Abstract
Small leucine-rich proteoglycans (SLRPs) represent the largest family of proteoglycans consisting of 18–19 members. They play diverse structural and biological roles by interacting with extracellular matrix components, growth factors, and cell surface receptors. One of the well-studied features of SLRPs is their structural control of collagen fibrillogenesis. Since fibrillar collagens are the structural basis for mineralization in bone, dentin, and cementum, such interactions may inhibit and/or facilitate mineralization. The ability to modulate specific growth factors can be used for effective mineralized tissue engineering. In this chapter, we will provide an overview of the basic structural and genomic features of SLRPs, their roles in collagen mineralization, cell signaling, and potential utility for mineralized tissue regeneration.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Proteoglycans are a class of molecules consisting of a protein core with one or more covalently bound glycosaminoglycan (GAG) chains. GAG is a linear polymer of repeating disaccharides and, based on the combination of the two saccharide units, there are six types of GAGs, i.e., chondroitin sulfate (CS), dermatan sulfate (DS), keratan sulfate (KS), heparan sulfate (HS), heparin (Hep), and hyaluronic acid (HA). Except for HA, GAGs are sulfated. Due to their highly negative charged nature, they interact with a number of positively charged molecules (see a review by Vallet et al. 2020). Proteoglycans are highly heterogeneous molecules and localized inside, on the surface, and outside of the cells (Karamanos et al. 2018) playing both structural and biological roles.
“SLRPs”, “Small Leucine-Rich Proteoglycans” (Iozzo and Murdoch 1996), were originally defined as proteoglycans with a relatively small protein core (36–42 kDa) harboring tandem leucine-rich repeats (LRRs), a hallmark motif LxxLxLxxNxL (L: leucine which can be substituted by isoleucine, valine, and other hydrophobic amino acids; x: any amino acids), with several posttranslational modifications including substitution with GAG side chains of various types.
Through the protein core, SLRPs are capable of binding a number of proteins including fibrillar collagens, growth factors including transforming growth factor-β (TGF-β), platelet-derived growth factor (PDGF), vascular endothelial growth factor A (VEGFA), connective tissue growth factor, and cell surface receptors including epidermal growth factor receptor (EGFR), c-Met, insulin-like growth factor receptor I (IGF-IR), vascular endothelial growth factor receptor 2 (VEGFR2), Toll-like receptors (TLRs). As such they are involved in a plethora of biological and pathological processes such as development, inflammation, autophagy, angiogenesis, and tumorigenesis (Iozzo and Schaefer 2015).
Thus, it is not surprising that SLRP members play important roles in the formation and maintenance of skeletal tissues including mineralized tissues like bones and teeth (enamel, dentin, and cementum)—see reviews by Nikitovic et al. (2012), Zappia et al. (2020), and Kram et al. (2020). In this chapter, we will provide an overview of the basic structures and functions of SLRPs, then focus on the specific SLRPs and their roles in mineralized tissues, especially, collagen-based mineralized dental tissues such as dentin and cementum, and bone, and their therapeutic potentials.
2 SLRP Family
There has been a number of SLRP genes identified by biochemical and molecular approaches. As such, the SLRP represents the largest family of proteoglycans (Karamanos et al. 2018) composed of 18–19 members (Iozzo and Schaefer 2015) (see below). These members are secreted extracellular matrix (ECM) molecules except nyctalopin that is located at the outer leaflet of the plasma membrane. Based on the protein, genomic structure, and chromosomal organization (see below), they are classified into five major classes. With the increase in the number of SLRP members, the definition and classification of SLRPs became less clear. For instance, the size of the protein core of some members such as chondroadherin-like is relatively large (~83 kDa) when compared to those of typical SLRP members (36–42 kDa). Some of the members such as asporin and chondroadherin lack GAG chains; thus, by definition, they are not “proteoglycans”. Nonetheless, in the following section, we will discuss SLRP members which (1) have “relatively” small protein core as compared to large proteoglycans like aggrecan and versican (>200 kDa), (2) do not have any transmembrane domains, and (3) have multiple LRR domains. Some other structural features of the protein core are also briefly discussed.
2.1 Protein Structures/Domains
-
1.
BMP-1/mammalian tolloid proteinase-processing motif
It has been reported that some SLRP family members are substrates for BMP-1, mammalian tolloid (mTLD), and mTLD-like proteinases (Scott et al. 2000; Von Marschall and Fisher 2010; Ge et al. 2004). It is well known that several ECM proteins including procollagen α1(I), α2(I), α1(II), α1(III), chordin, prolysyl oxidase are also processed by this protease family (Scott et al. 2000). BMP-1 and mTLD have been demonstrated to play important biological roles in the formation of ECM, for example, cleavage of the C-propeptides of procollagens I, II, and III (Kessler et al. 1996; Li et al. 1996) allowing collagen fibrillogenesis, and cleavage of the prodomain of prolysyl oxidase leading to its enzymatic activation to initiate cross-linking of collagen and elastin (Uzel et al. 2001). Among SLRP members, biglycan was the first that was shown to be secreted as a pro-form and cleaved by BMP-1 at the M(M/L)N-DEE site (Scott et al. 2000). Decorin also has a similar sequence of M(L/I)E-DE(A/G) that was susceptible to cleavage by BMP-1/mTLD members (Von Marschall and Fisher 2010). The immunoelectron microscopic study revealed that distribution of pro-decorin and pro-biglycan are more readily detected in predentin as compared to dentin (Septier et al. 2001) indicating that active enzymatic processing occurs prior to matrix mineralization. Osteoglycin, one of class III SLRP members, has also been reported that BMP-1/mTLD proteinases process its pro-form. Moreover, like decorin, the mature osteoglycin was shown to delay the rate of type I collagen fibrillogenesis in vitro as compared to the pro-form, indicating the cleavage of the prodomain enhances its biological activity (Ge et al. 2004). The significance of the pro versus mature forms of SLRPs in the process of mineralization is still not clear.
-
2.
Cysteine residues cluster motif
There are four cysteine residues commonly found at the N-terminal region, which is called a “capping motif”. This motif is often used to classify the SLRP members mainly based on the different spacing between cysteine residues. In general, class I has CX3CXCX6C, class II CX3CXCX9C, class III CX2CXCX6C, class IV CX3CXCX8C or CX3CXCX6C or CX3CXCX17C, and class V CX3CXCX7C (Fig. 6.1). Interestingly, chondroadherin-like, a newly identified SLRP member, has this capping motif not only at the N-terminal but also at the mid-region of the protein. The four cysteine residues are known to form a disulfide bond between the first LRR domain (LRR1) and β-hairpin structure. At the C-terminal region, SLRP members have the capping motif where two cysteine residues form a disulfide bond (Mcewan et al. 2006). One of the two C-terminal cysteines usually located at one LRR domain and another at the subsequent LRR. This has been well presented by the crystal structural analysis of decorin (Scott et al. 2004). There is one cysteine residue in LRR11, which is longer than other LRR motifs in decorin, bonded with another cysteine residue in LRR12. This longer LRR has been called “ear repeat” (Mcewan et al. 2006). It is considered that both N-terminal and C-terminal cysteine motifs of SLRPs would help stabilize the central LRR domain (Iozzo and Schaefer 2015).
There are several SLRP members expressed in the cornea, a fibrillar collagen-rich tissue. The mice lacking lumican, a collagen-binding SLRP, exhibits abnormal size and shape of collagen fibrils leading to cornea opacity (Chakravarti et al. 2000). Congenital stromal corneal dystrophy (CSCD) is a rare autosomal dominant eye disease characterized by corneal stromal opacification and visual loss with increasing corneal thickness and abnormal fibrils in the stroma. This disease is caused by the heterozygous mutation in the human decorin gene and the mutations cause frameshift leading to a truncation of the decorin protein (Bredrup et al. 2005; Rodahl et al. 2006; Jing et al. 2014). The truncated decorin lacks the C-terminal 33 amino acids, which disrupted the “ear repeat” domain. It is thus likely that loss of stabilization of the central LRR domain by truncation of the ear repeat domain could lead to abnormal collagen assembly.
-
3.
Glycosaminoglycan (GAG) attachment and other unique domains
As described above, many of the SLRP members are proteoglycans with covalently bound GAG(s) but some are known as “part-time” proteoglycans, i.e., partially or completely lacking GAG components. It is known that the CS/DS-type GAG attachment is initiated by transferring a UDP-xylose residue to specific serine moieties. This rate-limiting step is catalyzed by two enzymes, namely xylosyltransferase (XYLT) I and II. The consensus sequence for xylosylation has been reported as aaaa-GSG-aa/G-a, where a is aspartic acid (D) or glutamic acid (E) (Roch et al. 2010). For instance, human decorin contains a sequence of DEASGIGP and human biglycan, which has two GAG attachment sites, contains a sequence of DEEASGADTSGVLD (underlined amino acids are met with consensus). KS type GAG attachment is a more complicated process and there have been three types of KS structures identified. Keratan sulfate in the cornea (KS-I) is attached to asparagine via a complex-type N-linked oligosaccharide, while in cartilage, KS-II is O-linked via GalNAc to serine or threonine residues via the mucin core-2 structure. KS-III identified in the brain is attached mannose O-linked to serine (Funderburgh 2002). The GAG attachment is also required for efficient secretion of the proteoglycan (Seo et al. 2005), collagen interaction (Ruhland et al. 2007; Raspanti et al. 2008), and interaction with Lyme disease spirochete Borrelia burgdorferi (Benoit et al. 2011).
Within the protein core, some SLRP members have unique acidic amino acid structures outside of LRRs. Fibromodulin, osteoadherin/osteomodulin, and lumican, for instance, are known to have tyrosine sulfate residues, i.e., fibromodulin has up to nine sites at the N-terminal region prior to LRR1, osteoadherin has up to six sites at the N-terminal and two at the C-terminal regions, and lumican has up to two sites at the N-terminal region (Antonsson et al. 1991; Onnerfjord et al. 2004). Tyrosine sulfation is considered to enhance protein interaction. Another example is asporin, a class I SLRP member, whose name reflects the unique poly aspartate-stretch at the N terminus. It has been reported, in osteoarthritis, the human asporin allele having 14 aspartic acid repeats, designated D14, was overrepresented relative to the common allele having 13 aspartic acid repeats (D13), and its frequency increased with disease severity (Kizawa et al. 2005).
-
4.
LRR motifs
The core proteins of all SLRP members contain a central region composed of LRRs flanked by disulfide-bonded terminal domains as described above.
There are two types of LRR motifs that are based on the general consensus sequence (Matsushima et al. 2000), i.e., type T (zzxxaxxxxFxxaxxLxxLxLxxNxL) and type S (xxaPzxLPxxLxxLxLxxNxI), where “z” is frequently a gap, “x” indicates variable residues, “a” is valine, leucine, or isoleucine and I is isoleucine or leucine. Based on the criteria, class I and II SLRPs have 12 LRR motifs composed of four tandem STT “super-motifs,” i.e., (STT)4. Class III SLRPs, including epiphycan and osteoglycin, have seven LRRs composed of (ST)T(ST)2. Chondroadherin and nyctalopin, class IV members, contain only type T LRRs.
The LRR domains of many SLRP members bind collagens and modulate collagen fibrillogenesis in vitro. Indeed, decorin is named because of its ability to bind, thus, “decorate” collagen fibrils (Krusius and Ruoslahti 1986). Figure 6.2 shows a schematic representation of a human decorin protein structure containing 12 LRRs. SLRP-collagen binding has been extensively studied for the last two decades. It has been demonstrated that a small region of LRR6-LRR7 in decorin is responsible for binding type I collagen and the synthetic peptide of SYIRIADTNIT derived from decorin inhibits the binding of full-length decorin to type I collagen in vitro (Kalamajski et al. 2007). In another report, a region of LRR1 in fibromodulin (RLDGNEIKR) was shown to bind type I collagen (Kalamajski and Oldberg 2007). Apparently, lumican and fibromodulin compete with each other for the collagen binding indicating that both bind the same or close region of collagen (Svensson et al. 2000). It has also been demonstrated that a region of LRR7 in lumican binds type I collagen (Kalamajski and Oldberg 2009). These findings suggest that the binding of multiple SLRPs may regulate collagen fibrillogenesis in a concerted manner that may contribute to the formation of specific ECM architecture.
