Abstract
Care coordination is the cornerstone of most healthcare models in the United States. Effective care coordination occurs in many settings, including acute, primary, and ambulatory care; skilled nursing facilities; home care; schools; and community-based organizations. A growing body of evidence supports the relationship between care coordination and healthcare of higher quality and value for different populations, including children with medical complexity; adults with chronic and complex illness and social needs; individuals with mental and physical health conditions; people living with cancer; persons at the end of life; older adults with multiple health, social, and nonmedical needs; and veterans. This chapter explores the essential relationship of care coordination in the Quality Health Outcomes Model (QHOM). Specifically, one key component is the significant role of registered nurses (RNs) in providing care coordination as an intervention for individuals, families, communities, and populations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Definitions of care coordination have proliferated over the last decade. The most recent definition from the National Quality Forum’s (NQF) Care Coordination Endorsement Maintenance Project 2016–2017 is “a multidimensional concept that includes effective communication among healthcare providers, patients, families, caregivers (regarding chronic conditions); safe care transitions; a longitudinal view of care that considers the past, while monitoring present delivery of care and anticipating future needs; and the facilitation of linkages between communities and the healthcare system to address medical, social, educational and other support needs that align with patient goals” (National Quality Forum 2017, paragraph 1). Earlier definitions from NQF and the Agency for Healthcare Research and Quality (AHRQ) are given in Table 11.1 to provide a historical perspective. The definition of care coordination evolved to include the purposeful nature of the intervention, requirement for two or more participants, and most importantly the need for organization and harmonization of activities.
In the United States, 60% of adults have a chronic illness, and four in ten adults have two or more chronic illnesses (see Chap. 8). Chronic diseases are the leading causes of death and disability and leading drivers of the nation’s $3.3 trillion in annual healthcare costs (National Center for Chronic Disease Prevention and Health Promotion 2019). With such a large population of chronically ill, the need for improved care is evident. For individuals and families, the lack of coordination leads to fragmented, inconsistent, and poorly planned care. Medical errors, duplication of tests, and paper shuffling can occur, with results ranging from inconvenient to life-threatening. The lack of coordinating care can also lead to unnecessary emergency room visits and hospitalizations, avoidable readmissions, and excessive resource use. Conversely, effective care coordination supports achieving the quadruple aim, improving the care experience for individuals, improving individual health, reducing costs, and improving healthcare providers’ work-life (Bodenheimer and Sinsky 2014). Examining care coordination as an intervention is an essential first step in understanding all the activities/components that contribute to delivering quality and safe person-centered and system-level outcomes.
Care Coordination: Linkages to the QHOM
Care coordination is embedded in all components of the QHOM (Mitchell et al. 1998) with multidirectional relationships whereby nursing care coordination interventions act through client and system characteristics to improve health outcomes. Additionally, client and system interactions affect health outcomes. This chapter examines the characteristics of care coordination related to individuals, providers, and organizational perspectives and describes the multifocal relationships among these perspectives and nursing interventions and care coordination outcomes as depicted in Fig. 11.1.
System Characteristics of Care Coordination
Although the chapter focus is care coordination as an intervention, it is essential to explore this (a) in the context of the structure of care coordination, (b) from the clinician and organizational perspectives, and (c) to be cognizant that locations of care coordination by RNs include programs in primary care, acute care, ambulatory care, and home care; programs based in telehealth; and programs with remote monitoring (Conway et al. 2019).
Clinician Perspective
Care coordination requires a team to support the complex care and social support needs of individuals with chronic illnesses as they are typically high users of health, community, and social services (Heslop et al. 2014). While acknowledging care coordination is a part of the role for many healthcare professionals, this chapter focuses on the role of RNs in care coordination. Registered nurses are ideally positioned to be the point of accountability whether they are employed as care coordinators, in specific care coordinator roles, or whether they coordinate care in their everyday RN role.
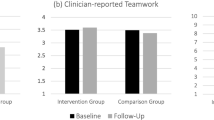
The structural component of care coordination is found in the evidence-based dimensions and competencies of Care Coordination and Transition Management (CCTM) provided by RNs and includes (1) support for self-management, (2) education and engagement of individuals and families, (3) coaching and counseling of individuals and families, (4) advocacy, (5) population health management, (6) teamwork and collaboration, (7) cross-setting communication and transition, (8) person-centered care planning, and (9) nursing process (Haas et al. 2013). A logic model was developed to identify structural components with associated activities, processes, and outcomes in each of the nine Care Coordination and Transition Management dimensions. A logic model linking these relationships is depicted in Fig. 11.2.
