Abstract
Since early stages are mostly asymptomatic, pancreatic cancer is often advanced by the time of diagnosis, which is associated with a poor prognosis and a very low 5-year-survival rate. Patients suffer from a range of debilitating symptoms, including pain, gastrointestinal symptoms, weight and appetite loss, jaundice and nausea and vomiting. Available treatment options have only limited capacities to prolong patients’ survival, which is why the patients’ quality of life is of utmost importance when it comes to treatment decisions and evaluating the impact of medical interventions. The gold standard to assess the patients’ quality of life is to capture their perspective of their health status by means of patient-reported outcomes. Those are self-reported statements, which come directly from the patient and are usually assessed using validated questionnaires. To measure the quality of life of pancreatic cancer patients, the most commonly used questionnaires are the EORTC-QLQ C30 and the diagnosis specific module QLQ-PAN26 and the FACT-Hep. Integrating routine assessments of quality of life offers several benefits like improved communication between health care professionals and patients, better treatment continuity or facilitation of patient-centred and tailored disease management. However, the implementation of quality of life assessments into the daily clinical routine remains a challenge. Software systems to assess, process and store patients’ quality of life electronically is one major advance new computer technology added to this field. Linking patients’ scores with sound medical information, contact details of health services and self-management advice can further foster the engagement of patients in their own health care. An increased research focus on making quality of life data actionable in routine care will help to promote their use for shared-decision making and individualized treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Quality of life
- Patient-reported outcomes
- Oncology
- Pancreatic neoplasms
- Electronic data collection
- Symptom management
- Daily clinical routine
-
Patient-reported outcomes are the gold standard to assess patients’ quality of life using validated questionnaires.
-
Before choosing a quality of life questionnaire, the purpose, timing and required content must be considered.
-
Modern assessment software is able to collect, process, calculate and present quality of life electronically in real time. Especially the increased data quality and the possibility of easy and cost-effective remote assessments (outside of the hospital setting) are major strengths of this assessment method.
-
Linking quality of life data to cut-off scores and thresholds enables indicating scores with clinically relevant impairments or changes and guiding which issues require further discussion and clinical action.
-
Patients are the experts for reporting their quality of life. They provide valuable information, which can inform their health care and disease management.
-
Validated instruments allow for the standardized assessment of quality of life of pancreatic cancer patients, considering their specific symptom burden (e.g. measuring pancreatic pain, gastrointestinal symptoms, weight loss, and taste changes).
-
Electronic assessment of patient’s quality of life data bears many advantages, (as immediate data processing, more complete data, automatically generated reports) and eye-catching cross-sectional or longitudinal quality of life data profiles ease its incorporation into the medical consultation.
-
There is still a need to catch up with promoting the use of quality of life data for shared-decision making and daily clinical routine.
-
Successful implementation of patient-reported outcome assessments into clinical routine remains a challenge, as it requires the alignment of multiple interacting stakeholders on different levels of the clinical system.
-
To encourage stakeholders to engage in routine quality of life assessments, recommendations for strategic and standardized implementation procedures should be developed and disseminated.
-
Evidence-based and scientifically sound learning material needs to be developed to inform and educate health care professionals. A profound understanding of quality of life data and how it can be used in routine care will promote its actual use.
-
The development of standardized assessment procedures and care pathways would support the uptake of routine quality of life assessments in daily clinical care, e.g. which measures are encouraged being used at different stages of pancreatic cancer including respective treatment recommendations.
-
Real-world data is needed to identify the impact of quality of life assessments and quality of life data use on the allocation of resources and the use of health care services.
1 Introduction
Pancreatic cancer is a lethal disease with an almost one-to-one ratio of new cases (ranked 13th) and cancer deaths (ranked 7th) worldwide in 2018 [1]. As it is commonly diagnosed at an advanced stage, the rate for 5-year-survival is only about 9% across all tumour stages with a more favourable outcome for resectable localized disease [2]. As 80–85% of patients are not eligible for surgery at the time of diagnosis [3], their prognosis is mostly poor and they have to deal with debilitating symptoms caused by the disease itself and/or the aggressive multimodal treatment. Hence, the patient’s quality of life (QOL) is paramount to both determining treatment goals and evaluating treatment success.
