Abstract
Spirometry is a fundamental test in the diagnosis of lung disease in children, including preschool children. It measures the amount (volume) and speed (flow) of air that can be inhaled and exhaled by the patient. The FVC (forced vital capacity) maneuver is the total amount of air exhaled forcefully following a maximal inhalation, and it is usually the only one performed. The FEV1 (Forced Expiratory Volume in one second) describes the speed (flow) of air exhaled in the first second of the expiratory phase of FVC maneuvers. FVC, FEV1, and the FEV1/FVC ratio are the essential data to evaluate the flow/volume curve of spirometry and differentiate normal, obstructive, restrictive, or mixed (obstructive/restrictive) spirometry patterns. Every anesthesiologist and surgeon must be familiar with spirometry data, essential in ascertaining preoperative lung function and in the follow-up of the patient after the surgical procedure, particularly in the case of thoracic surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Spirometry
- Lung function
- Bronchial hyperreactivity
- Bronchodilator response
- Metacholine challenge test
- Spirometry pattern
- FVC
- FEV1
- FEV1/FVC ratio
1 Spirometry
Spirometry is the procedure that measures the rate of changing lung volumes during breathing maneuvers. Specifically, it measures the amount (volume) and speed (flow) of air that can be inhaled and exhaled by the patient. It can be used to diagnose and monitor patients with a variety of respiratory diseases and to measure the respiratory function of a patient before and after a surgical procedure. For this practical reason, both anesthesiologists and surgeons must be able to interpret the spirometry results in the general clinical contest of the patient.
A variety of spirometers are available on the market, and the equipment must fulfill the American Thoracic Society/European Respiratory Society (ATS/ERS) recommendations for spirometry [1]. The recent electronic spirometers calculate the percentage of the predicted normal values based on reference values, according to the patient data: weight and height, age, sex, and race.
Many newer generation spirometers do not require calibration daily as used to be the case decades ago. The respiratory technician or the physician performing the spirometry tests requires training to perform the examination correctly.
It is possible to perform reliable spirometry tests even in preschool noncollaborating children. Other methods have been developed to assess lung function in infants and young children: the interrupter technique, the forced oscillation technique, the gas washout techniques, the tidal breathing techniques, and the rapid thoracoabdominal compression maneuver [2]. These maneuvers are usually performed in advanced respiratory laboratories and will be not discussed in this chapter.
2 Indications and Contraindications to Spirometry
Spirometry is indicated for children with recurrent wheezing/bronchial hyperreactivity, chronic cough, and for the diagnosis and management of asthma and cystic fibrosis. It is also used to measure lung involvement in systemic diseases that can affect the lungs as hemato-oncology conditions and connective tissue disorders. Spirometry is helpful in ascertaining preoperative lung function in chest deformities, such as pectus excavatum, scoliosis, and neuromuscular diseases, muscular dystrophy, and cerebral palsy. It is an essential test to evaluate the preoperative risk before general anesthesia, particularly for cardiothoracic surgery, so that both anesthesiologists and surgeons must be familiar with its interpretation and the consequent clinical indications.
No absolute contraindications are recognized for spirometry, and relative contraindications are acute respiratory tract infection, recurrent/sub-continuous cough, hemoptysis, pneumothorax and pneumomediastinum, aneurysm, uncontrolled hypertension, recent thoracic, abdominal or eye surgery, nausea, vomiting or pain, confusion, or dementia.
2.1 Performing the Spirometry Test
The patient’s weight and height have to be obtained and entered into the spirometry software along with the personal data: name, age, sex, race, and ID. The patient position for the test may be sitting or standing. A disposable mouthpiece is attached to the spirometer, and a nose clip is used to pinch the nose to avoid loose part of the blow through the nose. The FVC maneuver is the most useful and usually is the only one performed and the only one described for the scope of this chapter.
2.2 FVC Test Maneuver
The patient must take two to three tidal breaths with the lips sealed tightly around the mouthpiece and the nose closed by a clip; then, he/she is asked to take a deep breath and then blow air through the mouthpiece suddenly and as fast as possible and to continue to blow for as long as possible (preferably at least 6 seconds) until no air is left to exhale. The test should be repeated at least three times and checked for acceptability and repeatability as shown below. If the results are not acceptable, the test may be repeated another 4–5 times before abandoning the attempt.
In our experience, about 50% of the children aged 4–5 years are able to perform technically acceptable and reproducible spirometry maneuvers, and the percentage increases gradually with age: 90% of neurologically normal children aged 7–8 years are capable to perform reproducible pulmonary function test. During the test, at any age, it is essential to ensure that the child is cooperative and follows the instructions.
