Abstract
Peritoneal dialysis (PD) is an important dialysis modality that provides individuals with stage 5 kidney disease the opportunity to take a greater role in their own care and be relatively independent from the hospital. Although there is no demonstrable difference in survival between patients who choose PD compared with those who choose hemodialysis for their treatment, technique failure (TF) with PD limits the time on therapy for many patients. TF can be a consequence of the main complications of PD – these include access problems, infection, limitations on solute clearance and ultrafiltration as well as challenges for the individual in managing their treatment. International guidelines present the best evidence to reduce the risk of and to manage these complications which are most appropriately managed through center-based continuous quality improvement. Ongoing research studies including the Peritoneal Dialysis Outcomes and Practice Patterns Study aim to find the best clinical management approaches to deliver PD with the lowest possible risk of TF.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Peritoneal dialysis access
- Peritoneal infection
- Solute clearance
- Ultrafiltration
- Peritoneal membrane
- Metabolic complications
-
1.
Peritoneal dialysis is limited by technique failure (TF).
-
2.
The most important causes of TF include infection (peritonitis, exit site and tunnel infection), problems with the catheter, and limitations in solute and fluid removal.
-
3.
Each centre should audit peritoneal infection rates as well as the success and complications of catheter insertion on a regular basis and undertake root cause analysis to better understand causes and remediable actions.
-
4.
Regular multidisciplinary meetings should consider patient progress including the adequacy of solute clearance and volume management. These meetings should also consider patient requirements for support and how that changes over time.
-
5.
Guidelines to support patient management are available at ► ISPD.org.
1 Introduction
For many patients, peritoneal dialysis (PD) is an excellent therapy in which they can take control of their own care and remain independent from hospital. Outcomes are at least equal, if not better, for patients on peritoneal dialysis compared with hemodialysis (HD) [1] – however, most of the data is from registries. Only one randomized controlled trial has been published that compared dialysis modalities - however it was unable to recruit a sufficient number of patients [2]. A whole range of factors influence the comparison including comorbidity, age, residual renal function, late presentation, and the access used for HD. In general, effective management requires a multidisciplinary team-based approach that adheres to guidance produced by the International Society of Peritoneal Dialysis (► Box 84.1) underpinned by regular audit. Optimal care requires regular review of patient progress that includes problem-solving and prescription management, ultimately planning transfer to HD in those for whom PD is becoming no longer viable [3].
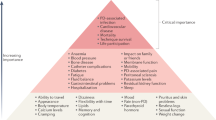
The likelihood of a particular PD-related complication is influenced to some extent by the time that the patient has been on PD, and a schema is presented in ◘ Fig. 84.1. Patients may discontinue PD for a range of reasons including access-related and mechanical complications, infection, problems with ultrafiltration and solute clearance as well as psychosocial problems [4]. This is described broadly as technique failure (TF) and is the primary outcome measure of the international Peritoneal Dialysis Outcomes and Practice Patterns Study [5]. Commonly emphasis is placed on the risk that patients on PD face without due recognition of the complications that are associated with HD. Although peritonitis is the most common complication of PD, bacteremia is rare and hospitalization for infection is similar between the modalities [6]. Low infection rates are possible based on regular education of patients and staff. When it comes to the important issue of access there is an appreciation of the difficulties that can occur when PD catheters don’t work properly, but the burden is similar to that experienced by HD patients requiring revision of their vascular access [7]. Encapsulating peritoneal sclerosis (EPS) is a dreaded potential complication of PD, but is exceptionally rare in the early years of PD, and is declining in incidence [8]. It is by no means as frequent a risk factor as the major causes of adverse outcome that affect our patients [9].
Case Study
Peritoneal Access
A 54-year-old male with progressive kidney disease is admitted to hospital feeling unwell. It is clear that he will need to start dialysis within the next few weeks. He works full time and is keen to remain as independent as possible. What considerations will you have as you plan his dialysis? How will you involve him in those discussions? What approach will you use for access placement and what will determine when dialysis can start?
Infection
A 74-year-old lady who has been on PD for 20 months presents with a 3-hour history of cloudy dialysate and abdominal pain. What initial assessment will you make and samples will you arrange? What will be your initial therapy and how will you assess response? At your unit, how frequent is PD peritonitis and what are the key steps that can be taken to reduce the rate?
Ultrafiltration
A 20-year-old student has recently transferred from HD to PD in order to have more time to attend college. At the first clinic attendance you note evidence of volume overload and poor blood pressure control. How will you go about assessing the patient and their therapy to inform decisions that can be made to resolve the problem?
2 Peritoneal Dialysis-Associated Infection
2.1 Prevention of PD-Associated Infection
In the early days of PD, infection was a common and difficult problem with peritonitis occurring every few months. Considerable attention has been given to this complication resulting in a marked improvement. Over the last 3 decades technical developments have included the change from glass bottles to plastic bags, improved systems (with the disconnect system and flush-before-fill), and more recently, the use of prophylactic antibacterial creams at the exit site. Emphasis has been placed on the importance of training for staff, patients, and carers and the role of audit to understand infection rates and causative organisms (◘ Fig. 84.2). There is evidence that the degree of nursing experience and patient training methods influence the risk of PD infections which should be based on the principles of adult education. Refresher courses are recommended for patients 3 months after initial training and routinely thereafter at a minimum of once a year as well as following hospitalization, episodes of peritonitis and catheter infection or if there is a change in dexterity, vision, or mental acuity. International society for peritoneal dialysis (ISPD) has published an open access curriculum for patient training [10].
► Box 84.2 summarizes multidisciplinary team-based initiatives that have an impact on preventing peritoneal dialysis-associated infection. Peritonitis rates are reported as episodes per patient-year of therapy with the best centers having rates that are less than 0.3 (equivalent to 1 infection per 36 months of treatment). For example, data from the French registry showed that half of the patients did not experience this complication in 31 months [11]. There are many publications on PD-associated infection, but few randomized controlled trials. The best resources are the guidelines from the ISPD [12] which are free to download from ► www.ispd.org (► Box 84.1).
An important part of infection prevention relates to the procedures for catheter placement and techniques focused on the prevention of exit site infection. Catheter placement should be governed by clear protocols [13] with the exit site location being selected preoperatively in discussion with the patient so that it is placed in a suitable position that is not at risk of abrasion from the belt and is easy for the patient to attend to. Recommendations regarding post-operative management of the PD catheter in order to minimize the risk of exit site infection are summarized in ► Box 84.3. There is good evidence for the preventative use of antibiotic creams at the exit site with meta-analysis showing benefit for mupirocin use on both exit site infection and peritonitis due to Staphylococcus aureus [14].
2.2 PD Peritonitis
PD peritonitis is the leading cause of TF and confers an increased mortality risk; if severe and prolonged, it can be associated with peritoneal membrane damage. It is diagnosed by the presence of abdominal pain and cloudy dialysate effluent that has a leucocyte count greater than 100/mm3. In APD with rapid cycling there may be a lower cell count; therefore, a differential count of >50% neutrophils is considered diagnostic. It is possible to overlook the diagnosis of peritonitis in automated peritoneal dialysis (APD) patients if the effluent line runs straight to a drain without collecting in a bag and leucocyte esterase sticks are sometimes used by patients to test the effluent dialysate. Patients presenting with peritonitis range from the mildly unwell, who can be managed easily as an outpatient, to those with marked features of systemic sepsis requiring admission to hospital. The principal sources of contamination include a break in the sterile technique and infection at the exit site – others are organisms within the catheter biofilm, transmural migration of organisms across the bowel wall and rarely hematogenous spread or vaginal leak.
