Abstract
Proprotein convertase/kexin type 9 (PCSK9) is produced and secreted by hepatocytes. Once in the extracellular milieu, PCSK9 can bind to the low-density lipoprotein receptor (LDLR) and regulates its cell surface expression. PCSK9 functions as a chaperone molecule. Though much remains to be elucidated about how PCSK9 orchestrates the intracellular routing of LDL-LDLR complexes within the cell, it is clear that PCSK9 promotes the entry of LDL-LDLR complexes into the lysosome where they are proteolytically catabolized. PCSK9 also regulates the expression of a number of other lipoprotein receptors, such as the apoE2 receptor, the VLDL receptor, the LDLR related protein 1, the fatty acid transport protein CD 36, and possibly the pathway (yet to be defined) for lipoprotein(a) clearance. Because it downregulates LDLR, PCSK9 reduces hepatocyte LDL-cholesterol (LDL-C) clearance capacity. Persons with gain-of-function mutations in PCSK9 have increased serum levels of LDL-C and increased risk for developing atherosclerotic cardiovascular disease (ASCVD). Persons with loss-of-function mutations in PCSK9 have reduced serum LDL-C and proportionately lower risk for ASCVD. The inhibition of PCSK9 with monoclonal antibodies or with antisense oligonucleotides directed against its mRNA has revolutionized the management of dyslipidemia. Either used as monotherapies or in combination with statins and other lipid-lowering drugs, the inhibition of PCSK9 allows for reductions in serum LDL-C to levels not previously thought possible. The reduction of pCSK9 availability dramatically increases hepatocyte cell surface expression of LDLR. The inhibition of PCSK9 has been shown to be safe and highly efficacious. Prospective, randomized outcomes trails with evolocumab and alirocumab demonstrate the capacity to reduce risk for myocardial infarction, ischemic stroke, revascularization, and hospitalization for unstable angina. In addition to their role in managing primary hyperlipidemia, the PCSK9 monoclonal antibodies have also been shown to be highly efficacious in the management of familial hypercholesterolemia and have the capacity to reduce rates of atherosclerotic plaque progression and induce plaque regression in the coronary tree.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atherosclerosis
- Epidermal growth factor A sequence
- Low-density lipoprotein receptor
- Lysosome
- Monoclonal antibody
- Proprotein convertase/kexin type 9
Introduction
A proprotein convertase is a proteolytic enzyme that converts an inactive precursor molecule into an active one [1]. An example of this is the conversion of a zymogen (a proenzyme) into a mature bioactive enzyme with catalytic activity in some aspect of intermediary metabolism [2]. There is a family of nine proprotein convertase subtilisin kexins (PCSK). Eight of the nine members are catalytically active and are responsible for the proteolytic conversion of a wide variety of molecules (including receptors, hormones, enzymes, transcription factors) into their bioactive forms [3]. The ninth member of this family (PCSK9) is the most recently discovered and is atypical. PCSK9 like other PVSKs is a serine protease. Once translated in the endoplasmic reticulum (ER), its signal peptide is cleaved by a signal peptidase to form zymogen proPCSK9 [4] (Fig. 14.1). In order to leave the ER and enter the cytosol, it catalyzes the autocleavage of a prosegment from itself. Subsequent to this step PCSK9 is no longer able to engage in a catalytic activity because the cleaved prosegment remains associated and it causes steric hindrance of this enzyme’s active site [5]. Enzymatically, PCSK9 has only a single molecular target: its own prosegment.
Schematic representation of proprotein convertase subtilisin kexin 9 (PCSK9) zymogen processing and binding to the low-density lipoprotein receptor (LDLR). (a) The autocatalytic zymogen processing of proPCSK9 (75 kDa) at Val-Phe-Ala-Gln152↓Ser-Ile-Pro (VFAQ152↓SIP) into the (prosegment (15 kDa) ≡ PCSK9 (62 kDa)) complex is emphasized, together with the positions of the active site Asp186, His226, and Ser386 and the oxyanion hole Asn317. The C-terminal hinge domain (H) and cys-his-rich domain (CHRD) are shown. (b) Cartoon representation of the cell surface interaction of the catalytic domain of PCSK9 with the epidermal growth factor-A (domain of the LDLR, as well as the suspected interaction of the prosegment with the β-barrel domain of the LDLR and the CHRD with a putative membrane-bound protein X. (c) Crystal structure of the ectodomain of the LDLR with PCSK9 emphasizing the interaction between them and the three subdomains in the CHRD (M1, M2, and M3). The interaction of protein X is presumed to be with one of the latter subdomains, possibly M2. (From Seidah et al. [4])
Low-density lipoprotein particles (LDL-P) are principally cleared from the systemic circulation by the LDL receptor (LDLR) [6]. LDL receptors are expressed along the surface of hepatocytes and are concentrated in clathrin-coated pits within cell membranes. Once an LDLR binds an LDL-P, it is configured within the clathrin-coated pit by LDLR adaptor protein 1 (aka clathrin associated sorting protein), though there is evidence that the protein disabled homolog adaptor protein 2 (dab-2) can also perform this role [7, 8]. An endosome forms and is covered with a clathrin polyhedral lattice [9] (Fig. 14.2). The endosome is released into the cytosol, the clathrin dissociates, and the internal milieu of the endosome is acidified. The drop in pH potentiates the dissociation of the LDLR from LDL-P. Through a mechanism that is yet to be defined, the LDL-P is specifically translocated into the lysosome for destruction by cathepsins and lipases. The LDLR is routed back to the hepatocyte cell surface to initiate another round of LDL-P uptake and catabolism (Fig. 14.3).
Endosome formation and uptake into the cytosol via a polyhedral clathrin cage. (From Trialsitenews.com)
LDL recycling, PCSK9 function, and effect of PCSK9 inhibition. Mechanism of action of PCSK9 inhibition for reduction of serum cholesterol concentration. Top panel: PCSK9 secreted by hepatocytes binds to LDL-R on the hepatocyte surface. Upon subsequent binding of the receptor by LDL, the PCSK9/LDL/LDL-R complex is internalized within an endosomal vesicle. The endosome fuses with a lysosome, and the PCSK9 chaperones the LDL/LDL-R complex into the lysosome for destruction. As a result, the number of LDL-Rs is decreased, resulting in less clearance of LDL from the circulation and elevated LDL concentration. Bottom panel: Monoclonal antibody binds to PCSK9 and prevents it from engaging the LDL-R. In the absence of PCSK9, the LDL-R is not routed to the lysosome for degradation and is returned instead to the hepatocyte surface. The recycled LDL-R is available for additional LDL binding and clearance, resulting in decreased levels of LDL. LDL, low-density lipoprotein; LDL-R, low-density lipoprotein receptor. (From Toth [96]. With permission from Elsevier)
PCSK9 regulates the expression of the LDLR (Fig. 14.3). Once in the extracellular milieu, PCSK9 can bind to the epidermal growth factor-like repeat A domain of LDLR [10]. LDLR bound to both an LDL-P and PCSK9 are also concentrated in clathrin-coated endosomes. However, in this instance, the PCSK9 holds the LDLR and LDL-P tightly together, and they do not dissociate as the intra-endosomal pH decreases [11]. The PCSK9 functions as a chaperone molecule of the LDLR-LDL-P complex into the lysosome. This results in LDLR catabolism and reduced cell surface expression of this receptor vital to LDL-P clearance.
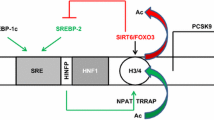
The PCSK9 gene localizes to chromosome 1 and, like the genes for LDLR and apoprotein B (apo B), is a locus for familial hypercholesterolemia [12, 13]. The expression of PCSK9 is regulated by the nuclear transcription factor sterol regulating element-binding protein-2 [14]. Gain-of-function mutations in PCSK9 such as D374Y and R496W lead to reduced LDLR expression, increased serum levels of LDL-P, and heightened risk for ASCVD [15, 16]. Such loss-of-function (LOF) mutations in PCSK9 as Y142X and C679X in persons of African descent [17] and Q152H in French Canadians [18] lead to increased LDLR expression, lower serum LDL-C, and reduced risk for ASCVD. Major prospective longitudinal cohorts confirm that LOF mutations in both men and women result in substantially lower LDL-C levels compared to patients with wild-type alleles for PCSK9 [19] (Fig. 14.4).
