Abstract
To evaluate cancer involvement of internal female genitalia of patients undergoing anterior exenteration for clinically organ confined transitional cell carcinoma of the bladder, and identify potential preoperative risk factors. Charts and anterior exenteration specimens from 54 women with clinically organ confined transitional cell bladder cancer were retrospectively reviewed. Emphasis was given to the presence of internal genitalia involvement and or primary gynecologic pathology. Unsuspected internal genitalia involvement was reported in only three patients (5.7%). The vagina was involved in two cases (3.8%) while the uterus in one (1.9%). In all cases involvement was due to direst extension from bladder tumors of the base and dome respectively. No preoperative variable could predict internal genitalia involvement in a statistical significant manner. Benign pathology of the female reproductive organs was observed in six patients and involved in all cases the uterus (11.5%). Internal genitalia involvement after radical cystectomy for TCC tumors of the bladder is rare (5.8%). Preoperative risk factors could not be identified although all involved genitalia were seen in tumors of the bladder dome and base. Therefore large multi-institutional studies are needed in order to identify preoperative risk factors for internal genitalia involvement in females with bladder cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Primary goal when performing a radical cystectomy for bladder cancer is complete eradication of the disease. In women close proximity of the uterus and vagina to the bladder makes local tumor extension from the bladder to these organs possible. Therefore in women, anterior exenteration involves the removal of the bladder and urethra together with the uterus, fallopian tubes, ovaries, and upper third of the anterior vaginal wall [1] even when there is no evidence preoperatively or intraoperatively of cancer extension to these organs.
With appropriate patient selection orthotopic bladder substitution can be done in women. In these cases preservation of the urethra and anterior vaginal wall has been performed with good cancer control and functional results [2–4]. In addition data evaluating female cystectomy specimens for bladder cancer have shown that the internal genitalia were rarely involved [5–7], and ovarian tumors secondary to bladder cancer is a very rare event [8]. In fact in younger patients an ovary can be left in order to preserve hormonal function [1]. A pregnancy has even been reported after orthotopic continent urinary diversion [9]. Therefore preservation of internal genitalia during radical cystectomy for bladder cancer seems intriguing especially for young women still in a childbearing age, but also for older women still sexually active and not in menopause. We studied the pathology of anterior exenteration specimens, performed for transitional cancer cell carcinoma in female patients in order to determine the impact of preserving the female internal genitalia on cancer control. In addition a variety of clinicopathological factors were evaluated in order to see if they were predictive of internal genitalia involvement.
2 Patients and methods
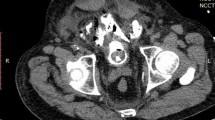
During a 10-year period (6/94–6/04) a total of 62 women underwent radical cystectomy and non-continent ileal urinary diversion. Indications were muscle invasive bladder cancer, and superficial TCC with high risk for progression despite intravesical therapy and multiple transurethral resections. We did not include patients with obvious metastatic and or locally advanced disease for whom radical cystectomy would be considered palliative. Patients with non-transitional cancer cell carcinoma were excluded as well. Diagnosis was made by histopathological analysis of the TUR specimen. The remaining 52 patients with TCC of the bladder comprised our study group. Metastatic evaluation was performed with bimanual examination under anesthesia, CT of the abdomen and pelvis; chest X-ray, and bone scan if indicated by elevated alkaline phosphatase, and clinical findings. All patients underwent a typical radical cystectomy with removal of the ovaries, fallopian tubes, uterus, and anterior vaginal wall. Bilateral pelvic lymphadenectomy and formation of an ileal conduit urinary diversion was performed in all cases. In no case was neoadjuvant radiation or systemic chemotherapy administered. Postoperative adjuvant therapy was individualized according to the final pathological findings.