2 Patient-Reported Outcomes and Quality of Life
Discussing the patients’ subjective view of their health status has always been an important part in modern clinical care, as a variety of symptoms and issues are only accessible for clinicians through patients’ self-reports. Only the respective person him- or herself can tell if and in which intensity certain symptoms occur (e.g. pain, depression, fatigue), if he or she feels impaired in his or her social life or if e.g. sleeping disturbances have been a problem. Such information can be summarised under the umbrella term Patient-Reported Outcomes (PROs) and includes all statements made by patients about their own health status and the possible effects of treatment they receive. More importantly, PROs are assessed without any interpretation, evaluation or modification by third parties [4]. Those self-reports of patients can encompass a variety of aspects like, amongst others, functioning (e.g. physically, socially, emotionally), symptoms (e.g. anxiety, nausea, vomiting, hair loss), satisfaction with care, perceived value of care or adherence to treatment regimen. QOL is a multidimensional construct that includes aspects of a patient’s perspective of his/ her health status and can be best captured by the PRO methodology (Fig. 75.1). Most QOL questionnaires capture physical, psychological (anxiety, depression) and social aspects, query symptoms (e.g. pain, sleep disorders, impairment due to weight gain/loss) and ideally also topics that are of particular relevance to the respective patient group (e.g. for pancreatic cancer patients: altered peristalsis and taste changes after pancreatic surgery, abdominal pain, anorexia or weight loss).
schematically depicts the characteristics of PROs and QOL and their theoretical association. However, not all patient statements can be assigned to the concept of PROs. If patients share their impressions on how they experienced the delivery of health care (e.g. waiting times, access to services, involvement in decision-making or timing of assistance), this is referred to as “patient-reported experiences” (PREs). Those are commonly used as an indicator for quality of care and patient-centeredness of services. Regardless of their conceptual differences, the gold standard for the assessment of PROs and PREs is the use of validated questionnaires
3 Standardized Assessment of Quality of Life
It is already common practice to discuss the patient’s symptoms and subjective health status during the medical encounter, but the duration, depth and focus of this discussion largely depends on the clinician and his/her knowledge and personal interest in QOL. The documentation is unspecific and inevitably contains both a selection and an interpretation by the health care professional. It may even happen that a detailed conversation about symptoms and impairments has taken place, but that it is not noted or traceable in the medical records. Furthermore, other factors can impact whether and in what way QOL is part of the medical encounter (e.g. stressful days with many patients, many difficult cases, few staff due to absences, etc. hinder to dedicate time to QOL issues) (Box 75.1).
Box 75.1 PRO Measures—Not Just the Reinvention of the Wheel
-
PRO measures provide a reliable method of complementing established outcome parameters with a standardized assessment of the patient’s perspective in order to gain a comprehensive and integrated picture of the patient’s health status.
-
By implementing PROs and the resulting standardized assessment of patients’ QOL, the so far common practice of informally discussing QOL during medical appointments is raised to a higher level of professionalization.
-
Integrating QOL data documentation into the electronic medical record ensures its accessibility to clinicians and other health care professionals, increases its transparency and allows to follow the development of symptoms across a longitudinal trajectory.
-
As time is more and more becoming one of the most precious resources in a busy clinical workflow, QOL data can add to a more effective allocation of resources, especially if it is used in conjunction with thresholds and cut-off scores indicating clinically relevant changes in QOL. Highlighted scores can guide the medical encounter and help the clinician to focus on those aspects that require further immediate attention due to clinical relevance.
-
QOL data is not only of interest for clinical routine, but also contributes to scientific knowledge (gained from real world data as well as from clinical study data), can complement clinical registries and can be used for quality assurance, benchmarking and health technology assessment analyses.
Usually, questionnaires are used to assess the patient’s QOL. Patients are required to complete these measures as independently as possible to obtain their unaltered perspective. It is also possible to conduct the questionnaires as interviews or to have them assessed by relatives, although these methods require special caution (specially trained staff, specific instruction of relatives). As such proxy ratings are likely to involve to some extent an interpretation process similar to that of clinicians’ ratings, preference should be given to independent completion of questionnaires by the patients themselves.
