Abstract
Background: Peritoneal dialysis (PD) technique failure remains a significant barrier to improving the outcomes for PD patients and increasing the uptake of PD worldwide. The Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS) has been developed to identify variations in clinical practices and potentially modifiable causes of technique failure with the objective to improve PD outcomes.
Methods: PDOPPS is a prospective cohort study initially involving seven different countries such as Australia, New Zealand, Canada, Japan, Thailand, the United Kingdom, and the United States. The primary outcome is all-cause PD technique failure, and the secondary outcomes include hospitalization rates, PD-related all-cause mortality, PD-related complications, cause-specific technique failure, and patient-reported outcomes.
Results: The PDOPPS clinical workgroups have collaborated to design, analyze, and publish several clinically relevant studies which focus on PD training and education, PD catheter access and function, infection prevention and management, patient support, dialysis prescription and fluid management, and clinical application of PD therapy. The common finding is of wide variations in clinical practice, not always aligned to international guidelines and differences in important outcomes known to impact technique failure.
Conclusion: The PDOPPS is an innovative, internationally collaborative research initiative which aims to advance the understanding in variations in PD practices and how these link to outcomes that are important to patients, with the overall goal of identifying optimal clinical practice, extending PD technique survival, and improving quality of life for PD patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Center effect
- Center size
- Cohort studies
- International cooperation
- Kidney failure
- Outcomes
- Peritoneal dialysis, Peritonitis
- Practice patterns
- Treatment failure
Introduction
Kidney failure is a leading contributor to the global public health burden with over 2.6 million people requiring kidney replacement therapy (KRT) or kidney transplantation [1]. Peritoneal dialysis (PD) is a form of KRT that is currently utilized by approximately 11% of maintenance dialysis patients worldwide [2] with an average of 20.8 people per million population (pmp) initiating PD each year treated by approximately 1.3 PD centers pmp [3]. PD is a cost-effective treatment [4, 5] which is associated with an initial survival advantage [6, 7] and offers patients a flexible, home-based therapy with increased treatment autonomy [8, 9]. Since the mid-1990s, there have been progressive improvements in patient survival on PD, which have outstripped those observed on HD [10, 11]. Over the same period, there have been concomitant improvements in PD technique survival, with progressively fewer patients transferring to hemodialysis [10]. However, technique survival varies widely both within and between countries, with 3-year rates ranging from 29% in Malaysia to 91% in China [2, 12]. This variation is not fully explained by casemix, suggesting that other factors, such as center practices, may play a role [13,14,15]. Technique failure has a major disruptive impact on the lives of patients and their caregivers, results in appreciable morbidity and mortality, and has been identified by clinicians and patients as a top research priority [16,17,18]. Technique failure also incurs considerable cost to healthcare systems, as evidenced by a Canadian study which showed that PD technique failure within the first 3 years resulted in a similar cost burden to patients treated with HD alone, thereby obviating the overall financial benefits that PD provides compared with HD [19]. As technique failure still remains one of the major factors limiting both the utility and utilization of PD as a therapy around the world [2, 12, 20,21,22], it is imperative that the factors underpinning technique failure are comprehensively identified and, where possible, mitigated.
This chapter will examine the importance of the problem of PD technique failure and provide an overview of the current status and early findings of the Peritoneal Dialysis Outcomes and Practice Patterns Study (PDOPPS), the prime objective of which is to identify modifiable practices associated with superior PD technique survival.
The Problem of Technique Failure
One of the key difficulties with technique failure is that there is significant variation in how it is defined in the published literature [23]. In particular, there is marked variation regarding when PD is considered to start and when it is considered to end. Although not often defined at all, some groups define PD to have started with the first exchange (e.g., the Registre de Dialyse Péritonéale de Langue Française), while others define it as the end of PD training (Brazilian PD study, BrazPD) [23]. A number of groups, such as USRDS, do not count PD at all unless patients were on that modality at 90 days following dialysis initiation, despite the fact that the first 90 days are a high-risk period for technique failure [24, 25]. Most studies also do not define how long a patient has to be off PD to qualify as a technique failure [23]. A recent Australia and New Zealand Dialysis and Transplant (ANZDATA) registry study explored a range of definitions used to describe PD technique failure and ultimately recommended that PD technique failure be standardly defined as a composite end point of transfer to hemodialysis for at least 30 days or death (either on PD or within 30 days of ceasing PD) [26]. They also recommended a secondary definition using a time window of 180 days, which provides additional information on the likelihood of return to PD [26]. Additional time windows, e.g., 60 days, may be reported. Having a standardized definition of technique failure is critical to benchmarking between centers and countries and to properly elucidating patient-level and center-level characteristics associated with technique failure.
