Abstract
Due to the close proximity of cavernous sinus meningiomas (CSMNs) to vital intracranial neurovascular structures, complete surgical resection may not always be possible. Hence, stereotactic radiosurgery (SRS) has been proposed as a primary, adjuvant and/or salvage treatment option for the management of such cases. The aims of this study were to assess the long-term outcomes of SRS on a large patient series and to identify any prognosticators significantly influencing local tumour control (LTC).
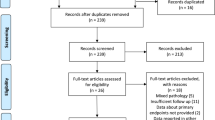
Materials and Methods: From February 1993 to December 2007, 200 patients with CSMN underwent Leksell Gamma Knife Radiosurgery (LGKRS) at our department. All selected patients (51 males and 149 females, mean age 53.7 years, age range 25–83) were followed up for at least 10 years. CSMNs were classified as limited to cavernous sinus (CS) or involving the nearby skull base. LGKRS was delivered as either primary therapy (for unresectable tumours) in 91/200 (45.5%) patients, adjuvant therapy (for residual tumour after subtotal resection) in 77/200 (38.5%) or salvage therapy (for observed progression in residual disease) in 32/200 (16.0%). Stereo-CT scan was used in 69 patients and MRI stereotactic localization in 131 CSMNs. Mean LGKRS dose planning parameters were as follows: gross target volume (GTV) 9.88 cc, range 1.4–42.6; prescription dose (PD) 14.2 Gy, range 10–22.5; prescription isodose (PI) 48.3%, range 30–60; maximum dose (MD) 29.8 Gy, range 16.9–66.7; integral dose (ID)169.7 mJ, range 26–713; and number of shots 13.8, range 3–35. Uni- and multivariate logistic regression analysis was performed to evaluate which of the independent variables (age, sex, GTV, PD, stereo-CT scan vs. stereo-MRI, CS only vs. nearby spread, primary vs. adjuvant/salvage radiosurgery and WHO classification Grade I vs. II/III) could potentially influence the LTC (end point).
Results: The median survival was 165.9 months (137.0–256.0). LTC was achieved in 171/200 patients (85.5%) with actuarial LTC rates of 91% and 89% at 10 years and 15 years, respectively. Neurological status was stable (52/200) or improved (121/200) in 173 patients (86.5%), irrespective of tumour shrinkage. Among the 27/200 patients with neurological deterioration, 22 worsened due to tumour progression. Slight LGKRS-associated permanent fifth and/or sixth cranial nerve deficit was observed in five cases (2.5%). Upon statistical analysis, the only independent variables which significantly influenced LTC were primary vs. adjuvant/salvage SRS (p = 0.037) and histology (p = 0.019).
Conclusions: LGKRS is an effective and safe treatment for CSMN with excellent long-term LTC. Primary vs. adjuvant/salvage treatment and WHO grade affect LGKRS outcome in such patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
7.1 Introduction
Cavernous sinus meningiomas (CSMNs) occur in 0.5/100,000 people in the general population, and account for more than 90% of cavernous sinus tumours [1, 2]. From an epidemiological perspective, CSMNs are more common in females and in middle to advanced age [2]. In most cases, CSMNs are histologically Grade I on the WHO classification or show imaging features compatible with benign forms [1, 3].
Surgical treatment is the primary therapeutic choice for intracranial meningiomas. However, CSMNs constitute a great surgical challenge due to their close anatomical relationships with particularly delicate and vital vascular, endocrine and nerve structures (cavernous segment of the inner carotid artery, upper and lower petrous sinuses, basilar plexus, cavernous sinus, anterior visual pathways, pituitary stalk, ocular nerves, first and second branches of the trigeminal nerve and brainstem) [4]. As a result, and despite considerable advances in neurosurgical technology and intraoperative neurophysiological monitoring methods, the surgical approach is burdened by a high risk of serious and long-lasting side effects, especially in attempts at radical resection. In fact, the literature reports high rates of permanent neurological complications (17.9–74.0%) and a post-operative mortality rate of up to 9.5% associated with such interventions [5,6,7].
Stereotactic radiosurgery (SRS), on the other hand, is minimally invasive and associated with excellent efficacy (high local tumour control, LTC) and safety, a very low risk of permanent neurological side effects and no secondary mortality. These features have facilitated the rapid diffusion of this therapeutic approach in selected cases of CSMNs (maximum diameter of less than 3 cm or volume less than 15–20 cm3 and which do not significantly compromise the anterior visual pathways) around the world, both as an alternative to surgery (primary treatment, especially when the morphological and volumetric features of a meningioma preclude the surgical approach) and as part of a combined surgical treatment (adjuvant removal of residual tumour following resection, or as a salvage treatment for progressing or recurring tumours) [8, 9].
Worldwide, over 10,000 CSMNs have thus far been treated via SRS and reported in the literature—a total of about 150 published articles. Reported outcomes are excellent, with regard to both LTC (85–100% at 5 years and 75–98% at 10 years) and risk of permanent side effects (an incidence of between 0% and 19%); radiosurgical treatment is associated with a 0.0% mortality rate (Table 7.1). That being said, few studies have evaluated the effectiveness and safety of SRS for CSMNs in the long term, i.e. after an observation period of longer than 10 years. Hence, in this chapter, we present the results of our retrospective study on 200 CSMN patients treated via Leksell Gamma Knife radiosurgery (LGKRS) and subjected to neuroradiological and clinical follow-up for at least 10 years. In addition, we share data from our uni- and multivariate statistical analysis, performed to assess the prognostic role of several independent variables, namely age, sex, gross tumour volume (GTV), prescription dose (PD), stereo-CT vs. stereo-MRI, location limited to the cavernous sinus vs. local spread, primary vs. adjuvant/salvage LGKRS and WHO Grade I vs. II classification, in the post-SRS LTC (end point). Finally, we compare our data with those collected from a wide range of literature reports on the subject.
