Abstract
Trauma-induced coagulopathy (TIC) and physiologic derangement occur within minutes of severe injury. For this reason, prehospital resuscitation strategies can significantly impact patient outcome. Prehospital resuscitation begins with large-bore peripheral intravenous access; however, intraosseous access is a rapid and simple option when patients are difficult to obtain intravenous access or are in extremis. Crystalloid is the mostly widely available prehospital resuscitation fluid but has deleterious pro-inflammatory effects and can exacerbate TIC. Prehospital crystalloid volume should be minimized except in patients with severe hypotension or traumatic brain injury, who may benefit from small boluses of 250–500 mL when crystalloid is the only resuscitation fluid available. Prehospital blood product transfusion has shown improved outcomes and is rapidly becoming the standard of care to treat hemorrhagic shock in the field. Strong evidence supports the use of plasma as a first resuscitation fluid in severely injured patients with prolonged transport times. Resuscitation adjuncts including tranexamic acid, fibrinogen concentrate, and prothrombin complex concentration are easily administered in the prehospital environment and show promise; however, prehospital outcome data are lacking. Whole blood is under investigation in the prehospital environment, allowing damage control resuscitation in the field while minimizing the blood products that need to be stored, carried, and administered by prehospital providers. Logistical challenges of storage are the primary barrier limiting widespread prehospital transfusion programs. Freeze-dried products overcome these barriers, as they have stable shelf lives without the need for refrigeration and are simple to reconstitute and administer in the field. Freeze-dried plasma is already available in some areas of the world, making transfusion potentially widely accessible in the prehospital environment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Prehospital
- Emergency medical services
- Field
- Ambulance
- Resuscitation
- Plasma
- Blood
- Crystalloid
- Transfusion
- Tranexamic acid
Introduction
While resuscitation of the injured patient has evolved substantially over the last two decades, only recently has it been recognized that prehospital resuscitation can have a significant impact on outcomes. There has been a focus on damage control resuscitation in the hospital-based setting, providing nearly equal ratios of packed red blood cells (PRBC), plasma, and platelets to not only replace oxygen-carrying capacity but also treat trauma-induced coagulopathy (TIC) [1, 2]. However, evidence demonstrates markers of a pro-inflammatory response and coagulopathy are present within minutes of injury at the scene [3, 4]. Thus, the type and volume of fluid that a severely injured patient receives or does not receive in the prehospital setting can set them on a trajectory toward a good or poor outcome.
While initially TIC was thought to be due to dilutional effects of crystalloid, recent work has demonstrated TIC develops with tissue injury and shock independent of resuscitation, shifting the focus toward directly addressing this TIC by restoring coagulation factors and limiting dilutional and pro-inflammatory effects from crystalloid that impair coagulation [5, 6]. Crystalloid remains the de facto resuscitation fluid in the field; however, prehospital blood product resuscitation is becoming more common [7]. This has led to a push to extend damage control resuscitation principles into the field for severely injured patients in hemorrhagic shock.
Resuscitation Access in the Field
Intravenous Access
Prehospital resuscitation begins with obtaining intravenous (IV) access in the field. Because flow rate is directly proportional to the inner cannula diameter and inversely proportional to the length of the catheter, short large-bore IVs are ideal in the bleeding trauma patient. This can be readily achieved with insertion of 16-gauge peripheral IVs. Intravenous access falls within the scope of practice for advanced life support (ALS) providers (i.e., paramedics and advanced emergency medical technicians as well as prehospital flight nurses and advance practice providers) . Attempts at peripheral access can prolong prehospital time up to 12 minutes, particularly with failed attempts [8,9,10]. Thus, transport should not be delayed for attempts at IV access, instead favoring access obtained en route. Current guidelines recommend only two attempts at peripheral IV access prior to moving on to another access modality [11].
Central venous access is rarely used in the US prehospital system but more commonly performed in European prehospital systems where physicians are routinely providing field care [12]. Some air medical services have the ability to insert central venous catheters in the United States, and studies suggest percutaneous Seldinger technique is preferred for safety and speed of access over cut-down methods [13].
Intraosseous Access
Intraosseous (IO) access has become the favored second-line access modality in most US prehospital systems, owing to its technical ease and speed of insertion with automated drills (Fig. 29.1) [15]. IO placement is commonly performed in the proximal tibia, humeral head, or occasionally the sternum. Further, IO allows infusion of fluids, medications, as well as blood products. Given these characteristics, IO access is often used as first-line access for patients in extremis or cardiac arrest.
Intraosseous access in the proximal tibia. (Reprinted with permission from Smart et al. [14])
Prehospital Crystalloid
Crystalloid Physiologic Effects
Crystalloid is the de facto resuscitation fluid used in the majority of prehospital systems in the United States. Crystalloid is inexpensive, widely available, and highly durable in a range of environmental conditions. Animal experiments in the 1960s and 1970s suggested extracellular fluid compartment deficits that required large volumes of crystalloid to correct in hemorrhagic shock [16, 17]. These findings led to the 3:1 rule of replacement with at least threefold greater volume of crystalloid than estimated blood loss and promulgation of the initial 2 l bolus of crystalloid for prehospital providers.
Subsequent investigation elucidated significant deleterious effects of crystalloid resuscitation, especially in large volumes. Saline in particular can cause metabolic hyperchloremic acidosis which in turn leads to dysregulation of the coagulation cascade enzymes at suboptimal pH levels with impaired thrombin generation. Acidosis from large volumes of saline can also impair cardiac contractility as well as the effectiveness of circulating catecholamines to effect compensatory vasoconstriction [18].
Further, crystalloid fluids incite a pro-inflammatory state with activation of neutrophils, increase neutrophil adhesion, and promote release of tumor necrosis factor-alpha, interleukin (IL)-6, IL-8, and IL-10 leading to intracellular edema and dysfunction, as well as vasodilation and capillary leak [19, 20]. Prehospital crystalloid volume has also been associated with hyperfibrinolysis in some patients, a highly lethal phenotype [21]. Dilutional effects on the coagulation proteins due to crystalloid infusion occur and contribute to clinical coagulopathic bleeding, although they are distinct from the pro-inflammatory effects promoting ongoing coagulopathy in injured patients [5, 18, 19, 22]. These detrimental effects have been borne out in clinical studies demonstrating increased mortality associated with greater volumes of prehospital crystalloid administration [21, 23,24,25].
Several groups investigated hypertonic saline as a potential prehospital resuscitation fluid, with early promising results [26,27,28,29]. Hypertonic saline was hypothesized to have a more favorable physiologic profile as it required a lower volume of fluid to restore intravascular volume and had less pro-inflammatory effects [30,31,32,33]. Two large prehospital resuscitation trials were conducted using hypertonic saline compared to isotonic crystalloid [34, 35]. One was performed in patients with traumatic brain injury (TBI) and one in patients in hemorrhagic shock; however, both were stopped early for futility (Table 29.1). Thus, hypertonic saline has not found use in prehospital resuscitation protocols in the United States.
Prehospital Crystalloid Volume
Given these findings, current practice has moved away from prehospital and early in-hospital resuscitation with large volumes of crystalloid. The landmark trial by Bickell et al. was one of the first to demonstrate withholding crystalloid infusion for patients with penetrating torso trauma until definitive hemorrhage control was achieved significantly improved survival to discharge (Table 29.1) [36]. However, not all studies have reported worse outcomes associated with higher prehospital crystalloid volume, and some have reported improved survival particularly in patients with TBI [37, 48,49,50,51,52,53]. The question of optimal prehospital crystalloid volume among different patient populations remains. This continues to be an important question, as crystalloid will continue to be the primary prehospital resuscitation fluid for the foreseeable future in the vast majority of ground emergency medical service systems, despite advances in prehospital transfusion and resuscitation.