Difference in low-density lipoprotein cholesterol (LDL-C) among participants with vs without PCSK9 loss-of-function (LOF) variants in individual studies and pooled analyses. AGES indicates Age, Gene, Environment, Susceptibility Study–Reykjavik; ARIC, Atherosclerosis Risk in Communities Study; CHS, Cardiovascular Health Study, CI confidence interval; FHS, Framingham Heart Study; Health ABC, Health, Aging, and Body Composition Study; JHS, Jackson Heart Study; LDL-C, low-density lipoprotein cholesterol; MESA, Multi-Ethnic Study of Atherosclerosis; PROSPER, PROspective Study of Pravastatin in the Elderly at Risk for vascular disease; REGARDS, REasons for Geographic and Racial Differences in Stroke Study. LDL-C differences are comparing participants with PCSK9 LOF variants to those without PCSK9 LOF variants (PCSK9 LOF variant minus no PCSK9 LOF variant). Models for each participating study include adjustment for age, sex, region/center, and statin use. Pooled analyses are performed using inverse-variance-weighted fixed-effect models. (From Kent et al. [19])
Lipoprotein receptor physiology is complex. PCSK9 also regulates cell surface expression of other lipoprotein receptors, possibly impacting serum levels of other lipoproteins and their subfractions (Fig. 14.5). PCSK9 regulates the expression of the very low-density lipoprotein receptor (VLDLR), the apolipoprotein E2 receptor, and the LDL receptor-related protein-1, all of which can participate in the clearance of various apo B-containing lipoproteins [20,21,22,23]. In addition, PCSK9 regulates the expression of a cluster of differentiation 36 (CD 36), which is a fatty acid translocase in adipocytes and hepatocytes [24]. The D374Y GOF mutation also suggests that PCSK9 upregulates Nieman Pick C1-like protein without impacting the expression of SR-BI or ABCG5/G8 [25].
Proprotein convertase subtilisin kexin type 9 (PCSK9) and lipoprotein trafficking. Subsequent to release from the Golgi apparatus, low-density lipoprotein receptors (LDLR) translocate to the cell membrane where they are concentrated in clathrin-coated pits. Hepatocytes secrete PCSK9 into the extracellular space which can bind to the epidermal growth-factor-like repeat A (EGF-A) domain of LDLR. Complexes composed of LDLR and LDL particles are internalized via endosomes. If the LDLR–LDL-P complex is bound with PCSK9, the complex is chaperoned into the lysosome for hydrolytic destruction. The LDLR in this case is not recycled to the cell surface. When LDLR–LDL-P complexes are not bound to PCSK9, the complex dissociates in response to a drop in pH within the endosome. The LDL-P is translocated to the lysosome for destruction, whereas LDLR is spared and recycled to the cell surface to initiate another round of LDL-P binding and uptake. The monoclonal antibodies directed against PCSK9 decrease LDLR translocation into the lysosome, increase LDLR surface expression, and significantly reduce plasma levels of LDL-P. Recent investigations demonstrate that PCSK9 can also regulate the expression of other cell surface receptors, such as a very-low-density lipoprotein receptor (VLDLR), the LDLR-related protein (LRP), an apoprotein E receptor, and cluster of differentiation 36 (CD36). In addition to its impact on cell surface receptor expression, PCSK9 potentiates the production of apo B and increases VLDL secretion by inhibiting the catabolism of apoB via an autophagosome/lysosome-dependent pathway. The serine protease furin (which is found in both membrane-bound and free forms) can cleave active, intact PCSK9 (62 kDa) into an inactive 55-kDa fragment. A small percentage of total circulating LDL and lipoprotein(a) (Lp(a)) can bind PCSK9. Although some Lp(a) is cleared by a pathway that is independent of LDLR, some is demonstrably cleared by LDLR. (From Toth [97])
Therapeutic Strategies for Inhibiting PCSK9
Monoclonal Antibodies
A monoclonal antibody is a highly specific antibody directed toward a single molecular target [26]. Given the fact that PCSK9 is a secreted protein, it can be targeted by a monoclonal antibody (mAb) in an effort to neutralize its activity. Two fully human mAbs (evolocumab and alirocumab) directed against PCSK9 have been developed for treating primary hyperlipidemia and familial hypercholesterolemia. They are fully human in an effort to reduce the risk of autoimmune responses and the generation of antibodies against them. This also reduces the risk of tachyphylaxis. These agents can be used independently of hepatic and renal function because they have no dependence on hepatic uptake and metabolism, and they do not depend on renal elimination for their clearance [27,28,29]. The antibody complexes formed between these agents and extracellular PCSK9 are cleared by the reticuloendothelial system (Kupffer cells, spleen, lymph nodes, bone marrow), and they do not promulgate drug interactions since they have no dependence for activity from organic anion transport proteins, the cytochrome P450 isozymes, or glucuronidation as there is no known antibody uptake pathway for the liver.
Evolocumab
LDL-C Reduction in Primary Hyperlipidemia
In patients with primary hyperlipidemia, evolocumab is a highly safe and efficacious therapy for reducing atherogenic lipoprotein burden in serum. It can be dosed at 140 mg subcutaneously (SQ) every 2 weeks or 420 mg SQ every 4 weeks. When used as monotherapy, evolocumab induces a 55%–57% reduction in LDL-C compared to placebo [30] (Table 14.1). When added to statin therapy (atorvastatin 10 mg or 80 mg; rosuvastatin 5 mg or 40 mg; simvastatin 40 mg), evolocumab provides a mean incremental reduction in LDL-C of 63% [31]. Among patients intolerant to two or more statins evolocumab provides a 38% reduction in LDL-C compared to ezetimibe [32]. For patients at various levels of ASCVD risk, the addition of evolocumab to ongoing lipid-lowering therapy (atorvastatin 10 mg or 80 mg daily or the combination of atorvastatin 80 mg daily with ezetimibe) provided a 48–62% incremental reduction of LDL-C compared to placebo [33].
LDL-C Reduction in Familial Hypercholesterolemia
Among patients with familial hypercholesterolemia (FH), as long as the patient is not a homozygote for a null mutation in PCSK9, mAbs directed against circulating PCSK9 would be expected to provide some degree of LDL-C reduction. In the reduction of LDL-C with PCSK9 Inhibition in Heterozygous Familial Hypercholesterolemia Disorder Study-2 (RUTHERFORD-2), evolocumab when dosed at either 140 mg every 2 weeks or 420 mg dosed every 4 weeks reduced LDL-C by 59% and 60%, respectively [34]. This result suggests that the upregulation of LDLR is so robust that patients with heterozygous FH (HeFH) respond to evolocumab with as much LDL-C reduction as patients with primary hyperlipidemia. As shown in the Trial Evaluating PCSK9 Antibody in Subjects with LDL Receptor Abnormalities Part B (TESLA), among patients with homozygous FH (HoFH), evolocumab reduces LDL-C 31% compared to placebo [34].
