Abstract
Acute aortic syndromes represent a spectrum of aortic pathology that most commonly manifest as an aortic dissection. The treatment of these potentially life-threatening conditions have benefited from a better understanding of their natural history along with advances in diagnostic and surgical technology. An overview of the historical evolution of these advances provides an insight into the pioneering work of numerous individuals that embraced the challenge of overcoming the barriers that stood between them and our current place in treating these complex patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Acute aortic syndromes are complex and potentially life-threatening pathologies of the aorta that have only been successfully managed in the last 70 years. The spectrum of disease ranges from intra-mural hematomas and penetrating aortic ulcers to aortic dissections and ruptured aneurysms, with dissections being the most frequent of these aortic pathologies. The ability to diagnose and treat these conditions have required advances in imaging as well as open and endovascular surgical techniques. The historical evolution of our understanding of these conditions and subsequent management reflect the critical nature of acute aortic syndromes and the pioneering efforts of innovators determined to improve the outcomes of these complex patients.
History of Acute Aortic Syndromes
The earliest reports of aortic pathology were noted in the Ebers Papyrus, an Egyptian scroll named after the Egyptologist, George Ebers (1837–1898 CE), which dates back to 1550 BCE. The scrolls are believed to be copied from earlier texts and it’s here that peripheral and abdominal aneurysms were first described [1]. The Greek physician, Galen de Pergamon (129-c. 200/c. 216 CE), described “localized pulsatile swellings” and a ruptured aneurysm: “when an aneurysm is wounded, the blood spouted out with so much violence that it can scarcely be arrested” [2]. A Greek surgeon and contemporary of Galen, Antyllos, further described aneurysms as being either false traumatic or true aneurysms. He also provided the earliest record of performing surgery to treat small peripheral aneurysms by ligating them proximally and distally followed by opening of the sac and evacuation of the thrombus. He further opposed surgery for larger aneurysms given that he believed they were too dangerous to treat. His approach to managing peripheral aneurysms remained the treatment of choice until the end of the nineteenth century [3, 4]. The Flemish physician, Andreas Vesalius (1514–1564 CE) was the first to solely use human anatomic dissections for what served as the modern recording of human anatomy. He identified aneurysms of the thoracic and abdominal aorta and considered them untreatable [5, 6]. German physician, Daniel Sennert (1572–1637 CE) appears to be the first to report aortic dissections, describing them as a separation of the aortic wall layers” while Giovanni Battista Morgagni (1682–1771 CE) reported several cases whereby blood forced its way through the wall “coming out under the external coat of the artery” [7, 8].
In 1760 George II, King of England, (Fig. 1) died in Kensington palace “while straining on the toilet”. The King had woken up at 6 am that morning and was following his morning routine when his “valet de chamber in waiting” heard a noise, after which he found the king lying on the floor, dead. The King’s personal physician, Frank Nicholls (1699–1778 CE), was ordered to open and embalm the body, which provided him with the opportunity to carefully document the cause of death. His detailed account of the findings served as the first documentation of pericardial tamponade caused by an aortic dissection. He specifically noted “…the pericardium was found distended with a quantity of coagulated blood, nearly a pint…; the whole heart was so compressed as to prevent any blood contained in the veins from being forced into the auricles; therefore the ventricles were found absolutely void of blood…; and in the trunk of the aorta we found a transverse fissure on its inner side, about an inch and a half long, through which some blood had recently passed under its external coat and formed an elevated ecchymosis” [9, 10]. Interestingly, King George II was also Duke of Hannover. This is the same Hannover in Germany that has been the site of many advances in aortic surgery.
