Abstract
Contemporary ceramic has superior tribological properties that translate to minimal osteolysis and extended prosthesis survival. It is more biocompatible than metal alloys. Although ceramic-on-ceramic (CoC) bearings represent an optimal choice for total hip arthroplasty (THA), ceramic fracture and noise are major concerns of CoC THA.
In this chapter, we review the evolution of ceramic bearings and updated information on the mechanism and prevention of ceramic fracture and squeaking.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Total hip arthroplasty (THA) is the most successful procedure to treat end-stage osteoarthritis of the hip. The use of contemporary bearings, highly cross-linked polyethylene, metal-on-metal (MoM), and ceramic-on-ceramic (CoC) bearings, which were expected to minimize wear and subsequent osteolysis, enabled surgeons to perform THA in young and active patients [1,2,3,4]. Among the contemporary bearings, MoM bearings were almost abandoned due to serious adverse local or systemic reactions [5, 6]. The CoC articulations offer superior wear properties and biocompatibility [7].
2 Evolution of Ceramic-on-Ceramic Bearings
In the 1970s, the first-generation CoC bearing was developed in France and Germany. The results of THA using the early-generation ceramic bearings were not satisfactory due to insufficient fixation of the acetabular cup and excessive wear [8]. The lack of bone-ingrown stability of the mono-block cup design and large grain size of the ceramic were thought to be the causes of failure [9,10,11].
To overcome these problems, third-generation alumina ceramic was developed, and a taper fixation of the ceramic liner in a metal-backed component was adopted in 1995. The mechanical properties of ceramic materials have been improved by hot isostatic pressing, laser marking, and nondestructive proof-testing, which translated to reduced grain size and increased strength of the ceramic composite [12]. Since then, alumina CoC bearings (Biolox Forte; CeramTec, Plochingen, Germany) were popularly used for THA of young patients [13]. This design has generated excellent survival and patient satisfaction compared to conventional metal-on-polyethylene bearing. However, ceramic fracture and squeaking appeared as major concerns of the third-generation alumina ceramic bearings [14].
3 Ceramic Head Fracture
A 28 mm short-neck head of pure alumina ceramic has a high risk for fracture. In 2008, Koo et al. reported five head fractures (1.4%) among 367 cementless THAs with the use of 28 mm alumina CoC bearing [15]. All fractures occurred in short-neck heads and involved the circumferential portion along the inner edge of the head bore (Fig. 13.1). The same finding was reported by registry studies. In a UK registry data involving 222,852 THAs with the use of contemporary CoC bearings, the use of 28 mm head was the highest risk factor for ceramic fracture (0.382%) [2]. In the Danish Hip Arthroplasty Registry data, ceramic component fracture occurred in 0.35% and all of them occurred in 28 mm femoral heads [4].
In 2004, Delta ceramic (Biolox Delta; CeramTec), a composite of 82% alumina, 17% zirconia, and 1% mixed oxides, was developed to reduce the rate of ceramic fracture [16]. This newest ceramic composite has a smaller grain size (less than 0.8 μm), higher bending strength, and increased toughness than previous alumina ceramic [17]. The strong toughness of Delta ceramic allowed the use of larger femoral heads and thinner liners, which increased the range of motion and reduced the rate of dislocation.
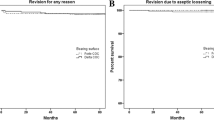
Recently, midterm results of THA with the use of Delta ceramic bearings have been reported [1, 3, 18,19,20,21,22]. The risk of head fracture has been reduced with the use of Delta ceramic (Table 13.1).
No fracture was seen in the Delta ceramic heads in the UK Registry data, and only one fracture was noted in 28 mm Delta heads in the Danish Registry data [2, 4].
4 Ceramic Liner Fracture
Although the use of Delta ceramic markedly reduced the incidence of ceramic head fracture, it did not significantly reduce the incidence of liner fracture. The overall survivorship of ceramic liners was similar between alumina and Delta ceramics. In the registry data from the UK, the fracture incidence was 0.112% (35/31258) in alumina liners and 0.126% (101/80170) in Delta liners [2]. The incidence of ceramic liner fracture from single-cohort studies ranged from 0 to 1.2% in alumina liners and from 0 to 0.8% in Delta liners (Table 13.1).
