Abstract
Cryptorchidism is a common finding in newborn males, with 20–30% of them exhibiting a non-palpable testis. Over time laparoscopy has become the gold standard for the diagnosis of non-palpable testis as well as treatment of intra-abdominal testis. This chapter describes the contemporary surgical techniques for laparoscopic orchiopexy, with emphasis on intra-operative findings. In addition, it discusses testicular vascular supply and how it impacts surgical decision making with regards to a single or staged surgery, as well as how to manage a long looping vas deferens. Newer techniques are reviewed as well as common complications, pitfalls, and long-term outcomes as described in the literature.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Cryptorchidism is the most common genitourinary malformation affecting newborn boys. Aside from aesthetic considerations, surgical correction of undescended testes is aimed at reducing the risk of malignancy and aiding in its surveillance, infertility, torsion and associated hernia [1].
The choice of surgical management for cryptorchidism depends most importantly whether or not the testicle is palpable on exam. If a testicle is felt on exam, then the preferred surgical approach is either scrotal or inguinal, while if the testicle is not found on exam, current guidelines recommend a laparoscopic approach [1, 2].
Among all children born with cryptorchidism, 20–30% of them will have non-palpable testes [3]. 20–40% of testicles that elude exam are absent or “vanished”, 15–35% will be in the inguinal canal or canalicular, 20–50% will be in the abdominal cavity and 2–9% will be ectopic [4,5,6,7,8,9,10].
Since its introduction in 1976, laparoscopy has been the gold standard for diagnosis of non-palpable gonads [11]. Despite being an invasive procedure, physical exam and imaging modalities fall short in: (1) Identifying whether or not the non-palpable testis is present; (2) determining whether the testis is intra-abdominal or in the inguinal canal [12].
Ultrasound is a readily available, low cost and minimally invasive diagnostic instrument, but according to a recent meta-analysis, the performance of ultrasound is poor, with a sensitivity and specificity in detecting a non-palpable testis of 45% and 78% respectively [13]. Magnetic resonance imaging outperform ultrasound, with improved sensitivity and specificity, ranging respectively between 85–96% and 79–100% [12], however it is hindered by its cost and the need for the child to be sedated.
The other advantage of laparoscopy is that other than being a diagnostic tool it also functions as a therapeutic one. Indeed, early reports of laparoscopy in non-palpable testes were focused mainly on its diagnostic nature, as a gateway to either abdominal or inguinal exploration. The first-stage Fowler-Stephens approach was first described in 1991 at a time when pelvic laparoscopy was becoming more common [14]. Two years later, use of laparoscopy had been extended to orchiectomies of dystrophic testes as well as for the second stage of a Fowler-Stephens [15]. Since then, laparoscopic orchiopexy has become a well-established approach to the abdominal testis.
In this chapter we will describe the main surgical technique as well as variations of laparoscopic orchiopexy, troubleshooting and complications, and briefly outcomes.
Surgical Technique
Positioning and Trocar Placement
The patient is positioned supine on the operating table. Once the child is anesthetized, a careful exam under anesthesia is conducted. If the testicle is felt, an inguinal or scrotal approach is chosen over laparoscopy.
In order to facilitate surgical ergonomics, the anesthesiology team is preferably positioned at the side of the bed (Fig. 19.1). This allows for the surgeon to operate at the head of the bed, “looking down” toward the pelvis.
The patient’s bladder is emptied at the beginning of the case and the bed is placed in a mild Trendelenburg position. The 5-mm camera port is inserted in an umbilical position and pneumoperitoneum is established with CO2 to 8–10 mmHg, to visualize the operative field.
The abdominal cavity is carefully explored to identify the testicle and its blood supply.
If working ports are needed, these can be placed under direct visualization. Usually 3- or 5-mm ports are used, based on the surgeon’s preference and size of instruments (e.g., a laparoscopic clip applier will require a 5-mm port). Working ports are usually placed lateral to the rectus muscle on either side at the level of the umbilicus or below. The ipsilateral port can be placed higher depending on the position of the testis (Fig. 19.2).