There is some evidence that patients with hypotension in the field benefit from crystalloid administration. Hampton and colleagues demonstrated that a 16% reduction in the hazard of mortality was independently associated with a median infusion of 700 mL of prehospital crystalloid among patients requiring early blood transfusion upon arrival to the trauma center [54]. Another retrospective review of severely injured blunt trauma patients compared high (>500 mL) versus low volume of prehospital crystalloid stratified by prehospital hypotension. Patients without hypotension have a nearly 2.5-fold increase in mortality if receiving >500 mL of prehospital crystalloid; however, there was no increase in mortality for hypotensive patients [48]. Further, the highest mortality among hypotensive patients was among those receiving no prehospital crystalloid. A recent secondary analysis of the Prehospital Air Medical Plasma (PAMPer) trial demonstrated similar findings, with the highest mortality among severely hypotensive patients (systolic blood pressure <70 mmHg) receiving no prehospital crystalloid but the lowest mortality among patients receiving 1–500 mL when crystalloid was the only available prehospital resuscitation fluid [55]. The Resuscitation Outcomes Consortium conducted a pilot study that randomized patients with hypotension in the field to receive a 2 l crystalloid bolus plus fluid to maintain a systolic blood pressure >110 mmHg or receive 250 mL boluses only when systolic blood pressure was <70 mmHg or non-palpable radial pulse (Table 29.1) [38]. The group found the controlled bolus strategy resulted in a lower volume of prehospital crystalloid (average 1 l compared to 2 l) with lower unadjusted 24-hour mortality, but not adjusted mortality. This effect was predominantly in blunt trauma patients.
The harmful effects of hypotension in the field on outcome in patients with TBI are well documented, with a doubling of mortality for even a single episode of prehospital hypotension [56]. One evaluation of lowest field systolic blood pressure demonstrated an inverse relationship between survival and systolic blood pressure between 40 and 120 mmHg, suggesting no specific threshold abates the mortality associated with secondary insult in TBI [57]. Current guidelines recommend fluid therapy in the prehospital setting to maintain a systolic blood pressure >90 mmHg to prevent secondary insult, despite no direct evidence that raising the blood pressure improves survival or functional outcome [11]. One recent study demonstrated that implementation of prehospital TBI management guidelines was associated with more crystalloid boluses given, less hypotension on arrival to the trauma center, and reduced mortality in severe TBI patients [53].
Given current evidence, when crystalloid is the only prehospital fluid available to prehospital providers, very limited (<500 cc) or no crystalloid should be provided to non-hypotensive patients. Severely hypotensive patients may still benefit from small amounts of crystalloid, with 250 mL boluses targeting a systolic blood pressure of 70–80 mmHg, palpable radial pulse, or normal mental status, especially in blunt trauma without TBI. Providers should aim for a total volume of 500 mL to a maximum of 1 l. Patients with penetrating torso trauma should receive limited or no prehospital fluid, and prehospital access/resuscitation attempts should not delay transport to a trauma center. Finally, in the absence of additional evidence, patients with suspected TBI should receive crystalloid boluses targeting a systolic blood pressure >90 mmHg.
Prehospital Blood Products
With mounting evidence of the deleterious effect of crystalloids in severely injured patients, the focus is now on damage control resuscitation with blood product component resuscitation and attention to the ratio of plasma and platelets to PRBC. The goal is to restore tissue oxygenation and a more physiologic coagulation milieu with the repletion of coagulation factors and platelets while avoiding the pro-inflammatory and dilutional coagulopathy induced from crystalloid infusion. This strategy has shifted toward earlier and higher ratio of blood product components, with a more balanced component transfusion in an attempt to approximate what is lost—whole blood. Given the success of damage control resuscitation employed early in the hospital setting [1, 2, 58, 59], it only makes sense to push this strategy into the field to address hemorrhagic shock as early as possible. Data demonstrating death from hemorrhage occurs within the first 3 hours from injury and one-third of deaths from exsanguination occur in the field highlight the critical window for blood product administration in the prehospital setting [60, 61].
The initial experience with prehospital blood product resuscitation dates back to military medicine in World War II [62] (see Chap. 1). More recently demonstrated in Iraq and Afghanistan, prehospital blood product resuscitation has shown improved survival and has become the standard of combat casualty care when available [63,64,65,66,67]. Guidelines for logistics and safety of such practices in civilian prehospital trauma care have prevented widespread generalizability until lately. A survey of level 1 and 2 trauma centers participating in the Trauma Quality Improvement Program (TQIP) indicated that 34% of emergency medical services have the capability to administer prehospital blood products [7].
Packed Red Blood Cells
Packed red blood cell transfusion is the most commonly available prehospital blood product [7]. To date PRBC capabilities have generally been limited to air medical transport agencies, and early evidence has shown the practice to be both safe and feasible [68, 69]. Although prehospital PRBC transfusion has been available for decades in some areas, it is only recently that data have shown support for this practice.
The military evidence has shown improvements in mortality for patients receiving prehospital PRBC in recent conflicts. Deployment of advanced medical platforms with prehospital PRBC transfusion capabilities in the US and UK military resulted in greater than expected survival for severely injured patients [70]. Morrison et al. demonstrated that advanced prehospital capabilities including transfusion of PRBC in one-third of casualties demonstrated a 6% absolute mortality reduction among patients with injury severity score >15 [65].
The civilian evidence for the effectiveness of prehospital PRBC is mounting as well. Early studies evaluated small numbers of patients without the power to truly demonstrate effectiveness [71]. One small study of 50 propensity-matched patients receiving prehospital PRBC from the Glue Grant multicenter collaborative found a reduction in 24-hour and 30-day mortality, as well as lower risk of TIC as approximated by INR [72]. A larger single-center propensity-matched cohort of 240 air medical patients receiving prehospital PRBC after injury from the same group demonstrated that prehospital PRBC transfusion was associated with improved 24-hour mortality, lower risk of shock on arrival, and fewer PRBC required in the first 24 hours after admission [73]. A systematic review of prehospital PRBC evaluated 16 case series and 11 comparative studies [74]. The authors noted low quality of evidence with no overall effect on early or late mortality; however, they noted that studies which matched patients for severity of injury consistently suggested modest survival improvement.
Plasma
Use of prehospital plasma transfusion has gained increasing interest. Plasma has several advantages as a resuscitation fluid. Like PRBC, plasma is iso-osmolar with circulating blood and thus is an ideal fluid expander. Unlike PRBC, however, plasma contains the clotting proteins to directly address the TIC that occurs early in patients with tissue injury and hemorrhagic shock [40]. Finally, there is increasing evidence that endothelial glycocalyx degradation results in coagulopathy and endothelial dysfunction in hemorrhagic shock [75, 76]. In preclinical data, plasma has been shown to attenuate the disruption of the endothelial glycocalyx, improving outcome [77, 78].
As prehospital PRBC have long been available, few studies evaluate the sole effect of prehospital plasma resuscitation for trauma. The Mayo Clinic transport program added plasma transfusion capabilities in 2011 and reported the first five patients receiving plasma only with TBI on warfarin for reversal [79]. All patients survived more than 24 hours and had a mean decrease of 1.2 in INR upon arrival at the trauma center. The same group updated their results in patients with TBI, comparing 36 patients receiving prehospital plasma to 40 patients receiving prehospital PRBC [80]. They found significantly improved neurologic outcomes at 6 months with higher functioning and lower disability among the prehospital plasma group.