Incomplete/asymmetric seating of the ceramic liner into the metal shell and dent of metal shell is a possible cause for liner fracture [23, 24]. Surgeons should be cautious to achieve firm symmetric seating of the liner along the Morse taper inside the metal cup [14, 22, 25, 26]. Heavy body weight has been reported as a risk for the liner fracture. The risk may be attributable to the difficulty of liner insertion during the operation of patients with high body mass index [22, 27, 28].
The use of a multi-bearing metal shell, which can be coupled with hard liners as well as polyethylene liner, appeared as a risk factor for malseating of the ceramic liner. This type of metal shell has an inner taper angle of 10° [1, 21]. In 2017, Lee et al. compared malseating rate of ceramic liners between two metal shell designs: one with an inner taper angle of 18° and the other with an inner taper angle of 10°. The malseating rate in the 10° metal shell was higher than that in the 18° metal shell (23.3% vs. 0%) (Fig. 13.2) [29]. Currently, most manufacturers have adopted 18° as the inner taper angle of metal shells for ceramic liner.
Thin metal shell is a risk factor of liner malseating. During firm impaction of a thin metal shell into sclerotic and inelastic acetabulum, a permanent deformation of the metal shell can occur. This deformation induces an uneven contact between the metal shell and the ceramic liners, which can lead to malseating and subsequent fracture of the ceramic liner [30]. This deformation of the thin acetabular component may not make a problem when coupled with a polyethylene liner, which is soft and elastic and easily slides into the deformed metal shell. However, the ceramic liner is plastic and would not be completely seated into the deformed metal shell [31].
5 Squeak
The squeaking has been reported as a complication of modern CoC bearings. Although the methods of measuring squeaking are not standardized, the incidence of squeaking after CoC THA ranged from 0.5 to 17% in the literature [23, 32, 33]. The exact mechanism of squeaking is unrevealed, but it seems to be multifactorial. To date, three contributing factors, (a) metal shell design, (b) metal shell position, and (c) patient’s constitution, have been known for the development of squeaking. A squeak occurs when the fluid film, which separates the ceramic head from the ceramic liner, is disrupted to allow a friction at the joint and to excite an audible vibration. The lubrication by synovial film is broken in specific conditions such as joint separation due to impingement, stripe wear, edge loading, and metal transfer [33,34,35].
The acetabular cup with an elevated metal rim (Trident® system; Stryker Orthopaedics, Mahwah, NJ, USA) has been known as a risk for squeaking (Fig. 13.3) [36]. This metal shell was designed to prevent an impingement between stem neck and brittle ceramic liner. However, it was associated with a reduced range of motion, leading to metal-to-metal contact between the stem neck and rim of metal shell. The metal-to-metal contact generates metal debris, which disrupts the fluid-film lubrication in the ceramic bearing surface and leads to squeaking. The neck-rim impingement increases the chance of lever out of the ceramic head, which leads to edge loading, stripe wear, and squeaking. Furthermore, elevated metal rim increases the resonance, which amplifies squeaking [35, 36].
Walter et al. showed that excessive or insufficient anteversion or inclination of the acetabular cup was associated with squeaking [37]. In their study, 94% of non-squeaking patients had 25° ± 10° of cup anteversion and 45° ± 10° of cup abduction, while 35% of squeaking patients had this range of cup position. Stem neck-metal shell impingement and edge loading in improperly positioned metal shells were the possible explanations for the squeaking.
Mai et al. reported that patients who had squeaking were taller than those who did not have [38]. Sexton et al. also reported that taller, heavier, and younger patients were more likely to squeak [39]. In the meta-analysis by Stanat and Capozzi, high body mass index was the only significant patient risk factor of squeaking [40].
6 Conclusions
Contemporary CoC bearings offer major advantages over other bearings. When surgeons use CoC bearings for THA, they should choose optimal implants, should be cautious about adequate positioning of implants, and should not make a scratch on the ceramic surface during the operation to minimize the risk of fracture and squeaking.
References
Lee YK, Ha YC, Yoo JI, Jo WL, Kim KC, Koo KH. Mid-term results of the BIOLOX delta ceramic-on-ceramic total hip arthroplasty. Bone Joint J. 2017;99-B(6):741–8.
Howard DP, Wall PDH, Fernandez MA, Parsons H, Howard PW. Ceramic-on-ceramic bearing fractures in total hip arthroplasty: an analysis of data from the National Joint Registry. Bone Joint J. 2017;99-B(8):1012–9.
Lim SJ, Ryu HG, Eun HJ, Park CW, Kwon KB, Park YS. Clinical outcomes and bearing-specific complications following fourth-generation alumina ceramic-on-ceramic total hip arthroplasty: a single-surgeon series of 749 hips at a minimum of 5-year follow-up. J Arthroplast. 2018;33(7):2182–6.e1.
