Abstract
Tracheostomy has attracted increasing attention in recent years, owing to progress in team-based care and demonstrable advances in weaning and decannulation. While many factors that affect survivorship after ICU stay are poorly understood, tracheostomy plays an important role in alleviating this burden. These observations highlight the importance of modernizing tracheostomy practice using evidence-based approaches. The COVID-19 pandemic, has underscored the importance of effective tracheostomy practice in efficient resource allocation and optimizing survivorship outcomes following ICU stay.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Tracheostomy
- Weaning
- Decannulation
- ICU capacity
- ICU surge
- Resource allocation
- Survivorship
- COVID-19
- Rehabilitation
- Length of stay
1 Introduction
Tracheostomy has attracted increasing attention in recent years, owing to progress in team-based care and demonstrable advances in weaning and decannulation. A cardinal objective of the intensive care unit (ICU) is to stabilize critically ill patients, but it is increasingly recognized that the quality of life that patients and their families experience after an ICU stay is also important. Many patients who require invasive mechanical ventilation will manifest long-lasting physical, cognitive and/or mental health impairments. While many factors that affect survivorship after an ICU stay are poorly understood, tracheostomy plays an important role in alleviating this burden through reducing cumulative sedation dose, expediting physical therapy and rehabilitation, and potentially allowing patient-focused benefits such as earlier eating, drinking, talking and mobilization. Such observations highlight the importance of modernizing tracheostomy practice using evidence-based approaches.
Tracheostomy is associated with significant healthcare expenditure as well as high personal and social costs secondary to reduced quality of live and dependency. Improved practices around tracheotomy care, weaning, and decannulation reduce ICU and hospital lengths of stay. The coronavirus disease 2019 (COVID-19) pandemic, which has seen a surge in patients requiring tracheostomy for prolonged mechanical ventilation, has underscored the importance of effective tracheostomy practice in efficient resource allocation and optimizing survivorship outcomes following ICU stay.
2 What is the Pre-COVID-19 Evidence for Early Tracheostomy?
Conflicting results regarding timing of tracheostomy were reported in meta-analyses published in 2015 [1,2,3,4], and repeated in 2018 [5, 6], with no major trials published between them. Most recently, a meta-analysis of 17 randomized trials and 3145 participants found that early tracheotomy in adults receiving invasive mechanical ventilation was associated with a decrease in the occurrence of ventilator-associated pneumonia (VAP), more ventilator-free days, and fewer ICU days [7]. However, the evidence suggests limited, if any, benefit on survival rates with early compared to later tracheostomy.
Despite the marked heterogeneity across trials, there are populations who benefit from early tracheostomy (e.g., selected patients with burns, trauma, or stroke), and there are also populations who are well-served by attempts at extubation without increasing length of ICU stay or duration of mechanical ventilation. Several mechanisms may account for this benefit from early tracheostomy. Tracheostomy reduces the cumulative sedation dose administered [8] and allows for earlier rehabilitation and physical therapy, thereby reducing the likelihood of venous thromboembolism and risk for critical illness myopathy. Early tracheostomy also allows for earlier walking, talking and eating [9]. Earlier extubation also reduces the risk of numerous airway complications that may arise from prolonged translaryngeal intubation, including laryngeal diastasis, scarring, tracheomalacia, and tracheal stenosis.
Nonetheless, an important caveat remains the heterogeneity found among trials. Studies vary in the patients recruited, definition of ‘early’ tracheostomy, and outcomes studied. Tracheostomy is performed for a variety of indications, and patients differ widely in their underlying disorders and morbidities. Furthermore, studies span multiple ICU settings: findings for stroke patients in the neuro-ICU may not generalize to patients with respiratory failure within the medical ICU. Randomized controlled trials conducted over several years may have confounders relating to evolving practices and protocols. The literature also reflects a wide range of disease severity. Finally, a critical knowledge gap remains on how to predict whether a patient will require prolonged mechanical ventilation.