Choosing a QOL assessment instrument requires the careful evaluation of its methodological and content-related quality, which is why the purpose of the assessment should be clear in advance. Questionnaires differ in their suitability for e.g. a general QOL screening, the evaluation of QOL during or after a certain treatment or for QOL follow-up. Attention must also be paid to the timing of data collection and the recall period of the used PRO measure, as before a medical intervention other areas might be relevant than shortly after or in long-term follow-up [5] and symptoms might occur with a delay, e.g. after administration of chemotherapy [6].
4 Quality of Life Measures for Pancreatic Cancer Patients
There is broad range of QOL assessment instruments available. Besides generic measures, which can be used irrespective of a person’s health status or a patient’s diagnostic group, there are also questionnaires available, which take special account of the needs of a certain disease group (e.g. oncological patients). A recent review, dedicated to the identification of PRO measures in pancreatic cancer patients, provides a broad overview of instruments used in this population group including those targeting QOL [7].
The choice of a generic or specific questionnaire should consider how the data collected will be used. For comparisons with a norm sample of the general population, generic instruments are useful, although disease-relevant areas are often neglected and their sensitivity to changes is low [8, 9]. In order to document the individual QOL trajectory of patients and to evaluate treatment decisions regarding their effect on QOL, disease- and/or treatment-specific measures should preferably be used. If several QOL measures are combined to capture a broader picture of the patient’s perspective, it is important to strike a careful balance between the quantity of items and their content. Merely focusing on the length of QOL measures could lead to neglecting QOL issues that are actually important for patients. Therefore, questionnaires should be chosen in such a way that they complement each other meaningfully with as few repetitions as possible [10]. Table 75.1 provides an overview of the most common generic and oncology specific QOL questionnaires or questionnaire systems including their instruments targeting pancreatic cancer.
The European Organisation for Research and Treatment of Cancer Quality of Life Questionnaires (EORTC-QLQ), the Functional Assessment of Chronical Illness Therapy (FACIT) and the Patient-Reported Outcomes Measurement Information System (PROMIS) are measurement systems for QOL in cancer patients with a modular structure. This means that a core questionnaire can be supplemented with diagnosis-specific modules or symptom indices. Furthermore, single items can be used to complement those “static” questionnaires, if important symptoms or issues are missing. As an example, the EORTC Item Library includes all items, scales and questionnaires that have been developed by the EORTC Quality of Life Group (QLG, https://qol.eortc.org) and a search function enables to quickly navigate through available measures. Since the EORTC QLQ-C30 and its disease specific module for malignancies of the pancreas QLQ-PAN26 and the FACT-Hep are the two most commonly used PRO measures to assess QOL in pancreatic cancer patients [7], those measures are described in more detail below.
4.1 Disease Specific Measures for Pancreatic Cancer
The EORTC QLQ-PAN26 targets QOL in pancreatic cancer patients and its 26 items cover the domains Pancreatic Pain, Digestive, Altered bowel habit, Hepatic, Body image, Health care satisfaction, and Sexuality. It is used as a disease-specific module for the EORTC QLQ-C30, a generic questionnaire originally developed for the assessment of cancer patients’ QOL in clinical trials. Except for the Physical Functioning scale of the QLQ-C30, the questionnaires use a recall period of 1 week and all items are rated on a 4-point Likert-scale (“not at all”, “a little”, “quite a bit”, “very much”, see Fig. 75.2). The validation of the QLQ-PAN26 in a mixed sample of pancreatic cancer patients is still pending, but there is a report on the psychometric characteristics of the questionnaire in pancreas-resected patients [21]. A recent study investigated the content validity of the QLQ-PAN26, stating that it is conceptually relevant, though it might further benefit from adding items regarding neuropathic symptoms [22]. Though the QLQ-C30 is available in more than 100 languages, translations of the QLQ-PAN26 so far only cover the ten European languages, which have been used for questionnaire development [13]. Regarding the interpretation of QOL scores assessed with EORTC measures, reference values [23], minimal important differences [24,25,26], clinically relevant thresholds for the QLQ-C30 and the QLQ CAT measures [27, 28] and general population normative data [29] are available.
