Abstract
Sensory nerves are harvested for nerve grafting, and the sural nerve is the most common donor nerve utilized. It can reliably provide 30 cm of usable nerve graft from one lower extremity with minimal donor site morbidity. In the setting of brachial plexus reconstruction, autologous nerve graft is the gold standard when possible; thus successful sural nerve harvest is a critical aspect of nerve reconstruction. Advances in minimally invasive harvest techniques in sural nerve graft harvest continue to improve associated donor site morbidity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
For grafting of mixed and motor nerve segments, autologous sural nerve remains the gold standard. The sural nerve can reliably provide 30 cm of usable nerve graft from one lower extremity with minimal donor site morbidity. Advances in minimally invasive harvest techniques in sural nerve graft harvest continue to improve donor site morbidity.
Anatomy
The sural nerve originates from nerve roots S1 and S2 and provides sensation to the distal posterolateral leg. It is formed by the confluence of the medial sural cutaneous nerve from the posterior tibial nerve and the lateral sural cutaneous nerve from the common peroneal nerve. The site of sural nerve origin is approximately 8 cm below the bifurcation of the sciatic nerve. The medial sural nerve continues on to exit from the subfascial plane deep to the gastrocnemius fascial raphe in the midline and will meet the lateral sural which is subcutaneous at approximately 20 cm proximal from the lateral malleolus. Anatomic variations are possible in approximately 20 percent of cases, with absent branching or more proximal branching possible [12]. The sural nerve will course within the subcutaneous plane in the posterolateral leg. Its distal continuation via the lateral calcaneal and lateral dorsal cutaneous branches provides sensation to the posterolateral aspect of the foot. Its contribution to the plantar foot sensation is insignificant and thus is acceptable for nerve graft harvest. For nerve harvest, the sural nerve can be identified between the lateral malleolus and Achilles tendon at the midpoint between the two structures 2 cm superior to the lateral malleolus in the subcutaneous plane . The lesser saphenous vein runs adjacent to the sural nerve and is typically located just posterior to the nerve. It can be useful as a marker for the nerve.
Total length of the sural nerve harvest may be longer than 30 cm. Sural nerve fibers are isolated from the other tibial and sciatic nerve fibers beyond its anatomical origin with a thin layer of epineurium [13]. Reidl et al. described an additional 14 cm of length, which may be harvested when an epineurolysis is performed proximally within the tibial nerve to separate the sural nerve fascicles . There is a potential risk associated with dissection adjacent to the important motoneurons of the tibial and sciatic nerve, but with meticulous, tension free dissection, the perineurium and nerve fibers remain uninjured [9, 13].
Blood Supply
The ideal nerve graft is a conduit that promotes rapid axon regeneration, and thus blood supply of the graft is a critical consideration for success [15]. Adequate vascularity is associated with the retention of Schwann cells and funicular architecture to facilitate the ingrowth and maturation of axons . In 1939 Sterling Bunnell first used thin autogenous grafts transferred to a healthy vascular bed for successful grafting [1]. Subsequently, in 1972 cable nerve grafting was refined by Millesi et al. allowing accurate interfascicular placement of grafts [11]. Nerve grafts are revascularized in a centripetal fashion and require a healthy recipient bed, evolving to the use of cable nerve grafting. Hence, the conventional nerve grafts of today rely on free cable grafts of thin long peripheral sensory nerves instead of a single large nerve graft to prevent central necrosis. The blood supply to a traditional nerve graft is provided with the longitudinal vessels which course axially on the surface of the nerve, supplying the epineurium, perineurium, and endoneurium with an anastomotic vascular network [16]. With the advent of microsurgery , Taylor et al. first described the free vascularized nerve graft utilizing the contralateral superficial radial nerve to reconstruct the median nerve in the setting of a patient with Volkmann’s ischemic contracture [16]. This was then expanded upon by Gilbert and Doi who described the vascularized sural nerve graft in 1984 [4, 6]. Vascularized nerve grafts are reported to allow faster nerve regeneration, averaging 2.4 mm per day compared to a standard 1 mm per day [15].
