Abstract
The development of proximal interphalangeal (PIP) joint arthroplasty has lagged behind that of the metacarpophalangeal (MCP) joint in the hand. Essentially the main reason for this is that in rheumatoid arthritis, the principal requirement for joint replacement is at the MCP rather than the PIP joint. It is for this reason that silicone implants have been so successfully used at the metacarpophalangeal joint. Almost as an afterthought a similar albeit smaller prosthesis was produced for the proximal interphalangeal joint. To date, whilst some authors have reported good results, the general impression is that whilst these joints undoubtedly give good pain relief, movement is often restricted. At the same time, recurrent deformity can develop although function remains surprisingly good. In addition, these implants are also known to fracture. As a consequence, whilst these implants are still used as an alternative to arthrodesis in the patient with inflammatory arthritis, they are less commonly used in patients with osteoarthritis or following trauma. With the advent of the newer two-part prosthesis manufactured from a combination of either cobalt chrome, titanium, high-density polyethylene or pyro-carbon, PIP joint replacement is gaining increased acceptance. Certainly, in the well-motivated patient, it is possible to achieve an excellent result. It remains to be seen, however, how good these results are generally and more importantly how long they last. Having said that I have no doubt that these implants will be refined further, specifically in design but also instrumentation, and more and more PIP joint arthroplasties will be undertaken. There seems no doubt that patients prefer arthroplasty to arthrodesis. In addition, given the similarities between the knee and the proximal interphalangeal joint, it may be possible to incorporate a number of the developments at that larger joint into those for the PIP. With these developments, I have no doubt that within the next 5–10 years, PIP joint arthroplasty will lie within the armamentarium of all hand surgeons. With this however will come an increasing number of complications, in the short and long term, for which expertise and techniques will need to be developed to aid in their management.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Replacement of the proximal interphalangeal joint (PIP jt) has followed that of the metacarpophalangeal joint (MCP jt); however, only recently has it become the focus of increasing interest. The reason for this has been the relative success of arthrodesis or fusion in a functional position. Certainly in the presence of a normal MCP joint, PIP fusion between 30° and 50° of flexion can work well providing the patient with a pain free, stable and strong grip. However, if the MCP/DIP (distal interphalangeal) joints are themselves diseased, then fusion of the PIP joints may result in increased stiffness of the whole finger and consequently reduced function. Plainly, in these circumstances, some form of athroplasty would be advantageous. Indeed, even if these joints are relatively normal, many patients prefer the retention of some movement over none at all. This was first recognised by Carroll and Taber in an article in 1954, when they reported the results of 30 patients treated by resection arthroplasty of the PIP joint without the interposition of any other material [1]. In selected patients, they were able to demonstrate encouraging results. Pellegrini and Burton in a publication in 1990 retrospectively reviewed a number of patients who had undergone various procedures on the proximal interphalangeal joint [2]. The majority of these patients were suffering with some form of erosive osteoarthritis, and the operations undertaken were an arthroplasty using either a flexible silicone interposition or a cemented Biomeric arthroplasty or an arthrodesis. All the cemented Biomeric implants failed at an average of 2.25 years after operation. Arthrodesis of the proximal interphalangeal joint in the radial digits provided the greatest improvement in lateral pinch strength, whilst flexible silicone interpositional arthroplasty in the ulna digits provided an average flexion arc of 56° with satisfactory pain relief. Although none required revision, radiographic evidence of bone erosion around the silicone implant was seen in 35% of cases at 2 years. As a result, the authors were unable to make a recommendation as to which procedure was the most optimal.
Whilst the retention of some movement has obvious advantages, there are also attendant risks. Indeed, these risks are not only present at the time of surgery but also subsequently as the years go by. Patients with arthroplasties in situ need access to continuing care, whilst patients with an arthrodesis when solid can often be discharged. The complications of PIP arthroplasty as with all implants include dislocation, infection and loosening. At this time, however, particularly for the newer “two-part” implants which are in their infancy, the exact incidence and subsequent management of these complications are poorly understood.
The history of arthroplasty of the PIP joint is undoubtedly short. In 1961, Adrian Flatt undertook trials with a metallic prosthetic replacement for the interphalangeal joints [3]. Whilst this prosthesis offered the advantage of inherent stability and an adequate range of motion, migration and erosion of the stems through the medullary canals and cortices became commonplace. This implant design is no longer available.
As with all arthroplasties of the hand and wrist, however, Al Swanson has contributed significantly to our understanding of PIP joint arthroplasty [4]. His Silastic hinged-type implant was first introduced in 1973 as an extension of the successful MCP joint Silastic interposition arthroplasty. At the same time, Neibauer (1969) introduced his version incorporating a Dacron core [5].
Further to this and as at the MCP joint other designs have subsequently been introduced. These include the Sutter (Stryker, Kalamazoo, MI, USA) and Neuflex (DePuy, Warsaw, IN, USA), the latter having a preformed angle of 15° which is said to mimic the normal resting position.
Alternatives in patients with osteoarthritis or following fracture have included excision of the articular surfaces with some form of interposition of soft tissue – the best known of these being the “volar plate” arthroplasty. Durham-Smith and McCarten from Australia reported their results in 1992 [6]. A series of 71 cases performed over 5 years were undertaken for fracture/subluxation of the joint. Sixty-two (87%) of the patients achieved a stable pain-free joint with movement from 5° to 95° within 2 months. Complications were uncommon with a high patient satisfaction rate (94%). Longer-term results of this procedure were reported by Dionysian and Eaton in May 2000 [7]. They examined 17 patients after an average of 11½ years following this procedure for fracture dislocation of the proximal interphalangeal joint. The operation was generally undertaken in a younger age group ranging from 17 to 61 years. Overall, there was satisfactory pain relief and a good active range of motion above 85°. They did note however that patients who underwent the operation earlier, that is, soon after the injury, seemed to do better. They concluded by suggesting that volar plate arthroplasty continues to be of benefit on a long-term basis. Similar results were reported by Burton et al., from Rochester, New York, in November 2002, although in this series the indication was osteoarthritis [8].