Phylogenetic analysis of all SLRP members. The SLRP protein sequences were obtained from the public database as the NCBI reference sequences. Phylogenetic analysis was performed using PhyML software program based on the multiple sequence alignment of these protein sequences by the Clustal-W program (Guindon and Gascuel 2003). The NCBI reference sequences used are: mouse Decorin (NP_001177380.1), mouse Biglycan (NP_031568.2), mouse Asporin (NP_001165952.1), mouse Lumican (NP_032550.2), mouse Fibromodulin (NP_067330.1), mouse Osteomodulin (NP_001347637.1), mouse PRELP (NP_473418.3), mouse Keratocan (NP_032464.1), mouse Osteoglycin (NP_032786.1), mouse Opticin (NP_473417.2), mouse Epiphycan (NP_001366385.1), mouse Nyctalopin (NP_775591.1), mouse Chondroadherin (NP_031715.1), mouse Chondroadherin-like (NP_001157792.1), mouse Podocan (NP_001272885.1), mouse Podocan-like (NP_001013402.2), mouse Tsukushin (NP_001019790.1), mouse Nephrocan (NP_079960.1). aTsukushin is a mouse ortholog of human Tsukushi. (m) indicates that Nephrocan is identified in mouse but not human. Note that the N-terminal Cysteine residues cluster varies in class IV members, i.e. CX3CXCX8C found in Chondroadherin and Chondroadherin-like, CX3CXCX6C in Nyctalopin and CX3CXCX17C in Tsukushin
Decorin domain structure. Schematic representation of protein domain structures in human decorin. Human decorin protein structure is illustrated (359 amino acids based on NCBI Reference Sequence; NP_001911.1). Each domain is symbolized such as Signal peptide domain (SP), prodomain (Pro), glycosaminoglycan (GAG) attachment site, cysteine cluster motifs at N and C terminal parts, Leucine-Rich Repeat (LRR) motif and N-glycosylation sites. S34 indicates serine residue with a GAG attachment site
3 SLRPs in Mineralized Tissues and Their Potential Functions
Biglycan and decorin, two of the most well-studied SLRP members, were first identified in bone (Fisher et al. 1983; Fisher et al. 1987) and named PG1 and 2, respectively. Extraction and identification of proteins in mineralized tissues such as bones and teeth are challenging because the proteins are embedded and protected by the minerals (see below). Thus, in order to isolate and characterize SLRPs in mineralized tissues, an extra step of “demineralization” is often required.
During the last several decades, several GAG components and SLRP members in dentin, cementum, and bone were characterized by biochemical, histochemical, immunohistochemical, immunogold-labeling, and spectroscopic (FTIR/Raman) approaches.
3.1 Identification and Localization of SLRPs in Pre- and Mineralizing-Fractions and Available Imaging Techniques
Several studies have employed multiple approaches to identify and localize SLRP members in predentin-dentin, precementum-cementum as well as in osteoid-mineralized bone matrices (Ababneh et al. 1999; Cheng et al. 1996, 1999; Goldberg et al. 2003; Hall and Embery 1997; Hoshi et al. 2001). Some of the studies on SLRPs in these tissues have been done biochemically by differential fractionation of mineralized matrices into mineral-unbound and -bound fractions by using chaotropic agents, e.g., guanidine-HCl, followed by demineralization with EDTA. Then, SLRPs could be isolated and identified from each fraction by a series of chromatography, Western blot, and N-terminal amino acid sequence analyses (Cheng et al. 1996, 1999). Studies in the late 1990s by Embery and Yamauchi’s groups (Ababneh et al. 1999; Cheng et al. 1996) are examples of two early and thorough evaluations of SLRPs in cementum. Below, we describe some of the approaches to localize GAGs, proteoglycans, and SLRPs in these mineralized tissues:
-
1.
Histochemical approach: Proteoglycans and their GAGs can be detected in tissues by histological staining using cationic dyes such as Safranin O, Cuprolinic blue, Alcian blue, and Toluidine blue (Hyllested et al. 2002). These dyes can bind anionic components such as GAGs and proteoglycans. One of the early methods was the staining with Cuprolinic blue (Sarathchandra et al. 2002). The native structure of proteoglycans appears as a stellate rod-like structure (Goldberg and Takagi 1993). Alcian blue staining which has a copper atom in its chromophore can be used for electron and light microscopy (Scott 1972; Tice and Barrnett 1965). Toluidine blue reacts with the negatively charged groups to produce a different intensity of colors depending on the extent of carbohydrates or other negatively charged molecules. In dental tissues, Goldberg and Takagi provided an extensive review on GAGs/proteoglycans in predentin and dentin characterized by using multiple cationic dyes, hyaluronidase-gold labeling, lectin-labeling, specific antibodies, and autoradiography. Based on the staining patterns, they proposed that there are two distinct groups of proteoglycans, one mineral inhibitor abundant in predentin and another mineralization promotor localized in dentin (Goldberg and Takagi 1993). Goldberg and Septier showed another method to stain GAGs in predentin and dentin by using various concentrations of magnesium chloride and showed how to best identify the presence of GAGs, although the type of GAGs could not be determined by this method (Goldberg and Septier 1992). Alcian blue, colloidal iron for acidic proteoglycans, and periodic acid-Schiff (PAS) for glycoproteins have also been used in combination to characterize bone proteoglycans in cortical versus trabecular; highly mineralized versus osteoid. Tissues rich in proteoglycans interfibrillarly (such as medullary bone area) is highly stained by these dyes (Bonucci and Gherardi 1975). GAGs can also be characterized by radiolabeling sulfate groups and quantified (Maccarana et al. 2017), by fluorophore-assisted carbohydrate electrophoresis (FACE) (Karousou et al. 2014), or by liquid chromatography combined with mass spectroscopy (Huang et al. 2013; Kubaski et al. 2017).
-
2.
Immunohistochemistry (IHC): When antibodies against specific proteoglycan molecules with no clear cross-reactivity to other molecules are used, IHC is a powerful approach to localize and semi-quantify the molecules within tissues. One of the early reports is by Embery’s group who utilized antibodies for versican (a large CS proteoglycan), biglycan, decorin, and lumican to examine their distribution in cementum. Samples were from human teeth with various age groups and healthy versus periodontitis groups. There was no difference among different age groups or disease conditions. But it was found through IHC that acellular cementum did not have those proteoglycans but cellular cementum did. Biglycan was concentrated around cementocytes and incremental lines (Ababneh et al. 1999). The distribution of fibromodulin was described by IHC in rat dental and periodontal tissues during cementogenesis and root development corroborating its role in mineralization (Matias et al. 2003).
Hall and co-workers reported that lumican is highly concentrated in predentin compared to dentin matrix in human teeth (Hall and Embery 1997). This is similar to the results reported by Cheng et al. showing that fibromodulin and lumican are almost exclusively localized in precementum and lacunae housing cementocytes, thus, pre-/non-mineralized matrices (Cheng et al. 1996). The latter group further reported that decorin and biglycan were also preferentially localized in pre-/non-mineralized matrix in cementum (Cheng et al. 1999). The tissue distribution of decorin and fibromodulin in bone, periodontal ligament, and cementum were examined using biglycan KO and wild-type mice revealing a compensatory function for decorin in periodontal tissues in the absence of biglycan (Chiu et al. 2012).
-
3.
Electron microscopy: In the last 20 years, electron microscopy has been widely used to localize proteoglycans in dental tissues by labeling SLRPs with colloidal gold particles. Using antibodies against pro- and mature-forms of decorin and biglycan, Septier and co-workers semi-quantified the immunoreactivities of these SLRP forms in rat incisors and demonstrated that the distribution pattern of the pro- and mature-forms of these SLRPs are distinct from each other and their concentrations change from predentin to dentin transition (Septier et al. 2001). If double labeling of an SLRP and collagen using different sizes of gold particles is used, a spatial correlation between the specific SLRP and collagen fibrils can be assessed. Using this technique, Orsini and co-workers examined the distribution of decorin and biglycan in human dentin and found that both SLRPs are associated with collagen fibrils in predentin and their immunoreactivities are weak in mineralized intertubular dentin (Orsini et al. 2007). Decorin appears to be abundant around odontoblast processes (Orsini et al. 2007).
-
4.
Fourier transform infrared imaging spectroscopy (FT-IRIS) and Raman spectroscopy: FT-IRIS imaging is sensitive to detect matrix composition including collagens and proteoglycans, and can be used alone or in combination with Near-Infrared spectroscopy which is highly sensitive to water content. Proteoglycans are measured in areas of absorbance at 985–1140 cm–1 (while collagen CH2 side chain is at 1326–1356 cm–1). These absorbance bands have been validated against histological staining in native, diseased, and engineered cartilage (Boskey and Pleshko Camacho 2007). Proteoglycan content and distribution can be evaluated across tissue and even correlated with mineral distribution and collagen maturation. With this technique, relative collagen content increased from cartilage toward bone while proteoglycan content is higher in deeper areas of the cartilage tissue (Khanarian et al. 2014). Raman Spectroscopy is also capable of assessing proteoglycan content in soft and mineralized tissues and may have an advantage over FT-IRIS because its spectral band for proteoglycan (~1375 cm–1) does not overlap with the phosphate band that is close to that of proteoglycan in the case of FT-IRIS (Gamsjaeger et al. 2014). Although both techniques can provide relative proteoglycan content, they cannot identify the specific proteoglycan species. However, Raman spectral signature comes from the glycosaminoglycan chains which are mostly of CS nature (~90% of total GAG content in bone and almost 100% in mineralized dentin) in mineralized tissues such as bone and dentin and are associated mostly with decorin and biglycan (Paschalis et al. 2017; Waddington et al. 2003).
3.2 Collagen-Based Mineralization and SLRPs
Bone, dentin, and cementum are primarily composed of two phases, inorganic minerals (mostly, carbonated hydroxyapatite) and organic fibrillar type I collagen. In these tissues, collagen fibrils are formed prior to mineralization creating a pre-mineralizing matrix, i.e., osteoid, predentin, and precementum, then mineralization occurs in and around the collagen fibrils (Mahamid et al. 2010). Though the exact mechanism of mineralization and the location of minerals are still controversial (Boskey 1998; Landis et al. 1996; Schwarcz 2015; Georgiadis et al. 2016; Xu et al. 2020), a number of early and recent in vitro and in vivo observations indicate that the majority of minerals are first deposited in the contiguous hole zones in the collagen fibrils, i.e., intermolecular channels (Katz and Li 1973; Weiner and Traub 1986, Landis et al. 1993, Nudelman et al. 2010, Wang et al. 2012, Zhou et al. 2016, Xu et al. 2020). Thus, minerals in the fibrillar collagens are deposited and organized in a highly specific manner resulting in a very stiff and durable biomaterial (Glimcher 1984). Unquestionably, collagen fibrils control the spatial aspect of mineralization in these tissues by defining the space for mineral deposition and growth. Apparently, as minerals grow in the fibrils, the fibrils are structurally distorted as observed in periodontal ligament-cementum interface (Quan and Sone 2015), turkey leg tendon (Fratzl and Daxer 1993; Yamauchi and Katz 1993), and bone (Burger et al. 2008) resulting in increasing intrafibrillar space to accommodate the final mass of minerals. There has been controversial if non-collagenous proteins are required to induce collagen mineralization, but some of the recent in vitro studies show that collagen alone is capable of initiating nucleation (Nudelman et al. 2010; Xu et al. 2020).
