Abstract
According to the World Health Organization (WHO) 2016 classification, secondary acute myeloid leukemia (sAML) is included in two diagnostic groups: therapy-related myeloid neoplasms (t-MN), along with therapy-related myelodysplastic syndrome/myeloproliferative neoplasm (MDS/MPN); and myelodysplasia-related changes with acute myeloid leukemia (MRC-AML), along with non-secondary AML subtypes. The incidence of sAML is estimated to be between 20 and 30% of all AML, with most of them having a prior history of MDS or MPN. Although sAML has commonly been considered an independent adverse prognostic condition, this might be questionable as sAML is closely related to older age, comorbidities, worse performance status (PS), and unfavorable genetic features. These baseline characteristics also lead physicians to frequently consider sAML patients unfit to receive curative therapies or be included in clinical trials. While several cytostatic drugs, such as alkylating agents or topoisomerase II inhibitors, have clearly been related to therapy-related AML (t-AML), other mechanisms and pathways that contribute to transformation to sAML have not been well established. The clinical presentation in sAML patients is similar to de novo, as a result of bone marrow insufficiency and tumor burden, while other signs and symptoms can be present depending on the type of sAML or the comorbidities, which could be consequence of previous disorders or treatments, and even due to the activity of the primary neoplasia. Enrolling sAML patients in clinical trials should be a priority, and whenever possible, they should be referred to an appropriate research center where experimental options are available. Beyond trials, therapy in sAML patients is based on intensive chemotherapy, with a combination of cytarabine for 7 days plus an anthracycline for 3 days, mainly idarubicin or daunorubicin, or more recently using CPX-351. After induction therapy, allogeneic hematopoietic stem cell transplantation (HSCT) is often the most recommended post-remission treatment. Patients considered unfit to receive 3 + 7 therapy may benefit from non-intensive approaches, such as hypomethylating agents (HMAs), or recently approved targeted therapies. Given the challenging condition that they represent, obtaining improvements in sAML should be a priority, warranting that this field is becoming an active research area in the forthcoming years.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
4.1 Introduction
Secondary acute myeloid leukemia (sAML) comprises all AML cases diagnosed after receiving cytotoxic agents, radiation therapy, immunosuppressive treatments, and those arising from prior hematologic disorders, such as myelodysplastic syndromes (MDS) or myeloproliferative neoplasms (MPN) (Hulegårdh et al. 2015; Østgård et al. 2010; Godley and Larson 2008; Larson 2007). According to the 2016 World Health Organization (WHO) classification, the majority of sAML are included in two different entities, therapy-related myeloid neoplasms (t-MN) and AML with myelodysplasia-related changes (AML-MRC). However, AML-MRC not only contains sAML, but also de novo AML with certain criteria (see below) (Arber et al. 2016; Döhner et al. 2017). Although it is generally believed that a higher risk to develop a t-MN exists after a primary neoplasia, there is no consensus on whether it is due to an individual predisposition for developing tumors or a consequence of prior exposure to leukemogenic agents. The term AML with antecedent hematological disorders (AHD-AML) can be used for AML derived from MDS or MPN, but also for those cases in which a prior diagnosis of MDS or MPN was suspected on the basis of documented blood count abnormalities. The term AHD-AML has been abandoned by the WHO, and has been replaced by MRC-AML, which is more inclusive and accurate. As sAML patients achieve lower complete remission (CR) rates and shorter overall survival (OS) compared with de novo AML, the diagnosis of sAML has been considered an independent prognostic factor per se (Larson 2007; Stölzel et al. 2011; Pulsoni and Pagano 2005; Rizzieri et al. 2009). However, its independent prognostic value has been questioned because sAML is associated with other well-established adverse prognostic features such as older age, worse performance status (PS), and unfavorable cytogenetic or molecular profile (Østgård et al. 2010; Stölzel et al. 2011; Pulsoni and Pagano 2005; Rizzieri et al. 2009).
Secondary acute promyelocytic leukemia (sAPL) cases are almost exclusively diagnosed after a primary neoplasia treated with chemotherapy, radiotherapy, or immunosuppressive agents for a previous non-malignant disease, and the term therapy-related APL (t-APL) is recommended (Lo-Coco et al. 2013). In contrast to sAML, only anecdotal cases of sAPL evolving from MDS or MPN have been reported. The available evidence shows a relationship between developing t-APL and prior exposure to alkylating agents and topoisomerase II inhibitors (Beaumont et al. 2003; Mays et al. 2010; Mistry et al. 2005; Cowell and Austin 2012). Unlike sAML, main characteristics and clinical outcomes of t-APL seem similar to de novo APL, and prognosis of t-APL patients is significantly better than in patients with other t-MN (Lo-Coco et al. 2013; Pulsoni et al. 2002).
4.2 Epidemiology
The reported incidence of sAML ranges between 20 and 30% of all AML cases (Juliusson et al. 2009; Bertoli et al. 2017; Medeiros et al. 2015; Hulegårdh et al. 2015; Østgård et al. 2010, 2015; Gangatharan et al. 2013; Szotkowski et al. 2010). Nevertheless, the real frequency could be higher as sAML patients are usually excluded from clinical trials and protocols. Furthermore, it is difficult to calculate how many patients diagnosed with de novo AML had previously an undiagnosed MDS or MPN (Sengsayadeth et al. 2018). It is estimated that in two-thirds of patients, the sAML was preceded by MDS or MPN, whereas one-third of them are considered t-MN (86% related to cytotoxic agents or radiation therapy and 13% after immunosuppressive treatments) (Hulegårdh et al. 2015; Østgård et al. 2010). In patients younger than 40 years, t-AML occurs in about 5% of cases, and its prevalence increases up to 10% in patients above 40 years. Likewise, AHD-AML is uncommon before the age of 40 years, increasing up to 30% between 70 and 79 years (Hulegårdh et al. 2015). Table 4.1 shows the main studies reporting the frequency of sAML.
Regarding secondary APL, few studies have reported the frequency of t-APL, ranging from 15 to 21% of all APL cases (Braun et al. 2015; Beaumont et al. 2003; Elliott et al. 2012). Although overall t-APL incidence appears to be constant throughout the time, some authors suggest that evolving treatment strategies for breast cancer (with less frequent use of alkylating agents, topoisomerase II inhibitors, and anthracyclines) could have decreased its occurrence in this setting (Braun et al. 2015).
4.3 Etiology and Pathogenesis
Prior exposure to cytotoxic drugs, radiation therapy, or immunosuppressive agents for treating neoplastic or non-neoplastic diseases are considered etiopathogenetic factors for the development of t-AML. Several cytostatic drugs, such as alkylating agents or topoisomerase II inhibitors, have clearly been related to the development of sAML, and thus were defining pathological entities according to 2001 WHO classification (Mistry et al. 2005; Kayser et al. 2017; Schoch et al. 2004; Felix 1998). However, since the WHO 2008 version, these subgroups were no more independent entities (Vardiman 2008), and the t-AML definition included other types of therapy, as no practical advantages were expected from further subcategorizations. Although t-AML seems to increase with age (median age at diagnosis is around 69 years) (Østgård et al. 2010), it can be found in younger patients, too. It has been proposed that some younger patients may have inheritable predisposition to the development of t-AML (Godley and Larson 2008).
The pathogenesis of t-AML may occur by direct induction of a fusion oncogene through chromosomal translocation, induction of genome instability, or selection of pre-existing treatment-resistant hematopoietic cell clones (Heuser 2016). The latter mechanism can explain the high frequency of TP53 mutations in patients with t-AML. Longitudinal assessments performed in some t-AML patients showed that these mutations were detected at low-variant allele frequency before AML diagnosis and even before exposure to any cytotoxic therapy. Thus, it has been suggested that chemotherapy or radiotherapy may not directly induce TP53 mutations but more probably select TP53 mutated clones of hematopoietic progenitor cells, which may expand after treatment for primary neoplasia. Moreover, de novo AML and t-AML show a similar percentage of therapy-related transversions and number of somatic nucleotide variants, suggesting that prior treatment may not inflict genome-wide DNA damage (Wong et al. 2015; Takahashi et al. 2017; Ok et al. 2015a).
The genetic evolution from MDS to sAML is not well known. Studies based on whole genome sequencing have shown that bone marrow cells from patients diagnosed with MDS progressing to sAML are clonally derived throughout a dynamic process based on numerous cycles of mutation acquisition and clonal selection (Walter et al. 2012). During this progression, acquired mutations often interfere with normal hematopoietic differentiation (e.g., mutations in RUNX1, GATA2, and CEBPA) and/or activate signaling pathways that upregulate proliferation (e.g., mutations in FLT3 or RAS family members) (Sperling et al. 2017).
