Abstract
This chapter provides an overview of the available literature examining the effects of renal replacement therapies, particularly dialysis, on the immediate and downstream neurocognitive outcomes in children with end-stage renal disease. Specific goals are to (a) discuss the renal-brain connection, (b) explore potential mechanisms of chronic kidney disease leading to brain dysfunction, (c) summarize known neurocognitive and neurologic findings related to dialysis, and (d) consider possible management strategies for cognitive dysfunction in children affected by ESRD. The available findings indicate the negative impact of dialysis, particularly hemodialysis, on neurocognitive functioning, particularly on intelligence and specific cognitive abilities (e.g., selected executive functions); however, the literature is plagued by small, highly heterogeneous samples, inconsistent neurocognitive measurement, and lack of a consistent protocol with respect to follow-up. The field is ripe for a well-controlled longitudinal study to determine the specific neurocognitive outcomes that are associated with specific forms of dialysis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Pediatric dialysis
- Neurological effects of dialysis
- Cognitive function
- Brain development
- End-stage kidney disease
Introduction
Children and adult survivors of childhood-onset chronic kidney disease (CKD) have a greater frequency of neurodevelopmental and cognitive challenges compared with the general population [1, 2]. The impact of this neurodevelopmental vulnerability persists into adulthood and contributes to clinical manifestations such as a lower intelligence quotient and a lower frequency of postsecondary education compared with the general population [2]. The mechanisms responsible for the brain dysfunction observed with CKD have not been established, although a number of mechanisms have been hypothesized and are discussed below. The goals of this chapter are to explore potential mechanisms leading to brain dysfunction—including renal-brain connections—summarize known neurocognitive and neurologic findings, and consider possible management strategies for neurocognitive dysfunction in children affected by CKD, particularly once they reach end-stage kidney disease (ESKD).
The Interaction of Brain Development, Kidney Disease, and Dialysis
Brain Development
Brain development is quite rapid during early childhood and, subtler but equally as critical, in later childhood and adolescence. Consequently, expectations for developmental attainment and general cognitive performance change as the child ages. The timing of this rapid neurodevelopmental growth places the developing brain at particular risk from injury or disease during infancy and childhood. Dennis et al. [3] and others [4] have suggested that the degree and severity of insult is likely related to when the insult occurs in the neurodevelopmental sequence and the cognitive reserve of the individual. Studies of other childhood chronic health conditions present from birth or shortly thereafter have found delays in language, motor skills, and overall developmental level [5,6,7,8]. In addition, children with early traumatic brain injury have shown deficits in academic achievement, behavior, cognitive, and motor functioning at the time of injury [9, 10], and these deficits persist long past the initial insult [11]. Given the rapid rate of this early neurodevelopmental growth, these deficits may be worse than brain insults obtained in later years [12]. Although there are relatively few studies of the longitudinal impact of CKD in infancy and early childhood , several studies suggest an increased risk of developmental delays in children with early-onset chronic kidney disease (CKD) or end-stage kidney disease (ESKD) [13,14,15] and in children with a longer duration of CKD or dialysis [16,17,18,19]. Further research is needed to improve our understanding of how CKD affects the developing brain and how factors such as age of onset, prematurity, disease severity, duration of disease, and treatment modality moderate immediate and downstream neurocognitive outcomes.
Kidney-Brain Connections
Given the above findings from the available pediatric neurocognitive and neurological literature, there is a clear connection between the kidney and brain. These observations generate key questions: How does kidney dysfunction contribute to brain dysfunction or damage? What do we know about possible mechanisms and how can they affect brain structure, brain function, and brain development?
Potential mechanisms of neurocognitive impairment in CKD include metabolic neuronal toxicity, vascular injury, and endothelial dysfunction, all of which are likely interrelated. At its simplest level, CKD may impact the nervous system by not effectively filtering neurotoxic chemicals and metabolites from the bloodstream, leading to metabolic neuronal injury. This mechanism may be most evident when the individual reaches end-stage kidney disease. Alterations in vascular integrity also may be present secondary to the metabolic changes associated with CKD as well as by its comorbidities such as hypertension, anemia, and dyslipidemia. Vascular injury may be further perpetuated by endothelial dysfunction, mediated by chronic inflammation, hypercoagulability, and oxidative stress [20].
In addition to the potential direct effects of kidney dysfunction on the brain, medical management of CKD and ESKD may affect neurocognitive outcomes. Factors such as malnutrition, aluminum intoxication, and psychosocial deprivation have historically contributed to adverse neurocognitive outcomes in children with CKD [21]. More modern treatment protocols may help to mitigate these effects by optimizing nutrition, reducing aluminum exposure by eliminating aluminum-containing phosphate binders and optimizing dialysis water treatment, and paying greater and more consistent attention to children’s cognitive, educational, and psychosocial needs during medical treatment. Similarly, improved management of anemia in children with ESKD may also buffer the impact of CKD on the nervous system based, in part, on findings in adults with ESKD [22]. Dialysis itself may also contribute to neurocognitive dysfunction in the long term, as discussed further in the next section.
Metabolic Changes in CKD
CKD causes retention of a large number of uremic toxins that differ in their molecular weight, protein binding, and ability to be removed by dialysis [23]. Many of these uremic toxins have known or putative roles in cerebral dysfunction. For example, guanidino compounds, which are known to have pro-convulsant properties [24, 25], have been found in elevated levels in the serum, urine, cerebrospinal fluid, and brain tissue of patients with CKD [26,27,28]. Another pathway known to be altered in CKD is the kynurenine pathway of tryptophan metabolism, which is also implicated in the pathogenesis of various cognitive and neurodegenerative disorders independent of CKD [29]. In one study of adults with stage 4 CKD, higher serum levels of kynurenic acid were associated with lower cognitive functioning, while higher serum levels of indole-3 acetic acid (IAA) were correlated with anxiety and depression [30].
The advent of metabolomic profiling, in which hundreds of compounds can be measured in a single sample, may help to broaden our understanding of the numerous metabolic changes associated with CKD and their relationship to neurocognitive function. In one study of adults on maintenance hemodialysis, metabolic profiling of pre-dialysis plasma samples showed that levels of four metabolites related to phenylalanine, benzoate, and glutamate metabolism were associated with impaired executive function [31].
Imaging methods, such as magnetic resonance spectroscopy (MRS), may also help to deepen our understanding of the relationship between metabolic changes and neurocognitive dysfunction in CKD. For example, in one study of children with stage 1–5 CKD, including children on dialysis, MRS of the brain showed that the intelligence quotient (IQ) correlated negatively with the brain myoinositol/creatine ratio and positively with the N-acetyl aspartate (NAA)/creatine ratio [32]—neurometabolites related to neurotransmission and tissue damage or necrosis, respectively.