Small joint reconstruction using a perichondrial graft was first described by Johansson and Engkvist in 1981 [9]. They reported the results of perichondrial arthroplasty in 50 joints mostly at the metacarpophalangeal and proximal interphalangeal joints of the hand. At that time, the operative technique was described together with post-operative management. In the 36 joints reviewed at more than 1 year, good or excellent results were reported in 75%. A more updated study was reported by Seradge et al. from Oklahoma City in 1984 [10]. They reported a retrospective review of 36 of these procedures, 20 of which had been undertaken at the proximal interphalangeal joint, with a minimum follow-up of 3 years. The overall results showed 55% to be good and 15% fair with 30% having been revised. All procedures undertaken for post-sepsis arthritis had failed. In addition, a concomitant tendon repair was another factor associated with a high failure rate. Finally, patients over 40 seemed to have better results. In 1992, Hasegawa and Yamano from Japan reported better results using sections from the costo-osteochondral junction including an osseous portion rather than costal cartilage alone [11]. In 1995, Katsaros reported another small series with encouraging results [12].
Finally, this section would not be complete without reference to the classic articles by Harrison from the UK in 1971 and Lipscomb from the USA in 1967 [13, 14]. Harrison categorised the type of surgery applicable to the rheumatoid proximal interphalangeal joint into either symptomatic, reparative or reconstructive. Symptomatic surgery was for either acute synovitis, proliferative synovitis or fibrinous synovitis and essentially took the form of a synovectomy. The operation is well described in this article. For reparative, Harrison meant the correction of either a flexion or extension deficit, in this case a Boutonniere or “Swan Neck” deformity. Again, the surgical treatment is described. Finally, for reconstruction, he recommended either arthrodesis or arthroplasty. Lipscomb also gave a detailed description of the technique of synovectomy of the interphalangeal joint of the finger as well as the metacarpophalangeal joint of the thumb.
Surgical Technique and Rehabilitation
As stated previously, arthroplasty of the proximal interphalangeal (PIP) joint is at a watershed and is yet to be accepted by the majority of hand surgeons. Faced with the options however of using these implants in what could already be a stiff finger, the retention of any movement seems logical. The indications for arthrodesis or arthroplasty are almost identical in that both give excellent pain relief and improvement in strength and function. Plainly, arthroplasty should allow the retention of some movement, where an arthrodesis will not. Our experience has been that patients far prefer arthroplasty despite the need for continuing care and the potential of increased complications. At this time, the only absolute contraindication at our institution would be in younger patients with an active lifestyle, in a manual worker, if there is significant bone loss or gross instability or in the presence of concomitant infection.
As with all implant surgery in the hand, it is crucial at the time of insertion that strict asepsis is observed. Whilst it is not the author’s practice to wear “body exhaust suits”, surgery is undertaken in a clean “laminar air” operating theatre with antibiotic cover. With regard to anaesthesia if more than one implant is being inserted, the author would normally advise the patient to have a general anaesthetic. If one finger is being operated upon, then local or regional anaesthesia is possible. The patient should be warned however that the operation can take up to 1 hour, and as such they would need to tolerate both the tourniquet and the operating room environment for that period.
With regard to the surgical approach itself, a number of techniques have been described based principally on the direction of the approach to the joint, i.e. palmar, lateral or dorsal. The palmar approach was popularised by Schneider from the USA in 1991 in an attempt to overcome the prolonged splinting required after the dorsal approach [15], the latter being required to protect the extensor tendon reconstruction. Via the volar approach, the whole flexor tendon sheath together with the palmar plate is mobilized from the middle phalanx after incision of the accessory collateral ligaments (Fig. 20.1). The dorsal components of the collateral ligaments are preserved. After repair, the joint is stable and suitable for early mobilization. Lin et al. (1995) from the USA reported their results of 69 proximal interphalangeal joint silicone arthroplasties in 36 patients inserted by this technique [16]. The average follow-up was 3.4 years. At review, they reported an improvement of the extensor deficit although the overall total active motion did not improve significantly from the pre-operative values. In addition, coronal plane deformities were not successfully corrected although pain relief was obtained in the majority of patients; five implants ultimately fractured.
The lateral approach uses a midline ulnar incision centred on the midpoint of the PIP joint. The neurovascular bundle is identified and retracted in a volar direction. The retinaculum ligament is incised and the extensor tendon mobilized and retracted dorsally. The collateral ligament is then detached from the bone although generally left attached to the volar plate (Fig. 20.2). This allows the joint to be opened up “like a book.” For closure, the volar plate and particularly the collateral ligament have to be repaired/reattached. The collateral ligament is reattached to its origin on the condyle of the proximal phalanx.
Undoubtedly, however, the dorsal approach has been the most widely used and is currently the approach of choice at Wrightington. The skin incision is oblique avoiding a direct longitudinal incision over the proximal interphalangeal joint (Fig. 20.3). The extensor tendon then has to be incised and retracted. This can be done either by fashioning a distally based flap in a Chevron fashion (Fig. 20.4) or by incising the tendon longitudinally dissecting the central slip off the base of the middle phalanx (Fig. 20.5). At this time, having used both approaches, the author favours the latter. More specifically, there appears to be less post-operative extension lag with this technique. It should be noted however that reconstruction of the extensor tendon is of paramount importance whichever approach is used. If the tendon is split longitudinally, the two components are re-anchored to the base of the middle phalanx by a suture passed through the bone (Fig. 20.6). This is supplemented by additional 4-0 absorbable sutures to co-apt the tendon. Usually during this approach, the dorsal quarter of the collateral ligaments has to be released to allow complete access. In addition and from time to time, a volar plate release has to be undertaken to either improve access or correct deformity. Generally, however, with this approach, an excellent view of the joint surfaces can be obtained allowing accurate resection and preparation with better alignment of the implant. For more details on this, the reader is referred to the relevant manufacturer’s instructions.