Although the mechanisms and pathways that contribute to transformation from MPN to AML have not been well established, two distinct routes for leukemic transformation have been described: (1) JAK2/MPL-positive MPN progress to JAK2/MPL-positive AML—this pathway is associated with the acquisition of additional genetic alterations, and (2) JAK2/MPL-positive MPN progress to JAK2/MPL-negative AML, which are clonally related on account of a pre-JAK2/MPL-mutant clone (Zhang et al. 2012; Abdel-Wahab et al. 2010; Harutyunyan et al. 2011; Green and Beer 2010; Theocharides et al. 2007; Campbell et al. 2006). Some studies have shown that post-MPN-AML has a somatic mutational spectrum different from that observed in de novo AML (e.g., JAK2V617F mutations are rare in de novo AML, and AML patients with JAK2V617F mutations normally have a history of previous MPN; moreover common mutations in de novo AML, such as NPM1 and FLT3, are usually absent in MPN-AML) (Fröhling et al. 2006a). In addition, MPN-AML is frequently characterized by mutations in TP53, IDH2, and ASXL1, and the acquisition of these somatic mutations may contribute to the progression from MPN to AML (e.g., loss of TP53 in combination with expression of JAK2V617F results in the development of post-MPN-AML) (Rampal et al. 2014).
The latency period between diagnosis of the primary disease or previous cytostatic therapy and sAML can range from few months to several years. While the median latency was 1.1 years in MDS-AML (Hulegårdh et al. 2015), leukemic transformation occurs over a 10-year period in essential thrombocythemia (7.6 years), polycythemia vera (7.3 years), and primary myelofibrosis (Cervantes et al. 1991). Median latency time in t-AML can vary between 4.0 and 6.2 years, being shorter after malignancies (5.8 years) and longer after non-malignant disorders (14.3 years) (Hulegårdh et al. 2015; Kayser et al. 2011). The latency period could depend on the cumulative dose, dose intensity, and type of preceding chemotherapy and/or radiation therapy (Godley and Larson 2008; Borthakur and Estey 2007). For instance, after receiving alkylating agents and/or radiation, patients can develop a t-AML in 5–10 years. However, patients who receive agents targeting topoisomerase II have often shorter latency period, approximately 1–5 years. In any case, such discrimination according to type of preceding therapy is not realistic, as patients often receive various types of agents. However, controversial data arise from some studies, which showed similar latency periods in patients with solid cancer who had not been exposed to previous therapy compared with those exposed to chemotherapy (Østgård et al. 2015). These findings suggest that, beyond clonal hematopoiesis selection or direct damage by leukemogenic agents, there might be a potential role of immune escape mechanisms in the pathogenesis of sAML in patients with a primary malignancy or autoimmune disease.
Regarding APL patients, those diagnosed with t-APL are older than those with de novo APL (mean age, 60.2 vs 48.7 years, respectively) (Braun et al. 2015). There is more prevalence of female gender, which may be related to the higher incidence of breast cancer and autoimmune diseases among primary disorders in female patients (Lo-Coco et al. 2013; Pulsoni et al. 2002; Kayser et al. 2017). The knowledge of the molecular pathogenesis of t-APL gained insights after identification of the role of DNA topoisomerase II (TOP2), a dimeric enzyme that plays an essential role in replication, transcription, chromosome condensation, and segregation. TOP2 facilitates one double-stranded DNA segment to pass through another, thus altering DNA topology. Before the re-ligation step, each monomer of TOP2 remains linked to DNA, forming double-strand breaks (DSB). Topoisomerase II inhibitors interfere in this re-ligation step, resulting in accumulation of DSB, which are cytotoxic and lead to apoptosis thought activation of the DNA damage response. Thus, chemotherapy-induced lesions are poorly repaired and generate a wide variety of genetic alterations like novel fusion genes, including t(15,17)(PML-RARA) (Mistry et al. 2005; Cowell and Austin 2012). Uneven distribution of DNA breakpoints at both PML and RARA loci suggest the existence of specific pathogenetic mechanisms in t-APL as compared with de novo APL (Hasan et al. 2010).
Latency between primary disorder and t-APL diagnosis ranges from few months to several years, with a median interval lower than 3.5 years (Kayser et al. 2017). Treatment with topoisomerase II-targeted drugs has commonly been related to shorter latency period, but recent studies suggested that only younger age at diagnosis of primary disorder was correlated with a shorter latency time (Beaumont et al. 2003; Kayser et al. 2011, 2017).
4.4 Clinical Features
Clinical presentation of sAML is variable and, similar to de novo AML, depending on three main factors: (1) bone marrow insufficiency, (2) presence of extramedullary disease, and (3) number of white blood cell (WBC) counts and presence of thrombogenic factors.
-
Clinical features related to medullar insufficiency:
-
Anemia: weakness, fatigue, tachycardia, dyspnea, headache, etc.
-
Neutropenia: fever and infections
-
Thrombocytopenia: hemorrhage symptoms (coagulopathy, gingival bleeding, epistaxis, menorrhagia, etc.)
-
-
Clinical features related to extramedullary disease:
-
Central nervous system (neurological disorders)
-
Hepatomegaly, splenomegaly, and lymphatic nodes
-
Skin (leukemia cutis)
-
Gingival hyperplasia
-
Granulocytic sarcoma
-
-
Clinical features related to number of WBC and release of intracellular substances:
-
Leukostasis (frequently related to hyperleukocytosis): lungs (respiratory failure, infiltrates), central nervous system (neurological disorders without blast cells in cerebrospinal fluid)
-
Thrombogenic substances delivery (coagulopathy, disseminated vascular coagulopathy with fibrinogen decreased, and thrombosis)
-
Tumor lysis syndrome: hyperuricemia, creatinine increase, hypocalcemia, hyperkalemia, hyperphosphatemia
-
In relation with the aforementioned characteristics, some patients can present at diagnosis some specific features according to the type of sAML. MPNs are hematopoietic disorders characterized by clonal proliferation of mature myeloid elements that manifest clinically as an excess of red blood cells, platelets, or WBC (Campbell et al. 2006). In these instances, sAML may present clinical symptoms related to the previous MPN, such as hepatomegaly and splenomegaly, or other manifestations related to the increased number of peripheral blood cells. AML from MDS is usually less proliferative and t-AML patients can show signs and symptoms of hematopoietic insufficiency due to prior antineoplastic therapies, in addition to damage in different organs because of therapy-related sequalae (Appelbaum et al. 2006). Moreover, concomitant activity or relapse of previous tumors can complicate the clinical course of t-AML.
Characteristics of t-APL seem to be similar to de novo APL, with no differences reported for baseline hemoglobin, WBC, or platelets counts (Lo-Coco et al. 2013; Beaumont et al. 2003; Yin et al. 2005). However, like non-APL sAML, t-APL patients are older than de novo APL and have worse PS at diagnosis, which may determine the treatment choice and the outcomes (Lo-Coco et al. 2013; Pulsoni et al. 2002).
4.5 Diagnosis
Diagnosis of AML is based on morphological findings, so the detection of ≥20% blast cells in peripheral blood or bone marrow is a requisite, except for t(8;21), t(16:16)/inv(16), or t(15;17). Although dysplasia is frequent in sAML, its presence is not a diagnostic criteria (Arber et al. 2016; Döhner et al. 2017).
sAML diagnosis requires a documented clinical history of previous diagnosis of MDS, MPN, or MDS/MPN (AHD-AML); or prior treatment with chemotherapy, radiotherapy, or immunosuppressive therapy for an unrelated malignancy or immune disorder (t-AML).
Immunophenotypic characterization by multiparameter flow cytometry (MFC) can be helpful to support the diagnosis of sAML, distinguishing myeloid lineage from ambiguous, mixed, or lymphoid leukemias, which might be classified as different entities. Another utility of MFC is to detect the minimal residual disease (MRD) after initial therapy, allowing to establish relapse risk in order to adapt the intensity of post-remission strategies.
Cytogenetics and molecular tests remain mandatory in the assessment of AML, in order to complete diagnosis and to identify those sAML patients with favorable recurrent genetic abnormalities (RGAs) who may benefit from intensive approaches not including allogeneic stem cell transplant. In addition to conventional karyotyping, fluorescent in situ hybridization (FISH) and reverse transcription polymerase chain reaction (RT-PCR) are useful tools to classify sAML patients. According to the 2017 panel of European Leukemia Net experts, genetic risk can be stratified in favorable, intermediate, and adverse, in both de novo AML and sAML.
The relevance of chromosomal alterations and gene variants for diagnosis, risk stratification, and choice of targeted therapies (i.e., FLT3 and IDH1/2 inhibitors) has remarkably increased the complexity of routine molecular diagnostic strategies. Next-generation sequencing (NGS) has been established as a new molecular diagnostic tool rapidly adopted by clinical laboratories, being able to simultaneously assess different genetic alterations such as rearrangements, single nucleotide variants, insertions-deletions, and copy number variations in a wide variety of genes. NGS gene panels have been preferentially adopted rather than whole genome or exome sequencing due to an easier interpretation of results, lower cost, and less time. As compared to NGS, conventional single-gene approaches by PCR are laborious and less efficient to detect minor clones, but they are still needed as rapid-screening tests for druggable variants. In addition, NGS has some limitations, which are often restricting its use to the context of research programs.
As compared to de novo AML, some gene mutations could be more frequent in t-AML patients (TP53 [36%], PTPN11 [12%], NRAS [10%], KRAS [5%]), equally frequent (IDH1 [10%], IDH2 [10%]), or less frequent (FLT3 [7%], DNMT3A [7%]) (Ok et al. 2015a).
