Abstract
Low plasma levels of cholesterol carried by high-density lipoprotein (HDL) particles are firmly established as a major cardiovascular risk factor. Paradoxically, cardiovascular mortality is also elevated at extremely high levels of HDL cholesterol. Furthermore, genetic epidemiology often does not support a causal relationship between HDL cholesterol and cardiovascular risk.
HDL particles contain multiple protein and lipid components and are highly heterogeneous in their metabolism, structure and biological function. Small, dense, protein-rich HDLs display elevated anti-atherogenic activities as compared to large, light, lipid-rich particles.
HDL metabolism and function are altered in both low and extremely high HDL cholesterol (HDL-C) states. Low HDL-C levels are typically accompanied by reduced circulating levels of large HDL and deficient biological activities of small HDL particles. Reduced capacity of HDL to efflux cholesterol from lipid-loaded macrophages is associated with both the presence of cardiovascular disease and the risk of future cardiovascular events. However, therapeutic HDL-C raising, which predominantly increases levels of large HDL, have repeatedly failed to reduce cardiovascular events in patients treated with statins. Such flagrant controversy between classic epidemiology, genetic epidemiology and clinical trials needs to be urgently resolved in order to allow further development of HDL-targeting therapies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Apolipoprotein A-I
- Cholesterol
- Liver
- Intestine
- Triglycerides
- Small, dense HDL
- Phospholipids
- Atherosclerosis
- Cardiovascular disease
Introduction
In 1929, Michel Macheboeuf, from the Pasteur Institute in Paris, precipitated the first lipoprotein from animal serum [1]. It was a lipid-rich ‘fraction A’ isolated by ultracentrifugation several decades later and termed high-density lipoprotein (HDL) by the laboratory of John Gofman at the University of California in Berkley [2]. In the very first studies of isolated lipoproteins, reduced cholesterol content was observed in HDL from a small group of patients with atherosclerotic cardiovascular disease (CVD) [3]. Based on this and other findings, the HDL hypothesis was proposed by Miller and Miller to postulate that ‘reduction of plasma HDL concentration may accelerate the development of atherosclerosis, and hence ischaemic heart disease, by impairing the clearance of cholesterol from the arterial wall’ [4]. When confirmed later in large-scale prospective epidemiological studies [5], the inverse relationship between circulating HDL-cholesterol (HDL-C) and CVD fuelled innumerable studies of HDL over the last decades. This work resulted in detailed characterization of both normal HDL metabolism and its abnormalities associated with CVD. As a possibly too straightforward corollary of the HDL hypothesis, HDL-C raising was broadly accepted as a promising approach to reduce CVD risk, opening a way to the development of HDL-targeting therapies. Quite unexpectedly, such therapies largely failed to provide clear benefits when added to standard treatment regimens involving statins, revealing the incompleteness of our understanding of HDL. This chapter reviews major aspects of current knowledge of this extensively studied but still enigmatic lipoprotein.
Normal Plasma HDL
HDL is a small, dense, protein-rich lipoprotein, possessing a mean size of 8–10 nm and density of 1.063–1.21 g/ml [6]. HDL particles are composed predominantly of polar lipids solubilized by apolipoproteins but equally contain numerous other proteins, including enzymes, lipid transfer proteins, acute-phase response proteins, complement components and proteinase inhibitors, and may contain small amounts of non-polar lipids.
Structure
HDL particles are plurimolecular, quasi-spherical or discoid, pseudomicellar complexes. HDL structure is predominantly defined by apolipoprotein A-I (apoA-I), the major HDL protein.
Reconstituted Discoid HDL
The amino acid sequence of apoA-I contains periodically repeating units organized in amphipathic α-helices which are responsible for the potent detergent-like ability of the protein, allowing it to avidly bind lipids and to solubilize them into stable lipoprotein particles. As a result of this rare property, apoA-I spontaneously forms discoid HDL in the presence of minute amounts of phospholipids, with the α-helices arranged around the circumference of HDL and their long axes perpendicular to the acyl chains of the phospholipids. According to such belt model [7], each discoid HDL particle contains two molecules of apoA-I together with 150–200 molecules of phospholipid, and is 9–10 nm in diameter and 4.7 nm in thickness [8]. Other amphipathic apolipoproteins, including apoA-II, apoE and apoM, are also capable of forming discoid HDL. Similarly, discoid HDLs which contain small amounts of cholesterol and some other lipids are present at low concentrations of <5% of total apoA-I in human plasma.
The belt model was later developed to the double belt model , in which two ring-shaped apoA-I molecules encapsulate a lipid membrane leaflet in an antiparallel orientation in which helices 5 of the both molecules directly oppose each other according to a left-to-left (LL) 5/5 interface [9]. In a refined belt and buckle model , the N- and C-terminal residues of apoA-I double back on the molecule [10], while a looped belt model proposes an existence of a looping region within helix 5 that causes a localized opening between the parallel belts, which may include a site of the action of lecithin–cholesterol acyltransferase (LCAT). An alternative solar flares refinement of the double belt model represents the N-termini of apoA-I molecules as globular nodules [11].
Reconstituted Spherical rHDL
The majority of HDL particles in human plasma are however spherical and contain a neutral lipid core composed of cholesteryl ester and triglyceride surrounded by a polar lipid monolayer composed of phospholipids and free cholesterol. The fundamental interactions of apoA-I helices with phospholipid acyl chains do not change markedly in reconstituted spherical HDL relative to the discs, resulting in the similarity in apoA-I structure between the two shapes. According to the trefoil model of spherical HDL [12], three or four apoA-I molecules, bent 120° on the kinks in helices 5 and 10, are organized in antiparallel belts as per the double belt model, forming a three-dimensional cage-like structure. This cage serves to encapsulate neutral lipid core and supports surface polar lipids in the intervening open spaces between the molecules. An alternative organization of apoA-I molecules in spherical HDL involves a helical dimer with hairpin , with two molecules in a double belt and the third as a separate hairpin [13], being similar to the trefoil model from a molecular perspective.
Native HDL Particles
Native spherical HDL particles contain from three to five molecules of apoA-I, with their surface being dominated by protein , which may account up to 87% of the surface of small, dense HDL. General features of apoA-I structure appear to be similar between native and reconstituted HDL (rHDL), extending across lipid-associated forms of all sizes, shapes and origin [8]. Indeed, similar cross-linking patterns of apoA-I molecules were found in human plasma HDL particles containing predominantly apoA-I, in reconstituted spheres and in reconstituted discs irrespective of the particle size or density [14]. HDL particle size appears thereby to be modulated via a twisting motion of the resident apoA-I molecules. However, subtle conformational adaptations including appearance of loop regions in helix 5 of apoA-I [15] may occur in localized regions of the protein in response to changes in either particle diameter or surface packing density.
Heterogeneity
Conformational flexibility of apoA-I forms a basis for the heterogeneity of HDL particles in physical properties and chemical composition. Analytic ultracentrifugation separates HDL in two subclasses, light, lipid-rich HDL2 (d 1.063–1.125 g/ml) and dense, protein-rich HDL3 (d 1.125–1.21 g/mL) [16]. HDL2 and HDL3 can be further fractionated by non-denaturing polyacrylamide gradient gel electrophoresis [16], which distinguishes between large HDL2b (size 9.7–12.0 nm) and HDL2a (8.8.–9.7 nm) and small HDL3a (8.2–8.8 nm), HDL3b (7.8–8.2 nm) and HDL3c (7.2–7.8 nm). Equivalent HDL subclasses can be isolated by isopycnic density gradient ultracentrifugation [16].
Agarose gel electrophoresis of HDL allows analytical separation of HDL according to surface charge and shape, into α-migrating particles, which represent the majority of circulating HDL, and pre-β-migrating particles, consisting of nascent discoid and poorly lipidated HDL [16]. The agarose and the gradient gel electrophoresis can be combined into a two-dimensional method which allows separation of up to 12 distinct apoA-I-containing HDL subclasses, including preβ1, preβ2, α1, α2, α3, α4, preα1, preα2 and preα3 particles [16].
Finally, NMR can quantify three distinct HDL subclasses differing in size, notably large (8.8–13.0 nm), medium (8.2–8.8 nm) and small (7.3–8.2 nm) HDL [16].
Composition
HDL contains a variety of protein and lipid components at a wide range of concentrations, together with microRNAs (miRs), which can be transported by HDL to various tissues.
Proteome
Proteins form the key structural and functional moiety of HDL. Elevated protein content of approximately 50 wt% entails high complexity to the protein composition of HDL which is enriched in different proteins as compared to other lipoprotein classes. Proteomic analyses identify a large number of HDL-associated proteins; thus, The HDL Proteome Watch at http://homepages.uc.edu/~davidswm/HDLproteome.html provides a list of 95 proteins that are reliably located on HDL as of 29 March 2019.
Apolipoproteins
Apo A-I is the major structural and functional HDL protein which accounts for approximately 70 wt% of total protein in HDL [6, 8]. Major functions of apoA-I involve interaction with cellular receptors, activation of LCAT and endowing HDL with multiple anti-atherogenic activities. ApoA-II is the second-major HDL apolipoprotein which represents approximately 15–20 wt% of total HDL protein. ApoA-II is more hydrophobic than apoA-I and circulates as a homodimer composed of two identical polypeptide chains connected by a disulphide bridge.
ApoCs form a family of small exchangeable apolipoproteins. ApoC-I is involved in the activation of LCAT and inhibition of hepatic lipase (HL) and cholesteryl ester transfer protein (CETP). ApoC-II functions as an activator of several triacylglycerol lipases, including lipoprotein lipase (LPL). ApoC-III inhibits LPL and HL and decreases the uptake of chylomicrons by hepatic cells. ApoE is an essential structural and functional glycoprotein component of HDL, which serves as a ligand for apoB/apoE receptors and ensures lipoprotein binding to cell-surface glycosaminoglycans. ApoM specifically binds small hydrophobic molecules, primarily sphingosine-1-phosphate (S1P). Other physiologically important HDL apolipoproteins include apoA-IV, apoD, apoF, apoJ and apoL-I.