Apo B, Non-HDL-C, and Lipoprotein(a) Reduction
Apo B and non-HDL-C are important measures of atherogenic lipoprotein burden in serum and are highly predictive of risk for ASCVD events [35, 36]. Lipoprotein(a) (Lp(a)) is an LDL-P modified with the covalent addition of apoprotein(a) to apoB [37, 38]. Lp(a) is highly proatherogenic, is an important delivery platform for oxidized phospholipid into the arterial wall, is prothrombotic, and is an established risk factor for ASCVD [39,40,41]. The mechanism(s) by which Lp(a) is cleared from the circulation are as yet undefined [42]. In a pooled analysis that includes 4943 participants in 15 phase 2 and phase 3 clinical trials, evolocumab dosed at 140 mg every 2 weeks or 420 mg every 4 weeks reduces median Lp(a) 22%–38% and 20%–33%, respectively [43]. Apo B is reduced by the 140 mg and 420 mg doses by 46%–52% and 40–48%, respectively. Non-HDL-C (defined as total cholesterol minus HDL-C) is reduced by the 140 mg and 420 mg doses of evolocumab by 49–56% and 48–52%, respectively. Compared to either placebo (most patients on intensive statin therapy except in patients with statin intolerance) or ezetimibe therapy, evolocumab dramatically increases the capacity to attain a non-HDL-C < 100 mg/dL (2.6 mmol/L) or an apo B < 80 mg/dL in patients with primary hyperlipidemia/mixed dyslipidemia, statin intolerance, HeFH, type 2 diabetes mellitus, and variable levels of ASCVD risk (in the DESCARTES trial) (Fig. 14.6).
Percent achievement in placebo or ezetimibe-controlled phase 2 and phase 3 evolocumab studies of (a) non-HDL-C < 100 mg/dL (2.6 mmol/L) and (b) ApoB <80 mg/dL. The percentages of patients who achieved non-HDL-C < 100 mg/dL (a) and ApoB <80 mg/dL (b) with evolocumab, ezetimibe, or placebo are depicted in this plot for all studies with a placebo or ezetimibe comparator. Results are shown separately for each patient population examined (hypercholesterolemia/mixed dyslipidemia, type 2 diabetes mellitus, heterozygous FH, and statin intolerance), all 12 weeks in duration, as well as for the 1-year study (DESCARTES). ApoB indicates apolipoprotein B; FH, familial hypercholesterolemia; non-HDL-C, non-high-density lipoprotein cholesterol. *Evolocumab-treated patients with ezetimibe comparator arm; †Evolocumab-treated patients with placebo comparator arm. (From Toth et al. [43])
Triglyceride-Enriched Lipoproteins and Lipoprotein Subfractions
Evolocumab promotes a range of changes in lipoprotein particles and subfractions. LDL-P number [44, 45] and size [46, 47], triglyceride-enriched lipoproteins and their remnants [48, 49], and HDL subfractions [50, 51] have been implicated as important risk factors for ASCVD. The apo B/apo A-I ratio is viewed as a strong predictor of CHD risk [52, 53]. Total LDL-P as well as both large and small LDL particles decrease significantly in response to evolocumab therapy [54] (Table 14.1). With the addition of evolocumab to statin therapy, the total LDL-P burden decreases from 1110 to 610 nmol/L. Total HDL particles increase significantly. In addition, the sum of chylomicron and very-low-density lipoprotein particles (VLDL-P) decrease, and both small VLDL-P and intermediate-density lipoprotein particles decrease significantly (Table 14.1). In this same study, HDL-C and apo A-I increased modestly compared to placebo by 5.7% and 2.5%, while VLDL-C and apoB/Apo A-I decreased by 13.0% and 43.2%, respectively [54]. These broad-spectrum changes in lipoproteins and their subfractions are generally viewed as beneficial.
Impact of Evolocumab on Coronary Atherosclerosis
The Global Assessment of Plaque Regression with a PCSK9 Antibody as Measured by Intravascular Ultrasound (GLAGOV) trial tested whether or not treatment of patients with evolocumab (dosed at 420 mg monthly) reduced the progression of atherosclerosis in coronary target lesions using intravascular ultrasonography [55]. When compared to placebo, evolocumab treatment reduced percent atheroma volume by −1.0% (p < 0.001), total atheroma volume decreased by −4.9 mm3 (p < 0.001), and more patients experienced plaque regression (17% and 12.5% more experienced reductions in percent atheroma volume and total atheroma volume, respectively (both p < 0.001)). Among patients who achieved LDL-C < 70 mg/dL, evolocumab therapy compared to placebo had an even more favorable impact on plaque features: percent atheroma volume decreased −1.62%, and the percentage of patients with regression of percent atheroma volume was 33.2% (both p < 0.001). Hence, evolocumab therapy potentiates significant plaque regression, and the lower the LDL-C was reduced, the greater the improvement in atherosclerotic plaque features.
Impact of Evolocumab on Cardiovascular Events
The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) trial evaluated the efficacy and safety of evolocumab therapy compared to placebo in 27,564 patients with established ASCVD already being treated with moderate or high intensity statin therapy [56]. Evolocumab reduced LDL-C by a mean of 59% (from 92 to 30 mg/dL). The primary composite endpoint was comprised of CV mortality, MI, stroke, hospitalization for unstable angina, or coronary revascularization. The secondary composite endpoint was comprised of CV death, MI, and stroke. The primary and secondary composite endpoints were reduced by evolocumab compared to placebo by 15% (p < 0.001) and 20% (p < 0.001), respectively. Myocardial infarction was reduced by 27% (p < 0.001), stroke was reduced by 21% (p < 0.01), and coronary revascularization was reduced by 22% (p < 0.001). The larger the LDL-C reduction, the bigger the benefit. There was continuous benefit all the way down to <10 mg/dL of LDL-C. When comparing an attained LDL-C of <10 mg/dL to >100 mg/dL, there was a 41% relative risk reduction for mortality, MI, and stroke (p = 0.02). Neither cardiovascular nor all-cause mortality was reduced by evolocumab. There was no heterogeneity for benefit among prespecified subgroups. Hepatic, skeletal muscle, neurocognitive, and other adverse events in general were not different between groups with the exception of injection site reactions, which occurred more frequently in patients treated with evolocumab.
In a post hoc analysis of the FOURIER trial, the impact of evolocumab therapy on CV event rates in 22,351 patients with a prior MI was evaluated with respect to time from most recent MI, number of prior MIs, and whether or not a patient had residual multivessel CAD (≥40% stenosis in ≥2 large vessels) [57]. For patients who sustained a qualifying MI < 2 years ago or ≥2 years ago, the composite of CV mortality, MI, and stroke were reduced by 24% (p < 0.001) and 13% (p = 0.04), respectively (Fig. 14.7). For patients who sustained ≥2 previous MIs vs 1 MI, this composite was reduced by 21% (p = 0.006) and 16% (p = 0.008), respectively. Having or not having multivessel disease was associated with a 30% (p < 0.001) and 11% (p = 0.055) reduction in this composite endpoint, respectively.
Incidence of the key secondary end point in patients stratified by high-risk features. Cumulative incidence curves for the key secondary end point by treatment arm in patients stratified by time from qualifying myocardial infarction (MI; a), number of prior MIs (b), and presence of residual multivessel coronary artery disease (c). P values for interactions between treatment and subgroups were 0.18, 0.57, and 0.03, respectively. CI indicates confidence interval; CV, cardiovascular; HR, hazard ratio; and RRR, relative risk reduction. (From Sabatine et al. [57])
In the setting of peripheral arterial disease (PAD), evolocumab appears to be particularly beneficial. When comparing evolocumab therapy to placebo in patients with and without PAD in the Fourier trial, the composite of CV death, MI, and stroke were reduced by 27% (p = 0.004) and 19% (p < 0.001), respectively [58]. For the trial as a whole, major acute limb events (defined as a composite of acute limb ischemia, major amputation (above the knee or below the knee, excluding forefoot or toe), and urgent revascularization (thrombolysis or urgent vascular intervention for ischemia) were reduced by evolocumab by 42% (p = 0.0093) (Fig. 14.8). Among patients with established PAD, evolocumab reduced major acute limb events by 37%, but this finding was not statistically significant. However, the event curves for the two groups separate in a compelling way (Fig. 14.8). For patients without a prior history of PAD, evolocumab reduced major acute limb events by 63% (p = 0.0197). In all three analyses, event curve separation is immediate and increases as a function of time. Benefit also increased as LDL-C decreased, even below 10 mg/dL.