The FACT-Hep comprises 45 items and is a combination of the fourth version of the FACT-G and a Hepatobiliary Subscale. The FACT-G has initially been developed and validated in cancer patients with mixed diagnoses and different disease stages and consists of 27-items covering four QOL domains: physical well-being, social/family well-being, emotional well-being, and functional well-being. The disease-specific hepatobiliary cancer subscale combines questions being relevant for patients with hepatobiliary cancers (liver, bile duct and pancreatic cancer) including back and stomach pain, anorexia, gastrointestinal symptoms, weight loss and jaundice. All items use a recall period of 1 week and a 5-point Likert-scale (“not at all”, “a little bit”, “somewhat”, “quite a bit”, and “very much”, see Fig. 75.3). The FACT-Hep is available in 43 languages. There are recommendations for the interpretation of raw score changes, but only for the FACT-G [30].
5 Challenges of Routine QOL Assessments
There is a fundamental discrepancy between acknowledging the importance of patient’s QOL and its integration into daily clinical care: While figures on mortality, morbidity, laboratory values and complication rates are established methods for evaluating treatments and disease progression, routine QOL assessments have not yet been fully implemented in clinical routine and do not represent a standard outcome measure. Many clinicians lack familiarity with the concept of QOL as well as specific knowledge on how to handle systematically collected QOL data. A common concern is that routine QOL assessments will additionally burden existing resources without offering clinical benefit [31]. There is still a widespread opinion that a patient’s QOL can be sufficiently rated by a clinician, though it is well researched that the concordance between clinician’s ratings and patient’s self-reports is often poor and even decreases over time [32,33,34,35,36,37]. Though the importance of PROs is broadly acknowledged, there are attempts to reduce the concept of QOL to the assessment of disease symptoms, physical functioning and adverse events [38]. Other criticisms are problems regarding the comparability of different PRO measures and doubts about the methodology of QOL assessment, as patients are supposed to not being able to make “true” statements about their condition and recall biases might influence the scores [39]. In the context of the current development towards a more participatory approach in medical care, it is important to acknowledge that QOL data represents a structured record of the patients’ subjective experience of specific areas of their health. These parameters are important in order to determine whether the patient’s QOL has been positively influenced by medical interventions and recommendations regarding routine QOL assessments are increasingly being incorporated into evidence-based guidelines for oncological treatment [40,41,42].
6 Benefits of Routine QOL Assessments
Routine assessment of patient’s QOL helps to improve communication with their health care professionals (e.g. increased discussion of symptoms [43, 44]). Patients themselves benefit from the use of PRO instruments, if clinicians explicitly use their collected QOL data [44]. Incorporating QOL data in their medical encounter helps clinicians to develop a better understanding of the patient’s functional level and subjective health status [45], to bring up intimate and otherwise often overlooked issues [45, 46], and to discuss chronic non-specific symptoms (e.g., sleep disorders, fatigue, loss of appetite) [44] without increasing the consultation time. In addition, the routine collection of QOL enables the identification of areas requiring treatment and the prompt referral of patients [47], which promotes patient-centred and individually tailored treatment [48, 49] and improves symptom management. Patients whose practitioners had access to QOL information reported better continuity of care than patients who did not complete QOL instruments at all. They also felt that treatment choices have been made with more consideration for their daily activities, emotional well-being and QOL [50]. Participatory decision-making can result in patients having greater confidence in their treatment decision, being more satisfied with the therapy, having a higher feeling of self-efficacy and greater trust in their caregivers [51]. QOL data even has predictive value for traditional clinical outcomes such as survival (Box 75.2) [24, 52, 53].
Box 75.2 Positive Effects of Using PRO Data in Clinical Care
-
improved communication
-
better understanding of the patients’ functional level and subjective health status
-
facilitated discussion of intimate or overlooked issues
-
more frequent discussion of chronic non-specific symptoms
-
no prolonging effect on consultation time
-
identification of need for clinical intervention and referral
-
facilitation of patient-centred care and individually tailored treatment
-
improved symptom management
-
better continuity of care
-
participatory decision-making empowers patients and increases their trust in their care
-
QOL has predictive value for survival
In addition to complex constructs such as QOL, PROs can also provide information about the patient’s view of the occurrence and intensity of treatment toxicities. The Common Toxicity Criteria of Adverse Events (CTCAE) of the National Cancer Institute have been further developed into a PRO instrument (PRO-CTCAE) [54] for those domains, which can be assessed by patients themselves. Using this new measure, ratings of adverse events, which underestimate in particular the occurrence of mild toxicities [55], can be meaningfully supplemented by the patient perspective [56]. However, neither PRO-CTCAE nor other symptom indices are an adequate substitute for established QOL instruments that are superior in terms of content validity [56]. A content analysis of the PRO-CTCAE and the EORTC QLQ instruments reports similar results since the EORTC QLQ system covers considerably more areas relevant to oncological surgery and radiotherapy than PRO-CTCAE [57].