In 1802, Jean Pierre Maunoir proposed the term “aortic dissection”, however in 1819, French surgeon René Théophile Laennec, the inventor of the stethoscope, was the first to use the term “dissecting aneurysm” [11, 12]. Since that time, this designation has created confusion regarding the nature of dissections and aneurysms and their distinct differences. In 1822, John Shekleton (1795–1824 CE) of Dublin was the first to report cases of chronic dissections, or what was described as “double barreled” aortas. His findings included a description of atheromatous changes on the lining of the aorta as well as the presence of a re-entry site into the original lumen [13]. In 1839, Viennese pathologist Carl von Rokitansky (1804–1878 CE) explained the difference between aortic dissection and spontaneous rupture [14]. In 1843 Thomas Peacock reported a case series of aortic dissections where he documented the importance of an intimal tear and hypothesized that the dissection was the result of a disruption of the “internal coats of the vessel”. Through experimental models of aortic dissections, he also described the reentry of flow back into the original vessel considering it an “imperfect natural cure of the disease”. He further described the difference in prognosis between dissections involving the ascending aorta versus those in the descending aorta [15, 16]. Other notable experts at that time offered an alternative theory to the concept of penetration of the aortic wall given that cases of dissection were identified that lacked a tear in the vessel. They believed that a primary cleavage of the media was the triggering event that led to dissection [17, 18]. At the end of the nineteenth century and into the early part of the twentieth century, several theories as to the pathophysiology of dissections existed. They varied from atheromatous ulcerations versus consequences of inflammation with “molecular changes of the elastic structures and subcellular events” along with stress from elevated blood pressure occurring in the wall of the aorta and lastly rupture of the vasa vasorum [19,20,21].
In 1934, Theodore Shennan published the largest series of aortic dissections at that time and proposed that degenerative changes in the media resulting in a loss of elasticity was an important factor leading to dissections. He also believed mechanical, inflammatory, and congenital factors could also be involved [22]. French pediatrician, Antoine Marfan, reported the first case of arachnodactyly in 1896 and studied the symptoms of the disease that would later bear his name but it was Helen Taussig and colleagues in 1943 that made the association between Marfan disease and aortic medianecrosis [23, 24]. That same year Lewis Etter reported the association between Marfan disease and aortic dissections [25]. In 1958, Albert E. Hirst published a report of over 500 aortic dissections that provided important detailed information about the etiology and pathogenesis of the disease along with valuable clinical insights. Also included in the report were the medical and surgical treatment strategies that had been employed up until that time [26].
Although less common than aortic dissection, intramural hematoma is another of the acute aortic syndromes. First described by Hans Eppinger Sr (1848–1916 CE) in 1887, it was Fredrich Krukenberg in 1920 that made the observation that a ruptured vaso vasorum can lead to a “dissection without intimal tear” [27, 28]. Penetrating aortic ulcer was first described as a clinical condition in 1986 by Anthony Stanson and colleagues and is also included in the scope of acute aortic syndromes [29].
Treatment of Acute Aortic Syndrome
Until surgical options became available, treatment of patients with aortic dissections centered largely around medical therapies. Mandatory bed rest was the mainstay of treatment in the eighteenth and nineteenth centuries and if patients were restless they received sedation along with morphine for pain. With the advent of antihypertensive medications, treating elevated blood pressures were felt to be of value by some, while others believed that the therapy itself encouraged dissections in patients with hypertension. In patients experiencing shock, the administration of whole blood plasma, intravenous fluids and vasoconstrictors were employed as these therapies became available [30,31,32]. Unfortunately, as can be expected, the success of these approaches was quite limited and reflected the need for more direct corrective therapies.
Throughout the nineteenth century, a variety of procedures were developed and used to address aortic aneurysms. Foreign bodies such as wires and needles were inserted into aneurysms along with the delivery of electrical currents with the idea of stimulating thrombus formation within the aneurysm sac. In doing so they would obliterate the artery thus stabilizing the aneurysm and preventing further growth or rupture [33,34,35]. The more sophisticated technique of endoaneurysmorrhaphy was introduced in the latter half of the century whereby surgeons would open the aneurysms with the intention of either obliterating the blood flow through the vessel from within versus reconstructing the vessel by creating a normal caliber lumen to maintain patency and excluding the aneurysm sac [36,37,38].
An alternative approach to addressing aneurysms and dissections were to wrap the involved vessels with either prosthetic or biologic materials in an attempt to stabilize the vessel and prevent rupture. The technique of wrapping cellophane around an aneurysm was introduced by Paul Harrison in 1943 whereby he wrapped two arteriovenous aneurysms of the subclavian artery resulting in their eventual elimination [39]. In 1948, James Edgar Paulin was the first to use cellophane to treat a dissection when he wrapped the material around a chronically dissected descending aorta [40]. Others reported the use of fascia lata, polyvinyl sponge, and dermal wrappings, all which were eventually abandoned due to poor results [41, 42]. After being diagnosed with an abdominal aortic aneurysm, Albert Einstein underwent cellophane wrapping of his aneurysm in 1948 but died 5 years later from subsequent rupture of the dilated vessel.