Though collagen fibrils alone are capable of directing crystal nucleation and growth (Silver and Landis 2011; Wang et al. 2012; Xu et al. 2020), the presence of non-collagenous proteins that bind collagen fibrils including SLRPs has a significant impact on the mineral ions sequestration and release, and the hydration state around collagen fibrils. The calcium-binding phosphorylated acidic proteins such as SIBLINGs (small integrin-binding ligand N-linked glycoproteins) including dentin sialophosphoprotein, dentin matrix protein 1, and bone sialoprotein were shown to bind both calcium ion and fibrillar type I collagen (Traub et al. 1992; George et al. 1996; He and George 2004; George and Veis 2008). By binding near the gap regions/hole channels of collagen fibrils, they may efficiently facilitate the initiation of collagen mineralization. The fact that various mutations in the human dentin sialophosphoprotein gene lead to type II dentinogenesis imperfecta supports this notion (Kim and Simmer 2007).
The proteoglycans in the dentin matrix represent less than 3% by volume (Bertassoni 2017), however, they have been found to play significant roles in tissue mineralization. In dentin and cementum, the most well-characterized and the major SLRPs are in class I (decorin and biglycan), and class II (fibromodulin, lumican, and osteoadherin/osteomodulin) members. In dentin and cementum, mineralization occurs in and around type I collagen fibrils, thus, collagen-binding SLRPs such as decorin, fibromodulin, and lumican likely play an important role in this process (Chen and Birk 2013). Though other members including biglycan and osteoadherin (aka osteomodulin) have been reported to bind collagen fibrils (Schonherr et al. 1995; Svensson et al. 1995; Tashima et al. 2015, 2018), their binding is relatively weak. Indeed, gain- and loss-of-function experiments indicated that the amounts of biglycan do not significantly affect collagen fibrillogenesis like decorin does (see below) (Parisuthiman et al. 2005; Mochida et al. 2009).
3.3 GAGs in Mineralization
In the predentin, biglycan and decorin are mostly modified with DS, however, in the predentin-dentin interface, CS becomes the major form, and in mineralized dentin. CS is the only GAG chain identified (Waddington et al. 2003), while KS distribution in the predentin forms a gradient with a maximum concentration toward the mineralization front (Goldberg et al. 2003). Moreover, the position of the sulfate within the GAG also varies within these tissues, and the length of GAG chains is longer in dentin than those in predentin and in the dentin/predentin interface (Waddington et al. 2003). For the early studies on the distribution and potential functions of various GAG species in dentin mineralization, see Embery’s review (Embery et al. 2001). Apparently, GAG components contribute to the mechanical properties of the dental tissues (De Mattos Pimenta Vidal et al. 2017) because of their physicochemical nature, capabilities of occupying a large space and retaining water, and forming bridges between collagen fibrils. GAGs are also thought to play a role in mineralization; in dentin, CS may facilitate the mineralization process by sequestering calcium ions.
3.4 SLRP Functions in Biomineralization
In our early studies, we identified several SLRP members in tooth cementum and dentin. In the former, lumican and fibromodulin were identified by immunohistochemical, Western blot, and amino acid sequence analyses. The former was the major species and the latter a minor, but both SLRPs were almost exclusively located in pre-mineralizing, i.e., precementum, and non-mineralized, i.e., pericementocytes, matrices (Cheng et al. 1996). In the same tissue, we also identified chondroitin-4-sulfate SLRPs, decorin, and biglycan. The former is closely associated with collagen fibers in the periodontal ligament and cementum, the latter with cementoblasts and precementum (Cheng et al. 1999). By employing a similar approach, we also identified and immunolocalized lumican and fibromodulin in predentin and dentin, and demonstrated that both are also mainly localized in pre- (predentin) and non-mineralized (peri-odontoblast processes) matrices (Yamauchi et al. 2000). Thus, in both mineralized dental tissues, these SLRP members appear to locate mainly in the “pre-mineralized” matrices, i.e., precementum and predentin, and “non-mineralized” matrices, i.e., lacunae housing cementocytes and intratubular dentin. These preferential localizations of SLRPs (and proteoglycans in general) in dental tissues have been reported by a number of groups (Takagi et al. 1990; Hall et al. 1997; Goldberg et al. 2005; Orsini et al. 2007; Nikdin et al. 2012; Randilini et al. 2020).
It has been reported that decorin is removed prior to bone mineralization (Hoshi et al. 1999). Similarly, fibromodulin that is abundant in articular cartilage surface decreases toward the cartilage–bone interface (Hedlund et al. 1994). Another class II SLRP member, ostoadherin, aka osteomodulin, is also almost exclusively localized in predentin but more concentrated toward the mineralization front (Nikdin et al. 2012).
All of these studies clearly demonstrate that these collagen-binding SLRPs are preferentially localized in pre-/non-mineralizing areas of mineralized tissues but at or prior to mineralization, they may be removed or partially degraded (Septier et al. 2001). Based on these observations and a gradient distribution pattern, some groups (Hall et al. 1997; Nikdin et al. 2012) speculate that some of these SLRP members play a critical role in facilitating matrix mineralization. However, on the contrary, some groups reported that these SLRPs rather inhibit premature collagen mineralization (Hoshi et al. 1999; Cheng et al. 1996; Yamauchi et al. 2000). Such inhibition can be done by binding and compressing the collagen fibrils through water-retaining GAG chains and/or by blocking the mineralization sites. Then after their removal/degradation, collagen fibrils get decompressed, thus, increases the intrafibrillar space to get mineralized (Cheng et al. 1996, 1999; Yamauchi et al. 2000) (Fig. 6.3). The decorin and biglycan gene knockout mouse models showed some phenotype in dentin, but it seems to be transient and self-repair (Goldberg et al. 2005). Biochemical studies in the past have indicated that there are two groups of proteoglycans: one in predentin matrix and the other transported to the mineralization front rapidly and incorporated into mineralized dentin matrix (Lormee et al. 1996). Apparently, fibromodulin and lumican belong to the former group and the regulation of collagen mineralization could be one of the functions of these proteoglycans.
Potential roles of collagen-binding SLRPs in collagen mineralization. In the pre-mineralizing state, they bind collagen fibril at or near the gap regions through the core proteins. Their GAG components attract and hold water molecules, thus, apply osmotic pressure to the fibril. These may inhibit premature collagen mineralization. Decorin is used as an example for this process in the illustration but other SLRPs such as fibromodulin and lumican may play this role as well. These SLRPs could be removed or degraded at/prior to mineralization, which decompresses the fibril and exposes the gap region of the fibril for mineralization. Some of the SLRPs/non-collagenous proteins such as SIBLINGs may, however, facilitate mineralization by sequestering and releasing calcium ions to collagen mineralization sites. Relative scale is not taken into consideration in this illustration
The above hypotheses on the role of SLRPs in inhibition and/or facilitation of dentin and cementum (bone as well) mineralization, are largely based on observational and correlative studies. To prove these functions, one viable approach is a gain- and loss-of-function study.
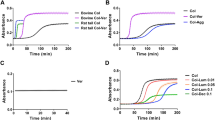
3.5 Effect of SLRPs on Biomineralization Through Gain- and Loss-of-Function Approaches In Vitro
To understand the molecular function of SLRPs in the biomineralization of dental tissues, several in vitro studies have been conducted. However, such studies are very limited largely due to the unavailability of well-established odontogenic cell lines such as odontoblasts, ameloblasts, and cementoblasts. Thus, one approach would be the use of a well-established osteoblastic cell line, e.g., MC3T3-E1 cells. These were originally established from newborn mouse calvaria (Sudo et al. 1983) and several subclones were further established (Wang et al. 1999). Subclone 26, which has a high differentiation/mineralization potential, has been widely used for functional studies (Mochida et al. 2003, 2009; Parisuthiman et al. 2005). Using this cell line, a single-cell-derived clones expressing higher or lower levels of decorin or biglycan were generated and characterized (Mochida et al. 2003; Parisuthiman et al. 2005). The levels of decorin did not affect cell proliferation or osteogenic marker expression. However, the decorin overexpression led to severely delayed mineralization, while its suppression resulted in accelerated mineralization. The timing of mineralization was inversely correlated to the expression levels of decorin in these clones (Mochida et al. 2003). The major phenotype in these clones was collagen fibrillogenesis. When decorin was overexpressed, collagen fibrils were markedly thinner, while decorin was suppressed, they were larger and irregular in shape. In the latter, the crystallinity of minerals was poor (Mochida et al. 2009). These results suggest that decorin inhibits mineralization by modulating collagen assembly. When the same approach was employed for biglycan, it was found that biglycan rather accelerates mineralization by positively modulating bone morphogenetic protein (BMP)2/4 function, thus, osteoblast differentiation. The effect of biglycan levels on collagen fibrillogenesis was minimal (Parisuthiman et al. 2005; Mochida et al. 2006). These results were confirmed by in vivo cell transplantation assays (Mochida et al. 2009; Parisuthiman et al. 2005). These studies indicate that these structurally similar class I SLRP members have distinct roles in matrix mineralization, i.e., decorin inhibits this process by controlling collagen fibrillogenesis while biglycan accelerates by positively modulating osteogenic BMP function.
To investigate the function of osteoadherin (aka osteomodulin), a class II SLRP member, in mineralization, a similar approach was also employed by using MC3T3-E1 cells (Rehn et al. 2008). Overexpression of osteoadherin reduced cell proliferation, increased alkaline phosphatase activity, and led to accelerated in vitro mineralization. The expression levels of osteocalcin (Ocn) and osteoglycin (Ogn), a class III SLRP, were upregulated, while bone sialoprotein (Bsp) level was unchanged in these overexpression clones. Repression of osteoadherin resulted in increased cell proliferation and reduced alkaline phosphatase activity; however, the extent of in vitro mineralization was unchanged. The expression of the level of Ocn and Bsp were unaffected while that of Ogn was downregulated. The results in this study appeared inconclusive possibly because these stably transfected clones were not established as a single-cell-derived, isolated clones, but maintained as a mixed population.
These studies described above may pose a limitation as only one cell type from calvaria/intramembranous ossification was investigated. However, the MC3T3-E1 cell is probably the only well-established non-transformed osteoblastic cell line that undergoes a normal process of differentiation and collagen mineralization with minimal inter-clonal variations. Thus, this is an excellent model to examine the roles of matrix molecules such as SLRPs in collagen fibrillogenesis and mineralization.
3.6 Gene KO Models: SLRPs Affect Bone/Tooth Structures/Mineralization
There have been 18 members of SLRPs identified in mice (Fig. 6.1), and almost all of the genes are targeted by conventional and/or conditional knockout (KO) technology based on the Mouse Genome Informatics (http://www.informatics.jax.org/). Among these KO mice, thus far, all of the published reports were based on the conventional KO approaches. In the following, we focus on the studies characterizing dental/bone phenotypes in several KO mouse models. Major dental/bone/collagen fibril phenotypes in these studies are summarized in Table 6.1. For the soft-tissue phenotypes in the SLRPs KO mice, see the following reviews (Reed and Iozzo 2002; Kao and Liu 2002; Chakravarti 2002).
Although biglycan is structurally quite similar to decorin (56% identity), the dental phenotypes of biglycan KO are very different from those of decorin KO mice though this is not surprising considering their distinct roles (see above). The thickness of the enamel matrix in biglycan KO molars at post-natal day 1 was significantly increased as compared to that in wild-type (WT) control molars with no visible rod formation (Goldberg et al. 2005). This observation was further supported by micro CT analysis that the mineralized enamel volume of 8-week-old biglycan KO in molar crowns was increased as compared to that of WT (Chiu et al. 2012), possibly by regulating amelogenin expression (Goldberg et al. 2005). On the other hand, the enamel matrix in decorin KO molars at post-natal day 1 was almost absent, although no structural difference was detected by the SEM study between decorin KO and WT mice at 6 weeks (Goldberg et al. 2005).