Some studies of the effects of dialysis and transplant on neurocognition also support the hypothesis that metabolic changes are at least partially responsible for neurocognitive dysfunction in CKD. In one small study, an electrophysiologic measure of cognitive potential, the P300 latency, was found to be impaired in adults with ESKD and also was found to normalize 3 months after successful kidney transplantation, presumably due to normalization of metabolic processes [33]. In another pilot study, transition of patients from conventional dialysis to nocturnal daily hemodialysis, which improves clearance of uremic toxins, was associated with improved psychomotor efficiency, attention, and working memory [34].
Vascular Integrity
Another potentially strong linkage between kidney disease and brain impairment relates to the vascular integrity in both of these organs. Indeed, there are a number of similarities in the vascular supply to both the brain and kidney, with both being low-resistance end organs that manage high volumes of blood flow. Murray [35] and others have argued for a linkage between the kidney and the brain that is based on a model of accelerated vascular cognitive impairment.
Adults with CKD and ESKD are at much higher risk for cerebrovascular complications than the general population. In the 2006 United States Renal Data System Annual Report, the incidence of stroke was 15.1% in hemodialysis patients and 9.6% in CKD patients, compared to only 2.6% in non-CKD Medicare patients [36]. Preliminary evidence also has begun to show significantly higher rates of stroke, even in children with mild to moderate CKD [37]. Although coexisting risk factors, such as hypertension, diabetes, and dyslipidemia, contribute to stroke risk in many adults with CKD, having a glomerular filtration rate (GFR) of <60 mL/min/1.73m2 has been shown to be independently associated with an increased risk of stroke [38]. Even in adults with CKD, but without a known clinical history of stroke or transient ischemic attacks, magnetic resonance imaging (MRI) studies have revealed a high prevalence of cerebrovascular abnormalities. In a study of more than 1000 adults, Liu et al. [39] found that GFR <60 mL/min/1.73m2 was associated with an increased prevalence of markers of cerebral small vessel disease (e.g., lacunes, white matter hyperintensities, cerebral microbleeds, enlarged perivascular space) in individuals <60 years old, even after adjustment for comorbidities such as hypertension and diabetes. In nondiabetic adults, aged 30–60 years, with stage 3–4 CKD, Martinez-Vea et al. [40] found that 1/3 had silent cerebral white matter lesions, with vascular nephropathy being the strongest independent risk factor for the presence of these lesions. Similarly, Kobayashi et al. [41] found a high prevalence of silent brain infarction (SBI) in adults with CKD, with hypertensive nephrosclerosis showing a strong association with SBI.
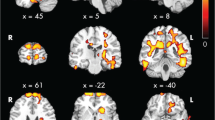
Although the pediatric data are more limited, MRI studies in children with CKD also show evidence of alterations in cerebral vascular integrity. Among children who received a kidney transplant before 5 years of age, Valanne et al. [42] showed a 54% prevalence of ischemic lesions in vascular border zones. Although overt MRI lesions are much less common in children and young adults with milder CKD [43], a study of cerebral blood flow (CBF) using arterial spin-labeled (ASL) MRI showed that individuals aged 8–25 years with CKD had higher global CBF than healthy controls (primarily related to anemia). In addition, white matter CBF was positively correlated with blood pressure in CKD patients but not in healthy controls, suggesting abnormal cerebrovascular autoregulation in individuals with CKD [44]. This study also showed that regional differences of CBF in the precuneus correlated with executive dysfunction. These findings provide some early mechanistic insights into how hypertension, a known risk factor for decreased neurocognitive performance in children both without [45] and with CKD [46, 47], may contribute to neurocognitive dysfunction.
Other factors that may contribute to impaired cerebral vascular integrity and cognitive impairment include hyperhomocysteinemia, oxidative stress, and inflammation. Hyperhomocysteinemia is common in patients with CKD [48] and may contribute to neurocognitive dysfunction both via endothelial pro-inflammatory effects and via its direct effects on the N-methyl-D-aspartate receptor [49, 50]. Oxidative stress, mediated by alterations in endothelial nitric oxide signaling, also has been linked to brain dysfunction in adults with CKD and in experimental models [51, 52].
The Impact of Dialysis on Kidney-Brain Connections
Chronic Dialysis
Although clearance of uremic toxins by dialysis may improve neurocognitive function, chronic dialysis is associated with physiologic changes that may negatively impact brain function. In adults, initiation of hemodialysis (HD) is associated with a higher incidence of dementia-related symptoms when compared to patients initiating peritoneal dialysis (PD), even after adjustment for comorbidities and controlling for factors that influence dialysis modality selection [53]. In a longitudinal study, cognitive function declined faster in adults on dialysis compared to those with CKD, and the decline was faster in patients on HD than patients on PD [54]. Factors contributing to cerebral dysfunction in dialysis may include repeated episodes of cerebral hypoperfusion caused by hypotension and fluid shifts, which can lead to increased risk of brain ischemia and watershed infarcts. In a study using positron emission tomography-computed tomography (PET-CT) in older adults on hemodialysis, global CBF was found to decline significantly during HD (mean decline of 10 ± 15%), and the degree of CBF decline was associated with higher ultrafiltration (UF) volume and UF rate [55]. Although HD is associated with greater degrees of hemodynamic changes compared to PD, the risk of stroke has been shown to increase in older adults within 30 days of initiating either dialysis modality [56], suggesting that cerebral hypoperfusion can occur with both HD and PD.
Even in stable chronic dialysis patients, HD has been shown to be associated with short-term changes in cognitive performance. In studies of adult patients receiving HD, Costa et al. [57] and Dasgupta et al. [58] demonstrated deterioration of cognitive function when comparing performance before HD versus immediately after HD. Murray et al. [59] showed that global cognitive function in adults varies during a dialysis cycle, with worse performance during the HD session and best performance either shortly before or on the day after the session.
As discussed in more detail in the next sections, multiple studies in children receiving chronic dialysis have shown impaired neurocognitive performance in various domains [60,61,62,63,64,65,66,67,68]. However, there is very little literature examining the extent to which dialysis-related physiologic changes contribute to neurocognitive impairment in children. In their study of children who received a kidney transplant before age 5 years, Valanne et al. [42] described three patients who had marked widening of the cortical and central cerebrospinal fluid spaces on CT scans performed while receiving chronic dialysis; importantly, it was reported that these abnormalities resolved on posttransplant MRI (Fig. 34.1). They postulated that this reversible “pseudoatrophy” was a result of reversible contraction of brain tissue caused by factors such as fluid/electrolyte shifts, hypoalbuminemia, or medications [42]. However, more definitive physiologic studies of the effects of dialysis on the pediatric brain are needed.
This CT scan presents reversible “pseudoatrophy” in a patient on dialysis. (a) shows the presence of larger and misshapen lateral ventricles as well as widening of the subarachnoid spaces in frontal brain regions during dialysis. (b) shows an apparent resolution of these abnormalities in the same patient several years posttransplant. (Reprinted with permission from Wiley & Sons)
Acute Dialysis
Dialysis disequilibrium syndrome can arise acutely during or immediately after a dialysis session, most commonly in patients receiving their first HD treatment [69]. Symptoms of dialysis disequilibrium can include headache, confusion, nausea, restlessness, and coma. These symptoms are primarily related to cerebral edema and increased intracranial pressure caused by osmotic movement of water into the brain.
