Abstract
Repetitive and restricted behaviors and interests (RRBI’s) described in individuals with Autism Spectrum Disorder (ASD) and defined in the DSM-5 criteria are diverse. They encompass repetitive behaviors, such as stereotyped motor movements, repetitive manipulation of objects, repetitive and stereotyped language, repetitive sensory behaviors and insistence on sameness. Many theories regarding the neurological mechanisms underlying RRBI’s in ASD have been suggested, ranging from psychological, structural and anatomical abnormalities to molecular and genetic impairments. In this chapter we elaborate on some of the leading theories concerning the neurological basis of RRBI’s in ASD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others

Keywords
- Repetitive and restricted behaviors and interests
- Repetitive and restricted behaviors
- Autism spectrum disorder
- Neurological mechanisms
Repetitive and restricted behaviors and interests (RRBI’s) described in individuals with Autism Spectrum Disorder (ASD) and defined in the DSM-5 criteria are diverse (American Psychiatric Association, 2013). They encompass repetitive behaviors, such as stereotyped motor movements (i.e. hand flapping), repetitive manipulation of objects (i.e. spinning objects), repetitive and stereotyped language (i.e. immediate and delayed echolalia), repetitive sensory behaviors (i.e. visual inspection of objects), and insistence on sameness (i.e. compulsions, rituals and routines, and narrow and circumscribed interests) (Jiujias, Kelley, Hall, & Kelley, 2017; Kim & Lord, 2010; M. Lewis & Kim, 2009b; Mark H. Lewis & Bodfish, 1998; Stratis & Lecavalier, 2013; Turner, 1999).
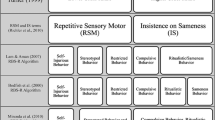
Research based on standardized diagnosing tools such as the Repetitive Behavior Scale-Revised (RBS-R) (Bodfish, Symons, Parker, & Lewis, 2000), the Autism Diagnostic Interview-Revised (ADI-R) (Lord, Rutter, & LeCouteur, 1994), and the Autism Diagnostic Observation Schedule (ADOS) (Lord et al., 2000) grouped these RRBI’s into two distinct categories: lower-level behaviors that include the repetitive behaviors, and high-level ones that include ritualistic habits and a strict adherence to well-established routines (Bishop et al., 2013; Kim & Lord, 2010; Richler, Huerta, Bishop, & Lord, 2010; Stratis & Lecavalier, 2013). The trajectory of RRBI’s presentation changes with age and level of cognition (Jiujias et al., 2017; Stratis & Lecavalier, 2013) and may increase in severity (Richler et al., 2010). In addition, restricted interests and rituals were shown to be more prevalent in children with higher scores of non-verbal IQ (NVIQ) than repetitive sensory motor behaviors (Bishop, Richler, & Lord, 2006).
Many theories regarding the neurological mechanisms underlying RRBI’s in ASD have been suggested, ranging from psychological, structural and anatomical abnormalities to molecular and genetic impairments. In this chapter we elaborate on some of the leading theories concerning the neurological basis of RRBI’s in ASD.
RRBI’s and Psychological Theories
Researchers throughout the years have attempted to explain what drives individuals with ASD to execute RRBI’s. Very early works hypothesized that individuals with ASD have a constant nonspecific activation of the ascending reticular activating system, and therefore wish to lower that arousal by engaging in RRBI’s to block new sensory input (B. Y. C. Hutt & Hutt, 1965; C. Hutt, Hutt, Lee, & Ounsted, 1964; Turner, 1999). Others refer to RRBI’s as a homeostatic mechanism, claiming that individuals with ASD tend to perform RRBI’s in situations involving lack of stimulation, or over stimulation from their environment (Sloman, LaRue, Weiss, & Hansford, 2013; Turner, 1999). However, a later work suggested that stereotyped behaviors were more likely to occur under conditions of low stimulation, and were less likely during conditions involving social contact (Hall, Thorns, & Oliver, 2003). Lovaas, Newsome, and Hickman (1987), hypothesized that RRBI’s stem from self-stimulatory behaviors, and therefore act as operant responses, meaning that the consequences of the behaviors act to reinforce the continuous use of RRBI’s by the individual.
Some other theories concerning RRBI’s’ etiology in individuals with ASD are based on the leading psychological theories for explaining the core symptoms of ASD: “Theory of Mind” (ToM), “weak central coherence” and “executive function deficits”. For example, it has been suggested that individuals with ASD have “weak central coherence”: as a result of deficits in information processing, they tend to focus on trivial details and miss the greater social context, leading to restricted and repetitive interests (Frith & Happe, 1994).
The “executive functioning deficits” theory has traditionally been thought of as the primary explanation for RRBI’s in ASD (Rosenthal et al., 2013). Executive functioning is an umbrella term, used to describe a wide range of behaviors involved in planning, controlling, and regulating higher-order mental processes (Rosenthal et al., 2013). Deficits in cognitive flexibility- the ability to shift thoughts and adapt behaviors to the changing environment- was consistently associated with the presence of RRBI’s in ASD (Street, 1994; Turner, 1999). Other executive function impairments, such as inhibitory and attentional deficits, were also suggested as part of RRBI’s etiology in individuals with ASD (Mostert-Kerckhoffs, Staal, & Houben, 2015; Schmitt, White, Cook, Sweeney, & Mosconi, 2017). In a study on 64 high-functioning individuals with ASD and 53 typically developing (TD) comparison participants, individuals with ASD showed significantly higher cognitive control dysfunctions. Moreover, the severity of inhibitory control and attentional flexibility deficits predicted the severity of RRBI’s in everyday life. Specifically, response inhibition in reaction to visual information, and task switching in reaction to auditory information, predicted motor and sensory stereotyped behavior (Mostert-Kerckhoffs et al., 2015).
Additionally, there are those who hypothesized that RRBI’s in ASD are correlated with anxiety levels (Sullivan et al., 2014). For example, it has been suggested that RRBI’s serve as a coping strategy for lowering high levels of anxiety in individuals with ASD. The anxiety may be caused by deficits in ToM, the understanding of other people’s mental state, which is the leading theory for explaining social-communication impairments in ASD (Baron-Cohen, 1989; Turner, 1999). In a different study, the correlation between anxiety levels and RRBI’s in individuals with ASD was compared with that of individuals with Down Syndrome and typically developing (TD) individuals. The researchers used questionnaires completed by the parents of the participants concerning their RRBI’s and anxiety levels. The results yielded a correlation between higher levels of anxiety and higher levels of RRBI’s only among individuals with ASD (D. W. Evans, 2017). This issue was addressed in an additional study, in which self-report questionnaires were used rather than parental reports. The results also indicated a significant relation between RRBI’s and anxiety, as reported by the individuals with ASD themselves (Joyce et al., 2017).