The TEM studies showed that dentin appeared to be porous and poorly mineralized in both biglycan and decorin KO molars. Metadentin in both biglycan KO and decorin KO molars at post-natal day 1 was enlarged as compared to that in WT molars. As compared to WT, the diameter of collagen fibrils in the proximal predentin of biglycan KO molars was smaller, however, significantly larger in the central and distal predentin. The density and spatial organization of collagen fibrils were not altered. On the other hand, the diameter of collagen fibrils in the decorin KO predentin was unchanged compared to that of WT, while decorin KO showed the increased density of collagen fibrils in the distal predentin (Goldberg et al. 2005). These observations suggest that biglycan and decorin play differential roles in dentin and enamel matrix formation as well as biomineralization, which is consistent with our previous studies (Mochida et al. 2009; Parisuthiman et al. 2005).
Among class II SLRPs, fibromodulin KO mice have also been characterized for their dental phenotype. The thickness of enamel in fibromodulin KO neonates at postnatal day 1 was significantly decreased while that of dentin and predentin was unchanged as compared to WT. The diameter of collagen fibrils in molar predentin in fibromodulin KO was significantly larger than that of WT. Ultrastructural analysis in molar dentin revealed that WT dentin showed homogeneously dense structure, while fibromodulin KO exhibited a heterogeneous appearance with hypomineralized electron-lucent areas (Goldberg et al. 2006). Three-week-old fibromodulin KO mice showed an increased size of pulp volume as compared to WT; however, the pulp volume appeared to be decreased and dentin volume was increased in 10-week-old fibromodulin KO mice (Goldberg et al. 2011). These results suggest that fibromodulin may play diverging roles in a mineralized tissue-specific manner or developmental stage-specific manner.
It has been more than 20 years since biglycan KO mice were generated and reported (Xu et al. 1998), demonstrating for the first time that a particular SLRP member exhibited a skeletal phenotype. As mouse biglycan gene is located on the X chromosome, characterization of mouse phenotype has been initially performed in males. Although apparently normal at birth, these mice displayed an age-dependent phenotype characterized by reduced growth rate and decreased bone mass. This may be the first report in which deficiency of a non-collagenous protein leads to a skeletal phenotype that is marked by low bone mass that becomes more obvious with age. Later, the bone phenotype in biglycan female KO mice was characterized upon ovariectomy (Nielsen et al. 2003). The results showed that biglycan deficiency had minimal effects on bone metabolism in females and biglycan deficiency protected trabecular bone loss caused by estrogen depletion, suggesting that there is a gender difference in response to its deficiency.
It has also been reported that using calvarial cells derived from biglycan KO neonatal mice, loss of biglycan caused reduced BMP4 binding to the osteoblast cell surface. This reduction of BMP4 binding resulted in lower sensitivity of BMP4 stimulation and reduced expression of Cbfa1, likely causing poor osteoblast differentiation (Chen et al. 2004). This notion was further supported by our study that responsiveness to BMP4 was enhanced in biglycan overexpressed MC3T3-E1 clones and impaired in biglycan suppressed clones (see above) (Parisuthiman et al. 2005). Later we found that biglycan directly binds BMP2 and its receptor, BMPR1B/ALK6, and enhances and sustains BMP2 signaling suggesting that biglycan may function as a bridge molecule for BMP2 signaling (Mochida et al. 2006). This study showed that biglycan also binds BMP4 and 6, but likely not via direct interaction.
Although decorin KO mice exhibited only mild ultrastructural changes in bone, when both decorin and biglycan were disrupted, bone phenotypes were synergized exhibiting severe osteopenia (Corsi et al. 2002), indicating a redundant function between decorin and biglycan in the biomineralization process in vivo.
More recently, a class IV SLRP member, tsukushin KO mice have been generated, and bone phenotype was reported (Yano et al. 2017). There have been many reports that tsukushin inhibits several signaling molecules including BMP, TGF-β, Wnt, and fibroblast growth factor (FGF) (Ohta et al. 2004, 2011; Morris et al. 2007; Niimori et al. 2012), suggesting the importance of tsukushin in skeletal development. Tsukushin KO exhibited reduced long bone phenotype as compared to WT showing significant decreases in trabecular number and thickness at both 3 and 20 weeks. The thickness of proliferating zone and hypertrophic zone, but not resting zone, in the tsukushin KO growth plate was markedly decreased accompanied by the reduced expression of Sox9 and Runx2 and increased expression of type X collagen and Mmp13. The results suggest that tsukushin plays an important role mainly in the endochondral ossification process.
Taken together, the dental/bone phenotypes of these SLRP KO mice are, overall, consistent with the results by in vitro cell culture studies, suggesting that biglycan in concert with decorin appears to be a major modulator in the assembly of the ECM in mineralized tissues and cell signaling.
4 SLRPs as Therapeutics and Tissue Engineering
As described above, several SLRP members interact with collagens including fibrillar and non-fibrillar collagens (Hocking et al. 1996; Pogany et al. 1994; Schonherr et al. 1995). SLRPs can also bind to growth factors such as TGF-β family, VEGF, PDGF, among others (Baghy et al. 2013; Berendsen et al. 2014; Tiedemann et al. 2005). The binding of decorin and biglycan to TGF-β1, 2, and 3, and TGF-β family members such as BMPs was the first description of SLRP binding to growth factors and their ability to regulate cell signaling (Hildebrand et al. 1994; Yamaguchi et al. 1990). Asporin also binds TGF-β1 and influences the expression of osteogenic markers, which highlights the importance of class I SLRPs on osteogenesis and mineralization (Hildebrand et al. 1994). Their involvement in other signaling pathways independent of TGF-β has been reported as well (Ameye and Young 2002; Hocking et al. 1998; Kresse and Schonherr 2001; Yoon and Halper 2005) including signaling through IGF-1R and EGFR (Aggelidakis et al. 2018; Mohan et al. 2019). Most studies of SLRPs in this field have focused on decorin and biglycan as they interact with various receptors, secreted molecules, and ECM components (Babelova et al. 2009; Desnoyers et al. 2001; Elefteriou et al. 2001; Gendelman et al. 2003; Krumdieck et al. 1992; Mochida et al. 2006; Nadesalingam et al. 2003; Pogany et al. 1994). Through these interactions, they modulate a variety of signaling pathways including Wnt, Smads, and mitogen-activated protein kinase (MAPKs) (Babelova et al. 2009; Schaefer et al. 2005; Wang et al. 2010; Yan et al. 2009). Biglycan, for instance, directly binds BMP2 and its receptors, which enhances BMP2-induced osteoblast differentiation (Mochida et al. 2006; Parisuthiman et al. 2005). This positive effect of biglycan on BMP2 function is derived from the core protein, not the GAG component (Miguez et al. 2011). Further, the addition of recombinant biglycan core protein to a low dose BMP2 significantly accelerated BMP2-induced bone formation in a rodent model of craniofacial bone regeneration (Miguez et al. 2014). In an attempt to identify the effector domain within the biglycan core protein, we recently tested several synthetic peptides that correspond to various domains of biglycan and evaluated their effects on BMP2-induced osteoblast differentiation and mineralization in vitro. The results indicated that LRR2-3 of biglycan core protein significantly enhanced BMP2 osteogenic function (Jongwattanapisan et al. 2018). Since high-dose BMP2 may cause significant adverse side effects (see reviews by Carreira et al. 2014; James et al. 2016), use of the synthetic effector with low-dose BMP2 may provide a means to enhance BMP2-induced bone formation and to minimize the risk of side effects (Jongwattanapisan et al. 2018).
Because of the ability of SLRPs to interact with collagen and other molecules such as growth factors, several research groups have been exploring the potential use of these SLRPs not only for tissue engineering, as described above but also for other therapeutic applications. Decorin and biglycan, for instance, have been explored as antithrombotic molecules by forming a DS proteoglycan-heparin cofactor II complex that inactivates thrombin (Delorme et al. 1998; Whinna et al. 1993).
Due to the ability to delay collagen fibrillogenesis and act as a TGF-β1/2 antagonist, decorin is an attractive therapeutic candidate for anti-scarring treatment (Yamaguchi et al. 1990). Decorin has been tested for corneal wound healing in the form of eye drops or subconjunctival injection prior to and after glaucoma surgery on rabbits showing significantly less scarring (Chouhan et al. 2019; Grisanti et al. 2005; Hill et al. 2018). Other antifibrosis applications have been demonstrated in kidneys, muscle, and lungs through its negative TGF-β regulation (Fukushima et al. 2001; Isaka et al. 1996; Kolb et al. 2001). In mice with epidermolysis bullosa, decorin was used as a TGF-β inhibitor and fibrotic traits were significantly reduced in injured skin (Cianfarani et al. 2019). Decorin has been also investigated in bone-muscle injury models with impaired vascularization by its co-delivery with BMP2 in a collagen hydrogel (Ruehle et al. 2019). The rationale behind the use of decorin was because of its ability to bind TGF-β growth factor and support angiogenesis in vitro.
Biglycan has been studied as a therapeutic in musculoskeletal disorders such as Duchenne muscular dystrophy as it can modulate collagen fibrillogenesis and interact with other proteins to improve muscle function (Young and Fallon 2012). In severe muscular dystrophies, increased levels of biglycan mRNA and protein are detected in muscle with increased fibrosis (Zanotti et al. 2005). Biglycan has been found to bind to alpha- and gamma-sarcoglycan in muscle and regulate their expression which is important for muscle development (Rafii et al. 2006; Zanotti et al. 2005). The non-glycanated form of biglycan has been shown to have a specific function in Wnt signaling in muscle preventing muscle wasting (Amenta et al. 2011; Young and Fallon 2012). The non-glycanated biglycan delivered to dystrophic mice was able to improve muscle health and function (Fallon and Mcnally 2018; Ito et al. 2017).
Biglycan has also been studied as a regulator of angiogenesis during bone fracture repair. In biglycan KO mice, the callus formation is smaller than wild-type showing less cartilage and woven bone, less fibrillar collagens, and diminished vascular endothelial growth factor (Berendsen et al. 2014). The reduced callus size was likely due to Wnt availability affected by the absence of biglycan (Berendsen et al. 2011). Later, it has been reported that, based on the analyses by micro-computed tomography and angiography, biglycan KO mice exhibited fewer and reduced vessel size and volumes as biglycan inhibits endostatin, an anti-angiogenic protein (Myren et al. 2016).
The role of GAG chains in biglycan function is still poorly understood. As described above, biglycan’s positive modulation of BMP2 function is likely derived from the specific LRR domains of its core protein, not GAG components (Miguez et al. 2011, 2014; Jongwattanapisan et al. 2018). The presence of GAGs reduced the ability of biglycan to promote osteogenesis suggesting that GAGs may negatively control the interaction between biglycan and BMP2/its receptors (Jongwattanapisan et al. 2018). A summary of biglycan in proteoglycan versus core versus peptide forms and their interactions with receptors associated with osteogenesis are depicted in Fig. 6.4. Biglycan proteoglycan form (with GAGs) has been implicated in inflammatory events interacting with TLR 2 and 4, and P2X receptors versus non-glycanated forms and peptides favoring interaction with BMP receptors (Fig. 6.4) (Babelova et al. 2009; Hsieh et al. 2014). The effect of bi- versus mono-glycanated forms of biglycan has not been investigated yet.
The proteoglycan form of biglycan (yellow half-moon shape) can be cleaved by proteolytic enzymes (brown Pacman shape) leading to glycanated and non-glycanated peptides (chopped yellow half-moons) (Hou et al. 2007; Johnstone et al. 1993; Roughley et al. 1993). Glycanated form of biglycan (N-terminal region with glycosaminoglycans) may interact preferentially with receptors associated with inflammatory and immune response [i.e., Toll-like receptors (TLR) 2 and 4 and P2X purinoceptor 7/4 (P2X)] (Babelova et al. 2009). Biglycan core or peptides of biglycan composed of mainly leucine-rich repeat (LRR) interact with transforming growth factor (TGF)-β family receptors [bone morphogenetic protein receptor (BMPR) I and II, TGF-βR] and Wnt signaling trait [low-density lipoprotein receptor (LRP) 6/5 and frizzled receptor (FZ)] and bind to BMP molecules (blue boomerang) (Desnoyers et al. 2001; Hildebrand et al. 1994; Mochida et al. 2006; Moreno et al. 2005). Other forms of biglycan such as mono-glycanated (mono-biglycan) and biglycan modified with various types of glycosaminoglycans have not been explored in terms of preferred binding partners. Created with Biorender.com
Fibromodulin has been studied for its role in angiogenesis and wound healing. Recombinant fibromodulin protein-enhanced human endothelial cell function in vitro (Jian et al. 2013) and increased capillary generation in in vivo chick embryo chorioallantoic membrane model (Zheng et al. 2014). In the rat Achilles tendon injury model, fibromodulin gene transfer improved biochemical and histological parameters of tendon injury (Delalande et al. 2015). Injection of fibromodulin protein reduced scar size and increased tensile strength of repaired tissue compared to a steroid treatment by local application in a pig wound model (Jiang et al. 2018). The osteogenic function of fibromodulin was also evaluated by implanting fibroblasts primed with fibromodulin in critical-sized mouse calvarial defects. The results showed that these cells lead to increased bone volume/total volume at 8-weeks post-surgery as compared to control groups. Possibly, fibromodulin is also a viable option for mineralized tissue reconstruction (Li et al. 2016).
