Abstracts
Deep brain stimulation (DBS) is a reversible technique of functional neurosurgery that is applied in pediatric patients for the treatment of movement disorders. It is a safe and effective technique especially in isolated dystonia or combined with myoclonus. Patient selection is essential. Two electrodes are implanted at the level of the Globus Pallidus internus (GPi) using stereotactic techniques, and a neurostimulator and connecting cables are implanted subcutaneously. Despite the relative high cost of this therapy, it is cost-efficient and represents a gain in QUALY (quality-adjusted life-year). Children affected of these disorders have specific needs and technical peculiarities, so that performing this therapy in a specifically pediatric multidisciplinary movement disorders unit is recommended.
In this chapter authors review current indications of DBS, the anatomical substrate of dystonia, its classification and genetic basis in the pediatric age, its assessment with the Burke-Fahn-Marsden Rating Scale, DBS surgical technique, stimulation programming, complications and adverse events, always focusing on pediatric patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Deep brain stimulation
- DBS
- Movement disorders
- Pediatric deep brain stimulation
- Pediatric movement disorders
- Surgery for movement disorders
- Dystonia
- Pediatric dystonia
- Pediatric functional neurosurgery
1 Introduction
Deep brain stimulation (DBS) is a reversible technique of functional neurosurgery that is applied for the symptomatic treatment of hypokinetic (Parkinson’s disease) and hyperkinetic movement disorders (tremor, dystonia , myoclonus, dyskinesias and Tourette syndrome) [1], as well as neuropsychiatric disorders.
DBS was developed initially in 1960s as a technique to treat neuropathic pain, without notably good results, while movement disorders , especially parkinsonian and essential tremors, were treated around that time by lesions in various targets of the basal ganglia. Levodopa and the complications of ablative surgery sent DBS to oblivion until 1987, when the effect of high frequency stimulation mimicking a lesion allowed thalamic stimulation to treat tremor safely [2]. Afterwards, different targets have been explored and indications have expanded.
DBS obtained CE marking as a treatment for essential tremor in 1993, for Parkinson’s disease in 1998, for dystonia in 2003, for obsessive-compulsive disorder in 2009, and for epilepsy in 2010. The FDA approved DBS for essential tremor in 1997, for Parkinson’s disease in 2002, for dystonia in 2003, for obsessive-compulsive disorder in 2009, and for epilepsy in 2018. There are clinical trials for chronic pain, major depression, Tourette syndrome, epilepsy, obesity, anorexia and Alzheimer’s disease.
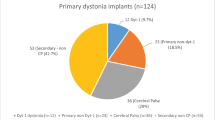
DBS in children has been applied predominantly for the treatment of dystonia [3, 4], although it has also been applied to other hyperkinetic movement disorders (chorea, tardive dyskinesias, etc.) [5]. Considering this fact, this chapter will refer first and foremost to dystonia.
Dystonia is defined as “a movement disorder produced by a simultaneous and sustained tonic contraction of agonist and antagonist muscles causing abnormal postures, repetitive and twisted movements, weakness, and osteo-articular deformities” [6].
Pallidotomy had previously demonstrated its effectiveness for tardive dyskinesias in Parkinson’s disease and for dystonia [7,8,9], but the long-term decrease in efficacy [10] led to the application of deep brain stimulation techniques. However, pallidotomy continues to play a role in selected cases [11, 12].
Without treatment, dystonia is associated with serious complications such as skeletal deformities, language difficulties (dysarthria or anarthria, dysphonia or aphonia), feeding difficulties (dysphagia, malnutrition), respiratory problems, sleep disorders, pain and a high degree of dependency for all activities of everyday life. It should be noted that, in most cases, cognitive functions are preserved, being the patients aware of their situation [1].
2 Basal Ganglia Anatomy
Dystonia has traditionally been considered a disease of the basal ganglia and thalamus, though more recently it has been emphasized that dystonia arises as a consequence of disruptions across a much broader whole-brain network, including regions of the cerebral cortex, brainstem and cerebellum. The input nuclei of the basal ganglia, the caudate, and putamen, receive excitatory input from almost all cortical areas. The main output nuclei are the internal segment of the globus pallidus (GPi) and the substantia nigra pars reticularis (SNpr) . The GPi sends inhibitory outputs to pallidal receiving areas of the motor thalamus and brainstem nuclei [13]. A schematic representation appears in Fig. 41.1.
Schematic representation of the connections of the basal ganglia, thalamus and cerebellum. Excitatory connections are represented by red arrows, inhibitory connections by blue arrows. Abbreviations: GPe Globus Pallidus Externa, GPi Globus Pallidus Interna, SNc Substantia Nigra Pars compacta, SNr Substantia Nigra Pars Reticulata, STN Subthalamic Nucleus. Modified from Lumsden et al. [13]
3 Classification of Dystonia in the Pediatric Age
A new classification scheme for dystonia was proposed in 2013 by Albanese et al. [6]. The diagnosis of dystonia was divided into two main axes: (1) the clinical features and (2) etiology. See Table 41.1.
This classification of Albanese is an evolution of the classical and etiogical division of dystonia into primary and secondary dystonia. Currently, the term “primary dystonia” is used as an etiological descriptor for genetic or idiopathic cases in which dystonia is isolated and there is no consistent pathologic change. While the term “secondary dystonia” may indicate non-isolated dystonia , a defined pathology or more generally a known etiology. The known genetic causes of dystonia presenting in childhood are summarized in Table 41.2.
Concepts relating to “pure dystonia” and “dystonia plus” syndromes are useful for clinical application, and they are based on phenomenology, not etiology. While etiology provides the organizational principle for “heredodegenerative” and most “secondary” categories. Secondary dystonia usually presents with evidence of structural lesions (bilirubin encephalopathy or kernicterus, inborn errors of metabolism like Lesch Nyhan or glutaric aciduria) or degeneration (abnormal iron deposition in Neurodegeneration with Brain Iron Accumulation disorders). Furthermore, this term could be associated with acquired causes of dystonia (perinatal brain injury, infection, neoplastic) [6, 14, 15].
