Abstract
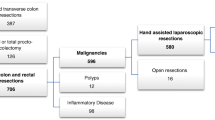
The use of minimally invasive approaches to colorectal pathologies has significantly increased in the past three decades. The benefits include faster recovery and better cosmetic results without an increase in complications or inferior oncologic outcomes. Hand assisted total abdominal colectomy is the most obvious example of a procedure that if done open would require a long and disfiguring incision and instead can now be done through a small suprapubic mini laparotomy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
A total colectomy may be performed for a variety of reasons. A common indication for total colectomy is patients with Ulcerative Colitis (UC) that have failed to respond to medical therapy, or when the side effects of medical therapy outweigh the benefits. Ulcerative Colitis also increases a patient’s risk for cancer and dysplasia [1]. Either of these findings in the setting of chronic pancolitis isan indication for surgery in UC [1]. Additional indications for total colectomy can include colonic inertia, familial cancer syndromes, toxic megacolon, hemorrhage, perforation, or obstruction. In the case of patients with acute UC or in unstable patients requiring an emergent operation, an end ileostomy is given rather than performing an anastomosis. The technique of hand-assisted laparoscopic total colectomy with end ileostomy will be the focus of this chapter.
The laparoscopic approach has been shown to be safe in acute UC [2,3,4]. A minimally invasive approach to colectomy reduces morbidity, length of stay, readmission rates, and results in better cosmesis than an open approach [5]. A hand-assisted approach for total colectomy facilitates colonic mobilization and is associated with a reduction in operative time and rate of conversion to open when compared to straight laparoscopy, with no difference in complication rates or short-term outcomes [6,7,8]. Compared to the open approach, patients with severe colitis that undergo laparoscopic total colectomy have a faster recovery, leading to quicker progression to completion of restorative proctocolectomy [9].
2 Clinical Presentation
Patients with life-threatening sepsis, hemorrhage, or perforation must be taken to the operating room emergently. Patients with refractory UC should be initially resuscitated with intravenous fluids and medically optimized prior to surgery. This includes optimizing medical management of their colitis, typically with steroids and rescue therapy of infliximab or cyclosporine [10]. These patients also often have severe malnutrition that may require preoperative parenteral nutrition. Anemia is a common finding secondary to chronic disease as well as blood loss from the colon, and should be corrected with blood transfusions and/or iron infusions based on the severity. If the patient fails to respond to medical management after a time period of 3–5 days for corticosteroids or 5–7 days for other rescue therapies, then operative intervention in the form of total colectomy should be considered [10].
3 Preoperative Evaluation
The patient should be marked for an ileostomy by the enterostomal therapist. Preoperative marking to ensure optimal stoma location increases the ability of the patient to care for the stoma and maintain a secure seal without leakage. Improperly located stomas lead to leakage of stool, peristomal skin inflammation and excoriation, emotional stress, and increased cost [11]. Preoperative education on life with an ileostomy and caring for an ostomy can help prepare a patient mentally and alleviate concerns.
The patient undergoes mechanical bowel preparation with the addition of oral antibiotics, in our practice metronidazole and neomycin. This practice has been shown to make the colon easier to handle during surgery and decrease the incidence of surgical site infections [12]. Patients are given clear liquids the day before surgery and up to 2 hours prior to the operation.
To reduce opioid use and ileus rates, patients are started preoperatively on a multimodal pain management protocol that includes celecoxib, gabapentin, acetaminophen, and alvimopan. Intravenous broad-spectrum antibiotics are given within 1 hour of skin incision in accordance with surgical quality guidelines. Stress dosing of steroids may be required for patients that have been on chronic corticosteroid therapy. Prophylactic dosing of enoxaparin or subcutaneous heparin and sequential compression device (SCD) stockings are placed prior to induction of anesthesia to prevent venous thromboembolism.
4 Technique
4.1 Patient Positioning
The patient is placed on a self-securing pad with a chest strap to prevent slippage with changes in bed position. Following induction of general anesthesia, an orogastric tube and indwelling urinary bladder catheter are placed. The patient is placed with buttocks at the bottom of the table in a modified lithotomy position using Yellofin ® Stirrups (Allen Medical, Acton, MA) with the thighs even with the hips and knees in line with the contralateral shoulder. All pressure points are appropriately padded, ensuring no pressure on the peroneal nerves. Both arms are tucked in the adducted position. Rectal irrigation is performed and a mushroom tip catheter is left in the rectum, connected to a drainage bag. The skin is prepped with 2% chlorhexidine-based solution and the patient is draped in a standard manner. Laparoscopic monitors are placed on either side of the patient at the shoulder.