There are two hypotheses for the mechanisms responsible for an osmotic gradient between the blood and the brain, namely, the “reverse urea” hypothesis and the “idiogenic osmoles” hypothesis [70]. The “reverse urea” effect is thought to occur because rapid removal of blood urea by dialysis leads to a blood-brain urea gradient, causing osmotic movement of water into the brain [71]. The “idiogenic osmoles” hypothesis arose from animal experiments in which rapid HD was associated with significantly higher brain tissue osmolality compared to the blood, which could not be fully explained by changes in electrolyte or urea concentrations [72]. This led the authors to conclude that the increased brain osmolality was caused by the new formation of organic molecules; however, a subsequent study of rapid HD in another animal model could not confirm the presence of “idiogenic osmoles” [73].
Regardless of the underlying mechanism, the primary method to prevent dialysis disequilibrium is to lower the blood urea concentration slowly, either via slow continuous HD or hemofiltration or by targeting lower urea reduction ratios [69]. Another approach to mitigate dialysis disequilibrium, and perhaps associated neurocognitive impairment, includes increasing blood osmolality by increasing dialysate sodium concentration [74] or by infusing mannitol [75].
Neurocognitive Functioning and Neuroimaging in Pediatric Dialysis
Neurocognitive Functioning in Pediatric Dialysis
Over the past 5 decades, the cognitive function of small cohorts of children receiving various forms of renal replacement therapy (RRT) has been evaluated. Although informative, results from investigations conducted prior to 1990 were likely significantly influenced by uncontrolled anemia, aluminum exposure, and potentially less stringent nutritional, dialytic, and transplantation services compared with present-day management. Despite the improvement in these treatments [76], even more contemporary findings continue to be plagued by small sample sizes, samples that combined multiple forms of treatments and associated treatment protocols without differentiation, and samples that combine patients with wide age ranges. Further, there is little consistency across the neurocognitive measures used so as to compare one study to the next. These are not research oversights by investigators in the dialysis literature, but rather the result of the challenges of subject ascertainment and the medical needs of the children. A summary of the findings from the available contemporary studies over the past three decades is provided in Table 34.1.
Early studies and overviews of the CKD literature indicated significant concerns for several developmental delays—including gross motor and language functions and other neurological problems (e.g., microcephaly) in both dialyzed and non-dialyzed infants with severe CKD and ESKD [79, 80]. As can be seen in Table 34.1, infants and very young children on dialysis show developmental delays and significantly lower IQ scores compared to healthy children [60,61,62,63,64]. With respect to overall developmental functioning, many children on dialysis have been reported to be in the intellectual disability range. For older children and adolescents, a similar pattern of findings has been present, with overall intellectual functioning being approximately 9–11 points lower than controls [65]. Further, older children and adolescents also have had evidence of poorer abilities in their gross motor, fine-motor coordination, visuomotor skills, short-term memory, verbal abilities, and attention [66,67,68, 81]. More specifically, memory impairments are particularly noteworthy relative to the healthy control populations, and this impairment is greatest with dialysis-dependent ESKD [68].
A variety of executive function problems also have been reported, with particular concerns noted for problems in working memory, initiation, and sustaining capabilities [68]. Significant problems also have been reported in academic achievement across reading, spelling, and math areas, increased school absences, more frequent grade retentions, and the presence of formal learning disabilities [82, 83]. Unfortunately, we have a paucity of information regarding the impact of CKD and dialysis on specific language functions, overall motor skills, and adaptive behavior in children.
In contrast, several studies have not uncovered significant differences between children with ESKD and controls in the areas of memory, selected executive functions, academic achievement, or self-assessment of health-related quality of life [65, 66, 68, 84]. Furthermore, follow-up studies of children who have received kidney transplants, typically following some time on dialysis, generally have shown relative improvements in overall cognitive functioning. For instance, attention appears to be most severely affected with dialysis-dependent ESKD but reportedly improves after transplantation [15, 21, 81]. Qvist et al. [85] reported low average to average IQ in school-age children who received transplants before age 5 years, with as many as a quarter of the children continuing to show some type of neurocognitive impairment several years posttransplant. Improvements in both verbal and nonverbal IQ have been consistently reported following kidney transplantation [60, 86,87,88], with about a 10–12-point improvement in IQ being demonstrated at least one month or more posttransplant. Significant improvements also have been observed in processing speed, reaction time, and working memory [81]. Nevertheless, having ESKD in childhood does not appear to bode well for individuals as they move into older childhood or adulthood, with findings suggesting lower verbal and nonverbal intellectual capacities [2], lower academic achievement, and the presence of metacognitive executive dysfunctions [15]. Shorter duration of dialysis in childhood and older age at the time of renal replacement therapies—including transplant—also have been related to better outcomes [2, 15, 89].
Neuroimaging Findings in Pediatric Dialysis
In addition to neurocognitive function , the impact of CKD has been demonstrated in various neuroimaging and electroencephalographic (EEG) procedures, as noted above. From the approximately 15 or so neuroimaging studies that have been conducted to date, structural analyses via magnetic resonance imaging (MRI) and computerized tomography (CT) have documented the presence of a variety of anomalies including chronic infarct lesions, ischemic watershed zone white matter lesions, early signs of cerebral vascular disease as demarcated by deep white matter hyperintensities and white matter lesions, and cerebral atrophy [90]; however, virtually none of the childhood studies have isolated children on dialysis, or various forms of dialysis, in their descriptions, with the work by Valanne et al. [42] being the one exception thus far.
Electrical conduction dysfunction has also been reported, with EEG abnormalities being reported in 42% of a pediatric cohort with CKD from infancy, and it has been associated with poorer kidney function and severity of anemia in adults [21, 42, 91]. Hurkx et al. [92] found no differences in auditory pathway nerve conduction between children with CKD and children undergoing PD. For the entire combined sample, high inter-peak latencies were found in the somatosensory cortex and were attributed to decreased cortical conduction via the thalamus. Brainstem conduction was normal for the combined group, with no differences noted between those with CKD and those receiving PD; however, delayed conduction was noted in the thalamocortical region for children less than 30 months of age for the combined sample, perhaps being secondary to delayed myelination in very young children with CKD. In addition to specific conduction abnormalities, children with CKD may be at risk for generalized conduction abnormalities which manifest as a seizure disorder as reported in 0% to 20% of children with CKD [92, 93]. The application of these findings to children receiving dialysis, though, remains unknown at present.