Dystonia is usually a fluctuating state, and clinically the intensity varies. At its most extreme, periods of severe dystonia may be life-threatening and the most commonly used term to describe this condition is “status dystonicus”. Manji et al. described the condition as an increasingly frequent and severe episodes of generalized dystonia which require urgent hospital admission [16, 17].
4 Dystonia Assesment: The Burke-Fahn-Marsden Dystonia Rating Scale
The Burke-Fahn-Marsden Dystonia Rating Scale (BFM-DRS) [18] was introduced to assess generalized dystonia patients. It is composed of a motor part assessing dystonia and a part assessing the resulting disability. The motor subscale evaluates two clinical features of dystonia (severity and provoking factors) in eight body regions (eyes, mouth, neck, and the four limbs) and one functional area (speech and swallowing). Severity ranges from 0 (no dystonia) to 4 (severe dystonia). The provoking factors assess the situation under which dystonia occurs and range from 0 (no dystonia) to 4 (dystonia at rest). These two features, severity and provoking factors, are multiplied and then scores are summed, except for the eyes mouth and neck which are halved before summing as they are considered regions of lower weight. The resulting maximum total score on the BFM severity is 120. The BFMDR S section on disability assesses the effects of dystonia on ADL (speech, handwriting, feeding, eating/swallowing, hygiene, dressing, and walking), and the total maximum score is 30 [19]. A scheme of BFM-DRS is shown in Table 41.3.
5 Treatment of Dystonia
The medical treatment of generalized dystonia is ineffective in most cases [20]. In patients with dystonia and parkinsonism (e.g. mutations in the Parkin gene), or in those with primary defects in dopaminergic synthesis (e.g. Segawa disease), dystonia can be dopa-sensitive and improve significantly with levodopa. In the remaining dystonias, anticholinergic drugs, dopamine antagonists, baclofen or benzodiazepines commonly produce minimal clinical benefits and great side effects. Botulinum toxin is useful only in focal dystonia. However, different from adults in whom dystonia is usually focal or segmental, in children dystonia is more frequently generalized and could be rapidly progressive [21]. The intrathecal baclofen pump can improve muscle tone, but not motor function, and consequently has a palliative indication in “secondary dystonia” [22].
Bilateral DBS is the treatment of choice in “primary dystonia” refractory to medical treatment and has also been applied in other secondary dystonia with partial clinical improvement [23]. Status dystonicus (SD), a medical emergency that could result of heterogeneous conditions with nonuniform underlying physiology, is potentially reversible. DBS is considered the most efficient therapeutic approach and should be proposed early in its treatment of SD [24, 25].
6 Efficacy of DBS in Dystonia
Across all patients reviewed by Hale et al. BFMDRS-M scores improved 43.8 ± 36 after surgery with 45% of individuals achieving ≥50% improvement, while BFMDRS-D improved by 43.7 ± 31 with 45% achieving ≥50% improvement [20]. As we have discussed previously , the efficacy of DBS will depend on the etiology of dystonia:
-
A.
Primary dystonia (DYT-TOR1A, DYT-SCGE or without identifiable genetic cause):
The efficacy of DBS in generalized idiopathic dystonia has been demonstrated in various centers worldwide [26,27,28,29]. Patients with primary dystonia are more likely to experience >50% improvement in BFMDRS-M scores after surgery compared to patients with other causes of dystonia. Improvement ranges from 63 ± 31% [30]. There is a better prognosis in pediatric patients and young adults, with a short time of evolution, who have not developed osteo-articular deformities, and in dystonia with a greater phasic component than in those with severe tonic postures. Patients with mutations in the TOR1A gene [31] and SGCE gene [32], also called myoclonic dystonia, have the best prognosis. The motor improvement of dystonia is associated with an improvement in functional capacity for activities of daily life and a better quality of life. Cognitive functions are not modified by DBS [33].
-
B.
Secondary dystonia
Patients with secondary dystonia obtain less benefit from surgery than those with primary dystonia [34]. In patients with secondary dystonia, the improvement in the BFMDRS scale would be 10–25%, but sustained over time [35,36,37] and preventing the appearance of contractures, which is why they are also considered candidates for surgery. The benefit of surgery seems to be conditioned by the structural integrity of the basal ganglia [38].
Patients with dystonia secondary to infantile cerebral palsy (PCI) require special mention. PCI is the most common cause of dystonia in children. About 10% of patients with PCI present a dyskinetic form. Early improvement of muscle tone and dystonic postures could prevent progression towards fixed contractures and dependency [39, 40].
Secondary dystonia caused by neurometabolic diseases has also been treated with DBS. Among them, pantothenate kinase deficiency (the most frequent NBIA disorder) shows an improvement of 24–80% [41, 42].
In some cases, a patient could present a complex movement disorder, with dystonia that could be associated with choreoathetosis. Chorea-Acanthocytosis or GNAO1-related encephalopathy are two examples that have demonstrated good response to GPi-DBS [43, 44].
In both primary and secondary dystonias efficacy correlates inversely with the duration of the disease [45,46,47].
Table 41.4 summarizes the efficacy of DBS based on the etiology.
8 The Importance of Patient Selection
Appropriate patient selection will be based on a multidisciplinary evaluation including pediatric neurologists, neurosurgeons, rehabilitators and neuropsychologists. All of these members should be familiar with understanding when during the course of each illness it is appropriate to consider the use of DBS.