7.2 Materials and Methods
Between February 1993 and December 2007, 200 CSMN patients underwent SRS with Leksell Gamma Knife (LGKRS) at our department. All selected patients were followed up for at least 10 years. At the time of admission, signed consent was obtained from all patients included in the study, as the general policy at our LGKRS centre (Verona University Hospital) is to acquire consent from all patients before their medical records and radiological images are used for research purposes. The sample comprised 51 males and 149 females, of average age 53.7 years (range 25–83 years). CSMNs were classified by site as either limited to the cavernous sinus (limited) or spread to nearby structures of the cranial base (spread). There were 97/200 WHO Grade I CSMNs, 91/200 with neuroradiological characteristics compatible with a benign form and 12/200 Grade II CSMNs. LGKRS was used as a primary treatment in 91/200 patients (45.5%), as an adjuvant in 77/200 cases (38.5%) and as salvage therapy in 32/200 patients (16.0%).
On the day of radiosurgical treatment, the MRI-compatible Leksell model G stereotactic frame (Elekta Instruments) was positioned to the patient’s head. Then, stereo-CT was performed in 69 patients and stereo-MRI in 131. Currently, our stereo-MRI protocol for CSMNs includes the following algorithms and specific sequences, all with contrast: T1 sequences for saturated fats, constructive interference in steady-state (CISS) sequences and 1 mm isovoxel Q1 volumetric sequences. SRS procedures were carried out using an LGK C 201 unit with Co60 source until June 2008, and LGK Perfexion (both from Elekta Instruments) thereafter. Three-dimensional treatment planning was developed using commercially available programmes, namely Kula (Elekta Instruments) from February 1993 to February 1998 and Leksell Gamma Plan (versions 4.12, 5.34 and 8.3, Elekta Instruments) after February 1998. The neurosurgeon, radio-oncologist and medical physicist jointly created an extremely conformational treatment plan using multiple collimators, selecting the dose most appropriate for the individual case. The treatment plan was carried out with the aim of achieving full and highly conformational coverage of the tumour, sparing and preserving the surrounding healthy structures (cranial nerves, pituitary stalk, etc.). The average parameters and their treatment plan ranges were as follows: GTV 9.88 cc (1.4–42.6), PD 14.2 Gy (10–22.5), PI 48.3% (48.3% 30–60), MD 29.8 Gy (16.9–66.7), ID 169.7 mJ (26–713) and number of shots 13.8 (3–35). The DP and MD of the SRS treatment were selected and administered in accordance with the known radio-tolerance levels for the optic nerve, optic chiasm and pituitary stalk.
The first scheduled follow-up was at 6 months after SRS, then annually for 2 years and then every 2–3 years. Patient status was monitored at these time points using MRI, field-of-vision analysis, Hess–Lancaster screen and full pituitary hormone profiling.
Actuarial LTC rate curves were plotted using the Kaplan–Meier method [10], and log-rank univariate analysis was used to assess factors potentially related to LTC. Statistical significance was calculated using Fisher’s exact test. Next, to assess statistical significance more accurately, regression analyses were performed using a logistic model. Uni- and multivariate statistical analyses were performed to assess which of the following independent variables could potentially affect the LTC (end point): age, gender, GTV, PD, stereo-CT vs. stereo-MRI, limited vs. spread site, primary vs. adjuvant/salvage LGKRS and WHO Grade I vs. II. Based on the internationally accepted criteria, p values ≤0.05 were considered statistically significant. Statistical analysis was performed using Stata software, version 13.1 (Stata Corp.). Since this is a retrospective, single-centre study, the possibility of bias in patient selection cannot be ruled out.
7.3 Results
The median observation period was 165.9 months (137.0–256.0). Clinical neurological outcome was classified as stable (52/200) or improved (121/200) in 173 patients (86.5%), regardless of the extent of tumour reduction. The median clinical performance index, based on Karnofsky classification, rose from 80.5% in the period prior to LGKRS to 85.7% at the last clinical-neurological check-up after radiosurgical treatment (p = 0.041). Among the 27/200 patients with neurological deterioration, 22 had worsened due to tumour progression. In five cases (2.5%) there was a slight permanent fifth and/or sixth cranial nerve deficit secondary to the LGKRS treatment. During the observation period, there were ten deaths, one being a patient with pre-LGKRS WHO Grade II MN which exhibited dramatic late progression leading to death; a further two patients diagnosed with WHO Grade I MN had uncontrollable local progression after LGKRS leading to their deaths; and in the remaining seven cases, the cause of death was not related to meningioma. None of the cases in our clinical series resulted in radiosurgery-related mortality, and in the 10 years after SRS, there were no cases of radiation-induced cancer or proven malignant transformation. Overall, 171/200 patients (85.5%) had actuarial LTC rates of 94%, 91% and 89% at 5, 10 and 15 years, respectively (Fig. 7.1 and Table 7.1). A comparison between Grade I CSMNs (97/200), or those with neuroradiological characteristics compatible with benign meningioma (91/200), and WHO Grade II (12/200) revealed actuarial LTCs of 94.9%, 94.9% and 89.3% at 10, 15 and 20 years, respectively, for Grade I CSMNs, and 76.2%, 76.2% and 0.0% at the corresponding time points for Grade II CSMNs (Fig. 7.2 and Table 7.2). Among the 27/200 CSMNs that displayed progression after LGKRS, 11/97 (11%) had originally been diagnosed as WHO Grade I, 9/91 (10%) had CSMNs with neuroradiological characteristics compatible with benign forms and 7/12 (58%) were originally WHO Grade II. According to uni- and multivariate statistical analyses, the only independent variables that significantly influenced the LTC were primary vs. adjuvant/salvage treatment (p = 0.037) and histology (WHO Grade I vs. Grade II) (p = 0.019). In other words, our results indicate that patients treated with LGKRS without having previously undergone neurosurgical intervention and those suffering from a CSMN of WHO Grade I or with neuroradiological characteristics compatible with benign forms have a more favourable prognosis for survival without local progression.