The first direct surgical treatment of an aortic dissection was performed by David Gurin and colleagues in 1935 to treat an ischemic leg caused by extension of the dissection into the right external iliac artery. Although the procedure was unsuccessful, Gurin attempted to reestablish blood flow into the leg by opening the vessel through the non-dissected segment and incising the intima into the dissected segment thus establishing a re-entry point for blood back into the true lumen [43]. In 1955, Robert S Shaw reported a similar strategy to improve blood flow back into the true lumen of a dissected thoracic and abdominal aorta. It was Shaw who coined the term “fenestration”, and this remains the name of the procedure to date. Despite its improvement of flow into the true lumen, the procedure did not address the complexities associated with ascending and arch dissections and was soon recognized as a largely palliative procedure [44].
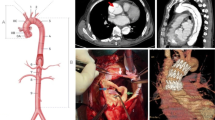
A critical step in the evolution of treating aortic pathology was the development of techniques that resected and subsequently replaced portions of the diseased vessel. The pioneering work of Nobel laureate Alexis Carrel along with Charles Guthrie led to the development of vascular anastomotic techniques and the use of homograft aortic substitutes [45]. Clarence Crafoord in 1944, was the first to resect a segment of the aorta and reestablish continuity with an end to end anastomosis to treat a coarctation and in 1948 Robert Gross was the first to replace a segment of the aorta using a homograft after resecting a coarctation [46, 47]. The direct repair of an aortic dissection was first performed by Michael DeBakey at Houston Methodist Hospital. In 1955 he reported a series of six cases whereby he repaired the descending thoracic aorta injured by dissection. In five of the procedures the aorta was transected and the false lumen was obliterated by sewing the true lumen circumferentially to the adventitia. Aortic continuity was then reestablished by either direct end to end anastomosis of the native aorta or placement of a homograft interposition (Fig. 2). The remaining case involved primary resection of a saccular aneurysm distal to the left subclavian artery followed by primary closure of the resultant defect [48].
The success of treating thoracic aortic pathology using homografts initially generated great hope and enthusiasm for the definitive treatment of conditions that were until that time felt to be untouchable. However, the limited durability and availability of homografts as well as less than optimal long-term outcomes, soon tempered that enthusiasm. As a result, a more durable and readily available alternative to homografts was needed. The development of synthetic arterial grafts began with the work of Arthur Voorhees who proposed the use of a tube constructed from fabric. First using a silk handkerchief and subsequently a material called “vinyon-N”, Voorhees reported the successful use of these prosthetic grafts in animal experiments in 1952 [49]. The first use of a synthetic graft to treat an aortic pathology was by Arthur Blakemore who used a graft made from vinyon-N to replace a ruptured abdominal aortic aneurysm in 1953 [50]. Charles Hufnagel reported the use of a Lucite tube containing his aortic assist valve to replace a large portion of descending thoracic aorta as a means of treating aortic insufficiency [51]. Although not intended to teat aortic pathology, this and the use of other synthetic grafts provided further proof of concept that the aorta can be replaced with a synthetic substitute. However, the poor physical adaptability, limited durability and inconsistent biocompatibility of vinyon-N and other materials such as Orlon and Teflon limited their wider acceptance and use. The polyester polymer Dacron, initially developed around 1939, was introduced to DeBakey in a department store when he was shopping for material to construct vascular grafts. Using his wife’s sewing machine, he created grafts that he then trialed in animals beginning in 1954. He found Dacron to be easier to sew to then vinyon-N and more physically adaptable for use in arterial reconstruction. In collaboration with industry, he led the development of seamless knit Dacron grafts of various sizes that were either tube shaped or had bifurcating segments to accommodate a variety of anatomic needs. The grafts were also constructed with circumferential crimping to allow for greater flexibility to shape the grafts without kinking. After 2 years of animal testing, DeBakey and his colleagues began to use the new grafts in humans and in 1958 they reported their experience of over 800 cases using these grafts in patients with occlusive disease of the abdominal aorta as well as the iliac and femoral arteries [52,53,54]. Further advances with synthetic grafts addressed issues of porosity and improved suture handling to the point where they have become the mainstay of arterial reconstruction.