The most commonly recognized patient-related risk factors for technique failure include younger age, higher body mass index, Indigenous race, lower socioeconomic status, and comorbidities (such as diabetes) [15, 27,28,29,30,31,32,33]. However, recent studies have demonstrated that center-level characteristics may play an even more significant role in PD technique failure variability [34]. Schaubel et al. collated data from the Canadian Organ Replacement Register and observed that a dialysis unit’s experience in treating PD patients had a significant impact on PD outcomes [35]. Overall, as the cumulative number of patients treated with PD increased and as the percentage of patients initiated on PD increased, mortality and technique failure rates both decreased [35]. Other registry-based studies completed in France, Netherlands, Brazil, Canada, and the United States have similarly shown a correlation between smaller PD center size and higher technique failure rates [35,36,37,38,39]. These findings were further distinguished in a systematic review by Pieper et al. which concluded that larger center volume was associated with an improved technique survival [40]. In an ANZDATA registry study of 9362 patients from 51 centers in Australia, Htay et al. observed sevenfold variation in technique failure across centers which was predominantly accounted for by modifiable, center-level factors (such as PD unit size and proportion of patients treated with PD) rather than patient characteristics [34]. Indeed, center variation in PD technique failure was reduced by 28% after adjusting for patient-specific factors and by a further 53% after adjusting for center-specific factors [34]. Similar findings were observed for rates [27] and outcomes [41] of peritonitis, which is the major cause of PD technique failure after death. These findings suggest the possibility that PD technique failure is strongly influenced by modifiable center characteristics relating to their practice and/or organization.
Another piece of evidence suggesting that PD technique failure is driven by modifiable center characteristics is the evidence that implementation of national quality initiatives has been associated with substantial improvements in technique survival rates. The best example of this is the Australian and New Zealand peritonitis continuous quality improvement (CQI) initiative, which involved generating better evidence to inform peritonitis guidelines, facilitating better translation of evidence and guidelines into clinical practice, and establishing CQI processes at local, state, and national levels through improved outcomes monitoring with quarterly audit and feedback, identification of barriers and enablers through implementation research, improved education targeting early career nephrologists, development of standardized peritonitis pathways, and incentivizing performance improvement [42]. These initiatives were quickly followed by a one-third reduction in peritonitis rates, a one-half reduction in between-center peritonitis rate variation, and a significant improvement in PD technique survival [42].
Due to the cumulative evidence that center-level characteristics are a significant driver for PD technique failure, a better understanding of the modifiable causes of PD technique failure is required. A limitation of the aforementioned studies is that they largely relied on information collected by registries, which lacked sufficient granularity of data (particularly in relation to center organization and practices) to comprehensively address this issue. With this in mind, PDOPPS was established as a global collaboration between the Arbor Research Collaborative for Health and the International Society for Peritoneal Dialysis (ISPD) to understand variation in PD practices and outcomes, identify optimal practices, and ultimately improve outcomes for patients treated with chronic PD [23].
PDOPPS: Design and Rationale
Rationale
Based on the findings of the aforementioned studies, the basic tenet of PDOPPS is that variable (and often poor) PD technique survival rates are driven by variable (and often poor) PD center practices, such that identifying those modifiable practices associated with superior PD outcomes (including PD peritonitis-free survival and technique survival) will help to better inform clinical practice and ultimately patient outcomes.
PDOPPS builds on the successful methodology established by Dialysis Outcomes and Practice Patterns Study (DOPPS), which was originally formed in 1996 to study in-center HD patients and practices [43]. The primary objective of DOPPS was to improve HD patients’ morbidity and mortality outcomes, inform policy changes, as well as influence patients’ health-related quality of life [43]. DOPPS has helped shape HD practices on a global scale and still remains a leading resource for the nephrology community worldwide with comprehensive data that have influenced clinical practice guidelines for HD [43,44,45,46,47,48,49]. DOPPS initially started with 308 HD units from 7 different countries [44] at initiation and then expanded to 21 countries, 580 facilities, and over 30,000 census patients by 2015 [50]. This large prospective cohort study has led to important practice policy changes such as the fistula first policy and strategies for improved management of anemia [51,52,53], mineral and bone disorders [54, 55], and quality of life among HD patients [56,57,58]. The program has now been expanded to include patients with chronic kidney disease (CKDopps) [59] and patients receiving peritoneal dialysis (PDOPPS) [23]. All three of these major projects share the common goal of identifying measurable differences in facility practices that will help inform strategies to improve patient outcomes.
Design
The PDOPPS is an international prospective cohort study of PD patients over the age of 18, which began recruitment in 2013. The primary outcome is all-cause PD technique failure, and the secondary outcomes include all-cause mortality, hospitalization rates, PD-related complications, patient-reported outcomes, and cause-specific technique failure [23]. The overall objective is to identify differences in clinical practice between centers to improve PD outcomes as well as to generate scientific hypotheses for the variations found in the study [23].