3 What Does ‘Early’ Tracheostomy Really Mean?
Definitions of early tracheostomy range from <4 to 15 days [10, 11], and criteria are invariably time-delimited, rather than linked to physiological parameters or phase of illness. This observation reflects our limited mechanistic understanding of the factors that determine weaning and course of illness. Studies that have found benefit with early tracheostomy have often reported reduced before-tracheostomy time or reduced weaning time only, not necessarily modifying the period spanning from onset of invasive mechanical ventilation to initiation of weaning [12, 13], thus making results difficult to compare depending on case-mix. To our knowledge, no trial has defined ‘early’ based on this more physiological concept, which is notable as weaning time may account for nearly 40% of total time on ventilator.
Some aspects of COVID-19 can substantially modify time on ventilator: first, time to tracheostomy may be delayed due to perceived risk for infection transmission to healthcare workers; second, the need for prone position during the early stage of the disease may delay tracheostomy; third, the surge conditions in overwhelmed units may modify bedside decisions over the course of successive pandemic waves; fourth, COVID-19 has a high prevalence of late complications (e.g., delirium, ICU-associated weakness, secondary nosocomial infections, etc.) prolonging the weaning time and posing difficulties in establishing when weaning attempts were initiated. Therefore, it has proven challenging to define the optimal early-timing for tracheostomy in the pre-COVID-19 era and even harder during the COVID-19 surges.
4 What Respiratory Parameters or Criteria Ensure It Is Safe to Perform a Tracheostomy?
Ensuring adequate pulmonary reserve was a key prerequisite for early tracheostomy prior to the COVID-19 era. A large randomized trial comparing early (after 6–8 days of endotracheal intubation) versus late (after 13–15 days of endotracheal intubation) tracheostomy, in which 46% of patients had primary respiratory failure, excluded patients from having a tracheostomy if they had recovered lung function up to a PaO2 >60 mmHg with a FiO2 <50% and a positive end-expiratory pressure (PEEP) <8 cmH2O [11]. The reason for this exclusion was to reduce the number of unnecessary tracheostomies. Using these criteria, 28.3% of enrolled patients did not receive a tracheostomy because they were close to fulfilling weaning criteria before day 15 (21.3% before day 11). Abe et al. [14] reported a 12.9% rate of tracheostomy after a median time of 14 days in a large population of patients with acute respiratory distress syndrome (ARDS), with a median PaO2/FiO2 ratio of 156 with a median PEEP of 8 cmH2O at ARDS onset. Moreover, in a randomized clinical trial comparing early (within 4 days) versus late (after 10 days) tracheostomy, Young et al. [10] included patients for tracheostomy if they had been receiving mechanical ventilation for less than 4 days and were expected by the attending physician to need mechanical ventilation for at least 7 more days, with no pre-specified ventilator setting limitation. This led to the exclusion from statistical analysis after randomization of 53.7% of the patients in the late tracheostomy group because they did not meet the attending physician criteria.
After the COVID-19 pandemic started in 2020, respiratory safety criteria for performing a tracheostomy changed, mainly because the overriding concern was to reduce unnecessary tracheostomies but to protect healthcare workers and unstable patients. Bier-Laning et al. [15] found, in their state-of-the-art review, 14 different protocols listing unstable respiratory status criteria contraindicating tracheostomy. Late tracheostomy is not usually limited by unstable respiratory conditions, but safety protocols for early tracheostomy demonstrate a wide range of criteria, from an apnea test [16] to definitions of very high ventilatory requirements (e.g., FiO2 >60–70% and/or PEEP >12 cmH2O) [17, 18].
