Abstract
This chapter presents an outline of relevant research on the interaction between depression and personality dysfunction. It starts with a discussion on the heterogeneity of depression at the phenotypic level and examines theoretical, instrumental, and empirical sources of variability in the depressive phenotype. Following this discussion, the chapter moves on to the concept of intermediate phenotypes as a useful framework to go beyond depressive phenomenology and into underlying affected functional domains. In this regard, the chapter proposes that functional domains related to personality dysfunction are relevant intermediate phenotypes that allow for parsing out the heterogeneity of depression as well as to produce etiopathogenic models and develop targeted anti-depressive interventions. A discussion on the scientific and clinical consequences of this framework is advanced.
Substantial contents of this chapter were taken from Behn et al. (2018).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Depression
- Personality dysfunction
- Borderline personality disorder
- Intermediate phenotypes
- Heterogeneity
1 Introduction
Globally, the lifetime prevalence of major depressive disorder (MDD) is 10–15% of the population (Lépine & Briley, 2011), constituting the third cause of morbidity and accounting for 4.3% of the global burden of illness. Especially when depression is long-lasting and of moderate or severe intensity, this illness may become a serious health condition in which the person suffers greatly and functions poorly at work, at school, and in the family. At its worst, depression can lead to suicide. Over 800,000 commit suicide every year, and it is the second leading cause of death in 15- to 29-year-olds. Treating depression should be a priority worldwide due to the high subjective, social, and economic burden of the illness. However, treatment effectiveness can be greatly improved. A study by Craighead and Dunlop (2014) found that even though two thirds of patients enrolled in randomized clinical trials (RCTs ) for depression show a positive response, only 30–40% present remission of symptoms. An additional factor adding to the social and subjective burden of depression has to do with the recurrent nature of the illness (DeRubeis et al., 2008). Between 50% and 60% of patients experimenting a first major depressive episode will experience a second episode, and of these patients, 70% will experience a third one and 90% a fourth episode (Hart et al., 2001). This means that many depressed patients spend up to 21% of their lives clinically depressed (Vos et al., 2004), which increases the risk for suicidality, comorbidity, and chronic physical illness and impairs physical and psychosocial functioning (Hardeveld et al., 2013).
2 Phenotypic Variability in Depression: Theoretical Heterogeneity
There is sufficient evidence in the field of psychology and psychiatry to support the clinical and scientific contention that depression is a rather heterogeneous clinical entity (Maj, 2012; Zimmerman et al., 2015). Furthermore, it has been argued vehemently that the somewhat disappointing scientific and clinical results may be related to substantive heterogeneity of the syndrome as well as to artificial heterogeneity related to diagnostic rules. In part, diagnostic heterogeneity across mental health conditions, including depression, is a structural result of the polythetic diagnostic system of DSM: a given clinical diagnosis can be arrived at by using different combinations of symptoms. As a result, there are 227 different symptom combinations that follow diagnostic rules for depression (Olbert et al., 2014; Zimmerman et al., 2015). Resulting combinations are varied and can be quite different and even contradictory at the phenotypic level. For example, a patient presenting with depressed mood, weight loss, insomnia, and psychomotor agitation can be diagnosed with major depressive disorder (MDD) as well as a patient suffering from anhedonia, weight gain, hypersomnia, and psychomotor retardation. Within the polythetic structure of DSM and ICD, this proliferation of seemingly opposite presentations can be accounted for by the existence of compound symptoms (including dimensional opposites, e.g., “sleep disturbances”) in addition to single symptoms (e.g., anhedonia) (Zimmerman et al., 2006). However, it can be argued that this heterogeneity is artificial, merely a result of theoretical symptom combinations due to the polythetic structure of DSM, and does not necessarily capture substantial heterogeneity in the clinical syndrome of depression as it occurs in nature, that is, at patient level. Thus, above and beyond the issue of theoretical heterogeneity, empirical heterogeneity needs to be examined as a way to map clinically relevant types of depression naturally presenting in individuals.
3 Phenotypic Variability in Depression: Instrumental Heterogeneity
An additional source of heterogeneity that is also not substantive is related to instrumental heterogeneity. Whatever method is used to analyze patient-level data, symptoms need to be collected using specific instrumentation. These instruments can be interview schedules, used by clinicians, or self-report questionnaires. There are many instruments that are typically used to measure depressive symptoms in individuals, both in clinical and research setting. The underlying assumption is that all these instruments map on the same set of symptoms that constitute a prototype for depression. However, many of the widely used screeners for depression are rather idiosyncratic, that is, there is scarce content overlap between items. According to Fried (2017), taken together, the most common measures used for research in depression map on 52 distinct symptoms, and some of them are compound symptoms that can be disaggregated in such a way that even more symptoms are available. Many of these symptoms are idiosyncratic, that is, they are present in only one or two measures. According to Fried (2017), only 12% of all symptoms were present in the seven most used depression schedules or questionnaires. Thus, the extent to which heterogeneity can be examined in depression appears to be largely contingent on the number of items included in a given instrument. For example, if one is to use the Patient Health Questionnaire (PHQ-9) to measure depression in a patient, less information is available (fewer items, fewer symptoms) compared to using the Beck Depression Inventory (more items, more symptoms). Whether a given questionnaire includes coverage of too few symptoms or too many symptoms depends on the specific use. Typically, practical needs (e.g. fast screening versus detailed case formulation) need to be weighted to decide on how to best strike a balance between fidelity (i.e. how much information is captured by an instrument) and compression (i.e. fewest number of items used to capture this information).