Enzymes
LCAT is a highly glycosylated enzyme which catalyses the esterification of cholesterol to cholesteryl esters in plasma lipoproteins, primarily in HDL (carrying approximately 75% of plasma LCAT activity) but also in apoB-containing particles. Human paraoxonases (PON) are calcium-dependent lactonases PON1, PON2 and PON3. In the circulation, PON1 is almost exclusively associated with HDL. Hydrolysis of homocysteine thiolactone has been proposed to represent a major physiologic function of PON1 [17]. Platelet-activating factor acetyl hydrolase (PAF-AH) , equally termed lipoprotein-associated phospholipase A2 (LpPLA2) , degrades PAF and cleaves phospholipid substrates with a short residue at the sn-2 position, such as proinflammatory oxidized short-chain phospholipids.
Lipid transfer proteins
CETP is a glycoprotein that shuttles between HDL and apoB-containing lipoproteins to facilitate a heteroexchange of cholesteryl esters and triglycerides. The structure of CETP includes a hydrophobic tunnel filled with two cholesteryl ester molecules and plugged by an amphiphilic phosphatidylcholine molecule at each end [18]. Phospholipid transfer protein (PLTP) is primarily associated with HDL and exchanges phospholipids between HDL particles, converting them into larger and smaller subspecies.
Other proteins
Positive acute-phase response proteins, including serum amyloid A (SAA) isoforms, whose plasma concentrations are much lower as compared to apolipoproteins but can be markedly elevated by acute inflammation, form a large family of HDL-associated proteins [19]. SAA1, the major member of the family, is predominantly carried by HDL. LPS-binding protein (LBP) is an acute-phase glycoprotein capable of binding the lipid A moiety of LPS and facilitating LPS diffusion [20]. Several proteins involved in complement regulation, including complement component 3 (C3), C4b binding protein, C9 and vitronectin, are equally present in isolated HDL. A family of HDL-associated serpin proteins exemplified by α-1-antitrypsin contains serine proteinase inhibitor domains [19].
Heterogeneity
Proteins are non-uniformly distributed across HDL subpopulations. Thus, HDL can be separated into particles containing apoA-I with (LpA-I:A-II) or without (LpA-I) apoA-II by electro-immunodiffusion in agarose gels [16].
Furthermore, proteomic analysis of HDL particle subpopulations isolated from normolipidemic subjects by density gradient ultracentrifugation, immunoprecipitation or FPLC identifies distinct patterns of distribution of individual proteins across the particles [21]. Distinct clusters of proteins bundled into HDL particles can be distinguished by similar functions including lipid metabolism, antioxidative/anti-inflammatory activity and haemostasis [22]. Specific protein–protein interactions appear to drive formation of such complexes which include lipid-poor particles dominated by PLTP, apoJ and proteins implicated in host defence and inflammation [23]. The diversity of molecules which bind to HDL suggests that the lipoprotein can serve as a versatile adsorptive surface for proteins and peptides to form complexes with distinct functionalities.
Lipidome
Phospholipids prevail in the HDL lipidome, accounting for 40–50 mol% of total lipid, with lesser proportions of cholesteryl esters (30–40 mol%), triglycerides (3–5 mol%) and free cholesterol (5–10 mol%) [24]. Phosphatidylcholine , the principal plasma phospholipid that accounts for 32–35 mol% of total lipids in HDL, is a structural lipid, consistent with its even distribution across HDL subpopulations Lysophosphatidylcholine is another important phospholipid subclass in HDL (1.4–8.1 mol % of total lipids) derived from regulated degradation of phosphatidylcholine by phospholipases, including LCAT. Phosphatidylethanolamine is moderately abundant in HDL (0.7–0.9 mol % of total lipids). Plasmalogens are minor phospholipids which contain a vinyl ether–linked fatty acid essential for their antioxidative properties [25]. Phosphatidylinositol , phosphatidylserine , phosphatidylglycerol , phosphatidic acid and cardiolipin are negatively charged minor (0.8 mol % of total lipids) phospholipids present in HDL which may impact its net surface charge and modulate lipoprotein interactions with lipases, extracellular matrix and other protein components [26].
Sphingomyelin , a structural lipid which enhances surface rigidity, is the major HDL sphingolipid (5.6–6.6 mol% of total lipids), which largely originates from triglyceride-rich lipoproteins (TGRL) [25]. Ceramide is a minor (<0.1 mol% of total lipids) sphingolipid intermediate implicated in cell signalling, apoptosis, inflammatory responses, mitochondrial function and insulin sensitivity. Both sphingomyelin and ceramide are enriched in large, light relative to small, dense HDL [26]. Among lysosphingolipids, S1P is particularly interesting, reflecting its key role in vascular biology [27]. S1P is associated preferentially with small, dense HDL particles [25], consistent with their elevated content of apoM [21].
Unesterified (free) sterols are located in the surface monolayer of HDL particles and regulate its fluidity. HDL sterols are dominated by cholesterol, reflecting the pivotal role of lipoproteins in the cholesterol transport through the body. Cholesteryl esters are largely (up to 80%) produced in HDL and form its lipid core [8]. Most of cholesteryl ester in HDL is accounted for by cholesteryl linoleate. HDL-associated triacylglycerides are dominated by species containing oleic, palmitic and linoleic acid moieties [8]. Minor HDL lipids include diacylglycerides, monoacylglycerides and free fatty acids.
Glycome
Protein moiety of HDL is covered by a carbohydrate coating accounting for up to 3.3 wt% of total protein [28, 29]. HDL carbohydrate residues form N-glycan antennas protruding outside of the particle and carrying N-acetylneuraminic (sialic) acid at their termini underlain by N-acetylglucosamine, fucose, mannose and galactose. Several HDL proteins, including LCAT, CETP, apoCs, fetuin A and α-1-antitripsin, are glycosylated, while the glycosylation of apoA-I remains controversial [28, 30, 31]. The presence of sialic acids at the termini of N-glycans may play a role in HDL metabolism.
Metabolism
Production
HDL production combines several multistep processes that rely on membrane-bound and plasma proteins and predominantly involves apoA-I, the major HDL component. ApoA-I is mainly produced and secreted by the liver and the intestine (Fig. 18.1). The liver is traditionally considered as the principal site of apoA-I production in humans; strikingly however, the amounts of apoA-I produced by the liver and the intestine are comparable [32].
Major pathways of normal and altered HDL metabolism (a), together with sites of action of HDL-targeting agents (b). (1) ApoA-I is secreted by hepatocytes and intestinal cells, in a lipid-free and/or lipid-poor (pre-beta) form. This pathway can be impaired in apoA-I deficiency, leading to low HDL-C and can be rescued by rHDL infusions to expand plasma pool of lipid-poor particles, or by agents enhancing apoA-I production. (2) Lipid-free and/or lipid-poor HDL are catabolised via kidneys. This pathway can be accelerated in dyslipidemic and inflammatory states, leading to low HDL-C. (3) ApoA-I lipidation occurs upon interaction with ABCA1, resulting in the formation of lipid-poor, discoid HDL particles. This pathway can be impaired in ABCA1 deficiency (Tangier disease), leading to low HDL-C. (4) Esterification of discoid HDL cholesterol catalysed by LCAT leads to the formation of HDL lipid core primarily composed of cholesteryl ester; HDL particles grow in size and become small, dense, lipid-poor spherical HDL3 and large, light, lipid-rich spherical HDL2. This pathway can be impaired in LCAT and apoA-I deficiency, leading to low HDL-C and can be rescued by infusions of recombinant LCAT. Both HDL3 and, particularly, HDL2 can accept cellular cholesterol and phospholipid via ABCG1- and SR-BI-mediated pathways, increasing HDL lipid load. (5) SAA produced by the liver displaces apoA-I in HDL under inflammatory conditions, with loss of apoA-I by the renal catabolism. This pathway can be accelerated in dyslipidemic and inflammatory states, leading to low HDL-C and can be normalized by anti-inflammatory agents. (6) Spherical HDL2 and HDL3 are remodelled by CETP which ensures cholesteryl ester transfer from HDL to TGRL and reciprocal triglyceride transfer; as a result, HDL particles become depleted in cholesteryl ester and enriched in triglyceride. This pathway can be accelerated in dyslipidemic and inflammatory states, leading to low HDL-C and can be normalized by CETP inhibitors. This pathway can also be delayed in CETP deficiency, leading to extremely high HDL-C. (7) Hydrolysis of TGRL by LPL induces transfer of surface apolipoproteins, phospholipid and free cholesterol to the plasma HDL pool. This pathway can be inhibited in LPL deficiency, leading to low HDL-C and can be rescued by apoC-III inhibition and LPL activation. This pathway can also be accelerated in apoC-III deficiency, leading to high HDL-C. (8) LDL and TGRL remnants are removed from the circulation via the LDL receptor (LDL-R). This pathway can be delayed in dyslipidemic states, including familial hypercholesterolemia (FH), and can be normalized by statins. (9) VLDL are produced and secreted by the liver. This pathway can be accelerated in dyslipidemic states, leading to hypertriglyceridemia and can be normalized by niacin. (10) Lipids in mature spherical HDL are hydrolysed by HL and EL to produce smaller HDL particles. This pathway can be accelerated in dyslipidemic states, leading to low HDL-C. This pathway can also be delayed in HL and EL deficiency, leading to high HDL-C. (11) Selective uptake of HDL cholesteryl ester via SR-BI recycles small, lipid-poor HDL subspecies and lipid-free/lipid-poor apoA-I. This pathway can be delayed in SR-BI deficiency, leading to extremely high HDL-C. Particle transformations and mass transfers are shown as solid and dotted lines, respectively. HDL components are listed in orange, enzymes and lipid transfer proteins are in blue, HDL-targeting therapies are in green and genetic deficiencies are in red. Abbreviations: A-I apoA-I, CE cholesteryl ester, CETPi CETP inhibitors, FC free cholesterol, FH familial hypercholesterolemia, HDL-R holoparticle HDL receptor, LDL-R LDL receptor, PL phospholipid, rLCAT recombinant LCAT, TG triglyceride
ApoA-I secreted by hepatocytes is either lipid-free or lipid-poor and needs to be lipidated in order to form HDL. Such HDL assembly typically occurs at the cell surface and begins with the transfer of membrane phospholipids and cholesterol to apoA-I. This process involves interaction of apoA-I with cell-surface ATP-binding cassette transporter A1 (ABCA1; Fig. 18.1). ABCA1 is a ubiquitous transmembrane protein which functions as a membrane phospholipid translocase whose enzymatic activity leads to the transfer of phospholipid molecules across a cell plasma membrane [33]. The presence of active ABCA1 promotes binding of apoA-I to the cell surface, predominantly to lipid domains in the membrane that are created by the activity of ABCA1 and only in a minor part to ABCA1 to stabilize the transporter. As a result of such interactions, heterogeneous populations of discoid nascent HDL particles are formed. ABCA1 thereby promotes the transfer of phospholipid and cholesterol from plasma membrane to lipid-free apolipoproteins or lipid-poor HDL that readily interact with ABCA1 in a process which is critical for plasma HDL metabolism [33]. Indeed, ABCA1-mediated lipidation of apoA-I increases the stability of the apolipoprotein in the circulation, preventing its rapid elimination through the kidney. Apolipoproteins other than apoA-I, including apoA-II, apoA-V, apoC-I, apoC-II, apoE and apoM, are also capable of forming nascent HDL upon interaction with ABCA1, indicating that they are also important in the HDL formation.