No differences have been reported regarding morphological and immunophenotypic characterization between t-APL and de novo APL (Duffield et al. 2012). To diagnose t-APL, demonstration of the t(15;17) or PML/RARA rearrangement is also mandatory. Some studies suggested that patients developing t-APL after mitoxantrone show a higher prevalence of long-type (bcr 1) PML/RARA isoform due to a specific DNA-break hotspot in the PML gene (Hasan et al. 2008). However, this has not been confirmed later (Kayser et al. 2017). It is expected that NGS studies will help to elucidate the genetic features of t-APL and the potential differences with de novo APL (Lo-Coco et al. 2013).
4.6 Classification
According to the WHO 2016 classification, patients diagnosed with AML diagnosed after receiving cytotoxic drugs, radiation therapy, or immunosuppressive agents for neoplastic and non-neoplastic diseases should be classified in the t-MN group (Arber et al. 2016; Döhner et al. 2017). However, this designation includes also patients diagnosed with MDS or MDS/MPN after mutagenic therapy, so t-AML seems to be a better term to differentiate AML from other t-MN diseases (Kayser et al. 2017). According to the WHO 2016, if a recurrent genetic abnormality is diagnosed, this should be added to the nomenclature (see Table 4.2). It remains controversial whether well-defined entities with particular treatment approaches and prognosis, such as APL or core-binding-factor (CBF) AML, should be included in the t-MN cluster, as recommended by WHO, or could preferably remain in their respective groups of recurrent genetic abnormalities.
The 2016 WHO AML with myelodysplasia-related changes (MRC-AML) is a wide entity that encompasses both sAML and de novo AML. The WHO 2001 defined AML with multilineage dysplasia (AML-MLD) as a new category, which was only defined by the presence of ≥50% dysplastic abnormalities in ≥2 hematopoietic cell lines. The AML-MLD was replaced by the MRC-AML in the WHO 2008 revision since several studies showed that MLD was not an independent factor when cytogenetics was incorporated into the prognostic models (Vardiman et al. 2009). With hindsight, more authors have insinuated the lack of prognostic significance of MLD (Miesner et al. 2010).
The WHO 2008 AML-MRC is defined as AML (≥20% blasts of bone marrow [BM] or peripheral blood [PB]) with at least one of the following criteria: (1) ≥50% dysplastic abnormalities in ≥2 hematopoietic cell lines (MLD); (2) prior history of MDS or MDS/MPN; and (3) MDS-related cytogenetic abnormalities and absence of recurrent genetic abnormalities.
Regarding MLD assessment, these are the current recommendations by WHO:
-
Dysgranulopoiesis: 25–100 neutrophils—hypogranular cytoplasm, hyposegmented nuclei or bizarrely segmented nuclei, cytoplasmic vacuoles—myeloperoxidase deficiency (50%, 20 cells)
-
Dyserythropoiesis: at least 25 mature erythroblasts—megaloblastosis, karyorrhexis and nuclear irregularity, fragmentation or multinucleation—ring sideroblasts, PAS positivity
-
Dysmegakaryopoiesis: at least six megakaryocytes—micromegakaryocytes, normal sized, or large megakaryocytes with non-lobulated or multiple nuclei
According to the WHO 2016 update, patients diagnosed with MRC-AML must meet at least one of the following criteria (along with the absence of both prior cytotoxic therapy for unrelated disease and recurrent genetic abnormalities [RGA]):
-
Previous history of MDS or MDS/MPN
-
Myelodysplasia-related cytogenetic abnormality (see Table 4.2)
-
Multilineage dysplasia (see Table 4.2)
Thus, AML patients with a medical history of hematologic disorder who have received therapy for any unrelated disease or show any RGA should not be classified as MRC-AML. Table 4.2 shows detailed information regarding sAML classification according to antecedent disorders, presence of RGA, and WHO 2016 terminology.
Although the WHO pathological classification attempts to define biologically homogeneous entities with similar prognosis, the WHO definitions should be used together with age, performance status (PS), cytogenetics, and molecular profile in order to decide the best available regimen for each entity and patient (Hulegårdh et al. 2015; Juliusson et al. 2009; Nilsson et al. 2019).
4.7 Prognosis
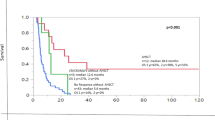
Similar to de novo AML patients, the prognosis of sAML patients is related to several factors as age, PS, cytogenetics, and molecular profile (Fig. 4.1) (Wheatley et al. 2009). However, sAML patients are often older, with worse PS and genetic features, so they tend to be more frequently considered unfit for intensive chemotherapy. Other baseline characteristics, such as WBC counts, previous comorbidities, or response to induction treatment, have been also associated with worse prognosis in AML (Wheatley et al. 2009; Schoch et al. 2004). It is expected that sAML patients could present with more comorbidities, since prior treatments or malignant disorders could have caused sequelae (e.g., other organ damage, low hematopoietic stem cell reserve, persistence of malignant disease). In addition, the prognostic impact of some well-established gene mutations in sAML is unclear (e.g., FLT3, NPM1), as available data mainly derive from studies performed in de novo AML patients with normal karyotype.
The dilemma about considering sAML as an independent prognostic factor remains unsolved as published manuscripts revealed discrepant results (Juliusson et al. 2009; Wheatley et al. 2009; Fröhling et al. 2006b; Szotkowski et al. 2010). Some studies have shown a different prognosis depending on the type of sAML: MPN patients who develop a leukemic transformation show the worst clinical outcomes, with a median survival between 6–11 months and 1-year OS of 10%, which is worse than 20% in t-AML, 41% in de novo AML, and 43% in AML from MDS (Østgård et al. 2015; Mesa et al. 2005; Thepot et al. 2010). As in de novo AML, molecular and cytogenetic changes play a relevant role in establishing the prognosis of sAML. t-AML patients with CBF have a longer OS than those with intermediate and adverse genetic risk, but prognosis seems to be worse than in de novo CBF AML patients (Borthakur et al. 2009). Mutations and loss of heterozygosity of TP53, which have been identified as independent negative prognostic factors for OS, are common in sAML (reported in 17–37% of t-MN patients) (Christiansen et al. 2001; Ok et al. 2015b). Similarly, shorter OS has also been observed in t-MN patients with amplification of the MLL gene, compared with patients without these mutations (Andersen et al. 2001). Table 4.3 shows the main studies analyzing the prognostic factors in sAML.
Unlike t-MN, the prognosis of t-APL is favorable with anthracycline-based chemotherapy plus all-trans-retinoic acid (ATRA) or ATRA plus arsenic trioxide (ATO). Several studies showed a similar prognosis as compared to de novo APL, particularly after adjusting by age and PS (Ammatuna et al. 2011; Dayyani et al. 2011; Lo-Coco et al. 2013).
4.8 Treatment
The optimal treatment options for sAML patients are not yet established. This therapeutic dilemma comes from the lack of well-designed studies in this subset of patients, as they are commonly excluded from trials and protocols (Juliusson et al. 2009; Mengis et al. 2003).
Despite new advances, front-line therapy remains a challenge in sAML. In addition to older age and worse PS of these patients, deteriorated baseline characteristics because of the preceding treatments or concomitant malignant disease activity must be taken into account to judge the best approach for each patient. As in de novo AML, genetic and molecular characterization is mandatory for the initial risk-assessment of sAML patients, which can be categorized in favorable, intermediate, and adverse groups. Although, in general, we can recommend that sAML patients should receive similar treatment as de novo AML, specific characteristics of sAML patients may justify a distinct approach in some instances. Table 4.4 shows detailed information on studies who analyzed treatment outcomes in sAML.
4.8.1 Younger Patients
As in young patients with de novo AML, induction therapy in sAML is based on intensive 3 + 7 chemotherapy, with a combination of cytarabine for 7 days plus an anthracycline for 3 days, usually idarubicin or daunorubicin. Nevertheless, other schedules have also been explored (Döhner et al. 2017; Fey and Buske 2013; Tallman et al. 2019; De Kouchkovsky and Abdul-Hay 2016; Lee et al. 2011; Burnett et al. 2013; Zeidner et al. 2015; Stone et al. 2015; Lee et al. 2017; Holowiecki et al. 2012; Burnett et al. 2015). Due to the high risk of relapse, the majority of sAML fit patients achieving a first complete remission (CR) will be candidates to receive an allogeneic hematopoietic stem cell transplantation (HSCT). In consequence, an early search for a suitable donor should be started at diagnosis. After achieving CR, consolidation cycles with high-dose cytarabine-based schedules are recommended for patients with optimal PS and favorable cytogenetic risk. In contrast, the preferred strategy to achieve long-term survival in patients with intermediate-risk genetics is to perform an allogeneic HSCT (De Kouchkovsky and Abdul-Hay 2016; Li et al. 2018; Sengsayadeth et al. 2018; Litzow et al. 2010; Yakoub-Agha et al. 2000). Unfortunately, the prognosis in patients with poor-risk cytogenetics is dismal, regardless of the treatment administered. Despite this, allogeneic HSCT remains the most appropriate post-remission modality for patients with high-risk cytogenetics sAML, especially in younger patients with good PS (Sengsayadeth et al. 2018; Kennedy et al. 2013). Few data have been published comparing patients with or without HSCT after induction therapy in sAML patients. Although treatment-related mortality and toxicity after allogeneic HSCT is suspected to be higher in sAML patients than in de novo AML, allogeneic HSCT improves survival and is considered the only realistic curative option in patients with sAML (Nilsson et al. 2019).