4 Phenotypic Variability in Depression: Empirical Heterogeneity
In contrast to theoretical and instrumental heterogeneity which stems from polythetic diagnostic criteria, empirical heterogeneity requires collecting patient-level data, typically using symptoms described in diagnostic systems and with specific instruments. This means that empirical heterogeneity is still fundamentally constrained for the most part by instrumentation and diagnostic systems. With this idea in mind, Fried and Nesse (2015) found 1030 unique symptom patterns emerging from a sample of 3703 outpatients diagnosed with depression from the STAR*D trial. An overwhelming majority of these profiles (84%) were present in only a handful of individuals, and half of the profiles were exclusively exhibited by one individual. Looking at empirical heterogeneity, other authors have tried to examine the latent structure of depressive symptoms in clinical samples using advanced statistical techniques, most notably latent class or latent profile analysis and taxometric analysis (Baptista et al., 2019; Wardenaar et al., 2017). This research has led to a plethora of studies and scientific articles that can be used to map symptomatic profiles occurring in real patients. However, it is still difficult to aggregate results from this literature, in part because of the great number of parameters that can be adjusted in this statistical models and that can result in different latent class descriptions (van Loo et al., 2018). Thus, if one takes into account the diagnostic rules advanced by the DSM as well as the latent structure literature, profile variability is ubiquitous and at times idiosyncratic, so that more stable patterns of heterogeneity are difficult to map. It is quite likely that heterogeneity cannot be sufficiently parsed out at the phenotypic level.
5 Intermediate Phenotypes as a Way to Parse Out Symptomatic Heterogeneity of Depression
Heterogeneity stemming from all these theoretical, instrumental, and empirical sources is problematic, basically because of the different sources of artificial heterogeneity. This has resulted in many authors advocating for substantial research in the area of differential etiopathogenic pathways towards depression. The principle behind this literature is that if variability cannot accurately or confidently be found at the level of the phenotype, there may be more stability to be found at the etiopathogenic level. The Research Domain Criteria (RDoC) strategy proposed by the National Institute of Mental Health (NIMH) represents perhaps the strongest push in this direction (Cuthbert & Insel, 2013). If stability is to be found in heterogeneity, this will not be accomplished at the phenotypic level but, rather, at the level of genetic vulnerability or at the level of intermediate phenotypes or endophenotypes which connect genetic components to symptom heterogeneity. This focus may be better suited to arrive at substantive models that can aspire to organize phenotypic variability as a secondary phenomenon. Interesting work has been carried out examining the endophenotype by phenotype interaction, including the review by Hasler et al. (2004). Heterogeneity in depression can thus be located not solely at the phenotype level but rather at the interaction between observable depressive symptoms and intermediate phenotypes, including negative mood bias, deficits in reward function, and increased stress sensitivity, among others. Observable symptoms are also not a unique manifestation of a specific vulnerability expressed by an intermediate phenotype. Different intermediate phenotypes can lead to similar symptoms in the same way that different conditions can lead a patient to develop a fever. Just like a fever, depressive symptoms are not univocally related to intermediate phenotypes. In terms of treatment development, this leads to personalized treatment models that target underlining disease mechanisms (intermediate phenotypes). Similarly, authors have looked at the genes by phenotype interaction searching for stability in the seemingly endless proliferation of distinct symptomatic profiles in depression (e.g., see Milaneschi et al., 2016 and Thorp et al., 2019). The great empirical heterogeneity of depressive presentations can be thus reconducted towards a distinct set of intermediate psychological and biological domains that bridge the relationship between genomic complexity and disease heterogeneity in depression (Insel & Cuthbert, 2009).
6 Domains of Personality Functioning Are Intermediate Phenotypes for Depression
The arguments presented above can be organized around two basic ideas. First, depression is a notoriously heterogeneous syndrome. Multiple attempts to organize things at the phenomenological level have largely failed (from Jaspers to the DSM, perhaps), to the extent that even though DSM-5 remains to be a categorical diagnostic tool for the most part, in the introduction of DSM-5, it can be read that “the once plausible goal of identifying homogeneous populations for treatment and research resulted in narrow diagnostic categories that did not capture clinical reality, symptom heterogeneity within disorders, and significant sharing of symptoms across multiple disorders” (APA, 2013, p. 12). Second, different (or the same) depressive symptoms can be explained by vulnerabilities in one or in several intermediate phenotypes; there are no established univocal pathways between symptoms and underlying causes. Thus, the question of the etiology of depression needs to be replaced by the etiologies of depression, in the plural. The concept of intermediate phenotypes is useful in this context.
At the level of intermediate phenotypes, one can locate psychological functions that can be broadly organized within the construct of the personality. The contention that heterogeneity in depressive symptoms can be partially explained by the operation of intermediate phenotypes related to personality functioning is consistent with a common clinical finding: many patients with depression also present with personality dysfunction, and in turn, many patients with personality dysfunction present with depression. The comorbidity of mood disorders including major depressive disorder (MDD), bipolar disorder (BP), and dysthymia (DY) with personality pathology is quite common in clinical settings. In a meta-analysis (Friborg et al., 2014), it was estimated that approximately 45% of patients with major depressive disorder also had a personality disorder and approximately 60% of patients with a diagnosis of personality disorder also have a concurrent diagnosis of a depressive disorder. One likely explanation for the frequency of this concurrent presentation is that there is partial overlap in intermediate phenotypes for both classes of disorders. Depression and personality researchers have not always shared this view, which has led to decades of diagnostic debates ever since systematic empirical research on personality pathology emerged in the 1980s, about three decades later than systematic empirical research on depression. Landmark studies that have characterized the occasional polarization of this debate include, from the mood disorders specialist perspective, Akiskal and McKinney Jr.’s (1973) widely cited study published in Science, arguing that depression is a single and stable clinical entity with rather strong diagnostic borders with other clinical entities. On the personality disorders specialist side, Gunderson and Phillips (1991) have argued that the most prototypical personality disorder, namely, borderline personality disorder (BPD; regarding the status of BPD as a prototypical personality disorder presentation, Wright & Zimmermann, 2015, offer a comprehensive review), exhibits weak and non-specific relationships to depression.