Lumican, another SLRP member, also controls collagen fibrillogenesis and interacts with growth factors via its core protein (Rada et al. 1993). Lumican can modulate wound healing and innate immunity by interacting with receptors of immune cells such as macrophages (Shao et al. 2012). Its deficiency, increased expression of receptor activator of nuclear factor kappa-B ligand (RANKL), and elevated number of osteoclasts around teeth (Wang et al. 2014). As a therapeutic, the administration of lumican has a positive effect on epithelial proliferation and migration (Yeh et al. 2005). By applying recombinant lumican on wounded mouse skin, wound healing was enhanced (Liu et al. 2013) possibly by promoting contraction of fibroblasts through the α2β1 integrin. Adenoviral expression of lumican in hypertrophic scarring animal as well as cell models showed the ability of lumican to reduce fibroblast proliferation via binding to α2β1 integrin and subsequent reduction of focal adhesion kinase phosphorylation (Zhao et al. 2016). Gesteira and co-workers designed a peptide mimicking the activity of 13 C-terminal amino acids of lumican and showed that it effectively forms a complex with type I receptor for TGF-β1 and promoted corneal wound healing in mice (Gesteira et al. 2017; Yamanaka et al. 2013).
Much remains to be unveiled for the roles of SLRPs in soft and mineralized tissue maintenance and repair. Nonetheless, the above studies show promise in utilizing these molecules as therapeutics in disease treatments and reconstructive therapies. Further, as these SLRPs are rich in GAGs which can be degraded by proteases in the wounds, they can release GAG-attached peptide fragments which may modulate tissue healing (Peplow 2005). The function of GAGs and their fragments with and without peptides in tissue engineering or therapeutics could also be an important subject for further investigations.
A Perspective
As described in this chapter, SLRPs may function as a modulator of mineralized tissue formation by controlling collagen fibrillogenesis, interacting with specific growth factors and their receptors. To further elucidate the specific roles of SLRP members in the process of mineralization, the generation of ameloblast/odontoblast/cementoblast/osteoblast-specific conditional knockout mice will be very helpful. Due to their multifaceted functions, their therapeutic applications are promising. Further understanding of the function of core versus proteoglycan forms of SLRPs may expand their applications. In addition, the utility of SLRPs, especially their short effector domains, for bone regeneration may advance therapies for bone defects.
References
Ababneh KT, Hall RC, Embery G (1999) The proteoglycans of human cementum: immunohistochemical localization in healthy, periodontally involved and ageing teeth. J Periodontal Res 34:87–96
Aggelidakis J, Berdiaki A, Nikitovic D, Papoutsidakis A, Papachristou DJ, Tsatsakis AM, Tzanakakis GN (2018) Biglycan regulates MG63 osteosarcoma cell growth through a LPR6/beta-catenin/IGFR-IR signaling axis. Front Oncol 8:470
Amenta AR, Yilmaz A, Bogdanovich S, Mckechnie BA, Abedi M, Khurana TS, Fallon JR (2011) Biglycan recruits utrophin to the sarcolemma and counters dystrophic pathology in mdx mice. Proc Natl Acad Sci U S A 108:762–767
Ameye L, Young MF (2002) Mice deficient in small leucine-rich proteoglycans: novel in vivo models for osteoporosis, osteoarthritis, Ehlers-Danlos syndrome, muscular dystrophy, and corneal diseases. Glycobiology 12:107R–116R
Antonsson P, Heinegard D, Oldberg A (1991) Posttranslational modifications of fibromodulin. J Biol Chem 266:16859–16861
Babelova A, Moreth K, Tsalastra-Greul W, Zeng-Brouwers J, Eickelberg O, Young MF, Bruckner P, Pfeilschifter J, Schaefer RM, Grone HJ, Schaefer L (2009) Biglycan, a danger signal that activates the NLRP3 inflammasome via toll-like and P2X receptors. J Biol Chem 284:24035–24048
Baghy K, Horvath Z, Regos E, Kiss K, Schaff Z, Iozzo RV, Kovalszky I (2013) Decorin interferes with platelet-derived growth factor receptor signaling in experimental hepatocarcinogenesis. FEBS J 280:2150–2164
Benoit VM, Fischer JR, Lin YP, Parveen N, Leong JM (2011) Allelic variation of the Lyme disease spirochete adhesin DbpA influences spirochetal binding to decorin, dermatan sulfate, and mammalian cells. Infect Immun 79:3501–3509
Berendsen AD, Fisher LW, Kilts TM, Owens RT, Robey PG, Gutkind JS, Young MF (2011) Modulation of canonical Wnt signaling by the extracellular matrix component biglycan. Proc Natl Acad Sci U S A 108:17022–17027
Berendsen AD, Pinnow EL, Maeda A, Brown AC, Mccartney-Francis N, Kram V, Owens RT, Robey PG, Holmbeck K, De Castro LF, Kilts TM, Young MF (2014) Biglycan modulates angiogenesis and bone formation during fracture healing. Matrix Biol 35:223–231
Bertassoni LE (2017) Dentin on the nanoscale: hierarchical organization, mechanical behavior and bioinspired engineering. Dent Mater 33:637–649
Bonucci E, Gherardi G (1975) Histochemical and electron microscopy investigations on medullary bone. Cell Tissue Res 163:81–97
Boskey AL (1998) Biomineralization: conflicts, challenges, and opportunities. J Cell Biochem 72(Suppl 30–31):83–91
Boskey A, Pleshko Camacho N (2007) FT-IR imaging of native and tissue-engineered bone and cartilage. Biomaterials 28:2465–2478
Bredrup C, Knappskog PM, Majewski J, Rodahl E, Boman H (2005) Congenital stromal dystrophy of the cornea caused by a mutation in the decorin gene. Invest Ophthalmol Vis Sci 46:420–426
Burger C, Zhou HW, Wang H, Sics I, Hsiao BS, Chu B, Graham L, Glimcher MJ (2008) Lateral packing of mineral crystals in bone collagen fibrils. Biophys J 95:1985–1992
Carreira AC, Alves GG, Zambuzzi WF, Sogayar MC, Granjeiro JM (2014) Bone morphogenetic proteins: structure, biological function and therapeutic applications. Arch Biochem Biophys 561:64–73
Chakravarti S (2002) Functions of lumican and fibromodulin: lessons from knockout mice. Glycoconj J 19:287–293
Chakravarti S, Petroll WM, Hassell JR, Jester JV, Lass JH, Paul J, Birk DE (2000) Corneal opacity in lumican-null mice: defects in collagen fibril structure and packing in the posterior stroma. Invest Ophthalmol Vis Sci 41:3365–3373
Chen S, Birk DE (2013) The regulatory roles of small leucine-rich proteoglycans in extracellular matrix assembly. FEBS J 280:2120–2137
Chen XD, Fisher LW, Robey PG, Young MF (2004) The small leucine-rich proteoglycan biglycan modulates BMP-4-induced osteoblast differentiation. FASEB J 18:948–958
Cheng H, Caterson B, Neame PJ, Lester GE, Yamauchi M (1996) Differential distribution of lumican and fibromodulin in tooth cementum. Connect Tissue Res 34:87–96
Cheng H, Caterson B, Yamauchi M (1999) Identification and immunolocalization of chondroitin sulfate proteoglycans in tooth cementum. Connect Tissue Res 40:37–47
Chiu R, Li W, Herber RP, Marshall SJ, Young M, Ho SP (2012) Effects of biglycan on physico-chemical properties of ligament-mineralized tissue attachment sites. Arch Oral Biol 57:177–187
Chouhan G, Moakes RJA, Esmaeili M, Hill LJ, Decogan F, Hardwicke J, Rauz S, Logan A, Grover LM (2019) A self-healing hydrogel eye drop for the sustained delivery of decorin to prevent corneal scarring. Biomaterials 210:41–50
Cianfarani F, De Domenico E, Nystrom A, Mastroeni S, Abeni D, Baldini E, Ulisse S, Uva P, Bruckner-Tuderman L, Zambruno G, Castiglia D, Odorisio T (2019) Decorin counteracts disease progression in mice with recessive dystrophic epidermolysis bullosa. Matrix Biol 81:3–16
Corsi A, Xu T, Chen XD, Boyde A, Liang J, Mankani M, Sommer B, Iozzo RV, Eichstetter I, Robey PG, Bianco P, Young MF (2002) Phenotypic effects of biglycan deficiency are linked to collagen fibril abnormalities, are synergized by decorin deficiency, and mimic Ehlers-Danlos-like changes in bone and other connective tissues. J Bone Miner Res 17:1180–1189
Delalande A, Gosselin MP, Suwalski A, Guilmain W, Leduc C, Berchel M, Jaffres PA, Baril P, Midoux P, Pichon C (2015) Enhanced Achilles tendon healing by fibromodulin gene transfer. Nanomedicine 11:1735–1744
Delorme MA, Xu L, Berry L, Mitchell L, Andrew M (1998) Anticoagulant dermatan sulfate proteoglycan (decorin) in the term human placenta. Thromb Res 90:147–153
De Mattos Pimenta Vidal C, Leme-Kraus AA, Rahman M, Farina AP, Bedran-Russo AK (2017) Role of proteoglycans on the biochemical and biomechanical properties of dentin organic matrix. Arch Oral Biol 82:203–208
Desnoyers L, Arnott D, Pennica D (2001) WISP-1 binds to decorin and biglycan. J Biol Chem 276:47599–47607
Elefteriou F, Exposito JY, Garrone R, Lethias C (2001) Binding of tenascin-X to decorin. FEBS Lett 495:44–47
Embery G, Hall R, Waddington R, Septier D, Goldberg M (2001) Proteoglycans in dentinogenesis. Crit Rev Oral Biol Med 12:331–349
Fallon JR, Mcnally EM (2018) Non-glycanated biglycan and LTBP4: leveraging the extracellular matrix for Duchenne muscular dystrophy therapeutics. Matrix Biol 68–69:616–627
Fisher LW, Termine JD, Dejter SW Jr, Whitson SW, Yanagishita M, Kimura JH, Hascall VC, Kleinman HK, Hassell JR, Nilsson B (1983) Proteoglycans of developing bone. J Biol Chem 258:6588–6594
Fisher LW, Hawkins GR, Tuross N, Termine JD (1987) Purification and partial characterization of small proteoglycans I and II, bone sialoproteins I and II, and osteonectin from the mineral compartment of developing human bone. J Biol Chem 262:9702–9708
Fratzl P, Daxer A (1993) Structural transformation of collagen fibrils in corneal stroma during drying. An x-ray scattering study. Biophys J 64:1210–1214
Fukushima K, Badlani N, Usas A, Riano F, Fu F, Huard J (2001) The use of an antifibrosis agent to improve muscle recovery after laceration. Am J Sports Med 29:394–402
Funderburgh JL (2002) Keratan sulfate biosynthesis. IUBMB Life 54:187–194
Gamsjaeger S, Mendelsohn R, Boskey AL, Gourion-Arsiquaud S, Klaushofer K, Paschalis EP (2014) Vibrational spectroscopic imaging for the evaluation of matrix and mineral chemistry. Curr Osteoporos Rep 12:454–464