Logic model for care coordination. Source: © 2018 by S. Haas & B.A. Swan. Reprinted with permission from Swan, B.A., Haas, S.A., Haynes, T.S., & Murray. (2019). Introduction. In S.A. Haas, B.A. Swan, & T.S. Haynes (Eds.), Care coordination and transition management core curriculum (pp. 14–16). American Academy of Ambulatory Care Nursing
The logic model has selected activities for each dimension listed, as well as specified outcomes. The logic model allows for RN contributions to be recognized and provides an estimate of RN value in care coordination and transition management, related to processes and outcomes of care (Haas and Swan 2014). These competencies relate to RNs in all settings across the healthcare continuum. They guide acute care practice and discharge teaching and planning, care transitions between different providers and settings of care, provision of surveillance, and support for persons with multiple chronic conditions as they live at home or in assisted living, or receive home care within the community, and cope with self-management of their health and healthcare (Swan et al. 2019). Consistent with the QHOM, these structural components link with interventions and resulting outcomes of care coordination.
Organizational Perspective
Healthcare systems have increased investment in care coordination service models such as patient-centered medical homes (PCMHs) and accountable care organizations (ACOs). Four examples of investment in care coordination services are the Serious Illness Care Program (Lakin et al. 2017), the Comprehensive Primary Care Initiative developed by the Centers for Medicare & Medicaid Services (CMS) (Peikes et al. 2018), a funded CMS innovation grant called COMPASS (Care of Mental, Physical, and Substance-Use Syndromes) (Katon and Unutzer 2006; Katon et al. 2005), and the Veterans Health Administration’s Patient Aligned Care Teams (PACTs) providing interprofessional care coordination in primary care (Zulman et al. 2017). These programs are described in Table 11.2; however, the programs’ common system characteristics are defined as care management, customized longitudinal care plans, and care coordination with other providers.
Client
From the individual and family perspective, people bring predisposing characteristics such as demographics, social structure, health beliefs, psychological characteristics, personal and family resources, individual’s ability to access care, individual’s self-perceived illness severity, and person-perceived need for care coordination (Vanderboom et al. 2017). Individuals needing care coordination may have multiple complex physical and social problems that are challenging to manage. The need for coordination is not defined by the number of diagnoses but by the complexity of health problems, the complexity of social situations, and the complexity manifested by frequent use of healthcare services (Vanderboom et al. 2015). Examples of challenges that exacerbate these complexities include (1) limited support from family and friends, limited social support, (2) limited financial resources, and (3) diverse language and cultural attributes (Vanderboom et al. 2015).
Effective care coordination by RNs occurs with different populations in a variety of settings. Populations include adults with diabetes; adults with dementia; adults with a terminal illness; children with special care needs; adults poststroke; adults with chronic obstructive pulmonary disease; adults with heart failure; disabled individuals with functional impairments; older adults in skilled nursing facilities; adults with chronic and complex illness and social needs; individuals with mental and physical health conditions; people living with cancer; persons at the end of life; older adults with multiple health, social, and nonmedical needs; and veterans (Breckenridge et al. 2019; Huitema et al. 2018; Kuo et al. 2018; Lee et al. 2018; Rentas et al. 2019; Rossom et al. 2017; Ruiz et al. 2017; Talley et al. 2018; Zulman et al. 2017).
Care Coordination Interventions
Care coordination is an effective intervention when working with various populations in many different settings, as described above. In the QHOM, RN care coordination can be a direct or indirect clinical process. For instance, a direct process would occur during a care visit, such as self-management education or teaching coping skills. An indirect clinical process would happen outside the care visit, such as telephone management of high-risk older adults at risk for hospitalization or facilitated communication between individual, family, and clinicians. Indirect care coordination focuses on activities such as administration, consultation, planning, and service development.
RN Clinical Processes: Direct Interventions
As a direct intervention, care coordination is delivered through a variety of activities. A systematic review of the nurse care coordinator role identified a range of in-person care coordination activities. These include developing plans of care, educating about disease and self-management using behavior change and health coaching principles, managing medications, performing comprehensive assessments, evidence-based care planning, and coaching for self-management (Conway et al. 2019).
Population care coordination utilizes principles from care coordination, case management, and population health to maximize health outcomes and resource utilization for populations and the individuals within them (Rushton 2015). There are many population-focused models using care coordination activities as an intervention. Two populations requiring ongoing, complex coordination are older adults and individuals living with cancer.