Advances in cardiopulmonary bypass allowed for more complex approaches to the management of aortic pathologies particularly those involving the ascending aorta and arch. Denton Cooley and DeBakey were the first to report the successful resection and reconstruction of an ascending aortic aneurysm using a homograft in 1956 [55]. The following year DeBakey and colleagues reported the first successful replacement of the aortic arch once again using a homograft [56]. The first report of successful treatment of an ascending aortic dissection was by William Muller in 1960. In this series of three patients with Marfan’s syndrome and aortic aneurysms with aortic insufficiency, two were found to have dissections. As a result, the ascending aorta was resected and replaced with a Teflon graft. (Fig. 3) The aortic insufficiency was addressed using a bicuspidization technique that resulted in reducing the size of the dilated aortic annulus. The noncoronary sinus, leaflet and annulus were excised followed by primary closure of the defect resulting in a competent bicuspid aortic valve [57]. This report also served as the first to describe the management of an aortic dissection in Marfan’s patients and addressed the treatment of aortic valve insufficiency that can result from dissections or dilation of the aortic root. Frank Spencer and colleagues also described repairing the aortic valve in patients with aortic dissections due to separation of the commissure from the aortic wall using commissural resuspension [58]. The first successful repair of an acute ascending aortic dissection performed emergently took place in 1962 once again by DeBakey and colleagues [59].
In an effort to simplify how aortic dissections were thought of and subsequently treated, DeBakey began publishing classification schemas as early as 1955. The schema he published in 1965, and then modified in 1982, serves as the classic DeBakey classification schema where he defined three types of aortic dissection. Type I was dissections originating in the ascending aorta and extending beyond the left subclavian to involve varying degrees of the descending thoracic and abdominal aorta. Type II dissections were those that originated and were isolated to the ascending aorta. And Type III dissections were those that originated in the descending thoracic aorta, sparing the ascending aorta and arch [60, 61]. In 1970 Pat Daily and his colleagues at Stanford reported their experience with treating acute aortic dissections and in doing so provided an alternative classification schema. They defined dissections that involved the ascending aorta, irregardless of distal extension, as Type A and dissections that spared the ascending aorta and arch as Type B (Fig. 4). The Stanford classification has become the more readily applied means of labeling dissections and with it has come the universal clinical understanding that Type A dissections are to be treated as a surgical emergency while uncomplicated Type B dissections are largely treated with medical therapy [62].
The next phase in the advancement of treating aortic pathology was the development of procedures to address the aortic root. In 1962, Myron Wheat and colleagues reported the first replacement of the entire ascending aorta from the annulus to the innominate artery except for two small tongues of aortic wall containing the coronary ostia. The aorta was replaced with a woven Teflon graft and the aortic valve was replaced using a Starr-Edwards aortic prosthetic valve [63]. Hugh Bentall and Antony DeBono, in 1968, reported their technique for replacing the entire ascending aorta including the aortic root using a prosthetic valved conduit. The coronary ostia were anastomosed to corresponding openings on the graft while still in continuity with the native aortic tissue, given that the native aorta was then wrapped around the graft [64]. Kouchoukos and colleagues later described the resection of the pathologic aortic tissue and formation of coronary “buttons” that were anastomosed directly to the graft [65]. For patients with structurally normal aortic valves, valve sparing techniques were developed. Tyrone David introduced the technique of valve “reimplantation” in 1992 which entails implantating the native aortic valve inside a tube graft that is anchored to the aortic annulus and Magdi Yacoub, in 1993, reported the aortic remodeling technique which involves resecting the aorta to within 2–3 mm of the valve leaflets and commissures and anastomosing the graft to the cut edge of the aorta [66, 67]. These aortic root replacement procedures have been employed quite successfully in patients with dissections that leave the root either irreparably injured or with significant aneurysmal dilation [68, 69]. The choice of sparing the valve in the context of treating an acute dissection is dependent on the anatomy of the native valve and the degree to which the patient can withstand a potentially longer procedure, all the while being balanced against the expertise of the surgeon.