7.4 Discussion
7.4.1 Epidemiology, Anatomy and Clinical Data
As mentioned in Sect. 7.1, CSMNs occur in 0.5/100,000 people in the general population, and account for more than 90% of tumours of the cavernous sinus [1, 2]. They are more common in the middle decades of life, but also occur frequently in old age. The ratio of female to male patients is 2:1 [2]. CSMNs have distinctive features related to their location, owing to their close anatomical relationships with particularly delicate but vital vascular, endocrine and nerve structures, including the cavernous segment of the inner carotid artery, upper and lower petrous sinuses, basilar plexus, cavernous sinus, anterior visual pathways, pituitary stalk, ocular nerves, first and second branches of the trigeminal nerve and brainstem [4]. Indeed, they tend to cause clinical symptoms secondary to compression or invasion of neighbouring neurovascular structures, often diplopia, ophthalmoplegia and/or eyelid ptosis. Compression of the anterior visual pathways or infiltration of the optic tract can cause visual impairment, resulting in complete loss of visual acuity, as well as a complete or partial trigeminal syndrome secondary to the compression of the fifth cranial nerve. More rarely, hormonal deficits due to impaired pituitary function are also seen. Patients with CSMNs involving the sphenoid wing and infiltrating the cavernous sinus may suffer seizures or corticospinal motor deficits. Finally, CSMNs are frequently associated with headache [2].
7.4.2 Imaging
The neuroradiological characteristics compatible with meningioma are extra-axial localization, homogeneous intake of contrast medium, base in the dura mater, clear demarcation from the normal surrounding brain tissue, slow and gradual tumour growth at repeat neuroradiological exams, exclusion of systemic metastasis and, in some cases, tumour calcification [3, 9]. These morphological features lend themselves to accurate localization using stereo-MRI. In addition, with their generally homogeneous capture of the contrast medium, clear and well-defined margins and excellent delimitation of the dural tail of the lesion, meningiomas—in particular CSMNs—are ideal targets for treatment via SRS. MRI sequences employed to obtain accurate CSMN localization for the purposes of SRS, all using contrast medium, generally include T1 sequences for saturated fats (to provide clear demarcation of the volume, morphology and boundaries of the MN); CISS sequences (for clear definition of the cranial nerves and other critical brain structures to be preserved during SRS); and axial T1 sequences; these imaging protocols provide excellent definition of the tumour margins within the cavernous sinus and orbit.
7.4.3 Surgical Treatment
Surgery is usually the primary treatment option proposed for intracranial meningioma. However, although technically possible in the case of CSMNs, surgical resection may involve a very laborious and complex operating procedure. In addition, due to above reasons it is also associated with a very high risk of permanent neurological side effects, and a non-negligible probability of post- and perioperative mortality, without ensuring the possibility of complete tumour removal. In fact, several literature reports, even those on recent and numerous CSMN case series, cite rates of permanent neurological damage ranging from 17.9% to 74.0%, and a post-operative mortality rate of between 0.0% and 9.5% [5, 7]. Moreover, the probability of recurrence after partial or subtotal surgical resection of CSMN remains significant (13% at 3 years and 38% at 5 years) [2].
7.4.4 SRS and Its Advantages
SRS, on the other hand, has numerous advantages over surgical treatment for CSMN. First and foremost, it is associated with excellent outcomes in terms of efficacy and safety. Actuarial survival rates with 5-year LTC are reported as being between 85.7% and 100%, associated with stable or improved neurological conditions in the vast majority of cases; SRS limits the progression of the disease in most patients, with very low risks of retreatment. In addition, SRS has very low morbidity and secondary mortality, with severe neurological deterioration being extremely rare. Indeed, via SRS it is possible to obtain extremely accurate tumour localization using stereo-MRI images, since CSMNs usually display homogeneous capture of the contrast medium, clear and well-defined margins and excellent delimitation of their dural tail. Additional advantageous features of the radiosurgical procedure include simple, easy and rapidly implemented treatment plan, modelled with multiple isocentres, and a non-invasive intervention that requires, in most cases, only a few hours of hospitalization.
Hence, hospitalization costs are also low as compared to surgery. According to the UK National Health Service (NHS) clinical commissioning policy for stereotactic radiosurgery/radiotherapy for meningioma (D05/P/e) published by the NHS England SRS reference group in September 2013 [11], there is evidence—from a comparative study of the costs of microsurgery vs. SRS—that the total expenditure on microsurgery is more than double that of SRS. Indeed, SRS requires significantly shorter hospitalization than microsurgery, and has a less harmful impact on the quality of life. Furthermore, secondary mortality is avoided, and there is a lower incidence of treatment-related complications, making the savings for the NHS in England considerable. In fact, SRS is usually carried out in day surgery under local anaesthesia, whereas microsurgical resection necessarily requires general anaesthesia, and usually entails operating from 2 to 10 h or more, depending on the complexity and volume of the meningioma to be removed. In addition, patients undergoing microsurgery require a minimum stay of 12–24 h in an intensive care environment. Hospital stays are usually between 4 and 10 days, but can extend to several weeks or months if post-operative complications occur (such as cerebrospinal fluid leak, severe motor deficits), which could put a strain on neurological rehabilitation resources. In conclusion, compared to microsurgery SRS offers shorter hospitalization, less harmful impact on quality of life, no post-operative mortality, lower incidence of treatment-related complications and much lower costs.