Patients referred for DBS surgery for treatment of dystonia should undergo a detailed history of illness and physical examination to determine the dystonia type and possible etiology. As mentioned, DBS is most often indicated in the treatment of isolated dystonias or “primary dystonias”. In this group, profound improvements in the severity of dystonia have been reported, maintaining the beneficial effect for several years. On the other hand, symptomatic or “secondary dystonia” is known to be less responsive to DBS, the reasons for which remain unclear. A special mention is required for status dystonicus, due to different etiological conditions, where outcomes improved in recent years, potentially as a consequence of increasing use of DBS [13, 17].
In recent years, some progress has been made in the patient selection process. Somatosensory Evoked Potentials (SEPs) and Central Motor Conduction Times (CMCT) have been recently studied as predictors of the outcome from Deep Brain Stimulation (DBS). Accordingly, better outcome was seen in those children with normal versus abnormal CMCT or normal versus abnormal SEPs. These associations were independent of dystonia etiology and cranial MRI findings; therefore, they can exceedingly contribute to patient selection in “secondary dystonia” [50].
Reasonable expectations on the part of the patient and their family regarding the outcome from DBS treatment should be discusses and must cover the less positive results reported for dysphonia and dysarthria and the development of tolerance to DBS in some cases. In the case of neurodegenerative “secondary dystonias” (e.g. NBIA) it is also essential to remark on the possible loss of beneficial effect secondary to the evolution of the disease [42, 51].
The features of dystonia should be monitored before DBS using the most appropriate among the available dystonia scales (BFMDRS).
General preoperative screening of cognition in patients with dystonia to evaluate baseline cognitive status and monitor for possible postoperative changes is recommended, although, the current evidence suggests that Gpi DBS does not cause cognitive decline in primary dystonia [52]. Similarly, assessment of quality of life (QoL) is crucial to determine the impact of the surgery on Activities of daily living [19].
Once a dystonia patient has been properly evaluated and screened for DBS, it is important to counsel the patient on the degree of expected improvement in symptoms with DBS treatment . Patients with primary generalized dystonia generally have the best outcome, with improvements of 50–70% as measured by the BFMDRS movement score commonly achieved. In the contrary, secondary dystonia typically responds more modestly (10–20%), although this level of improvement can be clinically significant.
Patients and parents additionally need to understand that the benefits of DBS will take time to accrue, considering that a number of visits may be required to optimize DBS programming.
9 Surgical Technique
Deep brain stimulation (DBS) surgery in dystonic patients basically consists in placing two brain electrodes usually at the dorsal and posterior part of the Globus Pallidus internus (GPi), a neurostimulator and two connecting cables between the pallidal electrodes and the neurostimulator [53]. The subthalamic nucleus (STN) has also been postulated as a stimulation target isolated [54, 55] or combined with the GPi [56].
In adult patients this surgery is usually performed in two stages: placement of the brain electrodes with the patient awake under local anesthesia during the first stage, and the neurostimulator and the connecting cables with the patient under general anesthesia on the second one. In our pediatric patients, we prefer to perform it under general anesthesia in a single stage and monitor the electrode placement using intraoperative neurophysiological techniques [57, 58]. However, there are hospitals that also operate pediatric patients awake [59].
The surgical technique for placing the electrodes at the level of the GPi has evolved enormously in recent years and there is great variability between surgeons and hospitals. However, in all cases it is based on stereotaxic principles.
Stereotaxic coordinates based on the Schaltenbrand-Wahren [60] and Talairach [61] atlas were initially used to locate the GPi. At present, direct MRI localization is preferable [53]. The target is chosen on an axial slice at the level of the anterior commissure (AC) at the junction between the two posterior quarters of the GPi. The software automatically calculates x, y and z coordinates. See Fig. 41.2a, b. The electrode direction is planned in the anterolateral direction as vertical as possible avoiding vessels, sulci and ventricles. Finally, it is confirmed that the position of the contacts is included in the GPi and that the tip of the electrode or its projection touches the lateral border of the optic tract in the three planes [57].
Target location and systems for electrodes insertion: (a) GPi target chosen on an axial slice at the level of the (AC) commissure at the junction between the two posterior quarters of the GPi. (b) The trajectory ends at the lateral border of the optic tract. (c) Leksell® stereotaxic frame. (d) Nexframe® neuronavigation guided system. (e) Neuromate® stereotaxic robot. (f) STarFix® and (g) Clearpoint® system
A stereotaxic framework (such as Leksell®), a neuronavigation-based guidance system (Nexframe®), a robotic arm (Neuromate® or Rosa®) [55, 62], a 3D printed disposable frame (STarFix®) [63] or a MR-guided system (Clearpoint®) [64] can be used to execute the trajectory. All these systems are based on stereotaxic coordinates. Some of these stereotaxic systems are shown in Fig. 41.2c–g.
10 Neurostimulation
The electrophysiological basis of this treatment is still unknown. High-frequency electrical stimulation through implanted electrodes mimics the effects of lesioning procedures previously employed (thalamotomies, pallidotomies or subthalamotomies), suggesting the inhibition of the circuit of neurons that with their abnormal functioning contribute to the movement disorder . On the contrary, low-frequency stimulation provokes fiber activation [65].
Different mechanisms of action that would combine inhibitory and excitatory processes have been proposed: jamming of a feedback loop, activation of inhibitory structures included in a more complex network, blockade of membrane ion channels, depolarization blockade, synaptic exhaustion, induction of early genes, changes in local blood flow, neuroplasticity, among others [65].
These different mechanisms vary in importance depending on the pathology to be treated and the target stimulated and it is probable that some are more involved in the acute effects and others in the long term changes, close to neuroplasticity [65].
This modulation of neuronal activity does not generate irreversible anatomic lesions in the stimulation zones, but rather produces a reversible clinical effect and the patient could return to his baseline clinical situation in the event of system disconnection. This disconnection should be performed progressively to avoid a “rebound effect”.