For Silastic implants however, again, it is worth emphasising the importance of the care that should be taken with any soft tissue releases and subsequent rebalancing. For the collateral ligaments, whilst generally it is the author’s opinion that these should be preserved at all costs in severe deformity or stiffness, a release may be required. These cases require sharp and delicate dissection. The fibres at the origin of the collateral ligament should be preserved by releasing the collateral ligament in continuity with a sleeve of periosteal tissue. With regard to bone preparation for the Swanson implant, bevelled ends are said to be of benefit. More specifically, cuts are angled from dorsal to volar in a distal to proximal direction. This is said to facilitate flexion. For all implants, it is also important to remove any sharp bone edges or osteophytes as this may lead to abrasion of the implant. Thereafter any synovial tissue should be removed and a soft tissue release on the volar aspect of the joint undertaken if necessary. This will be required specifically if there was a pre-operative flexion contracture. At the end of all this, it is important that the release is such that with the implant in situ, there is no buckling or pinching of the device if a Silastic device is used or undue tightness if a two-piece implant is used. Sizing of the implant also requires good judgement, since the proper implant should fit snugly in the joint and be wide enough to abut both bone ends in the midsection. With regard to any repair, this is better undertaken by suturing structures directly onto the bone. To facilitate this and prior to insertion of the implant, small holes should be made and sutures passed. This will allow sound repair of collateral ligaments or the extensor mechanism. Plainly, it is important that these structures are sutured back to their correct anatomical position. For patients with a Boutonnieres deformity, a central slip advancement or lateral band reattachment to the middle phalanx should be undertaken to prevent recurrence of the contracture. In the author’s opinion, it is also useful to perform a tenolysis of the long flexor tendons through a separate volar incision in the palm, particularly if there was some question about tendon excursion prior to surgery.
Finally, an alternative method of approaching the extensor expansion was described by Fahmy et al. in 2001 [17]. Essentially, they separated the lateral bands of the extensor expansion from the central slip, the tendons being retracted as necessary. On closure, the lateral bands are sutured back to the central slip. Plainly whilst this has the advantage following early active mobilization, visualisation of the proximal interphalangeal joint is more limited.
Post-operative Management
As with all specialised surgery to the hand and wrist, the involvement of a hand therapist is strongly recommended particularly someone with experience in managing these difficult procedures. The objectives of this type of surgery are to obtain a pain-free stable joint with a functional arc of movement of approximately 60° or more. At the time of surgery, it is to be hoped that a sound soft tissue repair has been undertaken, and as a consequence, the joint is stable. Generally, after the application of a dressing, a volar slab including the forearm, wrist and the fingertips is applied. Whilst the wrist is held in neutral, the metacarpophalangeal and proximal interphalangeal joints are immobilized in slight flexion. It is of crucial importance however that the arm is elevated post-operatively to reduce swelling and that patients receive adequate analgesia during this period. At the same time, it is our routine practice to give three doses of antibiotics, the first being given on induction prior to surgery and subsequent two doses intravenously at 6 and 12 hours, respectively.
If at the conclusion of surgery the surgeon is of the view that the joint is stable and suitable for early mobilization, on day 2, the dressings can be reduced, wound inspection undertaken and early mobilization begun. Essentially this option also depends on whether single or multiple fingers have been operated upon. Whichever is the case, however, it is important that the patient is given a resting splint to be worn between periods of mobilization and most importantly at night. The splint itself holds the wrist and MCP joints in neutral yet blocks PIP extension at between 20° and 30° (Fig. 20.7). The patient is then encouraged to undertake active PIP joint flexion for between 10 and 20 repetitions per hour. It is important that whilst this is undertaken, the MCP joint remains static. If the patient had a pre-operative Boutonniere deformity, a dynamic extension splint may also be added to the resting splint maintaining the proximal interphalangeal joint in full extension. If a collateral ligament has been repaired as in the lateral approach, this should be protected by a radial outrigger or by “buddy” strapping during mobilization. This method of mobilization continues for 3–4 weeks. From that time, if flexion is poor, then further splint modifications can be instigated. These include positioning the proximal interphalangeal joints in flexion at night and the addition of flexion assist splints during the day (Fig. 20.8). If however an extension lag is the problem, then extension assist splints could be introduced along with a splint to hold the PIP joints in full extension at night. During all this time, the patient is discouraged from undertaking activities of daily living, which could produce deformity of the joint, particularly power or pinch grip. At 6 weeks, protective splints are discontinued, although extension/flexion assist splints can be continued if necessary. A resting night splint is worn for a minimum of 3 months. At that time, a gradual reintroduction to normal function is begun although heavy manual work is avoided.
Finally, if at the time of surgery it is felt that joint is not stable enough to allow early active mobilization, a “delayed mobilization” programme can be instituted. Essentially this involves the patient wearing a resting splint for 3 weeks prior to mobilization. At that time, the programme described above is commenced.
Evaluation
Outcome is related to many factors, particularly the pre-operative status of the finger, any previous surgery as well as the extent of the surgical intervention or any soft tissue reconstruction. For most surgeons working in this field, 20° of extension lag or less with 60° of flexion, that is, movement from 20° to 60°, no angulation and no pain would be regarded as a good result. All of the above with movements from 0° to 75° would be regarded as an excellent result.
Given the close proximity of other joints in the hand particularly the metacarpophalangeal joint, it is plainly difficult to evaluate the outcome of surgery to the proximal interphalangeal joint in isolation. As much all that has been written in the “Evaluation” section of the metacarpophalangeal joint chapter also applies to the proximal interphalangeal joint. This is particularly so with regard to both local and global scoring systems. At this time, whilst little has been written, certainly, it would not be inappropriate to use either the DASH or the SF36 as a single evaluation tool after this surgery.
Generally, however, as with all such systems, any evaluation should also incorporate some measure of pain relief, movement, stability and strength and finally change in function. The former is simply assessed by a visual analogue score which has the added advantage of being able to be administered by post. Movement conversely has obviously to be measured by a clinician as does strength and stability. Function however, again, can be evaluated at a distance by postal questionnaire. The ideal system for measuring function is a series of validated questions based on activities of daily living. The patient responds by indicating their ability to undertake these particular tasks again on a visual analogue score. There are a number of these available for the hand generally, but none for the PIP jt specifically. As a consequence, whilst to date the outcome of PIP joint arthroplasty has been roughly assessed in this fashion, the author is unaware of any explicit scoring or points system.
In 1979, Linscheid et al. from the Mayo Clinic, reporting their results of PIP joint arthroplasty, felt that motion of 60° or more in the usual arc of flexion with the correction of any previous existing deformity to less than 10°, minimal pain and a minimal inhibition of distal interphalangeal joint motion constituted a good result [18]. Motion of 30° or more again in a useful arc with a flexion deformity of less than 60°, an improvement of pre-existing deformity and mild discomfort were signs of a satisfactory result, while motion of 30° or less with the persistence of a swan neck or flexion deformity greater than 60°, persisting pain and recurrence of angulation were an unsatisfactory result. Finally pronounced loss of joint movement, recurrent or worsening deviation, a flexion or extension contracture and significant pain with removal of the implant or revision were signs of a poor outcome.