It is well agreed that ASD is a highly heterogeneous neurodevelopmental disorder with complex genetic origin and epigenetic impact (a probable contributing environmental component). Yet, the exact etiology remains unknown. Recent advances in the field of neuroscience have pointed out that specific behaviors are mediated not by impairments in one brain region but rather by subtle alterations across multiple brain regions, neurotransmitter systems, and synaptic processes that converge as neural circuits. This would also be true for ASD, as researchers currently consider it a brain network connectivity disorder (Just, Cherkassky, Keller, & Minshew, 2004; Monk et al., 2009; Nomi & Uddin, 2015; Shih et al., 2010), in which multiple genes coding for synaptic functioning are involved, leading to impairments in large-scale neuronal networks (Muhle, Reed, Stratigos, & Veenstra-vanderweele, 2018). Hence, it is possible that ASD behaviors that are explained by different psychological theories, such as RRBI’s, originate from specific genetic and molecular etiologies and are related to specific brain structure and/or functional abnormalities.
Structural Abnormalities
Another hypothesis regarding the etiology of RRBI’s in individuals with ASD suggests that some anatomical changes in certain brain structures are correlated with the severity of the RRBI’s among individuals with ASD.
Most studies have focused on the basal ganglia and the striatum. The basal ganglia are a group of interconnected subcortical nuclei, the primary afferent structure being the striatum. In most mammals, including humans, the striatum contains the caudate and putamen, which are divided by the fibers of the internal capsule (Albin, Young, Penney, Roger, & Young, 1989). The basal ganglia and the striatum are associated with a number of roles, ranging from cognition to motor movements (Stocco, Lebiere, & Anderson, 2011). In addition, the classic inhibitory neurotransmitter of the basal ganglia is the neurotransmitter GABA (Albin et al., 1989), whereas dopamine and glutamate are the dominant excitatory neurotransmitters (Caravaggio et al., 2016). The basal ganglia activity is traditionally divided to two pathways. The “direct pathway” describes the inhibitory effect of the striatum on the substantia nigra reticulata (SNr) and the globus pallidus interna (GPi). This inhibition of SNr/GPi causes a dis-inhibitory effect on the thalamus. The “indirect pathway” has the opposite effect on the thalamus. This pathway proceeds through the globus pallidus externa (GPe) and the sub thalamic nucleus (STN), leading to an inhibitory effect on the thalamus (Stocco et al., 2011). These pathways are involved in the control of motor movements in a subtle and complex pattern, since the basal ganglia have a role in the generation and execution of context-dependent behaviors (Y. Smith, Bevan, Shink, & Bolam, 1998).
In a study that compared high functioning individuals with ASD aged 6–17 to a TD comparison group, it was shown that the individuals with ASD had significant impairments in several measures of motor control (Newschaffer, Denckla, Landa, & Mostofsky, 2006). In addition, there is a resemblance between the ritualistic, repetitive, stereotyped and compulsive behavior in ASD and behaviors observed in other psychiatric disorders, for example obsessive-compulsive disorder (OCD) Boyer & Lie’nard, 2006; D. W. Evans et al., 1997; Langen, Durston, Kas, Van Engeland, & Staal, 2011). It was also reported that there may be a connection between basal ganglia lesions and obsessive-compulsive behavior (Graybiel & Rauch, 2000; Langen et al., 2011). Hence, it is reasonable to investigate brain structure abnormalities, especially basal ganglia changes, in the context of RRBI’s in ASD.
In a study of 35 high functioning individuals with ASD and 36 TD individuals matched for age, gender and IQ (Ranson et al., 1999), the participants went through volumetric measurements of basal ganglia components (e.g. the bilateral caudate, putamen and globus pallidus) using Magnetic Resonance Imaging (MRI). The research revealed changes in the volume of the caudate nucleus, which was larger in participants diagnosed with ASD. Also, the increased caudate nucleus volume in ASD participants was correlative to an increase in their total brain volume, a phenomena that has been reported in several other studies (Anthony et al., 1989; Lainhart et al., 1997). The researchers claim that caudate volume in individuals with autism was associated with severity of compulsive behavior, difficulties with minor changes in routine, and motor stereotypies (Ranson et al., 1999).
The correlation between basal ganglia size, shape or volume and the degree of RRBI’s severity in ASD was examined in additional structural studies. Hollander et al. (2005) revealed a larger right caudate volume in ASD compared with TD individuals. They also pointed out a correlation between right caudate and total putamen volumes and repetitive behavior scores on the ADI repetitive behavior scores (ADI-C), especially in the higher order OCD-like repetitive behaviors.
In addition, the differences in basal ganglia size in participants with ASD who were not on medication compared to TD individuals was investigated in another study which indicated a significant enlargement of the total caudate nucleus and bilateral putamen in the group with ASD. However, no significant correlations between ADI-R scores for RRBI’s and basal ganglia structural changes were found (Langen, Durston, Staal, Palmen, & Van Engeland, 2007). Moreover, other studies indicate a positive correlation between basal ganglia volumes and metabolic activity and ASD (Buchsbaum et al., 2006; Voelbel, Bates, Buckman, Pandina, & Hendren, 2006). However, it is worth noting that some studies found no such correlations (Gaffney, Kuperman, Tsai, & Minchin, 1989; Goldman, O’Briend, Filipekf, Rapina, & Herbertg, 2013) or an opposite correlation (Estes et al., 2012).
A slightly different study using MRI focused on the cortico-striatal connectivity and not on the structural changes in volume. In this study, differences were found among the 50 participants with ASD, compared with 52 TD individuals (Abbott et al., 2018). The study’s results suggested a possible association between RRBI’s, as measured by the Repetitive Behavior Scale-Revised (RBS-R) scores, and imbalanced cortico-striatal intrinsic functional connectivity (iFC) in ASD, being increased for limbic circuits, but reduced for frontoparietal and motor circuits (Abbott et al., 2018).
Besides the basal ganglia, other brain structures were investigated in the context of RRBI’s in ASD. One such study used MRI to test the gray matter volume of 24 participants with ASD compared with 23 TD individuals. The results suggested that the volumes of the medial frontal gyri, left pre-central gyrus, right post-central gyrus, right fusiform gyrus, caudate nuclei, and left hippocampus were larger in the ASD group relative to the TD individuals, while regions exhibiting smaller volumes in the ASD group were observed exclusively in the cerebellum (Rojas et al., 2006). Additionally, significant partial correlations were found between a measure of RRBI’s in the ADI-R repetitive and stereotyped behavior domain and the volumes of the caudate nuclei, multiple frontal and temporal regions, and the cerebellum (Rojas et al., 2006). In a meta-analysis that investigated the differences between gray matter morphometric changes in boys diagnosed with ASD compared with girls, the girls showed less severe RRBI’s as measured by the ADI-R. In addition, gray matter patterns in the motor cortex, the supplementary motor area (SMA), the cerebellum, the fusiform gyrus and the amygdala accurately differentiated between girls and boys with ASD, but not TD boys and girls. Moreover, gray matter pattern differences in the motor cortex, the SMA and in parts of the cerebellum were correlated with RRBI’s severity in girls, whereas gray matter patterns in the right putamen were correlated with RRBI’s in boys (Supekar & Menon, 2015).