Significant research has also showed that first-line psychotherapeutic and pharmacological interventions to alleviate depressive mood have a diminished effect in patients with BPD and that depressive symptoms can remit with successful treatment of BPD (Gunderson et al., 2004), indicating that mood instability in the setting of personality pathology may exhibit a different pathogenesis than common depression (Stoffers et al., 2010). This debate is still quite active, and, according to recent accounts, “(…) the problem of the boundaries of mood and personality disorder is central to the identity of psychiatry and to its future” (Paris, 2015, p. 7).
Both clinically and scientifically, it is extremely important to further understand the interaction between depression and personality functioning. Personality can be defined as the integrated operation of multiple psychological systems, cognitive and self-functioning (including identity), affect modulation and regulation, behavioral control, and interpersonal functioning. These domains of functioning are consistent with the diagnostic criteria for personality disorders of DSM-IV through DSM-5’s Alternative Model as well as with the new diagnostic scheme proposed by the ICD-11. According to Hasler et al.’ (2004) review on endophenotypes of depression, negative mood bias, impaired learning and memory, impaired reward function, increased stress sensitivity, and executive functioning deficits are all stable endophenotypes for major depressive disorder (MDD). Three of these endophenotypes are also shared with BPD. Thus, personality dysfunction (i.e., impaired operation of psychological systems empirically related to depression) can contribute to the parsing out of symptomatic heterogeneity in depression. For enhanced precision of the argument, we would say that personality functioning can be understood more broadly as an intermediate phenotype, because it refers to psychological mechanisms related to phenotypic complexity (i.e., heterogeneity of depression), sometimes in the absence of clear or reasonable heritability, which is important for the consideration of endophenotypes (Goldman & Ducci, 2007; Gottesman & Gould, 2003; Lenzenweger, 2013). Intermediate phenotypes are a crucial component if one sets out to understand the complex and well-debated relationship between depression and personality dysfunction because, as Choi-Kain and Gunderson state in the conclusion of an excellent book on the subject of mood disorders and BPD (2015), both disorders are “superficially divergent [but] fundamentally overlapping” (p. 257). This formulation expresses precisely the idea that phenotypic variability can be reconducted to common disease mechanisms, that is, to common or at least overlapping intermediate phenotypes.
7 When Depression Is Complicated by Dysfunction in Intermediate Phenotypes Representing Personality Vulnerabilities
The issue of shared or overlapping intermediate phenotypes between personality dysfunction (particularly the case of BPD) and depression has been often framed in terms of a common-cause model (Klein et al., 2011). This model predicts that depression and personality disorders can be distinct entities, with seemingly robust diagnostic borders at the phenotypic level, but they likely share common etiopathogenetic mechanisms that mediate between genomic and symptomatic complexity. This view presupposes no causal influences between both entities in this specific model. In other words, patients frequently present with depression and personality dysfunction, because both problems have the same or similar causal influences, but a patient’s depression is not caused by his or her personality problems. A recent review by Goodman et al. (2015) has argued that MDD and BPD are likely two distinct disorders, sharing common disease mechanisms that account for affective dysregulation, regardless of specific phenotypes. Depressive disorders and personality disorders – in particular BPD, which likely constitutes a prototypical presentation in the realm of personality dysfunction – mainly overlap in the functional domain of affect regulation, that is, they share affective symptomatology. Clinically, BPD patients very often present with a major depressive episode (Newton-Howes et al., 2014). This co-occurrence has also been explained in terms of a diathesis of affective regulation, by an etiological influence related to the personality trait of negative affectivity or neuroticism (Reichborn-Kjennerud et al., 2010; Wright et al., 2012). Negative affectivity expresses a heritable trait characterized by exacerbated negative emotions, sensitivity, and reactivity to stress (Widiger, 2009), that is, it constitutes an endophenotype. In a meta-analysis, the negative affective trait managed to explain almost 30% of the variability in BPD symptoms and 22% of the variability in symptoms of a major depressive episode, suggesting an underlying etiological dimension to both disorders (Kotov et al., 2010; Samuel & Widiger, 2008).
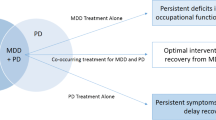
It is likely that the recurrence and treatment challenges related to depression are connected with underlying personality vulnerabilities that complicate the clinical management of patients (see Newton-Howes et al., 2014). These personality vulnerabilities may constitute a personality disorder, but additional clinical presentations where depression is nested within sub-threshold personality vulnerabilities are also likely part of this scenario. In fact, depressive disorders and personality disorders commonly present together. The ubiquity of this comorbidity has important consequences for patient prognosis and typically results in an augmentation of the burden of disease for patients with a depressive disorder (Soeteman, Verheul, & Busschbach, 2008) and consequently an increase in number of life years lost due to disability (Wittchen et al., 2011). Thus, the nature of personality pathology, or even sub-threshold personality vulnerabilities, needs to be examined to understand its contribution to the complication, recurrence, and treatment resistance of complex depression. Patients with comorbid depressive disorder and personality disorders have typically poorer adherence to treatments (Pompili et al., 2009), and their presentation usually configures a more clinically complex level of psychopathology (Friborg et al., 2014). In addition, patients with this dual presentation have almost double the risk to be non-responders after antidepressant psychotherapy compared to those patients with a single diagnosis of depression (Newton-Howes et al., 2014). Moreover, the psychosocial and occupational impairment is higher for patients with comorbid depression and personality pathology (Markowitz et al., 2006), and they appear to be at a higher risk to develop additional formerly designated Axis I psychopathology, especially anxiety (Stein et al., 1993).