There are several reasons for these pre- and post-COVID-19 differences. First, pre-COVID-19 randomized trials on this topic recruited patients in whom the tracheostomy was performed for indications other than primary respiratory failure. Such studies had a low percentage of patients with ARDS, limiting comparisons with COVID-19 evidence for early tracheostomy [10, 11]. Second, prioritization of healthcare worker safety resulted in modifications to procedural recommendations (e.g., disconnecting patients from mechanical ventilation before opening the trachea or delaying reconnection though tracheal cannula after cuff is inflated). These modifications result in a longer apnea period, often with total depressurization of the tracheal tree, thus putting patients at risk for respiratory deterioration. Third, some expert panels recommended the open technique, probably resulting in longer procedure times. In light of these observations, it seems that very high ventilatory requirements did not limit early tracheostomies, and severe deterioration was not reported after early tracheostomies in many experienced centers [13, 19].
5 What Does Predicting Prolonged Mechanical Ventilation Really Mean?
Traditional models for predicting prolonged mechanical ventilation aim to estimate at the earliest time point on mechanical ventilation the likely duration the patient will remain on the ventilator, ranging from 1 day to 21 days [20]. In addition, only one study has prospectively validated a model capable of predicting patients needing mechanical ventilation for more than 14 days [21]. This model loses close to 20% of the patients when optimizing specificity at 100%.
As already mentioned, a large UK trial aimed at elucidating a possible benefit for early tracheostomy, assessed the attending physicians’ ability 4 days after intubation to predict 7 additional days on the ventilator [10]. Others have randomized patients 3 days after endotracheal intubation, including those with persistent respiratory failure fulfilling gasometric criteria of moderate ARDS (PO2/FiO2 ratio <120 with a FiO2 ≥50% and PEEP ≥8 cmH2O) [11]. Importantly, this trial excluded patients with a respiratory infection mainly because of the increased difficulty in accurate prediction in these cases. Under these conditions, those trials lost 48.4% [10] and 18.6% [11] of the randomized patients because of clinical improvement.
In the case of COVID-19 patients, guidelines recommend performing a tracheostomy when the expected total duration of mechanical ventilation is greater than 10 days [16]. The median duration of mechanical ventilation in COVID-19 patients has been reported according to the severity of ARDS at onset, ranging from 12 (6–18) days in mild ARDS to 14 (10–19) days in severe cases, with tracheostomy rates ranging from 10% to 7% respectively [22]. Anticipating the clinical course of patients remains challenging, although innovations continue to emerge, including those arising from machine learning in tracheostomy [23] and more broadly in critical care [24].
6 Why Has Prone Position Been Considered a Limitation For Early Tracheostomy?
Prone positioning has traditionally been considered a relative contraindication for tracheostomy because of an increased risk for cannula displacement or accidental decannulation [25]. Prone ventilation has been extensively used in ARDS patients with COVID-19 with up to 80% of patients receiving at least one session in severe cases [22]. Most guidelines have recommended 12–16 h per day sessions and the median number of sessions reported in many large cohort studies is 3–4 (2–6) [22, 26], similar to that described previously in non-COVID-19 patients [27]. This observation means that around 25% of patients are definitively turned supine by day 3 after intubation and around 75% of patients who need prone positioning finish this therapy before the first week on mechanical ventilation. Some studies on tracheostomy in COVID-19 patients have reported pronation rates up to 80% within the first 14 days [13]. Although some COVID-19 patients require prolonged prone position therapy, it seems that most can safely receive a trachesotomy within the first 14 days after intubation without the need to modify postural therapies.
7 What Is the Real Risk for Healthcare Workers Performing Tracheostomies During the COVID-19 Pandemic?
Tran et al. [28] performed a systematic review of the risk of transmission of acute respiratory infections to healthcare workers during aerosol-generating procedures during the 2003 severe acute respiratory syndrome (SARS) pandemic, reporting an increased risk for tracheostomy (odds ratio 4.2 [1.5–11.5]). Notably, only one case-control study was included [29]. Moreover, tracheostomy was not independently related to the risk of infection transmission when the multivariable analysis included a logistic regression. Comparable data have not been published for COVID-19. The observational studies on tracheostomy during the COVID-19 pandemic have shown no infection or rates of infection no higher than the base rate for individuals involved in non-aerosol generating procedures. Most tracheostomies have been performed in a scheduled fashion, with minimal emergent techniques. The data on rates of healthcare worker infections associated with tracheostomies have largely demonstrated limited or absent viral transmission; however, many reports are anecdotal case series. Another limitation is that in cohorts with tracheostomy performed by proceduralists, viral transmission in the broader team was not reported.