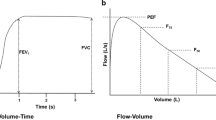
The technician/physician performing the test has to be careful that: the lips are tight around the mouthpiece (not obstructed by the tongue) and the nose clip is in position, the inhalation is complete, the exhalation start is fast and forceful without pause or cough, and the blow is continued until exhaustion, as suggested by a plateau on the volume-time curve (Fig. 7.1b) [3]. The plateau at the end of the expiratory phase of spirometry is generally absent in preschool children. In these patients, the presence of the plateau at the end of the FVC curve is no more a necessary criterion for evaluating a satisfactory expiration: a flow–volume curve demonstrating a rapid rise in the peak flow and a smooth descending limb is acceptable in these patients (Fig. 7.2), particularly if the FVC maneuver is reproducible in at least twice.
2.3 Rating the Spirometry Results
There are different steps to be considered in the following order:
Assessing the tests for acceptability and repeatability. First of all, errors or artifacts in performing the spirometry procedure can be detected simply by looking at the shape of the spirometry graphs. The errors may include poor effort and cough, mouthpiece partially obstructed by the tongue, hesitation in blowing the air, premature finish of the effort with an abrupt stop of expiration, and premature finish and restart with more than one breathing attempt. Two types of graphs are produced in spirometry: flow–volume curve (Fig. 7.1a) and volume–time curve (Fig. 7.1b). Both are used, but the most important and used in evaluating the spirometry is the flow–volume curve, especially in the expiratory part of the FVC maneuver (see subsequently). A spirogram is acceptable if it is free from errors or artifacts with a good start and a satisfactory expiration in accordance with ATS/ERS standards [1]. Some modifications in the criteria have been suggested in an ATS/ERS statement regarding preschool children [1, 4]. In these patients, as described before, the presence of the plateau at the end of the FVC curve is no more a necessary criterion for evaluating a satisfactory expiration: A flow–volume curve demonstrating a rapid rise of the peak flow and a smooth descending limb is acceptable (Fig. 7.2). Two acceptable spirograms are sufficient for this age, while for school-age children a minimum of three satisfactory spirograms is generally required to be sure about the test reproducibility.
-
1.
Identify the parameters to evaluate the spirometry results (Fig. 1a and b). The most used parameters are:
-
(a)
FVC (forced vital capacity): following a maximal inhalation, it is the total amount of air exhaled forcefully.
-
(b)
FEV1 (forced expiratory volume in 1 second): following a maximal inhalation, it is the amount of air exhaled in the first second. Preschool children have a short forced expiratory time; therefore FEV0.5 and FEV0.75 (second) may be used in preschool children (Fig. 7.2).
-
(c)
FEV1/FVC ratio is the most used indicator for identifying airway obstruction but not the most reliable, particularly in children, because it is strictly dependent on the expiratory effort expressed by the patient, and the effort is directly correlated to the patient’s age.
-
(d)
FEF25–75% or MEF50 (flow over the middle half of the FVC: from 25% to 75% of the FVC during forced expiration). It is a sensitive index of airflow obstruction because it is less dependent than FEV1/FVC ratio to the expiratory effort and it is therefore particularly useful in children. The ERS Global Lung Function Initiative has published the global multi-ethnic lung function for spirometry for the 3- to 95-year age range [5]. The comparison is expressed as a percentage of the predicted value or below the lower limit of normal (<90% confidence limit).
-
(a)
-
2.
Identifying the spirometry pattern (normal, obstructive, restrictive, or mixed).
Abnormalities in a spirometry test can be identified first of all by looking at the shape/morphology of the curve and then comparing the test values with the patient’s reference values (Figs. 7.1a, b, and 7.3).
-
(a)
A normal flow–volume curve has a shape like a sail rising very sharply toward the peak (Peak Expiratory Flow or PEF) and then descending shortly with a straight line at an angle of about 45° toward the end, the plateau (Fig. 7.3). Normal preschool children have smaller lung volume compared to rapid emptying of the airways: the result is a convex shape of the flow-volume expiratory curve after the PEF (Fig. 7.2). The expiratory shape becomes more linear (similar to adult PFT) as the child grows in school age. Normal values for FVC and FEV1 are considered >80% of predicted or above the lower limit of normal (Fig. 7.1a, b).