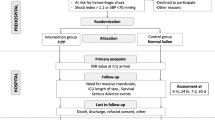
With the promising results of preclinical and early clinical prehospital plasma data, the US Department of Defense issued a program announcement to evaluate prehospital plasma resuscitation for hemorrhagic shock in the civilian population. Ultimately two randomized trials were funded and completed, the PAMPer trial and the Control Of Major Bleeding After Trauma (COMBAT) trial (Table 29.1) [81, 82]. The multicenter PAMPer trial used a cluster randomized design by helicopter base to randomize air medical patients with severe hypotension or hypotension plus tachycardia to receive two units of thawed plasma or standard prehospital resuscitation with crystalloid or PRBC. A total of 501 patients were included and the plasma group had a 10% absolute reduction in 30-day mortality compared to the standard care arm [39]. The separation in the survival curve became evident beginning at 3 hours from injury (Fig. 29.2). There were lower 24-hour mortality, slight reduction in 24-hour transfusion requirements, and no difference in adverse events in the plasma group.
The single-center COMBAT trial randomized patients to receive thawed plasma or crystalloid in an urban ground emergency medical services system with plasma delivered upon arrival to the trauma center in both groups. A total of 125 patients were included and no difference in 24-hour or 28-day mortality was seen between the plasma or crystalloid groups [40]. When taking both trials into consideration, it becomes apparent that different populations were studied. The COMBAT trial was an urban population with median prehospital time of 26 minutes, while the PAMPer trial included air medical patients with a median prehospital time of 41 minutes. Thus, it seems early plasma transfusion is necessary, whether at the trauma center when prehospital times are short or in the prehospital setting with prolonged prehospital times.
Packed Red Blood Cells and Plasma
Following the paradigm of damage control resuscitation in the hospital setting, investigation of resuscitation with a balanced ratio of plasma and PRBC in the prehospital setting is ongoing. Early results by Kim and colleagues in nine patients receiving prehospital PRBC and plasma compared to only PRBC suggested adding plasma resulted in greater improvement in coagulation status, higher plasma to PRBC ratio over the first 24 hours, and less crystalloid infusion [83]. As the military has added prehospital plasma capabilities to forward medical units, a retrospective matched cohort study of US combatants who experienced traumatic amputation or shock demonstrated that prehospital administration of PRBC and plasma resulted in a 15% and 12% reduction in mortality at 24 hours and 30 days, respectively [67]. Notably, of all injured patients who died, 70% where prior to hospital arrival, and of those, 74% were not transfused, again stressing the potential benefit of prehospital transfusion. A review of matched patients in the UK military experience also indicated an 11% reduction in casualties receiving prehospital PRBC and plasma transfusion [66].
Holcomb et al. reviewed their early experience of prehospital PRBC and plasma transfusion in their air medical transport program [84]. They compared 137 patients receiving PRBC and plasma to 169 controls with crystalloid only, demonstrating lower early hemorrhage rates and very early death from exsanguination in the first 6 hours, but no difference in 24-hour or 30-day mortality. A follow-up multicenter prospective study from this group compared air medical transport systems with PRBC and plasma to those without prehospital transfusion capabilities [85]. They did not find a difference in mortality; however, the data was hampered by significant differences in injury severity among patients receiving transfusion, as most systems now transfuse any severely injured patient with prehospital blood products when available. Most recently, Guyette and colleagues found that patients who received both PRBC and plasma in the PAMPer trial had the greatest survival benefit over patients receiving either PRBC or plasma alone (Fig. 29.3) [55]. A meta-analysis of prehospital transfusion suggested a pooled reduction in the odds of long-term mortality for prehospital transfusion of both PRBC and plasma, but not for PRBC alone [86].
Considering the body of evidence for improved outcomes with damage control resuscitation in the hospital setting and the more recent prehospital data, trauma patients at risk for hemorrhagic shock should be resuscitated with balanced blood product components as close to the time of injury as possible to prevent the development of coagulopathy and the ensuing shock and inflammatory state associated with early mortality, most commonly within 3 hours. High ratio blood product replacement in essence reconstitutes whole blood, and current data shows the use of PRBC and plasma is feasible within modern emergency medical service transport programs [87]. The benefit of this approach is less clear in urban ground emergency medical systems with short transport times to a trauma center with damage control resuscitation capabilities.
Platelets
There is evidence that platelets are a critical component of damage control resuscitation. Evaluation of platelet transfusion has shown that higher early ratios of platelet to PRBC transfusion are associated with reduced mortality, and platelet transfusion in the PROPPR trial was associated with lower early mortality and improved hemostasis [88,89,90]. These data suggest early platelet transfusion in the field may be beneficial, despite limited availability of platelets in the prehospital setting [91]. At current, no studies evaluate outcomes of prehospital platelet transfusion, although the Mayo Clinical transport program recently added cold stored platelets to their prehospital transfusion capabilities [92]. Storage in the prehospital environment presents a particular challenge for platelets, but given the evidence for prehospital PRBC and plasma, cold stored platelets and whole blood storage that retains platelet function are receiving increasing interest [93,94,95].
Logistical Considerations
There are several challenges associated with a prehospital transfusion program. Foremost is a good working relationship with the blood bank that will be supplying products to the prehospital agency. Agencies must determine what type of products they will carry. Many agencies carry universal donor products (O negative PRBC, AB plasma); however, given the limited supply of these blood types, arguments have been made for use of low titer O positive blood and A low titer B plasma [96, 97].
There are generally two models for prehospital blood product programs. For prehospital agencies that are based at a participating hospital, blood products may be obtained “on demand” from the in-house blood banks. This model significantly decreases regulatory oversight and costs to the agency; however, it is only available to units stationed at the hospital and may prolong response time while obtaining the required blood products. When bases are located away from a participating blood bank site, base accommodations must be made to store blood products on site. Depending on local practices and regulations, it may be necessary to certify the prehospital agency bases as satellite blood banks. The agency must then purchase blood products from the blood bank at a cost of $100 to $400 per unit depending on type of blood component, blood type, and regional availability. The base must also purchase a blood refrigerator for storage (approximately $3500–$7500). Prehospital personnel then become responsible for proper storage and transport, recycling of units to prevent wastage, and documentation for the blood products (Fig. 29.4).
Prehospital crews must undergo training for the proper care and storage of blood products. Products generally need to be kept between 1 and 6 °C. Crews must check products on a daily basis to ensure proper function of the storage refrigerator to maintain necessary temperatures, monitor expiration date, make sure products are free from contamination and proper functioning of transport coolers for missions. These responsibilities must be outlined in protocols for crews, as well as protocols for maintenance for the storage refrigerator and documentation of storage conditions. Policies must also be developed that outline how the blood will be transported on the vehicle or aircraft during missions.
Additionally, protocols must be adopted for ordering of new blood product units when transfused on a mission, as well as when products approach their expiration date. Agencies must work with their blood bank to determine when and how the products will be recycled back to an appropriate hospital blood bank for use in the general pool to prevent wastage. PRBC have a maximum shelf life of 42 days, liquid plasma of 21 days, and fresh frozen plasma of 5 days, although some lead time is necessary to allow for recycling into the blood bank inventory and release for transfusion prior to expiration. An inventory and expiration tracking log are essential and may be electronic or paper based.
Step-by-step protocols must be developed for the process and documentation of blood transfusion in the prehospital environment. The protocol must consider the applicable scope of practice to ensure transfusion falls within the scope of practice for the prehospital providers. Indications for transfusion must be clearly delineated, as well as process for direct medical command, and can be adapted from published protocols [73]. The protocol must also address monitoring, treatment, and documentation of potential transfusion reactions.