Even when infection occurs in healthcare professionals involved in performing tracheostomy, the source of infection is often unclear, as evident in the study by Rosano and colleagues, who collected data on severe acute respiratory coronavirus 2 (SARS-CoV-2) infection in ICU nurses and physicians involved in 121 percutaneous tracheostomies and compared it to the prevalence of SARS-CoV-2 infection in ICU healthcare professionals not participating in tracheostomies. The 7.7% prevalence of infection in doctors and nurses performing tracheostomies was not significantly different from the 11.5% prevalence of infection in healthcare worker not involved in any tracheostomy procedure [30].
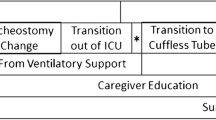
8 Post-tracheostomy Care
Most recent advances to accelerate weaning and decannulation in patients with a tracheostomy tube include aerosol-generating protocol modifications (e.g., disconnection from mechanical ventilation, increasing effective airway diameter including cuff deflation, use of tracheal high flow therapy) [31,32,33]. During the COVID-19 pandemic, perceived risk for healthcare workers took precedence, and guidelines on COVID-19 management have recommended against cuff deflation during the pandemic to protect healthcare workers [16,17,18]. We can interpret this information in two different ways: on the one hand, the risk for healthcare workers remains a challenge, and on the other hand, it can be assumed that the risk for infection transmission has declined by the time patients with a tracheostomy tube can be considered for disconnection from mechanical ventilation. Performing a tracheostomy in a COVID-19 patient has been delayed to a median time of about 19–20 days since symptom onset [16], and the first weaning attempts are delayed to about 28–30 days [13], thus likely increasing safety for healthcare workers.
Another important aspect of post-tracheostomy care is related to the expected probability of meaningful recovery. Many healthcare systems manage these patients in step-down units or long-term care centers, aiming to improve the quality of life of the patients with little hope of a full recovery [31]. However, recent advances in centers managing patients with a tracheostomy tube in high-dependency units report higher expectations for final decannulation when more aggressive protocols are applied [33].
Jubran et al. [31] reported several important results: first, close to 30% of patients with a tracheostomy tube were transferred to a chronic center without previous clear effort to advance in the disconnection process; second, in was not possible to wean 22.5% of a general population of tracheostomized patients under these conditions; third, patients with a limited pulmonary reserve detected by delayed failure after first disconnection were more prone to respond to aerosol-generating protocols. Hernandez et al. [33] found that reducing the effective airway diameter not only during weaning but also during the decannulation period reduced successful progression to final decannulation, as a prolonged capping trial seems to impose a limitation for secretion management, even increasing the probability of delayed weaning failure.
These recent advances in the management of patients with a tracheostomy tube include some aspects that must be taken into account [32]. A more proactive approach to early detection and treatment of the limiting factors for decannulation involves pre-emptive diagnostic testing. Both airway patency problems and risk of aspiration should be detected not after weaning but at its beginning, as clinically significant stenosis (secondary to inflammation due to the prolonged presence of the artificial airway or directly because the tracheal cannula reduces the effective airway diameter) calls for specific treatment or a down-sized tracheal cannula and severe risk for aspiration precludes some measures facilitating the weaning process (e.g., deflating the tracheal cuff).