Root cause analysis should be performed after every episode of peritonitis to understand modifiable risk factors as much as possible and plan an intervention strategy. There are a number of potentially modifiable risk factors associated with PD peritonitis including depression, hypoalbuminemia, hypokalemia, constipation, exit site colonization, infection, connection methodology, technique errors, prolonged antibiotics, and medical procedures.
It is important that peritonitis is diagnosed promptly so that appropriate treatment can be started immediately and therefore the patient and their carers require clear contact details of the unit. The health care team should be experienced in the diagnosis and management of peritonitis, supported by evidence-based protocols. Presentation to the incorrect hospital department can potentially lead to misdiagnosis and inappropriate management. A suitable technique for dialysate sampling is required in order to maximize the opportunity for identifying the causative organism. The recommended approach to dialysate sampling is either the inoculation of blood culture bottles or centrifugation of 50 mL of peritoneal effluent at 3000 g for 15 minutes, followed by resuspension of the sediment in 3–5 mL of sterile saline and inoculation of this material both on solid culture media and into a standard blood culture medium [12].
The differential diagnosis of cloudy dialysate fluid includes noninfectious causes such as chemical and allergic peritonitis, hemoperitoneum, malignancy, and chylous effluent. A dialysate sample should ideally be taken after a 2-hour dwell and samples taken from a “dry” abdomen can give a spuriously elevated WCC.
Inability to identify the causative organism has implications for primary cure with most studies showing poorer outcomes where the organism has not been identified. Causes of sterile peritonitis include poor dialysate sampling and culture techniques, as well as recent courses of antibiotics – for example, the treatment of an exit site infection (► Box 84.4). It is important to have a low threshold for the possibility of surgical peritonitis in a PD patient since this can pose diagnostic and therapeutic challenges and may occur in 10% of the cases, resulting from inflammation, perforation, or ischemia of intra-abdominal organs. There are several possible pitfalls in the diagnosis of that complication including the innocent finding of air under the diaphragm of patients on PD, the possibility that serum amylase may be spuriously low in patients on icodextrin, and poor diagnostic sensitivity of CT scanning. Delays in institution of appropriate treatment, particularly surgical intervention, lead to increased morbidity and mortality [15].
The nature of organisms causing PD peritonitis has changed over the last 3 decades. Whereas gram-positive organisms were the commonest, their relative frequency has been reduced by improvements in technology and technique as demonstrated by a 25-year single-center experience from Brazil [16]. As a result, patients presenting with PD peritonitis are more likely than previously to have gram-negative infections, which needs to be considered when designing treatment protocols. It is important that individual centers examine their own patterns of infection, causative organisms, and sensitivities and adapt protocols as necessary for local conditions.
2.3 Treatment of PD Peritonitis
The ideal antibiotic should give broad coverage of organisms, avoid disturbing normal bacterial flora, have a low side-effect profile, should not provoke the emergence of resistant organisms, and be convenient to administer and cheap. This will be influenced by the pharmacokinetic and pharmacodynamic profile as well as the potential side effects of particular antibiotics [17]. A number of factors impact on the choice of antibiotics that are used to treat peritonitis including the emergence of vancomycin-resistant enterococci, reports of vancomycin-intermediately sensitive S. aureus, methicillin resistance and gram-negative enteric bacteria such as E. coli and Klebsiella pneumoniae that produce Extended Spectrum β-Lactamases (ESBL) and carbapenemases [12, 18] as well as concern regarding the impact of aminoglycosides on residual renal function.
Initial empirical treatment for PD peritonitis should cover both gram-positive and gram-negative organisms and be governed by an understanding of local organisms and their sensitivities. The ISPD infection guidelines recommend possible antibiotic schedules including either the combination of a third-generation cephalosporin (ceftazidime) or an aminoglycoside for gram-negative cover with a first-generation cephalosporin (cephazolin) or vancomycin for gram-positive cover [12]. A Cochrane systematic review favored a vancomycin-based regimen; however, the evidence was graded as low quality [19]. It is important to liaise with the local microbiological team regarding the most appropriate protocol. Treatment should be adjusted once the organism has been identified and for detailed discussion the reader should access the guideline. Emphasis should be on preservation of the peritoneal membrane and the overall health of the patient rather than persisting with PD where the infection is not responding to treatment. It is recommended that the PD catheter should be removed if the patient does not respond within 5 days of treatment (► Box 84.5), however there should be a low threshold to remove it earlier if the patient is significantly unwell. It is often appropriate to consider returning to PD with a new catheter once the infection has cleared. Vancomycin and aminoglycoside doses require adjustment based on antibiotic levels due to complex pharmacodynamics which are influenced by a range of factors including patient size, dialysate flow rates, peritoneal membrane characteristics, the molecular weight of the antibiotic, degree of residual renal function, whether the patient is on continuous ambulatory peritoneal dialysis (CAPD) or APD, and whether it is administered continuously or intermittently [20].
3 Exit Site Infection (ESI)
The importance of ESI is that it is a risk factor for PD peritonitis. Once the exit site has become colonized with infecting organisms, eradication may be problematic and require prolonged courses of antibiotics. Strategies to reduce the risk of this complication are essential and are summarized in the appropriate guideline from the ISPD [21]. These start before the catheter is placed with a careful discussion with the patient regarding the location of the exit site, catheter placement protocols to minimize the risk of infection, and a rigorous approach to postoperative exit site care. Exit site prophylaxis with antibacterial creams have been demonstrated to have an impact on both exit site and peritonitis rates, in particular with gram-positive organisms [14]. A positive nose swab for Staphylococcus aureus is associated with an increased likelihood of developing an exit site infection.
Although purulent drainage from the exit site indicates the presence of infection, erythema is not specific. The identification of an organism in the absence of inflammation indicates colonization, and does not require treatment. An exit site scoring system recommended by the ISPD is based on the presence of swelling, redness, pain, and discharge [22] (◘ Fig. 84.3).
Exit site scoring using the ISPD recommended system [22]
Treatment of an infected exit site requires appropriate antibiotics based on swab results and a prolonged course of antibiotics may be necessary. Infecting organisms are most commonly Staphylococcus aureus, Staphylococcus epidermidis, Pseudomonas aeruginosa, and Escherichia coli. For chronic exit site infections, a combination of synergistic antibiotics is preferred to avoid the development of resistance. Response may be slow, appearances may change only gradually and deroofing of the tunnel with exteriorization or shaving of the cuff may be required. A variety of topical agents are used to clean the exit site according to custom and practice and these include sodium hypochlorite, povidone iodine, chlorhexidine, non-antibacterial, and antibacterial soap; however, care should be taken not to use agents that are potentially damaging to the skin. International variation in the use of such agents is reported from the international peritoneal dialysis outcomes and practice patterns study (PDOPPS) [23]. A tunnel infection may present as exit site discharge, erythema, edema, or tenderness over the subcutaneous pathway but is often clinically occult. Staphylococcus aureus and Pseudomonas aeruginosa exit site infections are very often associated with concomitant tunnel infections and are the organisms that most often result in catheter infection-related peritonitis; aggressive management is always indicated for these organisms. Ultrasound examination of the dacron cuffs and tunnel can assist in diagnosis and aid in making decision on removal of catheter. Catheter removal is required in non-responsive tunnel infections. Presence of fluid around the dacron cuffs is associated with a tunnel infection and consideration should be given to removal of the catheter.