Management of Cognitive Dysfunction in Children on Dialysis
Given the chronic nature of ESKD and its associated neurodevelopmental challenges, it is likely that children and adolescents with ESKD are in need of a variety of management strategies. This is true regardless of their treatment modality. There are various medical complications that many of these children experience that interfere with day-to-day functioning (e.g., school absences, medication compliance issues, etc.), and they likely will experience frequent challenges in the school and preschool settings secondary to their cognitive dysfunction and kidney-related medical complications. For example, there are high rates of low birth weight and prematurity in the CKD population, with rates as high as 18%, and these factors can influence brain development and associated cognitive functioning along with the kidney disease. Similarly, there are concomitant high rates of seizure disorders in children with kidney disease, with these rates ranging from approximately 7% to 18% for children on dialysis [85, 94], particularly those receiving HD [95]. These rates increase during dialysis to 29% for children who have had a prior history of seizures. Further, with respect to the presence of seizures pre-dialysis or the manifestations of seizures during dialysis, it is important for the pediatric nephrologist to understand potential adjustments to the anticonvulsant medications that might be required, particularly during the dialysis process, so as to lessen the chance of seizure occurrence [96]. Taken together with these (and other) medical management strategies, the management of the cognitive dysfunction in pediatric ESKD also requires significant attention by the pediatric nephrologist and the interdisciplinary health-care team.
Although there are no evidence-based educational management strategies or interventions explicitly linked to CKD, there are a number of empirically based interventions that have a demonstrated track record in working with children with learning and developmental difficulties. In addition to the necessary medical interventions detailed across many of the chapters in this text, management of the neurodevelopmental challenges also should be considered and implemented via a developmental framework; that is, these should be considered with the developmental level of the child in mind for their most efficacious applicability to a pediatric dialysis population, and they should be discussed routinely with the family by the interdisciplinary team of professionals caring for the child [97].
Early Intervention
The infant , toddler, and preschool periods of development are critical to the growth of the child. This time period, encompassing birth to approximately 5 years of age, is a remarkable time of development. It is the time when gross motor skills evolve into crawling, walking, running, jumping, and skipping. It is also the time when fine-motor skills evolve into grasping a snack with the rake of a hand to scribbling with a crayon to eventual adaptive skills and other important functions such as dressing and writing. This time period is critical in terms of the ongoing development of cognitive abilities, pre-academic skills, and increasingly complex social interactions [98]. As such, these first 5 years of life are at least as important as any other 5-year span in an individual’s life and perhaps can influence outcomes across the life span [13, 99].
The quality of neurodevelopmental outcomes also may be dependent on the type and quality of the early intervention services that they receive. The accumulating evidence suggests that the results of early efforts to remediate or attenuate a child’s deficits can be successful. Although more evidence exists to support the benefits of early intervention for children at environmental risk [98], research that supports services for young children with biological impairments, such as those receiving dialysis, is also growing. For example, Black et al. [100] examined the influence of home visiting on infants with failure to thrive syndrome using a standardized home intervention curriculum that focused on maternal sensitivity, parent-infant relationships , and child development. This group was compared with a group of typical infants and with a group of other infants with failure to thrive who did not receive home intervention, but were seen in a medical clinic for routine care. At 8-year follow-up, children in the typical growth group were taller and heavier and had better arithmetic scores than the clinic-only group. The home intervention group had intermediate results. There were no group differences in IQ, reading, or mother-reported behavior problems; however, children in the home intervention group had fewer teacher-reported problems and better work habits than the clinic-only group. How such a program would impact the developmental trajectory of young children with ESKD receiving dialysis remains to be determined; however, such an intervention may be quite applicable to the young dialysis population.
Additionally, it is important to note that there are a number of early intervention programs designed to improve specific developmental areas, such as motor functions, language abilities, and social-emotional skills in the early years [98]. It is suspected that young children with ESKD will respond positively to these types of early intervention approaches and programs. In the meantime, it will be important for pediatric nephrologists to be aware of such programs in their communities, or at least the early intervention programs and professionals, so as to work with their families and local developmental experts in providing the early intervention services that might be necessary for the preschool child with ESKD and receiving dialysis.
School Age
Despite many medical advances in pediatric nephrology, children with CKD are at risk for school-based challenges and failures. Further investigation is needed to potentially improve academic outcomes for this population through hospital-based intervention and special education planning. Although high rates of neurocognitive impairment have been reported, observational studies of school placements have revealed that most children with CKD attend regular education settings with or without special education and that their overall achievement skills are not overly impaired [101]. However, children with ESKD do show increased rates of school difficulties across all subject areas, and they experience increase rates of school absenteeism and grade retentions as shown in Table 34.1. Additional research is needed to better understand the special education and general learning needs of children with ESKD. There are, however, a variety of evidence-based instructional strategies that are likely applicable to children with ESKD.
Specifically, the interventions that have been developed for various aspects of reading have a clear scientific foundation with numerous studies demonstrating their effectiveness for children with reading disorders. For example, there is a preponderance of evidence to indicate the importance of explicit instruction in the alphabetic principle and phonological processing as critical components to reading intervention for children with reading recognition problems. Indeed, the National Reading Panel [102] showed the effects to be large in magnitude. Similarly, repeated reading interventions have been shown to improve reading fluency [103], and the development and use of strategies have been employed to improve reading comprehension [104]. Similar efforts have shown positive outcomes in the areas of mathematics [105] and written language [106, 107]. Another area that has evolved for children with various neurological and neurodevelopmental disorders is cognitive rehabilitation therapy; however, such computer-based treatments have not been applied to children with CKD or ESKD. The presence of neurocognitive difficulties in this population of children raises the potential for the use of these computer-based treatment strategies, particularly with respect to their applicability to the home , school, and clinic settings [108].
Adolescence and Adult Transition
In addition to many of the treatments available for school-age children, adolescents with ESKD face many barriers during their transition to early adulthood. The transition to adulthood is an important period in human development that requires an individual to increase his/her level of autonomy, find gainful employment, and build social relationships. Childhood-onset CKD/ESKD and the associated medical complications can prevent many adolescents from making this transition and facing these developmental challenges successfully [109]. Improvement of the current survival rates for adolescents with ESKD of 80% at 10 years must be coupled with successful transition expectations [110, 111].
To date, intervention research geared toward the medical and psychosocial barriers that impede transition to adulthood is in development, and intervention research geared toward understanding the cognitive barriers to transition remains nonexistent. Over 8 years ago, Bell et al. [112] noted the importance of the possible interaction between cognitive functioning and successful health-care transition for adolescents and emerging adults with end-stage kidney disease. They asserted the importance of the cognitive/developmental level of the patient as a key factor in successful transition, along with a host of other factors including available health resources, family functioning, and the need for family education about the challenges of health-care transition. Further, Bell et al. discussed the importance of collaboration and clear communication between the pediatric and adult health-care teams in the transition process, and this will be especially important for the adult nephrologist assuming the care of an emerging young adult receiving dialysis.