In 1994, Adamson et al. from Los Angeles in the USA concluded that a good result was a painless PIP joint that had a functional range of motion, a fair result was a painless joint with position or motion outside the functional range and a poor result was a painful joint with a position or motion outside of the functional range [19]. They felt that the functional range of movement of the proximal interphalangeal joint was between 35° and 85° of flexion. They also reported a radiological assessment although this does not appear to have been formalised. Indeed again from the literature whilst various radiological features have been noted, no systematic evaluation has yet been described. With regard to these various x-ray appearances, these include osteophyte or new bone formation which tends to be associated with joint stiffness. In addition, cysts or cortical erosions can be seen which are generally held to be indicators of either loosening or recurrent synovitis. Sclerotic lines around either a portion or an entire implant are also not uncommonly seen. These have been described around Silastic implants, but also the newer pyrocarbon devices. Their significance at this time, however, remains unclear, but presumably represents new bone formation. Finally, movement of the implant as seen on sequential x-rays is said to be a process known as “settling.” By this, it is meant that the implants subside into the bone over a period of time. Unfortunately, on occasion, this can lead to a reduction in the periarticular space with concomitant loss of movement.
Finally, in 1995, Iselin undertook a detailed evaluation of a number of patients who had undergone Swanson Silastic implants [20]. Their evaluation included active range of motion as measured by a goniometer, an evaluation of strength by way of a pinch metre and Jamar dynamometer, an evaluation of lateral stability and alignment, an assessment of pain and finally a radiographic review. For instability, they felt that between 10° and 15° of lateral deviation was probably of little consequence. With regard to the x-ray analysis, either bone resorption or new bone formation was seen around a small number of implants. Finally, he also reported patient satisfaction, that is, a patient evaluation of the outcome. As a result of all this, they classified their outcome into three groups:
-
Group I (good)
-
The arthroplasty met its essential goals: pain-free active flexion greater than 50°, good joint stability and alignment and very good functional results with minimal loss of strength.
-
Group II (fair)
-
Active flexion less than 50°, good stability and alignment and a good functional result.
-
Group III (poor)
-
Presence of one or more of the following: either stiffness, pain, instability or malalignment. These joints were usually further treated by revision or arthrodesis.
In the author’s opinion, there is no doubt that at least where the latest designs of PIP arthroplasty are being evaluated, detailed examination is crucial. It is also important for surgeons newly undertaking these operations that an accurate outcome audit is put in place. Whilst all the modalities of evaluation described above are relevant, particularly pain relief and improvement in function, it does appear that much store is set on active movement of the proximal interphalangeal joint. It is for this reason the author would suggest that a good result would be active movement from 30° to 60°, with no angulation and pain. Excellent results would again have no angulation or pain with a greater range of motion. Anything less than this should be classified as an unsatisfactory or poor result.
Results
Silastic Interposition Arthroplasty
The initial results of Silastic interposition arthroplasty or implant resection arthroplasty, as it was first described by Swanson, were reported in 1973 [4] (Fig. 20.9). In this article, the philosophy, surgical technique, post-operative management and initial results are described. Swanson even detailed the concomitant treatment of swan neck and boutonniere deformities. With regard to results, the outcome of 222 PIP joint replacements in 118 hands followed up for between 1 and 6 years was reported. Predominantly these were in patients with rheumatoid arthritis. The average range of motion was from 4° extension lag through to 67° of flexion. Significant improvement was also seen in patients with a pre-operative boutonniere or swan neck deformity. Complications only occurred in 2.2% with fractures in five cases (2%), subluxation in one (0.4%) and infection in one other (0.4%).
Updated results in 1985 reported 812 PIP implants; again there was a significant improvement in most cases with an active range of motion of greater than 40° [21]. In addition, the majority of patients (98.3%) reported significant pain relief, and radiologically a favourable bone response was observed. In a few cases, however, bone overgrowth was seen. A complication rate of 5.2% was noted, principally again fracture of the implant, the explanation for this being that this was with the original silicone rather than the latest composition available today. Recurrent “swan necking” was seen in 21% of cases and ulna deviation in 3.7%. Infection was again uncommon as was dislocation, the overall revision rate being 10.9%.
Since then there have been numerous reports from various units throughout the world on this particular implant; these are detailed in Table 20.1. Essentially, in patients with inflammatory arthritis, which is probably the predominant indication, most patients achieve satisfactory pain relief. Generally, however, there is little improvement in movement from pre-operative values. In addition, in patients with a pre-operative swan neck or boutonniere deformity, there is often a recurrence in the long term. Despite this, most authors report a significant improvement in function. Complications however continue to be reported and principally involve fracture of the implant. Takigawa et al. in 2004 reported cystic changes in the shafts of the proximal and middle phalanx in 45% of cases, a particularly worrying finding indicative of silicone synovitis [27]. When the implant is used following trauma, the initial results are again favourable. Ultimately, however, the implant breaks and a higher revision rate has been reported. Finally, there are few reports of this implant being used in patients with primary osteoarthritis.
A number of articles pertinent to this implant have been published, these are discussed below.
Sutter Design
The Sutter PIP joint arthroplasty is of an identical design to the Sutter MCP joint, although obviously with smaller dimensions (Fig. 20.10).
In 1999, Mathoulin and Gilbert from Paris reported their experience of 21 Sutter implants used for post-traumatic arthritis with an average follow-up of 2 years [30]. With these patients, there was a complete absence of pain in 18 with an active range of movement of 55° compared to 15° pre-operatively. Two implants however had fractured.
Neuflex Design
The Neuflex PIP joint arthroplasty is again a modification of the Swanson with a 15° flexion prebend potentially mimicking the anatomically neutral position. A publication by Merle et al. (2011) reviewed 51 arthroplasties in 43 patients followed up for a mean of 36 months [31]. Movement improved from 38° pre-operatively to 63° post-operatively. Added to that, functional scores improved although in five cases (10%) further surgery was required. One particular issue with the lateral approach was continuing instability.