On the contrary, fiber bundles are consistently activated at low or high frequencies. The hypothetical mechanisms envisioned should therefore be compatible and even produce these observed effects, to be acceptable as hypotheses. The mechanism could be either one or a combination of several causes: jamming of a feedback loop, activation of inhibitory structures included in a more complex network, blockade of membrane ion channels, depolarization blockade, synaptic exhaustion, induction of early genes, changes in local blood flow, neuroplasticity, etc. It is probable that some are more involved in the acute effects and others in the long-term changes, close to neuroplasticity.
Commercial neurostimulation systems allow to choose different stimulation modalities: monopolar or bipolar between different contacts located at different levels or orientations (Directional stimulation [66]) and to regulate the amplitude, the duration and the frequency of the electrical stimulus.
11 Early Postoperative Management and Initial Deep Brain Stimulation Programming
At least a 3–5-day in-hospital stay after DBS implantation is recommended for wound healing and effective postoperative pain management. When to start DBS programming to check benefits and side effects from stimulation settings varies in different centers from 2 days to 1 month [67]. The initial programming process begins with the review of the preoperative and intraoperative data. Checking electrodes placement post-operatively using MRI protocols is strongly advised.
Currently, certain software (e.g. SureTune® Medtronic) provide patient-specific visualization of lead location and simulated 3-dimensional volume of tissue activation helping make decisions on how to start programming the DBS therapy.
Regarding dystonia , there is a considerable heterogeneity of patients’ features and stimulation settings. It must be pointed out that dystonia requires a prolonged period of stimulation in order to appreciate a symptomatic benefit, in contrast to rigidity and tremor. This is indeed also the case of tonic component of dystonia, while the phasic component may improve early after stimulation [68].
At our center, DBS in-patient stimulation begins 48 h after surgery on electrodes 0 or 1 in monopolar configuration with standard parameters: 1.5 V 60 μs 130 Hz that are maintained until the first revision 1 month later. A wide range of stimulation parameters has been shown to be effective for GPi DBS in dystonia and these initial parameters may vary from center to center. Many dystonic patients benefit from the insertional trauma-related effect in the immediate postoperative period; therefore, it is not possible to assess with certainty the effect of the parameters programmed at that time.
After 3–4 weeks, each electrode can be tested in monopolar configuration to map motor and visual stimulation-related adverse effects up to 3–4 V using pulse width of 60 μs and rate of 130 Hz. The main goal is to determine the thresholds for side effects (muscle pulling, involuntary movement, visual phosphenes, paresthesia, confusion, malaise, nausea, etc.) for each contact with stepwise increase of amplitude (0.5 V).
Regarding adverse effects resulting from the position of the DBS lead,
-
1.
if the DBS lead is too ventral, electrical current will spread to the internal capsule, causing tonic muscular contraction, and to the optic tract, causing phosphenes
-
2.
if the DBS lead is too posterior, electrical current will spread to the internal capsule, causing tonic muscle contraction
-
3.
when DBS leads are too anterior or too lateral, most often symptomatic benefits are lost and large volumes of stimulation may be required to extend the field posteriorly and medially to reach the appropriate targets.
If there are no adverse effects, the patient is followed every 2–4 weeks or until the best parameters are found. In general, it is advised to keep the medical treatment unchanged for 1–3 months postoperatively . If there is a clear general improvement, the same stimulation is maintained, and medications are carefully reduced. After the first programming, routine follow-up at 4–12 weeks and subsequently every 6 months are recommended. It seems reasonable to assess the benefit 6 months after surgery, with annual evaluations [68].
In case of adverse effects, the stimulation is moved one electrode dorsally or double monopolar stimulation is considered. If the results are still unsatisfactory, patients may be trialed with bipolar stimulation. The process may be repeated until the patient presents a considerable improvement of dystonia in absence of side effects. It is safer to give the opportunity to switch back to the previous setting in case of side effects or worsening of dystonia (setting one of the stimulation group with the previous stimulation parameters). It is important to emphasize that impedances should be checked in every visit.
12 Long-Term Management of DBS in Dystonia
Beneficial effects of Gpi DBS will be sustained up to 10 years after electrode implant in “primary dystonia”. In contrast, it may be difficult to predict the extent and duration of improvement for “secondary dystonia”.
Programming strategies for long-term management of DBS in dystonia are not uniform and are guided by the needs of individual patients. In the event of reoccurrence of dystonic symptoms in the long term, device-related complication and reprogramming should be considered.
Failures to stimulation , especially in patients with “primary dystonia ”, should not be consent without further evaluation of the individual case. Electrodes that are placed suboptimally should be revised. In some cases, with partial response, alternative targets for chronic stimulation might be considered.
Adverse events should be systematically recorded over the long-term follow-up. It is considered mandatory to monitor proper function of the neurostimulation device at each visit. The battery life of the stimulator must be taken into account to prevent sudden cessation of stimulation, particularly in severe segmental/axial or generalized dystonia with swallowing and respiratory symptoms related to dystonia [51].
13 Adverse Events
DBS is a safe technique considering that adverse events are infrequent and, allmost all of them, reversible [69]. Complications may arise in 14–50% of cases [29], as a result of adverse events derived from the stimulation system (“hardware-related”) or from the stimulation itself.
Adverse events arising from the stimulation system/prosthesis can be intraoperative (hemorrhage, electrode malposition) or postoperative (infections, skin erosions, system disconnections, electrode migration, cable fracture, and neurostimulator failure/deprogramming) [51, 70, 71]. A large number of these problems will require surgical intervention.
Table 41.5 summarizes the complications related to the prosthesis.
Concerning adverse events derived from stimulation, they may be due to inadequate programming or to the appearance of secondary effects (mainly capsular) when trying to achieve therapeutic stimulation intensities in improperly positioned electrodes It is necessary to highlight that the adverse effects derived from stimulation are always reversible . In this regard, speech abnormalities (dysarthria, dysphonia, and stuttering) and parkinsonian motor sign (gait abnormalities, hypokinesia and micrographia) are the most common stimulation-related adverse events resulting from current spreading to the internal capsule or stimulation of the ventral contacts in Gpi stimulation, respectively. In each instance, these adverse events can be significantly reduced by decreasing the intensity of stimulation or by switching to dorsal contacts [68].