During the initial phase (Phase 1) that extended from 2013 to 2016, PDOPPS randomly selected at least 20 different PD centers with at least 20 prevalent PD patients from each of the 7 different countries (Australia, New Zealand, Canada, Japan, Thailand, the United Kingdom, the United States) (Fig. 28.1). At study initiation, all centers completed a census of their PD patients from which 20–30 prevalent patients were randomly selected independent of the dialysis unit’s size. A maximum of 25 incident patients (defined as patients initiating PD within 30 days of the PDOPPS census date and receiving at least one PD treatment at home or a nursing home) were also included. Patients continued to be followed up until kidney transplantation, transfer to a different dialysis unit, permanent hemodialysis transfer (>4 months), kidney function recovery, death, or PDOPPS ends. If patients left the study, they were replaced by randomly chosen patients (on an annual basis) who had entered the dialysis center since the last sampling period [23]. Within each country, national funding was utilized for data collection [23, 60]. All of the original seven countries, except for Australia and New Zealand, and two new countries (South Korea and Colombia) have participated in extended follow-up during phase 2 (2017–2020), during which the cohort has been enriched with incident patients (Fig. 28.1).
Study Data and Collection Instruments
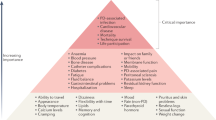
The data collected by PDOPPS using patient and facility questionnaires have been developed by six workgroups in the areas of infection prevention and management, patient support, PD catheter access and function, PD training and education, dialysis prescription and fluid management, and clinical application of PD therapy (Fig. 28.2). These workgroups consist of key international content experts who were carefully selected by the ISPD and Arbor Research Collaborative for Health to ensure diverse representation of disciplines, gender, ethnicity, and geographic regions.
Data collected by PDOPPS are depicted in Fig. 28.3. Demographic data, medical comorbidities and history, PD treatment, PD-related infections, and hospitalizations were collected at study enrolment. PD-related events or treatment changes were collected during follow-up by an interval summary questionnaire which was completed for each patient every 4 months. Furthermore, a standardized questionnaire was completed by patients, which focused on their quality of life and treatment satisfaction and was updated annually. From a center-level perspective, data collection forms were completed by the nurse unit manager and medical director to capture specific unit practices and clinical outcomes. All data were collected using standardized data collection procedures and tools, entered into an online data entry system (PDOPPSLink), and electronically submitted to the data management center at Arbor Research Collaborative for Health [23].
Analysis
Analytic methods used in PDOPPS have been described in detail previously [23]. Associations between practices and outcomes will be analyzed at both patient and center levels. In order to address possible bias introduced by unmeasured patient-level confounders, an instrumental variable analysis will also be applied, as has been done in other published DOPPS research [46]. Facility-based instrument variable analysis relies on the fact that patients are assigned to the facility’s treatment preferences in a “quasi-random” fashion, which is independent of unmeasured patient-level confounders and therefore allows more valid estimates of treatment effects.
Ancillary Studies
PDOPPS provides an important opportunity for investigator-initiated ancillary studies to be conducted. Groups are able submit proposals for analysis of existing PDOPPS data or new data collection in collaboration with PDOPPS. These proposals are reviewed and approved by the PDOPPS Steering Committee. To date, four ancillary studies have been approved:
-
(a)
The “Empowering Patients on Choices for Renal Replacement Therapy Study” (EPOCH-RRT), which aims to compare the effectiveness of hemodialysis and PD with respect to patient-centered outcomes and to develop a decision aid to assist patients with dialysis modality selection
-
(b)
“Biological Determinants of Peritoneal Dialysis Outcomes” (BIO-PD), which aims to identify and validate genetic variants that explain the interindividual variability in peritoneal membrane function in patients undergoing PD
-
(c)
“Optimizing Early Dialysis Catheter Function” (UKCath Study), which aims to establish the determinants of early PD access function, in particular “medical” versus “surgical” insertion methods and their associated treatment pathways, with the intention of improving PD access outcomes
-
(d)
“Optimizing Prevention of PD-Associated Peritonitis in the US” (OPPUS), which aims to identify patient and PD facility characteristics that are associated with PD peritonitis risk in PD patients and to foster the development and implementation of a standardized peritonitis definition and evidence-based best practice guidelines into dialysis provider organization clinical care pathways and national quality improvement initiatives with the aim of better preventing peritonitis
Current Status of PDOPPS
The initial countries participating in PDOPPS included Australia, New Zealand, Japan, the United Kingdom, Thailand, Canada, and the United States. During phase 1, 7629 patients were recruited from 215 dialysis units across the 7 countries. The study has evolved over time, and now a total of 11,688 patients have been consented for the study. The number of patients enrolled in PDOPPS from each country and the overall facility enrolment summary are summarized in Table 28.1. Additional countries joining PDOPPS in phase 2 include South Korea and Columbia.