Osseointegrated Implants
The first report on osseointegrated implants was from Moller et al. from Gotenberg, Sweden, in 1999 [32]. They reported the results of 32 implants in 12 patients suffering predominantly with rheumatoid arthritis. This implant has two screw-type titanium fixation devices, which are linked by a flexible silicone spacer. Iliac crest bone graft was used as a supplement in most cases. The follow-up was however short, being 27 months; movements averaged from 11° through to 67° with an average of 56° active movement. Of the 22 implants, 41 of the 44 titanium implants were osseointegrated radiologically. Unfortunately, in 4 of the 22 implants, there were fractures of the Silastic spacers, with deformity in 27%. Despite that, patient satisfaction was high, although it was felt that some modification of the Silastic spacer would be advisable.
Lundborg and Branemark in 2000 reported their results of 25 of the same implants in 19 patients [33]. The indications for surgery here were predominantly posttraumatic arthritis and primary osteoarthritis. At follow-up, at an average of 8.5 years, 47 of the 50 titanium fixtures were osseointegrated. Unfortunately, the Silastic spacers had again fractured in 68% and had to be replaced in a number. The active range of motion was 41°.
A further updated radiological evaluation, published in 2004, of 27 proximal interphalangeal and 212 metacarpophalangeal joints in 86 patients, again predominantly suffering with rheumatoid arthritis, revealed osseointegration in 94% of cases [34]. The authors also identified that, in a small number of cases, the proximal fixtures showed radiological signs of loosening mainly in the first 3 years after surgery. Again, they felt a more durable Silastic spacer would be advantageous.
Surface Replacement
Following the general dissatisfaction with PIP joint replacement in the late 1970s, Linscheid and others from the Mayo Clinic developed a surface replacement prosthesis using the more conventional materials of cobalt chrome and ultra-high molecular weight polyethylene (UHMWPE). The design was essentially anatomical with stem fixation into the proximal and middle phalanges (Fig. 20.11), the stems themselves extending beyond the midpoint of the phalanges being fixed by the use of polymethylmethacrylate cement. The authors did acknowledge that for this type of implant to be successful, it required precise alignment together with soft tissue preservation or repair for optimal function.
In 1979, they reported their results of 66 implants in 47 patients over a 14-year period. The diagnosis in 37 cases was of osteoarthritis, 16 had posttraumatic arthritis, and 13 had rheumatoid arthritis. The mean follow-up was 4.1 years (1–14 years). Using their own criteria previously described, the results were quoted as good in 32, fair in 19 and poor in 15. Otherwise having tried all the surgical approaches, they concluded that the dorsal approach was superior to the others. In addition, pre-existing deformity or extreme bone/soft tissue loss often resulted in poor results.
A further publication by Johnstone (2001) from Australia reported on his results of 20 joints in 13 patients [35]. Again the predominant indications were osteoarthritis or posttraumatic arthritis. Excellent long-term results were seen in 18 of the 20 patients with the active range of motion being 73°. Johnstone also felt that an early active mobilization was the best post-operative therapy programme.
Thereafter, there is a publication by Jennings and Livingstone (2015) which reported on the results of 39 cases followed up for 9.3 years [36]. The average arc of motion had deteriorated from 64° following surgery to 56 degrees at the latest follow-up. There were, however, no significant x-ray changes, and no further revisions had been undertaken.
Results of the Ascension Pyrocarbon PIP Joint Replacement
Pyrocarbon is a synthetic material formed by the pyrolysis of a hydrocarbon gas. This material is coated onto a high-strength graphite substrate to form the basis of an implant. In the case of the pyrocarbon PIP implant, this is similar in design to the surface replacement being unlinked, with stem fixation into the proximal and middle phalanges. Please note that polymethylmethacrylate cement is not used with this implant. There are however a set of instruments/cutting jigs which allow the implants to be inserted in a standard fashion, preserving the soft tissues, particularly the collateral ligaments and volar plate (Fig. 20.12).
The first published article of this implant was by Schulz et al. from Germany, who reported their results in 20 patients with idiopathic or posttraumatic arthritis affecting the proximal interphalangeal joint [37]. The range of follow-up was short between 0.5 and 2.5 years. The majority of patients were pleased with pain relief and had an average active range of motion of 50°. X-rays however did reveal some peri-prosthetic cyst formation with potential loosening of the proximal as well as the distal component in some patients. There was however no correlation between these radiological observations and clinical outcome. However, in three cases, the prosthesis had to be revised to an arthrodesis. In conclusion, the authors felt that further investigation was needed to improve the radiological results in the long term, particularly with regard to osseointegration.
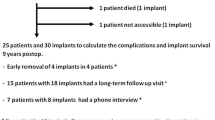
At Wrightington, our initial results were presented at the British Hand Society meeting in 2003 [38]. Here the results of 32 joints in 21 patients were submitted. Again, the follow-up was short, and the majority of patients had either osteoarthritis, a post-traumatic problem or rheumatoid arthritis. All implants were put in through a dorsal approach using the appropriate instruments. A number of complications were noted, subluxation in two patients, stiffness in another two who required further surgical intervention and finally a superficial infection in one. Movement improved significantly, particularly in patients with osteoarthritis who prior to surgery had only 30° active movement, compared to 55° at the latest follow-up. Patients with posttraumatic arthritis improved similarly although those with rheumatoid less so. Overall, the vast majority of patients were satisfied, and there was no radiological evidence of loosening.
Thereafter, there are a number of articles published on the outcome of this implant. These are consolidated in Table 20.2. Effectively these show good clinical results with a modest reoperation rate, the most potentially worrying issue being a high rate of subsidence/migration on later x-rays.
Other Proximal Interphalangeal Joint Implant Designs
Prior to the introduction of their pure surface replacement, Linscheid and others, from the Mayo Clinic, experimented with a constrained uniaxial linked implant in this situation. Again the implant was cemented and the two components linked by a polyethylene bushing. In a report in 1979, again mainly in patients with osteoarthritis, they found unsatisfactory or poor results in 47 of 67 implants followed up for 15 months, the principal problem being loosening of the components. It is my understanding that this implant is no longer available.
Dryer et al., from the University of Iowa, in 1984, reported their results with the Flatt implant amongst others in patients with rheumatoid arthritis [47]. Again, this is a linked-type implant, fixation being by two metal prongs into both the proximal and middle phalanx (Fig. 20.13). At an average 6.2-year follow-up, movements for the Flatt prosthesis ranged from 28° through to 45° with 15° of active movement. Further follow-up indicated that this movement gradually decreased over time. Radiographically cortical perforation by the prosthesis was common. Despite this, patient satisfaction was high although again I believe this implant is no longer available commercially.