In younger patients who are considered unfit for intensive schedules (e.g., because of another active malignancy or end-organ failure), front-line approaches using hypomethylating agents (HMAs) could prolong OS (Zeichner and Arellano 2015).
As a general recommendation, participating in clinical trials should be the preferred option for all sAML patients (Fey and Buske 2013; Tallman et al. 2019).
4.8.2 Older Patients
Older patients (especially those aged more than 70–75 years) are usually considered unfit and often receive non-curative schemes or supportive care exclusively. Intensive therapies in older patients are limited to those with optimal PS, and considered able to withstand very toxic schedules (Löwenberg et al. 1998; Anderson et al. 2002). In the last decades, through a more accurate risk stratification of patients and improvements in supportive therapy, intensive schedules have also been a more accessible option for some older patients, mainly in those with favorable genetic risk (Zeidner et al. 2015; Stone et al. 2015; Löwenberg et al. 2009; Chauncey et al. 2010; Röllig et al. 2010; Müller-Tidow et al. 2016; Lancet et al. 2014). On the contrary, patients with poor PS, poor cytogenetics, high age (>75 years old), active malignant disease, or serious comorbidities should be considered for non-intensive approaches (e.g., HMAs, low-dose cytarabine [LDAC]) (Dumas et al. 2017).
Due to the poor prognosis, enrolment in clinical trials also remains the first option in this population (Fey and Buske 2013; Tallman et al. 2019). This strategy could allow some patients to benefit from innovative treatments and targeted therapies.
4.8.3 APL
Patients diagnosed with t-APL must receive therapeutic approaches comprising differentiating agents, such as anthracycline-based chemotherapy plus all-trans-retinoic acid (ATRA) or ATRA plus arsenic trioxide (ATO). Several studies have reported comparable results in t-APL as comparted to de novo APL in patients treated with ATRA plus chemotherapy regimens, while there is scarce information for t-APL patients treated with ATO-based regimens (Beaumont et al. 2003; Pulsoni et al. 2002; Elliott et al. 2012; Kayser et al. 2017; Dayyani et al. 2011). ATO plus ATRA regimens are now considered standard front-line for low- and intermediate-risk de novo APL, and are under investigation for high-risk patients (>10 × 109/L WBC counts). As t-APL patients are systematically excluded from clinical trials, clinical outcomes under chemotherapy-free approaches must be extrapolated from studies performed in de novo cases. Although upfront approaches with ATRA plus anthracycline can be suitable for t-APL, chemotherapy-free schedules are more appealing for t-APL patients to avoid additive toxicity of chemotherapy (Kayser et al. 2017; Dayyani et al. 2011). As suggested by some authors, the cumulative dose of chemotherapy may be related to higher rates of death during induction, higher incidence of toxic death, and development of t-MN after APL (Kayser et al. 2017).
4.8.4 New Approaches
Novel therapies have recently been approved for the treatment of AML. Although the majority of studies have focused on de novo AML patients, some of the following agents have been properly evaluated in sAML.
4.8.4.1 CPX-351
CPX-351 (Vyxeos®, Jazz Pharmaceuticals) is a liposomal formulation of cytarabine and daunorubicin at a 5:1 molar ratio, which is delivered into leukemic cells (Kim et al. 2011; Lim et al. 2010). CPX-351 liposomes could deliver daunorubicin and cytarabine in optimal ratio to maintain a synergistic effect. In addition, the liposomal formulation could lead to selective accumulation of both drugs in the bone marrow.
In a randomized phase 3 trial, CPX-351 showed longer OS and higher CR plus CR with incomplete recovery (CRi) rate in comparison with 7 + 3 schedule (median OS: 9.6 vs 5.6 months, p = 0.005; and CR + CRi: 47.7% vs 33.3%, p = 0.016, respectively) in fit patients aged between 60 and 75 years with untreated AML and the following characteristics: t-AML, MDS-AML with and without prior HMA, AML with a history of chronic myelomonocytic leukemia (CMML), and de novo AML with MDS-related cytogenetic abnormalities (Lancet et al. 2018).Toxicity was similar in both groups.
Currently, CPX-351 is the only therapy specifically approved for adults with newly diagnosed t-AML and MRC-AML by the US Food and Drug Administration (FDA) since 2017 and by the European Medicines Agency (EMA) since 2018 (Talati and Lancet 2018; Vyxeos n.d.).
4.8.4.2 Venetoclax
Venetoclax (Venclyxto/Venclexta®, AbbVie) is a small-molecule inhibitor of Bcl-2 that targets AML cells whose survival could depend on anti-apoptotic proteins of the Bcl-2 family (Mihalyova et al. 2018).
Two studies contributed to the approval of venetoclax by the FDA in 2018, in combination with azacitidine or decitabine or LDAC, for the treatment of adult newly diagnosed AML patients aged 75 years or older, or who have comorbidities that preclude use of intensive induction chemotherapy (VENCLEXTA 2018). One of them was a phase 1/2 trial in which venetoclax plus LDAC was tested in 82 older patients with untreated AML, showing a CR + CRi rate of 35% in the group of patients with sAML (which represented 49% of the study cohort) (Wei et al. 2019). A phase 1b study explored venetoclax combined with HMA therapy (decitabine or azacitidine) in a similar cohort, but enrolled subjects could not have received HMAs for prior MDS or MDS/MPN. The CR + CRi rate in the subset of patients with sAML was 67% (DiNardo et al. 2019). Continued FDA approval for this indication is contingent upon verification of clinical benefit in confirmatory trials. Recently, the phase 3 trial VIALE-C comparing venetoclax plus LDAC versus placebo plus LDAC failed its primary endpoint of OS, although this was almost doubled in the experimental arm.
4.8.4.3 Gemtuzumab Ozogamicin (GO)
Gemtuzumab ozogamicin (GO; Mylotarg™, Pfizer) is a conjugate of an anti-CD33 antibody and the toxin calicheamicin. Its mechanism of action is based on the advantage of selective expression of CD33 by leukemic cells, but not in normal hematopoietic stem cells (Appelbaum and Bernstein 2017; Jen et al. 2018).
GO was approved by the FDA in 2017 and the EMA in 2018 for the treatment of adult patients with newly diagnosed CD33-positive AML, in combination with standard cytarabine and daunorubicin. Moreover, GO was also approved by the FDA as monotherapy for the treatment of patients ≥2 years of age with relapsed/refractory CD33-positive AML.
Although recent clinical trials have evaluated the possibility of adding GO to traditional schedules for the treatment of sAML patients, their results have not supported further development in this setting (de Witte et al. 2015; Burnett et al. 2011).
4.8.4.4 Glasdegib
The hedgehog signaling pathway is an attractive novel therapeutic target because of its biologic role in the maintenance and expansion of leukemic stem cells and the acquisition of a drug-resistant phenotype in AML (Aberger et al. 2017; Campbell and Copland 2015). Glasdegib (Daurismo™, Pfizer) blocks hedgehog signaling by inhibiting Smoothened, a transmembrane receptor with an integral function in the canonical hedgehog pathway (DAURISMO 2018).
In a randomized phase 2 study performed in unfit patients with newly diagnosed AML or high-risk MDS, glasdegib in combination with LDAC showed longer OS and achieved a higher CR rate than LDAC alone (Cortes et al. 2019). Afterward, glasdegib plus LDAC was approved by the FDA in 2018 for the treatment of newly diagnosed adult AML patients aged ≥75 years or who have comorbidities that preclude use of intensive induction chemotherapy (DAURISMO 2018). However, analysis of sAML patient group included in this study has not yet been published.
4.8.4.5 IDH Inhibitors
Leukemic IDH1 and IDH2 mutations confer a neomorphic enzymatic activity, impairing hematopoietic differentiation and promoting leukemogenesis (Figueroa et al. 2010). Mutations in IDH1 occur in approximately 6–10% of patients with AML and IDH2 mutations occur in 9–13% (DiNardo et al. 2018). Similar incidence has been reported in sAML (Ok et al. 2015a).
Ivosidenib (Tibsovo®, Agios) and enasidenib (Idhifa®, Celgene) induce myeloid differentiation and reduce blast counts by inhibiting mutant IDH1 and mutant IDH2, respectively (IDHIFA 2017; TIBSOVO 2018). The approval of ivosidenib by the FDA in 2018 was based on results of a phase 1 study, performed in adult patients with relapsed/refractory IDH1-mutated AML (35% were sAML). With ivosidenib monotherapy, a CR + CRi rate of 30% was achieved (DiNardo et al. 2018). Enasidenib was approved by the FDA in 2017 for the treatment of adult patients with relapsed or refractory IDH2-mutated AML. The results of a phase 1/2 trial with a CR + CRi rate of 26% and median OS of 9.3 months led to its approval (Stein et al. 2017).