Other advances resulted in improved outcomes for patients with complex aortic pathology. Improved imaging modalities such as CT angiography, echocardiography, and MRI have made it possible to rapidly obtain detailed images in order to facilitate timely intervention. Deep hypothermic circulatory arrest and the use of cerebral perfusion techniques increased the safety of performing more complete arch procedures or procedures involving thoracoabdominal reconstructions [70,71,72]. The medical management of aortic dissections with a focus on reducing the “impulse” force of blood ejected from the left ventricle along with improved blood pressure control was introduced by Wheat and colleagues in 1965. This approach was the result of poor outcomes with the surgical management of aortic dissections and has since evolved into the practice of using pharmacologic therapy as the first line approach for uncomplicated Type B aortic dissections [73]. Endovascular treatment of arterial pathology began in the 1980s with the development of the first aortic stent grafts. The first clinical use was in 1985 when Nikolai Volodos placed a stent graft in the left common and external iliac artery of a patient to treat stenotic atherosclerotic disease manifesting signs of ischemia. Volodos and his colleagues were also the first to use a stent graft in the aorta to treat a post-traumatic pseudoaneurysm of the thoracic aorta [74]. Julio Palmaz developed the first balloon-expandable stent and in collaboration with Juan Parodi performed the first endovascular repair of an abdominal aortic aneurysm in 1990 [75]. The first use of an endovascular approach to treat a descending thoracic aneurysm was reported by Michael Dake and colleagues in 1994, and in 1999 two back-to-back reports detailed the use of this strategy towards treating Type B aortic dissections [76,77,78] (Fig. 5). In recent years, more sophisticated endovascular techniques have been developed in conjunction with more aggressive open surgical operations. The classic elephant trunk operation, first reported by Hans Borst and used to aggressively treat Type A aortic dissections, has been transformed to an endovascular frozen elephant trunk procedure [79, 80]. Lastly, the application of endovascular therapy has made its way to the ascending aorta as well, whereby direct treatment of high-risk patients with Type A aortic dissections have been reported, however, these have been limited to case series and single center experiences [81].
Thoracic aortograms obtained before and immediately after stent–graft placement over the primary entry tear. (a) Before stent–graft deployment, there is flow of contrast medium from the true lumen (T) across the entry tear (arrow) into the false lumen (F). (b) After stent–graft placement, only the true lumen is evident. (Taken from: Dake MD, Kato N, Mitchell RS, Semba CP, Razavi MK, Shimono T, Hirano T, Takeda K, Yada I, Miller C. Endovascular stent-graft placement for the treatment of acute aortic dissection. N Engl J Med. 1999;340:1546–52
Treatment of the other acute aortic syndromes, and in particular intramural hematomas is somewhat controversial. Given that intramural hematomas have some similarities, but also some differences with acute aortic dissections, the management of this clinical entity has led to different schools of thought. In patients with involvement of the ascending aorta, some advocate surgical intervention based on a threshold of wall thickness, while others believe this presentation to be part of a spectrum of Type A dissections and should therefore be treated as such. Acute aortic dissections, intramural hematomas and penetrating aortic ulcers can occur simultaneously or separately, but they share the characteristic of being potentially lethal and therefore needing sound clinical judgment for their treatment.
The purpose of this book is to gather the opinions of many of the world’s experts in the treatment of acute aortic syndromes. It is meant to present a concise, practical approach to the diagnosis, treatment and surveillance of aortic disease. As with most difficult clinical conditions, opinions vary as to the best medical, surgical, and endovascular treatment. Importantly, it should be remembered that even though one author advocates one manner of treatment, there are many ways to manage acute aortic dissections and other acute aortic syndromes.
References
Ghalioungui P. The Ebers papyrus: a new English translation, commentaries and glossaries. Cairo: Academy of Scientific Research and Technology; 1987.
Galen J. Observations on aneurysms. London: Translated by John Eric Erichsen; 1986.
Daremberg C. Oevres d’Oribase. IV. Paris; 1867.
Sachs M. Die Methoden der Blutstillung in ihrer historischen Entwicklung. Hamostaseologie. 2000;20:83–9.
Vesalii A. De humani corporis fabrica libri septem. Padua; 1543.
Bonetus T. Sepulchretum anatomia practica ex cadaveribus morbo denatis. Book 3, Sect 2. Lugduni (Lyon); 1700. p. 290.
Sennertus Daniel. Opera. Op Omn Lib 5,1, Cap 42, p.306 Lugduni (Lyon); 1650.
Battista MG. De sedibus et causis morborum per anatomen indagates [the seats and causes of diseases investigated by anatomy; in five books, containing a great variety of dissections, with remarks]. Ep 26, Art 17 (Ep 48) F 50. Venice; 1761.
Nicholls L. Observations concerning the body of his late majesty. Philos Trans (Lond). 1761;52:265–74.