Care coordination for older adults is required in a variety of settings, including primary care and the community. Direct interventions in these models include assessing individual needs and goals; building and maintaining relationships; creating a plan of care; providing self-management support; providing transition management; linking individuals to community resources; coordinating medications; monitoring physical signs and symptoms; managing durable medical equipment; monitoring laboratory findings; communicating with primary care providers, pharmacists, caregivers, and community agencies; finding financial and community resources; and addressing complex physical, mental, social, and cultural needs (Kim et al. 2016; Scholz and Minaudo 2015; Vanderboom et al. 2015, 2017).
Complex cancer survivors require highly coordinated care to ensure optimal outcomes for their cancers, coexisting chronic conditions, and overall quality of life. Followed by oncologists with little or no care coordination with primary care providers, care is fragmented and providers are siloed, with suboptimal care quality (Lee et al. 2018). Care coordination interventions include both direct and indirect activities such as using an electronic health record-driven registry to facilitate individual’s transitions between primary care and oncology care; co-locating an RN within a complex care team providing clinical care coordination, continuity, and transition management, and assisting individual self-management; registry review; and enhancing teamwork through coaching (Lee et al. 2018).
At the start of cancer treatment, individuals have an in-person meeting with the RN. During treatment, the RN tracks individuals to ascertain completion of initial cancer treatment, coordinates appointments and lab tests between primary care and specialty clinics weekly, and makes appointments with the social worker. At the end of the treatment, the RN provides treatment summary and follow-up guidelines, encourages interaction with primary care, recommends a transition to the care team posttreatment, tracks appointment results via the registry, synthesizes health and cancer history, educates on follow-up for cancer recurrence, educates on self-management for chronic diseases, educates on long-term effects of cancer treatment, and coordinates specialty care referrals including smoking cessation, health behaviors, and psychosocial counseling (Lee et al. 2018).
Additional population-based models requiring similar direct RN care coordination interventions include children with asthma (Garwick et al. 2015), individuals with pneumonia (Seldon et al. 2016), individuals living with diabetes (Talley et al. 2018), and individuals at the end of life (Ruiz et al. 2017). Successful care coordination not only requires direct interventions; indirect activities are just as critical.
RN Clinical Processes: Indirect Interventions
A systematic review of the nurse care coordinator role identified a range of indirect care coordination activities including arranging consultations with healthcare providers, arranging consultations with community service providers, monitoring medication adherence, collaborating with providers, educating about communicating with members of the healthcare team, ongoing contact with the individual over time, addressing transitions in care, identifying an action plan for situations of clinical deterioration, providing home-based case management, liaising with other providers and settings, providing case management services, supporting clinical visits with home telephone support, monitoring proactively, supporting caregivers, accessing community-based services, and providing navigator activities (Conway et al. 2019).
Outcomes of Care Coordination
Care coordination is a crucial strategy for addressing complex health and social issues and improving quality outcomes and performance measures. Care coordination models have been developed, recognizing that coordinating care for individuals with chronic conditions and complex healthcare needs requires new ways to provide care. Care coordination is intended to prevent costly consequences of poor management and improve short- and long-term quality for individuals, families, communities, and populations. The body of evidence linking care coordination to important quality outcomes is described below.
Person-centered outcomes resulting from care coordination as an intervention include quality of life, decreased symptom severity both physical and mental (depression, cognition), greater symptom control, concerns and problems, self-efficacy, knowledge about disease and self-management, continuity of care, treatment adherence, individual satisfaction with care, family satisfaction with care, and morbidity (Conway et al. 2019).
Organizational or system-centered outcomes resulting from care coordination as an intervention include decreased preventable hospitalizations and rehospitalization; resource use during hospitalization; length of stay; and inappropriate use of the following services: emergency department, outpatient clinic, home visit, hospice, physician visits, community service, physical therapy, occupational therapy, and rehabilitation. Further, care coordination can improve the number of patients receiving appropriate care, who have no treatment delays, and who go for follow-up appointments. Finally, organizations’ throughput, costs, clinician satisfaction, and understanding of the care coordination role can all improve with care coordination (Conway et al. 2019).
Outcome Measures for RN Care Coordination
While the above quality outcomes are important, the creation of quality outcomes and performance measures that uniquely appraise the contribution of RNs to care coordination is critical. There is growing work by Start et al. (2018) in collaboration with Collaborative Alliance for Nursing Outcomes (CALNOC) that has led to developing outcome metrics for nine care coordination and transition management RN dimensions displayed in Table 11.3.
When implemented, these metrics will provide the data to track the outcomes of RN care coordination. Data will be even more robust when RN care coordination interventions are coded in SNOMED CT and tracked and linked to the outcomes achieved. Two articles discuss how to discover value in the care coordination work of RNs across the care continuum and track the impact of care coordination done by other members of the interprofessional team (Haas and Swan 2014; Haas et al. 2016).