Exit site infection, unresponsive to antibiotics, can be treated with exteriorization of the catheter, shaving of the superficial cuff, splicing of the catheter, or relocation of the exit to a distant site using extended catheter (presternal or upper abdominal).
5 Peritoneal Access-Related Problems
An adequately functioning PD catheter (PDC) is essential for successful PD and when the catheter does not work sufficiently this can prevent patients from receiving their chosen therapy and increase costs for health care systems. The UK Renal Registry reported considerable variation in 1 year catheter failure for 2015 with rates varying between 0 and 40% with the median being 13% [7]. Although it might appear that PDC are frequently causing problems and requiring replacement or repositioning it is relevant to note that vascular access causes at least as much of a problem for patients on HD [24]. PDC problems contribute significantly to early peritoneal TF [25] and therefore regular audit of primary catheter function and associated mechanical complications is essential to ensure that high standards are maintained. Systematic review has not demonstrated differences in outcome for PD catheters placed using the percutaneous, surgical method or laparoscopic methods [26,27,28] but does report advantage for the advanced laparoscopic technique that includes rectus sheath tunnelling and adjunctive procedures compared with basic laparoscopy with the caveat that only cohort studies were available for the analysis [29]. The medical Seldinger technique performed under local anesthetic has the advantage of being able to be performed by a nephrologist or specialist nurse, giving the control of catheter placement to the medical team, but it is not suitable for patients who have had previous lower abdominal surgery or in the obese. On the other hand, advanced laparoscopic techniques ensure that the catheter is placed in the pelvis and that necessary adjunctive interventions are performed. Whichever method is used, it is important that there is a team-based approach, that the service is responsive and that there is good availability of surgical support when required.
6 Common Catheter-Related Complications
The main complication of PDC is dysfunction. Since a PD catheter requires a flow of up to 300 ml/min it is necessary that the side holes are not obstructed and that the tip is well placed in the sump of the pelvis where the residual dialysate will be retained. If it is not appropriately placed this will result in a large residual volume reducing effective clearance and ultrafiltration, while increasing intra-abdominal pressure and associated complications. APD is more demanding on catheter function than CAPD and poor flows result in drainage alarms on the machine. This can be managed to some extent by the use of a tidal prescription (where a small amount of fluid is left in situ at the end of a dwell), however, if there are problems with clearance or ultrafiltration the catheter may need to be repositioned or replaced. Good early catheter function is essential if PD is to be used as treatment for patients presenting late with advanced uremia requiring dialysis.
Catheter dysfunction has several common causes including migration, which can be diagnosed by a plain abdominal film (◘ Fig. 84.4), as well as fecal loading which is commonly cited and often treated with beneficial results. Adequate bowel preparation is an essential part of the catheter insertion protocol. An uncommon cause of catheter dysfunction is the omental wrap which can be diagnosed and treated by laparoscopy. Catheter obstruction may result from fibrin or blood clots which can be resolved by the use of a urokinase lock into the catheter. Of course, catheter dysfunction is not easy to define, being described in practice more by the impact on the patient or nursing staff rather than objective measurements of flow.
Patients may complain of pain on inflow or drainage of PD fluid, which may be due to a local irritant effect of the dialysis fluid, a consequence of negative pressure (suction) particularly in APD or a mechanical consequence of tube position. Tidal APD is commonly used to reduce drainage pain, combined with avoiding a “dry day” by leaving a residual volume of approximately 200 ml in the peritoneal cavity. The use of more biocompatible neutral pH dialysates may ameliorate inflow pain possibly due to less chemical irritation of the membrane resulting in reduced stimulation of nociceptors. The position of the tube in the pelvis can lead to mechanical irritation which may be resolved by tube repositioning. Unfortunately, it is challenging to prove this etiology and some patients may be discouraged from persisting with PD.
7 Audit Standards for Catheter Placement
The minimization of catheter-related complications requires care and attention from the operator in the context of a consistent team-based approach supported by clear guidelines and protocols [30]. These describe the conditions necessary for optimal catheter function with minimization of complications. The only registry that reports primary catheter function is the French Speaking Registry, and this gives really excellent catheter function data [11]. However, in reality, many centers describe results that are considerably lower. The ISPD audit standards for catheter placement include a 1-year catheter survival of at least 80% and peritonitis within 30 days of catheter insertion of less than 5% [30] and this is audited by the UK Renal Registry [7]. There is an advantage in using an earlier time-point such as 3 months post catheter insertion as an audit measure since it provides more proximate data for clinical teams to use in their quality assurance.
8 Surgical Complications of PD
The surgical complications related to the insertion of the PD catheter can lead to morbidity, seriously compromise outcomes and result in loss of confidence for patients. Early complications include hemorrhage, perforated viscus, wound infection, catheter obstruction and displacement, and dialysate leak. Later complications include external cuff extrusion, dialysate leaks, hernias, erosion of abdominal organs, hemoperitoneum, and chylous effluent. Independent of the insertion technique, the operator must be able to recognize and manage the complications promptly and effectively. Preoperative evaluation and identification of potential risk factors are essential to prevent them [31].
9 Hemorrhage
Intraperitoneal hemorrhage may arise from trauma to the omental or mesenteric vessels, particularly during closed or blind insertion. This usually presents with blood staining of the effluent, which may be heavy. Slight bleeding may be treated expectantly; however, heavy bleeding, particularly in association with hypotension, will require return to theater for localization of the source of the bleeding and hemostasis. Extraperitoneal bleeding may be obvious from the wound edge (main wound or exit site) or an enlarging wound hematoma. Skin edge bleeding can be dealt with using either additional sutures or local injection with a local anesthetic solution containing adrenaline. Failure to evacuate a hematoma predisposes to delayed wound healing, dehiscence and infection with potential risk of tunnel infection and peritonitis.
10 Hematoperitoneum
Hemoperitoneum can appear dramatic, but generally settles spontaneously without the patient suffering harm. There is a long list of possible causes, summarized in an excellent review article [32]. There are rare occasions when it can signify a significant intraperitoneal hemorrhage, for example, following the rupture of a splenic artery aneurysm, although most commonly the cause is a bleed from a peritoneal capillary or due to either ovulation or retroperitoneal menstruation in women. In one series, the incidence of hemoperitoneum was 6%. Seventy percent of these did not require any active intervention apart from addition of heparin to the dialysate, with 20% requiring active intervention for significant hemorrhage and the remaining 10% having significant intra-abdominal pathology but minor hematoperitoneum [33]. Blood transfusion may be required with severe bleeding due to follicular or ovarian cyst rupture or coagulopathies.
11 Perforation or Laceration
Perforation of bowel and urinary bladder is a well-recognized but rare complication of closed PDC insertion, and it can also occur with open insertion. Injuries to liver, a polycystic kidney, aorta, mesenteric artery, and hernial sac have all been reported. Predisposing factors include abdominal adhesions and distensions due to paralytic ileus or bowel obstruction, and unconscious, cachectic, or heavily sedated patients. The bladder is at risk of injury if it is of high volume, for example in patients with chronic bladder outflow obstruction, and this can be avoided by preoperative voiding confirmed by ultrasound examination. Evidence of peritonitis associated with contaminated effluent is an indication for laparotomy and repair of the perforation. Delayed perforation of intestine, bladder, and vagina caused by pressure necrosis and erosion from an unused catheter has been described.