7 Use of Electronic Data Collection Methods in Clinical Routine
Assessing QOL electronically solves many hurdles imposed by conventional paper-pencil questionnaire data collection. Because patients enter their data directly, there are no transmission errors or data loss due to lost sheets of paper. Preparing a questionnaire is less laborious, might even be carried out automatically and the application of multilingual instruments increases inclusiveness. Furthermore, collecting data electronically benefits from immediate storage, data processing and automated score calculation, making the data immediately available to health care personnel right after the questionnaire has been completed. Normative data, thresholds and cut-off scores allow identifying and highlighting clinically relevant impairments. In this way, QOL data can be used for structuring and guiding the medical encounter by focusing on areas of special interest and in need of further in-depth discussion. In particular, the use of interfaces (e.g. using common Health Level 7 standards) simplifies the exchange of data between hospital information systems and electronic PRO systems and supports the automation of administrative processes. Next to a smooth integration of QOL data assessment into the existing clinical workflow, easy access to PRO data is an important aspect to promote their use by medical staff [58]. Electronic data assessment is necessary for the use of computer-adaptive testing (CAT), which achieves greater measurement precision with a smaller number of questions and thus reduces the burden on patients. In addition, the patients are given items relevant to them, as the questions to be asked are selected based on the previously given answers.
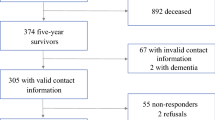
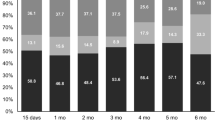
There is a broad range of assessment software available, most of which offer a variety of functionalities like data collection, processing and storage, score calculation and generation of cross-sectional or longitudinal reports, study monitoring and remote data collection including patient portals [59]. The Computer-based Health Evaluation System [60] (www.ches.pro, Fig. 75.4) is an example of a software solution which, due to its modular approach, can be used for QOL assessments in clinical routine, for conducting clinical studies and for clinical registries alike. Most software systems are internet-based, which means that access to the system is location independent. This is especially important for the use of patient portals with individual login data for patients. They facilitate to collect QOL data cost-effectively before, during, in between and after hospital stays as follow up. In addition to data assessment, such portals can also have other functionalities, such as providing trustworthy information on the disease and treatment, a presentation of one’s own QOL data with tailored self-management recommendations, and information on available health care services and their contact details. In a cohort of pancreatic and periampullary cancer undergoing pancreaticoduodenectomy, an App regularly collecting QOL data, providing tailored self-care advice and triggering alerts to a dedicated nurse who took immediate clinical action showed to be beneficial in terms of symptom control. Although the QOL scores of the patient group using the App and the control group were similar after 6 months, those of the App group indicated more stable QOL over time and especially better scores 6 weeks after surgery. They reported higher emotional functioning, fewer digestive symptoms and less pancreatic pain, less worry about low weight, less nausea/vomiting, less appetite loss, less pain, and less constipation than the control group [61].
Functionalities and structure of the Computer-based Health Evaluation System (CHES [60]) as an example for an electronic system assessing QOL
8 Conclusion
Patients are the experts for their subjective health status and validated QOL questionnaires can make their experience accessible to health care professionals in a structured way. Integrating PRO data in clinical care enhances the patient-clinician communication and promotes participatory decision-making, individual treatment management and the evaluation of medical interventions. Electronic QOL assessment contributes to effective data collection and processing, facilitates the collection of PROs outside the hospital setting (e.g. QOL data entry at home before hospital visits or long-term follow-up via a patient portal), provides additional information to patients and facilitates the use of QOL data for the medical encounter (e.g. immediate availability, application of thresholds, identification of clinically relevant symptoms and impairments). Hence, the collection of longitudinal data provides a detailed insight into the course of the disease and its treatment.
