorly to reveal the distal femur [1, 21]. During this approach, care should be taken, as the neurovascular bundle comprising the superficial femoral artery (transitioning to popliteal artery), femoral vein, and sciatic nerve (transitioning to common peroneal and tibial nerves) is encountered just posterior to the femur and beneath the adductor magnus [21].
This approach can be modified to fit the standard medial parapatellar approach to the distal femur/knee, such as in total knee arthroplasty, to help in the exposure of intra-articular fracture fragments [1].
7.3.3 Posterior Approach
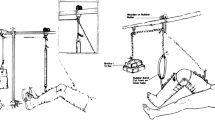
On rare occasions, a Hoffa fragment that is very posterior might need to be addressed. In these cases, a posterior approach to the knee is warranted for fragment fixation. The incision is centered midline at the popliteal fossa but is made in an S shape beginning proximal-laterally over the biceps femoris, then diagonally across the fossa and medial-distal over the medial gastrocnemius [25]. There is no formal interval, but once deep fascia is incised, extreme caution should be observed due to the number of important neurovascular structures encountered, including the tibial nerve medial and posterior to the semimembranosus and medial gastrocnemius, the common peroneal nerve lateral and posterior to the biceps femoris, and the popliteal artery and vein, both deep and medial to the tibial nerve [25] (Fig. 7.1). The approach can be extended proximally, with the important note that from proximal to distal, the sciatic nerve lies anterior to the biceps femoris, which runs in a medial to lateral course across the posterior thigh [25]. Therefore, for proximal posterior femur approaches, the biceps and sciatic should be retracted medially, whereas for more distal incisions, the biceps and sciatic should be retracted laterally [25] (Fig. 7.5).
Approaches to the distal femur. Green, lateral; blue, medial; orange, posterior; (1) femur; (2) popliteal a. and v.; (3) sciatic n. (3a common peroneal n., 3b tibial n.); (4) great saphenous v.; (5) quadriceps tendon; (6) vastus medialis; (7) vastus lateralis; (8) biceps femoris; (9) semimembranosus/semitendinosus; (10) gracilis; (11) patella; (12) lateral head of gastrocnemius; (13) medial head of gastrocnemius; (14) patellar tendon. Image art by Ivan Zapolsky, MD
7.4 Postoperative Course and Follow-Up After Plate and Screw Fixation of Distal Femur Fractures
Following plate and screw fixation of a distal femur fracture, a strict postoperative activity protocol is an important facet of success. Articular fractures require strict non-weight-bearing, while some types of fixation may allow weight-bearing immediately after surgery [26, 27]. Though rehabilitation after distal femur fractures has been poorly studied, literature suggests that postoperative protocols should include early mobilization and range of motion to reduce postoperative complications secondary to prolonged immobilization; low-force loading associated with immediate postoperative ROM has a beneficial effect on the healing of articular cartilage [3,4,5, 13, 26, 28]. Weight-bearing restrictions following plate and screw fixation of distal femur fractures depend on fracture geometry and patient factors. If the articular surface is involved in the fracture, a patient must have protected weight-bearing for 8–12 weeks with close follow-up and radiographic evidence of healing prior to advancement [26].
If the fracture is extra-articular, the surgeon should strive to provide a stable enough construct to allow a patient to be weight-bearing as tolerated immediately after surgery [18]. Provided that adequate length, alignment, and rotation were obtained, and the patient demonstrated minimal postoperative pain, immediate weight-bearing is recommended [18]. If the construct cannot provide this level of stability, a patient should be instructed to have protected weight-bearing. The patient may then be advanced after 6–8 weeks, as long as there is radiographic evidence of bone healing or callus formation [27, 29].
Gait training and knee motion with a hinged knee brace on postoperative day 1 with physical therapy has been shown to improve motion and function [1]. Utilizing a continuous passive motion machine may be necessary for patients unable to ambulate or incapable of moving the knee [3, 30]. Full knee extension should be emphasized during rehabilitation to prevent flexion contracture [1].
7.5 Clinical Case: Plate and Screw Fixation of a Distal Femur Fracture
A 24-year-old man was struck by an automotive, sustaining multiple injuries including an intra-articular distal femur fracture (Fig. 7.6). He was initially placed in a knee and ankle spanning external fixator (Fig. 7.7). The intra-articular component was addressed first through a medial parapatellar arthrotomy. Articular fragments were mobilized and reduced to form a single articular block. Once the articular block was restored, it was reduced as a unit back to the intact metadiaphysis utilizing the previously placed external fixation system and strategically placed bone clamps, restoring length, alignment, and rotation. An 18-hole variable angle curved condylar plate was placed on the lateral aspect of the femur in a submuscular fashion via a lateral approach. The plate was balanced and secured in place using k-wires. The plate was then secured with a nonlocking screw distally, and nonlocking screw proximally, just distal to the lesser trochanter, to compress the plate to bone and restore coronal and sagittal planes. The plate was then further secured utilizing hybrid fixation with locking screws distally and nonlocking screws proximally (Figs. 7.8 and 7.9).
References
Gwathmey FW, Jones-Quaidoo SM, Kahler D, Hurwitz S, Cui Q. Distal femoral fractures: current concepts. J Am Acad Orthop Surg. 2010;18:597–607.
Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–7.
Smith JRA, Halliday R, Aquilina AL, Morrison RJM, Yip GCK, McArthur J, Hull P, Gray A, Kelly MB, OTS COTS. Distal femoral fractures: the need to review the standard of care. Injury. 2015;46:1084–8.
Gangavalli AK, Nwachuku CO. Management of distal femur fractures in adults: an overview of options. Orthop Clin North Am. 2016;47:85–96.