Currently, it seems that there are no conclusive and convincing data from clinical trials regarding the significance of structural changes in the brains of individuals with ASD in general, and in the basal ganglia in particular, in relation to the prevalence and severity of RRBI’s.
Genetic Abnormalities
Thanks to great advancements in technology over the past decade, it is now clear that ASD has a robust genetic component, since it has strong familial inheritance patterns and approximately 1000 genes are potentially implicated (Ramaswami & Geschwind, 2018). The new discoveries in this field have led to the ability to determine the etiology of 10–20% of ASD cases (Geschwind, 2011). There are no common mutations that are responsible for most cases of ASD (Abrahams & Geschwind, 2009; Geschwind, 2011), and the roles of the genes implicated in ASD vary, from synaptic proteins, RNA processing, and many others (Geschwind, 2011). Gene-gene interactions and epigenetic mechanisms are also considered part of the genetic causes of ASD (Ma et al., 2005).
Focusing on the genetic basis of RRBI’s as one of the core features of ASD, some researchers have tried to find correlations between genetic variations and RRBI’s in ASD. One such study was based on major Genome-Wide Association Study (GWAS(data from large ASD family cohorts. They used the ADI-R to assess RRBI’s. Their results revealed that seven out of the 12 RRBI’s that were measured were significantly familial and variable, and hence were subjected to further investigations using the GWAS. These RRBI’s included circumscribed interests (68), repetitive use of objects (69), compulsions/rituals (70), unusual sensory interests (71), general sensitivity to noise (72), unusual attachments to objects (76), and stereotyped body movements (78). Eventually, after applying diverse methods of research and analysis, the researchers suggested two novel risk genes, SLC35B1 and PHB, for RRBI’s in ASD (Cantor et al., 2017).
A second group of researchers tried to identify common variants that are associated with RRBI’s. They performed the GWAS using the Autism Genetic Resource Exchange (AGRE) dataset and pointed out three Single Nucleotide Polymorphisms (SNPs) that might be correlated to RRBI’s, one of which was also linked to schizophrenia. Additionally, all of the most significantly associated SNPs were found to be in close proximity to genes that are involved in neuron development (Tao et al., 2016). A third study approached the heritability issue of RRBI’s in ASD from a different angle. The researchers examined the connection between severity of RRBI’s among parents of children diagnosed with ASD as measured by the Interest in Patterns and Resistance to Changes subscales of the Autism Quotient, and the severity of RRBI’s in the ASD diagnosed children themselves, measured by the Autism Diagnostic Observation Schedule RRB (ADOS RRB) standardized domain score. The results suggested that such a connection exists, as having both parents within the top 20% of RRBI’s scores was associated with increased RRBI’s scores for their children (Uljarevi, Evans, Alvares, & Whitehouse, 2016).
In a different genetic study, the researchers chose to focus on oxytocin (Francis, Kim, et al., 2016). Oxytocin is a neuropeptide that may have a role in the pathophysiology of ASD, and has even been suggested as a potential treatment for ASD (Anagnostou et al., 2012). This study tested whether there is a correlation between SNPs in genes related to oxytocin or arginine-vasopressin systems, and ASD and its core symptoms, social communication deficits and RRBI’s. The study results indicate that there is a correlation, with an especially significant association between SNP in the gene for oxytocin and having an ASD diagnosis (Francis, Kistner-griffin, et al., 2016). Another study by the same group also found a correlation between variants and SNPs in the receptors for oxytocin and vasopressin and being diagnosed with ASD. Specifically, variants correlated to RRBI’s severity as measured by the ADOS RRB scores (Francis, Kim, et al., 2016).
Others have tried to clarify the previously assumed connection between RRBI’s and several genetic disorders. In one study, the RRBI’s were characterized using a questionnaire (Repetitive Behavior Questionnaire, “RBQ“) with 797 participants who were diagnosed with specific genetic disorders such as Angelman, Cornelia de Lange, Cri du Chat, Fragile X, Lowe, Prader-Willi and Smith Magenis syndromes and a group of individuals with intellectual disability of heterogeneous etiologies. Comparing these genetic disorders, revealed they differ in their profile of RRBI. In Fragile X syndrome, hand stereotypies, lining up objects, restricted conversation, preference for routine and echolalia were the most prevalent forms of repetitive behavior. In Prader-Willi syndrome (PWS), hoarding and a preference for routine were more prevalent than other stereotyped behaviors. Attachment to objects was highly prevalent within the Cri du Chat syndrome and attachment to people was highly prevalent within the Smith-Magenis syndrome. Individuals with Angelman syndrome showed more heterogenicity in their RRBI’s profile (Moss, Oliver, Arron, Burbidge, & Berg, 2009).These findings may suggest that in these known genetic disorders, there is a connection between the specific genetic abnormality and the clinical manifestations of RRBI’s. The results support the claim that there is extreme heterogeneity of repetitive behavior across genetic syndromes, highlighting syndrome-specific profiles. A special focus in research was on PWS, a genetic disorder caused by the absence of paternally inherited genes in the 15q11-q13 region, as many individuals with PWS are diagnosed with ASD and high levels of RRBI’s were also described (Bittel & Butler, 2005; E. M. Dykens, Cassidy, & King, 1999; E. Dykens & Shah, 2003; M. Lewis & Kim, 2009b; State & Dykens, 2000; Veltman, Craig, & Bolton, 2005).
Furthermore, in a study of more than 3000 twin pairs, it was found that RRBI’s was both highly heritable and showed no shared environmental influence in univariate models (Ronald et al., 2006; Ronald, Happé, & Plomin, 2005), thereby adding reliability to the hypothesis that RRBI’s etiology has a strong genetic basis.
As of today, the efforts to discover the genetic basis of ASD and its core symptoms, including RRBI’s, are ongoing. Studies are being conducted worldwide in the hope of discovering new risk genes for ASD, in order to understand the impaired genetic mechanisms underlying this disorder and to find tailored treatments for ASD core symptoms.
Molecular (Neurotransmitters) Abnormalities
The last theory that will be presented in this chapter regarding the neurobiological basis of RRBI’s in ASD implies that these repetitive behaviors are a result of an imbalance in neurotransmission systems.