Diagnostic testing for impaired swallowing can be performed using a clinical test (e.g., deglutition test or FEES [fibreoptic endoscopic evaluation of swallow]), allowing for detection of severe cases of swallowing dysfunction. Mild and moderate swallowing dysfunction limit progression to oral intake, but do not delay progression to weaning and decannulation. Endoscopic procedures can confirm and specifically diagnose anatomical injuries needing direct attention by Head and Neck surgical teams. In addition, deflating the cuff has been associated with an improved recovery of swallowing function [32]. Although this result is hypothesis-generating and must be confirmed, reduced vertical movement of the trachea while swallowing with the cuff inflated could explain, at least in part, the frequent swallowing dysfunction observed in patients with a tracheostomy tube. Early restoration of translaryngeal airflow promotes laryngeal rehabilitation, coughing, swallowing and of course vocalization—all of which can have a positive physical and psychological benefit in those recovering from prolonged critical illness.
Conditioning the gases inhaled directly through the trachea helps accelerate both weaning and decannulation [32, 33] by improving secretion management and reducing the respiratory infection rate. Surprisingly, deflating the cuff significantly reduced the respiratory infection rate during weaning when combined with tracheal high flow. Although explanations for these results remain speculative, high flow seems to facilitate avoiding micro-aspirations around the cannula. This result was confirmed in a second study during the decannulation process [33].
These modifications taken together can increase the weaning and decannulation success rate by up to 93% and 95%, respectively [32, 33]. The subgroup of patients with a tracheostomy tube in which these aggressive protocols are limited are those with low level of consciousness, mainly because of a high risk of aspiration. Although level of consciousness is frequently recovered later in the course of the ICU or hospital admission, these patients are usually analyzed in specific studies and excluded from general trials because the time for recovery is difficult to predict and the time sensitive analysis of the trials could report spurious results depending on the case-mix. However, after these patients recover a good level of consciousness, the protocols could be applied without modification.
9 What Are the Implications of Tracheostomy for COVID-19 Survivorship?
Advances in critical care medicine are to be credited for the many survivors of severe COVID-19 (Table 13.1). Among such advances are the benefits of use of small tidal volumes, prone ventilation, conservative fluid management, lung protective ventilation, and other principles of the Surviving Sepsis Campaign guidelines for management of critically ill patients with COVID-19 [34]. However, despite this success, approximately 80% of patients surviving critical illness after mechanical ventilation in the ICU will experience physical, cognitive and/or mental health impairments, which are recognized as the post-intensive care syndrome (PICS).
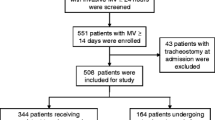
Timely tracheostomy, when indicated, may shorten the duration of ICU stay and thereby potentially reduce the impairments associated with PICS [35]. For some aspects of survivorship after critical illness, a longer duration of critical illness is associated with greater impairment. Patients’ survivorship experience reflects the complex interplay of critical illness and the iatrogenic effects of aggressive treatment. For example, the cumulative effects of sedation and restraints on the neuromuscular system, cognition, and overall rehabilitation are sometimes under-recognized. These are summarized in Figure 1. Temporary or permanent effects of translaryngeal intubation on dyphonia, dysphagia, and airway patency may not be recognized until long after the acute phase of illness and are increasingly documented in patients with COVID-19 [36]. Other physical impairments after critical illness may include joint contractures and critical illness-associated neuropathy or myopathy.
Modernizing tracheostomy care can serve as a catalyst for improving efficiencies in resource utilization and enhancing survivorship outcomes. Evidence-based, multidisciplinary critical care plays a critical role in improving patients’ long-term quality of life. Awareness of these survivorship considerations is important for all members of the healthcare team, including clinicians as well as patients and families, to maximize the likelihood of restoring fulfilling and meaningful lives (Figs. 13.1 and 13.2). Lack of coordination of care is a major factor in prolonged ICU stay and delayed decannulation. Patients may suffer persistent sleep impairment, pain, fatigue, and overall degraded health-related quality of life. Patients’ loved ones have significant rates of mental health impairment.