12 Wound Infection
Although unusual , this is a serious complication, which may lead to catheter loss. Usual organisms are Staphylococcus aureus and Pseudomonas species. Contamination of the wound should be prevented by strict adherence to aseptic technique, prophylactic antibiotics, and meticulous hemostasis. Treatment of established infection requires antibiotics, surgical drainage, and possibly catheter removal for intractable infection involving the catheter. ESI or peritonitis directly as a consequence of catheter placement should be a rare event. Treatment of catheter associated infections is summarized in the relevant ISPD guideline [21].
13 Hernias
It is estimated that between 10 and 20% of the CAPD population develop hernias due to raised intra-abdominal pressure associated with PD, which can be inguinal, umbilical and pericatheter in location. Part of the preoperative assessment of the prospective PD patient is to assess for the presence of hernias since these can be repaired at the time of catheter placement. However, often these are not present at the time of catheter insertion and develop later, more commonly in patients who use larger intraperitoneal volumes and in those with adult polycystic kidney disease.
Elective hernia repair should be undertaken if possible and if the peritoneum remains intact and the hernia repair is not extensive, disruption of PD is not required. A small volume and short cycle dwell regimen can be continued postoperatively. However, where the peritoneum is breeched during hernia repair, change to hemodialysis for at least 3 weeks to allow healing of the peritoneum is required since leakage of dialysis fluid through the hernia wound encourages infection of mesh used to reinforce the repair. Pericatheter hernias, which usually occur in the midline, are difficult to manage without removing the catheter. Any attempt to repair a pericatheter hernia leaving the catheter intact will either compromise the hernia repair or the catheter function. Meticulous attention to the technique in placement of the catheter will usually prevent such hernias from developing. Paramedian placement of the PDC reduces the incidence of pericatheter hernias.
14 Leaks
A dialysate leak can occur months or even years after starting PD in up to 25% of catheters placed through the mid-line, but is less common with a paramedian incision and has been reported in 7.4% of cases following a laparoscopic PD catheter insertion [34]. Clinically, leakage presents as clear dialysis fluid around the catheter at its exit site or as a localized swelling and edema of the abdominal wall due to infiltration with fluid (peaud’orange). The passage of dialysis fluid through a patent processus vaginalis may lead to gross scrotal and penile oedema in the male and labial oedema in the female. Occasionally, the oedema may be so marked that it is not possible to decide the side of origin of the leak. Hydrothorax, in a patient on PD, can result from leak of fluid through a congenital pleura-peritoneal communication or an acquired diaphragmatic hernia, which presents with chest pain and dyspnea. It is important to note that this complication may be silent; therefore, to exclude this, careful chest examination including percussion should be performed routinely in patients who are new to PD. If an effusion is found, the diagnosis is suggested by biochemical characteristics of aspirated fluid including a relatively high glucose (dialysate /serum ratio), low protein or LDH concentration in the pleural fluid and confirmed by an ultrasound, CT (◘ Fig. 84.5), or an MR scan. An isotope scan (peritoneo-scrotogram or pleural scintigraphy) will delineate the side of the leak (◘ Fig. 84.6a and b) which if negative allows the therapy to be continued while other causes are pursued.
Securing the PD catheter tightly at the deep cuff level or rectus sheath tunnelling reduces the risk of early leak and is recommended if there are plans to use the catheter early [35]. Early leaks can be managed by temporary discontinuation of PD, however, catheter replacement may be required. In a leak through patent processus vaginalis, PD should be discontinued until the oedema has subsided and then repair should be undertaken as for an inguinal hernia. If possible, the patient should be temporarily converted to hemodialysis for about 2 weeks following repair. Several approaches have been used to treat pleural leaks, although often the patient will require transfer to hemodialysis.
15 External Cuff Extrusion
Location of the subcutaneous cuff close to the exit site may lead to its protrusion, which can result either if the catheter becomes inadvertently pulled or may occur spontaneously due to its shape memory that tends to straighten the catheter. This complication can be avoided by placing the external cuff approximately 2–3 cm deep to the skin. If the subcutaneous cuff of the catheter begins to extrude, it may result in a persistent exit site infection. In the absence of signs of tunnel or deep cuff infection, removal of the subcutaneous cuff (shaving) allows the exit site infection to resolve in 50% of the cases unresponsive to antibiotic treatment. Failure of the infection to resolve mandates removal of the catheter.
16 Chylous Effluent
Chylous ascites , as defined by the presence of chylomicrons causing cloudiness of the effluent, is a rare entity which can occur with either no identifiable cause or in association with intra-abdominal malignancies (lymphoma and ovarian carcinoma), cirrhosis of liver, chronic pancreatitis, amyloidosis, cardiac failure, and patients on calcium channel blockers. In cases with no obvious cause, microtrauma to the peritoneal lymphatics is presumed to be the etiology, where improvement has been reported with cessation of PD, administration of medium chain triglycerides and octreotide. Continued loss of lymph (lymphocytes and fat) leads to malnutrition and immunosuppression, which may necessitate discontinuation of PD.
17 Indications for Catheter Removal
Catheter removal maybe required for malfunction which can result from intraluminal obstruction with blood or fibrin clots, omental tissue incarceration, catheter tip migration out of the pelvis with poor drainage, a catheter kink, catheter tip caught in an adhesion following severe peritonitis, or an accidental break. Indications for removal of a functioning catheter include severe, unresponsive or recurrent peritonitis, peritonitis due to exit site and/ or tunnel infection, persistent exit site infection, tunnel infection with abscess, late recurrent dialysate leak, atypical peritonitis, bowel perforation, severe abdominal pain due to the catheter impinging on internal organs, and catheter cuff extrusion with infection.
18 Metabolic Complications of Peritoneal Dialysis
The majority of PD exchanges rely on hypertonic glucose solutions to provide osmotic clearance of water in combination with a buffer for acid base correction. Perhaps, unsurprisingly, this process can lead to metabolic complications that can have either systemic or local effects on the peritoneal membrane. Components of PD fluid other than glucose can also have metabolic consequences and these will be considered. The potential for PD to cause adverse effects resulting in morbidity and mortality underlines the need to prescribe and manage PD responsibly. Research is a priority to identify mechanisms to ameliorate these complications.
19 Systemic Metabolic Complications of Peritoneal Dialysis
The use of glucose as the osmotic agent in PD leads to the absorption of approximately 800 g of glucose per week. In healthy people an excess of glucose will be utilized and stored as glycogen or later as lipids. It is therefore reasonable to propose that PD patients may manage excess glucose in this manner resulting in an increase in fat mass or body weight. However, the relationship between glucose exposure, fat mass, and body weight is not consistent suggesting that many factors influence metabolism in this group of patients.
Dialysis has the potential to impact on appetite in several ways. Leptin, the product of the Ob gene, is secreted by fat cells and regulates food intake and energy expenditure in animal models. Whether the hyperleptinemia observed in uremic patients is involved in the anorexia that is often identified in this group is unclear. Studies have observed that in PD patients, particularly those with diabetes, leptin levels and body fat content increase. In those who lost lean body mass, higher leptin and initial CRP levels were recorded [36]. It is of interest that insulin has been identified as a regulator of leptin gene expression. With chronic hyperinsulinemia, leptin levels can increase significantly.