Finally, a strong quality assurance program is necessary. This must incorporate monitoring and benchmarking of appropriate patient selection for transfusion, transfusion reactions, product usage and recycling, as well as wastage due to expiration or out of range temperature. Thus, prehospital blood transfusion programs can come with significant expense in both equipment and training. An analysis of the thawed plasma air medical program employed in the PAMPer trial demonstrated an annual cost of $25,000–$30,000 per helicopter base; however, most of the cost was due to courier costs to recycle plasma units with a short shelf life of only 5 days [98]. They suggest that liquid plasma with a longer shelf life and efficient recycling systems can mitigate a significant proportion of this cost. Up-front costs can be an investment of well over $10,000, with maintenance costs of several thousand dollars annually; however, evidence suggests real benefits to patients, and we believe the costs are well worth it when feasible to implement.
Prehospital Resuscitation Adjuncts
Tranexamic Acid
Several resuscitation adjuncts have emerged as part of hemostatic and damage control resuscitation principles and are now receiving interest in the prehospital arena. The adjunct that has garnered the most attention is prehospital use of tranexamic acid (TXA). Since the CRASH-2 trial was published demonstrating a reduction in mortality from exsanguination when TXA was administered within 3 hours of injury and the greatest benefit when given within 1 hour of injury [99], prehospital administration has become an attractive therapeutic option. Subsequent military and civilian data suggested a potential increased risk of venous thromboembolic events despite potential benefits, highlighting the need for appropriate patient selection [100, 101] (see Chap. 11).
Several prehospital systems have implemented prehospital TXA protocols in both ground and air transport systems, showing early feasibility of TXA administration in the field [102, 103]. Given the recent implementation of TXA in the prehospital environment, long-term outcomes are lacking with mixed early results. A Swiss study demonstrated reduced fibrinolysis in 24 patients receiving prehospital TXA, but no change in clinical outcomes compared to a propensity-matched cohort [104]. Neeki et al. propensity-matched 362 patients receiving prehospital TXA to a historical cohort and found lower mortality among patients receiving TXA, although there was no adjustment for secular trend and the study population had a low overall mortality rate [105]. Boudreau and colleagues found no difference in mortality for prehospital versus emergency department TXA administration; however, only 116 patients were included during the study period [106].
One criticism of the adoption of prehospital TXA based on the CRASH-2 trial is generalizability, as CRASH-2 was conducted in resource-poor environments without the capacity for damage control resuscitation. Thus, it’s not clear the same benefits will translate to more developed trauma and prehospital systems that have the capacity to provide prehospital transfusion and early damage control resuscitation. To that end, there are three current multicenter randomized trials underway that evaluate prehospital TXA in developed trauma systems, including the STAAMP trial, the PATCH trial, and the Prehospital Tranexamic Acid Use for Traumatic Brain Injury trial (Table 29.1) [107]. The highly anticipated results of these trials will elucidate the efficacy and dosing of TXA in the prehospital environment.
Fibrinogen
Fibrinogen concentrate is another proposed adjunct for early resuscitation. Fibrinogen levels are the first to become critically low and are associated with higher mortality in both civilian and combat casualties with TIC [108,109,110]. Fibrinogen concentrate is logistically appealing for the prehospital environment as it does not require thawing or crossmatching, and high doses can be rapidly administered over minutes. Early results suggest potential mortality improvements in severely injured patients with TIC that received fibrinogen. Stinger et al. showed that higher fibrinogen in the form of plasma, cryoprecipitate, whole blood, or platelets per unit of PRBC in massively transfused patients was associated with reduced mortality [110]. Administration of fibrinogen concentrate based on thrombelastography led to lower than predicted mortality in one study [111]. Finally, universal administration of 3 g of fibrinogen concentrate led to higher survival compared to no fibrinogen or administration only when plasma fibrinogen levels were low among severely injured patients [112]. Prehospital data on fibrinogen administration, however, is lacking. Two ongoing trials are evaluating the effects of fibrinogen concentrate in prehospital resuscitation algorithms and will help to shed light on the potential benefits of this adjunct (Table 29.1) [45, 113].
Prothrombin Complex Concentrate
The final resuscitation adjunct that is receiving attention is prothrombin complex concentrate (PCC), available in either 3 factor or 4 factor formulations. PCC has gained popularity owing to its rapid reversal of vitamin K antagonist anticoagulation, particularly in patients with TBI [114]. PCC again is attractive for prehospital use given its ease of storage and administration. Evidence suggest that 4 factor PCC may reverse coagulopathy faster, resulting in fewer transfusions than 3 factor formulations [115]. A recent propensity-matched study demonstrated reduced mortality associated with coadministration of PCC with plasma compared to plasma alone in patients with TIC in the absence of vitamin K antagonist use [116]. An ongoing trial is comparing addition of PCC to fibrinogen concentrate for in-hospital resuscitation of patients with TIC [117]. Prehospital data on PCC is limited to case reports and 1 small case series of 34 patients receiving PCC for pre-injury warfarin anticoagulation from a rural air medical transport service demonstrating reduced time to reversal of anticoagulation [118,119,120]. PCC appears to show promise in the prehospital environment for patients with known vitamin K antagonist anticoagulation, particularly in the setting of TBI; however, this requires further study given the lack of robust data and potential for thrombotic adverse events in TIC patients without pre-injury anticoagulation.
Future of Prehospital Resuscitation
Whole Blood
Given significant benefits of PRBC and plasma administered in the field to injured patients, the future of prehospital resuscitation lies with optimizing prehospital transfusion strategies. Currently, the logistical challenges of storage and space restrictions limit widespread applicability. Prehospital transfusion programs are largely confined to air medical transport programs and a very small number of well-resourced ground transport agencies. The promising results of prehospital transfusion of both PRBC and plasma over a single blood product suggest the use of prehospital whole blood may be the ideal approach to prehospital resuscitation [55, 86]. Whole blood has long been used in the military, demonstrating improved survival over component therapy in combat casualties [121]. Recently, the Army Rangers have developed an O low-titer whole blood program to provide whole blood transfusion at the point of wounding.
Cold stored whole blood transfusion for trauma has gained increasing interest given the benefits of damage control resuscitation which aims to reconstitute whole blood through high component ratios. Initial safety of cold stored whole blood has been demonstrated [95]. Several trauma centers across the United States have added whole blood capabilities to their initial resuscitation algorithm of injured patients [92, 97, 122]. Whole blood is not without issues, however, including reduced and dysfunctional platelets. Future challenges involve improving platelet sparing filter technology for whole blood preparation.
Use of whole blood in the prehospital arena reduces the space required to carry and store both PRBC and plasma for prehospital agencies. Further, since PRBC and plasma have different shelf lives, using a single product (i.e., whole blood) reduces the risk for wastage and burden on prehospital providers to track and appropriately return PRBC and plasma on differing schedules.
Whole blood has begun to make its way into the prehospital environment in select locations. The Norwegian air medical transport program deployed cold stored whole blood in 2015 [92]. The Norwegian service has long had a progressive prehospital transfusion program given the challenging geography and long distances over 370 miles between trauma centers in the county. In Texas, two emergency medical service agencies near Houston became the first prehospital ground agencies to carry whole blood, followed shortly by air and ground providers in San Antonio [97, 123]. The Mayo Clinic transport program which has long been a proponent of remote damage control resuscitation has added cold stored whole blood to their capabilities recently [92]. These early implementors are collecting ongoing data to evaluate outcomes; however, no prospective comparative or randomized data exists for prehospital whole blood administration in trauma. Thus, investigators at the University of Pittsburgh are conducting a randomized pragmatic trial to evaluate the efficacy of prehospital whole blood compared to standard prehospital resuscitation practice with crystalloid and PRBC (Table 29.1) [46].