In the next step, free cholesterol is transferred from the polar surface monolayer to the non-polar hydrophobic core as a result of esterification by LCAT, thereby creating spherical HDL possessing a hydrophobic core (Fig. 18.1). This reaction delays catabolism of discoid HDL, allowing progression to HDL maturation. As a result, spherical HDL particles displaying slow catabolic rate comprise the major fraction of plasma HDL. Interestingly, other HDL subpopulations are similarly metabolized within discrete, stable-size pools with little interconversion between them [34].
ApoA-I secreted by the intestine is predominantly present in chylomicrons; some part of intestinally synthesized apoA-I is carried by discoid HDL [35]. Together with apoB-48 and apoCs, apoA-I represents a major component of chylomicrons, accounting for up to 20 wt% of their protein [35]. This frequently neglected observation emphasizes physiologic importance of intestinally derived apoA-I in the HDL metabolism.
LPL is expressed in heart, muscle and adipose tissue and hydrolyses triglycerides carried by chylomicrons and very low-density lipoproteins (VLDL), producing free fatty acids for tissue cells. No other metabolic pathway can substitute for the LPL-catalysed lipid hydrolysis, rendering proper LPL functionality essential for energy production. In this pathway, LPL adds phospholipid, free cholesterol and apolipoproteins from the surface of TGRL to the circulating HDL pool (Fig. 18.1). Indeed, apoA-I and several other apolipoproteins readily move between lipoprotein particles and can be exchanged between TGRL and HDL. These processes are active in the both post- and interprandial phases, providing a quantitatively major contribution to HDL-C. Consistently, LPL activity is strongly correlated with HDL-C concentrations in healthy individuals [36].
Remodelling and Catabolism
Remodelling and catabolism of HDL are ensured by interactions with cellular receptors, transporters, plasma proteins and enzymes. Mature spherical HDL can further grow via efflux of cellular cholesterol and phospholipid through ATP-binding cassette transporter G1 (ABCG1; Fig. 18.1) [37]. In addition, cells possessing scavenger receptor class B type I (SR-BI) can transfer membrane cholesterol to spherical HDL in a process of passive diffusion according to concentration gradients (Fig. 18.1) [38].
In the circulation, HDL is extensively remodelled by lipid transfer proteins. Plasma CETP primarily transfers cholesteryl ester from mature spherical HDL to apoB-containing particles, particularly VLDL, in exchange for triglyceride [39]. As a result of CETP activity, HDL becomes depleted of cholesteryl ester and enriched in triglyceride, which accelerates HDL catabolism (Fig. 18.1). PLTP converts spherical HDL into both larger and smaller particles as well as transfers to HDL phospholipids which are removed from apoB-containing lipoproteins during lipolysis by LPL [39].
Both surface and core lipids of HDL are extensively modified by lipases. HL breaks down primarily tri- and diglycerides but also phospholipids of HDL, resulting in the reduction of HDL particle size (Fig. 18.1). Endothelial lipase (EL) primarily hydrolyses HDL phospholipids but also triglycerides. Upon interaction with the surface of hepatocytes, cholesteryl esters are transmitted from cholesterol-rich HDL to the liver by their selective uptake via SR-BI (Fig. 18.1). The activity of SR-BI in the selective cholesterol uptake leads to the formation of small, dense HDL particles depleted of cholesterol. Albeit extensively studied, this pathway represents a minor route of cholesteryl ester elimination from the circulation in humans, whereas the transfer of cholesteryl ester to apoB-containing lipoproteins by CETP with subsequent hepatic uptake of LDL quantitatively prevails [6]. Finally, large apoE-containing HDL can be internalized via interaction with apoB/apoE receptors [40].
Following removal through the liver, HDL-derived cholesterol is secreted into the bile [41]. In a non-biliary pathway, direct excretion of cholesterol occurs in the proximal small intestine. The major sites of catabolism of the protein HDL components are the liver and the kidney [6]. HDL particles can be removed from the circulation by holo-particle HDL receptors, such as cubilin present in kidney proximal tubules and the ectopic β-chain of ATP synthase at the surface of hepatocytes (Fig. 18.1).
Biological Activities of Normal Functional HDL
Plasma HDL displays multiple cardioprotective activities which may act cooperatively to ensure normal vascular function. However, it is challenging to determine their relative contributions to the vascular health. HDL is predominantly thought of as a lipid-carrying particle which is crucial in cholesterol clearance and metabolism [42]. Indeed, as peripheral mammalian cells cannot catabolize cholesterol to keep it at non-toxic levels, HDL can be essential for maintaining healthy levels of cholesterol in peripheral tissues through a pathway of reverse cholesterol transport (RCT), whereby HDL effluxes superfluous cholesterol from cells to transport it to the liver for excretion. However, diverse HDL components endow HDL with multiple cardioprotective activities beyond its role in RCT through inhibiting inflammation, thrombosis, cell death, acute-phase response and oxidative damage [6].
As a consequence, HDL particles display protective effects towards the endothelium. HDL-mediated removal of cellular cholesterol contributes to vasodilation. HDL particles equally protect the endothelium by suppressing superoxide production and expression of proinflammatory cytokines in both macrophages and endothelial cells [43]. Anti-thrombotic actions of HDL particles are largely attributed to their effect on platelets [44]. Through enhancing the production of nitric oxide and prostacyclin, HDL can attenuate platelet aggregation [43, 44].
Next, HDLs display anti-apoptotic effects, inhibiting apoptosis of endothelial and vascular smooth muscle cells on the one hand, and, on the other hand, enhancing their proliferation and migration [43]. SR-BI-initiated signalling pathway plays an important role in these protective effects.
HDLs beneficially influence insulin sensitivity. This effect may be underlain by enhanced glucose uptake in adipose tissues and accelerated insulin secretion from the pancreas [45].
HDL may protect against infections, such as via LBP and a specific apoL-I-containing lytic factor for Trypanosoma brucei [6]. This role of HDL is consistent with the hypothesis that HDL has evolved as a component of innate immunity [46].
As biological activities of HDL are defined by its composition, revealing relationships between composition, structure and function of HDL is critical for our understanding of HDL biology. ApoA-I provides a key contribution to multiple biological activities of HDL, which involve lipid binding [47]. Other apolipoproteins, including apoA-II, apoA-IV, apoC-I, apoE and apoM, can also ensure cellular cholesterol efflux. Several HDL apolipoproteins, particularly apoE, apoA-IV, apoA-V, apoJ, apoC-I, apoC-II, and apoC-III, display antioxidative activity, whereas apoJ and apoE protect endothelial cells from dysfunction and apoptosis. Cholesterol efflux capacity and cholesterol transport to the liver for excretion are largely related to proteins harboured by HDL [6].
HDL particles are heterogeneous in structure and composition; as a consequence, their biological activities equally differ across HDL subpopulations. Importantly, small, dense, protein-rich HDL display potent anti-atherogenic activities, consistent with their distinct content of multiple protein and lipid components [26].
Abnormal HDL Metabolism
Epidemiology of HDL
Altered HDL metabolism is manifested in abnormal levels of HDL-C, which can be either reduced or elevated as compared to healthy subjects. Low circulating levels of HDL-C are widely accepted as a strong and independent predictor of CVD as shown in large-scale cross-sectional and prospective studies, including the Framingham Heart Study and the PROCAM Study [48, 49]. Low HDL-C is a risk factor for multiple vascular diseases, including myocardial infarction, peripheral artery disease, ischemic stroke and deep vein thrombosis [6]. The inverse relationship between HDL-C and CV risk persists across multiple populations, ethnicities and disease states. Reflecting such robust data, HDL-C levels are included in all major algorithms to estimate CV risk, such as the Framingham risk prediction tool, the PROCAM score and the SCORE approach.
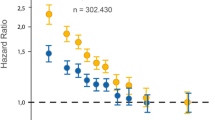
Low HDL-C levels are frequently observed in general populations and persist despite statin treatment [6]. By contrast, extremely high HDL-C is a rare condition; this observation hampered large-scale epidemiological studies of high HDL-C levels. Recently, several studies reported deleterious role of extremely high HDL-C for overall and CV mortality, resulting in the U-shape of the relationship between CV risk and HDL-C [50,51,52].
Epidemiologic studies of HDL are however limited by extensive confounding. Indeed, HDL-C levels are strongly linked to obesity, insulin resistance, exercise, and alcohol consumption, all of which feature elevated plasma triglyceride levels. It is important in this regards that genetic epidemiology does not necessarily support causal relationships between HDL-C and CV risk. Indeed, no association between HDL-C levels and CVD was observed in a large study using Mendelian randomization [53], suggesting that low HDL-C is not causatively related to atherosclerosis [54].