Introduction of 3 mm instruments directly into the abdomen via a skin puncture without trocars has been described as well. This approach does not seem to prolong operative times and has been shown to be cost-effective [16]. These incisions are small enough that they do not require fascial closure.
Single-Site Surgery
To further reduce invasiveness and improve the cosmetic results of laparoscopic orchiopexy, several authors have described single-site techniques [17,18,19,20]. These approaches utilize a single umbilical incision.
De Lima and coworkers relied on a single incision above the umbilicus, from the 3 to 9 o’clock. The placed a 5- of 10-mm trocar in the midline, using the traditional Hasson technique, and subsequently placed two other 3- or 5-mm ports on each side. These additional ports are placed through the same skin incision but enter the fascia at a different location than the camera port, making this a single-incision multiport technique. All fascial defects are closed at the end of the case [17]. In a similar manner, Li and colleagues described a multi-incision trans-umbilical approach. Instead of using a single incision for multiple ports, which would limit the range of motions of the instruments, they performed an infraumbilical incision from 4 to 8 o’clock for the 5-mm camera port as well as a second 5 mm working port which is placed at the 4 o’clock position of the same incision. Another incision, at the 10–11 o’clock position is used for the third trocar [18]. Noh et al. reported using a multichannel port through the umbilicus, aided by a flexible tip laparoscope and curved instruments [19]. However, this approach is burdened by the increase costs of specialized equipment. Finally, Mahdi and colleagues used a glove port to perform laparoscopic orchiopexy. This port is low cost and “home-made” alternative to a multiport channel. This technique used standard rigid instruments which must be crossed, making this a more technically demanding approach [20].
Laparoscopic Findings
At preliminary laparoscopy it is important to identify the location of the undescended testicle to plan the following surgical steps. If no testicle is seen upon initial evaluation, there are three possible scenarios: (a) testicular vessels are seen terminating before reaching a closed internal inguinal ring (i.e., “blind-ending” vessels); (b) testicular vessels enter the ring; (c) no vessels are visualized.
In the first case, the testicle has presumably atrophied from torsion, and is a “vanishing” testis, while in the second case, the testicular remnants or “nubbins” can be found in the inguinal canal or scrotum. If no vessels are seen, one must explore higher as testicles can be found as high as the kidney when not immediately identifiable down in the pelvis.
For a true vanishing testis no further treatment is recommended, while inguinal exploration for excision of testicular remnants has been debated. However, large series have shown that these nubbins harbor viable germ cells in 5.3–11% of the cases and seminiferous tubules in 10.7–24% [21,22,23].. Therefore, in case a vas and vessels are seen entering the inguinal canal in the setting of a non-palpable testis, inguinal exploration is recommended.
If a testicle is seen, it should first be assessed. In case of a dysmorphic testicle, an orchiectomy should be considered, while in the presence of a healthy appearing gonad, other findings will help determine the next step.
If the testis is found near the inguinal ring, careful inspection of the vas should be carried out, to assess whether it is looping into the inguinal canal or not. When a gonad localized at the internal inguinal ring or in a “peeping” position (moving into and out of the inguinal canal), usually a one-stage laparoscopic orchiopexy, with sparing of the testicular vessels, can be performed successfully.
However, if the testicle is in a high position, usually considered greater than 2 cm from the internal ring [24], ligation and division of the testicular vessels, whether with a one stage or two-stage Fowler-Stephens approach, is necessary.
Vascular Supply
The arterial blood supply to the testicle is three-fold: the testicular artery originating from the abdominal aorta or renal artery; the deferential artery originating from the superior or inferior vesical artery; the cremasteric artery, originating from the inferior epigastric artery. The fetal testis is always supplied by at least 2 of these arterial systems (usually the testicular and deferential arteries) [25, 26].