Freeze-Dried Products
Another exciting frontier for prehospital resuscitation is the use of lyophilized or freeze-dried products. The process involves applying low temperature, low moisture, and low pressure environment or spray-drying by aerosolizing the product into a high temperature chamber to remove moisture [124]. This obviates the need for cold storage of blood products in the prehospital environment. It also extends the shelf life to the order of years. Reconstitution is rapid and simple in the field with comparable physiologic activity [125], making freeze-dried products the ideal solution for prehospital resuscitation.
Lyophilization of red blood cells has been hampered by damage to the cells without cryoprotectants such as glycerol; however, significant progress has been made using novel processes that allow for small volumes of freeze-dried red blood cells with acceptable functional rehydration of cells [126]. Technology exists to freeze-dry platelets as well; however, the limiting factor has been safety concerns. Animal studies of lyophilized platelet transfusion demonstrate short activity, excess thrombogenicity, and splenic accumulation that limits clinical applicability in current form [127].
Freeze-dried plasma for prehospital use has been the focus of recent attention, particularly given the survival benefit seen in the PAMPer trial [39]. Freeze-dried plasma was used in World War II but abandoned due to high rates of hepatitis C (see Chap. 1), but pathogen reduction technology has eliminated this concern. Commercially available freeze-dried plasma products already exist from manufactures in Germany, France, and South Africa [128]; however, freeze-dried plasma is not Food and Drug Administration (FDA) approved for use in the United States due to historical concerns of infectious contamination risks [124]. Prehospital freeze-dried plasma has been used by French military and civilian trauma teams, Norwegian air medical transport services, and Israeli Defense Forces with data supporting feasibility in the prehospital environment [129,130,131]. A recent in-hospital pilot trial of freeze-dried plasma compared to fresh frozen plasma suggested freeze-dried plasma achieved higher fibrinogen concentrations and better thrombelastography parameters [132]. Large-scale studies of outcomes for prehospital administration of freeze-dried plasma are awaited from two ongoing phase III trials (Table 29.1) [133].
Freeze-dried plasma has received particular interest from the US military. The FDA recently approved the use of freeze-dried plasma for US military while evaluating civilian approval of the product [134]. The US Army is supporting the development of US-based freeze-dried products (Fig. 29.5) [133], and US special forces are currently carrying the French manufactured product [128]. The US military is also planning a multicenter trial to evaluate outcomes of prehospital freeze-dried plasma administration in collaboration with civilian trauma systems.
RePlas® freeze-dried plasma kit manufactured by Teleflex® Incorporated. (Photo credit: Teleflex® Incorporated United States Securities and Exchange Commission Filing Form 8-K, May 3rd, 2018; available at: https://teleflexincorporated.gcs-web.com/node/18871/html)
Summary
The onset of physiologic derangements including the development of TIC occurs within minutes of injury. Prehospital resuscitation is increasingly recognized to have significant influence on injured patients’ outcomes. Intravenous access with large-bore peripheral sites is the standard, although intraosseous access is gaining popularity when patients are difficult to obtain intravenous access or are in extremis. Crystalloid is the mostly widely available prehospital resuscitation fluid but has pro-inflammatory effects and can exacerbate TIC. Prehospital crystalloid volume should be minimized if any is infused, although patients with severe hypotension or TBI may benefit from a moderate amount of crystalloid when it is the only resuscitation fluid available. Prehospital blood product transfusion has shown improved outcomes over crystalloid and is rapidly becoming the standard of care for well-resourced air medical transport programs to treat hemorrhagic shock. Plasma in particular has strong supporting evidence in patients with prolonged transport times. Resuscitation adjuncts including tranexamic acid, fibrinogen concentrate, and prothrombin complex concentration are easily administered in the prehospital environment and show promise; however, prehospital outcome data are lacking. Whole blood may be an ideal resuscitation fluid in the prehospital setting, allowing damage control resuscitation in the field while minimizing the number of products that need to be stored, carried, and administered by prehospital providers. Logistical challenges of storage are the primary barrier limiting widespread prehospital transfusion programs, and freeze-dried products may eliminate these barriers, making prehospital damage control resuscitation accessible to all injured patients with hemorrhagic shock in the future.
References
Holcomb JB, del Junco DJ, Fox EE, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time-varying treatment with competing risks. JAMA Surg. 2013;148:127–36.
Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313:471–82.
Floccard B, Rugeri L, Faure A, et al. Early coagulopathy in trauma patients: an on-scene and hospital admission study. Injury. 2012;43:26–32.
Spielmann S, Kerner T, Ahlers O, et al. Early detection of increased tumour necrosis factor alpha (TNFα) and soluble TNF receptor protein plasma levels after trauma reveals associations with the clinical course. Acta Anaesthesiol Scand. 2001;45:364–70.
Chang R, Cardenas JC, Wade CE, et al. Advances in the understanding of trauma-induced coagulopathy. Blood. 2016;128:1043–9.
Gonzalez E, Moore EE, Moore HB, et al. Trauma-induced coagulopathy: an institution’s 35 year perspective on practice and research. Scand J Surg. 2014;103:89–103.
Camazine MN, Hemmila MR, Leonard JC, et al. Massive transfusion policies at trauma centers participating in the American College of Surgeons Trauma Quality Improvement Program. J Trauma Acute Care Surg. 2015;78:S48–53.
Carr BG, Brachet T, David G, et al. The time cost of prehospital intubation and intravenous access in trauma patients. Prehosp Emerg Care. 2008;12:327–32.
Sampalis JS, Tamim H, Denis R, et al. Ineffectiveness of on-site intravenous lines: is prehospital time the culprit? J Trauma Acute Care Surg. 1997;43:608–17.
SMITH JP, BODAI BI, HILL AS, et al. Prehospital stabilization of critically injured patients: a failed concept. J Trauma Acute Care Surg. 1985;25:65–70.
Cotton BA, Jerome R, Collier BR, et al. Guidelines for prehospital fluid resuscitation in the injured patient. J Trauma Acute Care Surg. 2009;67:389–402.
Fyntanidou B, Fortounis K, Amaniti K, et al. The use of central venous catheters during emergency prehospital care: a 2-year experience. Eur J Emerg Med. 2009;16:194–8.
Westfall MD, Price KR, Lambert M, et al. Intravenous access in the critically ill trauma patient: a multicentered, prospective, randomized trial of saphenous cutdown and percutaneous femoral access. Ann Emerg Med. 1994;23:541–5.
Smart RJ, Marsh S, Rosenberg M. Intraosseous access in oral and maxillofacial surgical practice. J Oral Maxillofac Surg. 2011;69(11):2708–13.
Frascone RJ, Jensen JP, Kaye K, et al. Consecutive field trials using two different intraosseous devices. Prehosp Emerg Care. 2007;11:164–71.
Bacter CR, Canizaro PC, Carrico CJ, et al. Fluid resuscitation of hemorrhagic shock. Postgrad Med. 1970;48:95–9.
Carrico CJ, Canizaro PC, Shires GT. Fluid resuscitation following injury: rationale for the use of balanced salt solutions. Crit Care Med. 1976;4:46–54.
Martini WZ, Cortez DS, Dubick MA. Comparisons of normal saline and lactated Ringer’s resuscitation on hemodynamics, metabolic responses, and coagulation in pigs after severe hemorrhagic shock. Scand J Trauma Resusc Emerg Med. 2013;21:86.
Cotton BA, Guy JS, Morris JA Jr, et al. The cellular, metabolic, and systemic consequences of aggressive fluid resuscitation strategies. Shock. 2006;26:115–21.
Rhee P, Wang D, Ruff P, et al. Human neutrophil activation and increased adhesion by various resuscitation fluids. Crit Care Med. 2000;28:74–8.