The cystectomy specimens were studied for type, grade, stage, and location of tumor. Emphasis was given to the presence of internal genitalia involvement and or primary gynecologic pathology. Sections of the vagina, cervix, and ovaries were routinely processed even if they were grossly uninvolved by tumor. Urethral and lymph node involvement were also recorded. All staining was performed by traditional hematoxylin and eosin methods. Tumor staging was assigned according to the American Joint Committee Criteria using the TNM staging system [10]. Clinical and pathological data were collected from the hospital records.
We performed univariate analyses of contingency tables using chi-square tests to assess the correlation between female internal genitalia involvement and several preoperative and postoperative variables (e.g., age, clinical stage, carcinoma in situ, tumor grade, tumor location, urethral, and nodal status). Exact methods were used to determine statistical significance when small numbers were encountered in the contingency tables (i.e., expected value of any cell is less than five).
3 Results
3.1 Characteristics of bladder cancer before cystectomy
From a total of 62 patients, six with evident locally advanced/and or metastatic disease, and four patients with non-TCC, carcinoma (one with sarcoma, two with squamous cell carcinoma and one with adenocarcinoma) were not included in the study group. Therefore anterior exenteration for transitional cancer cell carcinoma was evaluated in 52 patients, 34 with muscle invasive TCC, and 18 with superficial TCC. Indications for patients with superficial TCC were refractory carcinoma in situ in eight patients, diffuse high-grade Ta tumor in one, and rapidly recurring T1 tumors despite intravesical therapy in nine. Mean age at the time of surgery was 61.3 years (range from 36–76).
Preoperatively 10 tumors were located in the bladder dome, 16 in the lateral walls, 10 in the trigone, 11 in the bladder base, and 5 presented with diffuse foci. Two patients had Grade II tumors and 50 had Grade III. Before surgery seven women were premenopausal. The rest were menopausal and perimenopausal.
3.2 Characteristics of bladder cancer in cystectomy specimens
Final pathology report revealed 10 patients with superficial tumors (six carcinoma in situ, four T1) and 39 with invasive tumors (11 T2, 17 T3a, 8 T3b, and 3 T4a). In three specimens no residual tumor was present probably due to radical resection during transurethral surgery. Urethral involvement was present in 3 (5.7%) patients, all of whom had bladder neck involvement. Regional lymph nodes were positive in 5 (9.6%) patients.
3.3 Characteristics of bladder cancer in cases of internal genitalia involvement
Internal genitalia involvement was reported in only three patients (5.7%) and was always by direct extension from the bladder tumor. Table 1 describes the characteristics of patients with involvement of internal genitalia. The vagina was always invaded by basal bladder tumors while the uterus from the underlying bladder dome. P-values of each preoperative variable evaluated for internal genitalia involvement are presented in Table 2. No such variable reached statistical significance, although the bladder base and dome were correlated more than the other factors evaluated.
4 Discussion
Internal female reproductive organs are routinely removed during cystectomy for bladder cancer, safeguarding the main goal of cancer surgery, which is complete eradication of the disease. Most women that undergo cystectomy for bladder cancer are postmenopausal and hysterectomy with bilateral salpingo-oophorectomy seems a reasonable adjunct to cystectomy, but for younger women anterior exenteration for bladder cancer, although rarely performed, could have serious hormonal, sexual, and psychological implications.
Ovary removal causes acute early menopause, which is associated with increased risk of menopausal symptoms, ischemic heart disease, and osteoporosis. Hormone replacement therapy can alleviate symptoms but conveys a higher risk of breast cancer [11–12] and although the risk is bigger in older women; it is not negligible in younger ones who will be using hormone replacement for a long period of time. Therefore ovarian preservation during radical hysterectomy in young women (under 40 years old) can be performed and has been proven safe with no tumor recurrence or symptomatic ovarian cysts observed [13]. Similarly keeping one or both ovaries during anterior exenteration for bladder cancer seems intriguing since pregnancy is not contraindicated in such patients and in fact pregnancies have been carried out after urinary diversion without particular problems [14–15]. A step further would be preserving the uterus for gestation despite the fact that this organ has no endocrine or sexual function. In addition pelvic prolapse would be less likely to occur because the pelvic support provided by the pubocervical fascia and cardinal ligaments would remain intact. Similarly anterior enterocele formation would be inhibited because the intestine would not be able to fill the dead space created when all internal genitalia are removed. The same mechanism would prevent pouchocele formation of the neobladder by not allowing it to fold backwards and obstruct the internal urethral meatus causing voiding dysfunction.