Ge G, Seo NS, Liang X, Hopkins DR, Hook M, Greenspan DS (2004) Bone morphogenetic protein-1/tolloid-related metalloproteinases process osteoglycin and enhance its ability to regulate collagen fibrillogenesis. J Biol Chem 279:41626–41633
Gendelman R, Burton-Wurster NI, Macleod JN, Lust G (2003) The cartilage-specific fibronectin isoform has a high affinity binding site for the small proteoglycan decorin. J Biol Chem 278:11175–11181
George A, Veis A (2008) Phosphorylated proteins and control over apatite nucleation, crystal growth, and inhibition. Chem Rev 108:4670–4693
George A, Bannon L, Sabsay B, Dillon JW, Malone J, Veis A, Jenkins NA, Gilbert DJ, Copeland NG (1996) The carboxyl-terminal domain of phosphophoryn contains unique extended triplet amino acid repeat sequences forming ordered carboxyl-phosphate interaction ridges that may be essential in the biomineralization process. J Biol Chem 271:32869–32873
Georgiadis M, Muller R, Schneider P (2016) Techniques to assess bone ultrastructure organization: orientation and arrangement of mineralized collagen fibrils. J R Soc Interface 13
Gesteira TF, Coulson-Thomas VJ, Yuan Y, Zhang J, Nader HB, Kao WW (2017) Lumican peptides: rational design targeting ALK5/TGFBRI. Sci Rep 7:42057
Glimcher MJ (1984) Recent studies of the mineral phase in bone and its possible linkage to the organic matrix by protein-bound phosphate bonds. Philos Trans R Soc Lond B Biol Sci 304:479–508
Goldberg M, Septier DS (1992) Differential staining of glycosaminoglycans in the predentine and dentine of rat incisor using cuprolinic blue at various magnesium chloride concentrations. Histochem J 24:648–654
Goldberg M, Takagi M (1993) Dentine proteoglycans: composition, ultrastructure and functions. Histochem J 25:781–806
Goldberg M, Rapoport O, Septier D, Palmier K, Hall R, Embery G, Young M, Ameye L (2003) Proteoglycans in predentin: the last 15 micrometers before mineralization. Connect Tissue Res 44(Suppl 1):184–188
Goldberg M, Septier D, Rapoport O, Iozzo RV, Young MF, Ameye LG (2005) Targeted disruption of two small leucine-rich proteoglycans, biglycan and decorin, excerpts divergent effects on enamel and dentin formation. Calcif Tissue Int 77:297–310
Goldberg M, Septier D, Oldberg A, Young MF, Ameye LG (2006) Fibromodulin-deficient mice display impaired collagen fibrillogenesis in predentin as well as altered dentin mineralization and enamel formation. J Histochem Cytochem 54:525–537
Goldberg M, Ono M, Septier D, Bonnefoix M, Kilts TM, Bi Y, Embree M, Ameye L, Young MF (2009) Fibromodulin-deficient mice reveal dual functions for fibromodulin in regulating dental tissue and alveolar bone formation. Cells Tissues Organs 189:198–202
Goldberg M, Marchadier A, Vidal C, Harichane Y, Kamoun-Goldrat A, Kellermann O, Kilts T, Young M (2011) Differential effects of fibromodulin deficiency on mouse mandibular bones and teeth: a micro-CT time course study. Cells Tissues Organs 194:205–210
Grisanti S, Szurman P, Warga M, Kaczmarek R, Ziemssen F, Tatar O, Bartz-Schmidt KU (2005) Decorin modulates wound healing in experimental glaucoma filtration surgery: a pilot study. Invest Ophthalmol Vis Sci 46:191–196
Guindon S, Gascuel O (2003) A simple, fast, and accurate algorithm to estimate large phylogenies by maximum likelihood. Syst Biol 52:696–704
Hall RC, Embery G (1997) The use of immunohistochemistry in understanding the structure and function of the extracellular matrix of dental tissues. Adv Dent Res 11:478–486
Hall RC, Embery G, Lloyd D (1997) Immunochemical localization of the small leucine-rich proteoglycan lumican in human predentine and dentine. Arch Oral Biol 42:783–786
He G, George A (2004) Dentin matrix protein 1 immobilized on type I collagen fibrils facilitates apatite deposition in vitro. J Biol Chem 279:11649–11656
Hedlund H, Mengarelli-Widholm S, Heinegard D, Reinholt FP, Svensson O (1994) Fibromodulin distribution and association with collagen. Matrix Biol 14:227–232
Hildebrand A, Romaris M, Rasmussen LM, Heinegard D, Twardzik DR, Border WA, Ruoslahti E (1994) Interaction of the small interstitial proteoglycans biglycan, decorin and fibromodulin with transforming growth factor beta. Biochem J 302(Pt 2):527–534
Hill LJ, Moakes RJA, Vareechon C, Butt G, Ng A, Brock K, Chouhan G, Vincent RC, Abbondante S, Williams RL, Barnes NM, Pearlman E, Wallace GR, Rauz S, Logan A, Grover LM (2018) Sustained release of decorin to the surface of the eye enables scarless corneal regeneration. NPJ Regen Med 3:23
Hocking AM, Strugnell RA, Ramamurthy P, Mcquillan DJ (1996) Eukaryotic expression of recombinant biglycan. Post-translational processing and the importance of secondary structure for biological activity. J Biol Chem 271:19571–19577
Hocking AM, Shinomura T, Mcquillan DJ (1998) Leucine-rich repeat glycoproteins of the extracellular matrix. Matrix Biol 17:1–19
Hoshi K, Kemmotsu S, Takeuchi Y, Amizuka N, Ozawa H (1999) The primary calcification in bones follows removal of decorin and fusion of collagen fibrils. J Bone Miner Res 14:273–280
Hoshi K, Ejiri S, Ozawa H (2001) Localizational alterations of calcium, phosphorus, and calcification-related organics such as proteoglycans and alkaline phosphatase during bone calcification. J Bone Miner Res 16:289–298
Hou S, Maccarana M, Min TH, Strate I, Pera EM (2007) The secreted serine protease xHtrA1 stimulates long-range FGF signaling in the early Xenopus embryo. Dev Cell 13:226–241
Hsieh LT, Nastase MV, Zeng-Brouwers J, Iozzo RV, Schaefer L (2014) Soluble biglycan as a biomarker of inflammatory renal diseases. Int J Biochem Cell Biol 54:223–235
Huang R, Liu J, Sharp JS (2013) An approach for separation and complete structural sequencing of heparin/heparan sulfate-like oligosaccharides. Anal Chem 85:5787–5795
Hyllested JL, Veje K, Ostergaard K (2002) Histochemical studies of the extracellular matrix of human articular cartilage—a review. Osteoarthritis Cartilage 10:333–343
Iozzo RV, Murdoch AD (1996) Proteoglycans of the extracellular environment: clues from the gene and protein side offer novel perspectives in molecular diversity and function. FASEB J 10:598–614
Iozzo RV, Schaefer L (2015) Proteoglycan form and function: a comprehensive nomenclature of proteoglycans. Matrix Biol 42:11–55
Isaka Y, Brees DK, Ikegaya K, Kaneda Y, Imai E, Noble NA, Border WA (1996) Gene therapy by skeletal muscle expression of decorin prevents fibrotic disease in rat kidney. Nat Med 2:418–423
Ito M, Ehara Y, Li J, Inada K, Ohno K (2017) Protein-anchoring therapy of biglycan for Mdx mouse model of duchenne muscular dystrophy. Hum Gene Ther 28:428–436
James AW, Lachaud G, Shen J, Asatrian G, Nguyen V, Zhang X, Ting K, Soo C (2016) A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng Part B Rev 22:284–297
Jepsen KJ, Wu F, Peragallo JH, Paul J, Roberts L, Ezura Y, Oldberg A, Birk DE, Chakravarti S (2002) A syndrome of joint laxity and impaired tendon integrity in lumican- and fibromodulin-deficient mice. J Biol Chem 277:35532–35540
Jian J, Zheng Z, Zhang K, Rackohn TM, Hsu C, Levin A, Enjamuri DR, Zhang X, Ting K, Soo C (2013) Fibromodulin promoted in vitro and in vivo angiogenesis. Biochem Biophys Res Commun 436:530–535
Jiang W, Ting K, Lee S, Zara JN, Song R, Li C, Chen E, Zhang X, Zhao Z, Soo C, Zheng Z (2018) Fibromodulin reduces scar size and increases scar tensile strength in normal and excessive-mechanical-loading porcine cutaneous wounds. J Cell Mol Med 22:2510–2513
Jing Y, Kumar PR, Zhu L, Edward DP, Tao S, Wang L, Chuck R, Zhang C (2014) Novel decorin mutation in a Chinese family with congenital stromal corneal dystrophy. Cornea 33:288–293
Johnstone B, Markopoulos M, Neame P, Caterson B (1993) Identification and characterization of glycanated and non-glycanated forms of biglycan and decorin in the human intervertebral disc. Biochem J 292(Pt 3):661–666
Jongwattanapisan P, Terajima M, Miguez PA, Querido W, Nagaoka H, Sumida N, Gurysh EG, Ainslie KM, Pleshko N, Perera L, Yamauchi M (2018) Identification of the effector domain of biglycan that facilitates BMP-2 osteogenic function. Sci Rep 8:7022
Kalamajski S, Oldberg A (2007) Fibromodulin binds collagen type I via Glu-353 and Lys-355 in leucine-rich repeat 11. J Biol Chem 282:26740–26745
Kalamajski S, Oldberg A (2009) Homologous sequence in lumican and fibromodulin leucine-rich repeat 5-7 competes for collagen binding. J Biol Chem 284:534–539
Kalamajski S, Aspberg A, Oldberg A (2007) The decorin sequence SYIRIADTNIT binds collagen type I. J Biol Chem 282:16062–16067
Kao WW, Liu CY (2002) Roles of lumican and keratocan on corneal transparency. Glycoconj J 19:275–285
Karamanos NK, Piperigkou Z, Theocharis AD, Watanabe H, Franchi M, Baud S, Brezillon S, Gotte M, Passi A, Vigetti D, Ricard-Blum S, Sanderson RD, Neill T, Iozzo RV (2018) Proteoglycan chemical diversity drives multifunctional cell regulation and therapeutics. Chem Rev 118:9152–9232
Karousou E, Asimakopoulou A, Monti L, Zafeiropoulou V, Afratis N, Gartaganis P, Rossi A, Passi A, Karamanos NK (2014) FACE analysis as a fast and reliable methodology to monitor the sulfation and total amount of chondroitin sulfate in biological samples of clinical importance. Molecules 19:7959–7980
Katz EP, Li ST (1973) The intermolecular space of reconstituted collagen fibrils. J Mol Biol 73:351–369
Kessler E, Takahara K, Biniaminov L, Brusel M, Greenspan DS (1996) Bone morphogenetic protein-1: the type I procollagen C-proteinase. Science 271:360–362
Khanarian NT, Boushell MK, Spalazzi JP, Pleshko N, Boskey AL, Lu HH (2014) FTIR-I compositional mapping of the cartilage-to-bone interface as a function of tissue region and age. J Bone Miner Res 29:2643–2652
Kim JW, Simmer JP (2007) Hereditary dentin defects. J Dent Res 86:392–399
Kizawa H, Kou I, Iida A, Sudo A, Miyamoto Y, Fukuda A, Mabuchi A, Kotani A, Kawakami A, Yamamoto S, Uchida A, Nakamura K, Notoya K, Nakamura Y, Ikegawa S (2005) An aspartic acid repeat polymorphism in asporin inhibits chondrogenesis and increases susceptibility to osteoarthritis. Nat Genet 37:138–144
Kolb M, Margetts PJ, Sime PJ, Gauldie J (2001) Proteoglycans decorin and biglycan differentially modulate TGF-beta-mediated fibrotic responses in the lung. Am J Physiol Lung Cell Mol Physiol 280:L1327–L1334