Post-intensive care syndrome (PICS) affects patients and family members, affecting mental health, physical, and cognitive domains. From [35] with permission
Clinical courses of patients with COVID-19. a. Prototypical course of severe COVID-19, b. Progressive multiorgan failure; c. Protracted critical illness requiring extracorporeal membrane oxygenation (ECMO), d. Relapsing course requiring readmission. Other survivorship streams also depicted. Reproduced from [35] with permission
10 Lessons from COVID-19
The COVID-19 pandemic has overwhelmed ICUs around the world, affecting not only healthcare workers, but also ICU capacity including ICU beds and ventilators. What mainly defines an ICU bed is the attending staff and the supplies and equipment required to manage a patient with endotracheal intubation, so the limiting factor for ICU equipment capacity in this context is availability of ventilators. Unfortunately, few measures can help optimize this capacity, including considering transport ventilators, operating room equipment, military supplies, long-term ventilators, veterinary ventilators, magnetic resonance imaging compatible ventilators, non-invasive ventilators, or even prolonged manual ventilation [37, 38]. These recommendations are based on best practice statements, except the recommendation against using one ventilator for multiple patients (strong recommendation with low quality evidence), that was based on animal or mechanical models [38].
There is limited evidence for early timing of tracheostomy before the COVID-19 pandemic. There are many explanations for this paucity of evidence: first, the difficulty for physicians to predict prolonged mechanical ventilation and limited internal validity of randomized trials; second the great variability in definition of early tracheostomy, increasing the heterogeneity in meta-analyses, and the heterogeneous outcomes analyzed, with different results for duration of mechanical ventilation and ventilator-free days [2]. The reason for this disparity in results depending on the outcome analyzed could be the high mortality of patients needing prolonged mechanical ventilation, modifying the results when a failure-free days composite end-point is used instead of the duration of mechanical ventilation. A meta-analysis published in 2015 showed a significant increase in ventilator-free days with early tracheostomy (mean difference for ventilator-free days 2.12, 95% CI 0.94 to 3.30) [2], and others confirmed a reduced duration of mechanical ventilation with a trial-sequential analysis (mean difference -0.91, 95% CI -1.45 to -0.38) [5] in 2019. These results have been confirmed in a recent meta-analysis by Chorath et al. [7].
Specific data regarding COVID-19 patients is scarce, as performing a randomized trial is difficult under surge conditions. Some studies suggest a benefit for early trachoestomy in COVID-19 patients. Aviles-Jurado et al. [13] reported the possibility of decreased use of ICU beds during the pandemic when tracheostomy is properly indicated early in the course of the disease. Possible reasons for this include the following: first, it is easier to predict prolonged mechanical ventilation in this population, second the high volume of patients with low heterogeneity facilitate the statistical analysis.
Recommended ventilator settings for safely performing an early tracheostomy during the COVID-19 pandemic are the following: PEEP <12 cmH2O, FiO2 <60%, respiratory rate <30 bpm, PaCO2 <60 mmHg, and able to tolerate a period of apnea, but more relaxed approaches have shown good results. In their single center study, Aviles-Jurado et al. [13] performed tracheostomies within the first 8 days in patients with PEEP of 10 cmH2O and PaO2/FiO2 about 200.
11 Conclusion
Despite important recent advances in tracheostomy and post-tracheostomy care, we have a long way to go before we can confidently answer important questions about the insertion and subsequent management of tracheostomy for the maximum benefit of our patients and for our healthcare systems. We have detected a slowing down in progression, but the window for improvement remains open. The COVID-19 pandemic has increased our understanding of many aspects of tracheostomy care, but our learning must go on.
References
Liu CC, Livingstone D, Dixon E, Dort JC. Early versus late tracheostomy: a systematic review and meta-analysis. Otolaryngol Head Nek Surg. 2015;152:219–27.
Hosokawa K, Nishimura M, Egi M, Vincent JL. Timing of tracheotomy in ICU patients: a systematic review of randomized controlled trials. Crit Care. 2015;19:424.