Summary
The QHOM provides a framework to describe and discuss the structural characteristics, interventions, and outcomes of nursing care coordination in the context of client—individual, family, community, and population. This chapter examined system characteristics of care coordination related to clinicians and organizational perspectives and described the multifocal relationships among these perspectives and nursing interventions and care coordination outcomes. RNs are increasingly looked to for leadership in the transformation of healthcare. Leveraging the RN role in care coordination is a strategy aimed at increasing the value for individuals, families, communities, and populations across the care continuum. It requires a commitment from nursing to lead and facilitate performance improvement that focuses on quality and safety and enhanced care delivery.
References
Agency for Healthcare Research and Quality (2014) What is care coordination? In: Care coordination measures atlas update. AHRQ, Rockville, MD. https://www.ahrq.gov/ncepcr/care/coordination/atlas/chapter2.html
Beck A, Boggs JM, Alem A, Coleman KJ, Rossom RC, Neely C, Solberg LI (2018) Large-scale implementation of collaborative care management for depression and diabetes and/or cardiovascular disease. J Am Board Fam Med 31(5):702–711. https://doi.org/10.3122/jabfm.2018.05.170102
Bodenheimer T, Sinsky C (2014) From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 12(6):573–576. https://doi.org/10.1370/afm.1713
Breckenridge ED, Kite B, Wells R, Sunbury TM (2019) Effect of patient care coordination on hospital encounters and related costs. Populat Health Manag 22:406–414. https://doi.org/10.1089/pop.2018.0176
Coleman KJ, Magnan S, Neely C, Solberg L, Beck A, Trevis J, Williams S (2017) The COMPASS initiative: description of a nationwide collaborative approach to the care of patients with depression and diabetes and/or cardiovascular disease. Gen Hosp Psychiatry 44:69–76
Conway A, O’Donnell C, Yates P (2019) The effectiveness of the nurse care coordinator role on patient-reported and health service outcomes: a systematic review. Evaluat Health Profess 42:263–296. https://doi.org/10.1177/0163278717734610
Garwick AW, Svavarsdottir EK, Seppelt AM, Looman WS, Anderson LS, Orlygsdottir B (2015) Development of an international school nurse asthma care coordination model. J Adv Nurs 71(3):535–546. https://doi.org/10.1111/jan.12522
Haas S, Swan BA (2014) Developing the value proposition for the role of the registered nurse in care coordination and transition management in ambulatory care settings. Nurs Econ 32:70–79
Haas S, Swan BA, Haynes T (2013) Developing ambulatory care registered nurse competencies for care coordination and transition management. Nurs Econ 31(1):44–47
Haas SA, Vlasses F, Havey J (2016) Developing staffing models to support population health management and quality outcomes in ambulatory care settings. Nurs Econ 34(3):126–133
Heslop L, Power R, Cranwell K (2014) Building workforce capacity for complex care coordination: a function analysis of workflow activity. Hum Resour Health 12:52-4491-12-52. https://doi.org/10.1186/1478-4491-12-52
Huitema AA, Harkness K, Heckman GA, McKelvie RS (2018) The spoke-hub-and-node model of integrated heart failure care. Canadian J Cardiol 34(7):863–870
Katon W, Unutzer J (2006) Collaborative care models for depression: time to move from evidence to practice. Arch Intern Med 166(21):2304–2306. https://doi.org/10.1001/archinte.166.21.2304
Katon WJ, Schoenbaum M, Fan MY, Callahan CM, Williams J Jr, Hunkeler E, Unutzer J (2005) Cost-effectiveness of improving primary care treatment of late-life depression. Arch Gen Psychiatry 62(12):1313–1320. https://doi.org/10.1001/archpsyc.62.12.1313
Kim TY, Marek KD, Coenen A (2016) Identifying care coordination interventions provided to community-dwelling older adults using electronic health records. Comput Informat Nurs CIN 34(7):303–311. https://doi.org/10.1097/CIN.0000000000000232
Kuo DZ, McAllister JW, Rossignol L, Turchi RM, Stille CJ (2018) Care coordination for children with medical complexity: whose care is it, anyway? Pediatrics 141(Suppl 3):S224–S232. https://doi.org/10.1542/peds.2017-1284G