Measurement of apoA-I constitutes an acceptable alternative to the use of HDL-C in assessing CV risk. Evidence supporting the preferential use of apoA-I over HDL-C is however not yet conclusive [55].
Circulating concentrations of HDL subpopulations can also be employed to evaluate CV risk. Thus, both HDL2- and HDL3-cholesterol constitute strong predictors of coronary heart disease [16]. Plasma levels of large α1-HDL are consistently associated with protection from atherosclerosis [16]. Similarly, levels of large HDL measured by NMR typically display negative correlations with CV risk [16]. In addition, elevated levels of apoC-III-containing HDL may represent an important determinant of CVD [56]. However, clinical value of HDL subpopulations relative to that of plasma HDL-C remains to be firmly established.
Pathways of Abnormal HDL Metabolism
Studies of both rare genetic disorders and genetic associations are useful for identifying factors involved in HDL metabolism. HDL-C concentrations are under strong genetic control; effects of the majority of common gene variants on HDL-C are small, whereas effects of some rare variants can be pronounced.
Low HDL-C States
Homozygous or compound heterozygous apoA-I deficiency is a rare condition which results in complete absence of apoA-I from plasma accompanied by a marked decrease in HDL-C and increased risk of premature CVD [57]. Subjects with heterozygous forms of apoA-I deficiency feature plasma HDL-C and apoA-I levels that are about 50% of normal. HDL biogenesis is disrupted in apoA-I deficiency as a result of abnormal HDL production and deficient LCAT activation by apoA-I (Fig. 18.1). Remarkably, some rare variants of apoA-I, including apoA-I Milano and apoA-I Paris, are paradoxically associated with low HDL-C levels and reduced risk of CVD paralleled by greater longevity [58].
Most known ABCA1 mutations result in Tangier disease associated with the deficiency in cellular cholesterol efflux to lipid-free and lipid-poor apolipoproteins (Fig. 18.1) [59]. Low HDL-C is a common characteristic of ABCA1 deficiency, frequently resulting in elevated CV risk [59].
Naturally occurring mutations in LCAT are another common cause of low plasma HDL-C (Fig. 18.1) [60]. Familial LCAT deficiency results from the complete loss of LCAT activity, while fish-eye disease is associated with a change in the substrate specificity of LCAT that becomes inactive towards HDL, while retaining its cholesteryl ester-generating activity towards apoB-containing lipoproteins. The latter property can be important in accelerating atherosclerosis in fish-eye disease relative to familial LCAT deficiency [61]. In these diseases, plasma HDL-C and apoA-I levels are reduced, while plasma-free cholesterol is elevated.
Genetic defects of LPL may lead to hypertriglyceridemia and low HDL-C [62]. Thus, familial LPL deficiency is a rare disorder characterized by severe hypertriglyceridemia and marked reductions in HDL-C and LDL-C levels. Reduced LPL activity contributes to HDL-C lowering by reducing the availability of surface constituents of TGRL (Fig. 18.1) [63].
Genetically determined elevated CETP activity leads to decreased concentrations of HDL-C and hypertriglyceridemia (Fig. 18.1) [64]. HDL metabolism is substantially altered in dyslipidemic states of hypertriglyceridemia and insulin resistance , reflecting rapid removal from the circulation of small HDL particles which result from the intravascular lipolysis of triglyceride-enriched HDL. In hypercholesterolemia , abnormalities in HDL metabolism are primarily observed as moderate reductions in plasma apoA-I and HDL-C levels.
Finally, decrease in circulating HDL-C levels, increase in triglyceride levels and HDL enrichment in SAA at the expense of apoA-I are typical components of inflammatory states and the acute phase reaction [65].
High HDL-C States
Mutations that reduce CETP activity lead to elevated plasma HDL-C (Fig. 18.1) [66]. Homozygous CETP deficiency can be associated with complete loss of CETP activity, leading to the accumulation of large, cholesteryl ester-rich HDL and elevation of HDL-C levels up to fivefold, which do not reduce CV risk. By contrast, common CETP genotypes, including TaqIB, I405V and 629C > A, associated with lower CETP activity and higher HDL-C levels are inversely related to coronary risk [66]. However, concomitant reductions in apoB-containing lipoproteins (which may also occur in other states of abnormal HDL metabolism) complicate proper evaluation of the role of HDL-C raising in CETP deficiency. Loss-of-function mutations in SR-BI similarly result in markedly increased HDL-C levels (Fig. 18.1) which may [67], or may not [68], be associated with elevated risk of CVD.
Loss-of-function mutations in apoC-III lead to increased HDL-C and reduced triglyceride and LDL-C concentrations [69]. These effects are associated with reduced risk of CVD [69, 70].
Complete HL deficiency is a rare autosomal recessive condition resulting in elevated plasma concentrations of HDL-C and apoA-I with the accumulation of large HDL [62]. EL deficiency may equally induce hyperalphalipoproteinaemia [62]. However, HDL-C raising resulting from such mutations is not necessarily atheroprotective [53, 71].
Altered Structure, Composition and Function of HDL
All major atheroprotective functions of HDL, including cholesterol efflux capacity as well as other activities, can become deficient under conditions favouring accelerated development of CVD. Such proatherogenic conditions primarily involve atherogenic dyslipidaemia, insulin resistance, inflammation and infection, which often, but not always, feature low HDL-C levels [6]. Under these conditions, structure and particle profile of HDL are modified in such a way that functionally deficient small particles possessing abnormal composition and conformationally altered apoA-I preferentially accumulate at the expense of their large counterparts [72].
The capacity of the plasma HDL pool to remove cholesterol from peripheral cells can be reduced as a result of diminished circulating levels of HDL particles (i.e., diminished HDL quantity). The link between reduction in plasma HDL levels, impairment of normal clearance of cholesterol from the arterial wall and acceleration of atherosclerosis was proposed by Miller and Miller in 1975 [4]. An assay that quantifies clinically relevant functional properties of HDL (i.e., diminished HDL quality) rather than its plasma concentrations can however be more appropriate for the evaluation of CV risk. A considerable body of evidence points to cellular cholesterol efflux from macrophages as a biomarker of beneficial effects of HDL on CV health [73, 74]. The negative relationship between cholesterol efflux capacity of HDL and both the presence of CVD and the risk of future CV events is frequently independent of HDL-C concentrations [73, 74], additionally suggesting that low levels of HDL-C can represent a crude biomarker of impaired HDL function rather than be causally related to CVD.
Monogenetic forms of low HDL-C dyslipidaemia, such as apoA-I or LCAT deficiency, can be equally characterized by the presence of HDL with defective intrinsic cholesterol efflux capacity. HDL particles are also deficient in antioxidative activity in dyslipidemic states involving low HDL-C levels, often in association with insulin resistance [72].
Altered composition of HDL, primarily depletion of apoA-I paralleled by its oxidation and glycation as well as alterations in the HDL lipidome, typically underlies functional deficiency of HDL [6]. Furthermore, functionally relevant alterations in the HDL proteome occur under pro-atherogenic conditions [75], while inflammation-induced modifications of HDL composition may further contribute to HDL dysfunction [76]. In particular, SAA can replace apoA-I in HDL, attenuating anti-inflammatory properties of the lipoprotein, whereas deficiency in PON1, PAF-AH and/or LCAT can contribute to the impairment of HDL capacity to reduce oxidation [76]. In addition, HDL glycome can be altered under pathological conditions, bearing a potential to aggravate functional HDL deficiency. Such alterations may include desialylation which decreases size and negative charge of HDL and alters interactions with lipases and cellular proteins, resulting in diminished cholesterol efflux capacity and reduced LCAT activity [29].
Importantly, clinical relevance of impaired antiatherogenic activities of HDL in cardiometabolic diseases largely remains indeterminate. Indeed, the very concept of HDL dysfunction has been developed using ex vivo assays; it is unclear whether HDL particles are also dysfunctional in a setting of a living organism.
Therapeutic Correction of Abnormal HDL Metabolism
Reflecting growing knowledge of HDL, development of HDL-targeting therapeutics has been concentrated around several major directions including inhibition of CETP, infusions of rHDL, activation of LPL and use of nicotinic acid, in addition to a broad variety of other strategies (Table 18.1) (Fig. 18.1).
CETP Inhibition
The first clinical trial attempting to intervene into this pathway of HDL metabolism was conducted with torcetrapib which was administrated to patients prone to coronary events whose HDL-C levels were increased by +72% and LDL-C levels decreased by −25% [77]. Unexpectedly, both overall and CV mortality were significantly elevated in the treatment arm relative to placebo. This deleterious effect was proposed to reflect off-target hypertensive effects of the drug [78].
Dalcetrapib , the second CETP inhibitor which entered clinical trials, raised HDL-C by +35% without affecting LDL-C levels. The development of the drug was discontinued due to the lack of positive effects on overall and coronary events–associated mortality [79]. The increase in HDL-C was suggested to be too modest for potential clinical benefits.
Evacetrapib , another CETP inhibitor, was investigated in high-risk patients with vascular disease and did not result in a lower rate of CV events, whilst showing large increases in HDL-C (+133%) and reductions in LDL-C (−31%) concentrations [80].
Anacetrapib , the most recent addition to the class of CETP inhibitors, was thoroughly tested for safety and was found to be clinically effective, decreasing incidence of major coronary events in the absence of increased risk of death, cancer, or other serious adverse events [81]. The beneficial effect of the drug was however modest (−9%) despite large increase in HDL-C (+104%); in addition, anacetrapib was found to accumulate in adipose tissue [82] and its development was stopped. The clinical benefit of anacetrapib could be accounted for by the reduction in non-HDL-C, and more specifically, small VLDL levels, suggesting little clinical role of the HDL-C raising [82]. Therefore, despite considerable initial promise, CETP inhibition provides insufficient CV benefit for clinical use.
rHDL Infusion
The first drug of this class entering clinical trials was ETC-216 comprised of apoA-I Milano protein supplied with a phospholipid [83]. The infusions of ETC-216 were able to decrease the mean atheroma volume in patients with acute coronary syndrome (ACS) [83]. However, the drug was not pushed into further clinical development primarily due to high production costs compared to its moderate clinical benefit. Furthermore, ETC-216 was responsible for a dose-dependent increase in neutrophils [84].