Leonard JC. Thomas Bevill peacock and the early history of dissecting aneurysm. Br Med J. 1979;2:260–2.
Maunoir JP. Mémoires Physiologiques et Practiques sur l’Aneurysme et la Ligature des Artères. Géneva; 1802.
Laennec RT. De l’Auscultations Médiate, ou Traité du Diagnostic des Maladies des Poumons et du Coeur. Paris: Fondé Principalemente sur ce Nouveau Moyen d’Esploration; 1819.
Shekleton J. Dublin Hosp. Rep. 1822;3:231.
Rokitansky VK. Über spontane Zerreissungen der Aorta. Schmidts Jahrbuch. 1839;24:30–3.
Peacock TB. Report on cases of dissecting aneurysms. Trans Path Soc Land. 1863;14:87.
Peacock TB. An account of some experiments illustrative of the mode of formation of the dissecting aneurysm. Monthly J Med Sci. 1843;3:871–8.
Whitman RG, Stein HB. A contribution to the pathogenesis of dissecting aneurysms: a case of dissecting Mesaortitis (babes and Mironescu), without dissecting aneurysm. J Med Res. 1924;44:579–92.
Babes V, Mironescu T. Über dissezierende Arteriitis und Aneurysma dissecans. Beitr Pathol Anat Allg Pathol. 1910;48:221.
Virchow R. Handbuch der speciellen Pathologie und Therapie. Erlangen; 1854.
Recklinghausen FD. Auserlesene pathologisch-anatomische Betrachtungen. Virchows Arch Pathol Anat Physiol. 1864;30:372–87.
Recklinghausen FD. Handbuch der allgemeinen Pathologie des Kreislaufs und der Ernährung. Stuttgart; 1883.
Shennan T. Dissecting aneurysm. In: medical research council special report, series no. 193. London: His Majesty’s Stationary Office; 1934.
Marfan AB. Un cas de déformation congénitale des quatre members, plus prononcée aux extrémités, caracterisée par l’ allongement des os avec un certain degréd’ amincissement. Bull Mem Soc Med Hop Paris. 1896;13:220–6.
Baer RW, Taussig HB, Oppenheimer EH. Congenital aneurysmal dilation of the aorta associated with arachnodactyly. Bull John Hopk Hosp. 1943;72:309–32.
Etter LE, Glover LP. Arachnodactyly complicated by dislocated lens and death from rupture of dissected aneurysm of the aorta. J Am Med Assoc. 1943;123:88–9.
Hirst AE, Johns VJ, Kime SW. Dissecting aneurysms of the aorta: a review of 505 cases. Medicine. 1958;37:217–79.
Eppinger H. Pathogenesis, Histogenesis und Aetiologie der Aneurysmen, einschließlich des Aneurysma equi verminosum: Pathologisch-anatomische Studien. Berlin; 1887.
Krukenberg E. Beitrage zur Frage des Aneurysma dissecans. Beitr Pathol Anat Allg Pathol. 1920;67:329–51.
Stanson AW, Kazmier FJ, Hollier LH, et al. Penetrating atherosclerotic ulcers of the thoracic aorta: natural history and clinicopathologic correlations. Ann Vasc Surg. 1986;1:15–23.
Beaven DW, Murphy EA. Dissecting aneurysm during methonium therapy; report of nine cases treated or hypertension. Br M J. 1956;1:77–80.
MacCuish RK. Dissecting aortic aneurysm; varied clinical picture. Br M J. 1953;1:71–3.
Pyke DA. Dissecting aneurysm of aorta; recovery after treatment with hexamethonium. Lancet. 1953;2:1189–90.
Ciniselli L. Sugli aneurismi dell’aorta toracica finora trattati colla elettro-puntura. Ann Univ Med. 1870;214:292.
Weir RF, Page ED. Aneurysm of the ascending aorta treated by Macewen’s needling method for inducing white thrombus. NY Med J. 1892;55:510–1.
Siddique K, Alvernia J, Fraser K, Lanzino G. Treatment of aneurysms with wires and electricity: a historical overview. J Neurosurg. 2003;99:1102–7.
Matas R. Traumatic aneurysm of the left brachial artery. Incision and partial excision of the sac-recovery. Med New NY. 1888;53:462–6.
Matas R. Personal experiences in vascular surgery: a statistical synopsis. Ann Surg. 1940;112:802–39.