There are data showing that dopamine has a role in RRBI’s. First of all, dopamine is a principal player in the nigrostriatal dopamine pathway. As was mentioned earlier in this chapter, anatomical and physiological changes in the basal ganglia structures are considered by many to be a plausible cause for RRBI’s in ASD (Mark H. Lewis & Bodfish, 1998; Scheel-Krüger et al., 1978; Scheel-Kruger et al., 1980). Additionally, stereotypic behaviors can be induced in many mammals, humans among them, by direct and indirect dopamine agonists (Mark H. Lewis & Baumeister, 1982; Mark H. Lewis & Bodfish, 1998). Early works in animal models also exhibit the importance of dopaminergic activity in the basal ganglia for RRBI’s, as dopamine or dopamine agonists can cause RRBI’s (Ernst & Smelik, 1966; M. Lewis & Kim, 2009a). Furthermore, it was demonstrated that inhibiting dopamine synthesis resulted in a reduction in RRBI’s, while treating animals with a dopamine precursor caused increased RRBI’s patterns (Kennes, Odberg, & de Rycke, 1988; Mark H. Lewis & Bodfish, 1998). However, a clinical study on individuals with intellectual disability who also had RRBI’s revealed they had low plasma levels of homovanillic acid (HVA), a dopamine metabolite (M. H. Lewis et al., 1996; Mark H. Lewis & Bodfish, 1998). Later works indicated that having mutations in the dopamine signaling pathway was correlated with having an ASD diagnosis (Hamilton et al., 2014; Nguyen et al., 2014), and also with a specific type of RRBI’s (“insistence on sameness”) in ASD as measured by the ADI-R (Staal, De Krom, & De Jonge, 2012).
Gamma-aminobutyric acid (GABA) signaling pathways may also play a major role in the mechanism causing RRBI’s in ASD. Many researchers report a correlation between changes in components of the GABA signaling pathways and having an ASD diagnosis (Barnby et al., 2005; Coghlan, Horder, Inkster, Mendez, & Declan, 2012; Collins et al., 2006; Fatemi, Reutiman, Folsom, & Thoras, 2009; M. Lewis & Kim, 2009a; Ma et al., 2005). In addition, like dopamine, GABA has a role in the nigrostriatal dopamine system, which was mentioned in this chapter several times as a suggested mechanism that causes RRBI’s in ASD (Mark H. Lewis & Baumeister, 1982). Moreover, an animal study demonstrated that dysfunction of the MECP2 gene (a mutation in this gene may cause Rett syndrome) in GABAergic neurons can harm its function, and contribute to numerous neuropsychiatric phenotypes and symptoms, RRBI’s among them (Chao et al., 2011). In an MRS study on 18 children with primary complex motor stereotypies (CMS) and 24 TD individuals, it was demonstrated that children with CMS had lower levels of GABA in the anterior cingulate cortex (ACC) and in the striatum. Furthermore, within the CMS group, a reduced GABA/creatinine ratio in the ACC was significantly associated with greater severity of motor stereotypies (Harris et al., 2016). Moreover, in two mouse models for ASD, improvement in RRBI’s was demonstrated after treatment with GABAB receptor agonists (Silverman et al., 2015).
In addition to dopamine and GABA, there is a claim that serotonin (5-HT) is also related to RRBI’s in ASD, since 5-HT axons project from the raphe nuclei to basal ganglia structures, thereby creating dopamine-5-HT interactions (Mark H. Lewis & Bodfish, 1998). Like other neurotransmitters, genetic changes in genes involved in the 5-HT signaling were implicated in ASD (Chakrabotri et al., 2016; R. M. Smith, Banks, Hansen, Sadee, & Herman, 2014; Yonan et al., 2003). In an early work in this field, it was found that 6 out of 23 participants with ASD had higher blood 5-HT levels, compared with individuals with typical development and those with intellectual disability without autism (Schain & Freedman, 1961). Furthermore, some consider serotonin reuptake inhibitors (SSRIs) to be an effective treatment for RRBI’s (Sutcliffe et al., 2005). Additionally, reduction of central nervous system serotonin, induced by acute tryptophan depletion, caused a worsening of stereotyped behavior (Cook & Leventhal, 1996). However, results of a systematic review conclude that although SSRIs are sometimes given to reduce obsessive-compulsive behaviors, there is no evidence to support the use of SSRIs to treat autism in children, and there is limited evidence to suggest the effectiveness of SSRIs in adults with autism (Williams, Brignell, Randall, Silove, & Hazell, 2013).
Alongside the other aforementioned neurotransmitters, the glutamatergic system, which is a primary excitatory system involved in cognitive functions such as learning and memory (Jamain et al., 2002), also plays a key role in ASD pathogenesis (Yang & Chang, 2014). A correlation was found between genetic abnormalities in the glutamatergic system’s components and an ASD diagnosis (Jamain et al., 2002; Nguyen et al., 2014). Moreover, similarly to GABA, the dopaminergic system can modulate glutamatergic signaling (Li, Wang, & Gao, 2012; Nguyen et al., 2014), therefore it is probable that disturbances in glutamate signaling are also a part of the etiology of RRBI’s.
In conclusion, many neurotransmission systems are implicated in ASD, and may be a part of the etiology and pathophysiology of RRBI’s in ASD. However, the data from clinical studies on individuals with ASD in this field are rather sparse, and there is a need for more clinical evidence in order to support these theories.
Summary
Currently, the etiology of ASD in general, and of its specific core domains, the social-communication impairments and RRBI’s in particular, is not fully understood. Hence, suggested mechanisms regarding the pathophysiology of RRBI’s in ASD are copious, and range from psychological theories to genetic, anatomical, functional, and metabolic abnormalities. Considering the growing impact of the field of genetics on diagnosis of complex disorders in general, and of ASD in particular, it is likely that further genetic advancement will aid in uncovering the neurobiological basis of RRBI’s in ASD. The understanding of the underlying mechanisms of RRBI’s may lead to the development of personalized biological treatments to improve these restricted and repetitive behaviors that negatively impact the quality of life in ASD.
References
Abbott, A. E., Linke, A. C., Nair, A., Jahedi, A., Alba, L. A., Keown, C. L., et al. (2018). Repetitive behaviors in autism are linked to imbalance of corticostriatal connectivity: A functional connectivity MRI study. Social Cognitive and Affective Neuroscience, 13(1), 32–42. https://doi.org/10.1093/scan/nsx129.
Abrahams, B. S., & Geschwind, D. H. (2009). Advances in autism genetics: On the threshold of a new neurobiology. Nature Reviews Genettics, 9(5), 341–355. https://doi.org/10.1038/nrg2346.Advances.
Albin, R. L., Young, A. B., Penney, J. B., Roger, L. A., & Young, B. B. (1989). The functional anatomy of basal ganglia disorders. Trends in Neurosciences, 12(10), 366–375.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Retrieved from https://www.autismspeaks.org/what-autism/diagnosis/dsm-5-diagnostic-criteria.