7.4.5 Comparison of Different Cases
Thus far, there have been reports on several thousand patients treated via SRS for CSMNs published in the literature (Tables 7.3 and 7.4). These clinical series, with an average or median observation period of less than or equal to 62 months, indicate that the actuarial LTC rates range between 85.7% and 100% at 5 years and between 75.8% and 98% at 10 years (Table 7.3). Moreover, a clear relationship between the volume of the CSMNs treated and the post-SRS prognosis emerges. Specifically, when the average or median treatment volume remains below 10 mL, the LTC at 5 and 10 years generally remains above 90%. From a clinical perspective, the possibility of neurological improvement, especially at the expense of cranial nerve deficits, in patients already symptomatic before SRS treatment is very significant. In fact, the improvement frequency reported in the literature varies between 20% and 69.3% (Table 7.3). Conversely, the risk of permanent side effects secondary to SRS treatment is always very low (0.0–19.2%). Once again, a relationship seems to exist, this time directly proportional, between the treated tumour volume and the onset of complications. In fact, iatrogenic worsening due to radiation is usually reported as being less than 10% in clinical series with average or median treated volumes of less than 10 mL.
Patient series with a medium-term observation period of 62 months have also led to the identification of several prognostic factors related to LTC and neurological improvement (Table 7.3). In particular, the increased extent and volume of CSMNs, suboptimal coverage of tumour volume by the treatment dose and more aggressive histological grade (WHO Grade II/III) all appear to correlate with a lower probability of LTC. On the other hand, SRS treatments on CSMNs that have never previously been operated on (primary treatments) and the number and entity of modest cranial nerve deficits appear to be associated with a greater likelihood of neurological improvement after SRS (Table 7.3).
However, since CSMNs are usually benign and therefore affect patients with a prolonged life expectancy, it is fair to ask whether the effects of SRS, in terms of efficacy and safety, on this type of cranial base tumour are maintained in the long term. In order to clarify this issue, the outcomes in selected larger case series (exceeding 30 patients) and an average or median observation period of more than 62 months (Table 7.4) were compared. These studies also confirm the stability of the effects of radiosurgery for CSMN over time, with 15-year LTC rates ranging from 75% to 94.9%. In particular, in our study on 200 CSMNs treated via LGK and with a median observation period of 165.9 months, the LTC at 20 years in the 188 CSMNs with baseline WHO Grade I or neuroradiological features compatible with a benign form was extremely high (89.3%). From a clinical perspective, these patient series with long-term follow-up also demonstrate that SRS is associated with an improvement in the neurological status, especially with regard to cranial nerve deficit (from 21% to 60.5%) (Table 7.4). Similarly, the risk of permanent neurological complications secondary to SRS—especially those involving the cranial nerves—remains particularly low, with sequelae occurring in between 0.0% and 12.5% of cases.
Finally, studies with long observation periods and numerous cases (at least 100 patients) have also identified some prognostic factors related to LTC and neurological status. Specifically, SRS is associated with a greater success rate when applied as a primary treatment for WHO Grade I sporadic (i.e. single) meningiomas, particularly in females. Furthermore, success rates are higher when the treatment plan involves full tumour coverage and a radiant dose to the surface of ≥13 Gy. In contrast, adjuvant or salvage SRS for MN volumes >10 mL seems to be a factor associated with the onset of new cranial nerve deficits and worse neurological prognosis for CSMN patients (Table 7.4).
7.4.6 Long-Term Complications
7.4.6.1 Stroke Risk
Another pertinent topic is the long-term risk of stroke after radiosurgical treatment of CSMNs. While the risk of stroke after proton or photon RT for partially resected MN has been examined over long-term observation periods, the frequency of stroke after single-session SRS had never been previously studied in patients with MN. However, a recent randomized study by Massachusetts General Hospital on 44 patients with relapsed or progressed WHO Grade I MN who had previously undergone incomplete surgical resection and were subsequently treated using fractional proton-photon therapy at a minimum total dose of 55.8 Gy revealed that, at a median follow-up of 17.1 years, the risk of stroke onset was 20.5%, with an average interval between RT term and stroke diagnosis of 5.6 years [41]. This stroke risk is up to ten times higher than the 2–6% calculated and expected for the general population aged 40–79 years, according to recent statistics published by the American Heart Association [42]. However, more recently, prompted by this data, McClelland et al. [43] carried out a detailed study of PubMed looking for articles related to the treatment of SRS on MNs. On the basis of precise inclusion criteria—(a) median/average clinical follow-up of at least 6 years (interval chosen to ensure that these studies had exceeded the 5–6-year period between RT and stroke onset established by the Sanford et al. study); (b) minimum 30 patients; (c) written in English; (d) single-session SRS exclusively for meningioma; (e) inclusion of post-SRS morbidity analysis; and (f) patient pool not reported in multiple published studies—they selected 14 studies with long-term follow-up, comprising a total of 1431 patients followed up for a median/average interval of 75–144 months. Overall, stroke following SRS treatment was reported in 24 patients, i.e. 1.7%. This long-term stroke rate after single-session photon SRS for benign MN is more than 12 times lower than that reported in the above fractional proton-photon therapy clinical series, and was comparable to that expected for the general population. Most of these patients underwent surgical resection prior to SRS, and the authors concluded that to avoid the high risk of stroke associated with fractional proton-photon therapy, patients with benign MN should instead undergo SRS, which seems not to raise the stroke risk as compared to the general population.
7.4.6.2 Tumorigenesis and Malignant Transformation
There are two possible carcinogenic effects associated with SRS treatments: radiation-induced tumorigenesis (RIT) and malignant transformation (MT). Nonetheless, the real risk of RIT or MT after single-session SRS to intracranial targets remains undefined, despite more than 1,000,000 patients having already undergone this type of treatment to date. That being said, it does appear to be particularly low and is certainly significantly lower than that associated with fractional RT. The term “radiation-induced tumorigenesis”, however, seems inappropriate because it implies that there is definitive molecular evidence that radiation is the causal factor. This information has never been reported, and the term “radiation-associated” may therefore be a more appropriate definition [44, 45]. At present, however, the definition of SRS-associated tumorigenesis is still based on the indirect criteria developed by Cahan et al. [46] in 1948; specifically, secondary cancer must develop within the field of previous irradiation; it should not be present before RT; there must be some period of latency between the treatment and tumour onset (usually 5 years); the secondary cancer must be histologically distinct from the original pathology; and there must be no genetic predisposition for the onset of a secondary tumour or cancer progression.