4.8.4.6 FLT3 Inhibitors
FMS-like tyrosine kinase 3 (FLT3) is a transmembrane receptor tyrosine kinase specially expressed on hematopoietic progenitor cells and is involved in differentiation and proliferation (Lyman and Jacobsen 1998; McKenna et al. 2000). FLT3-ITD mutation occurs less frequently in patients with sAML than in de novo (9% vs 26%, respectively) and predicts a poor prognosis (Fröhling et al. 2002; Stone et al. 2018). Midostaurin (Rydapt®, Novartis), a small-molecule inhibitor of FLT3, was approved by the FDA and EMA in 2017 for the treatment of adult patients with newly diagnosed FLT3-mutated AML, in combination with cytarabine and daunorubicin chemotherapy (Stone et al. 2018). In a randomized phase 3 RATIFY study, midostaurin plus conventional chemotherapy showed longer OS and EFS compared with chemotherapy alone in FLT3 mutated patients aged ≤60 years with newly diagnosed AML (Stone et al. 2017). Of note, sAML patients were excluded from the RATIFY trial. Gilteritinib (Xospata®, Astellas Pharma) is other FLT3 kinase inhibitor, recently approved by FDA in 2018 for the treatment of adult patients with relapsed/refractory AML (XOSPATA 2018). Unfortunately, t-AML patients were excluded in all phase 3 trials with FLT3 inhibitors, and no data for second-generation inhibitors (gilteritinib or quizartinib) have yet been published with regard to MDS-AML.
4.9 Future Directions
Currently, patients diagnosed with sAML have a dismal prognosis, either because of the adverse biological features of the disease or the patient’s clinical characteristics. Scientific groups are continuously updating their treatment protocols to design tailored therapies according to prognostic factors, including sAML as a relevant decision factor. Nevertheless, there is an increasing need to improve treatment strategies for sAML patients, which may represent one of the most challenging AML subsets. In particular, older patients with sAML may represent a very frequent subgroup where no specific approaches have been designed. There is room for advances in this challenging population, but these will be obtained only through well-designed specific protocols. In this regard, the clinical development of CPX-351, from phase 2 to phase 3, is a good example of success within this therapeutic area.
The better understanding of molecular mechanisms of leukemogenesis has led to the development of new targeted molecules focusing on actionable mutations and pathways. Unfortunately, patients with sAML are often excluded from clinical trials and only some new agents have been tested in this subset of patients with promising results. CPX-351 was approved for adults with newly diagnosed t-AML or MRC-AML, venetoclax in combination with LDAC or HMAs has remarkable activity in unfit subjects, glasdegib was shown to be able to benefit unfit sAML patients, and IDH1/IDH2 inhibitors may be an option at least for relapsed/refractory sAML.
Based on new scientific evidence, the treatment landscape in sAML may change toward: (1) replacement of conventional 7 + 3 chemotherapy by CPX-351 as a backbone for fit patients; (2) combination of CPX-351 with a FLT3 or IDH inhibitor in sAML fit patients with FLT3 or IDH mutations; and (3) combination of venetoclax with HMAs or LDAC for patients considered unfit to receive intensive chemotherapy. The role of targeted- vs venetoclax- vs triple combinations-based approaches for unfit sAML harboring actionable mutations must be elucidated in the future.
We should highlight two groups of sAML patients in whom therapeutic improvements have not been achieved yet. The first group constitutes MRC-AML following HMA therapy. These patients are systematically excluded from phase 3 clinical trials in which an HMA is the control arm, so no evidence-based advances will be available for these patients from the majority of ongoing phase 3 trials. Only the combinations of glasdegib plus LDAC or venetoclax plus LDAC regimens could be applied in these patients with some background evidence, but unfortunately those regimens do not represent a therapeutic breakthrough for this population. On the other hand, younger fit patients developing sAML after HMA therapy have been classically treated with 3 + 7 or similar regimens and more recently with CPX-351, showing poor clinical outcomes in both scenarios. The second group of very difficult-to-treat sAML is composed by MRC-AML evolving from MPN. These patients are usually excluded from clinical trials, including the recently sAML-focused CPX-351 phase 3 trial.
Additionally, some early development stage therapies for AML may become promising treatment approaches for sAML patients. Some examples are chimeric antigen receptor T cells or agents targeting the TP53 pathway, which should be evaluated in patients with sAML in forthcoming studies.
4.10 Conclusions
According to the 2016 WHO classification, sAML is included in two diagnostic groups: t-MN, along with therapy-related MDS/MPN; and MRC-AML, along with non-secondary AML subtypes (Arber et al. 2016; Döhner et al. 2017). The incidence of sAML is estimated between 20 and 30% of all AML (Juliusson et al. 2009; Bertoli et al. 2017; Medeiros et al. 2015; Hulegårdh et al. 2015; Østgård et al. 2010, 2015; Gangatharan et al. 2013; Szotkowski et al. 2010), with most of them having a prior history of MDS or MPN (Hulegårdh et al. 2015; Østgård et al. 2010). Although sAML has commonly been considered an independent adverse prognostic condition, this might be questionable as sAML is closely related to older age, comorbidities, worse PS, and unfavorable genetic features (Larson 2007; Stölzel et al. 2011; Pulsoni and Pagano 2005; Rizzieri et al. 2009). These baseline characteristics also lead physicians to frequently consider sAML patients unfit to receive curative therapies or be included in clinical trials.
The frequency of adverse features, such as older age, worse PS, and adverse karyotype and molecular profile, is by far higher in sAML than in de novo AML. However, the most relevant prognostic factor in AML is the therapeutic approach itself, which is probably intended as curative option in the minority sAML patients. Enrolling sAML patients in clinical trials should be a priority, and whenever possible, they should be referred to an appropriate research center where experimental options are available. Only patients with hopeless prognosis who do not meet criteria to participate in these studies should be approached in a palliative way. Given the challenging condition that they represent, obtaining improvements in sAML should be a priority, warranting that this field is becoming an active area of basic and clinical research in the forthcoming years.
References
Abdel-Wahab O, Manshouri T, Patel J et al (2010) Genetic analysis of transforming events that convert chronic myeloproliferative neoplasms to leukemias. Cancer Res 70(2):447–452. https://doi.org/10.1158/0008-5472.CAN-09-3783
Aberger F, Hutterer E, Sternberg C, Del Burgo PJ, Hartmann TN (2017) Acute myeloid leukemia—strategies and challenges for targeting oncogenic hedgehog/GLI signaling. Cell Commun Signal 15(1):8. https://doi.org/10.1186/s12964-017-0163-4
Ammatuna E, Montesinos P, Hasan SK et al (2011) Presenting features and treatment outcome of acute promyelocytic leukemia arising after multiple sclerosis. Haematologica 96(4):621–625. https://doi.org/10.3324/haematol.2010.036657
Andersen MK, Christiansen DH, Kirchhoff M, Pedersen-Bjergaard J (2001) Duplication or amplification of chromosome band 11q23, including the unrearranged MLL gene, is a recurrent abnormality in therapy-related MDS and AML, and is closely related to mutation of the TP53 gene and to previous therapy with alkylating agents. Genes Chromosom Cancer 31(1):33–41. https://doi.org/10.1002/gcc.1115
Anderson JE, Kopecky KJ, Willman CL et al (2002) Outcome after induction chemotherapy for older patients with acute myeloid leukemia is not improved with mitoxantrone and etoposide compared to cytarabine and daunorubicin: a southwest oncology group study. Blood 100(12):3869–3876. https://doi.org/10.1182/blood-2001-12-0354
Appelbaum FR, Bernstein ID (2017) Gemtuzumab ozogamicin for acute myeloid leukemia. Blood 130(22):2373–2376. https://doi.org/10.1182/blood-2017-09-797712
Appelbaum FR, Gundacker H, Head DR et al (2006) Age and acute myeloid leukemia. Blood 107(9):3481–3485. https://doi.org/10.1182/blood-2005-09-3724