Cotton BA, Harvin JA, Kostousouv V, et al. Hyperfibrinolysis at admission is an uncommon but highly lethal event associated with shock and prehospital fluid administration. J Trauma Acute Care Surg. 2012;73:365–70.
Kaczynski J, Wilczynska M, Hilton J, et al. Impact of crystalloids and colloids on coagulation cascade during trauma resuscitation-a literature review. Emerg Med Health Care. 2013;1:1.
Haut ER, Kalish BT, Cotton BA, et al. Prehospital intravenous fluid administration is associated with higher mortality in trauma patients: a National Trauma Data Bank analysis. Ann Surg. 2011;253:371–7.
Hussmann B, Heuer M, Lefering R, et al. Prehospital volume therapy as an independent risk factor after trauma. Biomed Res Int. 2015;2015:354367.
Kasotakis G, Sideris A, Yang Y, et al. Aggressive early crystalloid resuscitation adversely affects outcomes in adult blunt trauma patients: an analysis of the Glue Grant database. J Trauma Acute Care Surg. 2013;74:1215–21; discussion 1221–2.
Vassar MJ, Fischer RP, O’Brien PE, et al. A multicenter trial for resuscitation of injured patients with 7.5% sodium chloride. The effect of added dextran 70. The Multicenter Group for the study of hypertonic saline in trauma patients. Arch Surg. 1993;128:1003–11; discussion 1011–3.
Vassar MJ, Perry CA, Gannaway WL, et al. 7.5% sodium chloride/dextran for resuscitation of trauma patients undergoing helicopter transport. Arch Surg. 1991;126:1065–72.
Vassar MJ, Perry CA, Holcroft JW. Prehospital resuscitation of hypotensive trauma patients with 7.5% NaCl versus 7.5% NaCl with added dextran: a controlled trial. J Trauma. 1993;34:622–32; discussion 632–3.
Bulger EM, Jurkovich GJ, Nathens AB, et al. Hypertonic resuscitation of hypovolemic shock after blunt trauma: a randomized controlled trial. Arch Surg. 2008;143:139–48; discussion 149.
Angle N, Hoyt DB, Coimbra R, et al. Hypertonic saline resuscitation diminishes lung injury by suppressing neutrophil activation after hemorrhagic shock. Shock. 1998;9:164–70.
Deitch EA, Shi HP, Feketeova E, et al. Hypertonic saline resuscitation limits neutrophil activation after trauma-hemorrhagic shock. Shock. 2003;19:328–33.
Gurfinkel V, Poggetti RS, Fontes B, et al. Hypertonic saline improves tissue oxygenation and reduces systemic and pulmonary inflammatory response caused by hemorrhagic shock. J Trauma. 2003;54:1137–45.
Kramer GC, English TP, Gunther RA, et al. Physiological mechanisms of fluid resuscitation with hyperosmotic/hyperoncotic solutions. Prog Clin Biol Res. 1989;299:311–20.
Bulger EM, May S, Brasel KJ, et al. Out-of-hospital hypertonic resuscitation following severe traumatic brain injury: a randomized controlled trial. JAMA. 2010;304:1455–64.
Bulger EM, May S, Kerby JD, et al. Out-of-hospital hypertonic resuscitation after traumatic hypovolemic shock: a randomized, placebo controlled trial. Ann Surg. 2011;253:431–41.
Bickell WH, Wall MJ Jr, Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331:1105–9.
Turner J, Nicholl J, Webber L, et al. A randomised controlled trial of prehospital intravenous fluid replacement therapy in serious trauma. Health Technol Assess. 2000;4:1–57.
Schreiber MA, Meier EN, Tisherman SA, et al. A controlled resuscitation strategy is feasible and safe in hypotensive trauma patients: results of a prospective randomized pilot trial. J Trauma Acute Care Surg. 2015;78:687–95; discussion 695–7.
Sperry JL, Guyette FX, Brown JB, et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379:315–26.
Moore HB, Moore EE, Chapman MP, et al. Plasma-first resuscitation to treat haemorrhagic shock during emergency ground transportation in an urban area: a randomised trial. Lancet. 2018;392:283–91.
Smith IM, Crombie N, Bishop JR, et al. RePHILL: protocol for a randomised controlled trial of pre-hospital blood product resuscitation for trauma. Transfus Med. 2018;28:346–56.
Brown JB, Neal MD, Guyette FX, et al. Design of the study of tranexamic acid during air medical prehospital transport (STAAMP) trial: addressing the knowledge gaps. Prehosp Emerg Care. 2015;19:79–86.
Pre-hospital Anti-fibrinolytics for Traumatic Coagulopathy and Haemorrhage (The PATCH Study). NCT02187120 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT02187120. Accessed 13 June 2019.
Prehospital tranexamic acid use for traumatic brain injury (TXA). NCT01990768 2019. Available at: https://clinicaltrials.gov/ct2/show/record/NCT01990768. Accessed 13 June 2019.
Maegele M, Zinser M, Schlimp C, et al. Injectable hemostatic adjuncts in trauma: fibrinogen and the FIinTIC study. J Trauma Acute Care Surg. 2015;78:S76–82.
Pragmatic prehospital group O whole blood early resuscitation trial (PPOWER). NCT03477006 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT03477006. Accessed 26 May 2019.
Pre-hospital administration of lyophilized plasma for post-traumatic coagulopathy treatment (PREHO-PLYO). NCT02736812 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT02736812. Accessed 26 May 2019.
Brown JB, Cohen MJ, Minei JP, et al. Goal-directed resuscitation in the prehospital setting: a propensity-adjusted analysis. J Trauma Acute Care Surg. 2013;74:1207–12; discussion 1212–4.
Dula DJ, Wood GC, Rejmer AR, et al. Use of prehospital fluids in hypotensive blunt trauma patients. Prehosp Emerg Care. 2002;6:417–20.
Dutton RP, Mackenzie CF, Scalea TM. Hypotensive resuscitation during active hemorrhage: impact on in-hospital mortality. J Trauma Acute Care Surg. 2002;52:1141–6.
Eckstein M, Chan L, Schneir A, et al. Effect of prehospital advanced life support on outcomes of major trauma patients. J Trauma Acute Care Surg. 2000;48:643–8.
Shackford SR. Prehospital fluid resuscitation of known or suspected traumatic brain injury. J Trauma. 2011;70:S32–3.
Spaite DW, Bobrow BJ, Keim SM, et al. Association of statewide implementation of the prehospital traumatic brain injury treatment guidelines with patient survival following traumatic brain injury: the excellence in prehospital injury care (EPIC) study. JAMA Surg. 2019:e191152.
Hampton DA, Fabricant Lö J, Differding J, et al. Pre-hospital intravenous fluid is associated with increased survival in trauma patients. J Trauma Acute Care Surg. 2013;75:S9–s15.
Guyette FX, Sperry JL, Peitzman AB, et al. Prehospital blood product and crystalloid resuscitation in the severely injured patient: a secondary analysis of the prehospital air medical plasma trial. Ann Surg. 2019. Epub ahead.
Manley G, Knudson MM, Morabito D, et al. Hypotension, hypoxia, and head injury: frequency, duration, and consequences. Arch Surg. 2001;136:1118–23.
Spaite DW, Hu C, Bobrow BJ, et al. Mortality and prehospital blood pressure in patients with major traumatic brain injury: implications for the hypotension threshold. JAMA Surg. 2017;152:360–8.
Sperry JL, Ochoa JB, Gunn SR, et al. An FFP:PRBC transfusion ratio >/=1:1.5 is associated with a lower risk of mortality after massive transfusion. J Trauma. 2008;65:986–93.