With regard to the risk of SRS-associated tumorigenesis, according to the literature data the incidence of SRS-associated cancers is between 0.0 and 3.0 per 200,000 patients per year [47], or, to cite a more recent estimate, between 0.04% and 2.6% at 15 years [48, 49]. In this regard, Rowe et al. [50] conducted a retrospective cohort study comparing the incidence of new central nervous system malignancies in their SRS-treated patients with the UK national incidence. Based on 4877 patients treated via SRS and more than 30,000 patients followed up for a median 5.2 years, the authors reported one new astrocytoma in the SRS group in the entire follow-up period, as compared to an expected incidence of 2.5 cases. In 2014, Patel and Chiang, on the other hand, reviewed the published literature on this topic and identified 19 cases of RIT and 17 cases of MT following SRS out of approximately 80,000 selected patients [48]. Based on this estimate of 80,000 patients treated via SRS for benign brain pathology with an observation period of at least 15 years, it was estimated that the combined risk of SRS-associated tumorigenesis and MT onset was 0.04% at 15 years.
Similarly, Rahman et al. compared the number of cancer cases observed in a group of patients after linac SRS with the number of cancer cases one would expect in a group of age- and sex-matched patients, as extracted from the Surveillance, Epidemiology and End Results (SEER) database [51]. Out of a total of 627 patients with more than 5 years of follow-up—comprising 202 MNs, 223 intracranial schwannomas, 165 arteriovenous malformations (AVM) and 37 other cancers—the cancer rate observed in patients with MN was 3.96%, as compared to the expected rate of 10% (binomial confidence interval of 95%, CI = 1.85–7.94). The authors concluded that after long periods of observation of a large population of patients treated for intracranial MN, there was no increased risk of cancer associated with linac SRS with respect to the general population. More recently, Kondziolka and Lunsford observed no cases of SRS-associated tumorigenesis in more than 13,000 SRS patients treated at the University of Pittsburgh between 1987 and 2013 [52]. Finally, Pollock et al. [53] carried out a retrospective review of 1142 patients treated via single-fraction intracranial radiosurgery at the Mayo Clinic College of Medicine between 1990 and 2009. Their sample comprised 233 AVM, 316 MN, 358 vestibular schwannomas, 188 pituitary adenomas and 47 jugular glomus tumours, divided into two patient populations, similar in gender, age, number of previous surgical resections, prescribed ID and number of doses, on the basis of whether they were excluded or included in the study. Specifically, patients were excluded if they refused permission for research, had a genetic predisposition for cancer or had been subjected to RT either previously or concurrently with the intracranial radiosurgery. Any case of RIT or MT was recorded, irrespective of the duration of the observation period, although the median neuroradiological follow-up of the 1142 patients was 9.0 years (range 5–24.9). The authors identified no cases of RIT in the 11,264 patients throughout the observation period. Therefore, according to the authors’ conclusions, the risk of developing a RIT after SRS remained 0.0% at 5, 10 and 15 years.
In summary, the lessons learned so far on the risk of SRS-associated RIT lead to the following final considerations and recommendations: (1) RIT can occur both within the full-dose region and in peripheral regions exposed to very low doses; (2) the risk of RIT is substantially lower with SRS than in patients treated with radiation to larger volumes and/or with fractionated treatment regimes; (3) the latency period after SRS is similar to that observed with fractionated RT, with a range of 6–20 years, and malignant tumours have a shorter latency period than benign radiation-induced forms; (4) a long-term observation period should be mandatory for all SRS patients to detect benign brain injuries; and (5) current standard guidance regarding SRS should not be changed, due to the extremely low risk of associated RIT.
As regards MT, this is defined as occurring when a purported or histologically proven benign tumour shows progression after SRS, and histopathological examination at surgery or re-intervention reveals a higher tumour grade or a real malignant cancer [53]. It is particularly unfeasible to assess the relative risk of MT in SRS for intracranial MNs without a non-irradiated control group of patients, since MN MT has also been observed in patients who have never been previously given RT [54, 55]. Nonetheless, Patel and Chiang [48] reported that the risk of MT following SRS was 0.04% at 15 years in a series of 80,000 patients treated for benign intracranial MN. Kondziolka et al. [56], on the other hand, published a retrospective study of 290 patients consecutively treated via LGKRS for intracranial MN (97% Grade I WHO or with imaging characteristics typical of benign MN) between 1987 and 1997, and with a median clinical observation period of 56 months after SRS. In the 6 patients who underwent surgical resection after MN progression following SRS, documented by imaging, no MT was identified. The same team [9] reported on 200 patients with WHO Grade I CSMNs consecutively treated via LGKRS and with an average neuroradiological follow-up time of 101 months. In this long-term observational study, no patient developed radiation-related secondary cancers. Finally, Pollock et al. [53] evaluated MT in a sample of 1142 patients who underwent single-session SRS and had a neuroradiological follow-up of at least 5 years. Of the 316 patients with MN, they observed MT in 7 (2.2%) over a median observation period of 4.9 years (range 2.8–13.8). They reported 5-, 10- and 15-year actuarial risks of MT of 0.5%, 0.8% and 2.4%, respectively. All seven affected patients had previously undergone surgical resection of the MN prior to SRS, and WHO Grade I was confirmed histologically in all cases. After re-intervention, however, MNs were found to be WHO Grade II in four cases and Grade III in three. Statistical analysis led the authors to conclude that patients with intracranial MN and previous surgical resection were at increased risk of MT. Nevertheless, a 2.2% rate of MT is extremely low as, if we consider the histopathological classification criteria and patterns reported for 2000, 2007 and 2016, the incidence of Grade II tumours has drastically increased in frequency from 3–4% to 20–35% in MNs recently subjected to primary resection and diagnosis [57,58,59]. In addition, several clinical series have shown that up to 2% of all benign MNs spontaneously turn into higher grade histological forms (II or III), while up to 28.5% of all previously irradiated surgical recurrences of benign MN turn out to be atypical or anaplastic at histological examination [60].