References
Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941–53.
National Cancer Institute. SEER cancer stat facts: pancreatic cancer. Bethesda, MDSeer 18 2009–2015. https://seer.cancer.gov/statfacts/html/pancreas.html.
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24(43):4846–61.
U.S. Department of Health and Human Services. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims: draft guidance. Health Qual Life Outcomes. 2006;4:79.
Neville A, Lee L, Antonescu I, Mayo NE, Vassiliou MC, Fried GM, et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br J Surg. 2014;101(3):159–70.
Giesinger JM, Wintner LM, Zabernigg A, Gamper EM, Oberguggenberger AS, Sztankay MJ, et al. Assessing quality of life on the day of chemotherapy administration underestimates patients’ true symptom burden. BMC Cancer. 2014;14:758.
Maharaj AD, Samoborec S, Evans SM, Zalcberg J, Neale RE, Goldstein D, et al. Patient-reported outcome measures (PROMs) in pancreatic cancer: a systematic review. HPB (Oxford). 2019;22(2):187–203.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Rautalin M, Färkkilä N, Sintonen H, Saarto T, Taari K, Jahkola T, et al. Health-related quality of life in different states of breast cancer – comparing different instruments. Acta Oncol. 2018;57(5):622–8.
Rolstad S, Adler J, Rydén A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health. 2011;14(8):1101–8.
The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569–85.
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–76.
Fitzsimmons D, Johnson CD, George S, Payne S, Sandberg AA, Bassi C, et al. Development of a disease specific quality of life (QoL) questionnaire module to supplement the EORTC core cancer QoL questionnaire, the QLQ-C30 in patients with pancreatic cancer. EORTC Study Group on Quality of Life. Eur J Cancer. 1999;35(6):939–41.
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–43.
Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79.
Cella D, Butt Z, Kindler HL, Fuchs CS, Bray S, Barlev A, et al. Validity of the FACT Hepatobiliary (FACT-Hep) questionnaire for assessing disease-related symptoms and health-related quality of life in patients with metastatic pancreatic cancer. Qual Life Res. 2013;22(5):1105–12.
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4.
Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11.
Gilson BS, Gilson JS, Bergner M, Bobbit RA, Kressel S, Pollard WE, et al. The sickness impact profile. Development of an outcome measure of health care. Am J Public Health. 1975;65(12):1304–10.
Wang XS, Williams LA, Eng C, Mendoza TR, Shah NA, Kirkendoll KJ, et al. Validation and application of a module of the M. D. Anderson Symptom Inventory for measuring multiple symptoms in patients with gastrointestinal cancer (the MDASI-GI). Cancer. 2010;116(8):2053–63.
Eaton AA, Karanicolas P, MChir C, Allen P, Gonen M. Psychometric validation of the EORTC QLQ-PAN26 pancreatic cancer module for assessing health related quality of life after pancreatic resection. J Pancreas. 2017;18:19–25.
Herman JM, Kitchen H, Degboe A, Aldhouse NVJ, Trigg A, Hodgin M, et al. Exploring the patient experience of locally advanced or metastatic pancreatic cancer to inform patient-reported outcomes assessment. Qual Life Res. 2019;28(11):2929–39.
Scott NW, Fayers P, Aaronson NK, Bottomley A, de Graeff A, Groenvold M, et al. EORTC QLQ-C30 reference values manual. Belgium: EORTC; 2008.
Musoro ZJ, Hamel JF, Ediebah DE, Cocks K, King MT, Groenvold M, et al. Establishing anchor-based minimally important differences (MID) with the EORTC quality-of-life measures: a meta-analysis protocol. BMJ Open. 2018;8(1):e019117.
Musoro JZ, Coens C, Fiteni F, Pogoda K, Cardoso F, Russell NS, et al. Minimally important differences for interpreting EORTC QLQ-C30 Scores in Patients with advanced breast cancer jnci cancer spectrum. JNCI Cancer Spectr. 2019;3(3)
Cocks K, King MT, Velikova G, de Castro G Jr, Martyn St-James M, Fayers PM, et al. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer. 2012;48(11):1713–21.
Giesinger JM, Loth FLC, Aaronson NK, Arraras JI, Caocci G, Efficace F, et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J Clin Epidemiol. 2020;118:1–8.