In spite of minimal response-to-intervention research within this population, several possibilities exist that might prove instrumental in smoothing the transition for adolescents with ESKD. In addition to the special education issues noted above, Icard et al. [113] examined specific transition issues including vocational rehabilitation services and mental health needs and stressed the need for the development of evidence-based transition programs that would facilitate the movement from late adolescence into adulthood [110]. The issue of medical transition also is critical to this population, particularly given the importance of medication adherence [114] and the treatment of the associated medical needs that will continue into adulthood.
Conclusions and Directions
This chapter outlined the neurodevelopmental challenges of children with ESKD, with a particular focus on the effects of dialysis on the brain. While it appears that nearly every neurocognitive function can be affected by ESKD and dialysis, the literature is compromised by a variety of methodological issues including small sample sizes, samples of convenience, highly heterogeneous samples (e.g., wide age ranges, different ages of treatment), heterogeneous treatments, and lack of consistency of measurement across studies [77]. Future studies clearly need to address these methodological issues in order to provide a clearer picture of the neurocognitive outcomes in children receiving dialysis.
Despite these methodological problems, it does appear that children receiving dialysis demonstrated significantly lower IQ when compared to controls, and they show a variety of other neurocognitive and learning difficulties as well. Children receiving hemodialysis may be at particular risk for showing neurocognitive impairments and higher rates of seizures, although this will require additional study, especially the possibility that there could be improvement posttransplant. Findings from the available literature also suggest that shorter durations of dialysis and early kidney transplant hold potential for lessening the degree of neurocognitive impairments. The application of developmentally appropriate interventions to optimize their cognitive trajectory and opportunities for independence as adults also is important, particularly as children move closer to ESKD and the possibility of renal replacement therapies. At a minimum, utilization of a multidisciplinary or interdisciplinary team model would be important to assist in managing the shifting developmental needs of the individual with ESKD and his/her family from a life course perspective, with ongoing neurodevelopmental surveillance being a critical component of that approach. Using a multidisciplinary and scientifically rigorous approach, we anticipate the coming decade to provide opportunities to progress from quantifying the developmental challenges to identifying the underlying mechanisms and associated evidence-based interventions for the cognitive dysfunction demonstrated in children requiring dialysis and other renal replacement therapies.
References
Gipson DS, Duquette PJ, Icard PF, Hooper SR. The central nervous system in childhood chronic kidney disease. Pediatr Nephrol. 2007;22:1703–10.
Groothoff JW, Grootenhuis M, Dommerholt A, Gruppen MP, Offringa M, Heymans HS. Impaired cognition and schooling in adults with end stage renal disease since childhood. Arch Dis Child. 2002;87:380–5.
Dennis M, Spiegler BJ, Juranek JJ, Bigler ED, Snead OC, Fletcher JM. Age, plasticity, and homeostasis in childhood brain disorders. Neurosci Biobehav Rev. 2013;37(10 Pt 2):2760–73.
Moser JJ, Veale PM, McAllister DL, Archer DP. A systematic review and quantitative analysis of neurocognitive outcomes in children with four chronic illnesses. Pediatr Anesth. 2013;23:1084–96.
Antonini TN, Dreyer WJ, Caudle SE. Neurodevelopmental functioning in children being evaluated for heart transplant prior to 2 years of age. Child Neuropsychol. 2018;24(1):46–60.
Hogan AM, Kirkham FJ, Prengler M, Telfer P, Lane R, Vargha-Khadem F, et al. An exploratory study of physiological correlates of neurodevelopmental delay in infants with sickle cell anaemia. Br J Haematol. 2006;132(1):99–107.
Caudle SE, Katzenstein JM, Karpen S, McLin V. Developmental assessment of infants with biliary atresia. J Pediatr Gastroenterol Nutr. 2012;55(4):384–9.
Compas BE, Jaser SS, Reeslund K, Patel N, Yarboi J. Neurocognitive deficits in children with chronic health conditions. Am Psychol. 2017;72(4):326–38.
Keenan HT, Hooper SR, Wetherington CE, Nocera M, Runyan DK. Neurodevelopmental consequences of early traumatic brain injury in 3-year-old children. Pediatrics. 2007;119(3):e616–23.
Gagner C, Landry-Roy C, Bernier A, Gravel J, Beauchamp MH. Behavioral consequences of mild traumatic brain injury in preschoolers. Psychol Med. 2018;48(09):1551–9.
Garcia D, Hungerford GM, Bagner DM. Topical review: negative behavioral and cognitive outcomes following traumatic brain injury in early childhood. J Pediatr Psychol. 2015;40(4):391–7.
Anderson VA, Spencer-Smith MM, Coleman L, Anderson PJ, Greenham M, Jacobs R, et al. Predicting neurocognitive and behavioural outcome after early brain insult. Dev Med Child Neurol. 2014;56(4):329–36.
Geary DF, Haka-Ikse K. Neurodevelopmental progress of young children with chronic renal disease. Pediatrics. 1989;84(1):68–72.
Hooper SR, Gerson AC, Johnson RJ, Mendley SR, Shinnar S, Lande MB, et al. Neurocognitive, social-behavioral, and adaptive functioning in preschool children with mild to moderate kidney disease. J Dev Behav Pediatr. 2016;37(3):231–8.
Johnson RJ, Warady BA. Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol. 2013;28(8):1283–91.
Mendley SR, Matheson MB, Shinnar S, Lande MB, Gerson AC, Butler RW, et al. Duration of chronic kidney disease reduces attention and executive function in pediatric patients. Kidney Int. 2014;87(4):800–6.
Slickers J, Duquette P, Hooper S, Gipson D. Clinical predictors of neurocognitive deficits in children with chronic kidney disease. Pediatr Nephrol. 2007;22(4):565–72.
Molnar-Varga M, Novak M, Szabo AJ, Kelen K, Streja E, Remport A, et al. Neurocognitive functions of pediatric kidney transplant recipients. Pediatr Nephrol. 2016;31(9):1531–8.
Hartmann H, Hawellek N, Wedekin M, Vogel C, Das AM, Balonwu K, et al. Early kidney transplantation improves neurocognitive outcome in patients with severe congenital chronic kidney disease. Transpl Int. 2015;28:429–36.
Bugnicourt J-M, Godefroy O, Chillon J-M, Choukroun G, Massy ZA. Cognitive disorders and dementia in CKD: the neglected kidney-brain axis. J Am Soc Nephrol. 2013;24:353–63.
Elzouki A, Carroll J, Butinar D, Moosa A. Improved neurological outcome in children with chronic renal disease from infancy. Pediatr Nephrol. 1994;8(2):205–10.
Pickett JL, Theberge DC, Brown WS, Schweitzer SU, Nissenson AR. Normalizing hematocrit in dialysis patients improves brain function. Am J Kidney Dis. 1999;33:1122–30.
Watanabe K, Watanabe T, Nakayama M. Cerebro-renal interactions: impact of uremic toxins on cognitive function. Neurotoxicology. 2014;44:184–93.
D’Hooge R, Pei YQ, Marescau B, De Deyn PP. Convulsive action and toxicity of uremic guanidino compounds: behavioral assessment and relation to brain concentration in adult mice. J Neurol Sci. 1992;112(1–2):96–105.