-
Troubleshooting: Placement in lithotomy position allows access to the rectum for irrigation and placement of the drainage tube, and also allows the surgeon or assistant to stand between the legs which is helpful when operating in the upper abdomen. Patient must be well-secured to the bed due to steep changes in position throughout the operation.
4.2 Port Placement
A circular incision is made at the future ileostomy site. Dissection is carried down through the subcutaneous tissue to the fascia. The fascia is freed from the subcutaneous tissue and a pursestring of 0 Vicryl suture is placed. The anterior rectus sheath is opened longitudinally, muscle fibers are retracted, and the posterior rectus sheath is opened longitudinally. A 12 mm trocar is inserted and secured in place with the pursestring. Pneumoperitoneum is established and maintained at 15 mm Hg. Two additional 5 mm trocars are placed in the umbilicus and left lower quadrant. The abdominal cavity is laparoscopically explored with a 5 mm camera at the umbilical port site, and if a laparoscopic operation appears to be feasible the hand port incision is created. A 7 cm transverse incision is made 2–3 cm superior to the pubic symphysis anddissection is carried to the fascia. The fascia is opened transversally for 7 cm, the muscle is dissected free from the anterior rectus sheath, and the midline and peritoneum are opened. A GelPort is placed (Applied Medical, Rancho Santa Margarita, CA) and pneumoperitoneum is reestablished (Fig. 27.1).
-
Troubleshooting: The open approach to placing the 12 mm trocar at the stoma site allows for safe access to the abdominal cavity using an incision that will be needed irrespective of the surgical approach. The purse-string suture must be tight enough to prevent pneumoperitoneum from escaping. We tighten the pursestring to the fascia by placing a small section of red rubber catheter over the suture and pushing it down to the fascia with a hemostat in the fashion of a Rommel tourniquet.
4.3 Specimen Mobilization
The patient is rotated to the left and in slight Trendelenburg position.With the surgeon standing on the patient’s left side with the left hand in the GelPort, right colon dissection is started in a medial to lateral fashion. The omentum is placed over the stomach into the left upper quadrant and small bowel swept to the left side. The cecum is retracted upward to the anterior abdominal wall to identify the ileocolic pedicle. The pedicle is grasped and elevated (Fig. 27.2). The avascular plane below the vascular pedicle is incised and dissected free to allow clear visualization of the duodenum below the mesentery. The vessel is divided using a vessel-sealing device such as the Ethicon EnSeal device (Ethicon Endo-Surgery, Cincinnati, OH) (Fig. 27.3).
-
Troubleshooting: Identification of the duodenum during isolation of the ileocolic pedicle is important prior to dividing the vessels. The duodenum can be in close proximity to the ileocolic vessels and can be injured if not identified and swept downward and away from the vessels.
Medial to lateral mobilization of the ascending colon is performedby using a posterior sweeping motion in the avascular plane to allow the mesentery and cecum to separate anteriorly from the posterior structures. The right colon should be completely mobilized from the retroperitoneum all the way out to the side wall of the abdomen using the left hand for retraction upward and a laparoscopic grasper or sealing device in the surgeon’sright hand to develop the plane. This is performed down to the cecum and up to the third portion of the duodenum and towards the hepatic flexure (Fig. 27.4). The duodenum should be separated from the overlying mesentery of the right colon using the left hand for anterior retraction of the mesentery all the way up to the hepatic flexure peritoneal attachments. Care is taken when sweeping the duodenum medially (Fig. 27.5).
-
Troubleshooting: mobilization of the mesentery from the retroperitoneum should be carried out as lateral as possible to the abdominal side wall laterally and to the hepatic flexure superiorly. This more clearly defines the lateral avascular plane and prevents dissection into the retroperitoneum when performing lateral mobilization.
The terminal ileum is released from inferior and lateral attachments to provide enough length to allow for a tension-free ileostomy (Fig. 27.6).The colon is retracted medially and the lateral attachments of the right colon are divided sharply, being careful to stay in the lateral avascular plane (Fig. 27.7).The right colon should now be mobilized completely from the retroperitoneum, exposing the entire sweep of the duodenum, a portion of the head of the pancreas, and right psoas muscle.
-
Troubleshooting: The right ureter may be visible near the base of the cecum as it passes over the iliac artery. Staying in the attachments close to the cecum and terminal ileum can prevent dissection into the retroperitoneum and possible injury of the ureter and vascular structures.