In a systematic review and meta-analysis, Köhling, Erenthal, Levy, Schauenberg, and Dinger (2015) concluded that depression in borderline personality disorder (BPD) is characterized by elevations in anger/hostility and self-criticism (as expected in introjective experiences of depression; Blatt & Zuroff, 1992); and for those patients with comorbid depression and BPD, depressive symptomatology is typically more severe when compared to depressed controls (Kohling et al., 2013). Even though a shared intermediate phenotype for depression and BPD includes affect dysregulation, in MDD, affect variability shows a different pattern than in BPD, and in the later, it appears to be restricted to affective reaction to interpersonal rejection (Goodman et al., 2010). A recent study using frequent ecological momentary assessment showed that MDD with BPD patients did not present with higher affective instability, compared to MDD patients (Köhling et al., 2015). The fact that MDD and BPD phenotypes of affect dysregulation are not easily distinguished provides compelling evidence for shared or largely overlapping intermediate phenotypes.
8 Longitudinal Course in Depression and in Personality Dysfunction
Initial accounts indicated that while in depression mood disturbances were episodic, more sustained, and less reactive to environmental stressors, mood dysregulation in BPD exhibited more intense fluctuations and high reactivity to environmental and, in particular, interpersonal stressors (Gunderson, 2007) and specifically sensitivity to interpersonal rejection (Staebler et al., 2011). However, data from longitudinal studies has revealed that the difference between episodic and stable mood symptoms in MDD and intense fluctuations in BPD is not necessarily warranted. Depression often exhibits a recurrent course with inter-episodic maintenance of residual symptoms (Frodl et al., 2008) or even a chronic course from the beginning (Klein, 2010). Notably, early-onset forms of chronic depression typically go along with severe impairment of interpersonal functioning, similar to those found in personality disorders (Klein, 2010), and have been conceptualized as a personality disorder in previous times (Herpertz et al., 1998). BPD patients, on the other hand, typically stop presenting diagnostic threshold symptomatology as time passes (Paris & Zweig-Frank, 2001; Zanarini et al., 2005). In longitudinal studies, remission of BPD in one wave is highly predictive of sustained remission in subsequent waves to a greater degree than remission of depression, which has been shown to have a rather recurrent course.
Taking this evidence into account, strong phenotypic differences between MDD and BPD are not quite as clear as initially had been thought. In fact, phenotypic stability of disorders is largely discussed in current research, particularly in light of recent large-scale studies that have argued for the presence of one common factor underlying pathways to severity across formerly called Axis I mental disorders (Caspi et al., 2014), as well as across personality disorders (Sharp et al., 2015). Regarding the later, the most recent version of the International Classification of Diseases (ICD-11) eliminates the specific classes of personality disorders (e.g., narcissistic, histrionic, and schizoid) and presents dimensional criteria for one single personality disorder, based on domains of functioning and a five-factor model of personality traits, while retaining BPD as qualifier of severity (Herpertz et al., 2017). This diagnostic modification in the realm of personality disorders was already available in part in the hybrid alternative model presented in DSM-5 (Widiger, 2011), which also relies on domains of functioning (which result in dimensional assessment of personality pathology) and on personality traits (which can lead to a categorical diagnosis based on specific trait configurations). Both modifications are substantial and contribute to solve the problem of frequent comorbidity among different personality disorders (Clark, 2005), underlining the idea of a single personality dysfunction component which can present phenotypic variability as a function of profiles of maladaptive personality traits.
9 The Issue of Differential Response in MDD and BPD to Antidepressant Pharmacological Interventions
As indicated before, concurrent presentation of MDD and personality dysfunction is common, and this is consistent with the idea of a common-cause or shared intermediate phenotypes. However, the issue of differential response to antidepressant medication in MDD with or MDD without concurrent personality pathology needs to be considered. If both disorders share the same intermediate phenotypes, then both disorders should exhibit similar patterns of response in depressive symptomatology when antidepressants are administered following clinical protocols, as long, of course, as medication effectively targets these underlying functions. This is, however, not the case. There may be different explanations for this. One explanation is that MDD and BPD (we are focusing on BPD because it concentrates most of the scientific evidence in personality dysfunction research and because it can be considered a prototype or a common factor across different personality disorders) share some intermediate phenotypes, but not others, and alas, common antidepressant medication may provide superior coverage of those intermediate phenotypes that do not significantly overlap with BPD. Another explanation is that MDD and BPD do share the same or most intermediate phenotypes but concurrent presentation of MDD and BPD represents a more extensive deficit of these functions, which may explain diminished effectivity of medication.
10 Is There a Specific Phenotype of Depression in Borderline Dysfunction?
The idea of two distinct yet commonly co-occurring disorders is largely sustained by the evidence pointing towards common disease mechanisms (i.e., a shared diathesis in affect regulation). From this perspective, of course MDD and BPD will often present together. However, authors have also advanced the idea of specific forms of depression that are secondary to personality dysfunction. This causal influence of personality over depression can be understood from the perspective of a predisposition model (Klein et al., 2011), which predicts that specific depressive phenotypes stem from specific personality vulnerabilities.