Varnum C, Pedersen AB, Kjaersgaard-Andersen P, Overgaard S. Comparison of the risk of revision in cementless total hip arthroplasty with ceramic-on-ceramic and metal-on-polyethylene bearings. Acta Orthop. 2015;86(4):477–84.
White PB, Meftah M, Ranawat AS, Ranawat CS. A comparison of blood metal ions in total hip arthroplasty using metal and ceramic heads. J Arthroplast. 2016;31(10):2215–20.
Lee YK, Yoon BH, Choi YS, Jo WL, Ha YC, Koo KH. Metal on metal or ceramic on ceramic for cementless total hip arthroplasty: a meta-analysis. J Arthroplast. 2016;31(11):2637–45.e1.
Sentuerk U, von Roth P, Perka C. Ceramic on ceramic arthroplasty of the hip: new materials confirm appropriate use in young patients. Bone Joint J. 2016;98-B(1 Suppl A):14–7.
Mahoney OM, Dimon JH 3rd. Unsatisfactory results with a ceramic total hip prosthesis. J Bone Joint Surg Am. 1990;72(5):663–71.
Nich C, Sariali E-H, Hannouche D, Nizard R, Witvoet J, Sedel L, et al. Long-term results of alumina-on-alumina hip arthroplasty for osteonecrosis. Clin Orthop Relat Res. 2003;(417):102–11.
Callaway GH, Flynn W, Ranawat CS, Sculco TP. Fracture of the femoral head after ceramic-on-polyethylene total hip arthroplasty. J Arthroplast. 1995;10(6):855–9.
Morlock M, Nassutt R, Janssen R, Willmann G, Honl M. Mismatched wear couple zirconium oxide and aluminum oxide in total hip arthroplasty. J Arthroplast. 2001;16(8):1071–4.
Skinner HB. Ceramic bearing surfaces. Clin Orthop Relat Res. 1999;(369):83–91.
Boutin P. [Total arthroplasty of the hip by fritted aluminum prosthesis. Experimental study and 1st clinical applications]. Rev Chir Orthop Reparatrice Appar Mot. 1972;58(3):229–46.
Kang BJ, Ha YC, Hwang SC, Lee YK, Koo KH. Midterm results of large diameter Biolox forte ceramic head on delta ceramic liner articulation in total hip arthroplasty. J Arthroplast. 2014;29(12):2412–4.
Koo KH, Ha YC, Jung WH, Kim SR, Yoo JJ, Kim HJ. Isolated fracture of the ceramic head after third-generation alumina-on-alumina total hip arthroplasty. J Bone Joint Surg Am. 2008;90(2):329–36.
Pitto RP, Garland M, Sedel L. Are ceramic-on-ceramic bearings in total hip arthroplasty associated with reduced revision risk for late dislocation? Clin Orthop Relat Res. 2015;473(12):3790–5.
Stewart TD, Tipper JL, Insley G, Streicher RM, Ingham E, Fisher J. Long-term wear of ceramic matrix composite materials for hip prostheses under severe swing phase microseparation. J Biomed Mater Res B Appl Biomater. 2003;66(2):567–73.
Yoon BH, Park IK. Atraumatic fracture of the BIOLOX delta ceramic liner in well-fixed total hip implants. Orthopedics. 2018;41(6):e880–e3.
Abdel MP, Heyse TJ, Elpers ME, Mayman DJ, Su EP, Pellicci PM, et al. Ceramic liner fractures presenting as squeaking after primary total hip arthroplasty. J Bone Joint Surg Am. 2014;96(1):27–31.
Taheriazam A, Mohajer MA, Aboulghasemian M, Hajipour B. Fracture of the alumina-bearing couple delta ceramic liner. Orthopedics. 2012;35(1):e91–3.
Hamilton WG, McAuley JP, Dennis DA, Murphy JA, Blumenfeld TJ, Politi J. THA with Delta ceramic on ceramic: results of a multicenter investigational device exemption trial. Clin Orthop Relat Res. 2010;468(2):358–66.
Baek SH, Kim WK, Kim JY, Kim SY. Do alumina matrix composite bearings decrease hip noises and bearing fractures at a minimum of 5 years after THA? Clin Orthop Relat Res. 2015;473(12):3796–802.