Seeking improvement in safety and efficacy, a formulation called MDCO-216 comprised of apoA-I Milano and phosphatidylcholine was introduced [85] which did not induce adverse immunostimulation [84], but neither showed effectiveness in a clinical setting [86].
The initial success with the trials of ETC-216 was followed by the development of CSL-111 consisting of normal human apoA-I combined with soybean phosphatidylcholine. Short-term infusions of CSL-111 did not reduce atheroma volume and were slightly hepatotoxic at high concentrations, but they did improve the plaque characterization index and coronary score [87]. The drug was reformulated as CSL-112 that did not contain hepatotoxic cholate and was essentially homogeneous in the particle size. In a phase II trial, CSL-112 was well tolerated and acutely enhanced cholesterol efflux in patients with CVD [88], probably acting via remodelling the circulating HDL pool through formation of small particles possessing enhanced anti-atherogenic activities [89].
Another infusion agent named CER-001 , a negatively charged rHDL containing human recombinant apoA-I, sphingomyelin and phosphatidylglycerol, was somewhat efficient in patients with extreme conditions including homozygous familial hypercholesterolemia [90] and extensive plaque-burdened ACS [91], but was eventually proven to be ineffective in patients with more typical presentation of ACS [92, 93].
A modification of HDL infusion therapy involved reinfusion of autologous delipidated HDL after their selective delipidation ex vivo [94]. This approach converted large, lipid-rich HDL to small, lipid-poor particles with enhanced atheroprotective activities [26] and tended to reduce total atheroma volume after seven weekly injections in ACS patients undergoing cardiac catheterization as compared to control plasma apheresis treatment [94].
ApoA-I-mimetic peptides structurally resemble apoA-I in the way that they all contain amphipathic α-helical structures albeit often do not share any sequence homology to apoA-I yet possessing similar biological function [95]. These agents can beneficially impact HDL metabolism upon infusion. Unlike recombinant or purified apoA-I proteins, apoA-I mimetics are short-chain and easy to produce. Moreover, they can be administered orally, though their oral bioavailability is limited [96]. Initial reports were promising on the effectiveness of these agents in animal models, but a recent report of aggregated results shows inconsistencies between in vitro and in vivo functional properties of seven apoA-I mimetic peptides [97].
Another therapeutic strategy features infusions of recombinant LCAT , a single HDL protein. A formulation called ACP-501 favourably modified HDL metabolism after a single intravenous infusion [98]; an approach involving multiple intravenous infusions is currently being assessed in a phase 2 trial.
To sum up, none of the HDL infusions has proven to be both effective and safe up to date; furthermore, intravenous infusions appeared to be too impractical for everyday therapy.
LPL Activation
Upregulation of LPL activity is normally considered as a means to reduce plasma triglycerides but this approach is highly effective in elevating HDL-C levels and can be added to the list of HDL-targeting therapies. ApoC-III represents a promising therapeutic target for the treatment of hypertriglyceridemia, as it inhibits TGRL hydrolysis by LPL [99]. Recent phase I trial of the administration of volanesorsen , an apoC-III antisense oligonucleotide in healthy subjects revealed reductions in plasma apoC-III and triglyceride levels accompanied by elevated HDL-C [99]. This approach is currently entering clinical trials [100].
Fibrates is a class of compounds that work by activating peroxisome proliferator-activated receptor α (PPARα). PPARα is active in hepatocytes where it stimulates production of apoA-I and apoA-II and inhibits production of apoC-III, thereby enhancing LPL activity [101]. As a result, fibrates increase concentrations of HDL-C and small pre-β1-HDL. Fibrates are normally considered for treatment of hypertriglyceridemia and provide moderate clinical benefits [102] but their side-effects include formation of cholesterol gallstones, rhabdomyolysis and myopathy. A novel member of this drug class, pemafibrate, did not show major adverse effects and recently passed phase 3 of clinical trials [103].
Another approach to combat hypertriglyceridemia employs an adenoviral vector AMT-011 expressing human LPL, with an intent to replace a faulty LPL gene with a properly functioning copy [104]. If successful, this strategy should equally be able to increase HDL-C.
Nicotinic Acid
In the pre-statin era, nicotinic acid , also known as niacin and vitamin B3, was considered as a promising candidate to prevent CVD, reflecting its ability to raise HDL-C, decrease triglycerides, alleviate carotid intima-media thickening and reduce incidence of stenosis [101]. However, recent large-scale studies performed in patients on statins failed to demonstrate clinical benefits of niacin treatment [105, 106]. In addition, Cochrane meta-analysis of long-term clinical trials did not find evidence for niacin’s efficiency in patients already treated with statins [107]. Prolonged exposure to niacin was also found to be associated with increased risk for onset of diabetes [107]. Despite these limitations, nicotinic acid may still be helpful for individuals not tolerating statins. Indeed, a meta-analysis reveals that niacin is capable of reducing CV events in the absence of statin treatment [108].
Other Agents
Other agents employed within the paradigm of HDL-targeting therapy can be classified into bromodomain and extra-terminal domain (BET) inhibitors, nuclear receptors agonists and miR inhibitors.
BETs are protein-interaction modules involved in chromatin organization and modulation of gene transcription. Apabetalone (RVX-208), a small BET inhibitor designed to directly upregulate hepatic secretion of apoA-I, moderately raised HDL-C and showed promising results in the early stages of clinical trials [109], but later failed to present significant clinical benefits compared to placebo [110]. In recent trials, vulnerability of atherosclerotic plaques was however favourably modified by apabetalone [111]. Pooled together, results from available clinical trials of apabetalone reveal a reduction in CV events relative to placebo [112].
Nuclear receptor agonists are represented by those acting on liver X receptor (LXR) and farnesoid X receptor (FXR). LXR agonists are activated by oxidized sterols, raise HDL-C and exert a multitude of antiatherogenic actions including beneficial effects on cholesterol metabolism, inflammation, proliferation and insulin sensitivity [113]. Major adverse effects of LXR agonists however involve hepatic steatosis and nervous system deficiency [114]. There are two LXR types, notably LXRα expressed in the liver, kidney, and several other organs, and LXRβ expressed ubiquitously [115]. Importantly, specific activation of LXRα receptors retains beneficial effects on HDL whilst lacking lipogenic effects and may represent a promising strategy of dyslipidaemia treatment.
FXR agonists are bile acid-activated nuclear receptors implicated in the regulation of cholesterol metabolism [116]. FXR activation reduces lipid synthesis and storage and ameliorates insulin resistance. As a result, FXR agonists increase faecal cholesterol excretion and reduce intestinal cholesterol reuptake, positively influencing net cholesterol metabolism. The major side effects of FXR activation are represented by the inhibition of bile acid synthesis and reduction of HDL-C [117].
MiRs are small RNAs that do not code proteins, and, hence, were earlier considered as ‘junk RNA’ to be later discovered to play important biological role in the development, repair and homeostasis. HDL transports miRs, one of which, miR-33, inhibitsABCA1 expression [118, 119]. Although animal models support the role of miR-33 as a potential therapeutic target for HDL biogenesis, the efficacy of this approach in humans remains to be established.
Conclusions
The research of HDL passed through a full cycle of discovery, data accumulation, drug development and clinical application. Yet after almost a century of studies, the available knowledge is still controversial. Most importantly, it remains unclear why HDL-targeting therapies do not provide expected clinical benefits despite robust epidemiological findings linking low HDL-C to CVD.
The simplest explanation is that HDL-C-raising resulted in deleterious off-target effects as observed with torcetrapib which increased blood pressure in atherosclerotic patients [77]. Other therapies did not however reveal major adverse effects, discounting this possibility. It is also possible that potential clinical benefits were abolished by the statin treatment. Indeed, all recent studies of HDL-targeting agents were performed in patients treated by statins which markedly modify lipoprotein metabolism. For example, statin therapy interferes with ABCA1-mediated macrophage cholesterol efflux and may thereby diminish anti-atherogenic function of HDL [120]. Furthermore, combined exposure to gene variants that encode targets of CETP inhibitors and statins was associated with discordant reductions in LDL-C and apoB levels and a corresponding risk of CV events that was proportional to the attenuated reduction in apoB but was significantly less than expected per unit change in LDL-C, weakening potential benefits of CETP inhibition [121].
Another possibility involves confinement of benefits to specific subgroups. Thus, patients homozygous for a variant in the ADCY9 gene responded positively to dalcetrapib and experienced a significant reduction in CV event under the drug [122]. In the torcetrapib trials, patients with highest HDL-C on-treatment levels were less likely to suffer major CV events or death, or to display atherosclerosis progression [123]. In the AIM-HIGH niacin trial, a significant 33% decrease in primary events in the niacin group beyond that conferred by statins alone was observed in patients with elevated triglyceride and reduced HDL-C levels [105]. Given that thorough subgroup analyses were performed in the large-scale studies, this possibility still looks remote.
Accumulation of dysfunctional HDL particles was invoked as another explanation of the failure of HDL-targeting therapeutics. It is however highly unlikely that mechanistically distinct HDL-C-raising agents all result in the formation of dysfunctional HDL. Consistent with this notion, available data do not detect dysfunctional HDL on treatment [124].
Given the high heterogeneity of HDL particles, it is possible that clinical studies did not target right HDL populations. Indeed, while therapeutic HDL-C-raising predominantly increases levels of large HDL, elevated anti-atherogenic activities are ascribed to small, dense, protein-rich particles [26]. Data directly supporting this hypothesis is however lacking.