During a Fowler-Stephens procedure, ligation of the testicular artery stimulates growth of the collateral arterial supply. Studies have shown arterial connections between the cremasteric artery, located in the gubernaculum, and the testicular and deferential ones [27, 28]. Collateral circulation tends to predominate from either the cremasteric or the deferential vessels, but never from both; 60% of the time it originates from the gubernaculum, and 40% around the vas deferens [28]. These collaterals were noted as early as 6 weeks after ligation of the vessels. Hence, in the setting of a short instead of long gubernaculum, if a staged Fowler-Stephens procedure is planned, it has been suggested that transection of the gubernaculum at the time of vessel ligation, might stimulate development of the deferential circulation.
One-Stage Orchiopexy
If a viable intra-abdominal testis has been found, the first consideration is whether or not it will be possible to perform an orchiopexy without division of the gonadal vessels during the same surgery. The limiting factor that would require a staged procedure is the length of the gonadal vessels. It can be difficult to determine if the length of these vessels will be adequate to reach the scrotum. If the testicle is found to be >2 cm from the internal inguinal ring, the vessels are often too short to allow proper positioning of the testicle in the scrotum [24]. In this setting, ligation of the vessels followed by a second stage surgery is recommended. One-stage Fowler-Stephens procedures (ligation of the vessels and orchiopexy in the same setting) are associated with lower testis survival rates (74% vs 88% for a staged procedure) [4].
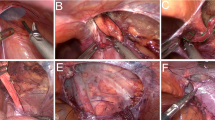
We begin by incising the peritoneum along the lateral aspect of the gonadal vessels up to the internal ring. The peritoneum is also incised along the vas deferens towards the internal ring to create a triangle of peritoneum between the vas deferens and gonadal vessels which will be mobilized. Any structures , namely the epididymis and vas deferens, that might be extending distally into the inguinal canal are carefully mobilized into the abdomen. The gubernaculum is then transected and used as a safe handle for further mobilization of the testis.
The testis is then mobilized on the resulting peritoneal flap until it can easily reach the contralateral internal ring. Once this has been accomplished typically there is typically enough length on the gonadal vessels to deliver the testis in the scrotum. Once adequate length is achieved, the testicle is ready to be brought down to the scrotum. Prentiss and colleagues were the first to describe the importance of delivering the testis in the scrotum without excessive tension, to prevent ischemic injury. In doing so, they reported that the shortest distance between the abdominal cavity to the scrotum is via a neo-canal that passes medial to the epigastric vessels and above the pubic bone [29]. To do so, first, a transverse skin incision is made onto the ipsilateral mid-scrotum. A sub-dartos pouch is created to harbor the testicle. Then, using a laparoscopic grasper from inside the abdominal cavity, a new tract is created by applying gentle pressure medial to the epigastric vessels . Externally, the tips of the grasper can be guided to make sure they pass over the pubic tubercle. The grasper is pushed until the tips exit at the level of the scrotal incision. A 12-mm port is inserted into the abdomen through the scrotal incision via the newly created channel. This is assisted by using the previously passed laparoscopic grasper to pull the end of the sheath of a Step Bladeless trocar (Medtronic, Minneapolis, USA) into the abdomen from scrotal incision (Fig. 19.3a, b). Once the port has been placed, a Maryland grasper can be introduced to grab the gubernaculum. The testis is then delivered into the scrotum via the port, and subsequently the port is removed under vision, ensuring that the cord is neither twisted nor under too much tension. Once in the scrotum, the testis is secured in the usual manner. Prior to removal of ports, the abdominal cavity is inspected and ports are removed under direct vision. All fascial defects are reapproximated once the pneumoperitoneum has been evacuated, and the skin is closed in the preferred manner.
Kahiri and coworkers have described inserting the scrotal trocar right after gubernacular dissection to aid with dissection of the vascular pedicle. Addition of this port early on allows for use of the dissecting instruments from below while the testis is lifted from one of the abdominal ports [30].
Two-Stage Orchiopexy
Fowler and Stephens were the first to describe ligation of testicular vessels in order to salvage high intra-abdominal testes [31].
During the first stage, the vessels are ligated close to the testis. This can be done with either clips or electrocautery. A study conducted by AbouZeid and coworkers did not show any differences in outcomes or testicular histology assess with biopsies between children who had their vessels controlled with clips or electrocautery , although the latter did provide an economical advantage [32].