Having multiple countries participate in PDOPPS provides a diversity of patients, PD practices, and cultures that can be evaluated throughout the study. In particular, PDOPPS contains a mix of high-income countries (Australia, New Zealand, Canada, Japan, South Korea, the United Kingdom, the United States) and low- and middle-income countries (Colombia, Thailand) from the major regions of the world (North America, South America, Europe, Asia, and Oceania). It also contains a mix of countries with different PD policies including PD-first (Thailand), PD-favored (Canada, the United States), home-based dialysis-first (Australia, New Zealand), and hemodialysis-favored (Japan) approaches [61, 62]. This greatly enhances the generalizability of PDOPPS’ findings and facilitates comprehensive evaluation of the impact of different practices and policies on PD outcomes. It also allows the examination of unique country practices, such as hybrid dialysis (a combination of PD and HD), which is utilized in approximately one-fifth of patients on PD in Japan but almost not at all in other countries [23, 63]. Moreover, the impact of any policy changes, for example, arising out of the OPPUS project, will be comprehensively evaluated via the PDOPPS platform.
Early Findings from PDOPPS
The findings collated in phase 1 of PDOPPS have thus far resulted in 19 abstracts presented at multiple international conferences and symposia, 15 published studies, and manuscripts in preparation [23, 60, 64, 65]. Some early findings from PDOPPS have been detailed below according to clinical workgroup.
Infection Prevention and Management
The infection prevention and management workgroup recently examined variations in prevention and treatment of PD-related infections in 170 centers caring for more than 11,000 patients in 7 countries [64]. The practices of each PDOPPS country were further compared against practices recommended by the ISPD guidelines, particularly with respect to monitoring the incidence of peritonitis and using prophylactic antimicrobials in the prevention of PD-related infections and empirical treatment of suspected peritonitis. Units consistently recorded and tracked peritonitis episodes in only five countries (Australia, New Zealand, Canada, the United Kingdom, and the United States), while Australia and New Zealand were the only countries in which 100% of PD units recorded and tracked exit site infections. Substantial practice variation was also observed in the use of daily topical antimicrobial prophylaxis (mupirocin or aminoglycoside) by PD units across Australia and New Zealand (ANZ, 94% of units), the United States (88%), Canada (80%), the United Kingdom (71%), Thailand (27%), and Japan (4%). This variation is difficult to understand given the strength of the practice recommendation by the ISPD guidelines (level 1B). Another key finding established was the suboptimal co-prescription of antifungal prophylaxis when PD patients received antibiotic courses to prevent fungal peritonitis, despite this being a level 1B ISPD guideline recommendation. No antifungal prophylaxis was prescribed at all in appreciable proportions of PD centers in ANZ (11%), Canada (45%), the United States (46%), Thailand (77%), the United Kingdom (88%), and Japan (93%). There was also variable administration of prophylactic antibiotics prior to PD catheter insertion despite this having a level 1A ISPD guideline recommendation. The lowest uptake of this guideline was in the United States (63%), and highest adherence was observed in the United Kingdom and Canada (100%). Considerable differences in facility adherence were also observed in the administration of prophylactic antibiotics prior to other invasive procedures, although these variable uptakes may have been explained by the limited quality and strength of the evidence in this area (levels 2C and 2D). Overall, this study highlighted the significant variations in PD peritonitis prevention and treatment practices among the participating countries, which often deviated from ISPD guideline recommendations.
The group has gone on to examine the association between selected facility practices and peritonitis rates. While the overall peritonitis rate averaged across the seven PDOPPS countries was 0.28 episodes per patient-year, country-specific rates ranged from 0.24 episodes per patient-year in the United States to 0.40 episodes per patient-year in the United Kingdom. Preliminary findings suggest that peritonitis risk is generally not associated with facility size, is lower with APD use, and is higher with failure to use preoperative prophylactic antibiotics prior to PD catheter insertion and possibly failure to use either topical exit site mupirocin or aminoglycoside ointment. These early observations suggest that poor adherence to specific clinical practice guideline recommendations was associated with a higher peritonitis risk.
Patient Support
The PDOPPS patient support workgroup has developed research questions that highlight patient-reported issues. A key focus of the group was functional impairment among PD patients, aiming to identify if there was variation between countries and if this is associated with permanent transfer to hemodialysis or higher mortality rates. Tennankore et al. assessed patient’s functional status via two self-reported questionnaires which were combined to create an overall score [65]. The study observed that functional impairment was highly prevalent among patients on PD, with significant differences between the participating PDOPPS countries. Patients in Thailand were shown to have the highest functional impairment, and Japan had the lowest. The study also established that impaired functional status was strongly associated with higher mortality rates; however, functionally impaired patients did not have an increased risk of permanent transfer to HD [65].
In a separate investigation, the workgroup has identified that patients reported a generally favorable perception of PD, with the most commonly reported advantages being home-based treatment and the lack of vascular cannulation, while the most commonly reported disadvantages were a feeling of abdominal fullness and PD fluid storage space requirements. Those patients seeing PD as more disadvantageous were more likely to be depressed, have a lower quality of life, and experience a transition to hemodialysis.