Most prominently, Sydney Blatt proposed in 1974 that depression may be a by-product of deficits in the structure of object relations, further advancing the idea of two distinct forms of depression, namely, anaclitic and introjective (Blatt, 1974). In his effort to understand the heterogeneity of depressive presentations, Blatt argued that anaclitic depression was characterized by a disruption of interpersonal relatedness (typically fears of abandonment), whereas introjective depression was characterized by deficits in self-integrity and in self-esteem (typically extreme self-criticism; Blatt & Zuroff, 1992). This initial distinction was further developed into a comprehensive theoretical model connecting personality predispositions with stressful life events. The latter is quite interesting, given the pertinence of the early life maltreatment literature to understand depression, personality pathology, and the interaction between the two (Heim & Binder, 2012; Pagano et al., 2004). Recently, Silva et al. (2017) have provided experimental evidence indicating that biological stress reactivity of individuals is modulated by their positioning within an anaclitic or introjective polarity of experience, with introjective individuals exhibiting more objective biological stress reactivity compared to anaclitic individuals, but anaclitic showing higher scores in self-report instruments. Thus, personality predispositions in the anaclitic versus introjective continuum provide a specific vulnerability for the development of depression, particularly when an individual is confronted with stressors.
Within the predisposition model, depression in the setting of BPD has been often investigated as a specific depressive phenotype alongside the literature on phenotypic heterogeneity of depression. This phenotype of borderline depression would be characterized mainly by accelerated patterns of emotional variability (Mneimne et al., 2018; Trull et al., 2008), emerging and hardly identifiable with retrospective self-reports, since these frequently over-represent extreme or concurrent affective states at the time of answering the questionnaire, not knowing the moment-to-moment variability in mood (Fredrickson, 2000; Hufford et al., 2001). In addition, patients with borderline depression would exhibit greater impulsivity, aggressiveness/hostility, and interpersonal hypersensitivity (Fertuck et al., 2013; Rogers et al., 1995). They are also patients who would present a greater risk of developing self-injurious and/or suicidal behaviors (Lieb et al., 2004). In summary, this particular phenotype would be characterized, therefore, by emergent and rapid psychic variability and by deficits in intermediate phenotypes underlying BPD, including affective dysregulation, impulsivity and behavioral dysregulation, and interpersonal hyper-responsiveness (Gunderson & Lyons-Ruth, 2008). This evidence may contribute to differential diagnosis between concurrent MDD and BPD, on the one hand, and borderline depression, on the other.
The predisposition model predicts that depression is tributary to, not concurrent with, the personality dysfunction. A careful evaluation of the level of the personality dysfunction within a continuum of severity is called for and prescribed by current diagnostic guidelines, including the ICD-11 and the DSM-5 alternative model. The level of personality function can be most aptly evaluated within the spectrum of self-other representations (Leising & Zimmermann, 2011). The operationalized psychodynamic diagnosis (OPD) system offers a useful theoretical and empirical framework for research and for clinical use (OPD Task Force, 2008). The OPD is a psychodynamically informed multiaxial system, initially developed over 25 years ago with the goal of providing a reliable diagnostic and research tool that would allow a more comprehensive evaluation of patient’s functioning, beyond symptomatic presentations typically covered by standard diagnostic manuals. A comprehensive review of the OPD system can be found elsewhere (e.g., in Cierpka et al., 2007). We will focus our discussion on Axis IV, which covers the concept of structure and that is useful to evaluate levels of personality functioning. Specifically, OPD operationalizes structure in terms of self-other functioning, including perception and cognition of the self and others, regulation of self and others, regulation of internal versus external representations of others, and the level of attachment to internal and external representations of the self and others (Zimmermann et al., 2012). What is essential to our current discussion is that the level of personality functioning appears to be sensitive in distinguishing between borderline depression and MDD comorbid with BPD, because it exhibits high correlations with clinically rated personality disorders, but not with Axis I diagnoses. This may indicate that the OPD system may go beyond the fact that MDD and BPD have likely common causes and provide subtle coverage of the predispositional component in borderline depression (Zimmermann et al., 2012).
11 Discussion
Significant advances in research on the etiology of depression are urgently needed. Treatment effectiveness is still not where it should be, and many patients do not experience full remission, or even remission that may translate in noticeable improvement of life quality. Complicating the advancement of robust etiological models is the fact that depression is a notoriously heterogeneous clinical syndrome, and this heterogeneity can be established at the theoretical, instrumental, and empirical level. Treatment development and delivery needs to be personalized and for this to be achieved, phenotypic heterogeneity must be parsed out at the level where it matters. This level can be aptly represented by the concept of intermediate phenotype. Intermediate phenotypes are underlying functional domains that may lead to different observable symptoms. Symptom heterogeneity is vast, but vulnerability in relevant functional domains that express at the phenotypic level can perhaps be reduced to only a few candidates.
Functional domains related to personality are good candidates to explain some of the heterogeneity of the depression. In other words, the question about the etiologies of depression is intimately related to the question of personality function, understood as a set of interrelated functional domains that can be conceptualized as intermediate phenotypes. Research in this area has been growing and presents a promising direction to improve models of disease mechanisms and, more importantly, to develop differential treatment components for patients that differ not at the level of phenotype but, rather, at the level of affected intermediate phenotypes. Future instrument development should also be calibrated to measure deficits in these dimensions. Thus, measuring personality functioning may be a promising route to design and deliver personalized mental health treatment.