The recent discovery of the U-shape relationship between HDL-C and CVD [50, 51] suggest an intriguing possibility that HDL-C-raising achieved on treatment was excessive. Epidemiology of genetically determined extremely high HDL-C is in part consistent with this suggestion which requires rigorous testing.
The last possibility is that HDL-C is not causatively related to CVD and represents a biomarker for elevated triglycerides [54], implying that HDL-C-raising per se is meaningless. In support of this hypothesis, Mendelian randomization studies often do not detect causal relationships between HDL-C and CVD [54]. Complex metabolic network underlying HDL metabolism is however not taken into account by these considerations.
Following the largely disappointing results of the clinical studies, the focus of HDL therapeutics is now shifting from the mere increase in HDL-C concentrations to the normalization of cardioprotective HDL functionality, primarily of cellular cholesterol efflux capacity of HDL. This shift of paradigm implies that a continuous, slow, steady-state flux through the dynamic RCT pathway is more important for the relationship between HDL-C and CVD than static levels of HDL-C, rendering HDL-C of secondary clinical significance [73, 74]. However, key metabolic links between HDL-C and triglycerides [54] are eloquently absent from this hypothesis, clearly demonstrating that HDL remains an exceedingly intriguing therapeutic target to reduce CV risk despite decades of intense research. Ongoing controversies between classic epidemiology, genetic epidemiology and clinical trials need to be urgently resolved in order to allow further development of HDL-targeting therapies.
References
Marcheboeuf M. Recherches sur les phosphoaminolipides et les stérides du sérum et du plasma sanguins; entraînement des phospholipides, des stérols et des stérides par les diverses fractions au cours du fractionnement des protéines du sérum. Bull Soc Chim Biol. 1929;11:268–93.
Jones HB, Gofman JW, Lindgren FT, Lyon TP, Graham DM, Strisower B, et al. Lipoproteins in atherosclerosis. Am J Med. 1951;11(3):358–80.
Barr DP, Russ EM, Eder HA. Protein-lipid relationships in human plasma: II. In atherosclerosis and related conditions. Am J Med. 1951;11(4):480.
Miller GJ, Miller NE. Plasma-high-density-lipoprotein concentration and development of ischaemic heart-disease. Lancet. 1975;1(7897):16–9.
Gordon DJ, Probstfield JL, Garrison RJ, Neaton JD, Castelli WP, Knoke JD, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79(1):8–15.
Kontush A, Chapman MJ. High-density lipoproteins: structure, metabolism, function and therapeutics. New York: Wiley; 2012. 648 p.
Wlodawer A, Segrest JP, Chung BH, Chiovetti R Jr, Weinstein JN. High-density lipoprotein recombinants: evidence for a bicycle tire micelle structure obtained by neutron scattering and electron microscopy. FEBS Lett. 1979;104(2):231–5.
Kontush A, Lindahl M, Lhomme M, Calabresi L, Chapman MJ, Davidson WS. Structure of HDL: particle subclasses and molecular components. Handb Exp Pharmacol. 2015;224:3–51.
Segrest JP, Jones MK, Klon AE, Sheldahl CJ, Hellinger M, De Loof H, et al. A detailed molecular belt model for apolipoprotein A-I in discoidal high-density lipoprotein. J Biol Chem. 1999;274(45):31755–8.
Bhat S, Sorci-Thomas MG, Alexander ET, Samuel MP, Thomas MJ. Intermolecular contact between globular N-terminal fold and C-terminal domain of ApoA-I stabilizes its lipid-bound conformation: studies employing chemical cross-linking and mass spectrometry. J Biol Chem. 2005;280(38):33015–25.
Wu Z, Wagner MA, Zheng L, Parks JS, Shy JM 3rd, Smith JD, et al. The refined structure of nascent HDL reveals a key functional domain for particle maturation and dysfunction. Nat Struct Mol Biol. 2007;14(9):861–8.
Silva RA, Huang R, Morris J, Fang J, Gracheva EO, Ren G, et al. Structure of apolipoprotein A-I in spherical high-density lipoproteins of different sizes. Proc Natl Acad Sci U S A. 2008;105(34):12176–81.
Wu Z, Gogonea V, Lee X, May RP, Pipich V, Wagner MA, et al. The low resolution structure of ApoA1 in spherical high density lipoprotein revealed by small angle neutron scattering. J Biol Chem. 2011;286(14):12495–508.
Huang R, Silva RA, Jerome WG, Kontush A, Chapman MJ, Curtiss LK, et al. Apolipoprotein A-I structural organization in high-density lipoproteins isolated from human plasma. Nat Struct Mol Biol. 2011;18(4):416–22.
Chetty PS, Nguyen D, Nickel M, Lund-Katz S, Mayne L, Englander SW, et al. Comparison of apoA-I helical structure and stability in discoidal and spherical HDL particles by HX and mass spectrometry. J Lipid Res. 2013;54(6):1589–97.
Rosenson RS, Brewer HB Jr, Chapman MJ, Fazio S, Hussain MM, Kontush A, et al. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin Chem. 2011;57(3):392–410.
Jakubowski H. Calcium-dependent human serum homocysteine thiolactone hydrolase. A protective mechanism against protein N-homocysteinylation. J Biol Chem. 2000;275(6):3957–62.
Qiu X, Mistry A, Ammirati MJ, Chrunyk BA, Clark RW, Cong Y, et al. Crystal structure of cholesteryl ester transfer protein reveals a long tunnel and four bound lipid molecules. Nat Struct Mol Biol. 2007;14(2):106–13.
Vaisar T, Pennathur S, Green PS, Gharib SA, Hoofnagle AN, Cheung MC, et al. Shotgun proteomics implicates protease inhibition and complement activation in the anti-inflammatory properties of HDL. J Clin Invest. 2007;117(3):746–56.
Wurfel MM, Kunitake ST, Lichenstein H, Kane JP, Wright SD. Lipopolysaccharide (LPS)-binding protein is carried on lipoproteins and acts as a cofactor in the neutralization of LPS. J Exp Med. 1994;180(3):1025–35.
Davidson WS, Silva RAGD, Chantepie S, Lagor WR, Chapman MJ, Kontush A. Proteomic analysis of defined HDL subpopulations reveals particle-specific protein clusters: relevance to antioxidative function. Arterioscler Thromb Vasc Biol. 2009;29(6):870–6.
Furtado JD, Yamamoto R, Melchior JT, Andraski AB, Gamez-Guerrero M, Mulcahy P, et al. Distinct proteomic signatures in 16 HDL (high-density lipoprotein) subspecies. Arterioscl Thromb Vasc Biol. 2018;38(12):2827–42.
Cheung MC, Vaisar T, Han X, Heinecke JW, Albers JJ. Phospholipid transfer protein in human plasma associates with proteins linked to immunity and inflammation. Biochemistry. 2010;49(34):7314–22.
Wiesner P, Leidl K, Boettcher A, Schmitz G, Liebisch G. Lipid profiling of FPLC-separated lipoprotein fractions by electrospray ionization tandem mass spectrometry. J Lipid Res. 2009;50(3):574–85.
Kontush A, Lhomme M, Chapman MJ. Unraveling the complexities of the HDL lipidome. J Lipid Res. 2013;54(11):2950–63.
Camont L, Lhomme M, Rached F, Le Goff W, Negre-Salvayre A, Salvayre R, et al. Small, dense high-density lipoprotein-3 particles are enriched in negatively charged phospholipids: relevance to cellular cholesterol efflux, antioxidative, antithrombotic, anti-inflammatory, and antiapoptotic functionalities. Arterioscler Thromb Vasc Biol. 2013;33(12):2715–23.
Lucke S, Levkau B. Endothelial functions of sphingosine-1-phosphate. Cell Physiol Biochem. 2010;26(1):87–96.
Krishnan S, Huang J, Lee H, Guerrero A, Berglund L, Anuurad E, et al. Combined high-density lipoprotein proteomic and glycomic profiles in patients at risk for coronary artery disease. J Proteome Res. 2015;14(12):5109–18.
Sukhorukov V, Gudelj I, Pucic-Bakovic M, Zakiev E, Orekhov A, Kontush A, et al. Glycosylation of human plasma lipoproteins reveals a high level of diversity, which directly impacts their functional properties. Biochim Biophys Acta Mol Cell Biol Lipids. 2019;1864(5):643–53.
Krishnan S, Shimoda M, Sacchi R, Kailemia MJ, Luxardi G, Kaysen GA, et al. HDL glycoprotein composition and site-specific glycosylation differentiates between clinical groups and affects IL-6 secretion in lipopolysaccharide-stimulated monocytes. Sci Rep. 2017;7:43728.
Majek P, Pecankova K, Maly M, Oravec M, Riedel T, Dyr JE. N-glycosylation of apolipoprotein A1 in cardiovascular diseases. Transl Res. 2015;165(2):360–2.
Bisgaier CL, Glickman RM. Intestinal synthesis, secretion, and transport of lipoproteins. Annu Rev Physiol. 1983;45:625–36.
Phillips MC. Is ABCA1 a lipid transfer protein? J Lipid Res. 2018;59(5):749–63.
Mendivil CO, Furtado J, Morton AM, Wang L, Sacks FM. Novel pathways of apolipoprotein A-I metabolism in high-density lipoprotein of different sizes in humans. Arterioscler Thromb Vasc Biol. 2016;36(1):156–65.
Field FJ, Mathur SN. Intestinal lipoprotein synthesis and secretion. Prog Lipid Res. 1995;34(2):185–98.
Nikkila EA, Taskinen MR, Sane T. Plasma high-density lipoprotein concentration and subfraction distribution in relation to triglyceride metabolism. Am Heart J. 1987;113(2 Pt 2):543–8.
Yvan-Charvet L, Wang N, Tall AR. Role of HDL, ABCA1, and ABCG1 transporters in cholesterol efflux and immune responses. Arterioscler Thromb Vasc Biol. 2010;30(2):139–43.
Hoekstra M. SR-BI as target in atherosclerosis and cardiovascular disease - a comprehensive appraisal of the cellular functions of SR-BI in physiology and disease. Atherosclerosis. 2017;258:153–61.