PD Training and Education
Significant variability has been found between countries in the delivery of training to PD patients. Striking differences were seen in the duration of PD training sessions with the majority of patients from Japan (88%) being trained for less than 2 hours and for 2–3 days (39%). In contrast, in Australia, 64% of patients received training sessions lasting up to 6 hours and typically over a 4–5-day period (69%). Interestingly, Japan also appeared to differ in the timing of training with 62% of patients having their training prior to PD catheter insertion, while most other countries confined training to after PD catheter insertion, typically following a period of 2–3 weeks. Canada (84%) and Japan (100%) predominantly trained patients in facilities, while Australia (57%) and the United Kingdom (50%) trained patients using a combination of home and facility. Future studies will evaluate the relationship between PD training practices and outcomes.
Dialysis Prescription and Fluid Management
Early findings from this workgroup have similarly shown that both PD prescriptions and the types of PD utilized were highly variable between the different PDOPPS countries. Most countries had a predominance of automated peritoneal dialysis (APD) use over continuous ambulatory peritoneal dialysis (CAPD) with utilization rates in the United States and Canada being 81% and 71%, respectively. However, in Thailand, the majority of PD patients were treated with CAPD (96%). Among the patients receiving APD, there were a broad number of exchanges that were prescribed to patients such that almost half of the PD patients in the United States and the United Kingdom were prescribed five or more exchanges overnight compared with 39% of patients receiving less than three exchanges in Japan. Similar degrees of national variation in practices were observed in the total dialysis volume prescribed, use of biocompatible solutions (including icodextrin), and the average concentrations of glucose employed.
Conclusion
PDOPPS is the largest and most comprehensive PD study to date. This multinational study has collected data and produced research, which will be extremely valuable to the PD community and help to provide strong evidence for improvements in PD practices. The formation of PDOPPS is unique in that it collaborates with multiple countries to create a diverse body of data for clinical research. Phase 1 has already documented wide variations in clinical practice that cannot be accounted for by patient factors as well as variation in important outcomes such as infection. The next step (Phase 2) will establish how these variations in practice associate with the primary outcome, technique failure. Future directions for PDOPPS remain vast, and the potential for further research opportunities, protocol establishment, and improvement of national and international guidelines are ongoing, providing an invaluable resource for clinicians, patients, and their caregivers.
References
Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet (London, England). 2015;385(9981):1975–82.
Li PK, Chow KM, Van de Luijtgaarden MW, Johnson DW, Jager KJ, Mehrotra R, et al. Changes in the worldwide epidemiology of peritoneal dialysis. Nat Rev Nephrol. 2017;13(2):90–103.
Bello AK, Levin A, Lunney M, Osman MA, Ye F, Ashuntantang G, et al. Global Kidney Health Atlas: a report by the International Society of Nephrology on the global burden of end-stage kidney disease and capacity for kidney replacement therapy and conservative care across world countries and regions. Brussels: International Society of Nephrology; 2019.
Kidney Health Australia. State of the Nations. 2016 Kidney Health Week Chronic Kidney Disease Hot Spots. 2016.
Just PM, Riella MC, Tschosik EA, Noe LL, Bhattacharyya SK, de Charro F. Economic evaluations of dialysis treatment modalities. Health Policy (Amsterdam, Netherlands). 2008;86(2–3):163–80.
Heaf JG, Lokkegaard H, Madsen M. Initial survival advantage of peritoneal dialysis relative to haemodialysis. Nephrol Dial Transplant. 2002;17(1):112–7.
Fenton SS, Schaubel DE, Desmeules M, Morrison HI, Mao Y, Copleston P, et al. Hemodialysis versus peritoneal dialysis: a comparison of adjusted mortality rates. Am J Kidney Dis. 1997;30(3):334–42.
Brown EA, Johansson L, Farrington K, Gallagher H, Sensky T, Gordon F, et al. Broadening options for long-term dialysis in the elderly (BOLDE): differences in quality of life on peritoneal dialysis compared to haemodialysis for older patients. Nephrol Dial Transplant. 2010;25(11):3755–63.
Rubin HR, Fink NE, Plantinga LC, Sadler JH, Kliger AS, Powe NR. Patient ratings of dialysis care with peritoneal dialysis vs hemodialysis. JAMA. 2004;291(6):697–703.
Mehrotra R, Devuyst O, Davies SJ, Johnson DW. The current state of peritoneal dialysis. J Am Soc Nephrol: JASN. 2016;27(11):3238–52.
Khawar O, Kalantar-Zadeh K, Lo WK, Johnson D, Mehrotra R. Is the declining use of long-term peritoneal dialysis justified by outcome data? Clin J Am Soc Nephrol: CJASN. 2007;2(6):1317–28.