Lakin JR, Koritsanszky LA, Cunningham R, Maloney FL, Neal BJ, Paladino J, Bernacki RE (2017) A systematic intervention to improve serious illness communication in primary care. Health Affairs (Project Hope) 36(7):1258–1264. https://doi.org/10.1377/hlthaff.2017.0219
Lee SJC, Jetelina KK, Marks E, Shaw E, Oeffinger K, Cohen D, Balasubramanian BA (2018) Care coordination for complex cancer survivors in an integrated safety-net system: a study protocol. BMC Cancer 18(1):1204-018-5118-7. https://doi.org/10.1186/s12885-018-5118-7
Mitchell PH, Ferketich S, Jennings BM (1998) Quality Health Outcomes Model. Image J Nurs Sch 30(1):43–46
National Center for Chronic Disease Prevention and Health Promotion (2019) Chronic diseases in America. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
National Quality Forum (2010) Care coordination. Retrieved from http://www.qualityforum.org/Publications/2010/10/Quality_Connections__Care_Coordination.aspx
National Quality Forum (2017) Care coordination endorsement maintenance project 2016–2017. http://www.qualityforum.org/ProjectDescription.aspx?projectID=83375
Peikes D, Dale S, Ghosh A, Taylor EF, Swankoski K, O’Malley AS, Brown RS (2018) The comprehensive primary care initiative: effects on spending, quality, patients, and physicians. Health Affairs (Project Hope) 37(6):890–899. https://doi.org/10.1377/hlthaff.2017.1678
Rentas KG, Buckley L, Wiest D, Bruno CA (2019) Characteristics and behavioral health needs of patients with patterns of high hospital use: implications for primary care providers. BMC Health Serv Res 19(1):81-019-3894-7. https://doi.org/10.1186/s12913-019-3894-7
Rossom RC, Solberg LI, Magnan S, Crain AL, Beck A, Coleman KJ, Unutzer J (2017) Impact of a national collaborative care initiative for patients with depression and diabetes or cardiovascular disease. Gen Hosp Psychiatry 44:77–85
Ruiz S, Snyder LP, Giuriceo K, Lynn J, Ewald E, Branand B, Bysshe T (2017) Innovative models for high-risk patients use care coordination and palliative supports to reduce end-of-life utilization and spending. Innov Aging 1(2):igx021. https://doi.org/10.1093/geroni/igx021
Rushton S (2015) The population care coordination process. Profess Case Manag 20(5):230–238; quiz 239-40. https://doi.org/10.1097/NCM.0000000000000105
Scholz J, Minaudo J (2015) Registered nurse care coordination: creating a preferred future for older adults with multimorbidity. Online J Issues Nurs 20(3):4
Seldon LE, McDonough K, Turner B, Simmons LA (2016) Evaluation of a hospital-based pneumonia nurse navigator program. J Nurs Adm 46(12):654–661. https://doi.org/10.1097/NNA.0000000000000422
Start R, Matlock AM, Brown D, Aronow H, Soban L (2018) Realizing momentum and synergy: benchmarking meaningful ambulatory care nurse-sensitive indicators. Nurs Econ 36:246–251
Swan BA, Conway-Phillips R, Haas S, De La Pena L (2019) Optimizing strategies for care coordination and transition management: recommendations for nursing education. Nurs Econ 37(2):77–85
Talley MH, Polancich S, Williamson JB, Frank JS, Curry W, Russell JF, Selleck C (2018) Improving population health among uninsured patients with diabetes. Populat Health Manag 21(5):373–377. https://doi.org/10.1089/pop.2017.0170
Vanderboom CE, Thackeray NL, Rhudy LM (2015) Key factors in patient-centered care coordination in ambulatory care: nurse care coordinators’ perspectives. Appl Nurs Res ANR 28(1):18–24. https://doi.org/10.1016/j.apnr.2014.03.004
Vanderboom CE, Holland DE, Mandrekar J, Lohse CM, Witwer SG, Hunt VL (2017) Predicting use of nurse care coordination by older adults with chronic conditions. West J Nurs Res 39(7):862–885. https://doi.org/10.1177/0193945916673999
Zulman DM, Pal Chee C, Ezeji-Okoye SC, Shaw JG, Holmes TH, Kahn JS, Asch SM (2017) Effect of an intensive outpatient program to augment primary care for high-need Veterans Affairs patients: a randomized clinical trial. JAMA Intern Med 177(2):166–175. https://doi.org/10.1001/jamainternmed.2016.8021
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Swan, B.A. (2021). Care Coordination. In: Baernholdt, M., Boyle, D.K. (eds) Nurses Contributions to Quality Health Outcomes. Springer, Cham. https://doi.org/10.1007/978-3-030-69063-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-030-69063-2_11
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-69062-5
Online ISBN: 978-3-030-69063-2
eBook Packages: MedicineMedicine (R0)