References
Akiskal, H. S., & McKinney, W. T. (1973). Depressive disorders: Toward a unified hypothesis: Clinical, experimental, genetic, biochemical, and neurophysiological data are integrated. Science, 182(4107), 20–29.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. American Psychiatric Association.
Baptista, M. N., Cunha, F., & Hauck, N. (2019). The latent structure of depression symptoms and suicidal thoughts in Brazilian youths. Journal of Affective Disorders, 254, 90–97.
Behn, A., Herpertz, S. C., & Krause, M. (2018). The interaction between depression and personality dysfunction: State of the art, current challenges, and future directions. Introduction to the special section. Psykhe, 27(2).
Blatt, S. J. (1974). Levels of object representation in anaclitic and introjective depression. The Psychoanalytic Study of the Child, 29, 107–157.
Blatt, S. J., & Zuroff, D. C. (1992). Interpersonal relatedness and self-definition: Two prototypes for depression. Clinical Psychology Review, 12, 527–562.
Caspi, A., Houts, R. M., Belsky, D. W., Goldman-Mellor, S. J., Harrington, H., Israel, S., … Moffitt, T. E. (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137.
Choi-Kain, L. W., & Gunderson, J. G. (2015). Conclusion: integration and synthesis. In Borderline personality and mood disorders (pp. 255–270). Springer.
Cierpka, M., Grande, T., Rudolf, G., Von Der Tann, M., & Stasch, M. (2007). The operationalized psychodynamic diagnostics system: Clinical relevance, reliability and validity. Psychopathology, 40(4), 209–220.
Clark, L. A. (2005). Stability and change in personality pathology: Revelations of three longitudinal studies. Journal of Personality Disorders, 19(5), 524–532.
Craighead, W. E., & Dunlop, B. W. (2014). Combination psychotherapy and antidepressant medication treatment for depression: For whom, when, and how. Annual Review of Psychology, 65, 267–300.
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126.
DeRubeis, R. J., Siegle, G. J., & Hollon, S. D. (2008). Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience, 9(10), 788–796.
Fertuck, E. A., Grinband, J., & Stanley, B. (2013). Facial trust appraisal negatively biased in borderline personality disorder. Psychiatry Research, 207(3), 195–202.
Fredrickson, B. L. (2000). Extracting meaning from past affective experiences: The importance of peaks, ends, and specific emotions. Cognition & Emotion, 14(4), 577–606.
Friborg, O., Martinsen, E. W., Martinussen, M., Kaiser, S., Øvergård, K. T., & Rosenvinge, J. H. (2014). Comorbidity of personality disorders in mood disorders: A meta-analytic review of 122 studies from 1988 to 2010. Journal of Affective Disorders, 152, 1–11.
Fried, E. I. (2017). The 52 symptoms of major depression: Lack of content overlap among seven common depression scales. Journal of Affective Disorders, 208, 191–197.
Fried, E. I., & Nesse, R. M. (2015). Depression is not a consistent syndrome: An investigation of unique symptom patterns in the STAR* D study. Journal of Affective Disorders, 172, 96–102.
Frodl, T., Möller, H. J., & Meisenzahl, E. (2008). Neuroimaging genetics: New perspectives in research on major depression? Acta Psychiatrica Scandinavica, 118(5), 363–372.
Goldman, D., & Ducci, F. (2007). Deconstruction of vulnerability to complex diseases: Enhanced effect sizes and power of intermediate phenotypes. The Scientific World Journal, 7, 124–130.
Goodman, M., Chowdhury, S., New, A. S., & Siever, L. J. (2015). Depressive disorders in borderline personality disorder: Phenomenology and biological markers. In Borderline personality and mood disorders (pp. 13–37). Springer.
Goodman, M., New, A. S., Triebwasser, J., Collins, K. A., & Siever, L. (2010). Phenotype, endophenotype, and genotype comparisons between borderline personality disorder and major depressive disorder. Journal of Personality Disorders, 24(1), 38–59.
Gottesman, I. I., & Gould, T. D. (2003). The endophenotype concept in psychiatry: Etymology and strategic intentions. American Journal of Psychiatry, 160(4), 636–645.
Gunderson, J. G. (2007). Disturbed relationships as a phenotype for borderline personality disorder. The American Journal of Psychiatry, 164, 1637–1640.
Gunderson, J. G., & Lyons-Ruth, K. (2008). BPD’s interpersonal hypersensitivity phenotype: A gene-environment-developmental model. Journal of Personality Disorders, 22(1), 22–41.
Gunderson, J. G., Morey, L. C., Stout, R. L., Skodol, A. E., Shea, M. T., McGlashan, T. H., ... & Bender, D. S. (2004). Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. Journal of Clinical Psychiatry, 65(8), 1049.
Gunderson, J. G., & Phillips, K. A. (1991). A current view of the interface between borderline personality disorder and depression. The American Journal of Psychiatry, 148(8), 967–975.
Hardeveld, F., Spijker, J., De Graaf, R., Nolen, W. A., & Beekman, A. T. F. (2013). Recurrence of major depressive disorder and its predictors in the general population: Results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Psychol Med, 43(1), 39–48.
Hart, A. B., Craighead, W. E., & Craighead, L. W. (2001). Predicting recurrence of major depressive disorder in young adults: A prospective study. Journal of Abnormal Psychology, 110(4), 633.
Hasler, G., Drevets, W. C., Manji, H. K., & Charney, D. S. (2004). Discovering endophenotypes for major depression. Neuropsychopharmacology, 29(10), 1765–1781.
Heim, C., & Binder, E. B. (2012). Current research trends in early life stress and depression: Review of human studies on sensitive periods, gene–environment interactions, and epigenetics. Experimental Neurology, 233(1), 102–111.