Major adverse limb events. Major adverse limb events (composite of acute limb ischemia, major amputation, or urgent revascularization) by treatment (evolocumab in red, placebo in blue) in all randomly assigned patients (a), in patients with symptomatic PAD (b), and in patients with no known PAD (c). CI indicates confidence interval, HR hazard ratio, and PAD peripheral artery disease. (From Bonaca et al. [58])
In a subgroup analysis of 11,033 participants with diabetes in the FOURIER trial, there was an 18% (p = 0.0021) and 22% reduction in the composite of CV death, MI, and stroke for patients with and without diabetes [59]. Evolocumab did not increase the incidence of diabetes in patients with either no diabetes or prediabetes. In addition, hemoglobin a1c and fasting plasma glucose levels remained unchanged between groups showing no disturbance in glycemic control induced by evolocumab.
As noted above, evolocumab reduces serum levels of Lp(a). Evolocumab reduced the risk of CV death, MI, or urgent revascularization by 23% (hazard ratio, 0.77; 95% CI, 0.67–0.88) in patients with a baseline Lp(a) >median and by 7% (hazard ratio, 0.93; 95% CI, 0.80–1.08; P interaction = 0.07) in those ≤median [60]. Hence, it is plausible to conclude that the Lp(a) reduction promoted by evolocumab therapy contributes to overall risk reduction.
Evolocumab and Neurocognitive Impairment
There has been lingering concern that lipid lowering, especially with statins, may be associated with cognitive impairment. Although largely based on speculation, there is particular concern that if LDL-C is lowered below 50 mg/dL, this may precipitate adverse changes in the brain resulting in memory impairment or frank dementia. While it is imperative that vigilance always be maintained for adverse side effects from any pharmacologic intervention, there has historically been no prospective clinical trial evidence that aggressive LDL-C reduction or statin therapy per se cognitive impairment. Cholesterol metabolism behind the blood-brain barrier is completely segregated from the central circulation. Within the brain, oligodendrocytes and astrocytes provide all of the cholesterol necessary for myelin formation and normal neuronal function [61, 62]. Neither cholesterol nor lipoproteins cross the blood brain barrier.
The National Lipid Association’s Statin Safety Task Force concluded that statins as a class are not associated with adverse effects on cognition (strength of recommendation: A) [63]. Neither the Heart Protection Study [64] nor the Prospective Study of Pravastatin in the Elderly at Risk [65] trials were unable to demonstrate any adverse impact of statin therapy on cognitive capacity in patients with dyslipidemia. An early meta-analysis suggested that statins reduce risk of neurocognitive impairment [66]. In a prospective cohort study, after adjusting for education, smoking status, the presence of at least one APOE ɛ4 allele, and history of stroke or diabetes at baseline, participants treated with statins had a 48% lower risk of developing dementia compared to those who had not been treated with a statin [67]. The Cardiovascular Health Study showed a similar 44% lower risk of Alzheimer’s type dementia compared to patients not taking lipid-lowering therapy [68]. Much of the concern surrounding lipid lowering and dementia relies on case reports, anecdote, and unconfirmed submissions to the adverse event reporting system of the Food and Drug Administration.
The Evaluating PCSK9 Binding Antibody Influence on Cognitive Health in High Cardiovascular Risk Subjects (EBBINGHAUS) study prospectively evaluated whether or not lipid-lowering therapy with a statin ± evolocumab very low LDL-C are associated with increased risk for cognitive impairment [69].
The Evaluating PCSK9 Binding Antibody Influence on Cognitive Health in High Cardiovascular Risk Subjects (EBBINGHAUS) study investigated whether or not lipid-lowering therapy with statins and evolocumab or low levels of LDL-C induce neurocognitive impairment. A 1204 patient subgroup of the FOURIER trial prospectively underwent assessment of their cognitive function using the Cambridge Neuropsychological Test Automated Battery (CANTAB). The CANTAB is a computer-based test that is valid independent of language and culture. Four components of cognition were evaluated: (1) spatial working memory strategy index of executive function, (2) spatial working memory between errors, (3) paired associates learning, and (4) reaction time. Patients also self-evaluated everyday cognition at the conclusion of the study. The EBBINGHAUS investigators were unable to detect any change in either individual components of the CANTAB or a global score between the beginning and end of the FOURIER trial. In addition, based on self-assessment, there was no between group differences in self-reported cognitive capacity or changes therein. These results applied even to patients who achieved ultra-low LDL-C of <10 mg/dL.
Overall Safety of Evolocumab
In addition to its efficacy, evolocumab has been shown to be safe. The most commonly occurring adverse events occurring in >5% of patients and more often than in placebo treated patients are nasopharyngitis, influenza-like reaction, upper respiratory infection, and injection site reactions [70]. In an analysis of over 6000 patients treated with evolocumab, the incidence of muscle, liver, and kidney related adverse events was similar to that observed with placebo (Table 14.2). Neurocognitive adverse events were also rare and on par with placebo, consistent with the Ebbinghaus trial (Table 14.3). Evolocumab therapy also does not increase risk for impaired glucose tolerance or diabetes mellitus [56, 70]. The side-effect profile of evolocumab is unchanged when comparing patients who achieve LDL-C levels on therapy of >40 mg/dL, 25–40 mg/dL, or <25 mg/dL [70].
Alirocumab
LDL-C Reduction in Primary Hyperlipidemia
Alirocumab can be dosed at 75 mg or 150 mg SQ every 2 weeks or 300 mg SQ every 4 weeks. In patients with primary hyperlipidemia, the 75 mg and 150 mg doses induce mean LDL-C reductions of 43% and 58%, respectively. When specifically evaluated in high-risk patients on maximally tolerated statin therapy given 75 mg every 2 weeks, mean LDL-C reduction was 48.2%, and patients in the alirocumab/statin treatment arm achieved LDL-C < 70 mg/dL 75% of the time after 6 months of therapy compared to 9% for placebo treatment [71]. Among patients with type 1 and type 2 diabetes mellitus (T1DM, T2DM) treated with maximally tolerated statin therapy, alirocumab treatment (either at 75 mg or 150 mg every 2 weeks if LDL-C not controlled with the lower dose) for 6 months decreased LDL-C by 49% and 47.8% in T2DM and T1DM patients, respectively, compared to placebo [72]. In addition, LDL < 70 mg/dL was achieved in 76.4% and 70.2% of T2DM and T1DM patients, respectively. In both groups, fasting blood glucose and glycated hemoglobin levels remained unchanged in the two treatment groups.
LDL-C Reduction in Familial Hypercholesterolemia
Alirocumab is indicated for the treatment of HeFH. In the Efficacy and Safety of Alirocumab Versus Placebo on Top of Lipid-Modifying Therapy in Patients with Heterozygous Familial Hypercholesterolemia Not Adequately Controlled with Their Lipid-Modifying Therapy (ODYSSEY FH I and FH II), patients were treated for 78 weeks with the highest tolerated dose of a statin ± other lipid-lowering therapy and then randomized to either alirocumab (75 mg every 2 weeks and then increased to 150 mg every 2 weeks if LDL-C > 70 mg/dL) [73]. The mean LDL-C decreased from 144.7 to 71.3 mg/dL (57.9% reduction compared to placebo) in FH I and decreased from 134.6 to 67.7 mg/dL (51.4% reduction compared to placebo) in FH II [73]. These changes in LDL-C were maintained through 78 weeks of treatment. In ODYSSEY High FH (HeFH with LDL-C > 160 mg/dL despite maximally tolerated statin therapy ± other lipid-lowering therapy), alirocumab dosed at 150 mg every 2 weeks reduced mean LDL-C by 90.8 mg/dL at week 24, and this change was maintained through 78 weeks of treatment [74]. Alirocumab is not yet indicated for the treatment of HoFH.