The impact of glucose-based PD on the glucose-insulin system has been investigated [37]. Galach et al. studied 3.86% glucose dwells lasting 6 hours in 13 nondiabetic patients who were clinically stable and fasting. Significant increases in plasma glucose and insulin were identified. Insulin resistance was noted in the majority of patients although they were, in general, able to control the glucose peaks related to PD. Disruption of the glucose insulin axis is one factor defining the metabolic syndrome. Other elements include hypertension, raised BMI, depressed high density lipoprotein levels, and raised triglycerides. Metabolic syndrome had been identified in approximately 50% of PD patients and is recognized as a risk factor for cardiovascular death [38]. The management of metabolic syndrome in PD patients is challenging as it can at least in part be attributed to the effects of exposure to hypertonic glucose dialysis solutions. Advice includes increased exercise to limit the effect of absorbed glucose and consequent fat deposition, often difficult to follow for patients with comorbid conditions. Pharmaceutical management of dyslipidemia is advisable as is BP control through appropriate salt water balance and use of hypotensive agents. Techniques to limit glucose exposure in peritoneal dialysis include the appropriate scheduling of exchanges, the use of non-glucose based fluids and optimization of residual renal function. As yet there are no controlled trials to guide the management of this complex metabolic problem; however, recommendations are made in the relevant ISPD guideline [39].
20 Long-Term Changes to the Peritoneal Membrane: Impact on Ultrafiltration Capacity and Patient Outcome
The Cardiff peritoneal biopsy registry explored the relationship between peritoneal structural changes and membrane functional in patients on PD [40]. Most prominently was the development of submesothelial fibrosis which increased significantly with the duration of PD, for example, 180 μm (micron) in those 0 to 24 months and up to 700 μm in those on PD for 97 months. Vascular abnormalities were also a prominent finding with degrees of vessel wall thickening and capillary dilation which was graded from 1 to 4 according to the degree of subendothelial hyaline material, luminal distortion or obliteration. The findings suggested a causal relationship between the vasculopathy and the membrane thickening implying that vasculopathy may result in relative ischemia exacerbating the fibrosis.
From the clinical perspective, long-term changes to the peritoneal membrane are demonstrated by a time-dependent increase in solute transfer associated with a decline in ultrafiltration capacity (the amount of water moving across the membrane in response to a particular glucose concentration over a defined time) occurring after about 4 years of treatment. In a study of 210 consecutive patients commencing PD, peritoneal kinetics stabilized in the first 6 months of treatment but thereafter there was a time dependent increase in solute transport which became significant at 42 months. In that study, high solute transport (measured using the peritoneal equilibration testFootnote 1) and earlier loss of residual renal function were associated with poor outcome in patients on CAPD [41]. The patients with increasing solute transport had earlier loss in residual renal function and had been exposed to significantly more hypertonic glucose during the first 2 years of treatment that preceded the increase in solute transport. This was associated with greater achieved UF compensating for reduced residual renal function. This finding was confirmed in a 2003 report in which early and higher dialysate glucose exposure, which was in the context of higher comorbidity and lower residual renal function, was associated with a more rapid deterioration in membrane function [42]. Thus, the changes in the structural-functional relationship of the membrane could be predicted to some extent by clinical factors present within the first year. Patients with PD technique survival beyond 5 years were more likely to have preserved residual renal function, maintained nutrition, and medium small solute transport characteristics [43]. The coupling between the increase in D/P creatinine and the reduction in UF is due to the earlier loss of the osmotic gradient leading to reduced aquaporin mediated water transport and increased water reabsorption. Importantly, a group of patients develop a disproportionate fall in UF with time on PD due to a marked loss of UF capacity which may be an important marker of significant membrane damage. This has been confirmed in studies that examined changes in the sodium “dip” which is the dialysate to plasma sodium ratio after a 1-hour dwell using a hypertonic solution. Loss of this sodium dip is a marker of a reduction in water movement through water only pores and is likely to be a marker of peritoneal fibrosis, correlating with the subsequent development of EPS [44]. Icodextrin and automated peritoneal dialysis can be used to improve volume status in patients with higher transport status who have insufficient urine volume and there is evidence from various reports of the benefits of this approach, in particular a meta-analysis suggesting that the adverse effect of the high transport status on outcome has been mitigated in recent years [45].
With time on, PD patients are often prescribed increasing glucose loads. The chicken and egg question has been whether increased glucose load results in changes to the membrane leading to impaired ultrafiltration or whether impaired ultrafiltration related to membrane changes comes first causing physicians to increase the glucose concentrations in the patients’ prescription. A retrospective analysis of prospectively gathered data from PD patients by Davies et al. [46] provided supporting evidence that the primary event is the exposure of the peritoneal membrane to hypertonic glucose which in turn contributes to changes in membrane function. A cohort of patients who had performed continuous PD for 5 years were identified and divided into those who had stable membrane function and those with increasing membrane transport characteristics. When these two groups were compared the patients with increasing membrane transport were noted to have experienced earlier loss of residual renal function and were exposed to higher glucose loads to compensate for this in advance of the recorded changes in membrane characteristics.
Concern has persisted regarding cytotoxic components of the dialysis fluid. Using in vitro techniques including cell growth inhibition and assessment of advanced glycosylation end-products (AGEs) formation, Wieslander and colleagues demonstrated that the low pH of glucose dialysates causes significant cytotoxicity, with glucose degradation products (GDP) and to a lesser extent osmolality and the presence of lactate also causing damage [47]. GDP are formed by the exposure of the dialysate glucose to heat during sterilization. The condensation of a carbonyl group on these sugars with a reactive amino group of a protein produces AGEs. In vivo studies have confirmed that the interaction of the AGE with the receptor (RAGE) leads to damage of the peritoneum in humans. Uremic patients’ peritoneum already shows changes of fibrosis, angiogenesis, and RAGE activation. Those patients exposed to peritoneal dialysis with glucose-based fluids demonstrated further increase in these parameters. The AGE molecules have a physical effect on the structure of the membrane causing disruption to the matrix of the membrane as well as a functional effect. The AGE / RAGE interaction triggers cellular signal pathways involved in inflammation and fibrosis.
The observed long-term changes in the integrity of the peritoneal membrane have led to the development of dialysis solutions that are intended to be more “biocompatible” utilizing a neutral pH, and lower concentrations of glucose degradation products and in some cases bicarbonate as a buffer. This development requires more complex (and consequently expensive) technology, including the use of twin chamber bags to separate the buffer from the electrolyte components until mixing just prior to use, and to allow the glucose to be heat sterilized at a lower pH than conventionally which reduces the formation of GDPs. Several studies have tested these more biocompatible solutions by examining their impact on biomarkers of peritoneal membrane integrity or inflammation, and on clinical aspects including UF, residual renal function, and solute transport [48]. The BalANZ study is the largest randomized controlled trial of biocompatible peritoneal dialysate vs. standard dialysate to date [49] recruiting 185 incident peritoneal dialysis patients to this 2-year study. Patients were randomized 1:1 to receive either a neutral pH, lactate buffered, low GDP Balance solution (Fresenius Medical Care, Bad Homburg, Germany) or a conventional, standard, lactate-buffered PD solution. The primary outcome measure was the difference in the slope of the decline in residual renal function and this was not met. However, there was a significant difference between the groups, both in time to anuria (p = 0.009) and time to first peritonitis episode (p = 0.01) in favor of the more biocompatible solution. Indeed, the peritonitis rate in the biocompatible group was 0.30 vs. 0.49 (p = 0.01) episodes per year. In addition, there was a significant reduction in overall infection in the biocompatible group (4 non-PD infections out of 91 patients vs. 20 out of 91 in the control group). Thus, the biocompatible group demonstrated meaningful benefits in terms of infection and time to anuria compared with the control solution. Systematic review has confirmed that the use of biocompatible solutions is associated with better preservation of residual renal function [50].