De Deyn PP, Vanholder R, Eloot S, Glorieux G. Guanidino compounds as uremic (neuro) toxins. Semin Dial. 2009;22(4):340–5.
Marescau B, Nagels G, Possemiers I, De Broe ME, Becaus I, Billiouw JM, et al. Guanidino compounds in serum and urine of nondialyzed patients with chronic renal insufficiency. Metabolism. 1997;46(9):1024–31.
De Deyn PP, Marescau B, Cuykens JJ, Van Gorp L, Lowenthal A, De Potter WP. Guanidino compounds in serum and cerebrospinal fluid of non-dialyzed patients with renal insufficiency. Clin Chim Acta. 1987;167(1):81–8.
De Deyn PP, Marescau B, D’Hooge R, Possemiers I, Nagler J, Mahler C. Guanidino compound levels in brain regions of non-dialyzed uremic patients. Neurochem Int. 1995;27:227–37.
Schwarcz R, Stone TW. The kynurenine pathway and the brain: challenges, controversies and promises. Neuropharmacology. 2017;112(Pt B):237–47.
Karu N, McKercher C, Nichols DS, Davies N, Shellie RA, Hilder EF, et al. Tryptophan metabolism, its relation to inflammation and stress markers and association with psychological and cognitive functioning: Tasmanian Chronic Kidney Disease pilot study. BMC Nephrol. 2016;17(1):171.
Kurella Tamura M, Chertow GM, Depner TA, Nissenson AR, Schiller B, Mehta RL, et al. Metabolic profiling of impaired cognitive function in patients receiving dialysis. J Am Soc Nephrol. 2016;27(12):3780–7.
Youssef DM, Mohamed AH, Kamel Attia WM, Mohammad FF, El Fatah NRA, Elshal AS. Cerebral metabolic alterations and cognitive dysfunction in children with chronic kidney disease using Magnetic Resonance Spectroscopy and Wechsler intelligence scale. Nephrology (Carlton). 2017;23(8):771–7.
Chhabra YK, Sood S, Rathi O, Mahajan S. Effect of renal transplantation on cognitive function in hemodialysis patients: a longitudinal study. Int Urol Nephrol. 2017;49(11):2071–8.
Jassal SV, Devins GM, Chan CT, Bozanovic R, Rourke S. Improvements in cognition in patients converting from thrice weekly hemodialysis to nocturnal hemodialysis: a longitudinal pilot study. Kidney Int. 2006;70(5):956–62.
Murray AM. The brain and the kidney connection: a model of accelerated vascular cognitive impairment. Neurology. 2009;73(12):916–7.
United States Renal Data System 2006 Annual Report. Morbidity & mortality. Neuroepidemiology: incident & prevalent stroke [Internet]. https://www.usrds.org/2006/pdf/06_morb_morte_06.pdf.
Kupferman JC, Matheson MB, Lande MB, Flynn JT, Furth S, Warady BA, Hooper SR. Increased history of ischemic stroke and decreased neurocognitive performance in children with chronic kidney disease. Pediatr Nephrol. 2020;35(7):1315−1321.
Lee M, Saver JL, Chang K-H, Liao H-W, Chang S-C, Ovbiagele B. Low glomerular filtration rate and risk of stroke: meta-analysis. BMJ. 2010;341(sep30 1):c4249.
Liu B, Lau KK, Li L, Lovelock C, Liu M, Kuker W, et al. Age-specific associations of renal impairment with magnetic resonance imaging markers of cerebral small vessel disease in transient ischemic attack and stroke. Stroke. 2018;49(4):899–904.
Martinez-Vea A, Salvadó E, Bardají A, Gutierrez C, Ramos A, García C, et al. Silent cerebral white matter lesions and their relationship with vascular risk factors in middle-aged predialysis patients with CKD. Am J Kidney Dis. 2006;47(2):241–50.
Kobayashi M, Hirawa N, Yatsu K, Kobayashi Y, Yamamoto Y, Saka S, et al. Relationship between silent brain infarction and chronic kidney disease. Nephrol Dial Transplant. 2009;24(1):201–7.
Valanne L, Qvist E, Jalanko H, Holmberg C, Pihko H. Neuroradiologic findings in children with renal transplantation under 5 years of age. Pediatr Transplant. 2004;8(1):44–51.
Hartung EA, Erus G, Jawad AF, Laney N, Doshi JJ, Hooper SR, et al. Brain magnetic resonance imaging findings in children and young adults with CKD. Am J Kidney Dis. 2018;72(3):349–59.
Liu H-S, Hartung EA, Jawad AF, Ware JB, Laney N, Port AM, et al. Regional cerebral blood flow in children and young adults with chronic kidney disease. Radiology. 2018;288(3):849–58.
Lande MB, Kupferman JC, Adams HR. Neurocognitive alterations in hypertensive children and adolescents. J Clin Hypertens (Greenwich). 2012;14(6):353–9.
Lande MB, Gerson AC, Hooper SR, Cox C, Matheson M, Mendley SR, et al. Casual blood pressure and neurocognitive function in children with chronic kidney disease: a report of the children with chronic kidney disease cohort study. Clin J Am Soc Nephrol. 2011;6:1831–7.
Ruebner RL, Laney N, Kim JY, Hartung EA, Hooper SR, Radcliffe J, et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am J Kidney Dis. 2016;67:567–75.
Cianciolo G, De Pascalis A, Di Lullo L, Ronco C, Zannini C, La Manna G. Folic acid and homocysteine in chronic kidney disease and cardiovascular disease progression: which comes first? Cardiorenal Med. 2017;7(4):255–66.
Bertsch T, Mielke O, Höly S, Zimmer W, Casarin W, Aufenanger J, et al. Homocysteine in cerebrovascular disease: an independent risk factor for subcortical vascular encephalopathy. Clin Chem Lab Med. 2001;39(8):721–4.
Lipton SA, Kim WK, Choi YB, Kumar S, D’Emilia DM, Rayudu PV, et al. Neurotoxicity associated with dual actions of homocysteine at the N-methyl-D-aspartate receptor. Proc Natl Acad Sci U S A. 1997;94(11):5923–8.
Kielstein H, Suntharalingam M, Perthel R, Song R, Schneider SM, Martens-Lobenhoffer J, et al. Role of the endogenous nitric oxide inhibitor asymmetric dimethylarginine (ADMA) and brain-derived neurotrophic factor (BDNF) in depression and behavioural changes: clinical and preclinical data in chronic kidney disease. Nephrol Dial Transplant. 2015;30(10):1699–705.
Askari H, Abazari MF, Ghoraeian P, Torabinejad S, Nouri Aleagha M, Mirfallah Nassiri R, et al. Ameliorative effects of hydrogen sulfide (NaHS) on chronic kidney disease-induced brain dysfunction in rats: implication on role of nitric oxide (NO) signaling. Metab Brain Dis. 2018;33(6):1945–54.