Cass J, Sems SA. Operative versus nonoperative management of distal femur fracture in myelopathic, nonambulatory patients. Orthopedics. 2008;31:1091.
Handolin L, Pajarinen J, Lindahl J, Hirvensalo E. Retrograde intramedullary nailing in distal femoral fractures—results in a series of 46 consecutive operations. Injury. 2004;35:517–22.
Ebraheim NA, Liu J, Hashmi SZ, Sochacki KR, Moral MZ, Hirschfeld AG. High complication rate in locking plate fixation of lower periprosthetic distal femur fractures in patients with total knee arthroplasties. J Arthroplast. 2012;27:809–13.
Hoffmann MF, Jones CB, Sietsema DL, Koenig SJ, Tornetta P. Outcome of periprosthetic distal femoral fractures following knee arthroplasty. Injury. 2012;43:1084–9.
Ruchholtz S, Tomás J, Gebhard F, Larsen MS. Periprosthetic fractures around the knee-the best way of treatment. Eur Orthop Traumatol. 2013;4:93–102.
Langford J, Burgess A. Nailing of proximal and distal fractures of the femur: limitations and techniques. J Orthop Trauma. 2009;23:S22–5.
Zlowodzki M, Williamson S, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system and the 95-degree angled blade plate for the internal fixation of distal femur fractures in human cadaveric bones with high bone mineral density. J Trauma: Injury, Infection, and Critical Care. 2006;60:836–40.
Zlowodzki M, Williamson S, Cole PA, Zardiackas LD, Kregor PJ. Biomechanical evaluation of the less invasive stabilization system, angled blade plate, and retrograde intramedullary nail for the internal fixation of distal femur fractures. J Orthop Trauma. 2004;18:494–502.
Poole WEC, Wilson DGG, Guthrie HC, Bellringer SF, Freeman R, Guryel E, Nicol SG. “Modern” distal femoral locking plates allow safe, early weight-bearing with a high rate of union and low rate of failure: five-year experience from a United Kingdom major trauma Centre. Bone Joint J. 2017;99-B:951–7.
Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004;12:12–20.
Maniar RN, Umlas ME, Rodriguez JA, Ranawat CS. Supracondylar femoral fracture above a PFC posterior cruciate-substituting total knee arthroplasty treated with supracondylar nailing. A unique technical problem. J Arthroplasty. 1996;11:637–9.
Hanks GA, Mathews HH, Routson GW, Loughran TP. Supracondylar fracture of the femur following total knee arthroplasty. J Arthroplasty. 1989;4:289–92.
Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999;30:209–14.
Ehlinger M, Adam P, Abane L, Arlettaz Y, Bonnomet F. Minimally-invasive internal fixation of extra-articular distal femur fractures using a locking plate: tricks of the trade. Orthop Traumatol Surg Res. 2011;97:201–5.
Collinge CA, Gardner MJ, Crist BD. Pitfalls in the application of distal femur plates for fractures. J Orthop Trauma. 2011;25:695–706.
Hierholzer C, Rüden C, Pötzel T, Woltmann A, Bühren V. Outcome analysis of retrograde nailing and less invasive stabilization system in distal femoral fractures: a retrospective analysis. Indian J Orthop. 2011;45:243–15.
Beltran MJ, Gary JL, Collinge CA. Management of distal femur fractures with modern plates and nails: state of the art. J Orthop Trauma. 2015;29:165–72.
Miller MD, Thompson SR, Hart J. Miller’s review of orthopaedics. Philadelphia: Elsevier Health Sciences; 2015.
Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res. 2013;99:353–60.
Collinge CA, Sanders RW. Percutaneous plating in the lower extremity. J Am Acad Orthop Surg. 2000;8:211–6.
Hoppenfeld S, de Boer P, Buckley R. Surgical exposures in Orthopaedics: the anatomic approach. Philadelphia: Lippincott Williams & Wilkins; 2016.
Smith TO, Hedges C, MacNair R, Schankat K. Early rehabilitation following less invasive surgical stabilisation plate fixation for distal femoral fractures. Physiotherapy. 2009;95:61–75.
Smith WR, Stoneback JW, Morgan SJ, Stahel PF. Is immediate weight bearing safe for periprosthetic distal femur fractures treated by locked plating? A feasibility study in 52 consecutive patients. Patient Saf Surg. 2016;10:26.
Salter RB, Simmonds DF, Malcolm BW, et al. The biological effect of continuous passive motion on the healing of full-thickness defects in articular cartilage. J Bone Joint Surg Am. 1980;62(8):1232–51.
Smith TO, Hedges C, MacNair R, Schankat K, Wimhurst JA. The clinical and radiological outcomes of the LISS plate for distal femoral fractures: a systematic review. Injury. 2009;40:1049–63.
Henderson CE, Lujan TJ, Kuhl LL, Bottlang M, Fitzpatrick DC, Marsh JL. 2010 mid-America Orthopaedic association physician in training award: healing complications are common after locked plating for distal femur fractures. Clin Orthop Relat Res. 2011;469:1757–65.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Canseco, J.A., Zapolsky, I.J., Prakash, P.S., Donegan, D.J. (2021). Plate and Screw Osteosynthesis of Distal Femur Fractures. In: Hanschen, M., Biberthaler, P., Waddell, J.P. (eds) Knee Fractures . Strategies in Fracture Treatments. Springer, Cham. https://doi.org/10.1007/978-3-030-81776-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-81776-3_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81775-6
Online ISBN: 978-3-030-81776-3
eBook Packages: MedicineMedicine (R0)