Giesinger JM, Loth FLC, Aaronson NK, Arraras JI, Caocci G, Efficace F, et al. Thresholds for clinical importance were defined for the European Organisation for Research and Treatment of Cancer Computer Adaptive Testing Core-an adaptive measure of core quality of life domains in oncology clinical practice and research. J Clin Epidemiol. 2020;117:117–25.
Nolte S, Liegl G, Petersen MA, Aaronson NK, Costantini A, Fayers PM, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the United States. Eur J Cancer. 2019;107:153–63.
Cella D, Hahn EA, Dineen K. Meaningful change in cancer-specific quality of life scores: differences between improvement and worsening. Qual Life Res. 2002;11(3):207–21.
Locklear T, Miriovsky BJ, Willig JH, Staman K, Bhavsar N, Weinfurt K, et al. Strategies for overcoming barriers to the implementation of patient-reported outcomes measures. An NIH Health Care Systems Research Collaboratory Patient Reported Outcomes Core White Paper. https://sites.duke.edu/rethinkingclinicaltrials/tools-for-research/strategies-for-overcoming-barriers-to-the-implementation-of-patient-reported-outcomes-measures/. 2014. Accessed 22 Oct 2019.
Atkinson TM, Rogak LJ, Heon N, Ryan SJ, Shaw M, Stark LP, et al. Exploring differences in adverse symptom event grading thresholds between clinicians and patients in the clinical trial setting. J Cancer Res Clin Oncol. 2017;143(4):735–43.
Chidambaram S, DeShields T, Potter P, Olsen S, Chen L. Patient and provider concordance on symptoms during the oncology outpatient clinic visit. J Community Support Oncol. 2014;12(10):370–7.
Barata A, Martino R, Gich I, García-Cadenas I, Abella E, Barba P, et al. Do patients and physicians agree when they assess quality of life? Biol Blood Marrow Transplant. 2017;23(6):1005–10.
Pakhomov SV, Jacobsen SJ, Chute CG, Roger VL. Agreement between patient-reported symptoms and their documentation in the medical record. Am J Manag Care. 2008;14(8):530–9.
Wilson KA, Dowling AJ, Abdolell M, Tannock IF. Perception of quality of life by patients, partners and treating physicians. Qual Life Res. 2000;9(9):1041–52.
Stephens RJ, Hopwood P, Girling DJ, Machin D. Randomized trials with quality of life endpoints: are doctors’ ratings of patients’ physical symptoms interchangeable with patients’ self-ratings? Qual Life Res. 1997;6(3):225–36.
Kluetz PG, Chingos DT, Basch EM, Mitchell SA. Patient-reported outcomes in cancer clinical trials: measuring symptomatic adverse events with the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). Am Soc Clin Oncol Educ Book. 2016;35:67–73.
Bossola M, Murri R, Onder G, Turriziani A, Fantoni M, Padua L. Physicians’ knowledge of health-related quality of life and perception of its importance in daily clinical practice. Health Qual Life Outcomes. 2010;8:43.
Association of Comprehensive Cancer Centres (ACCC). Oncoline Cancer Clinical Practice Guidelines. 2018. http://www.oncoline.nl/index.php. Zugriff am 01 Aug 2018.
Deutsche Krebsgesellschaft (DKG). Leitlinienprogramm Onkologie. 2018. https://www.krebsgesellschaft.de/deutsche-krebsgesellschaft/leitlinien.html. Zugriff am 01 Aug 2018.
DH on behalf of the National Health Service in England. Guidance on the routine collection of Patient Reported Outcome Measures (PROMs). 2008. http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_092625.pdf. Zugriff am 01 Aug 2018.
Takeuchi EE, Keding A, Awad N, Hofmann U, Campbell LJ, Selby PJ, et al. Impact of patient-reported outcomes in oncology: a longitudinal analysis of patient-physician communication. J Clin Oncol. 2011;29(21):2910–7.
Velikova G, Booth L, Smith AB, Brown PM, Lynch P, Brown JM, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–24.
Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA. 2002;288(23):3027–34.
Taenzer P, Bultz BD, Carlson LE, Speca M, DeGagne T, Olson K, et al. Impact of computerized quality of life screening on physician behaviour and patient satisfaction in lung cancer outpatients. Psychooncology. 2000;9(3):203–13.