Szakmany T, Russell P, Wilkes AR, Hall JE. Effect of early tracheostomy on resource utilization and clinical outcomes in critically ill patients: meta-analusis of randomized controlled trials. Br J Anaesth. 2015;114:396–405.
Siempos II, Ntaidou TK, Filippidis FT, Choi AMK. Effect of early verus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3:150–8.
Wang R, Pan C, Wang X, Xu F, Jiang S, Li M. The impact of tracheostomy timing in critically ill patients undergoing mechanical ventilation: a meta-analysis of randomized controlled trials with sequential analysis. Heart Lung. 2019;48:46–54.
Khammas AH, Dawood MR. Timing of tracheostomy in intensive care unit patients. Int Arch Otolaryngol. 2018;22:437–42.
Chorath K, Hoang A, Rajasekaran K, Moreira A. Association of early vs late tracheostomy placement with pneumonia and ventilator days in critically ill patients a meta-analysis. JAMA Otolaryngol Head Neck Surg. 2021;147:450–9.
Cagino LM, Kercheval JB, Kenes MT, McSparron JI, Blank R, Chinn SB, et al. Association of tracheostomy with changes in sedation during COVID-19: a quality improvement evaluation at the University of Michigan. Ann Am Thorac Soc. 2021;18:907–9.
Sutt AL, Tronstad O, Barnett AG, Kitchenman S, Fraser JF. Earlier tracheostomy is associated with an earlier return to walking, talking, and eating. Aust Crit Care. 2020;33:213–8.
Young D, Harrison DA, Cuthbertson BH, Rowan K. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation. The TrachMan randomized trial. JAMA. 2013;309:2121–9.
Terragni PP, Antonelli M, Fumagalli R, Faggiano C, Berardino M, Pallavicini FB, et al. Early vs late tracheostomy for prevention of penumonia in mechanically ventilated adult ICU patients. A randomized controlled trial. JAMA. 2010;303:1483–9.
Diaz-Prieto A, Mateu A, Gorriz M, Ortiga B, Truchero C, Sampietro N, et al. A randomized clinical trial for the timing of tracheostomy in critically ill patients: factors precluding inclusion in a single center study. Crit Care. 2014;18:585.
Aviles-Jurado FX, Prieto-Alhambra D, Gonzalez-Sanchez N, de Ossó J, Arancibia C, Rojas-Lechuga MJ, et al. Timing, complications, and safety of tracheotomy in critically ill patients with COVID-19. JAMA Otolaryngol Head Neck Surg. 2021;147:41–8.
Abe T, Madotto F, Pham T, Nagata I, Uchida M, Tamiya N, et al. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Crit Care. 2018;22:195.
Bier-Laning C, Cramer JD, Roy S, Palmieri PA, Amin A, Añon JM, et al. Tracheostomy during the COVID-19 pandemic: comparison of international perioperatove protocols and practices in 26 countries. Otolaryngol Head Neck Surg. 2021;164:1136–114.
McGrath B, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020;8:717–25.
Villalonga-Vadell R, Martin Delgado MC, Aviles-Jurado FX, Álvarez Escudero J, Aldecoa Álvarez-Santuyano C, de Haro López C, et al. Consensus document of the Spanish Society of intensive and critical care medicine and coronary units (SEMICYUC), the Spanish Society of Otolaryngology and Head and Neck Surgery (SEORL-CCC) and the Spanish Society of Anesthesiology and critical care (SEDAR) on tracheostomy in patients with COVID-19 infection. Rev Esp Anestesiol Reanim. 2020;67:504–10.
Lamb CR, Desai NR, Angel L, Chaddha U, Sachdeva A, Sethi S, et al. Use of tracheostomy during the COVID-19 pandemic: American College of Chest Physicians/American Association for Bronchology and Interventional Pulmonology/Association of Interventional Pulmonology Program Directors Expert Panel Report. Chest. 2020;158:1499–514.