Apo B, Non-HDL-C, and Lipoprotein(a) Reduction
In a pooled analysis of ten phase 3 ODYSSEY studies which included 4983 participants, alirocumab dose at 75 or 150 mg every week reduced non-HDL-C by approximately 42%–51% and 40% in patients who did and did not receive concomitant statin therapy, respectively [74]. Compared to statin monotherapy control arms, the addition of alirocumab to ongoing statin therapy increased the attainment of non-HDL-C < 100 mg/dL to 70–80% from 7%–10% (Fig. 14.9). Similarly, use of alirocumab at 75/150 mg every 2 weeks added to ongoing statin therapy reduced apoB by 40%–52%; among patients not treated with a statin, alirocumab decreased apoB by 36.5%. Alirocumab increased the goal attainment rate for apo B < 80 mg/dL to 78%–85% from approximately 20% on placebo (Fig. 14.9). For patients not on a statin alirocumab induced apo B <80 mg/dL in approximately 70% of patients.
Percent of patients achieving apoB levels<80 mg/dL during the studies (modified intention to treat population). P < 0.0001 vs control group at all time points and in all study pools. ApoB indicates apolipoprotein B, Q2W every 2 weeks. (From Bays et al. [98])
Alirocumab reduces Lp(a) significantly. In a pooled analysis of ten phase 3 studies including 4915 participants, alirocumab reduced Lp(a) from baseline by 23% to 27% with alirocumab 75/150-mg Q2W and 29% with alirocumab 150-mg Q2W (both p < 0.0001 vs placebo) at 6 months [75]. These reductions in Lp(a) were sustained over 78–104 weeks and were independent of race, gender, the presence of familial hypercholesterolemia, baseline Lp(a) and LDL-C concentrations, or use of statins.
Triglyceride-Enriched Lipoproteins and Lipoprotein Subfractions
A comprehensive analysis of changes induced by alirocumab in lipoproteins and their subfractions as well as apo B, apoA1, ApoCII, and ApoCIII are summarized in Table 14.4 [76]. LDL1–2 are larger, more buoyant LDL species, while LDL3–4 are smaller, denser LDL species. Remnant lipoproteins are defined as VLDL3-C + IDL-C. The ratio of apo B/apoA1 is a well-recognized marker of CV risk.
Alirocumab induces substantive reductions in triglycerides, LDL-C subfractions, VLDL-C and its subfractions, IDL-C, LDLR-C (LDLreal = LDL-C – Lp(a)-C – IDL-C), and remnant lipoprotein cholesterol (RLP-C) (Table 14.4). In addition, alirocumab therapy correlates with significant reductions in apoB/apoA1 ratio, ApoCII, and ApoCIII. All of these changes would be expected to be both advantageous and beneficial with regard to ASCVD risk.
Impact of Alirocumab on Cardiovascular Events
The clinical efficacy of alirocumab was evaluated in the ODYSSEY OUTCOMES trial, which included 18,924 patients who sustained an ACS within the year previous to enrollment [77]. All patients were treated with either high-intensity statin therapy of the highest dose of a statin they could tolerate. Patients were randomized to either alirocumab 75/150 mg every 2 weeks with the goal of an attained LDL-C on therapy of 25–50 mg/dL. The median duration of follow-up was 2.8 years. The primary composite endpoint included death from coronary heart disease, nonfatal MI, unstable angina requiring hospitalization, and fatal or nonfatal ischemic stroke. Alirocumab reduced the primary composite endpoint compared to placebo by 15% (p < 0.001). The composite of all-cause mortality, nonfatal MI, and nonfatal ischemic stroke was reduced by 14% (p < 0.001). Other endpoint reductions included nonfatal MI 14%, fatal or nonfatal ischemic stroke 27%, unstable angina requiring hospitalization 39%, and ischemia-driven revascularization 12%. Neither coronary nor cardiovascular mortality was reduced significantly.
A variety of additional analyses of ODYSSEY OUTCOMES demonstrate broad benefit from alirocumab. The number needed to treat to prevent major adverse cardiovascular events (MACE) over a period of 3 years decreases as a function of age: 43 at age 45 years, 26 at age 75 years, and 12 at age 85 years [78]. Relative risk reduction for MACE was consistent for person above or below the age of 65 years. Alirocumab decreases risk of any stroke (28%) without increasing the risk of hemorrhagic stroke, irrespective of attained LDL-C or history of cerebrovascular disease (Fig. 14.10). This is a highly reassuring finding given the longstanding concern that low LDL-C may correlate with increased risk for hemorrhagic stroke [79]. Although alirocumab therapy is not associated with a reduction in CV mortality, it is associated with a reduction in all-cause mortality (15%, P = 0.03) [80] (Fig. 14.11). This association must, however, be regarded as nominally significant because all-cause mortality followed CV and CHD mortality in the prespecified hierarchy of principal secondary endpoints. Among patients with a history of prior coronary artery bypass grafting prior to their qualifying ACS, alirocumab significantly reduced risk for MACE by 23% [81]. As observed in the FOURIER trial, the reduction of Lp(a) by alirocumab was shown to contribute to overall MACE reduction in the ODYSSEY OUTCOMES trial [82].
Kaplan-Meier curves for any stroke, ischemic stroke and hemorrhagic stroke. CI indicates confidence interval and HR hazard ratio. (From Jukema et al. [99])
All-cause, cardiovascular, and non-cardiovascular death (intention-to-treat population) shown as Kaplan-Meier curves (left panel) and in a forest plot (right panel). CV indicates cardiovascular and HR hazard ratio. (From Steg et al. [80])
Overall Safety of Alirocumab
The side-effect profile of alirocumab is similar to that of evolocumab. The most frequently occurring adverse events are skin reactions at the injection site. Nasopharyngitis, influenza-like reaction, and diarrhea occur slightly more frequently than placebo [83]. Neurocognitive adverse events are similar to placebo. When evaluating adverse events as a function of LDL-C < 15 mg/dL, < 25 mg/dL, or > 25 mg/dL, there are no substantive differences at these different LDL-C thresholds, including for neurocognitive side-effects [84]. In ODYSSEY OUTCOMES, there were no between group differences in hepatic, skeletal muscle, or renal side effects or toxicity [77]. Risk of worsening diabetes or new onset diabetes was not different between groups.
Inclisiran
A rapidly evolving field of novel pharmacologic therapeutic agents are single-stranded and double-stranded ribonucleic acid (ssRNA and dsRNA, respectively) oligonucleotides that antagonize the translation of specific gene products. Mipomersen is an example of an ssRNA oligonucleotide) [85] (Fig. 14.12). Mipomersen enters hepatocytes and binds to a complementary nucleotide sequence according to Watson-Crick base pairing along the messenger RNA (mRNA) for apoB. This interrupts mRNA translation along the ribosome and leads to reduced apo B and, hence, VLDL production, ultimately also resulting in lower serum levels of LDL-C and Lp(a) [86]. Inclisiran is an example of a dsRNA interfering or “silencing” RNA (siRNA). DNA replication and transcription are highly regulated processes within the nucleus of a cell. However, it has become increasingly clear that gene expression is also significantly impacted by microRNAs and siRNAs that inhibit or silence gene/mRNA expression posttranscriptionally [87]. Interfering RNAs are 20–30 nucleotides long and are composed of both an antisense strand that is complementary to a target sequence in the mRNA for a specific gene and a passenger strand [88]. The antisense strand is used to inhibit mRNA translation [89]. This, however, requires complex molecular machinery. The antisense strand is incorporated into the RNA induced silencing complex (RISC; Fig. 14.12). The RISC is a molecular complex that can be used by a cell to silence the expression of virtually any gene by three possible mechanisms: (1) interrupting mRNA translation, (2) promoting the degradation of mRNA, and (3) promoting the formation of heterochromatin or even inducing DNA elimination [87]. The antisense strand binds to an Argonaute protein which is critical for aligning the antisense strand with a target mRNA so that it can form a complementary Watson-Crick helix. Glycine-tryptophan protein of 182 kDa (GW182) promotes both translational suppression and the recruitment of CCR4–NOT deadenylase complex4 which hydrolyzes the RNA complex [89].