Creech O. Endo-aneurysmorrhaphy and treatment of aortic aneurysm. Ann Surg. 1966;164:935–46.
Harrison P, Chandy J. A subclavian aneurysm cured by cellophane fibrosis. Ann Surg. 1943;118:478–81.
Paullin JE, James DF. Dissecting aneurysms of the aorta. Postgrad Med. 1948;4:291–9.
Warren WD, Beckwith J, Muller WH. Problems in the surgical management of acute dissecting aneurysms of the aorta. Ann Surg. 1956;144:530–48.
Kirschner M, Schubert A. Lehrbuch der Chirurgie. Allgemeine u. spezielle chirurgische Operationslehre. Berlin; 1927.
Gurin D, Bulmer JW, Derby R. Dissecting aneurysm of the aorta: diagnosis and operative relief of acute arterial obstruction due to this cause. NY J Med. 1935;35:1200–2.
Shaw RS. Acute dissecting aortic aneurysms: treatment by fenestration of the internal wall of the aneurysm. N Engl J Med. 1955;253:331–3.
Smith RB. Presedential address: the foundations of modern aortic surgery. J Vasc Surg. 1998;27:7–15.
Crafoord C, Nylin G. Congenital coarctation of the aorta and its surgical treatment. J Thorac Surg. 1945;14:347–61.
Gross RE, Hurwitt ES, Bill AH, Peirce EC. Preliminary observations on the use of human arterial grafts in the treatment of certain cardiovascular defects. N Engl J Med. 1948;239:578–9.
DeBakey ME, Cooley DA, Creech O. Surgical considerations of dissecting aneurysms of the aorta. Ann Surg. 1955;142:586–610.
Voorhees AB, Jaretzki A, Blakemore AH. The use of tubes constructed from Vinyon “N” cloth in bridging arterial defects. Ann Surg. 1952;135:332–6.
Levin SM. Breakthrough: Arthur Blakemore and Arthur Voorhees Jr. J Vasc Surg. 2012;55:1829–31.
Hufnagel CA, Harvey WP, Rabil PJ, McDermott TF. Surgical correction of aortic insufficiency. Surgery. 1954;35:673–83.
DeBakey ME, Jordon GL, Abbott JP, Halpert B, O’Neal RM. The fate of dacron vascular grafts. Arch Surg. 1964;89:757–82.
DeBakey ME, Cooley DA, Crawford ES, Morris GC Jr. Clinical applications of a new flexible knitted dacron arterial substitute. Am Surg. 1958;24:862–9.
DeBakey ME, Crawford ES, Cooley DA, Morris GC Jr. Surgical considerations of occlusive disease of the abdominal aorta and iliac and femoral arteries; analysis of 803 cases. Ann Surg. 1958;148:62–80.
Cooley DA, DeBakey ME. Resection of entire ascending aorta in fusiform aneurysm using cardiac bypass. J Am Med Assoc. 1956;162:1158–9.
DeBakey ME, Crawford ES, Cooley DA, Morris GC Jr. Successful resection of fusiform aneurysm of aortic arch with replacement by homograft. Surg Gynecol Obstet. 1957;105:657–64.
Muller WH Jr, Dammann JF Jr, Warren WD. Surgical correction of cardiovascular deformities in Marfan’s syndrome. Ann Surg. 1960;152:506–16.
Spencer FC, Blake H. A report of the successful surgical treatment of aortic regurgitation from dissecting aortic aneurysm in a patient with the Marfan syndrome. J Thorac Cardiovasc Surg. 1962;44:238–45.
Morris GC, Henly WS, DeBakey ME. Correction of acute dissecting aneurysm of aorta with valvular insufficiency. J Am Med Assoc. 1963;184:185–6.
DeBakey ME, Henly WS, Cooley DA, Morris GC, Crawford ES, Beall AC. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg. 1965;49:130–49.
DeBakey ME, McCollum CH, Crawfrom ES, Morris GC Jr, Howell J, Noon GP, Lawrie G. Dissection and dissecting aneurysms of the aorta: twenty-year follow-up of five hundred twenty-seven patients treated surgically. Surgery. 1982;92:1118–34.
Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thor Surg. 1970;10:237–47.
Wheat MW Jr, Wilson JR, Bartley TD. Successful replacement of the entire ascending aorta and aortic valve. J Am Med Assoc. 1962;188:717–9.