21 Encapsulating Peritoneal Sclerosis
Encapsulating peritoneal sclerosis (EPS) is a rare but potentially devastating complication of peritoneal dialysis (PD). Diagnostic criteria have been published by the ISPD and are based on a combination of clinical features (such as the presence of inflammation, disturbance of gastrointestinal function) supported by confirmatory imaging (◘ Fig. 84.7) or laparotomy [51]. Onset is often insidious, presenting with nonspecific features of inflammation, weight loss and abdominal discomfort. Patient experience attests to often delayed diagnosis and a sense of “not being heard” by the medical team [52]. In full-blown form it causes failure of the gastrointestinal tract and death. Its sporadic nature, the difficulty in early diagnosis, as well as the lack of suitable animal models, means that at present the understanding of risk factors is incomplete and evidence-based therapies are lacking. In some patients EPS seems to be a self-limiting condition that can be managed with appropriate nutritional support; whereas in others, the progression is rapid with the development of obstructive features and in these cases there is growing evidence that timely surgical intervention can be successful.
The Scottish Renal Registry reviewed all cases of encapsulating peritoneal sclerosis (EPS) [53] identified in Scotland from January 1, 2000, until December 31, 2007, and found an overall rate of 1.5%, however, the incidence increased with time on PD, reaching 8.1% (95% confidence interval: 3.6–17.6%) for those with 4 to 5 years exposure to the therapy. The Scottish data gave a similar prevalence of EPS to other key papers published since the Millennium of approximately 2–3% [54, 55], generally higher than that reported in earlier papers.
In the Scottish study, at diagnosis, 26% were on PD, whereas 63% were diagnosed within 1 year and 72% within 2 years of stopping PD; in 50% of the cases, patients had received a renal transplant before the diagnosis of EPS. Patients were likely to have discontinued PD because of ultrafiltration failure or inadequate dialysis and 65% of the cohort had used high-strength dextrose (3.86%) and 98% had used icodextrin, whereas no patients had used “bio-compatible” dialysis fluids exclusively. The cumulative risk is modest at 2.6% by 5 years, reflecting the reality that few patients continue PD beyond 4 years (◘ Fig. 84.8), and thus in a sense EPS is a condition of survivors damaging the otherwise good prognosis in this younger group of patients. A recent analysis has demonstrated that EPS risk estimates are lower when calculated using competing risk of death analyses [56]. The mortality rate was 42% within 1 year of diagnosis, with the median survival from diagnosis being 180 days (range 1 to 1075).
Risk of encapsulating peritoneal sclerosis calculated using ‘standard’ and competing risks approaches (from Ref. [56])
Several cohort studies since the millennium [57,58,59,60,61] suggested either an increased disease frequency or at least an improved rate of diagnosis of PD-associated EPS, however more recently the Dutch EPS Registry reports a decline in incidence from 0.85% in 2009 to 0.14% in 2014 [8]. The reason for these changes is likely to be multifactorial and represents the influence of altered clinical management on a range of risk factors that are considered to be clinically relevant. These are reviewed in the latest ISPD guideline on this topic [9], and include PD exposure (time on PD), dialysate glucose concentrations and the possibility that icodextrin has a role as well as an association with discontinuing PD , and possibly renal transplantation. Good quality information on treatment for EPS is lacking and is based on case series reports; including nutritional optimization, the use of immunosuppressant agents, tamoxifen, and specialist surgery if clinical features fail to resolve with focused nutritional and medical treatment. The surgical method combines enterolysis with excision of the diseased peritoneum and cocooning membrane and should be performed at dedicated national centers [62]. Major outstanding questions remain around risk factors, diagnosis and treatment and large prospective studies are required.
Chapter Review Questions
-
1.
What factors influence the decision around the most appropriate catheter insertion technique?
-
2.
A patient on peritoneal dialysis is being treated with intraperitoneal antibiotics for an episode of peritonitis – what other treatment should be considered?
-
3.
A patient who has previously been well on peritoneal dialysis starts to develop oedema and weight gain – what is the most likely explanation?
-
4.
A patient on automated peritoneal dialysis who has lost residual renal function has become under dialysed. What is the first step?
-
5.
You are tasked to develop quality improvement systems for your PD unit. What should you focus on?
Answers
-
1.
Randomised controlled trials do not show advantage for one technique over another, although cohort studies suggest advantages for the laparoscopic insertion combined with advanced techniques. It is important that the catheter insertion pathway is responsive to need and is individualised. In other words for individuals within the normal body mass ranges who have not had previous lower abdominal surgery a percutaneous insertion under local anaesthetic by an expert operator is a good option – whereas in more complex cases surgical approaches will be necessary.
-
2.
It is important to prescribe antifungal therapy for the duration of the antibiotics to reduce the risk of subsequent fungal peritonitis. This can either take the form of oral nystatin or fluconazole.
-
3.
It is likely that the residual renal function has fallen. This can be measured using a 24 hour urine collection. If the patient is still passing urine one step that can be taken is to increase oral diuretic doses up to 240 mg of furosemide in divided doses (morning and lunch). A second step is to ensure that fluid is not being absorbed from any of the dialysis exchanges. The third step is to adjust the PD prescription to improve ultrafiltration.
-
4.
The easiest course of action is to add a day time exchange if they do not have one already. Subsequent to that, it may be necessary to increase the volume of the overnight exchanges. This is guided by the patient’s small solute transport status.
-
5.
The two key areas to focus on are access and infection. You should ensure that regular audit of peritonitis and exit site infection rates are being conducted and shared with the team with a focus on root cause analysis to under stand the causes of individual cases. It is also important to audit the outcome of peritoneal dialysis catheter insertion. Important audit targets are 0.5 episodes of peritonitis per year for patient at risk (see ► ispd.org for guideline documents); for catheter patency the following guidance has been given – “Catheter patency at 12 months of > 95% for advanced laparoscopic placement and > 80% for all other catheter insertion methods”. There is a value in auditing at 3 months post insertion since 1 year is rather too long to wait.
Notes
- 1.
The peritoneal equilibration test measures the dialysate to plasma ratio of creatinine (D/P creatinine) at the end of a 4-hour dwell using a dialysate with a 2.27% glucose concentration.
References
Yeates K, Zhu N, Vonesh E, Trpeski L, Blake P, Fenton S. Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant. 2012;27(9):3568–75.
Korevaar JC, Feith GW, Dekker FW, van Manen JG, Boeschoten EW, Bossuyt PM, et al. Effect of starting with hemodialysis compared with peritoneal dialysis in patients new on dialysis treatment: a randomized controlled trial. Kidney Int. 2003;64(6):2222–8.
Nataatmadja M, Cho Y, Johnson DW. Continuous quality improvement initiatives to sustainably reduce peritoneal dialysis-related infections in Australia and New Zealand. Perit Dial Int. 2016;36(5):472–7.