Wolfgram DF, Szabo A, Murray AM, Whittle J. Risk of dementia in peritoneal dialysis patients compared with hemodialysis patients. Perit Dial Int. 2015;35(2):189–98.
Iyasere O, Okai D, Brown E. Cognitive function and advanced kidney disease: longitudinal trends and impact on decision-making. Clin Kidney J. 2017;10(1):sfw128.
Polinder-Bos HA, García DV, Kuipers J, Elting JWJ, Aries MJH, Krijnen WP, et al. Hemodialysis induces an acute decline in cerebral blood flow in elderly patients. J Am Soc Nephrol. 2018;29(4):1317–25.
Murray AM, Seliger S, Lakshminarayan K, Herzog CA, Solid CA. Incidence of stroke before and after dialysis initiation in older patients. J Am Soc Nephrol. 2013;24:1166–73.
Costa AS, Tiffin-Richards FE, Holschbach B, Frank RD, Vassiliadou A, Krüger T, et al. Clinical predictors of individual cognitive fluctuations in patients undergoing hemodialysis. Am J Kidney Dis. 2014;64(3):434–42.
Dasgupta I, Patel M, Mohammed N, Baharani J, Subramanian T, Thomas GN, et al. Cognitive function declines significantly during haemodialysis in a majority of patients: a call for further research. Blood Purif. 2018;45(4):347–55.
Murray AM, Pederson SL, Tupper DE, Hochhalter AK, Miller WA, Li Q, et al. Acute variation in cognitive function in hemodialysis patients: a cohort study with repeated measures. Am J Kidney Dis. 2007;50(2):270–8.
Davis ID, Chang PN, Nevins TE. Successful renal transplantation accelerates development in young uremic children. Pediatrics. 1990;86:594–600.
Hulstijn-Dirkmaat GM, Damhuis IH, Jetten ML, Koster AM, Schroder CH. The cognitive development of pre-school children treated for chronic renal failure. Pediatr Nephrol. 1995;9:464–9.
Ledermann SE, Scanes ME, Fernando ON, Duffy PG, Madden SJ, Trompeter RS. Long-term outcome of peritoneal dialysis in infants. J Pediatr. 2000;136:24–9.
Madden SJ, Ledermann SE, Guerrero-Blanco M, Bruce M, Trompeter RS. Cognitive and psychosocial outcome of infants dialyzed in infancy. Child Care Health Dev. 2003;29(1):55–61.
Warady BA, Belden B, Kohaut E. Neurodevelopmental outcome of children initiating peritoneal dialysis in early infancy. Pediatr Nephrol. 1999;13:759–65.
Bawden HN, Acott P, Carter J, Lirenman D, MacDonald GW, McAllister M, McDonnell MC, Shea S, Crocker J. Neuropsychological functioning in end-stage renal disease. Arch Dis Child. 2004;89:644–7.
Eijsermans RM, Creemers DG, Helders PJ, Schroder CH. Motor performance, exercise tolerance, and health-related quality of life in children on dialysis. Pediatr Nephrol. 2004;19:1262–6.
Fennell RS, Fennell EB, Carter RL, Mings EL, Klausner AB, Hurst JR. Association between renal function and cognition in childhood chronic renal failure. Pediatr Nephrol. 1990;4:16–20.
Gipson DS, Hooper SR, Duquette PJ, Wetherington CE, Stellwagen KK, Jenkins TL, Ferris ME. Memory and executive functions in pediatric chronic kidney disease. Child Neuropsychol. 2006;12:391–405.
Zepeda-Orozco D, Quigley R. Dialysis disequilibrium syndrome. Pediatr Nephrol. 2012;27(12):2205–11.
Silver SM, Sterns RH, Halperin ML. Brain swelling after dialysis: old urea or new osmoles? Am J Kidney Dis. 1996;28(1):1–13.
Silver SM, DeSimone JA, Smith DA, Sterns RH. Dialysis disequilibrium syndrome (DDS) in the rat: role of the “reverse urea effect”. Kidney Int. 1992;42(1):161–6.
Arieff AI, Massry SG, Barrientos A, Kleeman CR. Brain water and electrolyte metabolism in uremia: effects of slow and rapid hemodialysis. Kidney Int. 1973;4(3):177–87.
Silver SM. Cerebral edema after rapid dialysis is not caused by an increase in brain organic osmolytes. J Am Soc Nephrol. 1995;6(6):1600–6.
Port FK, Johnson WJ, Klass DW. Prevention of dialysis disequilibrium syndrome by use of high sodium concentration in the dialysate. Kidney Int. 1973;3(5):327–33.
Rodrigo F, Shideman J, McHugh R, Buselmeier T, Kjellstrand C. Osmolality changes during hemodialysis. Natural history, clinical correlations, and influence of dialysate glucose and intravenous mannitol. Ann Intern Med. 1977;86(5):554–61.
Rees L, Schaefer F, Schmitt CP, Shraff R, Warady BA. Chronic dialysis in children and adolescents: challenges and outcomes. Lancet Child Adolesc Health. 2017;1:68–77.
Moodalbail DG, Hooper SR. Neurocognitive functioning in children undergoing dialysis. In: Nissenson AR, Fine RN, editors. Handbook of dialysis therapy. 5th ed. Philadelphia: Elsevier; 2017. p. 955–64.
Gipson DS, Hooper SR. Neurocognitive complications and management in pediatric kidney disease. In: Warady BA, Schaefer F, Alexander SR, editors. Pediatric dialysis. 2nd ed. New York: Springer; 2012.
Polinsky MS, Kaiser BA, Stover JB, Frankenfield M, Baluarte HJ. Neurologic development of children with severe chronic renal failure from infancy. Pediatr Nephrol. 1987;1:157–65.
Rotundo A, Nevins TE, Lipton M, Lockman LA, Mauer SM, Michael AF. Progressive encephalopathy in children with chronic renal insufficiency in infancy. Kidney Int. 1982;21:486–91.
Mendley SR, Zelko FA. Improvement in specific aspects of neurocognitive performance in children after renal transplantation. Kidney Int. 1999;56:318–23.
Brouhard BH, Donaldson LA, Lawry KW, McGowan KR, Drotar D, Davis I, Rose S, Cohn RA, Tejani A. Cognitive functioning in children on dialysis and post-transplantation. Pediatr Transplant. 2000;4:261–7.
Duquette PJ, Hooper SR, Wetherington CE, Icard PF, Gipson DS. Brief report: intellectual and academic functioning in pediatric chronic kidney disease. J Pediatr Psychol. 2007;32:1011–7.
Crocker JFS, Acott PD, Carter JEJ, Lirenman DS, MacDonald GW, McAllister M, McDonnell MC, Shea S, Bawden HN. Neuropsychological outcome in children with acquired or congenital renal disease. Pediatr Nephrol. 2002;17:908–12.