After ileal conduit urinary diversion for cancer, more than 80% of females who were sexually active before the operation reported either a decrease, or cessation of sexual activity [16] (i.e., coitus) postoperatively. Main problems were decrease in sexual desire, dyspareunia, and vaginal dryness. Preservation of the anterior vaginal wall has been described during orthotopic urinary diversion [1] with good continence and functional results [17]. In a paper by Horenblas et al. [18] a cystectomy termed sexuality preserving was performed with preservation of all internal genitalia in three women and ten men. All female patients had normal vaginal lubrication postoperatively. No local recurrences were reported attributed to careful preoperative selection. The limited number of female patients precludes general conclusions but internal genitalia preservation has been proven technically feasible.
The problem when considering sparing female reproductive organs during radical cystectomy for bladder cancer is tumor recurrence, and despite functional advantages of sparing these organs, compromising cancer cure for this reason is not acceptable. Therefore risk factors for internal genitalia involvement need to be identified if internal genitalia preservation is to be considered. These factors have not yet been recognized in part to the limited number of female patients undergoing cystectomy, in part to the fact that most studies focus on identifying factors for urethral preservation. This occurred because urethral preservation in women is necessary in order to perform an orthotopic urinary diversion and the main problem is the high incidence of urethral involvement, reported to be as high as 36% [19]. As appropriate studies [20] proposing several pathologic criteria helped identify the appropriate female candidates for orthotopic urinary diversion, similar studies are needed for female reproductive organ preservation.
None of the preoperative characteristics we studied (age, cTNM, grade, tumor location, carcinoma in situ) were correlated in a statistically significant manner with involvement of internal genitalia. In our series of 52 patients with clinically bladder-confined disease, the number of internal genitalia involvement was small (5.7%) and this is probably due to the fact that we did not include patients with evident metastatic or locally advanced disease since these patients would obviously not be candidates for internal genitalia preservation. In addition we excluded from further analysis patients with non-transitional cell carcinomas (one patient with sarcoma, two with squamous cell carcinoma and one with adenocarcinoma), which may have a variable prognosis. In a large series of radical cystectomies, bladders with TCC had a higher rate of gynecologic organ involvement compared to adenocarcinomas, and squamous cell carcinomas, and tumor grade was an important predictor of gynecologic organ involvement [21]. The above-mentioned histologic types of bladder tumors are rarer and do not respond to adjuvant chemo and radiotherapy. Since radical cystectomy is their only chance of cure we would not consider these patients for a less invasive operation despite the fact that in the particular study, internal genitalia involvement in adenocarcinomas, and squamous cell carcinomas was less frequent than in TCC tumors. However, the above-mentioned conclusion is not always the case. In fact Chin et al. [22] have previously reported that vaginal recurrence was more frequent in non-TCC cancers.
Lymph nodes, lungs bones, and liver are the major sites of metastatic TCC of the bladder [23], but microscopic metastases to the ovaries is rare even in patients dying from metastatic TCC and has been reported up to 4% [24] in autopsy series. One can easily conclude that isolated metastasis to the ovary from TCC should be an extraordinary rare event in patients with more confined disease and therefore could be left intact to preserve hormonal function [1]. Groutz et al. [25] reported one metachronous metastatic site in an ovary left in place. This was attributed to suboptimal management that altered the lymphatic spread in the pelvis since this patient before having a formal cystectomy was treated by transvesical resection of the tumor and radiation therapy. The authors concluded that ovary preservation should be only considered with proper initial management and when follow-up is performed with periodic pelvic examination and sonography. We agree that ovaries could be preserved since we also did not have any ovary involvement in our patients.