Overall, these studies show that the incidence of SRS-associated tumorigenesis is certainly extremely low, and that the potential risk of secondary cancer associated with SRS should be weighed against the potential benefits of the procedure. In particular, the oncogenic risk linked to SRS is generally considered to be significantly lower than that observed after fractional RT, due to the steeper dose gradients, minimal irradiated volumes of healthy cerebral parenchyma and significantly lower total doses overall associated with the former [61, 62]. In addition, there is growing evidence that the genesis of new cancers is more likely after combined treatment methods (radiotherapy and chemotherapy)—now an increasingly common therapeutic approach in clinical practice [44, 45]. Finally, it should always be borne in mind that alternative treatments, if available, are also not devoid of risk, and sometimes there are no other therapeutic options available in place of SRS. In summary, it is possible to conclude that the risk of RIT or MT after SRS is very low, and should not therefore be used as a justification for choosing alternative therapeutic approaches (surgical resection, observation) to SRS in properly selected patients suffering from intracranial MNs.
7.5 Conclusions
Our experience and the data collected from our careful literature review on the subject lead us to the following conclusions:
-
SRS is a safe, effective and reliable treatment option for symptomatic patients with CSMNs (volume <15–20 cc and not adhering to the anterior visual pathways), both as a first choice and as part of an approach combined with surgery (adjuvant or salvage treatment); in most cases SRS provides excellent LTC (volume reduction or halting tumour growth) and an improvement in or stabilization of neurological deficits, with a minimal risk of permanent neurological side effects, as confirmed by data after prolonged periods of observation (over 10 years).
-
Several prognostic factors related to LTC and neurological outcomes of SRS have been identified; greater success rates on CSMNs of volume >10 mL are associated with primary radiosurgical treatment, female sex, sporadic (i.e. single) WHO Grade I, inclusion of the entire volume of meningioma in the treatment plan and a radiation dose ≥13 Gy to the surface of the meningioma, whereas adjuvant or salvage SRS treatments following neurosurgery may be associated with the onset of new cranial nerve deficits and worse neurological prognosis.
-
Finally, numerous cases followed up over long periods of time reveal that SRS does not expose CSMN patients to an increased risk of either malignant transformation or an increase in the incidence of new cancers, as compared to the general population.
Abbreviations
- AVM:
-
Arteriovenous malformation
- CISS:
-
Constructive interference in steady state
- CS:
-
Cavernous sinus
- CSMN:
-
Cavernous sinus meningioma
- CT:
-
Computed tomography
- GTV:
-
Gross target volume
- Gy:
-
Gray
- ID:
-
Integral dose
- LGKRS:
-
Leksell Gamma Knife radiosurgery
- Linac:
-
Linear accelerator
- LTC:
-
Local tumour control
- MD:
-
Maximum dose
- MN:
-
Meningioma
- MRI:
-
Magnetic resonance imaging
- MT:
-
Malignant transformation
- NHS:
-
National Health Service
- PD:
-
Prescription dose
- PI:
-
Prescription isodose
- RIT:
-
Radiation-induced tumorigenesis
- RT:
-
Radiotherapy
- SRS:
-
Stereotactic radiosurgery
- WHO:
-
World Health Organization
References
Correa SF, Marta GN, Teixeira MJ. Neurosymptomatic cavernous sinus meningioma: a 15-years experience with fractionated stereotactic radiotherapy and radiosurgery. Radiat Oncol. 2014;9:27.
Hafez RF, Morgan MS, Fahmy OM. Stereotactic Gamma Knife surgery safety and efficacy in the management of symptomatic benign confined cavernous sinus meningioma. Acta Neurochir. 2015;157(9):1559–64.
Sheehan JP, Starke RM, Kano H, Barnett GH, Mathieu D, Chiang V, et al. Gamma Knife radiosurgery for posterior fossa meningiomas: a multicenter study. J Neurosurg. 2015;122(6):1479–89.
Fariselli L, Biroli A, Signorelli A, Broggi M, Marchetti M, Biroli F. The cavernous sinus meningiomas' dilemma: surgery or stereotactic radiosurgery? Rep Pract Oncol Radiother. 2016;21(4):379–85.
Kano H, Park KJ, Kondziolka D, Iyer A, Liu X, Tonetti D, et al. Does prior microsurgery improve or worsen the outcomes of stereotactic radiosurgery for cavernous sinus meningiomas? Neurosurgery. 2013;73(3):401–10.
Sindou M, Wydh E, Jouanneau E, Nebbal M, Lieutaud T. Long-term follow-up of meningiomas of the cavernous sinus after surgical treatment alone. J Neurosurg. 2007;107(5):937–44.
Sughrue ME, Rutkowski MJ, Aranda D, Barani IJ, McDermott MW, Parsa AT. Factors affecting outcome following treatment of patients with cavernous sinus meningiomas. J Neurosurg. 2010;113(5):1087–92.
Klinger DR, Flores BC, Lewis JJ, Barnett SL. The treatment of cavernous sinus meningiomas: evolution of a modern approach. Neurosurg Focus. 2013;35(6):E8.
Park KJ, Kano H, Iyer A, Liu X, Tonetti DA, Lehocky C, et al. Gamma Knife stereotactic radiosurgery for cavernous sinus meningioma: long-term follow-up in 200 patients. J Neurosurg. 2018:1–10. https://doi.org/10.3171/2018.2.JNS172361.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81.
National Health Service England Clinical Reference Group for Stereotactic Radiosurgery. NHS England D05/P/e. Clinical commissioning policy: stereotactic radiosurgery/radiotherapy for meningioma. September 2013 [cited 2019, 15 April]. Available on: https://www.england.nhs.uk/wp-content/uploads/2013/09/d05-pe1.pdf.