Anagnostou, E., Soorya, L., Chaplin, W., Bartz, J. A., Halpern, D., Wasserman, S., et al. (2012). Intranasal oxytocin versus placebo in the treatment of adults with autism spectrum disorders: A randomized controlled trial. Molecular Autism, 3(1), 16. https://doi.org/10.1186/2040-2392-3-16.
Anthony, B., Luthert, P., Bolton, P., Le Couteur, A., Rutter, M., & Harding, B. (1989). Autism and Megalencephaly. The Lancet, 341, 1225–1226.
Barnby, G., Abbott, A., Sykes, N., Morris, A., Weeks, D. E., Mott, R., et al. (2005). Candidate-gene screening and association analysis at the autism-susceptibility locus on chromosome 16p: Evidence of association at GRIN2A and ABAT. American Journal of Human Genetics, 76(6), 950–966.
Baron-Cohen, S. (1989). Do autistic children have obsessions and compulsions? British Journal of Clinical Psycology, 28(3), 193–200.
Bishop, S. L., Hus, V., Duncan, A., Huerta, M., Gotham, K., Pickles, A., et al. (2013). Subcategories of restricted and repetitive behaviors in children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(6), 1287–1297. https://doi.org/10.1007/s10803-012-1671-0.
Bishop, S. L., Richler, J., & Lord, C. (2006). Association between restricted and repetitive behaviors and nonverbal IQ in children with Autism Spectrum Disorders. Child Neuropsychology, 12(4–5), 247–267. https://doi.org/10.1080/09297040600630288.
Bittel, D. C., & Butler, M. G. (2005). Prader – Willi syndrome: Clinical genetics, cytogenetics and molecular biology. Expert Reviews in Molecular Medicine, 7(14), 1–20. https://doi.org/10.1017/S1462399405009531.
Bodfish, J. W., Symons, F. J., Parker, D. E., & Lewis, M. H. (2000). Varieties of repetitive behaviour in autism: Comparison to mental retardation. Journal of Autism and Developmental Disorders, 30(3), 237–243. https://doi.org/10.1023/A:1005596502855.
Boyer, P., & Lie’nard, P. (2006). Why ritualized behavior? Precaution Systems and action parsing in developmental, pathological and cultural rituals. Behavioral and Brain Science, 29, 595–650. https://doi.org/10.1017/S0140525X06009332.
Buchsbaum, M. S., Hazlett, E. A., Ph, D., Licalzi, E. M., Cartwright, C., & Hollander, E. (2006). Volumetric analysis and three-dimensional glucose metabolic mapping of the striatum and thalamus in patients with autism spectrum disorders. American Journal of Psychiatry, 163(7), 1252–1263.
Cantor, R. M., Navarro, L., Won, H., Walker, R. L., Lowe, J. K., & Geschwind, D. H. (2017). ASD restricted and repetitive behaviors associated at 17q21.33: Genes prioritized by expression in fetal brains. Molecular Psychiatry, 00(September 2016), 1–8. https://doi.org/10.1038/mp.2017.114.
Caravaggio, F., Nakajima, S., Plitman, E., Gerretsen, P., Chung, J. K., Iwata, Y., & Graff-Guerrero, A. (2016). The effect of striatal dopamine depletion on striatal and cortical glutamate: A mini-review. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 65, 49–53. https://doi.org/10.1016/j.pnpbp.2015.08.013.
Chakrabotri, B., Verma, D., Karmakar, A., Jaiswal, P., Sanyal, A., Paul, D., et al. (2016). Genetic variants of MAOB affect serotonin level and specific behavioral attributes to increase autism spectrum disorder (ASD) susceptibility in males. Progress in Neuropsychopharmacology and Biological Psychiatry, 71, 123–136. https://doi.org/10.1016/j.pnpbp.2016.07.001.
Chao, H., Chen, H., Samaco, R. C., Xue, M., Yoo, J., Neul, J. L., et al. (2011). GABAergic dysfunction mediates autism-like stereotypies and Rett syndrome phenotypes. Nature, 468(7321), 263–269. https://doi.org/10.1038/nature09582.GABAergic.
Coghlan, S., Horder, J., Inkster, B., Mendez, M. A., & Declan, G. (2012). GABA system dysfunction in autism and related disorders: From synapse to symptoms. Neuroscience & Biobehavioral Reviews, 36(9), 2044–2055. https://doi.org/10.1016/j.neubiorev.2012.07.005.GABA.
Collins, A. L., Ma, D., Whitehead, P. L., Martin, E. R., Wright, H. H., Abramson, R. K., et al. (2006). Investigation of autism and GABA receptor subunit genes in multiple ethnic groups. Neurogenetics, 7(3), 167–174. https://doi.org/10.1007/s10048-006-0045-1.
Cook, E. H., & Leventhal, B. L. (1996). The serotonin system in autism. Current Opinion in Pediatrics, 8(4), 348–354. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9053096.
Dykens, E. M., Cassidy, S. B., & King, B. H. (1999). Maladaptive behavior differences in Prader-Willi syndrome due to parental deletion versus maternal uniparental disomy. American Journal on Mental Retardation, 104(1), 67–77.
Dykens, E., & Shah, B. (2003). Psychiatric disorders in Prader-Willi syndrome epidemiology and management. CNS Drugs, 17(3), 167–178.
Ernst, A. M., & Smelik, P. G. (1966). Site of action of dopamine and apomorphine on compulsive gnawing behaviour in rats. Experientia, 22(12), 837–838. https://doi.org/10.1007/BF01897450.
Estes, A., Shaw, D. W. W., Sparks, B. F., Friedman, S., Giedd, J. N., Dawson, G., et al. (2012). Basal ganglia morphometry and repetitive behavior in young children with autism spectrum disorder. Autism Research, 4(3), 212–220. https://doi.org/10.1002/aur.193.Basal.
Evans, D. W. (2017). Relationship between repetitive behaviour and fear across normative development, autism spectrum disorder, and down syndrome. Autism Research, 10(3), 502–507. https://doi.org/10.1002/aur.1674.
Evans, D. W., Leckmn, J. F., Carter, A., Raznick, J. S., Henshaw, D., King, R. A., & Pauls, D. (1997). Rituals, habit and perfectionism: The prevalence and development of compulsive-like behavior in normal young children. Child Development, 68(1), 58–68.
Fatemi, S. H., Reutiman, T. T., Folsom, T. D., & Thoras, P. D. (2009). GABA A receptor downregulation in brains of subjects with autism. Journal of Autism and Developmental Disorders, 39, 223–230. https://doi.org/10.1007/s10803-008-0646-7.