Kwak PE, Connors JR, Benedict PA, Timen MR, Wang B, Zhang Y, et al. Early outcomes from early tracheostomy for patients with COVID-19. JAMA Otolaryngol Head Neck Surg. 2020;147:239–44.
Ghauri SK, Javaeed A, Mustafa KJ, Khan AS. Predictors of prolonged mechanical ventilation in patients admitted to intensive care units: a systematic review. Int J Health Sci (Qassim). 2019;13:31–8.
Clark PA, Inocencio RC, Lettieri CJ. I-TRACH: validating a tool for predicting prolonged mechanical ventilation. J Intens Care Med. 2018;33:567–73.
COVID-19 Group on Behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73.
Takhar A, Surda P, Ahmad I, Amin N, Arora A, Camporota L, et al. Timing of tracheostomy for prolonged respiratory wean in critically ill coronavirus disease 2019 patients: a machine learning approach. Crit Care Explor. 2020;2:e0279.
Mlodzinski E, Stone DJ, Celi LA. Machine learning for pulmonary and critical care medicine: a narrative review. Pulm Ther. 2020;6:67–77.
Pandian V, Murgu S, Lamb CR. Counterpoint: Tracheostomy in patients with COVID-19, should we do it before 14 days? No. Chest 2021;159:1727–29.
Weiss TT, Cerda F, Scott JB, Kaur R, Sungurlu S, Mirza SH, et al. Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to COVID-19: a retrospective observational cohort study. Br J Anaesth. 2021;126:48–55.
Guerin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–68.
Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7:e35797.
Chen WQ, Ling WH, Lu CY, Hao YT, Lin ZN, Ling L, et al. Which preventive measures might protect health care workers from SARS? BMC Public Health. 2009;9:81.
Rosano A, Martinelli E, Fusina F, Albani F, Caserta R, Morandi A, et al. Early percutaneous tracheostomy in coronavirus disease 2019: association with hospital mortality and factors associated with removal of tracheostomy tube at ICU discharge. A cohort study on 121 patients. Crit Care Med. 2021;49:261–70.
Jubran A, Grant BJB, Duffner LA, Collins EG, Lanuza DM, Hoffman LA, Tobin MJ. Effect of pressure support vs unassisted breathing through a tracheostomy collar on weaning duration in patients requiring prolonged mechanical ventilation: a randomized trial. JAMA. 2013;309:671–7.
Hernandez G, Pedrosa A, Ortiz R, Cruz Accuaroni Mdel M, Cuena R, Vaquero Collado C, et al. The effects of increasing effective airway diameter on weaning from mechanical ventilation in tracheostomized patients: a randomized controlled trial. Intensive Care Med. 2013;39:1063–70.
Hernandez G, Rodriguez ML, Vaquero MC, Ortiz R, Masclans JR, Roca O, et al. High-flow oxygen with capping or suctioning for tracheostomy decannulation. N Engl J Med. 2020;383:1009–17.
Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46:854–87.
Pandian V, Brodsky MB, Brigham EP, Parker AM, Hillel AT, Levy JM, et al. COVID-19 survivorship: How otolaryngologist-head and neck surgeons can restore quality of life after critical illness. Am J Otolaryngol. 2021;42:102917.
Rouhani MJ, Clunie G, Thong G, Lovell L, Roe J, Ashcroft M, et al. A prospective study of voice, swallow, and airway outcomes following tracheostomy for COVID-19. Laryngoscope. 2021;131:E1918–E1925.
Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–17.
Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46:1303–25.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hernandez, G., Brenner, M., McGrath, B.A. (2021). Modernizing Tracheostomy Practice to Improve Resource Utilization and Survivorship Outcomes. In: Vincent, JL. (eds) Annual Update in Intensive Care and Emergency Medicine 2021. Annual Update in Intensive Care and Emergency Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-73231-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-73231-8_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-73230-1
Online ISBN: 978-3-030-73231-8
eBook Packages: MedicineMedicine (R0)