In 1997, Condamine and others, from France, reported their results with the so-called digital joint arthroplasty (DJOA) implant used exclusively in patients with osteoarthritis between 1985 and 1994 [48], with the proximal interphalangeal joint being replaced in 19 cases. Range of motion at follow-up was only slightly improved by arthroplasty, measuring 50°, with some improvement in extension. The majority of patients however reported satisfactory pain relief. Radiologically there were late signs of periarticular ossification. At that time, the implant was being redesigned.
Subsequently in 2000, Mentzel from Ulm in Germany reported their experience with the DIGITOS-prosthesis [49]. This is a cemented, modular, hinged prosthesis, which was used in seven patients with osteoarthritis of the proximal interphalangeal joint. At follow-up of 2 years, the functional results were found to be good. Movement improved from 51.5° pre-operatively to 60.5° at 3 months after surgery, decreasing to 53° at 1 year and 49.5° by the end of the second year. Radiologically no implant was loose, and all patients were pain-free. These patients continue to be monitored carefully.
The preliminary results of the LPM prosthesis were presented at the British Society of Surgery of the Hand Autumn Meeting in 2005. Twenty-one implants had been inserted in 15 patients over a 1-year period. The average arc of movement was 50°, improving from 28° pre-operatively. The patients with osteoarthritis gained and maintained the largest improvement with those undertaken for trauma and rheumatoid arthritis less so. In this study, there were no post-operative complications, although a number of surgeons in the audience indicated that they had experienced problems including osteolysis with early to mid-term failure of the proximal component of the prosthesis. Subsequently more of these problems have been reported to the “Audit Committee” of the British Hand Society, and as a consequence, the implant has now been withdrawn.
In 2015, Schindele et al. reported the results of the CapFlex-PIP [50]. They reported ten patients in cases of osteoarthritis followed up for 12 months. They reported improved motion from 42° to 51° although this was not statistically significant. Pain, however, was reduced and functional scores improved. Two patients underwent tenolysis and tended to improve motion (Fig. 20.14).
Finally, in 2016, Flannery et al. reported the results of the MatOrtho proximal interphalangeal joint arthroplasty with a minimum 2-year follow-up [51]. This anatomical implant is based on work published by Lawrence et al. (2004) on the morphological appearance and measurements of the proximal interphalangeal joint [52]. The proximal phalanx component is made of cobalt chrome and the middle phalanx of high-density polyethylene which is mobile bearing. Both components are stemmed with hydroxyapatite coating. The implant is not linked (Fig. 20.15).
Of the original article, there were 100 implants followed up between 2 and 6.5 years. Implant survival was 85% from 4 years onwards. There were, however, 13 revisions in the first year for stiffness, instability and component disassembly. It was noted, however, that patients who had a stiff or deformed PIP joint prior to surgery did not do as well.
A more recent paper by Fowler et al. (submitted) reports the results of this implant inserted through a lateral approach rather than a dorsal [53]. It does appear that inserting this implant through a lateral approach results in significant improvement in post-operative range of motion.
Complications and Their Management
As with all implants, the potential range of complications is large. For the Silastic replacements however, a review of literature would indicate an overall revision rate of less than 10%. The principal complication with this type of implant is fracture of the silicone (Fig. 20.16); indeed, a similar problem has been noted with the linkage part of the titanium osseointegrated-type implant. Initial published series have reported between 5% and 10% incidence of this complication. Undoubtedly, however, the longer the follow-up, the more likely it is that this complication will occur. Having said that, this does not necessarily mean that revision surgery will be required, revision only being undertaken if there is significant pain and deformity. In the author’s experience, revision for this complication would take the form of either revision to another Silastic implant, arthrodesis or an excision arthroplasty.
Other complications include infection, which is obviously a complication of significant concern. Generally this is treated initially by removal of the implant, curettage and the administration of long-term antibiotics, with secondarily either leaving the joint as an excision arthroplasty, fusion or the secondary reinsertion of a further implant, either unlinked or linked (silastic). The authors’ experience with this complication is fortunately small, and of the three cases seen, all have been treated by excision arthroplasty. This has resulted in a complete resolution of the infection in all cases, although the patients have been left with some instability of the proximal interphalangeal joint. Fortunately, however, some movement has been retained with a complete absence of pain. As a consequence, the patients were generally reluctant to undergo a secondary procedure. I am however aware of a patient, under a colleagues care, who did undergo the successful reinsertion of a Silastic spacer, which helped stabilize the joint. Fortunately, it did not result in a recurrence of the infection.
The third most worrying complication is dislocation or instability. Obviously, this is far more common in patients with unlinked implants and can result in deformity and loss of movement. Interestingly enough however, they often remain pain-free. With regard to management, it is the authors’ opinion that for a surface replacement, the prevention of any recurrent deformity is of paramount importance. If the patient presents initially with a significant boutonniere or swan neck deformity or indeed radial or ulnar angulation, it is probably inadvisable to consider this type of implant. A better primary procedure would be either an arthrodesis or a linked-type implant. Whilst soft tissue realignment in combination with a surface replacement is feasible, the results are at best unpredictable. Secondly but of equal importance is that if at the time of surgery the surgeon is concerned that the new joint may not be stable, then he would recommend immobilization for a period of 3 weeks prior to beginning therapy. The position of immobilization would be with the PIP joint held at somewhere between 10° and 20° of flexion. Despite this, and if instability does develop, then revision can be undertaken. Again, the implant can be removed and replaced or the joint fused. However and perhaps ideally, any revision should be augmented by a soft tissue stabilization. Whilst this results in a somewhat diminished range of motion, the patient can be left with a pain-free joint, in a good functional position, with some movement. This situation is better than an arthrodesis.
Usage of some of the earlier types of linked implant with their high rates of loosening has resulted in an increase in expertise in the management of loose components. Generally, loosening of an implant will ultimately become symptomatic and result in its removal followed by either fusion, the insertion of another implant linked (Silastic) or unlinked with or without a soft tissue reconstruction. The insertion of a Silastic implant with soft tissue reconstruction has been particularly successful in the authors’ experience. More specifically, the operation is often easy to perform as removal of the primary implant leaves spaces in the phalanges, which readily accept a Silastic hinged-type implant. Again whilst the spacer will stabilize the joint and result in good pain relief, movements can be limited. At this time, the author has information on two cases of pyrocarbon implants, which have been revised for loosening. The first was revised with larger components, that is, with a thicker stem, with the additional insertion of bone graft and so far has remained stable. The second was revised to a fusion again requiring the insertion of a bone graft. At this time, whilst the arthrodesis is incomplete, the patient’s finger is pain-free and in a good functional position.