Silencing RNA (siRNA)-based versus antisense oligonucleotide-based approaches for reducing PCSK9 expression. (a) Antisense oligonucleotide technology employs a single-stranded RNase H mechanism. (b) By contrast, small interfering RNA (siRNA) technology utilizes a double-stranded RNA-induced silencing complex (RISC) mechanism. (From Nordestgaard et al. [100])
Inclisiran is an example of gene silencing technology that suppresses the expression of PCSK9 leading to the reduction of PCSK9 in both the intra- and extracellular compartments of the hepatocyte. Inclisiran is very specifically targeted to hepatocytes by being covalently bound to triantennaryN-acetylgalactosamine [90]. This allows inclisiran to very specifically bind to asialoglycoprotein receptors on the hepatocyte surface with high affinity [91]. In the Trial to Evaluate the Effect of Inclisiran Treatment on Low Density Lipoprotein Cholesterol (LDL-C) (ORION-1) trial, inclisiran induced a dose-dependent reduction in serum LDL-C; inclisiran dosed at 300 mg SQ on days 1 and 90 induced the following reductions by day 180 compared to baseline and placebo: LDL-C 52.6% (p < 0.001), non-HDL-C 46% (p < 0.001), triglycerides 14.2% (p < 0.05), VLDL 16% (p < 0.01), apo B 40.9% (p < 0.001), Lp(a) 25.6%, and PCSK9 69% (p < 0.001) [92]. Injection site reactions occurred in 5% of patients receiving inclisiran. Inclisiran had a comparable rate of liver and skeletal muscle related side effects relative to placebo. On this regimen, 48% of participants achieved an LDL-C < 50 mg/dL, and 66% achieved an LDL-C < 70 mg/dL. Because of its pharmacokinetic profile and mechanism of action, inclisiran can be dosed every 6 months and provide durable, stable reductions in LDL-C [93]. Inclisiran provides identical levels of LDL-C reducing capacity to diabetics and nondiabetics [94]. The clinical efficacy for reducing cardiovascular events by inclisiran is being evaluated in the ORION-4 trial which includes approximately 15,000 patients 55 years of age or older and with established ASCVD. It is anticipated the trial will require 5 years to complete [95].
Conclusions
-
1.
PCSK9 is an important regulator of LDL particle uptake and catabolism.
-
2.
PCSK9 impacts serum levels of multiple lipoprotein species and their subfractions by impacting the expression of multiple members of the LDLR family.
-
3.
PCSK9 monoclonal antibodies (evolocumab and alirocumab) reduce LDL-C markedly and dramatically increase goal attainment rates for LDL-C, apo B, and non-HDL-C.
-
4.
The PCSK9 mAbs have an excellent safety profile and are well tolerated.
-
5.
The PCSK9 mAbs impact risk for CV events significantly when used in combination with statins. The risk for MI, stroke, and need for revascularization are all significantly reduced. There is no increase in risk for hemorrhagic stroke with these agents.
-
6.
The reduction in Lp(a) by the PCSK9 mAbs contributes to ASCVD risk reduction.
-
7.
Inclisiran suppresses the translation of PCSK9 mRNA and provides substantial capacity for reducing LDL-C as well as VLDL, apo B, and non-HDL-C. Its unique mechanism of action allows for dosing this medication twice per year.
References
Seidah NG, Sadr MS, Chretien M, Mbikay M. The multifaceted proprotein convertases: their unique, redundant, complementary, and opposite functions. J Biol Chem. 2013;288:21473–81.
Chakraborty P, Acquasaliente L, Pelc LA, Di Cera E. Interplay between conformational selection and zymogen activation. Sci Rep. 2018;8:4080.
Turpeinen H, Ortutay Z, Pesu M. Genetics of the first seven proprotein convertase enzymes in health and disease. Curr Genomics. 2013;14:453–67.
Seidah NG, Awan Z, Chretien M, Mbikay M. PCSK9: a key modulator of cardiovascular health. Circ Res. 2014;114:1022–36.
Seidah NG, Mayer G, Zaid A, et al. The activation and physiological functions of the proprotein convertases. Int J Biochem Cell Biol. 2008;40:1111–25.
Goldstein JL, Brown MS. The LDL receptor. Arterioscler Thromb Vasc Biol. 2009;29:431–8.
He G, Gupta S, Yi M, Michaely P, Hobbs HH, Cohen JC. ARH is a modular adaptor protein that interacts with the LDL receptor, clathrin, and AP-2. J Biol Chem. 2002;277:44044–9.
Maurer ME, Cooper JA. The adaptor protein Dab2 sorts LDL receptors into coated pits independently of AP-2 and ARH. J Cell Sci. 2006;119:4235–46.
Popova NV, Deyev IE, Petrenko AG. Clathrin-mediated endocytosis and adaptor proteins. Acta Nat. 2013;5:62–73.
Kwon HJ, Lagace TA, McNutt MC, Horton JD, Deisenhofer J. Molecular basis for LDL receptor recognition by PCSK9. Proc Natl Acad Sci U S A. 2008;105:1820–5.
Lagace TA. PCSK9 and LDLR degradation: regulatory mechanisms in circulation and in cells. Curr Opin Lipidol. 2014;25:387–93.
Abifadel M, Varret M, Rabes JP, et al. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat Genet. 2003;34:154–6.
Abifadel M, Rabes JP, Devillers M, et al. Mutations and polymorphisms in the proprotein convertase subtilisin kexin 9 (PCSK9) gene in cholesterol metabolism and disease. Hum Mutat. 2009;30:520–9.
Jeong HJ, Lee H-S, Kim K-S, Kim Y-K, Yoon D, Park SW. Sterol-dependent regulation of proprotein convertase subtilisin/kexin type 9 expression by sterol-regulatory element binding protein-2. J Lipid Res. 2008;49:399–409.
Benjannet S, Hamelin J, Chretien M, Seidah NG. Loss- and gain-of-function PCSK9 variants: cleavage specificity, dominant negative effects, and low density lipoprotein receptor (LDLR) degradation. J Biol Chem. 2012;287:33745–55.
Benjannet S, Hamelin J, Chrétien M, Seidah NG. Loss- and gain-of-function PCSK9 variants: cleavage specificity, dominant negative effects, and low density lipoprotein receptor (LDLR) degradation. J Biol Chem. 2012;287:33745–55.
Cohen J, Pertsemlidis A, Kotowski IK, Graham R, Garcia CK, Hobbs HH. Low LDL cholesterol in individuals of African descent resulting from frequent nonsense mutations in PCSK9. Nat Genet. 2005;37:161–5.
Mayne J, Dewpura T, Raymond A, et al. Novel loss-of-function PCSK9 variant is associated with low plasma LDL cholesterol in a French-Canadian family and with impaired processing and secretion in cell culture. Clin Chem. 2011;57:1415–23.
Kent ST, Rosenson RS, Avery CL, et al. PCSK9 loss-of-function variants, low-density lipoprotein cholesterol, and risk of coronary heart disease and stroke: data from 9 studies of blacks and whites. Circ Cardiovasc Genet. 2017;10:e001632.
Schulz R, Schluter KD. PCSK9 targets important for lipid metabolism. Clin Res Cardiol Suppl. 2017;12:2–11.
Poirier S, Mayer G, Benjannet S, et al. The proprotein convertase PCSK9 induces the degradation of low density lipoprotein receptor (LDLR) and its closest family members VLDLR and ApoER2. J Biol Chem. 2008;283:2363–72.
Canuel M, Sun X, Asselin MC, Paramithiotis E, Prat A, Seidah NG. Proprotein convertase subtilisin/kexin type 9 (PCSK9) can mediate degradation of the low density lipoprotein receptor-related protein 1 (LRP-1). PLoS One. 2013;8:e64145.
Shan L, Pang L, Zhang R, Murgolo NJ, Lan H, Hedrick JA. PCSK9 binds to multiple receptors and can be functionally inhibited by an EGF-A peptide. Biochem Biophys Res Commun. 2008;375:69–73.