-
(b)
An obstructive flow–volume curve shows a good rise toward the PEF followed by a concave expiratory curve, indicating that the decrease in the expiratory flow is faster than the decrease in lung volume during the expiratory phase. It is usually characterized by decreased FEV1 (<80% of predicted or below the lower limit of normal), decreased FEV1/FVC, and normal FVC (Fig. 7.3). To determine if the FEF1/FVC ratio is low, indicating an obstructive defect in patients five to 18 years of age, the National Asthma Education and Prevention Program guideline says that a ratio of less than 85% is consistent with an obstructive defect as long as the patient has symptoms consistent with obstructive lung disease [6]. The FVC may be decreased even in case of severe obstruction, the expiratory curve is elongated and thin toward the end as a rat’s tail without a definite plateau (Fig. 7.3). FEF25–75% values below 60% of predicted also suggest an obstructive pattern. FEF25–75% or MEF50 (Fig. 7.1a), being mid expiratory flow, is less effort dependent than FEV1as explained before, it is considered a measurement of small airway patency, particularly useful in children with asthma [7].
-
(c)
A restrictive flow-volume curve is characterized by an expiratory line sharply descending toward the end with a consequent low FVC value, that is the distinctive/predominant pattern, with a normal or decreased FEV1 that can have the same value as the FVC (Fig. 7.3). The FEV1/FVC is consequently increased toward the value of 1 due to the low FVC value. It is very important at the moment of the spirometry procedure to keep in mind that a poor effort by the patient can falsely mimic the restrictive curve with a proportionate reduction in both FEV1 and FVC.
-
(d)
A mixed flow—volume pattern has a decreased value of all three values: FEV1, FVC, and FEV1/FVC and is common in severe bronchospasm/asthma.
-
(e)
An altered shape of flow–volume curve can be suggestive of central airway obstruction (larynx or trachea) (Fig. 7.4). Normal expiratory flow with a plateau-shaped inspiratory curve is suggestive of collapsible extra thoracic airway obstruction (e.g., laryngeal malacia or paralysis). On the contrary, normal inspiratory flow with a decreased maximal expiratory flow (PEF) and a box-shaped expiratory curve suggest collapsible major intrathoracic airway obstruction (e.g., vascular ring or extrinsic compression plus tracheomalacia as is quite common in esophageal atresia and tracheoesophageal fistula). If both inspiratory and expiratory flows are decreased, a severe, fixed intrathoracic, or extrathoracic airway obstruction is likely present.
-
(a)
2.4 Bronchodilator Response
The bronchodilator response (BDR) test is useful to assess reversibility of the obstructive pattern in spirometry, which is characteristic of asthma or bronchial/airway hyperreactivity. A baseline spirometry is performed in patients free of any kind of bronchodilator therapy: in the last 6 or 12 h, respectively, for short- and long-acting β2 agonist. A second spirometry is then performed after 10–15 min of 2–3 doses of 100 μg salbutamol spray, delivered by a metered dose inhaler (MDI) with a spacer. For a positive response to the bronchodilator, the thresholds considered significant are an improvement >12% in FEV1 or 15–25% in FEF25–75% in the post-salbutamol test and suggest reversibility of airway obstruction (Fig. 7.5) [8]. However, it is important to underline that the presence of airway obstruction in the spirometry without a significant BDR does not exclude the diagnosis of asthma because it can be the expression of a chronic inflammation condition of the bronchial wall not responsive to the β2agonist/salbutamol, due to poorly controlled asthma in children. These patients probably need a course of topic or oral corticosteroid before the test can be repeated. On the other hand, a negative BDR on a singular test does not exclude the diagnosis of bronchial hyperreactivity or asthma, clinical conditions characterized by a variable bronchoconstriction state and mutable clinical history, particularly in the pediatric age. A methacholine challenge test can be indicated in these patients to diagnose bronchial hyperreactivity.
Similarly, a baseline spirometry within normal ranges but followed by a BDR with a significant increase in the expiratory flow should be interpreted in these patients only as an expression of bronchial hyperreactivity, a clinical condition characterized by frequent bronchospasm episodes, mainly correlated with the recurrent viral infection characteristic of pediatric patients [9]. These considerations suggest that BDR may be a useful objective tool to assess the presence of a bronchoconstriction tone, particularly in children with bronchial hyperreactivity, and can suggest the prescription of maintenance therapy with bronchial anti-inflammatory drugs.
2.5 Methacholine Challenge Test (MCT)
In this test, also known as bronchoprovocation test, increasing doses of methacholine are delivered to the patient so as to achieve bronchoconstriction: the opposite effect of the BDR. Methacholine mimics the neurotransmitter acetylcholine to directly interact with muscarinic receptors on airway smooth muscle, resulting in airway narrowing and decreased expiratory flows. The test is indicated when the baseline spirometry is within the normal limits, the BDR is without significance, and the diagnosis of bronchial hyperreactivity/asthma is suspected on clinical records.