Francis, S. M., Kim, S., Kistner-griffin, E., Guter, S., Cook, E. H., Jacob, S., & Ebstein, R. P. (2016). ASD and genetic associations with receptors for oxytocin and vasopressin—AVPR1A, AVPR1B, and OXTR. Frontiers in Neuroscience, 10(November), 1–10. https://doi.org/10.3389/fnins.2016.00516.
Francis, S. M., Kistner-griffin, E., Yan, Z., Guter, S., Cook, E. H., & Jacob, S. (2016). Variants in adjacent oxytocin/vasopressin gene region and associations with ASD diagnosis and other autism related endophenotypes. Frontiers in Neuroscience, 10(May), 195. https://doi.org/10.3389/fnins.2016.00195.
Frith, U., & Happe, F. (1994). Autism: beyond “ theory of mind”. Cognition, 50, 115–132.
Gaffney, G. R., Kuperman, S., Tsai, L. Y., & Minchin, S. (1989). Forebrain structure in infantile autism. Journal of the American Academy of Child and Adolescent Psychiatry, 28(4), 534–537. https://doi.org/10.1097/00004583-198907000-00011.
Geschwind, D. H. (2011). Genetics of autism spectrum disorders. Trends in Cognitive Sciences, 15(9), 409–416. https://doi.org/10.1016/j.tics.2011.07.003.
Goldman, S., O’Briend, L. M., Filipekf, P. A., Rapina, I., & Herbertg, M. R. (2013). Motor stereotypies and volumetric brain alterations in children with Autistic Disorder. Research in Autism Spectrum Disorders, 7(1), 82–92. https://doi.org/10.1016/j.rasd.2012.07.005.Motor.
Graybiel, A. M., & Rauch, S. L. (2000). Toward a neurobiology of obsessive-compulsive disorder. Neuron, 28(4), 343–347.
Hall, S., Thorns, T., & Oliver, C. (2003). Structural and environmental characteristics of stereotyped behaviors. American Journal of Mental Retardation, 108(6), 391–402.
Hamilton, P. J., Campbell, N. G., Sharma, S., Erreger, K., Herborg Hansen, F., Saunders, C., et al. (2014). De novo mutation in the dopamine transporter gene associates dopamine dysfunction with autism spectrum disorder Peter. Molecular Psychiatry, 18(12), 1315–1323. https://doi.org/10.1038/mp.2013.102.De.
Harris, A. D., Singer, H. S., Horska, A., Kline, T., Ryan, M., Edden, R. A., & Mahone, E. M. (2016). GABA and glutamate in children with primary complex motor stereotypies: A1H MRS study at 7T. American Journal of Neuroradiology, 37(3), 552–557. https://doi.org/10.3174/ajnr.A4547.GABA.
Hollander, E., Anagnostou, E., Chaplin, W., Esposito, K., Haznedar, M. M., Licalzi, E., … Buchsbaum, M. (2005). Striatal volume on magnetic resonance imaging and repetitive behaviors in autism. Biological Psychiatry, 58(3), 226–232. https://doi.org/10.1016/j.biopsych.2005.03.040
Hutt, B. Y. C., & Hutt, S. J. (1965). Effects of environmental complexity on stereoptyped behaviours of children. Animal Behaviour, 13(1), 1–4.
Hutt, C., Hutt, S. J., Lee, D., & Ounsted, C. (1964). Arousal and childhood autism. Nature, 204(4961), 908–909.
Jamain, S., Betancur, C., Quach, H., Philippe, A., Fellous, M., Giros, B., et al. (2002). Linkage and association of the glutamate receptor 6 gene with autism. Molecular Psychiatry, 7(3), 302–310. https://doi.org/10.1038/sj/mp/4000979.
Jiujias, M., Kelley, E., Hall, L., & Kelley, E. (2017). Restricted, repetitive behaviors in autism spectrum disorder and obsessive – compulsive disorder: a comparative review. Child Psychiatry and Human Development, 48(6), 944–959. https://doi.org/10.1007/s10578-017-0717-0.
Joyce, C., Honey, E., Leekam, S. R., Barrett, S. L., Rodgers, J., & Joyce, C. (2017). Anxiety, intolerance of uncertainty and restricted and repetitive behaviour: Insights directly from young people with ASD. Journal of Autism and Developmental Disorders, 47(12), 3789–3802. https://doi.org/10.1007/s10803-017-3027-2.
Just, M. A., Cherkassky, V. L., Keller, T. A., & Minshew, N. J. (2004). Cortical activation and synchronization during sentence comprehension in high-functioning autism: Evidence of underconnectivity. Brain, 127, 1811–1821. https://doi.org/10.1093/brain/awh199.
Kennes, F. O., Odberg, Y. B., & de Rycke, P. H. (1988). Changes in naxolone and heloperidol effects during the development of captivity-induced jumping stereotypy in bank voles. European Journal of Pharmacology, 153(1), 19–24.
Kim, S. H., & Lord, C. (2010). Restricted and repetitive behaviors in toddlers and preschoolers with autism spectrum disorders based on the Autism Diagnostic Observation Schedule (ADOS). Autism Research, 3(4), 162–173. https://doi.org/10.1002/aur.142.
Lainhart, J. E., Piven, J., Wzorek, M., Ph, D., Landa, R., Ph, D., et al. (1997). Macrocephaly in children and adults with autism. Journal of the American Academy of Child and Adolescent Psychiatry, 36(2), 282–290. https://doi.org/10.1097/00004583-199702000-00019.
Langen, M., Durston, S., Kas, M. J. H., Van Engeland, H., & Staal, W. G. (2011). The neurobiology of repetitive behavior … and men. Neuroscience and Biobehavioral Reviews, 35(1), 356–365. https://doi.org/10.1016/j.neubiorev.2010.02.005.
Langen, M., Durston, S., Staal, W. G., Palmen, S. J. M. C., & Van Engeland, H. (2007). Caudate nucleus is enlarged in high-functioning medication-naive subjects with autism. Biological Psychiatry, 62(3), 262–266. https://doi.org/10.1016/j.biopsych.2006.09.040.
Lewis, M., & Kim, S.-J. (2009a). The pathophysiology of restricted repetitive behavior. Journal of Neurodevelopmental Disorders, 1(2), 114–132. https://doi.org/10.1007/s11689-009-9019-6.
Lewis, M., & Kim, S. (2009b). The pathophysiology of restricted repetitive behavior. Journal of Neurodevelopmental Disorders, 1(June), 114–132. https://doi.org/10.1007/s11689-009-9019-6.
Lewis, M. H., Bodfish, J. W., Powell, S. B., Wiest, K., Darling, M., & Golden, R. N. (1996). Plasma HVA in adults with mental retardation and stereotyped behavior: biochemical evidence for a dopamine deficiency model. American Journal of Mental Retardation: AJMR, 100(4), 413–418. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8718995.