Kram V, Shainer R, Jani P, Meester JAN, Loeys B, Young MF (2020) Biglycan in the Skeleton. J Histochem Cytochem 68:747–762
Kresse H, Schonherr E (2001) Proteoglycans of the extracellular matrix and growth control. J Cell Physiol 189:266–274
Krumdieck R, Hook M, Rosenberg LC, Volanakis JE (1992) The proteoglycan decorin binds C1q and inhibits the activity of the C1 complex. J Immunol 149:3695–3701
Krusius T, Ruoslahti E (1986) Primary structure of an extracellular matrix proteoglycan core protein deduced from cloned cDNA. Proc Natl Acad Sci U S A 83:7683–7687
Kubaski F, Osago H, Mason RW, Yamaguchi S, Kobayashi H, Tsuchiya M, Orii T, Tomatsu S (2017) Glycosaminoglycans detection methods: applications of mass spectrometry. Mol Genet Metab 120:67–77
Landis WJ, Song MJ, Leith A, Mcewen L, Mcewen BF (1993) Mineral and organic matrix interaction in normally calcifying tendon visualized in three dimensions by high-voltage electron microscopic tomography and graphic image reconstruction. J Struct Biol 110:39–54
Landis WJ, Hodgens KJ, Arena J, Song MJ, Mcewen BF (1996) Structural relations between collagen and mineral in bone as determined by high voltage electron microscopic tomography. Microsc Res Tech 33:192–202
Li SW, Sieron AL, Fertala A, Hojima Y, Arnold WV, Prockop DJ (1996) The C-proteinase that processes procollagens to fibrillar collagens is identical to the protein previously identified as bone morphogenic protein-1. Proc Natl Acad Sci U S A 93:5127–5130
Li CS, Yang P, Ting K, Aghaloo T, Lee S, Zhang Y, Khalilinejad K, Murphy MC, Pan HC, Zhang X, Wu B, Zhou YH, Zhao Z, Zheng Z, Soo C (2016) Fibromodulin reprogrammed cells: a novel cell source for bone regeneration. Biomaterials 83:194–206
Liu XJ, Kong FZ, Wang YH, Zheng JH, Wan WD, Deng CL, Mao GY, Li J, Yang XM, Zhang YL, Zhang XL, Yang SL, Zhang ZG (2013) Lumican accelerates wound healing by enhancing alpha2beta1 integrin-mediated fibroblast contractility. PLoS One 8:e67124
Lormee P, Septier D, Lecolle S, Baudoin C, Goldberg M (1996) Dual incorporation of (35S)sulfate into dentin proteoglycans acting as mineralization promotors in rat molars and predentin proteoglycans. Calcif Tissue Int 58:368–375
Maccarana M, Svensson RB, Knutsson A, Giannopoulos A, Pelkonen M, Weis M, Eyre D, Warman M, Kalamajski S (2017) Asporin-deficient mice have tougher skin and altered skin glycosaminoglycan content and structure. PLoS One 12:e0184028
Mahamid J, Aichmayer B, Shimoni E, Ziblat R, Li C, Siegel S, Paris O, Fratzl P, Weiner S, Addadi L (2010) Mapping amorphous calcium phosphate transformation into crystalline mineral from the cell to the bone in zebrafish fin rays. Proc Natl Acad Sci U S A 107:6316–6321
Matias MA, Li H, Young WG, Bartold PM (2003) Immunohistochemical localization of fibromodulin in the periodontium during cementogenesis and root formation in the rat molar. J Periodontal Res 38:502–507
Matsushima N, Ohyanagi T, Tanaka T, Kretsinger RH (2000) Super-motifs and evolution of tandem leucine-rich repeats within the small proteoglycans—biglycan, decorin, lumican, fibromodulin, PRELP, keratocan, osteoadherin, epiphycan, and osteoglycin. Proteins 38:210–225
Mcewan PA, Scott PG, Bishop PN, Bella J (2006) Structural correlations in the family of small leucine-rich repeat proteins and proteoglycans. J Struct Biol 155:294–305
Miguez PA, Terajima M, Nagaoka H, Mochida Y, Yamauchi M (2011) Role of glycosaminoglycans of biglycan in BMP-2 signaling. Biochem Biophys Res Commun 405:262–266
Miguez PA, Terajima M, Nagaoka H, Ferreira JA, Braswell K, Ko CC, Yamauchi M (2014) Recombinant biglycan promotes bone morphogenetic protein-induced osteogenesis. J Dent Res 93:406–411
Mochida Y, Duarte WR, Tanzawa H, Paschalis EP, Yamauchi M (2003) Decorin modulates matrix mineralization in vitro. Biochem Biophys Res Commun 305:6–9
Mochida Y, Parisuthiman D, Yamauchi M (2006) Biglycan is a positive modulator of BMP-2 induced osteoblast differentiation. Adv Exp Med Biol 585:101–113
Mochida Y, Parisuthiman D, Pornprasertsuk-Damrongsri S, Atsawasuwan P, Sricholpech M, Boskey AL, Yamauchi M (2009) Decorin modulates collagen matrix assembly and mineralization. Matrix Biol 28:44–52
Mohan RR, Tripathi R, Sharma A, Sinha PR, Giuliano EA, Hesemann NP, Chaurasia SS (2019) Decorin antagonizes corneal fibroblast migration via caveolae-mediated endocytosis of epidermal growth factor receptor. Exp Eye Res 180:200–207
Moreno M, Munoz R, Aroca F, Labarca M, Brandan E, Larrain J (2005) Biglycan is a new extracellular component of the Chordin-BMP4 signaling pathway. EMBO J 24:1397–1405
Morris SA, Almeida AD, Tanaka H, Ohta K, Ohnuma S (2007) Tsukushi modulates Xnr2, FGF and BMP signaling: regulation of Xenopus germ layer formation. PLoS One 2:e1004
Myren M, Kirby DJ, Noonan ML, Maeda A, Owens RT, Ricard-Blum S, Kram V, Kilts TM, Young MF (2016) Biglycan potentially regulates angiogenesis during fracture repair by altering expression and function of endostatin. Matrix Biol 52–54:141–150
Nadesalingam J, Bernal AL, Dodds AW, Willis AC, Mahoney DJ, Day AJ, Reid KB, Palaniyar N (2003) Identification and characterization of a novel interaction between pulmonary surfactant protein D and decorin. J Biol Chem 278:25678–25687
Nielsen KL, Allen MR, Bloomfield SA, Andersen TL, Chen XD, Poulsen HS, Young MF, Heegaard AM (2003) Biglycan deficiency interferes with ovariectomy-induced bone loss. J Bone Miner Res 18:2152–2158
Niimori D, Kawano R, Felemban A, Niimori-Kita K, Tanaka H, Ihn H, Ohta K (2012) Tsukushi controls the hair cycle by regulating TGF-beta1 signaling. Dev Biol 372:81–87
Nikdin H, Olsson ML, Hultenby K, Sugars RV (2012) Osteoadherin accumulates in the predentin towards the mineralization front in the developing tooth. PLoS One 7:e31525
Nikitovic D, Aggelidakis J, Young MF, Iozzo RV, Karamanos NK, Tzanakakis GN (2012) The biology of small leucine-rich proteoglycans in bone pathophysiology. J Biol Chem 287:33926–33933
Nudelman F, Pieterse K, George A, Bomans PH, Friedrich H, Brylka LJ, Hilbers PA, De With G, Sommerdijk NA (2010) The role of collagen in bone apatite formation in the presence of hydroxyapatite nucleation inhibitors. Nat Mater 9:1004–1009
Ohta K, Lupo G, Kuriyama S, Keynes R, Holt CE, Harris WA, Tanaka H, Ohnuma SI (2004) Tsukushi functions as an organizer inducer by inhibition of BMP activity in cooperation with chordin. Dev Cell 7:347–358
Ohta K, Ito A, Kuriyama S, Lupo G, Kosaka M, Ohnuma S, Nakagawa S, Tanaka H (2011) Tsukushi functions as a Wnt signaling inhibitor by competing with Wnt2b for binding to transmembrane protein Frizzled4. Proc Natl Acad Sci U S A 108:14962–14967
Onnerfjord P, Heathfield TF, Heinegard D (2004) Identification of tyrosine sulfation in extracellular leucine-rich repeat proteins using mass spectrometry. J Biol Chem 279:26–33
Orsini G, Ruggeri A Jr, Mazzoni A, Papa V, Mazzotti G, Di Lenarda R, Breschi L (2007) Immunohistochemical identification of decorin and biglycan in human dentin: a correlative field emission scanning electron microscopy/transmission electron microscopy study. Calcif Tissue Int 81:39–45
Parisuthiman D, Mochida Y, Duarte WR, Yamauchi M (2005) Biglycan modulates osteoblast differentiation and matrix mineralization. J Bone Miner Res 20:1878–1886
Paschalis EP, Gamsjaeger S, Klaushofer K (2017) Vibrational spectroscopic techniques to assess bone quality. Osteoporos Int 28:2275–2291
Peplow PV (2005) Glycosaminoglycan: a candidate to stimulate the repair of chronic wounds. Thromb Haemost 94:4–16
Pogany G, Hernandez DJ, Vogel KG (1994) The in vitro interaction of proteoglycans with type I collagen is modulated by phosphate. Arch Biochem Biophys 313:102–111
Quan BD, Sone ED (2015) Structural changes in collagen fibrils across a mineralized interface revealed by cryo-TEM. Bone 77:42–49
Rada JA, Cornuet PK, Hassell JR (1993) Regulation of corneal collagen fibrillogenesis in vitro by corneal proteoglycan (lumican and decorin) core proteins. Exp Eye Res 56:635–648
Rafii MS, Hagiwara H, Mercado ML, Seo NS, Xu T, Dugan T, Owens RT, Hook M, Mcquillan DJ, Young MF, Fallon JR (2006) Biglycan binds to alpha- and gamma-sarcoglycan and regulates their expression during development. J Cell Physiol 209:439–447
Randilini A, Fujikawa K, Shibata S (2020) Expression, localization and synthesis of small leucine-rich proteoglycans in developing mouse molar tooth germ. Eur J Histochem 64
Raspanti M, Viola M, Forlino A, Tenni R, Gruppi C, Tira ME (2008) Glycosaminoglycans show a specific periodic interaction with type I collagen fibrils. J Struct Biol 164:134–139
Reed CC, Iozzo RV (2002) The role of decorin in collagen fibrillogenesis and skin homeostasis. Glycoconj J 19:249–255
Rehn AP, Cerny R, Sugars RV, Kaukua N, Wendel M (2008) Osteoadherin is upregulated by mature osteoblasts and enhances their in vitro differentiation and mineralization. Calcif Tissue Int 82:454–464
Roch C, Kuhn J, Kleesiek K, Gotting C (2010) Differences in gene expression of human xylosyltransferases and determination of acceptor specificities for various proteoglycans. Biochem Biophys Res Commun 391:685–691
Rodahl E, Van Ginderdeuren R, Knappskog PM, Bredrup C, Boman H (2006) A second decorin frame shift mutation in a family with congenital stromal corneal dystrophy. Am J Ophthalmol 142:520–521
Roughley PJ, White RJ, Magny MC, Liu J, Pearce RH, Mort JS (1993) Non-proteoglycan forms of biglycan increase with age in human articular cartilage. Biochem J 295(Pt 2):421–426
Ruehle MA, Li MA, Cheng A, Krishnan L, Willett NJ, Guldberg RE (2019) Decorin-supplemented collagen hydrogels for the co-delivery of bone morphogenetic protein-2 and microvascular fragments to a composite bone-muscle injury model with impaired vascularization. Acta Biomater 93:210–221
Ruhland C, Schonherr E, Robenek H, Hansen U, Iozzo RV, Bruckner P, Seidler DG (2007) The glycosaminoglycan chain of decorin plays an important role in collagen fibril formation at the early stages of fibrillogenesis. FEBS J 274:4246–4255
Sarathchandra P, Cassella JP, Ali SY (2002) Ultrastructural localization of proteoglycans in bone in osteogenesis imperfecta as demonstrated by Cuprolinic Blue staining. J Bone Miner Metab 20:288–293