Lewis GF, Rader DJ. New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res. 2005;96(12):1221–32.
Hatters DM, Peters-Libeu CA, Weisgraber KH. Apolipoprotein E structure: insights into function. Trends Biochem Sci. 2006;31(8):445–54.
Dikkers A, Tietge UJ. Biliary cholesterol secretion: more than a simple ABC. World J Gastroenterol. 2010;16(47):5936–45.
Rosenson RS, Brewer HB Jr, Davidson WS, Fayad ZA, Fuster V, Goldstein J, et al. Cholesterol efflux and atheroprotection: advancing the concept of reverse cholesterol transport. Circulation. 2012;125(15):1905–19.
Mineo C, Shaul PW. Role of high-density lipoprotein and scavenger receptor B type I in the promotion of endothelial repair. Trends Cardiovasc Med. 2007;17(5):156–61.
Nofer JR, Brodde MF, Kehrel BE. High-density lipoproteins, platelets and the pathogenesis of atherosclerosis. Clin Exp Pharmacol Physiol. 2010;37(7):726–35.
Brunham LR, Kruit JK, Pape TD, Timmins JM, Reuwer AQ, Vasanji Z, et al. Beta-cell ABCA1 influences insulin secretion, glucose homeostasis and response to thiazolidinedione treatment. Nat Med. 2007;13(3):340–7.
Esteve E, Ricart W, Fernandez-Real JM. Dyslipidemia and inflammation: an evolutionary conserved mechanism. Clin Nutr. 2005;24(1):16–31.
Kontush A. HDL-mediated mechanisms of protection in cardiovascular disease. Cardiovasc Res. 2014;103(3):341–9.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62(5):707–14.
Assmann G, Schulte H, von Eckardstein A, Huang Y. High-density lipoprotein cholesterol as a predictor of coronary heart disease risk. The PROCAM experience and pathophysiological implications for reverse cholesterol transport. Atherosclerosis. 1996;124 Suppl:S11–20.
Ko DT, Alter DA, Guo H, Koh M, Lau G, Austin PC, et al. High-density lipoprotein cholesterol and cause-specific mortality in individuals without previous cardiovascular conditions: the CANHEART study. J Am Coll Cardiol. 2016;68(19):2073–83.
Madsen CM, Varbo A, Nordestgaard BG. Extreme high high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017;38(32):2478–86.
Bowe B, Xie Y, Xian H, Balasubramanian S, Zayed MA, Al-Aly Z. High density lipoprotein cholesterol and the risk of all-cause mortality among US veterans. Clin J Am Soc Nephrol. 2016;11(10):1784–93.
Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380(9841):572–80.
Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. 2014;384(9943):626–35.
Movva R, Rader DJ. Laboratory assessment of HDL heterogeneity and function. Clin Chem. 2008;54(5):788–800.
Jensen MK, Aroner SA, Mukamal KJ, Furtado JD, Post WS, Tsai MY, et al. High-density lipoprotein subspecies defined by presence of apolipoprotein C-III and incident coronary heart disease in four cohorts. Circulation. 2018;137(13):1364–73.
von Eckardstein A. Differential diagnosis of familial high-density lipoprotein deficiency syndromes. Atherosclerosis. 2006;186(2):231–9.
Chiesa G, Sirtori CR. Apolipoprotein A-I Milano: current perspectives. Curr Opin Lipidol. 2003;14(2):159–63.
Oram JF, Vaughan AM. ATP-binding cassette cholesterol transporters and cardiovascular disease. Circ Res. 2006;99(10):1031–43.
Ossoli A, Simonelli S, Vitali C, Franceschini G, Calabresi L. Role of LCAT in atherosclerosis. J Atheroscler Thromb. 2016;23(2):119–27.
Oldoni F, Baldassarre D, Castelnuovo S, Ossoli A, Amato M, van Capelleveen J, et al. Complete and partial lecithin:cholesterol acyltransferase deficiency is differentially associated with atherosclerosis. Circulation. 2018;138(10):1000–7.
Weissglas-Volkov D, Pajukanta P. Genetic causes of high and low serum HDL-cholesterol. J Lipid Res. 2010;51(8):2032–57.
Lamarche B, Rashid S, Lewis GF. HDL metabolism in hypertriglyceridemic states: an overview. Clin Chim Acta. 1999;286(1–2):145–61.
Thompson JF, Wood LS, Pickering EH, DeChairo B, Hyde CL. High-density genotyping and functional SNP localization in the CETP gene. J Lipid Res. 2007;48(2):434–43.
Khovidhunkit W, Kim MS, Memon RA, Shigenaga JK, Moser AH, Feingold KR, et al. Effects of infection and inflammation on lipid and lipoprotein metabolism: mechanisms and consequences to the host. J Lipid Res. 2004;45(7):1169–96.
Thompson A, Di Angelantonio E, Sarwar N, Erqou S, Saleheen D, Dullaart RP, et al. Association of cholesteryl ester transfer protein genotypes with CETP mass and activity, lipid levels, and coronary risk. JAMA. 2008;299(23):2777–88.
Zanoni P, Khetarpal SA, Larach DR, Rader DJ. Rare variant in scavenger receptor BI raises HDL cholesterol and increases risk of coronary heart disease. Science. 2016;351:1166–71.
Helgadottir A, Sulem P, Thorgeirsson G, Gretarsdottir S, Thorleifssoni G, Jensson BO, et al. Rare SCARB1 mutations associate with high-density lipoprotein cholesterol but not with coronary artery disease. Eur Heart J. 2018;39(23):2172–8.
TG and HDL Working Group of the Exome Sequencing Project NH, Lung, and Blood Institute, Crosby J, Peloso GM, Auer PL, Crosslin DR, Stitziel NO, et al. Loss-of-function mutations in APOC3, triglycerides, and coronary disease. N Engl J Med. 2014;371:22–31.
Jorgensen AB, Frikke-Schmidt R, Nordestgaard BG, Tybjaerg-Hansen A. Loss-of-function mutations in APOC3 and risk of ischemic vascular disease. N Engl J Med. 2014;371(1):32–41.
Singaraja RR, Sivapalaratnam S, Hovingh K, Dubé M-P, Castro-Perez J, Collins HL, et al. The impact of partial and complete loss-of-function mutations in endothelial lipase on high-density lipoprotein levels and functionality in humans. Circ Cardiovasc Genet. 2013;6:54–62.
Kontush A, Chapman MJ. Antiatherogenic function of HDL particle subpopulations: focus on antioxidative activities. Curr Opin Lipidol. 2010;21:312–8.
Khera AV, Cuchel M, de la Llera-Moya M, Rodrigues A, Burke MF, Jafri K, et al. Cholesterol efflux capacity, high-density lipoprotein function, and atherosclerosis. N Engl J Med. 2011;364(2):127–35.
Rohatgi A, Khera A, Berry JD, Givens EG, Ayers CR, Wedin KE, et al. HDL cholesterol efflux capacity and incident cardiovascular events. N Engl J Med. 2014;371(25):2383–93.
Gordon SM, Chung JH, Playford MP, Dey AK, Sviridov D, Seifuddin F, et al. High density lipoprotein proteome is associated with cardiovascular risk factors and atherosclerosis burden as evaluated by coronary CT angiography. Atherosclerosis. 2018;278:278–85.
Van Lenten BJ, Hama SY, de Beer FC, Stafforini DM, McIntyre TM, Prescott SM, et al. Anti-inflammatory HDL becomes pro-inflammatory during the acute phase response. Loss of protective effect of HDL against LDL oxidation in aortic wall cell cocultures. J Clin Invest. 1995;96(6):2758–67.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357(21):2109–22.
Connelly MA, Parry TJ, Giardino EC, Huang Z, Cheung WM, Chen C, et al. Torcetrapib produces endothelial dysfunction independent of cholesteryl ester transfer protein inhibition. J Cardiovasc Pharmacol. 2010;55(5):459–68.
Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J, et al. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367(22):2089–99.
Lincoff AM, Nicholls SJ, Riesmeyer JS, Barter PJ, Brewer HB, Fox KAA, et al. Evacetrapib and cardiovascular outcomes in high-risk vascular disease. N Engl J Med. 2017;376(20):1933–42.
Group HTRC, Bowman L, Hopewell JC, Chen F, Wallendszus K, Stevens W, et al. Effects of anacetrapib in patients with atherosclerotic vascular disease. N Engl J Med. 2017;377(13):1217–27.
Armitage J, Holmes MV, Preiss D. Cholesteryl Ester transfer protein inhibition for preventing cardiovascular events JACC review topic of the week. J Am Coll Cardiol. 2019;73(4):477–87.
Nissen SE, Tsunoda T, Tuzcu EM, Schoenhagen P, Cooper CJ, Yasin M, et al. Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290(17):2292–300.
Reijers JAA, Kallend DG, Malone KE, Jukema JW, Wijngaard PLJ, Burggraaf J, et al. MDCO-216 does not induce adverse immunostimulation, in contrast to its predecessor ETC-216. Cardiovasc Drugs Ther. 2017;31(4):381–9.
Kempen HJ, Schranz DB, Asztalos BF, Otvos J, Jeyarajah E, Drazul-Schrader D, et al. Incubation of MDCO-216 (ApoA-IMilano/POPC) with human serum potentiates ABCA1-mediated cholesterol efflux capacity, generates new prebeta-1 HDL, and causes an increase in HDL size. J Lipids. 2014;2014:923903.
Nicholls SJ, Puri R, Ballantyne CM, Jukema JW, Kastelein JJP, Koenig W, et al. Effect of infusion of high-density lipoprotein mimetic containing recombinant apolipoprotein A-I Milano on coronary disease in patients with an acute coronary syndrome in the MILANO-PILOT trial a randomized clinical trial. JAMA Cardiol. 2018;3(9):806–14.
Tardif JC, Gregoire J, L'Allier PL, Ibrahim R, Lesperance J, Heinonen TM, et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297(15):1675–82.