The patient is placed in reverse Trendelenburg position and an initial gentle left tilt. The surgeon moves to the patient’s right side with the assistant between the legs. The hand is used to apply downward traction on the omentum as the stomach is retracted cephalad. The omentum is divided with the specimen just distal to the gastroepiploic arcade to enter the lesser sac (Figs. 27.8 and 27.9).
-
Troubleshooting: Staying close to the transverse colon provides dissection of the omentum in a relatively avascular plane and prevents injury to the gastric vessels. The posterior wall of the stomachshould be visualized as the lesser sac is entered.
This dissection plane is continued from right to left, progressively rotating the patient to the right. This is continued toward the splenic flexure, fully exposing the lesser sac and facilitating exposure of the transverse colon mesentery. Once the omentum is divided, the transverse colon is grasped and elevated anteriorly. Beginning at the edge of mesentery created by dividing the ileocolic pedicle, the transverse mesocolon is divided from the patient’s right to the left (Fig. 27.10). Care is taken to isolate the middle colic vessels prior to dividing with the energy device to ensure hemostasis (Fig. 27.11).
-
Troubleshooting: When dividing the major vessels to the colon, including the ileocolic and the middle colic arteries, occasionally there is incomplete hemostasis and bleeding results. Use the intraabdominal hand to grab the base of the pedicle during division. This allows for placement of a vessel loop or repeat cauterization prior to possible retraction of the vessel into the mesentery which can make it difficult to identify and ligate.
The patient is fully tilted to the right and the small bowel is swept to the patient’s right side. The splenic flexure is mobilized bluntly and by using the vessel sealing device to sharply dividethe distal transverse mesocolon and attachments to the greater omentum (Fig. 27.12).
The tip of the spleen and the anterior surface of the kidney are exposed as the suspensory ligaments are divided and the splenic flexure is mobilized medially. This sharp dissection is continued into the lateral attachments and down to the pelvic brim as the colon is retracted medially. Blunt dissection in the avascular plane is used to mobilize the left colon medially and expose the retroperitoneal structures including the tail of the pancreas (Fig. 27.13).
-
Troubleshooting: The splenic flexure may be difficult to visualize and mobilize. Approaching from both the medial and lateral sides can help identify attachments which need to be divided. Retraction of the omentum must be done carefully, as attachments to the spleen can be present and can cause significant bleeding if tears in the splenic capsule result.
The colon is retracted anteriorly, elevating the mesentery which is divided continuing at the edge just past the division of the middle colic vessels and into the descending colon,progressively moving back into Trendelenburg position until the pelvic brim is reached.
We typically preserve the Inferior Mesenteric Artery and its branches to the rectum when this operation is performed for benign disease. In patients with acute colitis, with possible immunosuppression and malnutrition, there is concern for breakdown of the rectal stump staple line. Preserving the Superior Rectal Artery improves perfusion to this segment of bowel. In addition, limiting dissection below the sacral promontory preserves intact pelvic planes for future operations and minimizes injury to the sympathetic nerves.
4.4 Transection
After the specimen is fully mobilized, the GelPort cap is removed and the specimen is delivered through the incision (Fig. 27.14). The terminal ileum is dissected free from its mesentery and divided with an linear cutting stapler. The rectosigmoid junction is dissected from the mesorectum and divided with a linear stapler. The specimen is sent to pathology for permanent section. The specimen should be opened on the back table in oncologic cases to assess for margins. The GelPort and laparoscopic trocars are removed and the pursestring suture is removed from the ostomy site. The terminal ileum is properly oriented and delivered through the previously developed ileostomy site.
-
Troubleshooting: The trocars can be removed under direct visualization through the Pfannenstiel incision to ensure there is no intraabdominal bleeding. The rectosigmoid junction staple line can be oversewn prior to returning it to the abdomen if there is concern for integrity in patients with acute UC and a rectal tube for decompression is used in severely inflammed rectal stumps.
4.5 Closure of Incisions and Creation of Ileostomy
The Pfannenstiel incision is closed in layers. The peritoneum is closed with a running 3-0 Vicryl suture and the fascia is closed using interrupted 0 Vicryl suture. The skin of the Pfannenstiel incision and port sites are closed using running 4-0 Monocryl suture in a subcuticular fashion and sealed with sterile surgical glue.