Herpertz, S. C., Huprich, S. K., Bohus, M., Chanen, A., Goodman, M., Mehlum, L., ... & Sharp, C. (2017). The challenge of transforming the diagnostic system of personality disorders. Journal of personality disorders, 31(5), 577–589.
Herpertz, S., Steinmeyer, E. M., & Saß, H. (1998). On the conceptualisation of subaffective personality disorders. European Psychiatry, 13(1), 9–17.
Hufford, M. R., Shiffman, S., Paty, J., & Stone, A. A. (2001). Ecological momentary assessment: Real-world, real-time measurement of patient experience. In J. Fahrenberg & M. Myrtek (Eds.), Progress in ambulatory assessment: Computer-assisted psychological and psychophysiological methods in monitoring and field studies (pp. 69–92). Hogrefe/Huber Publishers.
Insel, T. R., & Cuthbert, B. N. (2009). Endophenotypes: Bridging genomic complexity and disorder heterogeneity. Biological Psychiatry, 66(11), 988–989.
Klein, D. N. (2010). Chronic depression: Diagnosis and classification. Current Directions in Psychological Science, 19(2), 96–100.
Klein, D. N., Kotov, R., & Bufferd, S. J. (2011). Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology, 7, 269–295.
Köhling, J., Ehrenthal, J. C., Levy, K. N., Schauenburg, H., & Dinger, U. (2015). Quality and severity of depression in borderline personality disorder: A systematic review and meta-analysis. Clinical Psychology Review, 37, 13–25.
Köhling, J., Moessner, M., Ehrenthal, J. C., Bauer, S., Cierpka, M., Kämmerer, A., ... & Dinger, U. (2016). Affective instability and reactivity in depressed patients with and without borderline pathology. Journal of Personality Disorders, 30(6), 776–795.
Kotov, R., Gamez, W., Schmidt, F., & Watson, D. (2010). Linking “big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin, 136, 768–821.
Leising, D., & Zimmermann, J. (2011). An integrative conceptual framework for assessing personality and personality pathology. Review of General Psychology, 15(4), 317.
Lenzenweger, M. F. (2013). Endophenotype, intermediate phenotype, biomarker: Definitions, concept comparisons, clarifications. Depression and Anxiety, 30(3), 185–189.
Lépine, J. P., & Briley, M. (2011). The increasing burden of depression. Neuropsychiatric Disease and Treatment, 7(Suppl 1), 3.
Lieb, K., Zanarini, M. C., Schmahl, C., Linehan, M. M., & Bohus, M. (2004). Borderline personality disorder. The Lancet, 364(9432), 453–461.
Maj, M. (2012). Development and validation of the current concept of major depression. Psychopathology, 45(3), 135–146.
Markowitz, J. C., Skodol, A. E., & Bleiberg, K. (2006). Interpersonal psychotherapy for borderline personality disorder: Possible mechanisms of change. Journal of Clinical Psychology, 62, 431–444.
Milaneschi, Y., Lamers, F., Peyrot, W. J., Abdellaoui, A., Willemsen, G., Hottenga, J. J., … Boomsma, D. I. (2016). Polygenic dissection of major depression clinical heterogeneity. Molecular Psychiatry, 21(4), 516–522.
Mneimne, M., Fleeson, W., Arnold, E. M., & Furr, R. M. (2018). Differentiating the everyday emotion dynamics of borderline personality disorder from major depressive disorder and bipolar disorder. Personality Disorders: Theory, Research, and Treatment, 9(2), 192.
Newton-Howes, G., Tyrer, P., Johnson, T., Mulder, R., Kool, S., Dekker, J., & Schoevers, R. (2014). Influence of personality on the outcome of treatment in depression: Systematic review and meta-analysis. Journal of Personality Disorders, 28, 577–593.
Olbert, C. M., Gala, G. J., & Tupler, L. A. (2014). Quantifying heterogeneity attributable to polythetic diagnostic criteria: Theoretical framework and empirical application. Journal of Abnormal Psychology, 123(2), 452.
OPD Task Force. (Ed.). (2008). Operationalized psychodynamic diagnosis OPD-2: Manual of diagnosis and treatment planning. Hogrefe Publishing.
Pagano, M. E., Skodol, A. E., Stout, R. L., Shea, M. T., Yen, S., Grilo, C. M., … Gunderson, J. G. (2004). Stressful life events as predictors of functioning: Findings from the collaborative longitudinal personality disorders study. Acta Psychiatrica Scandinavica, 110, 421–429.
Paris, J. (2015). Mood disorders and personality disorders: Simplicity and complexity. In Borderline personality and mood disorders (pp. 3–9). Springer.
Paris, J., & Zweig-Frank, H. (2001). The 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry.
Pompili, M., Di Cosimo, D., Innamorati, M., Lester, D., Tatarelli, R., & Martelletti, P. (2009). Psychiatric comorbidity in patients with chronic daily headache and migraine: a selective overview including personality traits and suicide risk. The journal of headache and pain, 10(4), 283–290.
Reichborn-Kjennerud, T., Czajkowski, N., Røysamb, E., Ørstavik, R. E., Neale, M. C., Torgersen, S., & Kendler, K. S. (2010). Major depression and dimensional representations of DSM-IV personality disorders: A population-based twin study. Psychological Medicine, 40, 1475–1484.
Rogers, J. H., Widiger, T. A., & Krupp, A. (1995). Aspects of depression associated with borderline personality disorder. The American Journal of Psychiatry, 152(2), 268–270.