Michael Gibson C, Korjian S, Tricoci P, Daaboul Y, Yee M, Jain P, et al. Safety and tolerability of CSL112, a reconstituted, infusible, plasma-derived apolipoprotein A-I, after acute myocardial infarction: the AEGIS-I trial (ApoA-I event reducing in ischemic syndromes I). Circulation. 2016;134(24):1918–30.
Didichenko SA, Navdaev A, Cukier AM, Gille A, Schuetz P, Spycher MO, et al. Enhanced HDL functionality in small HDL species produced upon remodeling of HDL by reconstituted HDL, CSL112: effects on cholesterol efflux, anti-inflammatory and antioxidative activity. Circ Res. 2016;119(6):751–63.
Kootte RS, Smits LP, van der Valk FM, Dasseux JL, Keyserling CH, Barbaras R, et al. Effect of open-label infusion of an apoA-I-containing particle (CER-001) on RCT and artery wall thickness in patients with FHA. J Lipid Res. 2015;56(3):703–12.
Kataoka Y, Andrews J, Duong M, Nguyen T, Schwarz N, Fendler J, et al. Regression of coronary atherosclerosis with infusions of the high-density lipoprotein mimetic CER-001 in patients with more extensive plaque burden. Cardiovasc Diagn Ther. 2017;7(3):252–63.
Tardif JC, Ballantyne CM, Barter P, Dasseux JL, Fayad ZA, Guertin MC, et al. Effects of the high-density lipoprotein mimetic agent CER-001 on coronary atherosclerosis in patients with acute coronary syndromes: a randomized trial. Eur Heart J. 2014;35(46):3277–86.
Nicholls SJ, Andrews J, Kastelein JJP, Merkely B, Nissen SE, Ray KK, et al. Effect of serial infusions of CER-001, a pre-beta high-density lipoprotein mimetic, on coronary atherosclerosis in patients following acute coronary syndromes in the CER-001 atherosclerosis regression acute coronary syndrome trial a randomized clinical trial. JAMA Cardiol. 2018;3(9):815–22.
Waksman R, Torguson R, Kent KM, Pichard AD, Suddath WO, Satler LF, et al. A first-in-man, randomized, placebo-controlled study to evaluate the safety and feasibility of autologous delipidated high-density lipoprotein plasma infusions in patients with acute coronary syndrome. J Am Coll Cardiol. 2010;55(24):2727–35.
Navab M, Shechter I, Anantharamaiah GM, Reddy ST, Van Lenten BJ, Fogelman AM. Structure and function of HDL mimetics. Arterioscler Thromb Vasc Biol. 2010;30(2):164–8.
Bloedon LT, Dunbar R, Duffy D, Pinell-Salles P, Norris R, DeGroot BJ, et al. Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients. J Lipid Res. 2008;49(6):1344–52.
Ditiatkovski M, Palsson J, Chin-Dusting J, Remaley AT, Sviridov D. Apolipoprotein A-I mimetic peptides: discordance between in vitro and in vivo properties-brief report. Arterioscler Thromb Vasc Biol. 2017;37(7):1301–6.
Shamburek RD, Bakker-Arkema R, Shamburek AM, Freeman LA, Amar MJ, Auerbach B, et al. Safety and tolerability of ACP-501, a recombinant human lecithin:cholesterol acyltransferase, in a phase 1 single-dose escalation study. Circ Res. 2016;118(1):73–82.
Graham MJ, Lee RG, Bell TA 3rd, Fu W, Mullick AE, Alexander VJ, et al. Antisense oligonucleotide inhibition of apolipoprotein C-III reduces plasma triglycerides in rodents, nonhuman primates, and humans. Circ Res. 2013;112(11):1479–90.
Yang XH, Lee SR, Choi YS, Alexander VJ, Digenio A, Yang QQ, et al. Reduction in lipoprotein-associated apoC-III levels following volanesorsen therapy: phase 2 randomized trial results. J Lipid Res. 2016;57(4):706–13.
Chapman MJ, Redfern JS, McGovern ME, Giral P. Niacin and fibrates in atherogenic dyslipidemia: pharmacotherapy to reduce cardiovascular risk. Pharmacol Ther. 2010;126(3):314–45.
Millan J, Pinto X, Brea A, Blasco M, Hernandez-Mijares A, Ascaso J, et al. Fibrates in the secondary prevention of cardiovascular disease (infarction and stroke). Results of a systematic review and meta-analysis of the Cochrane collaboration. Clin Investig Arterioscler. 2018;30(1):30–5.
Araki E, Yamashita S, Arai H, Yokote K, Satoh J, Inoguchi T, et al. Effects of pemafibrate, a novel selective PPAR alpha modulator, on lipid and glucose metabolism in patients with type 2 diabetes and hypertriglyceridemia: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care. 2018;41(3):538–46.
Scott LJ. Alipogene tiparvovec: a review of its use in adults with familial lipoprotein lipase deficiency. Drugs. 2015;75(2):175–82.
Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–67.
Group HTC, Landray MJ, Haynes R, Hopewell JC, Parish S, Aung T, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203–12.
Schandelmaier S, Briel M, Saccilotto R, Olu KK, Arpagaus A, Hemkens LG, et al. Niacin for primary and secondary prevention of cardiovascular events. Cochrane Database Syst Rev. 2017;6(6):CD009744.
Keene D, Price C, Shun-Shin MJ, Francis DP. Effect on cardiovascular risk of high-density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients. BMJ. 2014;349:g4379.
Nicholls SJ, Gordon A, Johansson J, Wolski K, Ballantyne CM, Kastelein JJ, et al. Efficacy and safety of a novel oral inducer of apolipoprotein A-I synthesis in statin-treated patients with stable coronary artery disease a randomized controlled trial. J Am Coll Cardiol. 2011;57(9):1111–9.
Nicholls SJ, Puri R, Wolski K, Ballantyne CM, Barter PJ, Brewer HB, et al. Effect of the BET protein inhibitor, RVX-208, on progression of coronary atherosclerosis: results of the phase 2b, randomized, double-blind, multicenter, ASSURE trial. Am J Cardiovasc Drugs. 2016;16(1):55–65.
Shishikura D, Kataoka Y, Honda S, Takata K, Kim SW, Andrews J, et al. The effect of Bromodomain and extra-terminal inhibitor Apabetalone on attenuated coronary atherosclerotic plaque: insights from the ASSURE trial. Am J Cardiovasc Drugs. 2019;19(1):49–57.
Nicholls SJ, Ray KK, Johansson JO, Gordon A, Sweeney M, Halliday C, et al. Selective BET protein inhibition with Apabetalone and cardiovascular events: a pooled analysis of trials in patients with coronary artery disease. Am J Cardiovasc Drugs. 2018;18(2):109–15.
Nomiyama T, Bruemmer D. Liver X receptors as therapeutic targets in metabolism and atherosclerosis. Curr Atheroscler Rep. 2008;10(1):88–95.
Katz A, Udata C, Ott E, Hickey L, Burczynski ME, Burghart P, et al. Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants. J Clin Pharmacol. 2009;49(6):643–9.
Yonezawa S, Abe M, Kawasaki Y, Natori Y, Sugiyama A. Each liver X receptor (LXR) type has a different purpose in different situations. Biochem Biophys Res Commun. 2019;508(1):92–6.
Fiorucci S, Cipriani S, Baldelli F, Mencarelli A. Bile acid-activated receptors in the treatment of dyslipidemia and related disorders. Prog Lipid Res. 2010;49(2):171–85.
Mencarelli A, Renga B, Distrutti E, Fiorucci S. Antiatherosclerotic effect of farnesoid X receptor. Am J Physiol Heart Circ Physiol. 2009;296(2):H272–81.
Najafi-Shoushtari SH, Kristo F, Li Y, Shioda T, Cohen DE, Gerszten RE, et al. MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasis. Science. 2010;328(5985):1566–9.
Rayner KJ, Suarez Y, Davalos A, Parathath S, Fitzgerald ML, Tamehiro N, et al. MiR-33 contributes to the regulation of cholesterol homeostasis. Science. 2010;328(5985):1570–3.
Chen WM, Sheu WH, Tseng PC, Lee TS, Lee WJ, Chang PJ, et al. Modulation of microRNA expression in subjects with metabolic syndrome and decrease of cholesterol efflux from macrophages via microRNA-33-mediated attenuation of ATP-binding cassette transporter A1 expression by statins. PLoS One. 2016;11(5):e0154672.
Ference BA, Kastelein JJP, Ginsberg HN, Chapman J, Nicholls SJ, Ray KK, et al. Association of genetic variants related to CETP inhibitors and statins with lipoprotein levels and cardiovascular risk. JAMA. 2017;318(10):947–56.
Tardif JC, Rheaume E, Lemieux Perreault LP, Gregoire JC, Feroz Zada Y, Asselin G, et al. Pharmacogenomic determinants of the cardiovascular effects of dalcetrapib. Circ Cardiovasc Genet. 2015;8(2):372–82.
Nicholls SJ, Tuzcu EM, Brennan DM, Tardif JC, Nissen SE. Cholesteryl ester transfer protein inhibition, high-density lipoprotein raising, and progression of coronary atherosclerosis: insights from ILLUSTRATE (Investigation of Lipid Level Management Using Coronary Ultrasound to Assess Reduction of Atherosclerosis by CETP Inhibition and HDL Elevation). Circulation. 2008;118(24):2506–14.
Yvan-Charvet L, Kling J, Pagler T, Li H, Hubbard B, Fisher T, et al. Cholesterol efflux potential and antiinflammatory properties of high-density lipoprotein after treatment with niacin or anacetrapib. Arterioscler Thromb Vasc Biol. 2010;30(7):1430–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Darabi, M., Zakiev, E., Kontush, A. (2021). High-Density Lipoproteins. In: Davidson, M.H., Toth, P.P., Maki, K.C. (eds) Therapeutic Lipidology. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-030-56514-5_18
Download citation
DOI: https://doi.org/10.1007/978-3-030-56514-5_18
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-56513-8
Online ISBN: 978-3-030-56514-5
eBook Packages: MedicineMedicine (R0)