Brown JB, Cohen MJ, Minei JP, et al. Debunking the survival bias myth: characterization of mortality during the initial 24 hours for patients requiring massive transfusion. J Trauma Acute Care Surg. 2012;73:358–64; discussion 364.
Drake SA, Holcomb JB, Yang Y, et al. Establishing a regional trauma preventable/potentially preventable death rate. Ann Surg. 2020;271(2):375–82.
Holcomb JB. Transport time and preoperating room hemostatic interventions are important: improving outcomes after severe truncal injury. Crit Care Med. 2018;46:447–53.
Chatfield-Ball C, Boyle P, Autier P, et al. Lessons learned from the casualties of war: battlefield medicine and its implication for global trauma care. J R Soc Med. 2015;108:93–100.
Butler FK, Holcomb JB, Schreiber MA, et al. Fluid resuscitation for hemorrhagic shock in tactical combat casualty care: TCCC guidelines change 14-01--2 June 2014. J Spec Oper Med. 2014;14:13–38.
Malsby RF 3rd, Quesada J, Powell-Dunford N, et al. Prehospital blood product transfusion by U.S. army MEDEVAC during combat operations in Afghanistan: a process improvement initiative. Mil Med. 2013;178:785–91.
Morrison JJ, Oh J, DuBose JJ, et al. En-route care capability from point of injury impacts mortality after severe wartime injury. Ann Surg. 2013;257:330–4.
O’Reilly DJ, Morrison JJ, Jansen JO, et al. Prehospital blood transfusion in the en route management of severe combat trauma: a matched cohort study. J Trauma Acute Care Surg. 2014;77:S114–20.
Shackelford SA, Del Junco DJ, Powell-Dunford N, et al. Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30-day survival. JAMA. 2017;318:1581–91.
Berns KS, Zietlow SP. Blood usage in rotor-wing transport. Air Med J. 1998;17:105–8.
Higgins GL 3rd, Baumann MR, Kendall KM, et al. Red blood cell transfusion: experience in a rural aeromedical transport service. Prehosp Disaster Med. 2012;27:231–4.
Apodaca A, Olson CM Jr, Bailey J, et al. Performance improvement evaluation of forward aeromedical evacuation platforms in Operation Enduring Freedom. J Trauma Acute Care Surg. 2013;75:S157–63.
Sumida MP, Quinn K, Lewis PL, et al. Prehospital blood transfusion versus crystalloid alone in the air medical transport of trauma patients. Air Med J. 2000;19:140–3.
Brown JB, Cohen MJ, Minei JP, et al. Pretrauma center red blood cell transfusion is associated with reduced mortality and coagulopathy in severely injured patients with blunt trauma. Ann Surg. 2014;261:997–1005.
Brown JB, Sperry JL, Fombona A, et al. Pre-trauma center red blood cell transfusion is associated with improved early outcomes in air medical trauma patients. J Am Coll Surg. 2015:797–808.
Smith IM, James RH, Dretzke J, et al. Prehospital blood product resuscitation for trauma: a systematic review. Shock. 2016;46:3–16.
Johansson PI, Stensballe J, Rasmussen LS, et al. A high admission syndecan-1 level, a marker of endothelial glycocalyx degradation, is associated with inflammation, protein C depletion, fibrinolysis, and increased mortality in trauma patients. Ann Surg. 2011;254:194–200.
Ostrowski SR, Johansson PI. Endothelial glycocalyx degradation induces endogenous heparinization in patients with severe injury and early traumatic coagulopathy. J Trauma Acute Care Surg. 2012;73:60–6.
Peng Z, Pati S, Potter D, et al. Fresh frozen plasma lessens pulmonary endothelial inflammation and hyperpermeability after hemorrhagic shock and is associated with loss of syndecan 1. Shock. 2013;40:195–202.
Torres LN, Sondeen JL, Ji L, et al. Evaluation of resuscitation fluids on endothelial glycocalyx, venular blood flow, and coagulation function after hemorrhagic shock in rats. J Trauma Acute Care Surg. 2013;75:759–66.
Zielinski MD, Smoot DL, Stubbs JR, et al. The development and feasibility of a remote damage control resuscitation prehospital plasma transfusion protocol for warfarin reversal for patients with traumatic brain injury. Transfusion. 2013;53(Suppl 1):59S–64S.
Hernandez MC, Thiels CA, Aho JM, et al. Prehospital plasma resuscitation associated with improved neurologic outcomes after traumatic brain injury. J Trauma Acute Care Surg. 2017;83:398–405.
Brown JB, Guyette FX, Neal MD, et al. Taking the blood bank to the field: the design and rationale of the prehospital air medical plasma (PAMPer) trial. Prehosp Emerg Care. 2015;19:343–50.
Moore EE, Chin TL, Chapman MC, et al. Plasma first in the field for postinjury hemorrhagic shock. Shock. 2014;41(Suppl 1):35–8.
Kim BD, Zielinski MD, Jenkins DH, et al. The effects of prehospital plasma on patients with injury: a prehospital plasma resuscitation. J Trauma Acute Care Surg. 2012;73:S49–53.
Holcomb JB, Donathan DP, Cotton BA, et al. Prehospital transfusion of plasma and red blood cells in trauma patients. Prehosp Emerg Care. 2014;19:1–9.
Holcomb JB, Swartz MD, DeSantis SM, et al. Multicenter observational prehospital resuscitation on helicopter study. J Trauma Acute Care Surg. 2017;83:S83–91.
Rijnhout TWH, Wever KE, Marinus R, et al. Is prehospital blood transfusion effective and safe in haemorrhagic trauma patients? A systematic review and meta-analysis. Injury. 2019;50:1017–27.
Jenkins D, Stubbs J, Williams S, et al. Implementation and execution of civilian remote damage control resuscitation programs. Shock. 2014;41 Suppl 1:84–9.
Cardenas JC, Zhang X, Fox EE, et al. Platelet transfusions improve hemostasis and survival in a substudy of the prospective, randomized PROPPR trial. Blood Adv. 2018;2:1696–704.
Holcomb JB, Zarzabal LA, Michalek JE, et al. Increased platelet:RBC ratios are associated with improved survival after massive transfusion. J Trauma. 2011;71:S318–28.
Perkins JG, Cap AP, Spinella PC, et al. An evaluation of the impact of apheresis platelets used in the setting of massively transfused trauma patients. J Trauma. 2009;66:S77–84; discussion S84–5.
Yonge JD, Schreiber MA. The pragmatic randomized optimal platelet and plasma ratios trial: what does it mean for remote damage control resuscitation? Transfusion. 2016;56(Suppl 2):S149–56.
Zielinski MD, Stubbs JR, Berns KS, et al. Prehospital blood transfusion programs: capabilities and lessons learned. J Trauma Acute Care Surg. 2017;82:S70–8.
Espinosa A, Dybvik B, Medby C, et al. Implementation of a protocol for prehospital transfusion of low-titer, leukocyte-depleted whole blood for civilian bleeding patients. Transfus Apher Sci. 2019;58:212–5.
Milford EM, Reade MC. Comprehensive review of platelet storage methods for use in the treatment of active hemorrhage. Transfusion. 2016;56(Suppl 2):S140–8.
Yazer MH, Jackson B, Sperry JL, et al. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. J Trauma Acute Care Surg. 2016;81:21–6.
Dunbar NM, Yazer MH, Biomedical Excellence for Safer Transfusion C, et al. Safety of the use of group A plasma in trauma: the STAT study. Transfusion. 2017;57:1879–84.
McGinity AC, Zhu CS, Greebon L, et al. Prehospital low-titer cold-stored whole blood: philosophy for ubiquitous utilization of O-positive product for emergency use in hemorrhage due to injury. J Trauma Acute Care Surg. 2018;84:S115–9.