Arber DA, Orazi A, Hasserjian R et al (2016) The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood 127(20):2391–2405. https://doi.org/10.1182/blood-2016-03-643544
Armand P, Kim HT, DeAngelo DJ et al (2007) Impact of cytogenetics on outcome of de novo and therapy-related AML and MDS after allogeneic transplantation. Biol Blood Marrow Transplant 13(6):655–664. https://doi.org/10.1016/j.bbmt.2007.01.079
Beaumont M, Sanz M, Carli PM et al (2003) Therapy-related acute promyelocytic leukemia. J Clin Oncol 21(11):2123–2137. https://doi.org/10.1200/JCO.2003.09.072
Bertoli S, Tavitian S, Huynh A et al (2017) Improved outcome for AML patients over the years 2000-2014. Blood Cancer J 7(12):1–8. https://doi.org/10.1038/s41408-017-0011-1
Borthakur G, Estey EE (2007) Therapy-related acute myelogenous leukemia and myelodysplastic syndrome. Curr Oncol Rep 9(5):373–377. https://doi.org/10.1007/s11912-007-0050-z
Borthakur G, Lin E, Jain N et al (2009) Survival is poorer in patients with secondary core-binding factor acute myelogenous leukemia compared with de novo core-binding factor leukemia. Cancer 115(14):3217–3221. https://doi.org/10.1002/cncr.24367
Braun T, Cereja S, Chevret S et al (2015) Evolving characteristics and outcome of secondary acute promyelocytic leukemia (APL): a prospective analysis by the French-Belgian-Swiss APL group. Cancer 121(14):2393–2399. https://doi.org/10.1002/cncr.29389
Burnett AK, Hills RK, Milligan D et al (2011) Identification of patients with acute myeloblastic leukemia who benefit from the addition of Gemtuzumab Ozogamicin: results of the MRC AML15 trial. J Clin Oncol 29(4):369–377. https://doi.org/10.1200/JCO.2010.31.4310
Burnett AK, Russell NH, Hills RK et al (2013) Optimization of chemotherapy for younger patients with acute myeloid leukemia: results of the medical research council AML15 trial. J Clin Oncol 31(27):3360–3368. https://doi.org/10.1200/JCO.2012.47.4874
Burnett AK, Russell NH, Hills RK et al (2015) A randomized comparison of daunorubicin 90 mg/m2 vs 60 mg/m2in AML induction: results from the UK NCRI AML17 trial in 1206 patients. Blood 125(25):3878–3885. https://doi.org/10.1182/blood-2015-01-623447
Campbell V, Copland M (2015) Hedgehog signaling in cancer stem cells: a focus on hematological cancers. Stem Cells Cloning Adv Appl 8:27–38. https://doi.org/10.2147/SCCAA.S58613
Campbell PJ, Baxter EJ, Beer PA et al (2006) Mutation of JAK2 in the myeloproliferative disorders: timing, clonality studies, cytogenetic associations, and role in leukemic transformation. Blood 108(10):3548–3555. https://doi.org/10.1182/blood-2005-12-013748
Cervantes F, Tassies D, Salgado C, Rovira M, Pereira A, Rozman C (1991) Acute transformation in nonleukemic chronic myeloproliferative disorders: actuarial probability and main characteristics in a series of 218 patients. Acta Haematol 85(3):124–127. https://doi.org/10.1159/000204873
Chauncey TR, Gundacker H, Shadman M et al (2010) Sequential phase II southwest oncology group studies (S0112 and S0301) of daunorubicin and cytarabine by continuous infusion, without and with ciclosporin, in older patients with previously untreated acute myeloid leukaemia. Br J Haematol 148(1):48–58. https://doi.org/10.1111/j.1365-2141.2009.07919.x
Christiansen DH, Andersen MK, Pedersen-Bjergaard J (2001) Mutations with loss of heterozygosity of p53 are common in therapy-related myelodysplasia and acute myeloid leukemia after exposure to alkylating agents and significantly associated with deletion or loss of 5q, a complex karyotype, and a poor prognosis. J Clin Oncol 19(5):1405–1413. https://doi.org/10.1200/JCO.2001.19.5.1405
Cortes JE, Heidel FH, Hellmann A et al (2019) Randomized comparison of low dose cytarabine with or without glasdegib in patients with newly diagnosed acute myeloid leukemia or high-risk myelodysplastic syndrome. Leukemia 33(2):379–389. https://doi.org/10.1038/s41375-018-0312-9
Cowell IG, Austin CA (2012) Mechanism of generation of therapy related leukemia in response to anti-topoisomerase II agents. Int J Environ Res Public Health 9(6):2075–2091. https://doi.org/10.3390/ijerph9062075
DAURISMO™ (glasdegib) tablets [packet insert]. New York: Pfizer Labs; 2018
Dayyani F, Kantarjian H, O’Brien S et al (2011) Outcome of therapy-related acute promyelocytic leukemia with or without arsenic trioxide as a component of frontline therapy. Cancer 117(1):110–115. https://doi.org/10.1002/cncr.25585
De Kouchkovsky I, Abdul-Hay M (2016) Acute myeloid leukemia: a comprehensive review and 2016 update. Blood Cancer J. 6(7):e441. https://doi.org/10.1038/bcj.2016.50
de Witte T, Suciu S, Meert L et al (2015) Idarubicin and cytarabine in combination with gemtuzumab ozogamicin (IAGO) for untreated patients with high-risk MDS or AML evolved from MDS: a phase II study from the EORTC and GIMEMA leukemia groups (protocol 06013). Ann Hematol 94(12):1981–1989. https://doi.org/10.1007/s00277-015-2486-9
DiNardo CD, Stein EM, De Botton S et al (2018) Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J Med 378(25):2386–2398. https://doi.org/10.1056/NEJMoa1716984
DiNardo CD, Pratz K, Pullarkat V et al (2019) Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood 133(1):7–17. https://doi.org/10.1182/blood-2018-08-868752
Döhner H, Estey E, Grimwade D et al (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129(4):424–447. https://doi.org/10.1182/blood-2016-08-733196
Duffield AS, Aoki J, Levis M et al (2012) Clinical and pathologic features of secondary acute promyelocytic leukemia. Am J Clin Pathol 137(3):395–402. https://doi.org/10.1309/AJCPE0MV0YTWLUUE
Dumas PY, Bertoli S, Bérard E et al (2017) Azacitidine or intensive chemotherapy for older patients with secondary or therapy-related acute myeloid leukemia. Oncotarget 8(45):79126–79136. https://doi.org/10.18632/oncotarget.15988
Elliott MA, Letendre L, Tefferi A et al (2012) Therapy-related acute promyelocytic leukemia: observations relating to APL pathogenesis and therapy. Eur J Haematol 88(3):237–243. https://doi.org/10.1111/j.1600-0609.2011.01727.x
Felix CA (1998) Secondary leukemias induced by topoisomerase-targeted drugs. Biochim Biophys Acta 1400(1-3):233–255. https://doi.org/10.1016/S0167-4781(98)00139-0
Fey MF, Buske C (2013) Acute myeloblastic leukaemias in adult patients: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 24 Suppl 6:vi138–vi143. https://doi.org/10.1093/annonc/mdt320
Figueroa ME, Abdel-Wahab O, Lu C et al (2010) Leukemic IDH1 and IDH2 mutations result in a hypermethylation phenotype, disrupt TET2 function, and impair hematopoietic differentiation. Cancer Cell 18(6):553–567. https://doi.org/10.1016/j.ccr.2010.11.015
Fröhling S, Schlenk RF, Breitruck J et al (2002) Prognostic significance of activating FLT3 mutations in younger adults (16 to 60 years) with acute myeloid leukemia and normal cytogenetics: a study of the AML study group Ulm. Blood 100(13):4372–4380. https://doi.org/10.1182/blood-2002-05-1440
Fröhling S, Lipka DB, Kayser S et al (2006a) Rare occurrence of the JAK2 V617F mutation in AML subtypes M5, M6, and M7. Blood 107(3):1242–1243. https://doi.org/10.1182/blood-2005-09-3644
Fröhling S, Schlenk RF, Kayser S et al (2006b) Cytogenetics and age are major determinants of outcome in intensively treated acute myeloid leukemia patients older than 60 years: results from AMLSG trial AML HD98-B. Blood 108(10):3280–3288. https://doi.org/10.1182/blood-2006-04-014324
Gangatharan S, Grove CS, P’ng S et al (2013) Acute myeloid leukaemia in Western Australia 1991-2005: a retrospective population-based study of 898 patients regarding epidemiology, cytogenetics, treatment and outcome. Intern Med J 43(8):903–911. https://doi.org/10.1111/imj.12169
Godley LA, Larson RA (2008) Therapy-related myeloid leukemia. Semin Oncol 35(4):418–429. https://doi.org/10.1053/j.seminoncol.2008.04.012
Green A, Beer P (2010) Somatic mutations of IDH1 and IDH2 in the leukemic transformation of myeloproliferative neoplasms. N Engl J Med 362(4):369–370. https://doi.org/10.1056/NEJMc0910063
Harutyunyan A, Klampfl T, Cazzola M, Kralovics R (2011) p53 lesions in leukemic transformation. N Engl J Med 364(5):488–490. https://doi.org/10.1056/NEJMc1012718
Hasan SK, Mays AN, Ottone T et al (2008) Molecular analysis of t(15;17) genomic breakpoints in secondary acute promyelocytic leukemia arising after treatment of multiple sclerosis. Blood 112(8):3383–3390. https://doi.org/10.1182/blood-2007-10-115600