Another complication is bone overgrowth and stiffness. Swanson reported this in approximately 5% of his cases following Silastic replacement, although other authors have reported a higher incidence. This tends to be seen more in patients with osteoarthritis rather than rheumatoid arthritis. Interestingly enough, whilst this complication does lead to reduced movement, the patient is left with little pain, stability and satisfactory function. As a consequence of this, many patients are reluctant to undergo revision surgery. However if revision is undertaken, effectively this includes refashioning of the bony cuts, the reinsertion of often larger components and a further soft tissue release.
Whilst loosening can also occur with a Silastic implant, this complication is undoubtedly uncommon and occurs much less frequently than fracture of the stem. Radiologically however, cysts can sometimes be seen surrounding Silastic implants. These are felt predominantly to be due to silicone synovitis, which is a giant cell reaction to small fragments of silicone. A number of authors have reported this radiological finding, although surprisingly only a few have described undertaking any revision surgery. Certainly, the author has never had to perform any procedure for this complication at the PIP level. One would assume however that treatment would involve removal of the silicone implant, curettage, bone grafting and fusion as appropriate.
Finally, given the potential for complications, it should again be noted that in virtually all the series reviewed, the incidence of revision surgery is less than 10%. Even then, in patients who develop complications, there are a number of surgical options which can ultimately lead to a pain-free, stable and functional joint.
References
Carroll RE, Taber TH. Digital arthroplasty of the proximal interphalangeal joint. J Bone Joint Surg. 1954;36A(5):912–20.
Pellegrini VD, Burton RI. Osteoarthritis of the proximal interphalangeal joint of the hand: arthroplasty or fusion? J Hand Surg. 1990;15A:194–209.
Flatt AE, Powers WR. Rheumatoid hand. Physical therapy following insertion of Flatt prosthesis. Phys Ther Rev. 1961;41:709–13.
Swanson AB. Implant resection arthroplasty of the proximal interphalangeal joint. Orthop Clin North Am. 1973;4(4):1007–29.
Neibauer JJ, Shaw JL, Doren WW. Silicone-dacron hinge prosthesis. Design, evaluation and application. Ann Rheum Dis. 1969;28(5:Suppl):56–8.
Durham-Smith G, McCarten GM. Volar plate arthroplasty for closed proximal interphalangeal joint injuries. J Hand Surg (Br). 1992;17B:422–8.
Dionysian E, Eaton RG. The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg. 2000;25A:429–37.
Burton RI, Campolattaro RM, Ronchetti PJ. Volar plate arthroplasty for osteoarthritis of the proximal interphalangeal joint: a preliminary report. J Hand Surg. 2002;27A:1065–72.
Johansson SH, Engkvist O. Small joint reconstruction by perichondrial arthroplasty. Clin Plast Surg. 1981;8(1):107–14.
Seradge H, Kutz JA, Kleinert HE, Lister GD, Wolff TW, Atasoy E. Perichondrial resurfacing arthroplasty in the hand. J Hand Surg. 1984;9A(6):880–6.
Hasegawa T, Yamano Y. Arthroplasty of the proximal interphalangeal joint using costal cartilage grafts. J Hand Surg (Br). 1992;17B:583–5.
Katsaros J, Milner R, Marshall NJ. Perichondrial arthroplasty incorporating costal cartilage. J Hand Surg [Br]. 1995;20B(2):137–42.
Harrison SH. The proximal interphalangeal joint in rheumatoid arthritis. Hand. 1971;3(2):125–30.
Lipscomb PR. Synovectomy of the distal two joints of the thumb and fingers in rheumatoid arthritis. J Bone Joint Surg. 1967;49A(6):1135–9.
Schneider LH. Proximal interphalangeal joint arthroplasty: the volar approach. Semin Arthroplasty. 1991;2(2):139–47.
Lin HH, Wyrick JD, Stern PJ. Proximal interphalangeal joint silicone replacement arthroplasty: clinical results using an anterior approach. J Hand Surg. 1995;20A:123–32.
Fahmy NR, Lavender A, Brew C. A conservative approach for proximal interphalangeal joint arthroplasty. J Hand Surg (Br). 2001;26B:235–7.
Linscheid RL, Dobyns JH, Beckenbaugh RD, Cooney WP. Proximal interphalangeal joint arthroplasty with a total joint design. Mayo Clin Proc. 1979;54:227–40.
Adamson GJ, Gellman H, Brumfield RH, Kuschner SH, Lawler JW. Flexible implant resection arthroplasty of the proximal interphalangeal joint in patients with systemic inflammatory arthritis. J Hand Surg. 1994;19A:378–84.
Iselin F, Conti E. Long-term results of proximal interphalangeal joint resection arthroplasties with a silicone implant. J Hand Surg. 1995;20A(3:Part 2):95–7.
Swanson AB, Maupin BK, Gajjar NV, de Groot Swanson G. Flexible implant arthroplasty in the proximal interphalangeal joint of the hand. J Hand Surg. 1985;10A:796–805.
Iselin F. Arthroplasty of the proximal interphalangeal joint after trauma. Hand. 1975;7(1):41–2.
Iselin F, Pradet G. Resection arthroplasty with Swanson’s implant for posttraumatic stiffness of proximal interphalangeal joints. Bull Hosp Jt Dis Orthop Inst. 1984;44(2):233–47.
Ashworth CR, Hansraj KK, Todd AO, Dukhram KM, Ebramzadeh E, Boucree JB, Hansraj MS. Swanson proximal interphalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res. 1997;342:34–7.
Hage JJ, Yoe EPD, Zevering JP, de Groot PJM. Proximal interphalangeal joint silicone arthroplasty for posttraumatic arthritis. J Hand Surg. 1999;24A:73–7.
Herren DB, Simmen BR. Palmar approach in flexible implant arthroplasty of the proximal interphalangeal joint. Clin Orthop Relat Res. 2000;371:131–5.