The incisions are protected with a sterile towel. The staple line is excised and the ileostomy is matured in the standard Brooke fashion using 3-0 chromic interrupted suture (Fig. 27.15). An ostomy appliance is placed around the ileostomy.
5 Postoperative Management
Patients are placed on an Enhanced Recovery After Surgery (ERAS) protocol. Multimodal analgesia is used to decrease opioid use. Scheduled acetaminophen, gabapentin, and celecoxib are given. Tramadol is used for breakthrough pain and low dose ketamine drip is added as needed. Alvimopan is given in opioid-naïve patients until return of bowel function. Patients are offered clear liquids following surgery and given a low residue diet on the first postoperative day. The bladder catheter is removed in the morning on the first postoperative day. The rectal tube is removed on postoperative day 2. Patients are encouraged to use incentive spirometry. Patients are given deep vein thrombosis prophylaxis, SCDs are used, and they are encouraged to ambulate a minimum of 3 times daily. Patients are discharged when they tolerate a diet with adequate ileostomy output, pain is controlled on oral medications, and the patient or family is able to care for the ostomy, typically within 2–3 days.
References
Bohl JL, Sobba K. Indications and options for surgery in ulcerative colitis. Surg Clin North Am. 2015. Dec;95(6):1211–32.
Dunker MS, Bemelman WA, Slors JF, van Hogezand RA, Ringers J, Gouma DJ. Laparoscopic-assisted vs open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): a retrospective study in 42 patients. Surg Endosc. 2000;14(10):911–4.
Marohn MR, Hanly EJ, McKenna KJ, Varin CR. Laparoscopic total abdominal colectomy in the acute setting. J Gastrointest Surg. 2005;9(7):881–7.
Watanabe K, Funayama Y, Fukushima K, Shibata C, Takahashi K, Sasaki I. Hand-assisted laparoscopic vs. open subtotal colectomy for severe ulcerative colitis. Dis Colon Rectum. 2009;52(4):640–5.
Leraas HJ, Ong CT, Sun Z, Adam MA, Kim J, Gilmore BF, Ezekian B, Nag US, Mantyh CR, Migaly J. Hand-assisted laparoscopic colectomy improves perioperative outcomes without increasing operative time compared to the open approach: a national analysis of 8791 patients. J Gastrointest Surg. 2017. Apr;21(4):684–91.
Rivadeneira DE, Marcello PW, Roberts PL, Rusin LC, Murray JJ, Coller JA, Schoetz DJ. Benefits of hand-assisted laparoscopic restorative proctocolectomy: a comparative study. Dis Colon Rectum. 2004. Aug;47(8):1371–6.
Marcello PW, Fleshman JW, Milsom JW, Read TE, Arnell TD, Birnbaum EH, Feingold DL, Lee SW, Mutch MG, Sonoda T, Yan Y, Whelan RL. Hand-assisted Laparoscopic vs laparoscopic colorectal surgery: multicenter, prospective, randomized trial. Dis Colon Rectum. 2008. Jun;51(6):818–26.
Boushey RP, Marcello PW, Martel G, Rusin LC, Roberts PL, Schoetz DJ. Laparoscopic total colectomy: an evolutionary experience. Dis Colon Rectum. 2007. Oct;50(10):1512–9.
Chung TP, Fleshman JW, Birnbaum EH, Hunt SR, Dietz DW, Read T, Mutch MG. Laparoscopic vs open total abdominal colectomy for severe colitis: impact on recovery and subsequent completion restorative proctectomy. Dis Colon Rectum. 2009. Jan;52(1):4–10.
Whaley KG, Rosen MJ. Contemporary medical management of acute severe ulcerative colitis. Inflamm Bowel Dis. 2019;25(1):56–66.
Person B, Ifargan R, Lachter J, Duek SD, Kluger Y, Assalia A. The impact of preoperative stoma site marking on the incidence of complications, quality of life, and patient’s independence. Dis Colon Rectum. 2012;55(7):783–7.
Kiran RP, Murray AC, Chiuzan C, Estrada D, Forde K. Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg. 2015;262(3):416–25.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The authors have no conflict of interest to declare.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Stringfield, S., Fichera, A. (2021). Hand Assisted Total Colectomy. In: Patti, M.G., Zureikat, A.H., Fichera, A., Schlottmann, F. (eds) Techniques in Minimally Invasive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-67940-8_27
Download citation
DOI: https://doi.org/10.1007/978-3-030-67940-8_27
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-67939-2
Online ISBN: 978-3-030-67940-8
eBook Packages: MedicineMedicine (R0)