Once the vessels have been transected, it is preferred to wait 6 months after the first stage, to allow adequate collaterals to develop. A vascularized peritoneal flap is then created very carefully, maintaining the collateral blood supply that developed from the deferential artery. To do so, the peritoneum is incised sharply lateral and above the internal inguinal ring. The incision is then continued medially ensuring that enough peritoneum is left covering the vas. This will create a V-shaped flap that should cover the vas and testis. At this point, the testicle is then brought down to the scrotum in the same manner as one would do during a one stage orchiopexy. Due to evidence of collateral blood flow developing through the gubernaculum via the cremasteric artery, some surgeons have developed gubernaculum-sparing approaches.
To do so, the dissection of the peritoneum starts as usual lateral to the internal inguinal ring and is carried out medially along the superior margin of the ring. Then, more dissection of the peritoneum is performed proximally at the bifurcation of the iliac vessels. Finally, a laparoscopic grasper is advanced through the internal inguinal ring alongside the gubernaculum, if the ring was open. If the ring is closed, a 5-mm trocar is advanced intra-abdominally through the usual scrotal incision, via the inguinal canal. The testis is then brought down with the preserved gubernaculum. If the testis is under tension, more proximal peritoneal dissection is performed [33, 34]. This technique has shown significantly lower atrophy rates compared to classic laparoscopic orchiopexy (0.6% vs 28.3%, respectively) [33].
Another group described a gubernacular-sparing approach involving a first laparoscopic stage, for vessel ligation, followed by a second stage that combines laparoscopic peritoneal dissection with a groin approach during which the testicle is externalized by gentle traction on gubernacular attachments and blunt dissection [35].
A similar concept of sparing the gubernaculum should be considered when the testis is found high in the abdomen. In this scenario a two stage Fowler Stephens approach can be utilized. The vessels are clipped as done with an ordinary Fowler Stephens approach. The second stage is undertaken 6 months later . At this stage the testis is mobilized on a peritoneal flap whose boarders are the vas deferens and the long gubernacular structures which can be found extending up from the internal ring to the testis. The gubernaculum is spared and passed with the testis through the tunnel created in a similar fashion as is described above.
Surgical Considerations and Debated Topics
Bilateral Laparoscopic Orchiopexy
In the presence of bilateral undescended and non-palpable testicles, in whom disorders of sexual differentiation have been ruled out, judgment should be used when decided to perform orchiopexy at the same time, especially in the setting of high testicles both requiring vessel ligation. If vessel ligation is required for both gonads, then it is prudent to ligate one vessel at the time. In case one testicle can be brought down in the scrotum in one setting and the other requires ligation, it is recommended to first perform the orchiopexy prior to ligating vessels. If both testicles are low intra-abdominally, then bilateral orchiopexy can be performed in the same setting. Kaye and colleagues have reported outcomes of bilateral laparoscopic orchiopexy in 21 patients [36]. Out of 42 gonads, a Fowler-Stephens approach was required in only 4 testicles. Only 2 gonads eventually atrophied, one of which underwent a one-stage Fowler-Stephens and another that underwent a primary laparoscopic orchiopexy. Out of 21 children, 16 underwent only one surgery.
Long-Looping Vas
Occasionally a long vas is noted departing from the intra-abdominal test, entering the inguinal canal via the internal ring and looping back into the abdominal cavity. The looping vas can be gently brought back into the abdominal cavity by careful blunt dissection and indirect grasping. To facilitate handling of long looping limbs, Shalaby and coworkers described wrapping the vas in a fascial sheath to use for traction . In case they weren’t able to safely dissect the looping vas, an inguinal incision was required to complete the dissection [37].
On the other hand, Dave and colleagues noted in their series that among children who underwent staged orchiopexy, those with a long-looping vas had significantly lower rates of atrophic gonads at follow up if their second stage was performed with an open approach versus a laparoscopic one (0% vs 83%, 5 patients in each group, respectively) [38]. These results could be explained that during laparoscopic dissection of a looping vas, the collateral vessels around the vas might be accidentally injured by traction.