Lewis, M. H., & Baumeister, A. A. (1982). Stereotyped mannerisms in mentally retarded persons: Animal models and theoretical analyses. International Review of Research in Mental Retardation, 11, 123–161.
Lewis, M. H., & Bodfish, J. W. (1998). Repetitive behavior disorders in autism. Mental Retardation and Developmental Disabilities Research Reviews, 4, 80–89.
Li, Y.-C., Wang, M.-J., & Gao, W.-J. (2012). Hyperdopaminergic modulation of inhibitory transmission is dependent on GSK-3β signaling-mediated trafficking of GABAA receptors. Journal of Neurochemistry, 122(2), 308–320. https://doi.org/10.1111/j.1471-4159.2012.07790.x.
Lord, C., Risi, S., Lambrecht, L., Cook, E. H. J., Leventhal, B. L., DiLavore, P. C., et al. (2000). The Autism Diagnostic Schedule – Generic: A standard measures of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. https://doi.org/10.1023/A:1005592401947.
Lord, C., Rutter, M., & LeCouteur, A. (1994). Autism diagnostic interview: A revised version of a diagnostic interview for caregivers of individual s with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders, 24(5), 659–685. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=epref&AN=JADD.BD.FEI.LORD.ADIRVD&site=ehost-live.
Lovaas, I., Newsome, C., & Hickman, C. (1987). Self-stimulatory behavior and perceptual reinforcement. Journal of Applied Behavior Analysis, 20(1), 45–68.
Ma, D. Q., Whitehead, P. L., Menold, M. M., Martin, E. R., Mei, H., Ritchie, M. D., et al. (2005). Identification of significant association and gene-gene interaction of GABA receptor subunit genes in autism. The American Journal of Human Genetics, 77(3), 377–388.
Monk, C. S., Peltier, S. J., Wiggins, J. L., Weng, S. J., Carrasco, M., Risi, S., & Lord, C. (2009). Abnormalities of intrinsic functional connectivity in autism spectrum disorders. NeuroImage, 47(2), 764–772. https://doi.org/10.1016/j.neuroimage.2009.04.069.
Moss, J., Oliver, C., Arron, K., Burbidge, C., & Berg, K. (2009). The prevalence and phenomenology of repetitive behavior in genetic syndromes. Journal of Autism and Developmental Disorders, 39(4), 572–588. https://doi.org/10.1007/s10803-008-0655-6.
Mostert-Kerckhoffs, M. A. L., Staal, W. G., & Houben, R. H. (2015). Stop and change: Inhibition and flexibility skills are related to repetitive behavior in children and young adults with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45(10), 3148–3158. https://doi.org/10.1007/s10803-015-2473-y.
Muhle, R. A., Reed, H. E., Stratigos, K. A., & Veenstra-vanderweele, J. (2018). The emerging clinical neuroscience of autism spectrum disorder A review. JAMA Psychiatry, 75(5), 514–523. https://doi.org/10.1001/jamapsychiatry.2017.4685.
Newschaffer, C. J., Denckla, Æ. M. B., Landa, R., & Mostofsky, Æ. S. H. (2006). Motor signs distinguish children with high functioning autism and Asperger’s syndrome from controls. Journal of Autism Developmentall Disorder, 36(1), 613–621. https://doi.org/10.1007/s10803-006-0109-y.
Nguyen, M., Roth, A., Kyzar, E. J., Poudel, M. K., Wong, K., Stewart, A. M., & Kalueff, A. V. (2014). Decoding the contribution of dopaminergic genes and pathways to autism spectrum disorder (ASD). Neurochemistry International, 66(1), 15–26. https://doi.org/10.1016/j.neuint.2014.01.002.
Nomi, J. S., & Uddin, L. Q. (2015). Developmental changes in large-scale network connectivity in autism. NeuroImage: Clinical, 7, 732–741. https://doi.org/10.1016/j.nicl.2015.02.024.
Ramaswami, G., & Geschwind, D. H. (2018). Genetics of autism spectrum disorder. In Handbook of clinical neurology (Vol. 147, 1st ed.). https://doi.org/10.1016/B978-0-444-63233-3.00021-X.
Ranson, B. J., Piven, J., Lonnie, L., Vest, C., Mohamed, S., Bailey, J., et al. (1999). An MRI study of the basal ganglia in autism. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 23(Apa 1995), 613–624.
Richler, J., Huerta, M., Bishop, S. L., & Lord, C. (2010). Developmental trajectories of restricted and repetitive behaviors and interests in children with autism spectrum disorders. Development and Psychopathology, 22(1), 55–69. https://doi.org/10.1017/S0954579409990265.
Rojas, D. C., Peterson, E., Winterrowd, E., Reite, M. L., Rogers, S. J., & Tregellas, J. R. (2006). Regional gray matter volumetric changes in autism associated with social and repetitive behavior symptoms. BMC Psychiatry, 6(1), 56. https://doi.org/10.1186/1471-244X-6-56.
Ronald, A., Happ, F., Bolton, P., Sych, F. R. C. P., Butcher, L. E. E. M., Price, T. S., & Wheelwright, S. (2006). Genetic heterogeneity between the three components of the autism spectrum: A twin study. Journal of the American Academy of Child & Adolescent Psychiatry, 45(6), 691–699. https://doi.org/10.1097/01.chi.0000215325.13058.9d.
Ronald, A., Happé, F., & Plomin, R. (2005). The genetic relationship between individual differences in social and nonsocial behaviours characteristic of autism. Developmental Science, 8(5), 444–458. https://doi.org/10.1111/j.1467-7687.2005.00433.x.
Rosenthal, M., Wallace, G. L., Lawson, R., Wills, M. C., Dixon, E., Yerys, B. E., & Kenworthy, L. (2013). Impairments in real-world executive function increase from childhood to adolescence in autism spectrum disorders. Neuropsychology, 27(1), 13–18. https://doi.org/10.1037/a0031299.
Schain, R. J., & Freedman, D. X. (1961). Studies on 5-bydroxyindole metabolism in autistic and other mentally retarded children. The Journal of Pediatrics, 58(3), 315–320.
Scheel-Krüger, J., Arnt, J., Braestrup, C., Christensen, A. V., Cools, A. R., & Magelund, G. (1978). GABA-dopamine interaction in substantia nigra and nucleus accumbens -relevance to behavioral stimulation and stereotyped behavior. Advances in Biochemical Psychopharmacology, 19, 343–346. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/567933.
Scheel-Kruger, J., Arnt, J., Magelund, G., Olianas, M., Przewlocka, B., & Christensen, A. V. (1980). Behavioural functions of GABA in basal ganglia and limbic system. Brain Research Bulletin, 5(2), 261–267.