Qvist E, Pihko H, Fagerudd P, Valanne L, Lamminranta S, Karikoski J, Sainio K, Ronnholm K, Jalanko H, Holmberg C. Neurodevelopmental outcome in high-risk patients after renal transplantation in early childhood. Pediatr Transplant. 2002;6:53–62.
Falger J, Latal B, Landolt MA, Lehmann P, Neuhaus TJ, Laube GF. Outcome after renal transplantation. Part I: intellectual and motor performance. Pediatr Nephrol. 2008;23:1339–45.
Icard P, Hooper SR, Gipson DS, Ferris ME. Cognitive improvement in children with CKD after transplant. Pediatr Transplant. 2010;14:887–90.
Rasbury WC, Fennell RS, Fennell EB, Morris MK. Cognitive functioning in children with end stage renal disease pre- and post-dialysis session. Int J Pediatr Nephrol. 1986;7:45–50.
Popel J, Joffe R, Acton BV, Bond G, Joffe AR, Midgley J, Robertson CMT, Sauve RS, Morgan C. Neurocognitive and functional outcomes at 5 years of age after renal transplant in early childhood. Pediatr Nephrol. 2019;34:889.
Moodabail DG, Reiser KA, Detre JA, Schultz RT, Herrington JD, Davatzikos C, Doshi JJ, Erus G, Liu HS, Radcliffe J, Furth SL, Hooper SR. Systematic review of structural and functional neuroimaging findings in children and adults with CKD. Clin J Am Soc Nephrol. 2013;8:1429–48.
Nichols SL, Press GA, Schneider JA, Trauner DA. Cortical atrophy and cognitive performance in infantile nephropathic cystinosis. Pediatr Neurol. 1990;6:379–81.
Hurkx W, Hulstijn D, Pasman J, Rotteveel J, Visco Y, Schroder C. Evoked potentials in children with chronic renal failure, treated conservatively or by continuous ambulatory peritoneal dialysis. Pediatr Nephrol. 1995;9:325–8.
Teschan PE, Ginn HE, Bourne JR, Ward JW, Hamel B, Nunnally JC, Musso M, Vaughn WK. Quantitative indices of clinical uremia. Kidney Int. 1979;15:676–97.
Albaramki JH, Al-Ammouri IA, Akl KF. Neurological and cardiac complications in a cohort of children with end-stage renal disease. Saudi J Kidney Dis Transpl. 2016;27:507–11.
Glenn CM, Astley SJ, Watkins SL. Dialysis-associated seizures in children and adolescents. Pediatr Nephrol. 1992;6:182–6.
Porto I, John EG, Heilliczer J. Removal of phenobarbital during continuous cycling peritoneal dialysis in a child. Pharmacotherapy. 1997;17:832–5.
Sanderson KR, Warady BA. End-stage kidney disease in infancy: an educational review. Pediatr Nephrol. 2020;35(2):229–40.
Hooper SR, Umansky W, editors. Young children with special needs. 6th ed. Columbus: Pearson/Prentice-Hall; 2014.
Coulthard MG, Crosier J. Outcome of reaching end stage renal failure in children under 2 years of age. Arch Dis Child. 2002;87:511–7.
Black MM, Dubowitz H, Krishnakumar A, Starr RH Jr. Early intervention and recovery among children with failure to thrive: follow-up at age 8. Pediatrics. 2007;120:59–69.
Harshman LA, Johnson RE, Kogon A, Matheson M, Shinnar S, Mendley S, Gerson A, Warady BA, Furth SR, Hooper SR. Academic achievement outcomes in children with mild to moderate chronic kidney disease: a report from the CKiD cohort. J Pediatr Nephrol. 2019;34(4):689–96.
National Reading Panel. Report of the National Reading Panel. Teaching children to read: an evidence-based assessment of the scientific research literature on reading and its implications for reading instruction (NIH Publication No. 00–4754). Washington, DC: U.S. Government Printing Office; 2000.
Wexler J, Vaughn S, Edmonds M, Reutebuch DK. A synthesis of fluency interventions for secondary struggling readers. Read Writ. 2008;21:317–47.
Solis M, Ciullo S, Vaughn S, Pyle N, Hassaram B, Leroux A. Reading comprehension interventions for middle school students with learning disabilities. J. Learning Dis. 2012;45:327–40. https://doi.org/10.1177/0022219411402691.
Baker S, Gersten R, Lee D. A synthesis of empirical research on teaching mathematics to low-achieving students. Elem Sch J. 2002;103:51–73.
Hooper SR, Wakely MB, de Kruif REL, Swartz CW. Aptitude-treatment interactions revisited: effect of a meta-cognitive intervention on subtypes of written expression in elementary school students. Dev Neuropsychol. 2006;29:217–41.
Graham S, Harris KR. Almost 30 years of writing research: making sense of it all with the wrath of Khan. Learn Disabil Res Pract. 2009;24:58–68.
Javalkar K, Ferris ME, Cuttance J, Hooper SR. Cognitive remediation in pediatric CKD: rationale, programmatic approaches, and potential applicability. Pediatr Nephrol. 2017;32:2027–35.
Ferris ME, Gipson DS, Kimmel PL, Eggers PW. Trends in treatment and outcomes of survival of adolescents initiating end-stage renal disease care in the United States of America. Pediatr Nephrol. 2006;21:1020–6.
McDonald SP, Craig JC. Australian and New Zealand Paediatric Nephrology Association long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350:2654–62.
Grootenhuis MA, Stam H, Last BF, Groothoff JW. The impact of delayed development on the quality of life of adults with end-stage renal disease since childhood. Pediatr Nephrol. 2006;21:538–44.
Bell LE, Ferris ME, Fenton N, Hooper SR. Health care transition for adolescents with CKD-the journey from pediatric to adult care. Adv Chronic Kidney Dis. 2011;18:384–90.
Icard PF, Hower SJ, Kuchenreuther AR, Hooper SR, Gipson DS. The transition from childhood to adulthood with ESRD: educational and social challenges. Clin Nephrol. 2008;69:1–7.
Foster BJ, Pai ALH, Zelikovsky N, Amaral S, Bell L, Dharnidharka VR, Herbert D, Holly C, Knauper B, Matsell D, Phan V, Rogers R, Smith JM, Zhao H, Furth SL. A randomized trial of a multicomponent intervention to promote medication adherence: the Teen Adherence in Kidney Transplant Effectiveness of Intervention Trial (TAKE-IT). Am J Kidney Dis. 2018;72:30–41.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hooper, S.R., Hartung, E.A. (2021). Neurocognitive Functioning in Pediatric Dialysis. In: Warady, B.A., Alexander, S.R., Schaefer, F. (eds) Pediatric Dialysis. Springer, Cham. https://doi.org/10.1007/978-3-030-66861-7_34
Download citation
DOI: https://doi.org/10.1007/978-3-030-66861-7_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66860-0
Online ISBN: 978-3-030-66861-7
eBook Packages: MedicineMedicine (R0)