Kolesnyk I, Dekker FW, Boeschoten EW, Krediet RT. Time-dependent reasons for peritoneal dialysis technique failure and mortality. Perit Dial Int. 2010;30(2):170–7.
Perl J, Davies SJ, Lambie M, Pisoni RL, McCullough K, Johnson DW, et al. The peritoneal dialysis outcomes and practice patterns study (PDOPPS): unifying efforts to inform practice and improve global outcomes in peritoneal dialysis. Perit Dial Int. 2016;36(3):297–307.
Williams VR, Quinn R, Callery S, Kiss A, Oliver MJ. The impact of treatment modality on infection-related hospitalization rates in peritoneal dialysis and hemodialysis patients. Perit Dial Int. 2011;31(4):440–9.
Hole B, Caskey F, Evans K, Fluck R, Kumwenda M, Steenkamp R, et al. UK renal registry 19th annual report: chapter 12 multisite dialysis access audit in England, Northern Ireland and Wales in 2015 and 2014 PD one year follow-up: national and Centre-specific analyses. Nephron. 2017;137(Suppl 1):269–96.
Betjes MG, Habib SM, Boeschoten EW, Hemke AC, Struijk DG, Westerhuis R, et al. Significant decreasing incidence of encapsulating peritoneal sclerosis in the dutch population of peritoneal dialysis patients. Perit Dial Int. 2017;37(2):230–4.
Brown EA, Bargman J, van Biesen W, Chang MY, Finkelstein FO, Hurst H, et al. Length of time on peritoneal dialysis and encapsulating peritoneal sclerosis - position paper for ISPD: 2017 update. Perit Dial Int. 2017;37(4):362–74.
Figueiredo AE, Bernardini J, Bowes E, Hiramatsu M, Price V, Su C, et al. A syllabus for teaching peritoneal dialysis to patients and caregivers. Perit Dial Int. 2016;36(6):592–605.
Verger C, Ryckelynck JP, Duman M, Veniez G, Lobbedez T, Boulanger E, et al. French peritoneal dialysis registry (RDPLF): outline and main results. Kidney Int Suppl. 2006;103:S12–20.
Li PK, Szeto CC, Piraino B, de Arteaga J, Fan S, Figueiredo AE, et al. ISPD peritonitis recommendations: 2016 update on prevention and treatment. Perit Dial Int. 2016;36(5):481–508.
Crabtree JH, Shrestha BM, Chow KM, Figueiredo AE, Povlsen JV, Wilkie M, et al. Creating and maintaining optimal peritoneal dialysis access in the adult patient: 2019 update. Perit Dial Int. 2019;39(5):414–36.
Xu G, Tu W, Xu C. Mupirocin for preventing exit-site infection and peritonitis in patients undergoing peritoneal dialysis. Nephrol Dial Transplant. 2010;25(2):587–92.
Shrestha BM, Brown P, Wilkie M. Surgical peritonitis in patients on peritoneal dialysis. Perit Dial Int. 2008;28(4):331–4.
Moraes TP, Pecoits-Filho R, Ribeiro SC, Rigo M, Silva MM, Teixeira PS, et al. Peritoneal dialysis in Brazil: twenty-five years of experience in a single center. Perit Dial Int. 2009;29(5):492–8.
Van Biesen W, Veys N, Vanholder R, Lameire N. Peritoneal-dialysis-related peritonitis: the art of rope-dancing. Nephrol Dial Transplant. 2002;17(11):1878–82.
Toleman MA. The future of peritoneal dialysis in a moving landscape of bacterial resistance. Perit Dial Int. 2017;37(2):134–40.
Ballinger AE, Palmer SC, Wiggins KJ, Craig JC, Johnson DW, Cross NB, et al. Treatment for peritoneal dialysis-associated peritonitis. Cochrane Database Syst Rev. 2014;4:CD005284.
Bailie GR, Eisele G. Pharmacokinetic issues in the treatment of continuous ambulatory peritoneal dialysis-associated peritonitis. J Antimicrob Chemother. 1995;35(5):563–7.
Szeto CC, Li PK, Johnson DW, Bernardini J, Dong J, Figueiredo AE, et al. ISPD catheter-related infection recommendations: 2017 update. Perit Dial Int. 2017;37(2):141–54.
Schaefer F, Klaus G, Muller-Wiefel DE, Mehls O. Intermittent versus continuous intraperitoneal glycopeptide/ceftazidime treatment in children with peritoneal dialysis-associated peritonitis. The Mid-European Pediatric Peritoneal Dialysis Study Group (MEPPS). J Am Soc Nephrol. 1999;10(1):136–45.
Boudville N, Johnson DW, Zhao J, Bieber BA, Pisoni RL, Piraino B, et al. Regional variation in the treatment and prevention of peritoneal dialysis-related infections in the Peritoneal Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant. 2019;34(12):2118–26.
Oliver MJ, Verrelli M, Zacharias JM, Blake PG, Garg AX, Johnson JF, et al. Choosing peritoneal dialysis reduces the risk of invasive access interventions. Nephrol Dial Transplant. 2012;27(2):810–6.
See EJ, Johnson DW, Hawley CM, Pascoe EM, Badve SV, Boudville N, et al. Risk predictors and causes of technique failure within the first year of peritoneal dialysis: an Australia and New Zealand dialysis and transplant registry (ANZDATA) study. Am J Kidney Dis. 2018;72(2):188–97.
Boujelbane L, Fu N, Chapla K, Melnick D, Redfield RR, Waheed S, et al. Percutaneous versus surgical insertion of PD catheters in dialysis patients: a meta-analysis. J Vasc Access. 2015;16(6):498–505.
Tullavardhana T, Akranurakkul P, Ungkitphaiboon W, Songtish D. Surgical versus percutaneous techniques for peritoneal dialysis catheter placement: a meta-analysis of the outcomes. Ann Med Surg (Lond). 2016;10:11–8.
Xie H, Zhang W, Cheng J, He Q. Laparoscopic versus open catheter placement in peritoneal dialysis patients: a systematic review and meta-analysis. BMC Nephrol. 2012;13:69.
Shrestha BM, Shrestha D, Kumar A, Shrestha A, Boyes SA, Wilkie ME. Advanced laparoscopic peritoneal dialysis catheter insertion: systematic review and meta-analysis. Perit Dial Int. 2018;38(3):163–71.
Crabtree J, Shrestha B, Chow KM, Figueiredo A, Povlsen J, Wilkie M, Abdel-Aal A, Cullis B, Goh BL, Briggs V, Brown E, Dor F. Creating and maintaining optimal peritoneal dialysis access in the adult patient: 2019 update. Perit Dial Int. 2019 - in press Peritoneal Dialysis International.
Campos RP, Chula DC, Riella MC. Complications of the peritoneal access and their management. Contrib Nephrol. 2009;163:183–97.
Lew SQ. Hemoperitoneum: bloody peritoneal dialysate in ESRD patients receiving peritoneal dialysis. Perit Dial Int. 2007;27(3):226–33.
Greenberg A, Bernardini J, Piraino BM, Johnston JR, Perlmutter JA. Hemoperitoneum complicating chronic peritoneal dialysis: single-center experience and literature review. Am J Kidney Dis. 1992;19(3):252–6.