Adams PW, Warren KA, Guyette FX, et al. Implementation of a prehospital air medical thawed plasma program: is it even feasible? J Trauma Acute Care Surg. 2019;87(5):1077–81.
Shakur H, Roberts I, Bautista R, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376:23–32.
Morrison JJ, Dubose JJ, Rasmussen TE, et al. Military application of tranexamic acid in trauma emergency resuscitation (MATTERs) study. Arch Surg. 2012;147:113–9.
Myers SP, Kutcher ME, Rosengart MR, et al. Tranexamic acid administration is associated with an increased risk of posttraumatic venous thromboembolism. J Trauma Acute Care Surg. 2019;86:20–7.
Strosberg DS, Nguyen MC, Mostafavifar L, et al. Development of a prehospital tranexamic acid administration protocol. Prehosp Emerg Care. 2016;20:462–6.
Vu EN, Schlamp RS, Wand RT, et al. Prehospital use of tranexamic acid for hemorrhagic shock in primary and secondary air medical evacuation. Air Med J. 2013;32:289–92.
Stein P, Studt JD, Albrecht R, et al. The impact of prehospital tranexamic acid on blood coagulation in trauma patients. Anesth Analg. 2018;126:522–9.
Neeki MM, Dong F, Toy J, et al. Tranexamic acid in civilian trauma care in the California prehospital antifibrinolytic therapy study. West J Emerg Med. 2018;19:977–86.
Boudreau RM, Deshpande KK, Day GM, et al. Prehospital tranexamic acid administration during aeromedical transport after injury. J Surg Res. 2019;233:132–8.
Napolitano LM. Prehospital tranexamic acid: what is the current evidence? Trauma Surg Acute Care Open. 2017;2:e000056.
Inaba K, Karamanos E, Lustenberger T, et al. Impact of fibrinogen levels on outcomes after acute injury in patients requiring a massive transfusion. J Am Coll Surg. 2013;216:290–7.
Schochl H, Schlimp CJ, Maegele M. Tranexamic acid, fibrinogen concentrate, and prothrombin complex concentrate: data to support prehospital use? Shock. 2014;41(Suppl 1):44–6.
Stinger HK, Spinella PC, Perkins JG, et al. The ratio of fibrinogen to red cells transfused affects survival in casualties receiving massive transfusions at an army combat support hospital. J Trauma. 2008;64:S79–85; discussion S85.
Schochl H, Nienaber U, Hofer G, et al. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Crit Care. 2010;14:R55.
Yamamoto K, Yamaguchi A, Sawano M, et al. Pre-emptive administration of fibrinogen concentrate contributes to improved prognosis in patients with severe trauma. Trauma Surg Acute Care Open. 2016;1:e000037.
Transfusion of red blood cells tranexamic acid, and fibrinogen concentrate for severe trauma hemorrhage at pre-hospital phase of care (PRETIC). NCT03780894 2018. Available at: https://clinicaltrials.gov/ct2/show/NCT03780894. Accessed 26 May 2019.
Joseph B, Hadjizacharia P, Aziz H, et al. Prothrombin complex concentrate: an effective therapy in reversing the coagulopathy of traumatic brain injury. J Trauma Acute Care Surg. 2013;74:248–53.
Zeeshan M, Hamidi M, Kulvatunyou N, et al. 3-Factor Vs. 4-Factor PCC in coagulopathy of trauma: four is better than three. Shock. 2019;52(1):23–8.
Zeeshan M, Hamidi M, Feinstein AJ, et al. 4-Factor prothrombin complex concentrate is associated with improved survival in trauma related hemorrhage: a nationwide propensity matched analysis. J Trauma Acute Care Surg. 2019;87(2):274–81.
Early administration of prothrombin concentrate complex in patients with acute hemorrhage following severe trauma (PROCOAG). NCT03218722 2018. Available at: https://clinicaltrials.gov/ct2/show/NCT03218722. Accessed 26 May 2019.
Lendrum RA, Kotze JP, Weaver AE. Pre hospital administration of prothrombin complex concentrate in the head injured patient, a service evaluation. Scand J Trauma Resusc Emerg Med. 2013;21:S12. https://doi.org/10.1186/1757-7241-21-S1-S12. eCollection 2013.
Lendrum RA, Kotze JP, Lockey DJ, et al. Case studies in prehospital care from London HEMS: pre-hospital administration of prothrombin complex concentrate to the head-injured patient. Emerg Med J. 2013;30:247–8.
Vines C, Tesseneer SJ, Cox RD, et al. Air ambulance delivery and administration of four-factor prothrombin complex concentrate is feasible and decreases time to anticoagulation reversal. Acad Emerg Med. 2018;25:33–40.
Spinella PC, Perkins JG, Grathwohl KW, et al. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66:S69–76.
Condron M, Scanlan M, Schreiber M. Massive transfusion of low-titer cold-stored O-positive whole blood in a civilian trauma setting. Transfusion. 2019;59:927–30.
Friedman C. SAFD medics now doing blood transfusions in ambulances, saving lives with whole blood 2018. Available at: https://www.ksat.com/news/safd-medics-now-doing-blood-transfusions-in-ambulances-saving-lives-with-whole-blood. Accessed 26 May 2019.
Inaba K. Freeze-dried plasma. J Trauma. 2011;70:S57–8.
Martinaud C, Civadier C, Ausset S, et al. In vitro hemostatic properties of French lyophilized plasma. Anesthesiology. 2012;117:339–46.
Arav A, Natan D. Freeze drying (lyophilization) of red blood cells. J Trauma. 2011;70:S61–4.
Cap AP, Perkins JG. Lyophilized platelets: challenges and opportunities. J Trauma. 2011;70:S59–60.
Gauss T, Maegele M, Harris T. Is pre-hospital coagulation management in trauma feasible? ICU Manag Pract. 2018;18:97–101.
Glassberg E, Nadler R, Gendler S, et al. Freeze-dried plasma at the point of injury: from concept to doctrine. Shock. 2013;40:444–50.
Shlaifer A, Siman-Tov M, Radomislensky I, et al. Prehospital administration of freeze-dried plasma, is it the solution for trauma casualties? J Trauma Acute Care Surg. 2017;83:675–82.
Sunde GA, Vikenes B, Strandenes G, et al. Freeze dried plasma and fresh red blood cells for civilian prehospital hemorrhagic shock resuscitation. J Trauma Acute Care Surg. 2015;78:S26–30.
Garrigue D, Godier A, Glacet A, et al. French lyophilized plasma versus fresh frozen plasma for the initial management of trauma-induced coagulopathy: a randomized open-label trial. J Thromb Haemost. 2018;16:481–9.
Buckley L, Gonzales R. Challenges to producing novel therapies – dried plasma for use in trauma and critical care. Transfusion. 2019;59:837–45.
US Food and Drug Administration. FDA takes action to support American military personnel by granting an authorization for freeze-dried plasma product to enable broader access while the agency works toward approval of the product 2018. Available at: https://www.fda.gov/news-events/press-announcements/fda-takes-action-support-american-military-personnel-granting-authorization-freeze-dried-plasma. Accessed 26 May 2019.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Deeb, AP., Brown, J.B. (2021). Prehospital Resuscitation. In: Moore, H.B., Neal, M.D., Moore, E.E. (eds) Trauma Induced Coagulopathy. Springer, Cham. https://doi.org/10.1007/978-3-030-53606-0_29
Download citation
DOI: https://doi.org/10.1007/978-3-030-53606-0_29
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53605-3
Online ISBN: 978-3-030-53606-0
eBook Packages: MedicineMedicine (R0)