14 Special Characteristics in Pediatric Patients
Children with dystonia have specific needs derived from their young age [59]. For this reason, it is particularly important to develop this program within a specifically pediatric multidisciplinary unit [1].
We perform direct targeting of the GPi on the preoperative MRI and we have realized that using this method the x coordinate is 2–4 mm more medial than in most published series [45, 57, 72].
Nutritional status should be examined to prevent skin ulceration and infection specially in younger patients. In fact, in younger children with a poor nutritional state who require DBS surgery due to the severity of the disease, subfascial placement of the neurostimulator should be considered [57].
Brain growth following electrode implantation may also result in relative retraction of contact positions compared to the original target position. Brain growth has been previously modeled suggesting a relative retraction of brain electrodes of between 5 and 10 mm between 4 and 18 years, mostly occurring before 5 years of age and to a lesser extent between 5 and 7 years [73].
The third point is the use of general anesthesia in pediatric patients. In adult patients, the surgery is usually performed with the patient awake, if the severity of the dystonia allows it. Although some authors also operate on pediatric patients while the patients are awake [59], we prefer to do it under general anesthesia. Intraoperative neurophysiological tests can be useful to determine the proximity of the electrode to the internal capsule and the secondary effect threshold [57]. Intraoperative imaging (MRI [64] or CT [74]) are highly recommendable in asleep DBS surgery.
Finally, the young age of most patients and the high voltage required for the treatment of dystonia, makes advisable the use of rechargeable neurostimulators in these patients [75] to prevent numerous replacements and its potential complications and financial cost along patient’s lifetime.
References
Candela S, Pérez B, Rumià J. Estimulación cerebral profunda como tratamiento de los trastornos del movimiento en la edad pediátrica. In: Orduna Martínez J, López Pisón J, editors. Neurocirugía Pediátrica. Fundamentos de patología neuroquirúrgica para pediatras. Madrid: Ergon; 2017. [Chapter in Spanish].
Benabid AL, Chabardes S, Torres S, Torres N, Piallat B, Krack P, et al. Functional neurosurgery for movement disorders: a historical perspective. Prog Brain Res. 2009;175:379–91. https://doi.org/10.1016/s0079-6123(09)17525-8.
Coubes P, Echenne B, Roubertie A, Vayssière N, Tuffery S, Humbertclaude V, et al. Treatment of early-onset generalized dystonia by chronic bilateral stimulation of the internal globus pallidus. Apropos of a case. Neurochirurgie. 1999;45(2):139–44. [Article in French]
Coubes P, Roubertie A, Vayssiere N, Hemm S, Echenne B. Treatment of DYT-1-generalised dystonia by stimulation of the internal globus pallidus. Lancet. 2000;355:2220–1. https://doi.org/10.1016/s0140-6736(00)02410-7.
Smith KM, Spindler MA. Uncommon applications of deep brain stimulation in hyperkinetic movement disorders. Tremor Other Hyperkinet Mov (NY). 2015;5:278. https://doi.org/10.7916/d84x56hp.
Albanese A, Bhatia K, Bressman SB, Delong MR, Fahn S, Fung VS, et al. Phenomenology and classification of dystonia: a consensus update. Mov Disord. 2013;28(7):863–73. https://doi.org/10.1002/mds.25475.
Guiot G, Brion S. Traitement des mouvements anormaux par la coagulation pallidale. Technique et résultats. Rev Neurol. 1953;89:578–80. [Article in French]
Cooper IS. Intracerebral injection of procaine into the globus pallidus in hyperkinetic disorders. Science. 1954;119:417–9. https://doi.org/10.1126/science.119.3091.417.
Laitinen LV, Bergenheim AT, Hariz MI. Leksell’s posteroventral pallidotomy in the treatment of Parkinson’s disease. J Neurosurg. 1992;76:53–61. https://doi.org/10.3171/jns.1992.76.1.0053.
Gros C, Frerebeau PH, Perez-Dominguez E, Bazin M, Privat JM. Long-term results of stereotaxic surgery for infantile dystonia and dyskinesia. Neurochirurgie. 1976;19:171–8. [Article in French]
Marras C, Zorzi G, Lenardi C, Rizzi M, Messina G, Alimehmeti R, et al. Deep brain stimulation electrode used for radiofrequency lesion of the globus pallidus internus in dystonia. Stereotact Funct Neurosurg. 2009;87(6):348–52. https://doi.org/10.1159/000236368.
Marras CE, Rizzi M, Cantonetti L, Rebessi E, De Benedictis A, Portaluri F, et al. Pallidotomy for medically refractory status dystonicus in childhood. Dev Med Child Neurol. 2014;56(7):649–56. https://doi.org/10.1111/dmcn.12420.
Lumsden DE, Kaminska M, Ashkan K, Selway R, Lin JP. Deep brain stimulation for childhood dystonia: is ‘where’ as important as in ‘whom’? Eur J Paediatr Neurol. 2017;21(1):176–84. https://doi.org/10.1016/j.ejpn.2016.10.002.
Fahn S, Eldridge R. Definition of dystonia and classification of the dystonic states. Adv Neurol. 1976;14:1–5.
Fahn S, Bressman SB, Marsden CD. Classification of dystonia. Adv Neurol. 1998;78:1–10.
Manji H, Howard RS, Miller DH, Hirsch NP, Carr L, Bhatia K, et al. Status dystonicus: the syndrome and its management. Brain. 1998;121(Pt2):243–52. https://doi.org/10.1093/brain/121.2.243.