Schmitt, L. M., White, S. P., Cook, E. H., Sweeney, J. A., & Mosconi, M. W. (2017). Cognitive mechanisms of inhibitory control deficits in autism spectrum disorder. Journal of Child Psychology and Psychiatry, 59(5), 586–595. https://doi.org/10.1111/jcpp.12837.
Shih, P., Shen, M., Öttl, B., Keehn, B., Gaffrey, M. S., & Müller, R. A. (2010). Atypical network connectivity for imitation in autism spectrum disorder. Neuropsychologia, 48(10), 2931–2939. https://doi.org/10.1016/j.neuropsychologia.2010.05.035.
Silverman, J. L., Pride, M. C., Hayes, J. E., Puhger, K. R., Butler-struben, H. M., Baker, S., & Crawley, J. N. (2015). GABA B receptor agonist R-baclofen reverses social deficits and reduces repetitive behavior in two mouse models of autism. Neuropsychopharmacology, 40(9), 2228–2239. https://doi.org/10.1038/npp.2015.66.
Sloman, K. N., LaRue, R. H., Weiss, M. J., & Hansford, A. S. (2013). Best practices in the assessment and treatment of stereotypical behaviour in individuals with autism. In J. M. Zachor & A. Ditza (Eds.), Understanding autism (pp. 29–37). Nova Science Publishers.
Smith, R. M., Banks, W., Hansen, E., Sadee, W., & Herman, G. E. (2014). Family-based clinical associations and functional characterization of the serotonin 2A receptor gene (HTR2A) in autism spectrum disorder. Autism Research, 7(4), 459–467. https://doi.org/10.1002/aur.1383.
Smith, Y., Bevan, M. D., Shink, E., & Bolam, J. P. (1998). Microcircuitry of the direct and indirect pathways of the basal ganglia. Neuroscience, 86(2), 353–387.
Staal, W. G., De Krom, M., & De Jonge, M. V. (2012). Brief report: The dopamine-3-receptor gene (DRD3) is associated with specific repetitive behavior in autism spectrum disorder (ASD). Journal of Autism and Developmental Disorders, 42(5), 885–888. https://doi.org/10.1007/s10803-011-1312-z.
State, M. W., & Dykens, E. M. (2000). Genetics of childhood disorders: XV. Prader-Willi syndrome: Genes, brain, and behavior. Developmental Neurobiology, 39(6), 797–800. https://doi.org/10.1097/00004583-200006000-00021.
Stocco, A., Lebiere, C., & Anderson, J. R. (2011). Conditional routing of information to the cortex: A model of the basal Ganglia’s role in cognitive coordination. Psychologic Review, 117(2), 541–574. https://doi.org/10.1037/a0019077.Conditional.
Stratis, E. A., & Lecavalier, L. (2013). Restricted and repetitive behaviors and psychiatric symptoms in youth with autism spectrum disorders. Research in Autism Spectrum Disorders, 7(6), 757–766. https://doi.org/10.1016/j.rasd.2013.02.017.
Street, D. (1994). The psychology of perservative and stereotyped behaviour. Progress in Neurobiology, 44(2), 221–231.
Sullivan, J., Rodgers, J., Lidstone, J., Uljarevic, M., Mcconachie, H., Freeston, M., et al. (2014). Research in Autism Spectrum Disorders Relations among restricted and repetitive behaviors, anxiety and sensory features in children with autism spectrum disorders. Research in Autism Spectrum Disorders, 8(2), 82–92. https://doi.org/10.1016/j.rasd.2013.10.001.
Supekar, K., & Menon, V. (2015). Sex differences in structural organization of motor systems and their dissociable links with repetitive/restricted behaviors in children with autism. Molecular Autism, 6(50). https://doi.org/10.1186/s13229-015-0042-z.
Sutcliffe, J. S., Delahanty, R. J., Prasad, H. C., Mccauley, J. L., Han, Q., Jiang, L., et al. (2005). Allelic heterogeneity at the serotonin transporter locus (SLC6A4) confers susceptibility to autism and rigid-compulsive behaviors. American Journal of Human Genetics, 77, 265–279.
Tao, Y., Gao, H., Ackerman, B., Guo, W., Saffen, D., & Shugart, Y. Y. (2016). Evidence for contribution of common genetic variants within chromosome 8p21.2-8p21.1 to restricted and repetitive behaviors in autism spectrum disorders. BMC Genomics, 17(163), 1–15. https://doi.org/10.1186/s12864-016-2475-y.
Turner, M. (1999). Repetitive behaviour in autism: A review of psychological research. Journal of Child Psychology and Psychiatry, 40(6), 839–849.
Uljarevi, M., Evans, D. W., Alvares, G. A., & Whitehouse, A. J. O. (2016). Short report: Relationship between restricted and repetitive behaviours in children with autism spectrum disorder and their parents. Molecular Autism, 7(29), 1–5. https://doi.org/10.1186/s13229-016-0091-y.
Veltman, M. W. M., Craig, E. E., & Bolton, P. F. (2005). Autism spectrum disorders in Prader – Willi and Angelman syndromes: A systematic review. Psychiatric Genetics, 15(4), 243–254.
Voelbel, G. T., Bates, M. E., Buckman, J. F., Pandina, G., & Hendren, R. L. (2006). Caudate nucleus volume and cognitive performance: Are they related in childhood psychopathology? Biological Psychiatry, 60(9), 942–950. https://doi.org/10.1016/j.biopsych.2006.03.071.
Williams, K., Brignell, A., Randall, M., Silove, N., & Hazell, P. (2013). Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD) (Review). Cochrane Database of Systematic Reviews, ((8), CD004677. https://doi.org/10.1002/14651858.CD004677.pub3. https://www.cochranelibrary.com/.
Yang, P., & Chang, C.-L. (2014). Glutamate-mediated signaling and autism spectrum disorders: Emerging treatment targets. Current Pharmaceutical Design, 20(32), 5186–5193. https://doi.org/10.2174/1381612819666140110120725.
Yonan, A. L., Alarco, M., Cheng, R., Magnusson, P. K. E., Spence, S. J., Palmer, A. A., et al. (2003). A genomewide screen of 345 families for autism-susceptibility loci. American Journal of Human Genetics, 73(4), 886–897.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Poleg, S., Zachor, D.A. (2021). Neurological Mechanisms Underlying Repetitive and Restricted Behaviors in Autism Spectrum Disorders. In: Gal, E., Yirmiya, N. (eds) Repetitive and Restricted Behaviors and Interests in Autism Spectrum Disorders. Autism and Child Psychopathology Series. Springer, Cham. https://doi.org/10.1007/978-3-030-66445-9_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-66445-9_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-66444-2
Online ISBN: 978-3-030-66445-9
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)