Keshvari A, Najafi I, Jafari-Javid M, Yunesian M, Chaman R, Taromlou MN. Laparoscopic peritoneal dialysis catheter implantation using a Tenckhoff trocar under local anesthesia with nitrous oxide gas insufflation. Am J Surg. 2009;197(1):8–13.
Sharma AP, Mandhani A, Daniel SP, Filler G. Shorter break-in period is a viable option with tighter PD catheter securing during the insertion. Nephrology (Carlton). 2008;13(8):672–6.
Stenvinkel P, Lindholm B, Lonnqvist F, Katzarski K, Heimburger O. Increases in serum leptin levels during peritoneal dialysis are associated with inflammation and a decrease in lean body mass. J Am Soc Nephrol. 2000;11(7):1303–9.
Galach M, Waniewski J, Axelsson J, Heimburger O, Werynski A, Lindholm B. Mathematical modeling of the glucose-insulin system during peritoneal dialysis with glucose-based fluids. ASAIO J. 2011;57(1):41–7.
Park JT, Chang TI, Kim DK, Lee JE, Choi HY, Kim HW, et al. Metabolic syndrome predicts mortality in non-diabetic patients on continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant. 2010;25(2):599–604.
Wang AY, Brimble KS, Brunier G, Holt SG, Jha V, Johnson DW, et al. ISPD cardiovascular and metabolic guidelines in adult peritoneal dialysis patients Part II – management of various cardiovascular complications. Perit Dial Int. 2015;35(4):388–96.
Williams JD, Craig KJ, Topley N, Von Ruhland C, Fallon M, Newman GR, et al. Morphologic changes in the peritoneal membrane of patients with renal disease. J Am Soc Nephrol. 2002;13(2):470–9.
Davies SJ, Phillips L, Russell GI. Peritoneal solute transport predicts survival on CAPD independently of residual renal function. Nephrol Dial Transplant. 1998;13(4):962–8.
Davies SJ. Longitudinal relationship between solute transport and ultrafiltration capacity in peritoneal dialysis patients. Kidney Int. 2004;66(6):2437–45.
Davies SJ, Phillips L, Griffiths AM, Russell LH, Naish PF, Russell GI. What really happens to people on long-term peritoneal dialysis? Kidney Int. 1998;54(6):2207–17.
Morelle J, Sow A, Hautem N, Bouzin C, Crott R, Devuyst O, et al. Interstitial fibrosis restricts osmotic water transport in encapsulating peritoneal sclerosis. J Am Soc Nephrol. 2015;26(10):2521–33.
Brimble KS, Walker M, Margetts PJ, Kundhal KK, Rabbat CG. Meta-analysis: peritoneal membrane transport, mortality, and technique failure in peritoneal dialysis. J Am Soc Nephrol. 2006;17(9):2591–8.
Davies SJ, Phillips L, Naish PF, Russell GI. Peritoneal glucose exposure and changes in membrane solute transport with time on peritoneal dialysis. J Am Soc Nephrol. 2001;12(5):1046–51.
Wieslander A, Linden T, Kjellstrand P. Glucose degradation products in peritoneal dialysis fluids: how they can be avoided. Perit Dial Int. 2001;21(Suppl 3):S119–24.
Pajek J, Kveder R, Bren A, Gucek A, Ihan A, Osredkar J, et al. Short-term effects of a new bicarbonate/lactate-buffered and conventional peritoneal dialysis fluid on peritoneal and systemic inflammation in CAPD patients: a randomized controlled study. Perit Dial Int. 2008;28(1):44–52.
Johnson DW, Brown FG, Clarke M, Boudville N, Elias TJ, Foo MWY, et al. Effects of biocompatible versus standard fluid on peritoneal dialysis outcomes. J Am Soc Nephrol. 2012;23(6):1097–107.
Seo EY, An SH, Cho JH, Suh HS, Park SH, Gwak H, et al. Effect of biocompatible peritoneal dialysis solution on residual renal function: a systematic review of randomized controlled trials. Perit Dial Int. 2014;34(7):724–31.
Kawaguchi Y, Kawanishi H, Mujais S, Topley N, Oreopoulos DG. Encapsulating peritoneal sclerosis: definition, etiology, diagnosis, and treatment. International Society for Peritoneal Dialysis Ad Hoc Committee on Ultrafiltration Management in Peritoneal Dialysis. Perit Dial Int. 2000;20(Suppl 4):S43–55.
Hurst H, Summers A, Beaver K, Caress AL. Living with encapsulating peritoneal sclerosis (EPS): the patient’s perspective. Perit Dial Int. 2014;34(7):758–65.
Brown MC, Simpson K, Kerssens JJ, Mactier RA. Encapsulating peritoneal sclerosis in the new millennium: a national cohort study. Clin J Am Soc Nephrol. 2009;4(7):1222–9.
Kawanishi H, Kawaguchi Y, Fukui H, Hara S, Imada A, Kubo H, et al. Encapsulating peritoneal sclerosis in Japan: a prospective, controlled, multicenter study. Am J Kidney Dis. 2004;44(4):729–37.
Summers AM, Clancy MJ, Syed F, Harwood N, Brenchley PE, Augustine T, et al. Single-center experience of encapsulating peritoneal sclerosis in patients on peritoneal dialysis for end-stage renal failure. Kidney Int. 2005;68(5):2381–8.
Lambie M, Teece L, Johnson DW, Petrie M, Mactier R, Solis-Trapala I, et al. Estimating risk of encapsulating peritoneal sclerosis accounting for the competing risk of death. Nephrol Dial Transplant. 2019;34(9):1585–91.
Korte MR, Sampimon DE, Lingsma HF, Fieren MW, Looman CW, Zietse R, et al. Risk factors associated with encapsulating peritoneal sclerosis in Dutch EPS study. Perit Dial Int. 2011;31(3):269–78.
Johnson DW, Cho Y, Livingston BE, Hawley CM, McDonald SP, Brown FG, et al. Encapsulating peritoneal sclerosis: incidence, predictors, and outcomes. Kidney Int. 2010;77(10):904–12.
Lambie ML, John B, Mushahar L, Huckvale C, Davies SJ. The peritoneal osmotic conductance is low well before the diagnosis of encapsulating peritoneal sclerosis is made. Kidney Int. 2010;78(6):611–8.
Gayomali C, Hussein U, Cameron SF, Protopapas Z, Finkelstein FO. Incidence of encapsulating peritoneal sclerosis: a single-center experience with long-term peritoneal dialysis in the United States. Perit Dial Int. 2011;31(3):279–86.
Balasubramaniam G, Brown EA, Davenport A, Cairns H, Cooper B, Fan SL, et al. The pan-Thames EPS study: treatment and outcomes of encapsulating peritoneal sclerosis. Nephrol Dial Transplant. 2009;24(10):3209–15.
Kawanishi H, Banshodani M, Yamashita M, Shintaku S. Surgical treatment for encapsulating peritoneal sclerosis: 24 years’ experience. Perit Dial Int. 2018;39(2):169–74.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Jenkins, S., Shrestha, B., Wilkie, M. (2022). Complications of Peritoneal Dialysis. In: Harber, M. (eds) Primer on Nephrology. Springer, Cham. https://doi.org/10.1007/978-3-030-76419-7_84
Download citation
DOI: https://doi.org/10.1007/978-3-030-76419-7_84
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76418-0
Online ISBN: 978-3-030-76419-7
eBook Packages: MedicineMedicine (R0)