Smith SK, Rowe K, Abernethy AP. Use of an electronic patient-reported outcome measurement system to improve distress management in oncology. Palliat Support Care. 2014;12(1):69–73.
Duman-Lubberding S, van Uden-Kraan CF, Jansen F, Witte BI, van der Velden LA, Lacko M, et al. Feasibility of an eHealth application “OncoKompas” to improve personalized survivorship cancer care. Support Care Cancer. 2015;24(5):2163–71.
Warrington L, Absolom K, Velikova G. Integrated care pathways for cancer survivors – a role for patient-reported outcome measures and health informatics. Acta Oncol. 2015;54(5):600–8.
Velikova G, Keding A, Harley C, Cocks K, Booth L, Smith AB, et al. Patients report improvements in continuity of care when quality of life assessments are used routinely in oncology practice: secondary outcomes of a randomised controlled trial. Eur J Cancer. 2010;46(13):2381–8.
Kane HL, Halpern MT, Squiers LB, Treiman KA, McCormack LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. 2014;64(6):377–88.
Denis F, Lethrosne C, Pourel N, Molinier O, Pointreau Y, Domont J, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst. 2017;109(9)
Rees JR, Rees M, McNair AG, Odondi L, Metcalfe C, John T, et al. The prognostic value of patient-reported outcome data in patients with colorectal hepatic metastases who underwent surgery. Clin Colorectal Cancer. 2016;15(1):74–81.e1.
Basch E, Reeve BB, Mitchell SA, Clauser SB, Minasian LM, Dueck AC, et al. Development of the National Cancer Institute’s patient-reported outcomes version of the common terminology criteria for adverse events (PRO-CTCAE). J Natl Cancer Inst. 2014;106(9)
Falchook AD, Green R, Knowles ME, Amdur RJ, Mendenhall W, Hayes DN, et al. Comparison of patient- and practitioner-reported toxic effects associated with chemoradiotherapy for head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2016;142(6):517–23.
Groenvold M, Aaronson NK, Darlington AE, Fitzsimmons D, Greimel E, Holzner B, et al. Focusing on core patient-reported outcomes in cancer clinical trials-letter. Clin Cancer Res. 2016;22(22):5617.
O’Connell Francischetto E, Gilbert A, Velikova G, Blazeby J. Is the CTCAE system suitable to use in trials in surgery and radiotherapy? A content analysis of the NCI-PRO-CTCAE and EORTC systems. In: Quality of life research, vol. 23. Amsterdam: Elsevier; 2014.
Fritz F, Dugas M. Are physicians interested in the quality of life of their patients? Usage of EHR-integrated patient reported outcomes data. Stud Health Technol Inform. 2013;192:1039.
Jensen RE, Snyder CF, Abernethy AP, Basch E, Potosky AL, Roberts AC, et al. Review of electronic patient-reported outcomes systems used in cancer clinical care. J Oncol Pract. 2014;10(4):e215–22.
Holzner B, Giesinger JM, Pinggera J, Zugal S, Schopf F, Oberguggenberger AS, et al. The Computer-based Health Evaluation Software (CHES): a software for electronic patient-reported outcome monitoring. BMC Med Inform Decis Mak. 2012;12:126.
Gustavell T, Sundberg K, Segersvärd R, Wengström Y, Langius-Eklöf A. Decreased symptom burden following surgery due to support from an interactive app for symptom management for patients with pancreatic and periampullary cancer. Acta Oncol. 2019;58(9):1307–14.
Acknowledgments
Icons used within Fig. 75.4 made by Freepik from www.flaticon.com.
Conflicts of interest: Bernhard Holzner holds intellectual property rights of the CHES software. The other authors do not state any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wintner, L.M., Sztankay, M., Holzner, B. (2021). Patient-Reported Outcomes and Quality of Life in Pancreatic Cancer. In: Søreide, K., Stättner, S. (eds) Textbook of Pancreatic Cancer. Springer, Cham. https://doi.org/10.1007/978-3-030-53786-9_75
Download citation
DOI: https://doi.org/10.1007/978-3-030-53786-9_75
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53785-2
Online ISBN: 978-3-030-53786-9
eBook Packages: MedicineMedicine (R0)