Bentall H, DeBono A. A technique for complete replacement of the ascending aorta. Thorax. 1968;23:338–9.
Kouchoukos NT, Wareing TH, Murphy SF, Perrillo JB. Sixteen-year experience with aortic root replacement. Results of 172 operations. Ann Surg. 1991;214:308–18.
David TE, Feindel CM. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J Thorac Cardiovasc Surg. 1992;103:617–21.
Sarsam MA, Yacoub M. Remodeling of the aortic valve annulus. J Thorac Cardiovasc Surg. 1993;105:435–8.
Irimie V, Atieh A, Kucinoski G, Jankulovski A, Zacher M, Urbanski PP. Long-term outcomes after valve-sparing anatomical aortic root reconstruction in acute dissection involving the root. J Thorac Cardiovasc Surg. 2019 Apr 25 [Online ahead of print].
Rosenblum JM, Leshnower BG, Moon RC, Lasanajak Y, Binongo J, McPherson L, Chen EP. Durability and safety of David V valve-sparing root replacement in acute type A aortic dissection. J Thorac Cardiovasc Surg. 2019;157:14–23.
Griepp RB, Stinson EB, Hollingsworth JF, Buehler D. Prosthetic replacement of the aortic arch. J Thorac Cardiovasc Surg. 1975;70:1051–63.
Kouchoukos NT, Wareing TH, Izumoto H, Klausing W, Abboud N. Elective hypothermic cardiopulmonary bypass and circulatory arrest for spinal cord protection during operations on the thoracoabdominal aorta. J Thorac Cardiovasc Surg. 1990;99:659–64.
Stamou SC, Rausch LA, Kouchoukos NT, Lobdell KW, Khabbaz K, Murphy E, Hagberg RC. Comparison between antegrade and retrograde cerebral perfusion or profound hypothermia as brain protection strategies during repair of type A aortic dissection. Ann Cardiothorac Surg. 2016;5:328–35.
Wheat MW Jr, Palmer RF, Bartley TD, Seelman RC. Treatment of dissecting aneurysms of the aorta without surgery. J Thorac Cardiovasc Surg. 1965;50:364–73.
Volodos NL. Historical perspective: the first steps in endovascular aortic repair: how it all began. J Endovasc Ther. 2013;20:S3–23.
Parodi JC, Palmaz JC, Barone H. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991;5:491–9.
Dake MD, Miller DC, Semba CP, Mitchell RS, Walker PJ, Liddell RP. Transluminal placement of endovascular stent-grafts for the treatment of descending thoracic aortic aneurysms. N Engl J Med. 1994;331:1729–34.
Nienaber CA, Fattori R, Lund G, Dieckmann C, Wolf W, von Kodolitsch Y, Nicolas V, Pierangeli A. Nonsurgical reconstruction of thoracic aortic dissection by stent-graft placement. N Engl J Med. 1999;340:1539–45.
Dake MD, Kato N, Mitchell RS, Semba CP, Razavi MK, Shimono T, Hirano T, Takeda K, Yada I, Miller C. Endovascular stent-graft placement for the treatment of acute aortic dissection. N Engl J Med. 1999;340:1546–52.
Borst HG, Walterbusch G, Schaps D. Extensive aortic replacement using the “elephant trunk” prosthesis. Thorac Cardiovasc Surg. 1983;31:37–40.
Karck M, Chavan A, Hagl C, Friedich H, Galanski M, Haverich A. The frozen elephant trunk technique: a new treatment for thoracic aortic aneurysms. J Thorac Cardiovasc Surg. 2003;125:1550–3.
Vallabhajosyula P, Gottret J-P, Bavaria J, Desai ND, Szeto WY. Endovascular repair of the ascending aorta in patients at high risk for open repair. J Thorac Cardiovasc Surg. 2015;149:S144–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ehsan, A., Sellke, F.W. (2021). Overview and History of Aortic Dissection and Other Acute Aortic Syndromes. In: Sellke, F.W., Coselli, J.S., Sundt, T.M., Bavaria, J.E., Sodha, N.R. (eds) Aortic Dissection and Acute Aortic Syndromes. Springer, Cham. https://doi.org/10.1007/978-3-030-66668-2_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-66668-2_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66667-5
Online ISBN: 978-3-030-66668-2
eBook Packages: MedicineMedicine (R0)