Salo PP, Honkanen PB, Ivanova I, Reito A, Pajamaki J, Eskelinen A. High prevalence of noise following Delta ceramic-on-ceramic total hip arthroplasty. Bone Joint J. 2017;99-B(1):44–50.
Rambani R, Kepecs DM, Makinen TJ, Safir OA, Gross AE, Kuzyk PR. Revision total hip arthroplasty for fractured ceramic bearings: a review of best practices for revision cases. J Arthroplast. 2017;32(6):1959–64.
Langdown AJ, Pickard RJ, Hobbs CM, Clarke HJ, Dalton DJ, Grover ML. Incomplete seating of the liner with the Trident acetabular system: a cause for concern? J Bone Joint Surg Br. 2007;89(3):291–5.
Bascarevic Z, Vukasinovic Z, Slavkovic N, Dulic B, Trajkovic G, Bascarevic V, et al. Alumina-on-alumina ceramic versus metal-on-highly cross-linked polyethylene bearings in total hip arthroplasty: a comparative study. Int Orthop. 2010;34(8):1129–35.
Choy WS, Kim KJ, Lee SK, Bae KW, Hwang YS, Park CK. Ceramic-on-ceramic total hip arthroplasty: minimum of six-year follow-up study. Clin Orthop Surg. 2013;5(3):174–9.
Elkins JM, Pedersen DR, Callaghan JJ, Brown TD. Do obesity and/or stripe wear increase ceramic liner fracture risk? An XFEM analysis. Clin Orthop Relat Res. 2013;471(2):527–36.
Lee YK, Kim KC, Jo WL, Ha YC, Parvizi J, Koo KH. Effect of inner taper angle of acetabular metal shell on the malseating and dissociation force of ceramic liner. J Arthroplast. 2017;32(4):1360–2.
Squire M, Griffin WL, Mason JB, Peindl RD, Odum S. Acetabular component deformation with press-fit fixation. J Arthroplast. 2006;21(6 Suppl 2):72–7.
Hothan A, Huber G, Weiss C, Hoffmann N, Morlock M. Deformation characteristics and eigen frequencies of press-fit acetabular cups. Clin Biomech. 2011;26(1):46–51.
D’Antonio JA, Capello WN, Naughton M. Ceramic bearings for total hip arthroplasty have high survivorship at 10 years. Clin Orthop Relat Res. 2012;470(2):373–81.
Park YS, Park SJ, Lim SJ. Ten-year results after cementless THA with a sandwich-type alumina ceramic bearing. Orthopedics. 2010;33(11):796.
Taylor S, Manley MT, Sutton K. The role of stripe wear in causing acoustic emissions from alumina ceramic-on-ceramic bearings. J Arthroplast. 2007;22(7 Suppl 3):47–51.
Walter WL, O’Toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplast. 2007;22(4):496–503.
Swanson TV, Peterson DJ, Seethala R, Bliss RL, Spellmon CA. Influence of prosthetic design on squeaking after ceramic-on-ceramic total hip arthroplasty. J Arthroplast. 2010;25(6 Suppl):36–42.
Walter WL, Insley GM, Walter WK, Tuke MA. Edge loading in third generation alumina ceramic-on-ceramic bearings: stripe wear. J Arthroplast. 2004;19(4):402–13.
Mai K, Verioti C, Ezzet KA, Copp SN, Walker RH, Colwell CW Jr. Incidence of ‘squeaking’ after ceramic-on-ceramic total hip arthroplasty. Clin Orthop Relat Res. 2010;468(2):413–7.
Sexton SA, Yeung E, Jackson MP, Rajaratnam S, Martell JM, Walter WL, et al. The role of patient factors and implant position in squeaking of ceramic-on-ceramic total hip replacements. J Bone Joint Surg Br. 2011;93(4):439–42.
Stanat SJ, Capozzi JD. Squeaking in third- and fourth-generation ceramic-on-ceramic total hip arthroplasty: meta-analysis and systematic review. J Arthroplast. 2012;27(3):445–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Yoon, BH., Cha, YH., Lee, S.J., Parvizi, J., Koo, KH. (2021). Ceramic-on-Ceramic Total Hip Arthroplasty. In: Drescher, W.R., Koo, KH., Windsor, R.E. (eds) Advances in Specialist Hip Surgery . Springer, Cham. https://doi.org/10.1007/978-3-030-61830-8_13
Download citation
DOI: https://doi.org/10.1007/978-3-030-61830-8_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-61829-2
Online ISBN: 978-3-030-61830-8
eBook Packages: MedicineMedicine (R0)