Lumdsen DE, King MD, Allen NM. Status dystonicus in childhood. Curr Opin Pediatr. 2017;29(6):674–82. https://doi.org/10.1097/mop.0000000000000556.
Burke RE, Fahn S, Marsden CD, Bressman SB, Moskowitz C, Friedman J. Validity and reliability of a rating scale for the primary torsion dystonias. Neurology. 1985;35:73–7. https://doi.org/10.1212/wnl.35.1.73.
Thobois S, Taira T, Comella C, Moro E, Bressman S, Albanese A. Pre-operative evaluations for DBS in dystonia. Mov Disord. 2011;26(Suppl1):S17–22. https://doi.org/10.1002/mds.23481.
Hale AT, Monsour MA, Rolston JD, Naftel RP, Englot DJ. Deep brain stimulation in pediatric dystonia: a systematic review. Neurosurg Rev. 2018;43(3):873–80. https://doi.org/10.1007/s10143-018-1047-9.
Jankovic J. Medical therapy and botulinum toxic in dystonia. Adv Neurol. 1998;78:169–83.
Lake W, Shah H. Intrathecal baclofen infusion for the treatment of movement disorders. Neurosurg Clin N Am. 2019;30(2):203–9. https://doi.org/10.1016/j.nec.2018.12.002K.
Koy A, Hellmich M, Pauls KAM, Marks W, Lin JP, Fricke O, et al. Effects of deep brain stimulation in Dyskinetic cerebral palsy: a meta-analysis. Mov Disord. 2013;28(5):647–54. https://doi.org/10.1002/mds.25339.
Nerrant E, Gonzalez V, Milesi C, Vasques X, Ruge D, Rougeau T. Deep brain stimulation treated dystonia-trajectory via status dystonicus. Mov Disord. 2018;33(7):1168–73. https://doi.org/10.1002/mds.27357.
Ben-Haim S, Flatow V, Cheung T, Cho C, Tagliati M, Alterman RL. Deep brain stimulation for status dystonicus: a case series and review of the literature. Stereotact Funct Neurosurg. 2016;94(4):207–15. https://doi.org/10.1159/000446191.
Vidailhet M, Vercueil L, Houeto JL, Krystkowiak P, Benabid AL, Cornu P, et al. Bilateral deep-brain stimulation in primary generalized dystonia. N Engl J Med. 2005;352:459–67. https://doi.org/10.1056/nejmoa042187.
Kupsch A, Benecke R, Müller J, Trottenberg T, Schneider GH, Poewe W, et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med. 2006;355:1978–90. https://doi.org/10.1056/nejmoa063618.
Cif L, Vasques X, Gonzalez V, Ravel P, Biolsi B, Collod-Beroud G, et al. Long-term follow-up of DYT1 dystonia patients treated by deep brain stimulation: an open-label study. Mov Disord. 2010;25(3):289–99. https://doi.org/10.1002/mds.22802.
Valldeoriola F, Regidor I, Mínguez-Castellanos A, Lezcano E, García-Ruiz P, Rojo A, et al. Efficacy and safety of pallidal stimulation in primary dystonia: results of the Spanish multicentric study. J Neurosurg Pssychiatry. 2010;81:65–9. https://doi.org/10.1136/jnnp.2009.174342.
Borggraefe I, Mehrkens JH, Telegravciska M, Berweck S, Bötzel K, Heinen F. Bilateral pallidal stimulation in children and adolescents with primary generalized dystonia—report of six patients and literature-based analysis of predictive outcomes variables. Brain and Development. 2010;32:223–8. https://doi.org/10.1016/j.braindev.2009.03.010.
Brüggemann N, Kühn A, Schneider SA, Kamm C, Wolters A, Krause P, et al. Short- and long-term outcome of chronic pallidal neurostimulation in monogenic isolated dystonia. Neurology. 2015;84(9):895–903. https://doi.org/10.1212/wnl.0000000000001312.
Ramdhani RA, Frucht SJ, Behnegar A, Kopell B. Improvement of Isolated Myoclonus Phenotype in Myoclonus Dystonia after Pallidal Deep Brain Stimulation. Tremor Other Hyperkinet Mov (NY). 2016;6:369. https://doi.org/10.7916/d8f47p0c.
Owen T, Gimeno H, Selway R, Lin JP. Cognitive function in children with primary dystonia before and after deep brain stimulation. Eur J Paediatr Neurol. 2015;19(1):48–55. https://doi.org/10.1016/j.ejpn.2014.09.004.
Badhiwala JH, Karmur B, Elkim LM, Alotaibi NM, Morgan BR, Lipsman N, De Vloo P, Kalia SK, Lozano AM, Ibrahim GM. Clinical phenotypes associated with outcomes following deep brain stimulation for childhood dystonia. J Neurosurg Pediatr. 2019:1–9. https://doi.org/10.3171/2019.5.peds1973.
Katsakiori PF, Kefalopoulou Z, Markaki E, Paschali A, Ellul J, Kagadis GC, et al. Deep brain stimulation for secondary dystonia: results in 8 patients. Acta Neurochir. 2009;151:473–8. https://doi.org/10.1007/s00701-009-0281-x.
Fitgerald JJ, Rosendal F, de Pennington N, Joint C, Forrow B, Fletcher C, et al. Long-term outcome of deep brain stimulation in generalized dystonia: a series of 60 cases. J Neurol Neurosurg Psychiatry. 2014;85(12):1371–6. https://doi.org/10.1136/jnnp-2013-306833.
Olaya JE, Christian E, Ferman D, Luc Q, Krieger MD, Sanger TD, et al. Deep brain stimulation in children and young adults with secondary dystonia: the Children’s Hospital Los Angles experience. Neurosurg Focus. 2013;35(5):E7. https://doi.org/10.3171/2013.8.focus13300.