Schaefer L, Babelova A, Kiss E, Hausser HJ, Baliova M, Krzyzankova M, Marsche G, Young MF, Mihalik D, Gotte M, Malle E, Schaefer RM, Grone HJ (2005) The matrix component biglycan is proinflammatory and signals through Toll-like receptors 4 and 2 in macrophages. J Clin Invest 115:2223–2233
Schonherr E, Witsch-Prehm P, Harrach B, Robenek H, Rauterberg J, Kresse H (1995) Interaction of biglycan with type I collagen. J Biol Chem 270:2776–2783
Schwarcz HP (2015) The ultrastructure of bone as revealed in electron microscopy of ion-milled sections. Semin Cell Dev Biol 46:44–50
Scott JE (1972) Histochemistry of Alcian blue. 3. The molecular biological basis of staining by Alcian blue 8GX and analogous phthalocyanins. Histochemie 32:191–212
Scott IC, Imamura Y, Pappano WN, Troedel JM, Recklies AD, Roughley PJ, Greenspan DS (2000) Bone morphogenetic protein-1 processes probiglycan. J Biol Chem 275:30504–30511
Scott PG, Mcewan PA, Dodd CM, Bergmann EM, Bishop PN, Bella J (2004) Crystal structure of the dimeric protein core of decorin, the archetypal small leucine-rich repeat proteoglycan. Proc Natl Acad Sci U S A 101:15633–15638
Seo NS, Hocking AM, Hook M, Mcquillan DJ (2005) Decorin core protein secretion is regulated by N-linked oligosaccharide and glycosaminoglycan additions. J Biol Chem 280:42774–42784
Septier D, Hall RC, Embery G, Goldberg M (2001) Immunoelectron microscopic visualization of pro- and secreted forms of decorin and biglycan in the predentin and during dentin formation in the rat incisor. Calcif Tissue Int 69:38–45
Shao H, Lee S, Gae-Scott S, Nakata C, Chen S, Hamad AR, Chakravarti S (2012) Extracellular matrix lumican promotes bacterial phagocytosis, and Lum-/- mice show increased Pseudomonas aeruginosa lung infection severity. J Biol Chem 287:35860–35872
Silver FH, Landis WJ (2011) Deposition of apatite in mineralizing vertebrate extracellular matrices: a model of possible nucleation sites on type I collagen. Connect Tissue Res 52:242–254
Sudo H, Kodama HA, Amagai Y, Yamamoto S, Kasai S (1983) In vitro differentiation and calcification in a new clonal osteogenic cell line derived from newborn mouse calvaria. J Cell Biol 96:191–198
Svensson L, Heinegard D, Oldberg A (1995) Decorin-binding sites for collagen type I are mainly located in leucine-rich repeats 4-5. J Biol Chem 270:20712–20716
Svensson L, Aszodi A, Reinholt FP, Fassler R, Heinegard D, Oldberg A (1999) Fibromodulin-null mice have abnormal collagen fibrils, tissue organization, and altered lumican deposition in tendon. J Biol Chem 274:9636–9647
Svensson L, Narlid I, Oldberg A (2000) Fibromodulin and lumican bind to the same region on collagen type I fibrils. FEBS Lett 470:178–182
Takagi M, Hishikawa H, Hosokawa Y, Kagami A, Rahemtulla F (1990) Immunohistochemical localization of glycosaminoglycans and proteoglycans in predentin and dentin of rat incisors. J Histochem Cytochem 38:319–324
Tashima T, Nagatoishi S, Sagara H, Ohnuma S, Tsumoto K (2015) Osteomodulin regulates diameter and alters shape of collagen fibrils. Biochem Biophys Res Commun 463:292–296
Tashima T, Nagatoishi S, Caaveiro JMM, Nakakido M, Sagara H, Kusano-Arai O, Iwanari H, Mimuro H, Hamakubo T, Ohnuma SI, Tsumoto K (2018) Molecular basis for governing the morphology of type-I collagen fibrils by Osteomodulin. Commun Biol 1:33
Tice LW, Barrnett RJ (1965) Diazophthalocyanins as reagents for fine structural cytochemistry. J Cell Biol 25:23–41
Tiedemann K, Olander B, Eklund E, Todorova L, Bengtsson M, Maccarana M, Westergren-Thorsson G, Malmstrom A (2005) Regulation of the chondroitin/dermatan fine structure by transforming growth factor-beta1 through effects on polymer-modifying enzymes. Glycobiology 15:1277–1285
Traub W, Arad T, Weiner S (1992) Origin of mineral crystal growth in collagen fibrils. Matrix 12:251–255
Uzel MI, Scott IC, Babakhanlou-Chase H, Palamakumbura AH, Pappano WN, Hong HH, Greenspan DS, Trackman PC (2001) Multiple bone morphogenetic protein 1-related mammalian metalloproteinases process pro-lysyl oxidase at the correct physiological site and control lysyl oxidase activation in mouse embryo fibroblast cultures. J Biol Chem 276:22537–22543
Vallet SD, Clerc O, Ricard-Blum S (2020) Glycosaminoglycan-protein interactions: the first draft of the glycosaminoglycan interactome. J Histochem Cytochem 69(2):93–104
Von Marschall Z, Fisher LW (2010) Decorin is processed by three isoforms of bone morphogenetic protein-1 (BMP1). Biochem Biophys Res Commun 391:1374–1378
Waddington RJ, Hall RC, Embery G, Lloyd DM (2003) Changing profiles of proteoglycans in the transition of predentine to dentine. Matrix Biol 22:153–161
Wang D, Christensen K, Chawla K, Xiao G, Krebsbach PH, Franceschi RT (1999) Isolation and characterization of MC3T3-E1 preosteoblast subclones with distinct in vitro and in vivo differentiation/mineralization potential. J Bone Miner Res 14:893–903
Wang X, Harimoto K, Xie S, Cheng H, Liu J, Wang Z (2010) Matrix protein biglycan induces osteoblast differentiation through extracellular signal-regulated kinase and Smad pathways. Biol Pharm Bull 33:1891–1897
Wang Y, Azais T, Robin M, Vallee A, Catania C, Legriel P, Pehau-Arnaudet G, Babonneau F, Giraud-Guille MM, Nassif N (2012) The predominant role of collagen in the nucleation, growth, structure and orientation of bone apatite. Nat Mater 11:724–733
Wang L, Foster BL, Kram V, Nociti FH Jr, Zerfas PM, Tran AB, Young MF, Somerman MJ (2014) Fibromodulin and biglycan modulate periodontium through TGFbeta/BMP signaling. J Dent Res 93:780–787
Weiner S, Traub W (1986) Organization of hydroxyapatite crystals within collagen fibrils. FEBS Lett 206:262–266
Whinna HC, Choi HU, Rosenberg LC, Church FC (1993) Interaction of heparin cofactor II with biglycan and decorin. J Biol Chem 268:3920–3924
Xu T, Bianco P, Fisher LW, Longenecker G, Smith E, Goldstein S, Bonadio J, Boskey A, Heegaard AM, Sommer B, Satomura K, Dominguez P, Zhao C, Kulkarni AB, Robey PG, Young MF (1998) Targeted disruption of the biglycan gene leads to an osteoporosis-like phenotype in mice. Nat Genet 20:78–82
Xu Y, Nudelman F, Eren ED, Wirix MJM, Cantaert B, Nijhuis WH, Hermida-Merino D, Portale G, Bomans PHH, Ottmann C, Friedrich H, Bras W, Akiva A, Orgel J, Meldrum FC, Sommerdijk N (2020) Intermolecular channels direct crystal orientation in mineralized collagen. Nat Commun 11:5068
Yamaguchi Y, Mann DM, Ruoslahti E (1990) Negative regulation of transforming growth factor-beta by the proteoglycan decorin. Nature 346:281–284
Yamanaka O, Yuan Y, Coulson-Thomas VJ, Gesteira TF, Call MK, Zhang Y, Zhang J, Chang SH, Xie C, Liu CY, Saika S, Jester JV, Kao WW (2013) Lumican binds ALK5 to promote epithelium wound healing. PLoS One 8:e82730
Yamauchi M, Katz EP (1993) The post-translational chemistry and molecular packing of mineralizing tendon collagens. Connect Tissue Res 29:81–98
Yamauchi M, Uzawa K, Katz EP, Lopes M, Verdelis K, Cheng H (2000) Distribution of small keratan sulfate proteoglycans in predentin and dentin. In: Goldberg M, Boskey A, Robinson C (eds) Proceedings of the interantonal conference on chemistry and biology of mineralized tissues. American Academy of Orthopaedic Surgeons, pp 305–310
Yan W, Wang P, Zhao CX, Tang J, Xiao X, Wang DW (2009) Decorin gene delivery inhibits cardiac fibrosis in spontaneously hypertensive rats by modulation of transforming growth factor-beta/Smad and p38 mitogen-activated protein kinase signaling pathways. Hum Gene Ther 20:1190–1200
Yano K, Washio K, Tsumanuma Y, Yamato M, Ohta K, Okano T, Izumi Y (2017) The role of Tsukushi (TSK), a small leucine-rich repeat proteoglycan, in bone growth. Regen Ther 7:98–107
Yeh LK, Chen WL, Li W, Espana EM, Ouyang J, Kawakita T, Kao WW, Tseng SC, Liu CY (2005) Soluble lumican glycoprotein purified from human amniotic membrane promotes corneal epithelial wound healing. Invest Ophthalmol Vis Sci 46:479–486
Yoon JH, Halper J (2005) Tendon proteoglycans: biochemistry and function. J Musculoskelet Neuronal Interact 5:22–34
Young MF, Fallon JR (2012) Biglycan: a promising new therapeutic for neuromuscular and musculoskeletal diseases. Curr Opin Genet Dev 22:398–400
Zanotti S, Negri T, Cappelletti C, Bernasconi P, Canioni E, Di Blasi C, Pegoraro E, Angelini C, Ciscato P, Prelle A, Mantegazza R, Morandi L, Mora M (2005) Decorin and biglycan expression is differentially altered in several muscular dystrophies. Brain 128:2546–2555
Zappia J, Joiret M, Sanchez C, Lambert C, Geris L, Muller M, Henrotin Y (2020) From translation to protein degradation as mechanisms for regulating biological functions: a review on the SLRP family in skeletal tissues. Biomolecules 10
Zhao Y, Li X, Xu X, He Z, Cui L, Lv X (2016) Lumican alleviates hypertrophic scarring by suppressing integrin-FAK signaling. Biochem Biophys Res Commun 480:153–159
Zheng Z, Jian J, Velasco O, Hsu CY, Zhang K, Levin A, Murphy M, Zhang X, Ting K, Soo C (2014) Fibromodulin enhances angiogenesis during cutaneous wound healing. Plast Reconstr Surg Glob Open 2:e275
Zhou HW, Burger C, Wang H, Hsiao BS, Chu B, Graham L (2016) The supramolecular structure of bone: X-ray scattering analysis and lateral structure modeling. Acta Crystallogr D Struct Biol 72:986–996
Acknowledgments
Fundings—Boston University Henry Goldman School of Dental Medicine (YM), NIH/NIDCR R03DE028035 and NIH CTSA – NCTraCs 550KR211924 (PM) and the University of North Carolina at Chapel Hill Adams School of Dentistry (MY).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mochida, Y., Miguez, P., Yamauchi, M. (2021). Small Leucine-Rich Proteoglycans (SLRPs) and Biomineralization. In: Goldberg, M., Den Besten, P. (eds) Extracellular Matrix Biomineralization of Dental Tissue Structures. Biology of Extracellular Matrix, vol 10. Springer, Cham. https://doi.org/10.1007/978-3-030-76283-4_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-76283-4_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-76282-7
Online ISBN: 978-3-030-76283-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)