Samuel, D. B., & Widiger, T. A. (2008). A meta-analytic review of the relationships between the five-factor model and DSM-IV-TR personality disorders: A facet level analysis. Clinical Psychology Review, 28, 1326–1342.
Sharp, C., Wright, A. G. C., Fowler, J. C., Frueh, B. C., Allen, J. G., Oldham, J., & Clark, L. A. (2015). The structure of personality pathology: Both general (‘g’) and specific (‘s’) factors? Journal of Abnormal Psychology, 124, 387–398.
Silva, J. R., Vivanco-Carlevari, A., Barrientos, M., Martínez, C., Salazar, L. A., & Krause, M. (2017). Biological stress reactivity as an index of the two polarities of the experience model. Psychoneuroendocrinology, 84, 83–86.
Soeteman, D. I., Verheul, R., & Busschbach, J. J. (2008). The burden of disease in personality disorders: diagnosis-specific quality of life. Journal of personality disorders, 22(3), 259–268.
Staebler, K., Helbing, E., Rosenbach, C., & Renneberg, B. (2011). Rejection sensitivity and borderline personality disorder. Clinical psychology & psychotherapy, 18(4), 275–283.
Stein, D. J., Hollander, E., & Skodol, A. E. (1993). Anxiety disorders and personality disorders: A review. Journal of Personality Disorders, 7(2), 87–104.
Stoffers, J., Völlm, B. A., Rücker, G., Timmer, A., Huband, N., & Lieb, K. (2010). Pharmacological interventions for borderline personality disorder. The Cochrane Database of Systematic Reviews, 6, Article CD005653.
Thorp, J. G., Marees, A. T., Ong, J. S., An, J., MacGregor, S., & Derks, E. M. (2019). Genetic heterogeneity in self-reported depressive symptoms identified through genetic analyses of the PHQ-9. Psychological Medicine, 1–12.
Trull, T. J., Solhan, M. B., Tragesser, S. L., Jahng, S., Wood, P. K., Piasecki, T. M., & Watson, D. (2008). Affective instability: Measuring a core feature of borderline personality disorder with ecological momentary assessment. Journal of Abnormal Psychology, 117, 647–661.
van Loo, H. M., Wanders, R. B., Wardenaar, K. J., & Fried, E. I. (2018). Problems with latent class analysis to detect data-driven subtypes of depression. Molecular Psychiatry, 23(3), 495–496.
Vos, T., Haby, M. M., Barendregt, J. J., Kruijshaar, M., Corry, J., & Andrews, G. (2004). The burden of major depression avoidable by longer-term treatment strategies. Archives of General Psychiatry, 61(11), 1097–1103.
Wardenaar, K. J., Wanders, R. B., ten Have, M., de Graaf, R., & de Jonge, P. (2017). Using a hybrid subtyping model to capture patterns and dimensionality of depressive and anxiety symptomatology in the general population. Journal of Affective Disorders, 215, 125–134.
Widiger, T. A. (2009). Neuroticism. In M. R. Leary & R. H. Hoyle (Eds.), Handbook of individual differences in social behavior (pp. 129–146). Guilford Press.
Widiger, T. A. (2011). The DSM-5 dimensional model of personality disorder: Rationale and empirical support. Journal of Personality Disorders, 25(2), 222–234.
Wittchen, H. U., Jacobi, F., Rehm, J., Gustavsson, A., Svensson, M., Jönsson, B., … Fratiglioni, L. (2011). The size and burden of mental disorders and other disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21(9), 655–679.
Wright, A. G., Thomas, K. M., Hopwood, C. J., Markon, K. E., Pincus, A. L., & Krueger, R. F. (2012). The hierarchical structure of DSM-5 pathological personality traits. Journal of Abnormal Psychology, 121, 951–957.
Wright, A. G. C., & Zimmermann, J. (2015). At the nexus of science and practice: Answering basic clinical questions in personality disorder assessment and diagnosis with quantitative modeling techniques. In S. K. Huprich (Ed.), Personality disorders: Assessment, diagnosis, and research (pp. 109–144). American Psychological Association.
Zanarini, M. C., Frankenburg, F. R., Hennen, J., Reich, D. B., & Silk, K. R. (2005). The McLean Study of Adult Development (MSAD): Overview and implications of the first six years of prospective follow-up. Journal of Personality Disorders, 19(5), 505–523.
Zimmerman, M., Ellison, W., Young, D., Chelminski, I., & Dalrymple, K. (2015). How many different ways do patients meet the diagnostic criteria for major depressive disorder? Comprehensive Psychiatry, 56, 29–34.
Zimmerman, M., McGlinchey, J. B., Young, D., & Chelminski, I. (2006). Diagnosing major depressive disorder: II: Is there justification for compound symptom criteria? The Journal of Nervous and Mental Disease, 194(4), 235–240.
Zimmermann, J., Ehrenthal, J. C., Cierpka, M., Schauenburg, H., Doering, S., & Benecke, C. (2012). Assessing the level of structural integration using operationalized psychodynamic diagnosis (OPD): Implications for DSM-5. Journal of Personality Assessment, 94, 522–532.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Behn, A., Krause, M. (2021). Depression and Personality Dysfunction: Moving from Descriptive Comorbidity to the Identification of Common Intermediate Phenotypes. In: Jiménez, J.P., Botto, A., Fonagy, P. (eds) Etiopathogenic Theories and Models in Depression. Depression and Personality. Springer, Cham. https://doi.org/10.1007/978-3-030-77329-8_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-77329-8_14
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-77328-1
Online ISBN: 978-3-030-77329-8
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)