Hazar M, Kazemi F, Jahanbakhshi A, Chanideh I, Jalessi M, Amini E, et al. Gamma Knife Radiosurgery for Cavernous Sinus Meningiomas: Analysis of Outcome in 166 Patients. Stereotact Funct Neurosurg. 2017;95(4):259–67.
Zeiler FA, McDonald PJ, Kaufmann AM, Fewer D, Butler J, Schroeder G, et al. Gamma Knife radiosurgery of cavernous sinus meningiomas: an institutional review. Can J Neurol Sci. 2012;39(6):757–62.
Hayashi M, Chernov M, Tamura N, Tamura M, Horiba A, Konishi Y, et al. Gamma knife radiosurgery for benign cavernous sinus tumors: treatment concept and outcomes in 120 cases. Neurol Med Chir (Tokyo). 2012;52(10):714–23.
Kimball MM, Friedman WA, Foote KD, Bova FJ, Chi YY. Linear accelerator radiosurgery for cavernous sinus meningiomas. Stereotact Funct Neurosurg. 2009;87(2):120–7.
Franzin A, Vimercati A, Medone M, Serra C, Marzoli SB, Forti M, Gioia L, Valle M, Picozzi P. Neuroophthalmological evaluation after Gamma Knife surgery for cavernous sinus meningiomas. Neurosurg Focus. 2007;23(6):E10.
Hasegawa T, Kida Y, Yoshimoto M, Koike J, Iizuka H, Ishii D. Long-term outcomes of Gamma Knife surgery for cavernous sinus meningioma. J Neurosurg. 2007;107(4):745–51.
Pamir MN, Kiliç T, Bayrakli F, Peker S. Changing treatment strategy of cavernous sinus meningiomas: experience of a single institution. Surg Neurol. 2005;64(Suppl. 2):S58–66.
Pollock BE, Stafford SL. Results of stereotactic radiosurgery for patients with imaging defined cavernous sinus meningiomas. Int J Radiat Oncol Biol Phys. 2005;62(5):1427–31.
Maruyama K, Shin M, Kurita H, Kawahara N, Morita A, Kirino T. Proposed treatment strategy for cavernous sinus meningiomas: a prospective study. Neurosurgery. 2004;55(5):1068–75.
Iwai Y, Yamanaka K, Morikawa T, Ishiguro T, Honda Y, Matsusaka Y, et al. The treatment for asymptomatic meningiomas in the era of radiosurgery. No Shinkei Geka. 2003;31(8):891–7.
Spiegelmann R, Nissim O, Menhel J, Alezra D, Pfeffer MR. Linear accelerator radiosurgery for meningiomas in and around the cavernous sinus. Neurosurgery. 2002;51(6):1373–9. discussion 1379-80
Nicolato A, Foroni R, Alessandrini F, Bricolo A, Gerosa M. Radiosurgical treatment of cavernous sinus meningiomas: experience with 122 treated patients. Neurosurgery. 2002;51(5):1153–9. discussion 1159-61
Lee JY, Niranjan A, McInerney J, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. J Neurosurg. 2002;97(1):65–72.
De Salles AA, Frighetto L, Grande CV, Solberg TD, Cabatan-Awang C, Selch MT, Wallace R, Ford J. Radiosurgery and stereotactic radiation therapy of skull base meningiomas: proposal of a grading system. Stereotact Funct Neurosurg. 2001;76(3–4):218–29.
Shin M, Kurita H, Sasaki T, Kawamoto S, Tago M, Kawahara N, et al. Analysis of treatment outcome after stereotactic radiosurgery for cavernous sinus meningiomas. J Neurosurg. 2001;95(3):435–9.
Roche PH, Régis J, Dufour H, Fournier HD, Delsanti C, Pellet W, et al. Gamma knife radiosurgery in the management of cavernous sinus meningiomas. J Neurosurg. 2000;93(Suppl. 3):68–73.
Liscák R, Simonová G, Vymazal J, Janousková L, Vladyka V. Gamma knife radiosurgery of meningiomas in the cavernous sinus region. Acta Neurochir. 1999;141(5):473–80.
Sibtain A, Plowman PN. Stereotactic radiosurgery. VII. Radiosurgery versus conventionally-fractionated radiotherapy in the treatment of cavernous sinus meningiomas. Br J Neurosurg. 1999;13(2):158–66.
Chang SD, Adler JR Jr, Martin DP. LINAC radiosurgery for cavernous sinus meningiomas. Stereotact Funct Neurosurg. 1998;71(1):43–50.
Pendl G, Schröttner O, Eustacchio S, Ganz JC, Feichtinger K. Cavernous sinus meningiomas—what is the strategy: upfront or adjuvant gamma knife surgery? Stereotact Funct Neurosurg. 1998;70(Suppl. 1):33–40.
Kurita H, Sasaki T, Kawamoto S, Taniguchi M, Terahara A, Tago M, et al. Role of radiosurgery in the management of cavernous sinus meningiomas. Acta Neurol Scand. 1997;96(5):297–304.
Duma CM, Lunsford LD, Kondziolka D, Harsh GR 4th, Flickinger JC. Stereotactic radiosurgery of cavernous sinus meningiomas as an addition or alternative to microsurgery. Neurosurgery. 1993;32(5):699–704. discussion 704-5
Nicolato A, Hasanbelliu A, Foroni R, Longhi M, Ricciardi GK, De Simone A, et al. Gamma knife radiosurgery in cavernous sinus meningiomas: results on 170 patients with at least 10-year-follow up period. J Radiosurg SBRT. 2013;2(Suppl. 1):130.
Pollock BE, Stafford SL, Link MJ, Garces YI, Foote RL. Single-fraction radiosurgery of benign cavernous sinus meningiomas. J Neurosurg. 2013;119(3):675–82.
Santacroce A, Walier M, Régis J, Liščák R, Motti E, Lindquist C, et al. Long-term tumor control of benign intracranial meningiomas after radiosurgery in a series of 4565 patients. Neurosurgery. 2012;70(1):32–9. discussion 39
dos Santos MA, de Salcedo JB, Gutiérrez Diaz JA, Calvo FA, Samblás J, Marsiglia H, Sallabanda K. Long-term outcomes of stereotactic radiosurgery for treatment of cavernous sinus meningiomas. Int J Radiat Oncol Biol Phys. 2011;81(5):1436–41.