The patient has to be out of every medication for at least 1 week for inhaled corticosteroids and antileukotrienes and 6–36 h for short and long bronchodilators prescribed in pediatric age [10]. After a baseline spirometry test, the methacholine challenge can start only if the FEV1 is at least >60% of the predicted value [10]. The test starts with a very small dose of methacholine (<0.25 mg/mL), then the doses are progressively increased, and after every dosage an FCV is performed. The test has to be interrupted when, compared with the baseline value, a 20% decrease in FEV1 is recorded. The smaller the methacholine dose necessary to cause a 20% decrease of FEV2, the higher the degree of airway hyperreactivity. The PC2O is the provocative concentration (methacholine mg/mL) causing a 20% fall in FEV1, and the PD20 is the provocative dose causing a 20% fall in FEV1 (extrapolated by the last two PC20 delivered to the patient), according to the new recommendations [10]. The Airway hyperresponsiveness (AHR) is rated as normal, borderline, mild, moderate, and severe, according to the PD20 values (Table 7.1).
The MCT is highly sensitive for diagnosing airway hyperreactivity/asthma; however, its low specificity results in false-positive results; on the other hand, a negative test means that a diagnosis of bronchial hyperreactivity/asthma is unlikely.
3 Conclusions
Spirometry is a fundamental test in the diagnosis of lung disease in pediatric age and, with the availability of better equipment with incentives for children, even preschool patients can perform acceptable/reproducible spirometry. There has been much progress over the past decade regarding the standardization of spirometry, which includes differences recognized between spirometry performed by children and adults. Therefore, there is no more excuse to underuse spirometry in pediatric age, and there is a need to encourage its use by all the pediatricians treating children with respiratory diseases to monitor disease and response to therapy. The various measurements obtained from spirometry with the ancillary tests as the BDR and the MCT test can be very useful even in evaluating the patients before a surgical procedure to avoid the occurrence of respiratory failure due to intraoperative bronchospasm or to an underdiagnosed baseline poor respiratory function.
References
Miller MR, Hankinson J, Brusasco V, et al. ATS/ERS Task Force. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Escobar H, Carver TW Jr. Pulmonary function testing in young children. Curr Allergy Asthma Rep. 2011;11:473–81.
Seed L, Wilson D, Coates AL. Children should not be treated like little adults in the PFT lab. RespCare. 2012;57(1):61–71.
Beydon N, Davis SD, Lombardi E, et al. American Thoracic Society/European Respiratory Society Working Group on Infant and Young Children Pulmonary Function Testing. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J RespirCrit Care Med. 2007;175(12):1304–45.
Quanjer PH, Stanojevic S, Cole TJ, et al. The ERS global lung function initiative. Multi-ethnic reference values for spirometry for the 3-95 year age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–43.
National Asthma Education and Prevention Program. Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma—summary report 2007 [published correction appears in J Allergy Clin Immunol. 2008;121(6):1330. J Allergy Clin Immunol. 2007;120(5 suppl):S94–S138
Simon MR, Chinchilli VM, Phillips BR, et al. Childhood Asthma Research and Education Network of the National Heart, Lung, and Blood Institute. Forced expiratory flow between 25% and 75% of vital capacity and FEV1/forced vital capacity ratio in relation to clinical and physiological parameters in asthmatic children with normal FEV1 values. J Allergy Clin Immunol. 2010;126(3):527–34.
Levy ML, Quanjer PH, Booker R, Cooper BG, Holmes S, Small I, General Practice Airways Group. Diagnostic spirometry in primary care: proposed standards for general practice compliant with American Thoracic Society and European Respiratory Society recommendations: a General Practice Airways Group (GPIAG) document in association with the Association for Respiratory Technology & Physiology (ARTP) and Education for Health. Prim Care Respir J. 2009;18(3):130–47.
Galant SP, Morphew T, Newcomb RL, Hioe K, Guijon O, Liao O. The relationship of the bronchodilator response phenotype to poor asthma control in children with normal spirometry. J Pediatr. 2011;158(6):953–959.e1.
Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J. 2017;49:1601526.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Sacco, O. (2021). Pulmonary Function Tests. In: Mattioli, G., Petralia, P., Torre, M. (eds) Pediatric Thoracic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-74668-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-030-74668-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-74667-4
Online ISBN: 978-3-030-74668-1
eBook Packages: MedicineMedicine (R0)