Demers A, Samami S, Lauzier B, et al. PCSK9 induces CD36 degradation and affects long-chain fatty acid uptake and triglyceride metabolism in adipocytes and in mouse liver. Arterioscler Thromb Vasc Biol. 2015;35:2517–25.
Schulz R, Schlüter K-D. PCSK9 targets important for lipid metabolism. Clin Res Cardiol Suppl. 2017;12:2–11.
Rajewsky K. The advent and rise of monoclonal antibodies. Nature. 2019;575:47–9.
Gibbs JP, Slatter JG, Egbuna O, et al. Evaluation of evolocumab (AMG 145), a fully human anti-PCSK9 IgG2 monoclonal antibody, in subjects with hepatic impairment. J Clin Pharmacol. 2016;57:513.
Kasichayanula S, Grover A, Emery MG, et al. Clinical pharmacokinetics and pharmacodynamics of Evolocumab, a PCSK9 inhibitor. Clin Pharmacokinet. 2018;57:769–79.
Martinez J-M, Brunet A, Hurbin F, DiCioccio AT, Rauch C, Fabre D. Population pharmacokinetic analysis of alirocumab in healthy volunteers or hypercholesterolemic subjects using a Michaelis–Menten approximation of a target-mediated drug disposition model—support for a biologics license application submission: part I. Clin Pharmacokinet. 2019;58:101–13.
Koren MJ, Lundqvist P, Bolognese M, et al. Anti-PCSK9 monotherapy for hypercholesterolemia: the MENDEL-2 randomized, controlled phase III clinical trial of evolocumab. J Am Coll Cardiol. 2014;63:2531–40.
Robinson JG, Nedergaard BS, Rogers WJ, et al. Effect of evolocumab or ezetimibe added to moderate- or high-intensity statin therapy on LDL-C lowering in patients with hypercholesterolemia: the LAPLACE-2 randomized clinical trial. JAMA. 2014;311:1870–82.
Stroes E, Colquhoun D, Sullivan D, et al. Anti-PCSK9 antibody effectively lowers cholesterol in patients with statin intolerance: the GAUSS-2 randomized, placebo-controlled phase 3 clinical trial of evolocumab. J Am Coll Cardiol. 2014;63:2541–8.
Blom DJ, Hala T, Bolognese M, et al. A 52-week placebo-controlled trial of evolocumab in hyperlipidemia. N Engl J Med. 2014;370:1809–19.
Raal FJ, Stein EA, Dufour R, et al. PCSK9 inhibition with evolocumab (AMG 145) in heterozygous familial hypercholesterolaemia (RUTHERFORD-2): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;385:331–40.
Carr SS, Hooper AJ, Sullivan DR, Burnett JR. Non-HDL-cholesterol and apolipoprotein B compared with LDL-cholesterol in atherosclerotic cardiovascular disease risk assessment. Pathology. 2019;51:148–54.
Sniderman AD, Robinson JG. ApoB in clinical care: pro and con. Atherosclerosis. 2019;282:169–75.
Orso E, Schmitz G. Lipoprotein(a) and its role in inflammation, atherosclerosis and malignancies. Clin Res Cardiol Suppl. 2017;12:31–7.
Tsimikas S. Potential causality and emerging medical therapies for lipoprotein(a) and its associated oxidized phospholipids in calcific aortic valve stenosis. Circ Res. 2019;124:405–15.
Boffa MB, Koschinsky ML. Lipoprotein (a): truly a direct prothrombotic factor in cardiovascular disease? J Lipid Res. 2016;57:745–57.
Boffa MB, Koschinsky ML. Oxidized phospholipids as a unifying theory for lipoprotein(a) and cardiovascular disease. Nat Rev Cardiol. 2019;16:305–18.
Burgess S, Ference BA, Staley JR, et al. Association of LPA variants with risk of coronary disease and the implications for lipoprotein(a)-lowering therapies: a Mendelian randomization analysis. JAMA Cardiol. 2018;3:619–27.
Nestel P. Lipoprotein(a) removal still a mystery. J Am Heart Assoc. 2019;8:e011903.
Toth PP, Jones SR, Monsalvo ML, Elliott-Davey M, López JAG, Banach M. Effect of evolocumab on non-high-density lipoprotein cholesterol, apolipoprotein B, and lipoprotein(a): a pooled analysis of phase 2 and phase 3 studies. J Am Heart Assoc. 2020;9:e014129.
Cromwell WC, Otvos JD, Keyes MJ, et al. LDL particle number and risk of future cardiovascular disease in the Framingham offspring study – implications for LDL management. J Clin Lipidol. 2007;1:583–92.
Cantey EP, Wilkins JT. Discordance between lipoprotein particle number and cholesterol content: an update. Curr Opin Endocrinol Diabetes Obes. 2018;25:130–6.
Lamarche B, St-Pierre AC, Ruel IL, Cantin B, Dagenais GR, Després JP. A prospective, population-based study of low density lipoprotein particle size as a risk factor for ischemic heart disease in men. Can J Cardiol. 2001;17:859–65.
Superko HR, Gadesam RR. Is it LDL particle size or number that correlates with risk for cardiovascular disease? Curr Atheroscler Rep. 2008;10:377–85.
Varbo A, Nordestgaard BG. Remnant lipoproteins. Curr Opin Lipidol. 2017;28:300–7.
Joshi PH, Khokhar AA, Massaro JM, et al. Remnant lipoprotein cholesterol and incident coronary heart disease: the Jackson Heart and Framingham Offspring Cohort Studies. J Am Heart Assoc. 2016;5:e002765.
Martin SS, Khokhar AA, May HT, et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: the lipoprotein investigators collaborative. Eur Heart J. 2014;36:22–30.
Toth PP, Jones SR, Slee A, et al. Relationship between lipoprotein subfraction cholesterol and residual risk for cardiovascular outcomes: a post hoc analysis of the AIM-HIGH trial. J Clin Lipidol. 2018;12:741–747.e11.
Walldius G, AASTVEIT AH, Jungner I. Stroke mortality and the apoB/apoA-I ratio: results of the AMORIS prospective study. J Intern Med. 2006;259:259–66.
Tian M, Li R, Shan Z, Wang DW, Jiang J, Cui G. Comparison of Apolipoprotein B/A1 ratio, Framingham risk score and TC/HDL-c for predicting clinical outcomes in patients undergoing percutaneous coronary intervention. Lipids Health Dis. 2019;18:202.
Toth PP, Sattar N, Blom DJ, et al. Effect of evolocumab on lipoprotein particles. Am J Cardiol. 2018;121:308–14.
Nicholls SJ, Puri R, Anderson T, et al. Effect of evolocumab on progression of coronary disease in statin-treated patients. JAMA. 2016;316:2373.
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22.
Sabatine MS, De Ferrari GM, Giugliano RP, et al. Clinical benefit of evolocumab by severity and extent of coronary artery disease. Circulation. 2018;138:756–66.
Bonaca MP, Nault P, Giugliano RP, et al. Low-density lipoprotein cholesterol lowering with evolocumab and outcomes in patients with peripheral artery disease. Circulation. 2018;137:338–50.
Sabatine MS, Leiter LA, Wiviott SD, et al. Cardiovascular safety and efficacy of the PCSK9 inhibitor evolocumab in patients with and without diabetes and the effect of evolocumab on glycaemia and risk of new-onset diabetes: a prespecified analysis of the FOURIER randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5:941–50.
O’Donoghue ML, Fazio S, Giugliano RP, et al. Lipoprotein(a), PCSK9 inhibition, and cardiovascular risk. Circulation. 2019;139:1483–92.
BjöRkhem I, Meaney S. Brain cholesterol: long secret life behind a barrier. Arterioscler Thromb Vasc Biol. 2004;24:806–15.
Katsuno M, Adachi H, Sobue G. Getting a handle on Huntington’s disease: the case for cholesterol. Nat Med. 2009;15:253–4.