Hasan SK, Ottone T, Schlenk RF et al (2010) Analysis of t(15;17) chromosomal breakpoint sequences in therapy-related versus de novo acute promyelocytic leukemia: association of DNA breaks with specific DNA motifs at PML and RARA loci. Genes Chromosom Cancer 49(8):726–732. https://doi.org/10.1002/gcc.20783
Heuser M (2016) Therapy-related myeloid neoplasms: does knowing the origin help to guide treatment? Hematology 2016(1):24–32. https://doi.org/10.1182/asheducation-2016.1.24
Holowiecki J, Grosicki S, Giebel S et al (2012) Cladribine, but not fludarabine, added to daunorubicin and cytarabine during induction prolongs survival of patients with acute myeloid leukemia: a multicenter, randomized phase III study. J Clin Oncol 30(20):2441–2448. https://doi.org/10.1200/JCO.2011.37.1286
Hulegårdh E, Nilsson C, Lazarevic V et al (2015) Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish acute leukemia registry. Am J Hematol 90(3):208–214. https://doi.org/10.1002/ajh.23908
IDHIFA® (enasidenib) tablets [packet insert]. Summit: Celgene Corporation; 2017
Jen EY, Ko CW, Eun Lee J et al (2018) FDA approval: Gemtuzumab ozogamicin for the treatment of adults with newly diagnosed CD33-positive acute myeloid leukemia. Clin Cancer Res 24(14):3242–3246. https://doi.org/10.1158/1078-0432.CCR-17-3179
Juliusson G, Antunovic P, Derolf A et al (2009) Age and acute myeloid leukemia: real world data on decision to treat and outcomes from the Swedish acute leukemia registry. Blood 113(18):4179–4187. https://doi.org/10.1182/blood-2008-07-172007.An
Kayser S, Döhner K, Krauter J et al (2011) The impact of therapy-related acute myeloid leukemia (AML) on outcome in 2853 adult patients with newly diagnosed AML. Blood 117(7):2137–2145. https://doi.org/10.1182/blood-2010-08-301713
Kayser S, Krzykalla J, Elliott MA et al (2017) Characteristics and outcome of patients with therapy-related acute promyelocytic leukemia front-line treated with or without arsenic trioxide. Leukemia 31(11):2347–2354. https://doi.org/10.1038/leu.2017.92
Kennedy JA, Atenafu EG, Messner HA et al (2013) Treatment outcomes following leukemic transformation in Philadelphia-negative myeloproliferative neoplasms. Blood 121(14):2725–2733. https://doi.org/10.1182/blood-2012-10-464248
Kim HP, Gerhard B, Harasym TO, Mayer LD, Hogge DE (2011) Liposomal encapsulation of a synergistic molar ratio of cytarabine and daunorubicin enhances selective toxicity for acute myeloid leukemia progenitors as compared to analogous normal hematopoietic cells. Exp Hematol 39(7):741–750. https://doi.org/10.1016/j.exphem.2011.04.001
Lancet JE, Cortes JE, Hogge DE et al (2014) Phase 2 trial of CPX-351, a fixed 5:1 molar ratio of cytarabine/daunorubicin, vs cytarabine/daunorubicin in older adults with untreated AML. Blood 123(21):3239–3246. https://doi.org/10.1182/blood-2013-12-540971
Lancet JE, Uy GL, Cortes JE et al (2018) Cpx-351 (cytarabine and daunorubicin) liposome for injection versus conventional cytarabine plus daunorubicin in older patients with newly diagnosed secondary acute myeloid leukemia. J Clin Oncol 36(26):2684–2692. https://doi.org/10.1200/JCO.2017.77.6112
Larson RA (2007) Is secondary leukemia an independent poor prognostic factor in acute myeloid leukemia? Best Pract Res Clin Haematol 20(1):29–37. https://doi.org/10.1016/j.beha.2006.10.006
Lee JH, Joo YD, Kim H et al (2011) A randomized trial comparing standard versus high-dose daunorubicin induction in patients with acute myeloid leukemia. Blood. 118(14):3832–3841. https://doi.org/10.1182/blood-2011-06-361410
Lee JH, Kim H, Joo YD et al (2017) Prospective randomized comparison of idarubicin and high-dose daunorubicin in induction chemotherapy for newly diagnosed acute myeloid leukemia. J Clin Oncol 35(24):2754–2763. https://doi.org/10.1200/JCO.2017.72.8618
Li Z, Labopin M, Ciceri F et al (2018) Haploidentical transplantation outcomes for secondary acute myeloid leukemia: acute leukemia working party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT) study. Am J Hematol 93(6):769–777. https://doi.org/10.1002/ajh.25087
Lim WS, Tardi PG, Dos Santos N et al (2010) Leukemia-selective uptake and cytotoxicity of CPX-351, a synergistic fixed-ratio cytarabine: Daunorubicin formulation, in bone marrow xenografts. Leuk Res 34(9):1214–1223. https://doi.org/10.1016/j.leukres.2010.01.015
Litzow MR, Tarima S, Pérez WS et al (2010) Allogeneic transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia. Blood 115(9):1850–1857. https://doi.org/10.1182/blood-2009-10-249128
Lo-Coco F, Hasan SK, Montesinos P, Sanz MA (2013) Biology and management of therapy-related acute promyelocytic leukemia. Curr Opin Oncol 25(6):695–700. https://doi.org/10.1097/CCO.0000000000000013
Löwenberg B, Suciu S, Archimbaud E et al (1998) Mitoxantrone versus daunorubicin in induction-consolidation chemotherapy—the value of low-dose cytarabine for maintenance of remission, and an assessment of prognostic factors in acute myeloid leukemia in the elderly. J Clin Oncol 16(3):872–881. https://doi.org/10.1200/JCO.1998.16.3.872
Löwenberg B, Ossenkoppele GJ, Van Putten W et al (2009) High-dose daunorubicin in older patients with acute myeloid leukemia. N Engl J Med 361(13):1235–1248. https://doi.org/10.1056/NEJMoa0901409
Lyman SD, Jacobsen SEW (1998) C-kit ligand and flt3 ligand: stem/progenitor cell factors with overlapping yet distinct activities. Blood 91(4):1101–1134. https://doi.org/10.1182/blood.V91.4.1101
Mays AN, Osheroff N, Xiao Y et al (2010) Evidence for direct involvement of epirubicin in the formation of chromosomal translocations in t(15;17) therapy-related acute promyelocytic leukemia. Blood 115(2):326–330. https://doi.org/10.1182/blood-2009-07-235051
McKenna HJ, Stocking KL, Miller RE et al (2000) Mice lacking flt3 ligand have deficient hematopoiesis affecting hematopoietic progenitor cells, dendritic cells, and natural killer cells. Blood 95(11):3489–3497. https://doi.org/10.1182/blood.v95.11.3489.011k45_3489_3497
Medeiros BC, Satram-Hoang S, Hurst D, Hoang KQ, Momin F, Reyes C (2015) Big data analysis of treatment patterns and outcomes among elderly acute myeloid leukemia patients in the United States. Ann Hematol 94(7):1127–1138. https://doi.org/10.1007/s00277-015-2351-x
Mengis C, Aebi S, Tobler A, Dähler W, Fey MF (2003) Assessment of differences in patient populations selected for or excluded from participation in clinical phase III acute myelogenous leukemia trials. J Clin Oncol 21(21):3933–3939. https://doi.org/10.1200/JCO.2003.03.186
Mesa RA, Li CY, Ketterling RP, Schroeder GS, Knudson RA, Tefferi A (2005) Leukemic transformation in myelofibrosis with myeloid metaplasia: a single-institution experience with 91 cases. Blood 105(3):973–977. https://doi.org/10.1182/blood-2004-07-2864
Miesner M, Haferlach C, Bacher U et al (2010) Multilineage dysplasia (MLD) in acute myeloid leukemia (AML) correlates with MDS-related cytogenetic abnormalities and a prior history of MDS or MDS/MPN but has no independent prognostic relevance: a comparison of 408 cases classified as “AML not otherwise specified” (AML-NOS) or “AML with myelodysplasia-related changes” (AML-MRC). Blood 116(15):2742–2751. https://doi.org/10.1182/blood-2010-04-279794
Mihalyova J, Jelinek T, Growkova K, Hrdinka M, Simicek M, Hajek R (2018) Venetoclax: a new wave in hematooncology. Exp Hematol 61:10–25. https://doi.org/10.1016/j.exphem.2018.02.002
Mistry AR, Felix CA, Whitmarsh RJ et al (2005) DNA topoisomerase II in therapy-related acute promyelocytic leukemia. N Engl J Med 352(15):1529–1538. https://doi.org/10.1056/NEJMoa042715
Müller-Tidow C, Tschanter P, Röllig C et al (2016) Azacitidine in combination with intensive induction chemotherapy in older patients with acute myeloid leukemia: the AML-AZA trial of the study alliance leukemia. Leukemia 30(3):555–561. https://doi.org/10.1038/leu.2015.306
Nagel G, Weber D, Fromm E et al (2017) Epidemiological, genetic, and clinical characterization by age of newly diagnosed acute myeloid leukemia based on an academic population-based registry study (AMLSG BiO). Ann Hematol 96(12):1993–2003. https://doi.org/10.1007/s00277-017-3150-3
Nilsson C, Hulegårdh E, Garelius H et al (2019) Secondary acute myeloid leukemia and the role of allogeneic stem cell transplantation in a population-based setting. Biol Blood Marrow Transplant 25(9):1770–1778. https://doi.org/10.1016/j.bbmt.2019.05.038
Ok CY, Patel KP, Garcia-Manero G et al (2015a) Mutational profiling of therapy-related myelodysplastic syndromes and acute myeloid leukemia by next generation sequencing, a comparison with de novo diseases. Leuk Res 39(3):348–354. https://doi.org/10.1016/j.leukres.2014.12.006