Eltahawy HA, Saint-Cyr J, Giladi N, Lang AE, Lozano AM. Primary dystonia is more responsive than secondary dystonia to pallidal interventions: outcome after pallidotomy or pallidal deep brain stimulation. Neurosurgery. 2004;54:613–9. https://doi.org/10.1227/01.neu.0000108643.94730.21.
Vidailhet M, Yelnik J, Lagrange C, Fraix V, Grabli D, Thobois S, et al. Bilateral pallidal deep brain stimulation for the treatment of patients with dystonia-choreoathetosis cerebral palsy: a prospective pilot study. Lancet Neurol. 2009;8:709–17. https://doi.org/10.1016/s1474-4422(09)70151-6.
Keen JR, Przekop A, Olaya JE, Zouros A, Hsu FPK. Deep brain stimulation for the treatment of childhood dystonic cerebral palsy. J Neurosurg Pediatr. 2014;14(6):585–93. https://doi.org/10.3171/2014.8.peds141.
Castelnau P, Cif L, Valente EM, Vayssiere N, Hemm S, Gannau A, et al. Pallidal stimulation improves panthotenate kinase-associated neurodegeneration. Ann Neurol. 2005;57:738–41. https://doi.org/10.1002/ana.20457.
Timmermann L, Pauls KA, Wieland K, Jech R, Kurlemann G, Sharma N, et al. Dystonia in neurodegeneration with brain iron accumulation: outcome of bilateral pallidal stimulation. Brain. 2010;133(Pt3):701–12. https://doi.org/10.1093/brain/awq022.
Liu Z, Liu Y, Wan X, Yang Y, Wang L, Dou W, et al. Pallidal deep brain stimulation in patients with chorea-acanthocytosis. Nuromodulation. 2018;21(8):741–7. https://doi.org/10.1111/ner.12763.
Koy A, Cirak S, Gonzalez V, Becker K, Roujeau T, Milesi C, et al. Deep brain stimulation is effective in pediatric patients with GNAO1 associated severe hyperkinesia. J Neurol Sci. 2018;391:31–9. https://doi.org/10.1016/j.jns.2018.05.018.
Isaias IU, Volkman J, Kupsch A, Burgunder JM, Ostrem JL, Alterman RL, et al. Factors predicting protracted improvement after pallidal DBS for primary dystonia: the role of age and disease duration. J Neurol. 2011;258:1469–76. https://doi.org/10.1007/s00415-011-5961-9.
Markun LC, Starr PA, Air EL, Marks WL, Volz MM, Ostrem JL. Shorter disease duration correlates with improved long-term deep brain stimulation outcomes in young-onset DYT1 dystonia. Neurosurgery. 2012;71(2):325–30. https://doi.org/10.1227/neu.0b013e318258e21b.
Lumsden DE, Kaminska M, Gimeno H, Tustin K, Baker L, Perides S, et al. Proportion of life lived with dystonia inversely correlates with response to pallidal deep brain stimulation in both primary and secondary childhood dystonia. Dev Med Child Neurol. 2013;55(6):567–74. https://doi.org/10.1111/dmcn.12117.
Diamond A, Jankovic J. The effect of deep brain stimulation on quality of life in movement disorders. J Neurol Neurosurg Psychiatry. 2005;76:1188–93. https://doi.org/10.1136/jnnp.2005.065334.
Valldeoriola F, Morsi O, Tolosa E, Rumià J, Martí MJ, Martínez-Martin P. Prospective comparative study on cost-effectiveness of subthalamic stimulation and best medical treatment in advanced Parkinson’s disease. Mov Disord. 2007;22(15):2183–91. https://doi.org/10.1002/mds.21652.
McClelland VM, Fialho D, Flexney-Briscoe D, Holder GE, Elze MC, Gimeno H, et al. Somatosensory evoked potentials and central motor conduction times in children with dystonia and their correlation with outcomes from Deep Brain Stimulation of the Globus pallidus internus. Clin Neurophysiol. 2018;129(2):473–86. https://doi.org/10.1016/j.clinph.2017.11.017.
Tagliati M, Krack P, Volkmann J, Aziz T, Krauss JK, Kupsch A, et al. Long-term management of DBS in dystonia: response to stimulation, adverse events, battery changes, and special considerations. Mov Disord. 2011;26(Suppl 1):S54–62. https://doi.org/10.1002/mds.23535.
Jahanshahi M, Czernecki V, Zurowski M. Neuropsychological, neuropsychiatric, and quality of life issues in DBS for dystonia. Mov Disord. 2011;26(Suppl 1):S63–78. https://doi.org/10.1002/mds.23511.
Coubes P, Vayssiere N, El Fertit H, Hemm S, Cif L, Kienlen J, et al. Deep brain stimulation for dystonia. Surgical technique. Stereot Funct Neurosurg. 2002;78:183–91. https://doi.org/10.1159/000068962n.
Lin S, Wu Y, Li H, Zhang Z, Wang T, Pan Y, He L, Shen R, Deng Z, Sun B, Ding J, Li D. Deep brain stimulation of the globus pallidus internus versus the subthalamic nucleus in isolated dystonia. J Neurosurg. 2019;8:1–12. https://doi.org/10.3171/2018.12.jns181927.
Wu YS, Ni LH, Fan RM, Yao MY. Meta-regression analysis of the long-term effects of pallidal and subthalamic deep brain stimulation for the treatment of isolated dystonia. World Neurosurg. 2019;129:e409–16. https://doi.org/10.1016/j.wneu.2019.05.165.
Schjerling L, Hjermind LE, Jespersen B, Madsen FF, Brennum J, Jensen SR, Løkkegaard A, Karlsborg M. A randomized double-blind crossover trial comparing subthalamic and pallidal deep brain stimulation for dystonia. J Neurosurg. 2013;119(6):1537–45. https://doi.org/10.3171/2013.8.jns13844.