Jose MD, Johnson DW, Mudge DW, Tranaeus A, Voss D, Walker R, et al. Peritoneal dialysis practice in Australia and New Zealand: a call to action. Nephrology (Carlton, Vic.). 2011;16(1):19–29.
Perl J, Wald R, Bargman JM, Na Y, Jassal SV, Jain AK, et al. Changes in patient and technique survival over time among incident peritoneal dialysis patients in Canada. Clin J Am Soc Nephrol: CJASN. 2012;7(7):1145–54.
Mehrotra R, Kermah D, Fried L, Kalantar-Zadeh K, Khawar O, Norris K, et al. Chronic peritoneal dialysis in the United States: declining utilization despite improving outcomes. J Am Soc Nephrol: JASN. 2007;18(10):2781–8.
Shen JI, Mitani AA, Saxena AB, Goldstein BA, Winkelmayer WC. Determinants of peritoneal dialysis technique failure in incident US patients. Perit Dial Int. 2013;33(2):155–66.
Manera KE, Tong A, Craig JC, Brown EA, Brunier G, Dong J, et al. Standardized outcomes in nephrology-peritoneal dialysis (SONG-PD): study protocol for establishing a core outcome set in PD. Perit Dial Int. 2017;37(6):639–47.
Manera KE, Johnson DW, Craig JC, Shen JI, Ruiz L, Wang AY, et al. Patient and caregiver priorities for outcomes in peritoneal dialysis: multinational nominal group technique study. Clin J Am Soc Nephrol: CJASN. 2019;14(1):74–83.
Standardised Outcomes In Nephrology (SONG). SONG-PD [cited 2019 Mar 6]. Available from: http://songinitiative.org/projects/song-pd/.
Chui BK, Manns B, Pannu N, Dong J, Wiebe N, Jindal K, et al. Health care costs of peritoneal dialysis technique failure and dialysis modality switching. Am J Kidney Dis. 2013;61(1):104–11.
Mudge DW, Boudville N, Brown F, Clayton P, Duddington M, Holt S, et al. Peritoneal dialysis practice in Australia and New Zealand: a call to sustain the action. Nephrology (Carlton, Vic). 2016;21(7):535–46.
Registry A. 41st Report, Chapter 5: Peritoneal dialysis. Australia and New Zealand Dialysis and Transplant Registry, Adelaide, Australia. 2018. Available at: http://www.anzdata.org.au.
United States Renal Data System. URDS annual data report: epidemiology of kidney disease in the United States, Volume 2 ESRD, Chapter 1. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018.
Perl J, Davies SJ, Lambie M, Pisoni RL, McCullough K, Johnson DW, et al. The peritoneal dialysis outcomes and practice patterns study (PDOPPS): unifying efforts to inform practice and improve global outcomes in peritoneal dialysis. Perit Dial Int. 2016;36(3):297–307.
Cho Y, See EJ, Htay H, Hawley CM, Johnson DW. Early peritoneal dialysis technique failure: review. Perit Dial Int. 2018;38(5):319–27.
See EJ, Johnson DW, Hawley CM, Pascoe EM, Badve SV, Boudville N, et al. Risk predictors and causes of technique failure within the first year of peritoneal dialysis: an Australia and New Zealand Dialysis and Transplant Registry (ANZDATA) Study. Am J Kidney Dis. 2018;72(2):188–97.
Lan PG, Clayton PA, Johnson DW, McDonald SP, Borlace M, Badve SV, et al. Duration of hemodialysis following peritoneal dialysis cessation in Australia and New Zealand: proposal for a standardized definition of technique failure. Perit Dial Int. 2016;36(6):623–30.
Nadeau-Fredette AC, Johnson DW, Hawley CM, Pascoe EM, Cho Y, Clayton PA, et al. Center-specific factors associated with peritonitis risk-a multi-center registry analysis. Perit Dial Int. 2016;36(5):509–18.
Castledine C, Gilg J, Rogers C, Ben-Shlomo Y, Caskey F. UK Renal Registry 13th Annual Report (December 2010): Chapter 15: UK renal centre survey results 2010: RRT incidence and use of home dialysis modalities. Nephron Clin Pract. 2011;119(Suppl 2):c255–67.
Ghali JR, Bannister KM, Brown FG, Rosman JB, Wiggins KJ, Johnson DW, et al. Microbiology and outcomes of peritonitis in Australian peritoneal dialysis patients. Perit Dial Int. 2011;31(6):651–62.
Kerschbaum J, Konig P, Rudnicki M. Risk factors associated with peritoneal-dialysis-related peritonitis. Int J Nephrol. 2012;2012:483250.
Lim WH, Boudville N, McDonald SP, Gorham G, Johnson DW, Jose M. Remote indigenous peritoneal dialysis patients have higher risk of peritonitis, technique failure, all-cause and peritonitis-related mortality. Nephrol Dial Transplant. 2011;26(10):3366–72.