Takigawa S, Meletiou S, Sauerbier M, Cooney WP. Long-term assessment of Swanson implant arthroplasty in the proximal interphalangeal joint of the hand. J Hand Surg. 2004;29A:785–95.
Bales JG, Wall LB, Stern PJ. Long-term results of Swanson silicone arthroplasty for proximal interphalangeal joint osteoarthritis. J Hand Surg. 2014;39A(3):455–61.
Proubasta IR, Lamas CG, Natera L, Millan A. Silicone proximal interphalangeal joint arthroplasty for primary osteoarthritis using a volar approach. J Hand Surg. 2014;39A(6):1075–81.
Mathoulin C, Gilbert A. Arthroplasty of the proximal interphalangeal joint using the Sutter implant for traumatic joint destruction. J Hand Surg. 1999;24B(5):565–9.
Merle M, Villani F, Lallemand B, Vaienti L. Proximal interphalangeal joint arthroplasty with silicone implants (NeuFlex) by a lateral approach: a series of 51 cases. J Hand Surg. 2011;37E(1):50–5.
Möller K, Sollerman C, Geijer M, Brånemark PI. Early results with osseointegrated proximal interphalangeal joint prostheses. J Hand Surg. 1999;24A:267–74.
Lundborg G, Brånemark PI. Osseointegrated proximal interphalangeal joint prostheses with a replacable flexible joint spacer-long term results. Scand J Plast Reconstr Surg Hand Surg. 2000;34:345–53.
Möller K, Sollerman C, Lundborg G. Radiographic evaluation of osseointegration and loosening of titanium implants in the MCP and PIP joints. J Hand Surg. 2004;29A:32–8.
Johnstone BR. Proximal interphalangeal joint surface replacement arthroplasty. Hand Surg. 2001;6(1):1–11.
Jennings CD, Livingstone DP. Surface replacement arthroplasty of the proximal interphalangeal joint using the SR PIP implant: long-term results. J Hand Surg. 2015;40A(3):469–73.
Schulz M, Müller-Zimmermann, Behrend M, Krimmer H. Frühe Ergebnisse der Fingermittelgelenkendo-prothetik mit der Pyrocarbonprothese (Ascension) bei idiopathischen und posttraumatischen Arthrosen. Handchir Mikrochir Plast Chir. 2005;37:26–34.
Watts AC, Hearnden AJ, Trail IA, Hayton MJ, Nuttall D, Stanley JK. Pyrocarbon proximal interphalangeal joint arthroplasty: minimum 2 year follow-up. J Hand Surg. 2012;37A:882–8.
McGuire DT, White CD, Carter SL, Solomons MW. Pyrocarbon proximal interphalangeal joint arthroplasty: outcomes of a cohort study. J Hand Surg. 2011;37E(6):490–6.
Hutt JRB, Gilleard O, Hacker A, Citron N. Medium-term outcomes of pyrocarbon arthroplasty of the proximal interphalangeal joint. J Hand Surg. 2012;37E(6):497–500.
Mashhadi SA, Chandrasekharan L, Pickford MA. Pyrolytic carbon arthroplasty for the proximal interphalangeal joint: results after minimum 3 years of follow-up. J Hand Surg. 2012;37E(6):501–5.
Tägil M, Geijer M, Abramo A, Kopylov P. Ten years’ experience with a pyrocarbon prosthesis replacing the proximal interphalangeal joint. A prospective clinical and radiographic follow-up. J Hand Surg. 2014;39E(6):587–95.
Heers G, Springorum HR, Baier C, Götz J, Grifka J, Renkawitz T. Proximal interphalangeal joint replacement with an unconstrained pyrocarbon prosthesis (Ascension): a long-term follow-up. J Hand Surg. 2012;38E(6):680–5.
Reissner L, Schindele S, Hensler S, Marks M, Herren DB. Ten year follow-up of pyrocarbon implants for proximal interphalangeal joint replacement. J Hand Surg. 2014;39E(6):582–6.
Storey PA, Goddard M, Clegg C, Birks ME, Bostock SH. Pyrocarbon proximal interphalangeal joint arthroplasty: a medium to long term follow-up of a single surgeon series. J Hand Surg. 2015;40E(9):952–6.
Pettersson K, Amilon A, Rizzo M. Pyrolytic carbon hemiarthroplasty in the management of proximal interphalangeal joint arthritis. J Hand Surg. 2015;40A(3):462–8.
Dryer RF, Blair WF, Shurr DG, Buckwalter JA. Proximal interphalangeal joint arthroplasty. Clin Orthop Relat Res. 1984;185:187–94.
Condamine JL, Fourquet M, Matcucci L, Pichereau D. L’arthrose primitive métacarpo- phalangienne et interphalangienne proximale à la main. Ann Chir Main. 1997;16(1):66–78.
Mentzel M, Hoss H, Ebinger T, Halder A, Kinzl L, Wachter NJ. DIGITOS- Fingermittelgelenk-prothesen-Zweijahresergebnisse. Handchir Mikrochir Plast Chir. 2000;32:347–52.
Schindele SF, Hensler S, Audigé L, Marks M, Herren DB. A modular surface gliding implant (CapFlex-PIP) for proximal interphalangeal joint osteoarthritis: a prospective case series. J Hand Surg Am. 2015;40(2):334–40.
Flannery O, Harley O, Badge R, Birch A, Nuttall D, Trail IA. MatOrtho proximal interphalangeal joint arthroplasty: minimum 2 year follow up. J Hand Surg. 2016;41E(9):910–6.
Lawrence T, Trail IA, Noble J. Morphological measurements of the proximal interphalangeal joint. J Hand Surg. 2004;29B:244–9.
Fowler A, Arshad S, Talwalkar S, Trail IA. MatOrtho proximal interphalangeal joint arthroplasty via lateral approach: minimum 2-year follow-up. Asian Pac J Hand Surg. 2020, Submitted.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Trail, I.A. (2021). Primary Proximal Interphalangeal Joint Arthroplasty. In: King, G.J.W., Rizzo, M. (eds) Arthroplasty of the Upper Extremity. Springer, Cham. https://doi.org/10.1007/978-3-030-68880-6_20
Download citation
DOI: https://doi.org/10.1007/978-3-030-68880-6_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-68879-0
Online ISBN: 978-3-030-68880-6
eBook Packages: MedicineMedicine (R0)