Candela S, Vanegas MI, Darling A, Ortigoza-Escobar JD, Alamar M, Muchart J, et al. Frameless robot-assisted pallidal deep-brain stimulation surgery in pediatric patients with movement disorders. J Neurosurg Pediatr. 2018;22:416–25. https://doi.org/10.3171/2018.5.peds1814.
Pinsker MO, Volkman J, Falk D, Herzog J, Steigerwald F, Deuschl G, Mehdorn HM. Deep brain stimulation of the internal globus pallidus in dystonia: target localisation under general anaesthesia. Acta Neurochir. 2009;151(7):751–8. https://doi.org/10.1007/s00701-009-0375-5.
Marks WA, Honeycutt J, Acosta F, Reed M. Deep brain stimulation for pediatric movement disorders. Semin Pediatr Neurol. 2009;16(2):90–8. https://doi.org/10.1016/j.spen.2009.04.001.
Schaltenbrand G, Wahren W. Atlas for stereotaxy of the human brain. Stuttgart: Thieme; 1977.
Talairach J, Szikla G. Atlas of stereotactic concepts to the surgery of epilepsy. Paris: Masson; 1967.
De Benedictis A, Trezza A, Carai A, Genovese E, Procaccini E, Messina R, et al. Robot-assisted procedures in pediatric neurosurgery. Neurosurg Focus. 2017;42(5):E7. https://doi.org/10.3171/2017.2.focus16579.
Konrad PE, Neimat JS, Yu H, Kao CC, Remple MS, D’Haese PF, Dawant BM. Customized, miniature rapid-prototype stereotactic frames for use in deep brain stimulator surgery: initial clinical methodology and experience from 263 patients from 2002 to 2008. Stereotact Funct Neurosurg. 2011;89(1):34–41. https://doi.org/10.1159/000322276.
Starr PA, Markun LC, Larson PS, Volz MM, Martin AJ, Ostrem JL. Interventional MRI-guided deep brain stimulation in pediatric dystonia: first experience with the Clearpoint system. J Neurosurg Pediatr. 2014;14:400–8. https://doi.org/10.3171/2014.6.peds13605.
Benabid AL, Benazzous A, Pollak P. Mechanisms of deep brain stimulation. Mov Disord. 2002;17(Suppl 3):s73–4. https://doi.org/10.1002/mds.10145.
Schüpbach WMM, Chabardes S, Matthies C, Pollo C, Steigerwald F, Timmermann L, et al. Directional leads for deep brain stimulation: opportunities and challenges. Mov Disord. 2017;32(10):1371–5. https://doi.org/10.1002/mds.27096.
Kupsch A, Tagliati M, Vidailhet M, Aziz T, Krack P, Moro E, et al. Early postoperative management of DBS in dystonia: programming, response to stimulation, adverse events, medication changes, evaluations, and troubleshooting. Mov Disord. 2011;26(Suppl 1):S37–53. https://doi.org/10.1002/mds.23624.
Picillo M, Lozano AM, Kou N, Munhoz RP, Fasano F. Programming deep brain stimulation for tremor and dystonia: the Toronto Western hospital algorithms. Brain Stimul. 2016;9(3):438–52. https://doi.org/10.1016/j.brs.2016.02.003.
Fenoy AJ, Simpson RK Jr. Risks of common complications in deep brain stimulation surgery: management and avoidance. J Neurosurg. 2014;120(1):132–9. https://doi.org/10.3171/2012.1.jns111798.
Kaminska M, Perides S, Lumsden DE, Nakou V, Selway R, Ashkan K, et al. Complications of deep brain stimulation (DBS) for dystonia in children – The challenges and 10 year experience in a large paediatric cohort. Eur J Paediatr Neurol. 2017;21(1):168–75. https://doi.org/10.1016/j.ejpn.2016.07.024.
Koy A, Weinsheimer M, Pauls KAM, Kühn AA, Krause P, Huebl J, et al. German registry of paediatric deep brain stimulation in patients with childhood-onset dystonia (GEPESTIM). Eur J Paediatr Neurol. 2017;21(1):136–46. https://doi.org/10.1016/j.ejpn.2016.05.023.
Haridas A, Tagliati M, Osborn I, Isaias I, Gologorsky M, Bressman SB, et al. Pallidal deep brain stimulation for primary dystonia in children. Neurosurgery. 2011;68:738–43. https://doi.org/10.1227/neu.0b013e3182077396.
Lumsden DE, Ashmore J, Charles-Edwards G, Selway R, Lin JP, Ashkan K. Observation and modelling of deep brain stimulation electrode depth in the pallidal target of the developing brain. World Neurosurg. 2015;83:438–46. https://doi.org/10.1016/j.wneu.2015.01.012.
Cardinale F, Rizzi O, d’Orio P, Casaceli G, Arnulfo G, Narizzano M, et al. A new tool for touch-free patient registration for robot-assisted intracranial surgery: application accuracy from a phantom study and a retrospective surgical series. Neurosurg Focus. 2017;42:E8. https://doi.org/10.3171/2017.2.focus16539.
Lumsden DE, Kaminska M, Tustin K, Gimeno H, Baker L, Ashkan K, et al. Battery life following deep brain stimulation (DBS) in children and young people with severe primary and secondary dystonia. Childs Nerv Syst. 2012;28:1091–7. https://doi.org/10.1007/s00381-012-1728-6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Candela-Cantó, S., Ortigoza-Escobar, J.D., Darling, A., Rumià, J. (2022). Deep Brain Stimulation for Pediatric Movement Disorders. In: Alexiou, G., Prodromou, N. (eds) Pediatric Neurosurgery for Clinicians. Springer, Cham. https://doi.org/10.1007/978-3-030-80522-7_41
Download citation
DOI: https://doi.org/10.1007/978-3-030-80522-7_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-80521-0
Online ISBN: 978-3-030-80522-7
eBook Packages: MedicineMedicine (R0)