Nessim SJ, Bargman JM, Austin PC, Nisenbaum R, Jassal SV. Predictors of peritonitis in patients on peritoneal dialysis: results of a large, prospective Canadian database. Clin J Am Soc Nephrol. 2009;4(7):1195–200.
McDonald SP, Collins JF, Rumpsfeld M, Johnson DW. Obesity is a risk factor for peritonitis in the Australian and New Zealand peritoneal dialysis patient populations. Perit Dial Int. 2004;24(4):340–6.
Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau-Fredette A-C, Hawley C, et al. Multicenter registry analysis of center characteristics associated with technique failure in patients on incident peritoneal dialysis. Clin J Am Soc Nephrol: CJASN. 2017;12(7):1090–9.
Schaubel DE, Blake PG, Fenton SS. Effect of renal center characteristics on mortality and technique failure on peritoneal dialysis. Kidney Int. 2001;60(4):1517–24.
Guillouët S, Veniez G, Verger C, Béchade C, Ficheux M, Uteza J, et al. Estimation of the center effect on early peritoneal dialysis failure: a multilevel modelling approach. Perit Dial Int. 2016;36(5):519–25.
Afolalu B, Troidle L, Osayimwen O, Bhargava J, Kitsen J, Finkelstein FO. Technique failure and center size in a large cohort of peritoneal dialysis patients in a defined geographic area. Perit Dial Int. 2009;29(3):292–6.
Huisman RM, Nieuwenhuizen MG, Th de Charro F. Patient-related and centre-related factors influencing technique survival of peritoneal dialysis in The Netherlands. Nephrol Dial Transplant. 2002;17(9):1655–60.
Martin LC, Caramori JC, Fernandes N, Divino-Filho JC, Pecoits-Filho R, Barretti P. Geographic and educational factors and risk of the first peritonitis episode in Brazilian Peritoneal Dialysis study (BRAZPD) patients. Clin J Am Soc Nephrol: CJASN. 2011;6(8):1944–51.
Pieper D, Mathes T, Marshall MR. A systematic review of the impact of center volume in dialysis. BMC Res Notes. 2015;8:812.
Htay H, Cho Y, Pascoe EM, Darssan D, Nadeau-Fredette AC, Hawley C, et al. Center effects and peritoneal dialysis peritonitis outcomes: analysis of a national registry. Am J Kidney Dis. 2018;71(6):814–21.
Nataatmadja M, Cho Y, Johnson DW. Continuous Quality Improvement Initiatives to Sustainably Reduce Peritoneal Dialysis-Related Infections in Australia and New Zealand. Perit Dial Int. 2016;36(5):472–7.
Robinson BM, Bieber B, Pisoni RL, Dialysis Outcomes PFK. Practice Patterns Study (DOPPS): its strengths, limitations, and role in informing practices and policies. Clin J Am Soc Nephrol: CJASN. 2012;7(11):1897–905.
Pisoni RL, Gillespie BW, Dickinson DM, Chen K, Kutner MH, Wolfe RA. The Dialysis Outcomes and Practice Patterns Study (DOPPS): design, data elements, and methodology. Am J Kidney Dis. 2004;44(5 Suppl 2):7–15.
Robinson B, Fuller D, Zinsser D, Albert J, Gillespie B, Tentori F, et al. The Dialysis Outcomes and Practice Patterns Study (DOPPS) Practice Monitor: rationale and methods for an initiative to monitor the new US bundled dialysis payment system. Am J Kidney Dis. 2011;57(6):822–31.
Pisoni RL, Arrington CJ, Albert JM, Ethier J, Kimata N, Krishnan M, et al. Facility hemodialysis vascular access use and mortality in countries participating in DOPPS: an instrumental variable analysis. Am J Kidney Dis. 2009;53(3):475–91.
Okamoto K, Kobayashi S, Noiri E. Longer treatment time and slower ultrafiltration in hemodialysis: associations with reduced mortality in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006;70(10):1877; author reply −8.
Hecking M, Karaboyas A, Saran R, Sen A, Horl WH, Pisoni RL, et al. Predialysis serum sodium level, dialysate sodium, and mortality in maintenance hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2012;59(2):238–48.
Pisoni RL, Young EW, Mapes DL, Keen ML, Port FK. Vascular access use and outcomes in the U.S., Europe, and Japan: results from the Dialysis Outcomes and Practice Patterns Study. Nephrol News Issues. 2003;17(6):38–43. 7
Ten Years of Collaboration: DOPPS Research The European Dialysis Transplant Nurses Association/European Renal Care Association (EDTNA/ERCA), Arbor Research Collaborative for Health, and the Dialysis Outcomes and Practice Patterns Study (DOPPS). (2019). [ebook] Available at: https://www.edtnaerca.org/resource/edtna/files/Ten%20Years%20of%20Collaboration_DOPPS%20Research_January%202017.pdf. Accessed 6 Feb 2019.