In this series of patients the vagina was the most frequent internal female organ involved (3.8%). This has also been described by others [5–6] and has been stated to be as high as 20.4% [22]. Direct invasion is the most probable way of spread, but unfortunately can be undetectable by CT or bimanual examination if extension is not bulky, as in our two cases. The role of Papanicolaou smear in this setting has not been evaluated. Finger and Freiha [26] preserved the anterior vaginal wall only if cancer was located at the anterior bladder wall or dome and would not involve the bladder neck or base, infact reflecting their concerns for direct invasion through the vesicovaginal space. Direct extension can be explained by the fact that the vesicovaginal and vesicocervical areas do not form a barrier that can prevent cancer spread, as does for example Denonvilliers’ fascia in prostate cancer. We had two cases of vaginal involvement all of which were direct invasion from tumors of the bladder base. Tumor location and internal genitalia involvement were not statistically correlated; although tumor of the bladder base had initially a statistical significant correlation with vaginal invasion this correlation lost significance when it was corrected for small number in the contingency tables, stressing the need for a larger number of patients, through multicenter trials.
Involvement of the uterus was observed intraoperatively in one patient and direct extension from the bladder dome was confirmed. CT or clinical examination showed no suspicion of involvement preoperatively. This percentage (1.9%) is small and again due to the low stage disease in the majority of patients. Benign pathology was observed in six patients and involved in all cases the uterus (11.5%).
When lymph nodes are grossly involved prognosis is grim and organ preservation surgery has no meaning. Metastasis to the internal genitalia through the lymphatic vessels is rather unusual despite the fact that the urethra, bladder, and internal genitalia share common lymphatic drainage both to the internal and external inguinal nodes. Retrograde lymphatic seeding of tumor can be possible only due to lymphatic blockage of diseased lymph nodes. In our five patients with positive lymph nodes only one had extension to the vagina and cervix, possibly because all positive nodes had only microscopic tumor involvement.
Overall studies on female cystectomy specimens revealed that internal genitalia were rarely the site of cancer spread. Stein et al. [7] found 10.4% of such involvement with involvement of the vagina, uterus, and ovaries, 5.2%, 3.9%, and 1.3% respectively. These rates are slightly higher than ours but their study group comprised patients with more advanced disease. Chang et al. [8] presented lower overall rates (7.5%) and involvement included in all cases the uterus, but non-TCC tumors were not excluded and only 60% of the total study group had the uterus in place.
Unsuspected internal genitalia involvement after radical cystectomy for TCC tumors of the bladder is rare (5.8%) in clinically organ-confined disease and occurs mainly by direct extension from the bladder. Preoperative risk factors could not be identified although all involved genitalia were seen in tumors of the bladder dome and base. Therefore large multi-institutional studies are needed in order to identify preoperative risk factors for internal genitalia involvement in females with bladder cancer.