Closure of the Internal Inguinal Ring
The need to close the internal inguinal ring to prevent hernias has been debated. There are only anecdotal reports in the literature reporting cases of inguinal hernia [39].
In the largest series assessing this issue, Kahiri and coworkers assessed 388 boys who underwent laparoscopic orchiopexy. In 46% of them, the right was closed, and in the remaining 54% it was left open. No hernia developed at a mean follow up of 41 months [40].
Traction Orchiopexy
Data from open series where the testicle was placed in the dependent portion of the scrotum under traction with skin puckering have shown good results, with healthy testis in the expected location [41, 42]. Hence, to reduce the number of cases of intra-abdominal testis for which vessel ligation is required, Shehata and colleagues proposed a new staged laparoscopic technique involving application of tension on the testicle to allow for gradual stretching [43]. The patient is not a candidate for this technique if the testicle is >4 cm away from the internal inguinal ring (hence a Fowler-Stephens procedure was recommended) or if the testicle was able to reach the contralateral internal inguinal ring (hence a one-stage laparoscopic orchiopexy was performed).
During the first the gubernaculum was transected and the peritoneum lateral to the vessels was incised. Then, the testicle was fixed with a transcutaneous Ethibond stitch one inch superior and medial the contralateral anterior superior iliac spine.
The second stage was performed 12 weeks after the first one, the stitch was released and the testicle was delivered into the scrotum. If the stitch was noted to have come loose, a new stitch was placed and a third stage was planned.
In their series they were able to document a mean gain of 4.7 cm on vessel length. The success rate with regards to viable testes was 84%. The highest success was in boys younger than 2 years of age (90.3%) as well as in patients with a testis <2 cm from the ipsilateral internal ring (93% vs 78% for testes between 2 and 4 cm). The authors do not recommend this procedure if the testicle is more than 4 cm from the internal inguinal ring.
In theory, the traction is slowly and gently applied by the weight of the intestines. In addition, the testicle is fixed to the anterior abdominal wall, which is mobile and indents, hence not causing too much traction. In all cases, during the second stage, the bowels were seen overlying the vessels. However, no cases of internal hernias were noted in 124 patients.
In a smaller series, Elsherbeny and coworkers replicated similar results [44]. However, when they performed this procedure on two gonads in the same child, they found adhesions between the two vessels where they crossed over each other. Similarly, they were unable to gain enough length on the vessels despite traction for patients with testicles located more than 2 cm from the internal inguinal ring.
Complications
Complications during laparoscopic orchiopexy are relatively rare. The most common complications involved pre-peritoneal insufflation, which limits visibility.
Since the first trocar is placed with the Hasson technique and subsequent trocars are placed under direct vision, viscera and vascular injuries are theoretical and have not been described.
Rough handling of the vessels could lead to vascular injury and subsequent atrophy. Accidental grasping of the vas, apart from potentially damaging the collateral blood supply, could cause long-term blockage of the vas deferens.
Finally, the bladder can be injured when creating a neo-inguinal canal. Hsieh and coworkers reported on 3 bladder injuries in their institution [45]. In all instances, the tunnel towards the scrotum was created medial to the medial umbilical ligament. Furthermore, in one case, the bladder was not emptied at the beginning of the case. Two patients had injuries recognized intra-operatively due to hematuria: one patient had a cystoscopy at time of surgery that showed the cord traversing the bladder dome. Another patient had irrigation fluid extravasating into the abdomen when the bladder was filled. The third patient had a delayed diagnosis when he developed abdominal bloating and pain on the first post-operative day. Interestingly a cystogram was negative but the bladder was under distended. Eventually he underwent cystoscopy which identified the defect. Two of the boys had an open repair and one had a laparoscopic repair. In order to avoid bladder injuries, it is recommended first, to empty the bladder at the beginning of the case, second to create the tunnel lateral to the medial umbilical ligament and medial to the epigastric vessels or to utilize the native inguinal canal.