Locatelli F, Pisoni RL, Combe C, Bommer J, Andreucci VE, Piera L, et al. Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2004;19(1):121–32.
Locatelli F, Pisoni RL, Akizawa T, Cruz JM, DeOreo PB, Lameire NH, et al. Anemia management for hemodialysis patients: Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines and Dialysis Outcomes and Practice Patterns Study (DOPPS) findings. Am J Kidney Dis. 2004;44(5 Suppl 2):27–33.
Bailie GR, Larkina M, Goodkin DA, Li Y, Pisoni RL, Bieber B, et al. Variation in intravenous iron use internationally and over time: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2013;28(10):2570–9.
Young EW, Albert JM, Satayathum S, Goodkin DA, Pisoni RL, Akiba T, et al. Predictors and consequences of altered mineral metabolism: the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2005;67(3):1179–87.
Tentori F, Blayney MJ, Albert JM, Gillespie BW, Kerr PG, Bommer J, et al. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2008;52(3):519–30.
Rayner HC, Zepel L, Fuller DS, Morgenstern H, Karaboyas A, Culleton BF, et al. Recovery time, quality of life, and mortality in hemodialysis patients: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Am J Kidney Dis. 2014;64(1):86–94.
Tentori F, Elder SJ, Thumma J, Pisoni RL, Bommer J, Fissell RB, et al. Physical exercise among participants in the Dialysis Outcomes and Practice Patterns Study (DOPPS): correlates and associated outcomes. Nephrol Dial Transplant. 2010;25(9):3050–62.
Elder SJ, Pisoni RL, Akizawa T, Fissell R, Andreucci VE, Fukuhara S, et al. Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol Dial Transplant. 2008;23(3):998–1004.
Mariani L, Stengel B, Combe C, Massy ZA, Reichel H, Fliser D, et al. The CKD outcomes and practice patterns study (CKDopps): rationale and methods. Am J Kidney Dis. 2016;68(3):402–13.
DOPPS. Peritoneal dialysis outcomes and practice patterns study [Internet] 2019, [updated October 2018; cited 2019 Feb 4. Available from: https://www.dopps.org/OurStudies/PeritonealDialysisPDOPPS.aspx.
Dhanakijcharoen P, Sirivongs D, Aruyapitipan S, Chuengsaman P, Lumpaopong A. The “PD First” policy in Thailand: three-years experiences (2008-2011). J Med Assoc Thailand = Chotmaihet thangphaet. 2011;94(Suppl 4):S153–61.
Liu FX, Gao X, Inglese G, Chuengsaman P, Pecoits-Filho R, Yu A. A global overview of the impact of peritoneal dialysis first or favored policies: an opinion. Perit Dial Int. 2015;35(4):406–20.
Kawanishi H, Moriishi M, Katsutani S, Sakikubo E, Tsuchiya S. Hemodialysis together with peritoneal dialysis is one of the simplest ways to maintain adequacy in continuous ambulatory peritoneal dialysis. Adv Perit Dial Conf Perit Dial. 1999;15:127–31.
Boudville N, Johnson DW, Zhao J, Bieber BA, Pisoni RL, Piraino B, et al. Regional variation in the treatment and prevention of peritoneal dialysis-related infections in the Peritoneal Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant. 2018;34(12):2118–26, 2019.
Tennankore KK, Zhao J, Karaboyas A, Bieber B, Robinson BM, Morgenstern H, et al. The association of functional status with mortality and dialysis modality change: results from the peritoneal dialysis outcomes and practice patterns study (PDOPPS). Perit Dial Int. 2019. (in press).
Acknowledgments
PDOPPS receives financial support from several sources that together make this enterprise possible, including Baxter Healthcare (Core Funding, Arbor Research Collaborative for Health); Canadian Institutes of Health Research; National Health and Medical Research Council of Australia; Japanese Society for Peritoneal Dialysis; Research for Patient Benefit Programme, National Institute for Health Research, UK (includes funding of ancillary UK Catheter Study); Kidney Research UK (UK Phase 2 participation); Thailand Research Foundation, National Research Council of Thailand; Patient-Centered Outcomes Research Institute, USA (EPOCH-RRT and OPUSS ancillary study); and National Institutes of Health, USA (Bio-PD ancillary study).
PDOPPS is made possible by the willing participation of many. We gratefully acknowledge the members of the study workgroups, the country investigators and their teams, and, above all, the patients.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stallard, B., Johnson, D.W., Perl, J., Davies, S.J. (2021). The Peritoneal Dialysis Outcomes and Practice Patterns Study. In: Rastogi, A., Lerma, E.V., Bargman, J.M. (eds) Applied Peritoneal Dialysis. Springer, Cham. https://doi.org/10.1007/978-3-030-70897-9_28
Download citation
DOI: https://doi.org/10.1007/978-3-030-70897-9_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-70896-2
Online ISBN: 978-3-030-70897-9
eBook Packages: MedicineMedicine (R0)