In a study comparing vascularized versus conventional nerve graft within a well-vascularized wound bed, no difference in speed of recovery or final outcome was noted for axillary nerve defects. However, for long nerve gaps between 7 and 14 cm in patients with ulnar or radial nerve lesions, earlier and improved functional recovery with vascularized nerve grafts than conventional grafts has been reported [5]. Doi et al. conclude that consideration for vascularized nerve graft should be given in the case of a nerve gap larger than 6 cm associated with a skin defect or compromised wound bed [5]. Doi described a technique for harvesting a vascularized sural nerve. The procedure is challenging and time consuming with a steep learning curve. Most reports are in the setting of large nerve gaps where the recipient bed is heavily scarred and also requires the transfer of a thick nerve; thus the applications of a vascularized sural nerve graft are quite limited [15]. If a patient necessitates vascularized nerve graft, it is likely best served with a different donor nerve , such as vascularized ulnar nerve [4].
Operative Techniques
Patient positioning varies depending on the surgical situation. Prone positioning is the most conducive for sural nerve harvest, but often does not facilitate the primary operation. The patient may be lateral decubitus or supine. If supine, an assistant can either maintain positioning of the lower extremity . Downsides to this can include congestion of the operating room space secondary to the additional assistant and if a trainee, whether medical student or resident, is holding the extremity, precludes visualization of the procedure and compromises intraoperative education. Our preference is to use a lower extremity limb positioner (SPIDER2 Limb Positioner, Smith and Nephew, Andover, MA) during nerve harvest. The limb positioner may be used with an ankle distractor accessory to elevate the leg and provide exposure to the posterior lower leg without the need to reposition the patient.
The traditional open technique of sural nerve harvest uses a single longitudinal incision along the lower leg in line with the course of the nerve beginning distally within the groove between the Achilles tendon and the lateral malleolus. The lesser saphenous vein is identified, preserved, and retracted. Once the nerve is identified , it is mobilized tagged with a vessel loop, which provides identification, gentle handling, and mild traction. The dissection is carried out proximally to the level of the popliteal fossa. This open approach provides visualization of the entire sural nerve anatomy, especially of the lateral branch which can be harvested if additional length is needed. The main advantages of this approach are that the direct visualization allows for meticulous hemostasis, careful handling of the nerve, and proper treatment of any diverging nerve branches. However, a stocking seam incision may be excessively morbid for some patients, and minimally invasive techniques have been described [3]. Starting distally, several (typically 3–4) 2–3 cm “stair-step” or counter incisions can be made along the length of the nerve until the popliteal fossa is reached with the nerve transected distally and then proximally. This technique can limit incision burden, yet the scars can still be unsightly.
An alternative would be to use a nerve or tendon stripper. With these devices, a limited distal incision is made, and the stripper is passed through the end of the nerve and then gently passed proximally in a rotary maneuver until the tip of the instrument can be palpated near the popliteal fossa [8]. This technique allows for two total incisions (distal and proximal). Potential complications of using a stripper include injury to the nerve during dissection as well inadvertent transection of the sural nerve graft. The communicating branch of the peroneal nerve is transected in a potentially traumatic, avulsing manner with this technique since it is not directly visualized . The entire dissection is completed without any direct visualization, and just by proprioception and when resistance is met, typically at the site of nerve branching, inadvertent force could potentially transect the nerve. It is critical to understand the expected anatomic course of the nerve and position the instrument in the direction toward the primary nerve and not any lateral branch points.
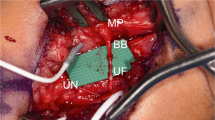
To circumvent such a complication, endoscopic sural nerve harvest is a technique to allow direct visualization of the dissection. A limited (1–2 cm) distal incision is made and the sural nerve identified; a vessel loop may be placed around the nerve for gentle traction. There are variations in harvest technique—the number of incisions and preferred dissecting instruments (tenotomy, endoscopic scissor, nerve or tendon stripper, or Foley catheter balloon) [2, 7, 10, 14]. A cone tip endoscopic dissector typically used for vessel harvest in vascular surgery such as the VasoView (Guidant Co., Natick, MA) is used with a 0 degree, 5 mm endoscope (Storz Instruments, San Dimas, CA). The VasoView conical dissectors seem to be the optimal instrument for endoscopic sural nerve harvest compared to the Foley catheter or standard endoscopic view port. The cone dissector is inserted from the distal incision and CO2 is used for light insufflation. Dissection is directly visualized and carried out throughout the length of the sural nerve using only the cone dissector. This is a rapid and facile dissection with minimal bleeding. No additional endoscopic instruments are necessary. The nerve can be free circumferentially from the surrounding subcutaneous tissue to allow full mobilization and carried up to the popliteal fossa where the medial and lateral sural nerve join. A counter incision is then made at the level approximately 2 cm below the popliteal fossa in a transverse fashion to allow for harvesting of the sural nerve proximally under direct visualization using the endoscope. The lateral sural nerve branch may be separated at this time and either harvest in conjunction or left in place. A transverse incision at this level takes advantage of the skin tension lines in this area and will optimize scar healing. The sural nerve is then extracted through the distal wound. The endoscopic technique allows for shorter incisions, less visible scarring, decreased post-operative pain, and shorter recovery [2, 3]. In pediatric patients especially, a standard telescope can even be utilized to facilitate endoscopic dissection if a cone tip dissector is not available given the shorter length of the pediatric limb.