Outcomes
Overall success of laparoscopic orchiopexy in a large multi-centric cohort has been reported to be 92.8% [4]. Success was defined as a viable testicle in a dependent scrotal location. When broken down by approach, the highest success rate was seen in primary laparoscopic orchiopexy (97.2%), the lowest was in one-stage Fowler-Stephens (74.1%) while staged Fowler-Stephens had intermediate results (87.9%).
Atrophy was more common in the one-stage Fowler-Stephens (22.2%), followed by the staged approach (10.3%) and the one-stage classic orchiopexy (2.2%). With regards to testicular retraction, once again the one-stage Fowler-Stephens had higher rates (7.4%) followed by the one stage approach (1.7%) and the classic orchiopexy (0.6%). Interestingly, while the outcome differences were statistically significant between classic laparoscopic orchiopexy and the Fowler-Stephens approaches but were not statistically different between the two Fowler-Stephens groups. To date, only one randomized trial assessing differences in outcomes between one- versus two-staged laparoscopic Fowler-Stephens has been published. This small trial, including 27 patients did not show any differences in atrophy rates between one- and two-stages (7% and 8%, respectively) [46].
Long-term outcomes for patients undergoing laparoscopic staged Fowler-Stephens who were followed for >10 years have shown an 83% success rate. The operated testicle was viable but always slightly smaller than the contralateral one, suggesting long term success of this procedure [47].
References
Kolon TF, Herndon CD, Baker LA, Baskin LS, Baxter CG, Cheng EY, et al. Evaluation and treatment of cryptorchidism: AUA guideline. J Urol. 2014;192(2):337–45.
Radmayr C, Dogan HS, Hoebeke P, Kocvara R, Nijman R, Silay S, et al. Management of undescended testes: European Association of Urology/European Society for Paediatric Urology Guidelines. J Pediatr Urol. 2016;12(6):335–43.
Cendron M, Huff DS, Keating MA, Snyder HM 3rd, Duckett JW. Anatomical, morphological and volumetric analysis: a review of 759 cases of testicular maldescent. J Urol. 1993;149(3):570–3.
Baker LA, Docimo SG, Surer I, Peters C, Cisek L, Diamond DA, et al. A multi-institutional analysis of laparoscopic orchidopexy. BJU Int. 2001;87(6):484–9.
Denes FT, Saito FJ, Silva FA, Giron AM, Machado M, Srougi M. Laparoscopic diagnosis and treatment of nonpalpable testis. Int Braz J Urol. 2008;34(3):329–34; discussion 35.
Ferro F, Lais A, Bagolan P, Talamo M, Caterino S. Impact of primary surgical approach in the management of the impalpable testis. Eur Urol. 1992;22(2):142–6.
Ferro F, Lais A, Gonzalez-Serva L. Benefits and afterthoughts of laparoscopy for the nonpalpable testis. J Urol. 1996;156(2 Pt 2):795–8; discussion 8.
Froeling FM, Sorber MJ, de la Rosette JJ, de Vries JD. The nonpalpable testis and the changing role of laparoscopy. Urology. 1994;43(2):222–7.
Kirsch AJ, Escala J, Duckett JW, Smith GH, Zderic SA, Canning DA, et al. Surgical management of the nonpalpable testis: the Children’s Hospital of Philadelphia experience. J Urol. 1998;159(4):1340–3.
Merguerian PA, Mevorach RA, Shortliffe LD, Cendron M. Laparoscopy for the evaluation and management of the nonpalpable testicle. Urology. 1998;51(5A Suppl):3–6.
Cortesi N, Ferrari P, Zambarda E, Manenti A, Baldini A, Morano FP. Diagnosis of bilateral abdominal cryptorchidism by laparoscopy. Endoscopy. 1976;8(1):33–4.
Tasian GE, Copp HL, Baskin LS. Diagnostic imaging in cryptorchidism: utility, indications, and effectiveness. J Pediatr Surg. 2011;46(12):2406–13.
Tasian GE, Copp HL. Diagnostic performance of ultrasound in nonpalpable cryptorchidism: a systematic review and meta-analysis. Pediatrics. 2011;127(1):119–28.