Skeie BS, Enger PO, Skeie GO, Thorsen F, Pedersen PH. Gamma knife surgery of meningiomas involving the cavernous sinus: long-term follow-up of 100 patients. Neurosurgery. 2010;66(4):661–8. discussion 668-9
Spiegelmann R, Cohen ZR, Nissim O, Alezra D, Pfeffer R. Cavernous sinus meningiomas: a large LINAC radiosurgery series. J Neuro-Oncol. 2010;98(2):195–202.
Metellus P, Regis J, Muracciole X, Fuentes S, Dufour H, Nanni I, et al. Evaluation of fractionated radiotherapy and gamma knife radiosurgery in cavernous sinus meningiomas: treatment strategy. Neurosurgery. 2005;57(5):873–86. discussion 873-86
Sanford NN, Yeap BY, Larvie M, Daartz J, Munzenrider JE, Liebsch NJ, et al. Prospective, randomized study of radiation dose escalation with combined proton-photon therapy for benign meningiomas. Int J Radiat Oncol Biol Phys. 2017;99(4):787–96.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics - 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322.
McClelland S 3rd, Ciporen JN, Mitin T, Jaboin JJ. Long-term stroke risk of single-fraction photon-based stereotactic radiosurgery for meningioma. Clin Neurol Neurosurg. 2018;173:169–72.
Loeffler JS, Niemierko A, Chapman PH. Second tumors after radiosurgery: tip of the iceberg or a bump in the road? Neurosurgery. 2003;52(6):1436–40.
Niranjan A, Kondziolka D, Lunsford LD. Neoplastic transformation after radiosurgery or radiotherapy: risk and realities. Otolaryngol Clin N Am. 2009;42(4):717–29.
Cahan WG, Woodard HQ, Higonbotham NL. Sarcoma arising in irradiated bone; report of 11 cases. Cancer. 1948;1(1):3–29.
Ganz JC. Gamma knife radiosurgery and its possible relationship to malignancy: a review. J Neurosurg. 2002;97(Suppl 5):644–52.
Patel TR, Chiang VL. Secondary neoplasms after stereotactic radiosurgery. World Neurosurg. 2014;81(3–4):594–9.
Starke RM, Yen CP, Chen CJ, Ding D, Mohila CA, Jensen ME, et al. An updated assessment of the risk of radiation-induced neoplasia after radiosurgery of arteriovenous malformations. World Neurosurg. 2014;82(3–4):395–401.
Rowe J, Grainger A, Walton L, Silcocks P, Radatz M, Kemeny A. Risk of malignancy after gamma knife stereotactic radiosurgery. Neurosurgery. 2007;60(1):60–5.
Rahman M, Neal D, Baruch W, Bova FJ, Frentzen BH, Friedman WA. The risk of malignancy anywhere in the body after linear accelerator (LINAC) stereotactic radiosurgery. Stereotact Funct Neurosurg. 2014;92(5):323–33.
Kondziolka DS, Lunsford L. Black holes, white dwarfs, and supernovas: the complications of radiosurgery. J Neurosurg. 2015;122:A1566.
Pollock BE, Link MJ, Stafford SL, Parney IF, Garces YI, Foote RL. The risk of radiation-induced tumors or malignant transformation after single-fraction intracranial radiosurgery: results based on a 25-year experience. Int J Radiat Oncol Biol Phys. 2017;97(5):919–23.
Al-Mefty O, Kadri PA, Pravdenkova S, Sawyer JR, Stangeby C, Husain M. Malignant progression in meningioma: documentation of a series and analysis of cytogenetic findings. J Neurosurg. 2004;101(2):210–8.
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM. Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol. 1997;21(12):1455–65.
Kondziolka D, Patel AD, Kano H, Flickinger JC, Lunsford LD. Long-term outcomes after gamma knife radiosurgery for meningiomas. Am J Clin Oncol. 2016;39(5):453–7.
Endo T, Narisawa A, Ali HS, Murakami K, Watanabe T, Watanabe M, et al. A study of prognostic factors in 45 cases of atypical meningioma. Acta Neurochir. 2016;158(9):1661–7.
Messerer M, Richoz B, Cossu G, Dhermain F, Hottinger AF, Parker F, et al. Recent advances in the management of atypical meningiomas. Neurochirurgie. 2016;62(4):213–22.
Valery CA, Faillot M, Lamproglou I, Golmard JL, Jenny C, Peyre M, et al. Grade II meningiomas and Gamma Knife radiosurgery: analysis of success and failure to improve treatment paradigm. J Neurosurg. 2016;125(Suppl 1):89–96.
Modha A, Gutin PH. Diagnosis and treatment of atypical and anaplastic meningiomas: a review. Neurosurgery. 2005;57(3):538–50.
Gross BA, Chiocca EA. Neoplasm development after stereotactic radiosurgery for arteriovenous malformations. World Neurosurg. 2014;82(3–4):304–6.
Sheehan JP, Niranjan A, Sheehan JM, Jane JA Jr, Laws ER, Kondziolka D, et al. Stereotactic radiosurgery for pituitary adenomas: an intermediate review of its safety, efficacy, and role in the neurosurgical treatment armamentarium. J Neurosurg. 2005;102(4):678–91.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Longhi, M. et al. (2021). Stereotactic Radiosurgery for Cavernous Sinus Meningiomas. In: Longhi, M., Motti, E.D.F., Nicolato, A., Picozzi, P. (eds) Stereotactic Radiosurgery for the Treatment of Central Nervous System Meningiomas. Springer, Cham. https://doi.org/10.1007/978-3-030-79419-4_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-79419-4_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-79418-7
Online ISBN: 978-3-030-79419-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)