References
Marshal F, Treiger B (1991) Radical cystectomy (anterior exenteration) in the female patient. Urol Clin North Am 18:765–775
Schoenberg M, Hortopan S, Schlossberg L, et al (1999) Anatomical anterior exenteration with urethral and vaginal preservation: illustrated surgical method. J Urol 161:569–572
Mills RD, Studer UE (2000) Female orthotopic bladder substitution: a good operation in the right circumstances. J Urol 163:1501–1504
Shimogaki H, Okada H, Fujisawa M, et al (1999) Long term experience with orthotopic reconstruction of the lower urinary tract in women. J Urol 161:573–577
Chen M, Pisters L, Malpica A, et al (1997) Risk of urethral, vaginal and cervical involvement in patients undergoing radical cystectomy for bladder cancer: results of a contemporary cystectomy series from M.D. Anderson Cancer Center. J Urol 157:2120–2123
Stein J, Cote R, Freeman J, et al (1995) Indication for lower urinary tract reconstruction in women after cystectomy for bladder cancer: a pathological review of female cystectomy specimens. J Urol 154:1329–1333
Chang S, Cole E, Smith J, et al (2002) Pathological findings of gynecologic organs obtained at female radical cystectomy. J Urol 168:147–149
Groutz A, Gillon G, Shimonov M, et al (1996) Late isolated secondary ovarian transitional cell carcinoma: an unusual course of bladder malignancy. Br J Urol 78:759–766
Kennedy WA, Hensle TW, Reiley EA, et al (1993) Pregnancy after orthotopic continent urinary diversion. Surg Gynecol Obstet 177:405–409
Beahrs OH, Meyers MH (1983) Manual for staging of cancer. (Chapt. 29) Philadelphia: J. B. Lippincott Co., pp 171
Colditz GA, Hankinson SE, Hunter DJ, et al (1995) The use of estrogens and progestins and the risk of breast cancer in postmenopausal women. N Engl J Med 332:1589–1593
Weiss LK, Burkman RT, Cushing-Haugen KL, et al (2002) Hormone replacement therapy regimens and breast cancer risk. Obstet Gynecol 100:1148–1158
Ishii K, Aoki Y, Takakuwa K, et al (2001) Ovarian function after radical hysterectomy with ovarian preservation for cervical cancer. J Repr Med 46:347–352
Barrett RJ II, Peters WA III (1983) Pregnancy following urinary diversion. Obstet Gynecol 62:582–586
Volkmer BG, Seidl EM, Gschwend JE, et al (2002) Pregnancy in women with ureterosigmoidostomy. Urology 60:979–982
Nordstrom GM, Nyman CR (1992) Male and female sexual function and activity following ileal conduit urinary diversion. Br J Urol 70:33–39
Blute RD, Gburek BM (1998) Continent orthotopic urinary diversion in female patients: early Mayo Clinic experience. Mayo Clin Proc 73:501
Horenblas S, Meinhardt W, Ijzerman W, et al (2001) Sexuality preserving cystectomy and neobladder: initial results. J Urol 166:837–840
De Paepe ME, Andre R, Mahadevia P (1990) Urethral involvement in female patients with bladder cancer. A study of cystectomy specimens. Cancer 65:1237–1241
Stein JP, Esrig D, Freeman JA, et al (1998) Prospective pathologic analysis of female cystectomy specimens: risk factors for orthotopic diversion in women. Urology 51:951–955
Ali-El-Dein B, Abdel-Latif M, Mosbah A, et al (2004) Secondary malignant involvement of gynaecology organs in radical cystectomy specimens in women: is it mandatory to remove these organs routinely? J Urol 172:885–887
Chin JL, Wolf RM, Huben RP, et al (1985) Vaginal recurrence after cystectomy for bladder cancer. J Urol 134:58–61
Kishi K, Hirota T, Matsumoto K, et al (1981) Carcinoma of the bladder: a clinical and pathological analysis of 87 autopsy cases. J Urol 125:36–39
Babaian RJ, Johnson DE, Liamas L, et al (1980) Metastases from transitional cell carcinoma of the urinary bladder. Urology 16:142–144
Groutz A, Gillon G, Konichezky M, et al (1999) Involvement of internal genitalia in female patients undergoing radical cystectomy for bladder cancer: a clinicopthologic study of 37 cases. Int J Gynecol Cancer 9:302–306
Eigner EB, Freiha FS (1990) The fate of the remaining bladder following supravesical diversion. J Urol 144:31–33
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varkarakis, I.M., Pinggera, G., Antoniou, N. et al. Pathological review of internal genitalia after anterior exenteration for bladder cancer in women. Evaluating risk factors for female organ involvement. Int Urol Nephrol 39, 1015–1021 (2007). https://doi.org/10.1007/s11255-006-9158-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-006-9158-6