Bloom DA. Two-step orchiopexy with pelviscopic clip ligation of the spermatic vessels. J Urol. 1991;145(5):1030–3.
Bogaert GA, Kogan BA, Mevorach RA. Therapeutic laparoscopy for intra-abdominal testes. Urology. 1993;42(2):182–8.
Noh PH, Kalyanaraman B. Single trocar skin puncture laparoscopic orchidopexy. Urology. 2012;80(3):695–7.
de Lima GR, da Silveira RA, de Cerqueira JB, de Abreu AC, de Abreu Filho AC, Rocha MF, et al. Single-incision multiport laparoscopic orchidopexy: initial report. J Pediatr Surg. 2009;44(10):2054–6.
Li N, Zhang W, Yuan J, Zhou X, Wu X, Chai C. Multi-incisional transumbilical laparoscopic surgery for nonpalpable undescended testes: a report of 126 cases. J Pediatr Surg. 2012;47(12):2298–301.
Noh PH, Vinson MA, Bansal D. LaparoEndoscopic Single Site orchidopexy for intra-abdominal testes in the pediatric population with a multichannel single port and flexible tip laparoscope. J Endourol. 2013;27(11):1381–3.
Mahdi BD, Rahma C, Mohamed J, Hayet Z, Riadh M. Single port laparoscopic orchidopexy in children using surgical glove port and conventional rigid instruments. Korean J Urol. 2015;56(11):781–4.
Bader MI, Peeraully R, Ba’ath M, McPartland J, Baillie C. The testicular regression syndrome--do remnants require routine excision? J Pediatr Surg. 2011;46(2):384–6.
Nataraja RM, Asher CM, Nash R, Murphy FL. Is routine excision of testicular remnants in testicular regression syndrome indicated? J Pediatr Urol. 2015;11(3):151 e1–5.
Nataraja RM, Yeap E, Healy CJ, Nandhra IS, Murphy FL, Hutson JM, et al. Presence of viable germ cells in testicular regression syndrome remnants: is routine excision indicated? A systematic review. Pediatr Surg Int. 2018;34(3):353–61.
Yucel S, Ziada A, Harrison C, Wilcox D, Baker L, Snodgrass W. Decision making during laparoscopic orchiopexy for intra-abdominal testes near the internal ring. J Urol. 2007;178(4 Pt 1):1447–50; discussion 50.
Sampaio FJ, Favorito LA, Freitas MA, Damiao R, Gouveia E. Arterial supply of the human fetal testis during its migration. J Urol. 1999;161(5):1603–5.
Yalcin B, Komesli GH, Ozgok Y, Ozan H. Vascular anatomy of normal and undescended testes: surgical assessment of anastomotic channels between testicular and deferential arteries. Urology. 2005;66(4):854–7.
Ellis R, Lahiri R, Mahomed A. Mapping testicular blood supply in gubernaculum-sparing second-stage Fowler-Stephens procedure. Surg Endosc. 2014;28(11):3158–61.
Hay SA. Collateral circulation after spermatic vessel ligation for abdominal testis and its impact on staged laparoscopically assisted orchiopexy. J Laparoendosc Adv Surg Tech A. 2007;17(1):124–7.
Prentiss RJ, Weickgenant CJ, Moses JJ, Frazier DB. Undescended testis: surgical anatomy of spermatic vessels, spermatic surgical triangles and lateral spermatic ligament. J Urol. 1960;83:686–92.
Khairi A, El-Kholi N, Shehata S. Early insertion of trans-scrotal port during laparoscopic orchidopexy: a new concept. J Pediatr Urol. 2011;7(5):548–51.
Fowler R, Stephens FD. The role of testicular vascular anatomy in the salvage of high undescended testes. Aust N Z J Surg. 1959;29:92–106.
AbouZeid AA, Moussa MH, Shalaby MS, Safoury HS, El-naggar O, Hay S. Feasibility and safety of monopolar diathermy as an alternative to clip ligation in laparoscopic Fowler-Stephens orchiopexy. J Pediatr Surg. 2012;47(10):1907–12.