Rojas-Fernandez CH, Goldstein LB, Levey AI, Taylor BA, Bittner V. An assessment by the statin cognitive safety task force: 2014 update. J Clin Lipidol. 2014;8:S5–S16.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22.
Trompet S, van Vliet P, de Craen AJ, et al. Pravastatin and cognitive function in the elderly. Results of the PROSPER study. J Neurol. 2010;257:85–90.
Etminan M, Gill S, Samii A. The role of lipid-lowering drugs in cognitive function: a meta-analysis of observational studies. Pharmacotherapy. 2003;23:726–30.
Cramer C, Haan MN, Galea S, Langa KM, Kalbfleisch JD. Use of statins and incidence of dementia and cognitive impairment without dementia in a cohort study. Neurology. 2008;71:344–50.
Rea TD, Breitner JC, Psaty BM, et al. Statin use and the risk of incident dementia. Arch Neurol. 2005;62:1047.
Giugliano RP, Mach F, Zavitz K, et al. Cognitive function in a randomized trial of evolocumab. N Engl J Med. 2017;377:633–43.
Toth PP, Descamps O, Genest J, et al. Pooled safety analysis of evolocumab in over 6000 patients from double-blind and open-label extension studies. Circulation. 2017;135:1819–31.
Kereiakes DJ, Robinson JG, Cannon CP, et al. Efficacy and safety of the proprotein convertase subtilisin/kexin type 9 inhibitor alirocumab among high cardiovascular risk patients on maximally tolerated statin therapy: the ODYSSEY COMBO I study. Am Heart J. 2015;169:906–915.e13.
Leiter LA, Cariou B, Muller-Wieland D, et al. Efficacy and safety of alirocumab in insulin-treated individuals with type 1 or type 2 diabetes and high cardiovascular risk: the ODYSSEY DM-INSULIN randomized trial. Diabetes Obes Metab. 2017;19:1781–92.
Kastelein JJ, Ginsberg HN, Langslet G, et al. ODYSSEY FH I and FH II: 78 week results with alirocumab treatment in 735 patients with heterozygous familial hypercholesterolaemia. Eur Heart J. 2015;36:2996–3003.
Ginsberg HN, Rader DJ, Raal FJ, et al. Efficacy and safety of alirocumab in patients with heterozygous familial hypercholesterolemia and LDL-C of 160 mg/dl or higher. Cardiovasc Drugs Ther. 2016;30:473–83.
Gaudet D, Watts GF, Robinson JG, et al. Effect of alirocumab on lipoprotein(a) over >/=1.5 years (from the phase 3 ODYSSEY program). Am J Cardiol. 2017;119:40–6.
Toth PP, Hamon SC, Jones SR, et al. Effect of alirocumab on specific lipoprotein non-high-density lipoprotein cholesterol and subfractions as measured by the vertical auto profile method: analysis of 3 randomized trials versus placebo. Lipids Health Dis. 2016;15:28.
Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097–107.
Sinnaeve PR, Schwartz GG, Wojdyla DM, et al. Effect of alirocumab on cardiovascular outcomes after acute coronary syndromes according to age: an ODYSSEY OUTCOMES trial analysis. Eur Heart J. 2019;41:2248.
Endres M, Nolte CH, Scheitz JF. Statin treatment in patients with intracerebral hemorrhage. Stroke. 2018;49:240–6.
Steg PG, Szarek M, Bhatt DL, et al. Effect of alirocumab on mortality after acute coronary syndromes. Circulation. 2019;140:103–12.
Goodman SG, Aylward PE, Szarek M, et al. Effects of alirocumab on cardiovascular events after coronary bypass surgery. J Am Coll Cardiol. 2019;74:1177–86.
Bittner VA, Szarek M, Aylward PE, et al. Effect of alirocumab on lipoprotein(a) and cardiovascular risk after acute coronary syndrome. J Am Coll Cardiol. 2020;75:133–44.
Jones PH, Bays HE, Chaudhari U, et al. Safety of alirocumab (a PCSK9 monoclonal antibody) from 14 randomized trials. Am J Cardiol. 2016;118:1805–11.
Robinson JG, Rosenson RS, Farnier M, et al. Safety of very low low-density lipoprotein cholesterol levels with alirocumab. Pooled data from randomized trials. J Am Coll Cardiol. 2017;69:471–82.
Toth PP. Emerging LDL therapies: Mipomersen—antisense oligonucleotide therapy in the management of hypercholesterolemia. J Clin Lipidol. 2013;7:S6–S10.
Fogacci F, Ferri N, Toth PP, Ruscica M, Corsini A, Cicero AFG. Efficacy and safety of mipomersen: a systematic review and meta-analysis of randomized clinical trials. Drugs. 2019;79:751–66.
Pratt AJ, Macrae IJ. The RNA-induced silencing complex: a versatile gene-silencing machine. J Biol Chem. 2009;284:17897–901.
Kosmas CE, Munoz Estrella A, Sourlas A, et al. Inclisiran: a new promising agent in the management of hypercholesterolemia. Diseases. 2018;6:63.
Nakanishi K. Anatomy of RISC: how do small RNAs and chaperones activate Argonaute proteins? Wiley Interdiscip Rev RNA. 2016;7:637–60.
Nair JK, Willoughby JLS, Chan A, et al. Multivalent N-acetylgalactosamine-conjugated siRNA localizes in hepatocytes and elicits robust RNAi-mediated gene silencing. J Am Chem Soc. 2014;136:16958–61.
Bon C, Hofer T, Bousquet-Melou A, Davies MR, Krippendorff BF. Capacity limits of asialoglycoprotein receptor-mediated liver targeting. MAbs. 2017;9:1360–9.
Ray KK, Landmesser U, Leiter LA, et al. Inclisiran in patients at high cardiovascular risk with elevated LDL cholesterol. N Engl J Med. 2017;376:1430–40.
Ray KK, Stoekenbroek RM, Kallend D, et al. Effect of 1 or 2 doses of inclisiran on low-density lipoprotein cholesterol levels: one-year follow-up of the ORION-1 randomized clinical trial. JAMA Cardiol. 2019;4:1067–75.
Leiter LA, Teoh H, Kallend D, et al. Inclisiran lowers LDL-C and PCSK9 irrespective of diabetes status: the ORION-1 randomized clinical trial. Diabetes Care. 2019;42:173–6.
Stoekenbroek RM, Kallend D, Wijngaard PL, Kastelein JJ. Inclisiran for the treatment of cardiovascular disease: the ORION clinical development program. Futur Cardiol. 2018;14:433–42.
Toth PP. Novel therapies for lowdensity lipoprotein cholesterol reduction. Am J Cardiol. 2016;118(6, Supplement):19A–32A.
Toth PP. PCSK9 and lipoprotein(a): the plot thickens. Circ Res. 2016;119:3–6.
Bays HE, et al. Alirocumab treatment and achievement of non-high-density lipoprotein cholesterol and apolipoprotein B goals in patients with hypercholesterolemia: pooled results from 10 phase 3 ODYSSEY trials. J Am Heart Assoc. 2017;6:e005639.
Jukema JW, et al. Effect of alirocumab on stroke in ODYSSEY OUTCOMES. Circulation. 2019;140(25):2054–62.
Nordestgaard BG, et al. Advances in lipid-lowering therapy through gene-silencing technologies. Nat Rev Cardiol. 2018;15(5):261–72.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Toth, P.P. (2021). Proprotein Convertase Subtilisin/Kexin Type 9: Functional Role in Lipid Metabolism and Its Therapeutic Inhibition. In: Davidson, M.H., Toth, P.P., Maki, K.C. (eds) Therapeutic Lipidology. Contemporary Cardiology. Humana, Cham. https://doi.org/10.1007/978-3-030-56514-5_14
Download citation
DOI: https://doi.org/10.1007/978-3-030-56514-5_14
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-030-56513-8
Online ISBN: 978-3-030-56514-5
eBook Packages: MedicineMedicine (R0)