Ok CY, Patel KP, Garcia-Manero G et al (2015b) TP53 mutation characteristics in therapy-related myelodysplastic syndromes and acute myeloid leukemia is similar to de novo diseases. J Hematol Oncol 8:45. https://doi.org/10.1186/s13045-015-0139-z
Østgård LSG, Kjeldsen E, Holm MS et al (2010) Reasons for treating secondary AML as de novo AML. Eur J Haematol 85(3):217–226. https://doi.org/10.1111/j.1600-0609.2010.01464.x
Østgård LSG, Medeiros BC, Sengeløv H et al (2015) Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a national population-based cohort study. J Clin Oncol 33(31):3641–3649. https://doi.org/10.1200/JCO.2014.60.0890
Pulsoni A, Pagano L (2005) Treatment of secondary acute myeloid leukemia. J Clin Oncol 23(4):926–927. https://doi.org/10.1200/JCO.2005.05.202
Pulsoni A, Pagano L, Lo Coco F et al (2002) Clinicobiological features and outcome of acute promyelocytic leukemia occurring as a second tumor: the GIMEMA experience. Blood 100(6):1972–1976. https://doi.org/10.1182/blood-2001-12-0312
Rampal R, Ahn J, Abdel-Wahaba O et al (2014) Genomic and functional analysis of leukemic transformation of myeloproliferative neoplasms. Proc Natl Acad Sci U S A 111(50):E5401–E5410. https://doi.org/10.1073/pnas.1407792111
Rizzieri DA, O’Brien JA, Broadwater G et al (2009) Outcomes of patients who undergo aggressive induction therapy for secondary acute myeloid leukemia. Cancer 115(13):2922–2929. https://doi.org/10.1002/cncr.24379
Röllig C, Thiede C, Gramatzki M et al (2010) A novel prognostic model in elderly patients with acute myeloid leukemia: results of 909 patients entered into the prospective AML96 trial. Blood 116(6):971–978. https://doi.org/10.1182/blood-2010-01-267302
Schoch C, Kern W, Schnittger S, Hiddemann W, Haferlach T (2004) Karyotype is an independent prognostic parameter in therapy-related acute myeloid leukemia (t-AML): an analysis of 93 patients with t-AML in comparison to 1091 patients with de novo AML. Leukemia 18(1):120–125. https://doi.org/10.1038/sj.leu.2403187
Sengsayadeth S, Labopin M, Boumendil A et al (2018) Transplant outcomes for secondary acute myeloid leukemia: acute leukemia working party of the European Society for blood and bone marrow transplantation study. Biol Blood Marrow Transplant 24(7):1406–1414. https://doi.org/10.1016/j.bbmt.2018.04.008
Sperling AS, Gibson CJ, Ebert BL (2017) The genetics of myelodysplastic syndrome: from clonal haematopoiesis to secondary leukaemia. Nat Rev Cancer 17(1):5–19. https://doi.org/10.1038/nrc.2016.112
Stein EM, DiNardo CD, Pollyea DA et al (2017) Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 130(6):722–731. https://doi.org/10.1182/blood-2017-04-779405
Stölzel F, Pfirrmann M, Aulitzky WE et al (2011) Risk stratification using a new prognostic score for patients with secondary acute myeloid leukemia: results of the prospective AML96 trial. Leukemia 25(3):420–428. https://doi.org/10.1038/leu.2010.279
Stone RM, Mazzola E, Neuberg D et al (2015) Phase III open-label randomized study of cytarabine in combination with amonafide L-malate or daunorubicin as induction therapy for patients with secondary acute myeloid leukemia. J Clin Oncol 33(11):1252–1257. https://doi.org/10.1200/JCO.2014.57.0952
Stone RM, Mandrekar SJ, Sanford BL et al (2017) Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med 377(5):454–464. https://doi.org/10.1056/NEJMoa1614359
Stone RM, Manley PW, Larson RA, Capdeville R (2018) Midostaurin: its odyssey from discovery to approval for treating acute myeloid leukemia and advanced systemic mastocytosis. Blood Adv 2(4):444–453. https://doi.org/10.1182/bloodadvances.2017011080
Szotkowski T, Rohon P, Zapletalova J, Sicova K, Hubacek J, Indrak K (2010) Secondary acute myeloid leukemia—a single center experience. Neoplasma 57(2):170–178. https://doi.org/10.4149/neo_2010_02_170
Takahashi K, Wang F, Kantarjian H et al (2017) Preleukaemic clonal haemopoiesis and risk of therapy-related myeloid neoplasms: a case-control study. Lancet Oncol 18(1):100–111. https://doi.org/10.1016/S1470-2045(16)30626-X
Talati C, Lancet JE (2018) CPX-351: changing the landscape of treatment for patients with secondary acute myeloid leukemia. Future Oncol 14(12):1147–1154. https://doi.org/10.2217/fon-2017-0603
Tallman MS, Wang ES, Altman JK et al (2019) Acute myeloid leukemia, version 3.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 17(6):721–749. https://doi.org/10.6004/jnccn.2019.0028
Theocharides A, Boissinot M, Girodon F et al (2007) Leukemic blasts in transformed JAK2-V617F-positive myeloproliferative disorders are frequently negative for the JAK2-V617F mutation. Blood 110(1):375–379. https://doi.org/10.1182/blood-2006-12-062125
Thepot S, Itzykson R, Seegers V et al (2010) Treatment of progression of Philadelphia-negative myeloproliferative neoplasms to myelodysplastic syndrome or acute myeloid leukemia by azacitidine: a report on 54 cases on the behalf of the Groupe francophone des Myelodysplasies (GFM). Blood 116(19):3735–3742. https://doi.org/10.1182/blood-2010-03-274811
TIBSOVO® (ivosidenib tablets) [packet insert]. Cambridge: Agios Pharmaceuticals, Inc.; 2018
Vardiman J, SSHCEHNLJESPSASHTJ, Swerdlow SH, Campo E, et al (2008) WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon
Vardiman JW, Thiele J, Arber DA et al (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114(5):937–951. https://doi.org/10.1182/blood-2009-03-209262
VENCLEXTA® (venetoclax tablets) [packet insert]. North Chicago: AbbVie Inc. 2018
Vyxeos (n.d.) Summary of product characteristics. https://www.ema.europa.eu/en/documents/product-information/vyxeos-liposomal-epar-product-information_es.pdf. Accessed 17 May 2020
Walter MJ, Shen D, Ding L et al (2012) Clonal architecture of secondary acute myeloid leukemia. N Engl J Med 366(12):1090–1098. https://doi.org/10.1056/NEJMoa1106968
Wei A, Strickland SA, Hou J-Z, et al (2019) Venetoclax with low-dose Cytarabine induces rapid, deep, and durable responses in previously untreated older adults with AML ineligible for intensive chemotherapy. Blood. https://doi.org/10.1182/blood-2018-99-118729
Wheatley K, Brookes CL, Howman AJ et al (2009) Prognostic factor analysis of the survival of elderly patients with AML in the MRC AML11 and LRF AML14 trials. Br J Haematol 145(5):598–605. https://doi.org/10.1111/j.1365-2141.2009.07663.x
Wong TN, Ramsingh G, Young AL et al (2015) Role of TP53 mutations in the origin and evolution of therapy-related acute myeloid leukaemia. Nature 518(7540):552–555. https://doi.org/10.1038/nature13968
XOSPATA® (gilteritinib)[packet insert]. Northbrook: Astellas Pharma US, Inc.; 2018.
Yakoub-Agha I, De La Salmonière P, Ribaud P et al (2000) Allogeneic bone marrow transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia: a long-term study of 70 patients—report of the French society of bone marrow transplantation. J Clin Oncol 18(5):963–971. https://doi.org/10.1200/JCO.2000.18.5.963
Yin CC, Glassman AB, Lin P et al (2005) Morphologic, cytogenetic, and molecular abnormalities in therapy-related acute promyelocytic leukemia. Am J Clin Pathol 123(6):840–848. https://doi.org/10.1309/TJFFK819RPCLFKJ0
Zeichner SB, Arellano ML (2015) Secondary adult acute myeloid leukemia: a review of our evolving understanding of a complex disease process. Curr Treat Options Oncol 16(8):37. https://doi.org/10.1007/s11864-015-0355-3
Zeidner JF, Foster MC, Blackford AL et al (2015) Randomized multicenter phase II study of flavopiridol (alvocidib), cytarabine, and mitoxantrone (FLAM) versus cytarabine/daunorubicin (7+3) in newly diagnosed acute myeloid leukemia. Haematologica 100(9):1172–1179. https://doi.org/10.3324/haematol.2015.125849
Zhang SJ, Rampal R, Manshouri T et al (2012) Genetic analysis of patients with leukemic transformation of myeloproliferative neoplasms shows recurrent SRSF2 mutations that are associated with adverse outcome. Blood 119(19):4480–4485. https://doi.org/10.1182/blood-2011-11-390252
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Montesinos, P., Martínez-Cuadrón, D. (2021). Secondary AML. In: Röllig, C., Ossenkoppele, G.J. (eds) Acute Myeloid Leukemia . Hematologic Malignancies. Springer, Cham. https://doi.org/10.1007/978-3-030-72676-8_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-72676-8_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-72675-1
Online ISBN: 978-3-030-72676-8
eBook Packages: MedicineMedicine (R0)