Braga LH, Farrokhyar F, McGrath M, Lorenzo AJ. Gubernaculum testis and cremasteric vessel preservation during laparoscopic orchiopexy for intra-abdominal testes: effect on testicular atrophy rates. J Urol. 2019;201(2):378–85.
Robertson SA, Munro FD, Mackinlay GA. Two-stage Fowler-Stephens orchidopexy preserving the gubernacular vessels and a purely laparoscopic second stage. J Laparoendosc Adv Surg Tech A. 2007;17(1):101–7.
Mahomed A, Adams S, Islam S. Initial success with gubernacular-sparing laparoscopic-assisted Fowler-Stephens orchidopexy for intra-abdominal testes. J Laparoendosc Adv Surg Tech A. 2012;22(2):192–4.
Kaye JD, Palmer LS. Single setting bilateral laparoscopic orchiopexy for bilateral intra-abdominal testicles. J Urol. 2008;180(4 Suppl):1795–9; discussion 9.
Shalaby MM, Shoma AM, Elanany FG, Elganainy EO, El-Akkad MA. Management of the looping vas deferens during laparoscopic orchiopexy. J Urol. 2011;185(6 Suppl):2455–7.
Dave S, Manaboriboon N, Braga LH, Lorenzo AJ, Farhat WA, Bagli DJ, et al. Open versus laparoscopic staged Fowler-Stephens orchiopexy: impact of long loop vas. J Urol. 2009;182(5):2435–9.
Metwalli AR, Cheng EY. Inguinal hernia after laparoscopic orchiopexy. J Urol. 2002;168(5):2163.
Khairi A, Shehata S, El-Kholi N. Is it necessary to close the peritoneum over the deep inguinal ring during laparoscopic orchidopexy? J Pediatr Urol. 2013;9(2):157–60.
Daher P, Nabbout P, Feghali J, Riachy E. Is the Fowler-Stephens procedure still indicated for the treatment of nonpalpable intraabdominal testis? J Pediatr Surg. 2009;44(10):1999–2003.
Dessanti A, Falchetti D, Iannuccelli M, Milianti S, Altana C, Tanca AR, et al. Cryptorchidism with short spermatic vessels: staged orchiopexy preserving spermatic vessels. J Urol. 2009;182(3):1163–7.
Shehata S, Shalaby R, Ismail M, Abouheba M, Elrouby A. Staged laparoscopic traction-orchiopexy for intraabdominal testis (Shehata technique): stretching the limits for preservation of testicular vasculature. J Pediatr Surg. 2016;51(2):211–5.
Elsherbeny M, Abdallah A, Abouzeid A, Ghanem W, Zaki A. Staged laparoscopic traction orchiopexy for intra-abdominal testis: is it always feasible? J Pediatr Urol. 2018;14(3):267 e1–4.
Hsieh MH, Bayne A, Cisek LJ, Jones EA, Roth DR. Bladder injuries during laparoscopic orchiopexy: incidence and lessons learned. J Urol. 2009;182(1):280–4; discussion 4–5.
Ostlie DJ, Leys CM, Fraser JD, Snyder CL, St Peter SD. Laparoscopic orchiopexy requiring vascular division: a randomized study comparing the primary and two-stage approaches. J Laparoendosc Adv Surg Tech A. 2015;25(6):536–9.
Esposito C, Vallone G, Savanelli A, Settimi A. Long-term outcome of laparoscopic Fowler-Stephens orchiopexy in boys with intra-abdominal testis. J Urol. 2009;181(4):1851–6.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Passoni, N.M., Jacobs, M.A. (2020). Laparoscopic Orchiopexy. In: Gargollo, P.C. (eds) Minimally Invasive and Robotic-Assisted Surgery in Pediatric Urology. Springer, Cham. https://doi.org/10.1007/978-3-030-57219-8_19
Download citation
DOI: https://doi.org/10.1007/978-3-030-57219-8_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-57218-1
Online ISBN: 978-3-030-57219-8
eBook Packages: MedicineMedicine (R0)