Complications
The sural nerves can provide an abundant source of graft material with minimal branching and functional deficit associated with harvest. It is easily accessible and has large fascicles to facilitate successful grafting. Complications associated with nerve graft harvest include injury to the nerve during dissection, primarily with traction and handling, which may compromise the quality of the nerve graft . This emphasizes the importance of gentle handling of the nerve throughout the harvest and using as atraumatic a technique as possible. When harvesting additional length beyond the popliteal fossa, there is the potential for injury to the sciatic or tibial nerves. When additional length is necessary after bilateral harvest, proximal dissection should be done under direct visualization as with open harvest. There is the risk of symptomatic neuroma at the remaining stump of the sural nerve. However, by harvesting the nerve proximal to its course within the gastrocnemius fascia, the remaining nerve stump may be buried within the muscle belly and is rarely symptomatic.
References
Bunnell S, Boyes JH. Nerve grafts. Am J Surg. 1939;44(1):64–75. ISSN 0002-9610, https://doi.org/10.1016/S0002-9610(39)90934-7. (https://www.sciencedirect.com/science/article/pii/S0002961039909347).
Butler DP, Johal KS, Wicks CE, Grobbelaar AO. Objective sensory and functional outcomes at the donor site following endoscopic-assisted sural nerve harvest. J Plast Reconstr Aesthet Surg. 2017;70:659–65.
Capek L, Clarke HM, Zuker RM. Endoscopic sural nerve harvest in the pediatric patient. Plast Reconstr Surg. 1996;98:884–8.
Doi K, Kuwata N, Kawakami F, Tamaru K, Kawai S. The free vascularized sural nerve graft. Microsurgery. 1984;5:175–84.
Doi K, Tamaru K, Sakai K, Kuwata N, Kurafuji Y, Kawai S. A comparison of vascularized and conventional sural nerve grafts. J Hand Surg Am. 1992;17:670–6.
Gilbert A. Vascularized sural nerve graft. Clin Plast Surg. 1984;11:73–7.
Hadlock TA, Cheney ML. Single-incision endoscopic sural nerve harvest for cross face nerve grafting. J Reconstr Microsurg. 2008;24:519–23.
Hill HL, Vasconez LO, Jurkiewicz MJ. Method for obtaining a sural nerve graft. Plast Reconstr Surg. 1978;61:177–9.
Jaroszynski G, Johnston GH. Harvesting of the sural nerve with a tendon stripper. Microsurgery. 1996;17:217–20.
Koh KS, Park S. Endoscopic harvest of sural nerve graft with balloon dissection. Plast Reconstr Surg. 1998;101:810–2.
Millesi H, Meissl G, Berger A. The interfascicular nerve-grafting of the median and ulnar nerves. J Bone Joint Surg Am. 1972;54:727–50.
Ortiguela ME, Wood MB, Cahill DR. Anatomy of the sural nerve complex. J Hand Surg Am. 1987;12:1119–23.
Riedl O, Koemuercue F, Marker M, Hoch D, Haas M, Deutinger M. Sural nerve harvesting beyond the popliteal region allows a significant gain of donor nerve graft length. Plast Reconstr Surg. 2008;122:798–805.
Spinks TJ, Adelson PD. Pediatric sural nerve harvest: a fully endoscopic technique. Neurosurgery. 2009;64:360–3; discussion 363–4.
Taylor GI. Free vascularized nerve transfer in the upper extremity. Hand Clin. 1999;15:673–95, ix–x.
Taylor GI, Ham FJ. The free vascularized nerve graft. A further experimental and clinical application of microvascular techniques. Plast Reconstr Surg. 1976;57:413–26.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Oh, C., Pulos, N., Shin, A.Y. (2021). Sural Nerve Harvest. In: Shin, A.Y., Pulos, N. (eds) Operative Brachial Plexus Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-69517-0_27
Download citation
DOI: https://doi.org/10.1007/978-3-030-69517-0_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69516-3
Online ISBN: 978-3-030-69517-0
eBook Packages: MedicineMedicine (R0)